Abstract
During the past few years, the Internet has started to change lifestyles and affect all life domains, including working life. It is also increasingly used for targeting mental health issues. The “application of information technology in mental and behavioral health” (Andersson G, Riper H, Carlbring P (2014) Editorial: Introducing Internet interventions—a new open access journal. Internet Intervent 1:1–2) is becoming common in health-care; interventions have already been incorporated into routine care in countries such as the Netherlands, Sweden, the UK, Australia, and the USA. As a next step, Internet interventions in the area of occupational health are progressively emerging. They may offer an evidence-based, cost-effective, and convenient way of promoting workers’ mental health on a large scale. Currently, Internet interventions for workers are the most promising approach in the field of occupational e-mental health. The evolution of occupational e-mental health is embedded in interdisciplinary research, practice, and policy. In the first section of this chapter, the origins of occupational e-mental health will be outlined and a definition proposed. Following this, different approaches to occupational e-mental health will be described and their potentials elucidated. A comparison between Internet interventions and traditional stress-management trainings will provide further insights into the design and characteristics of the most elaborated approach in occupational e-mental health. Subsequently, various Internet training programs will be introduced and the evidence for their efficacy summarized. Finally, important topics for further research and implementation will be outlined.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
In 1950, the International Labor Organization and World Health Organization defined the aims of occupational health as “the promotion and maintenance of the highest degree of physical, mental and social well-being of workers”. Later, in the 1970s, the psychosocial aspects of work increasingly gained interest, attention being paid to the consequences of occupational stress regarding safety issues, health, and mental health. In the late 1980s and the 1990s, efforts were made to bridge the gap between the disciplines of occupational health and psychology. The potential of psychology to contribute to occupational health was described as “industrial/organizational psychology provides expertise in work organization and job design, and the fields of health psychology and clinical and counseling psychology provide expertise on stress, health and mental health” (Sauter et al. 1999). As a result, a new discipline was established: occupational health psychology. Cox et al. (2000, p. 101) stated that occupational health psychology is “the contribution of applied psychology to occupational health”. Similarly, Sauter et al. (1999) referred to the definition of occupational health psychology proposed by the American National Institute for Occupational Safety and Health as “the application of psychology to improving the quality of worklife, and to protecting and promoting the safety, health and well-being of workers” (National Institute for Occupational Safety and Health 2005). Houdmont and Leka (2010) emphasized the applied, evidence-based, and multidisciplinary character of occupational health psychology and its focus on interventions as particularly desirable characteristics.
The term e-health had come into use by the year 2000 and has since become widely prevalent (Pagliari et al. 2005). Although there is no consensus about its definition (Oh et al. 2005; Pagliari et al. 2005), e-health can be summarized as “the use of emerging information and communications technology, especially the Internet, to improve or enable health and healthcare” (Eng 2001, p. 8) and “in a broader sense, the term characterizes not only a technical development, but also a new way of working, an attitude, and a commitment for networked, global thinking, to improve health-care locally, regionally, and worldwide by using information and communication technology” (Eysenbach 2001). E-mental health was defined by Christensen et al. (2002, p. 17) as a “form of e-health which deals with mental health and mental health disorders”.
The term occupational e-mental health combines the trajectories of occupational health psychology and e-mental health. In general, occupational e-mental health can be described as the application of e-mental health in the specific life domain of work; its aims include improving the quality of working life and protecting and promoting the safety, health, and well-being of workers. Adopting a more detailed definition of e-mental health proposed by Riper et al. (2010) and adapting it to the working-life context, we define occupational e-mental health as a generic term that describes the use of information and communication technology to deliver psycho-education, health risk assessment, work-place health promotion, preventive interventions (universal, selected, or indicated), treatment, relapse prevention, and return-to-work assistance for the mental health of workers as well as to improve occupational health-care delivery, professional education (e-learning), and online research in the field of occupational mental health. Thus, occupational e-mental health covers person- and organization-focused approaches. Beyond mental health, the more generic term “occupational e-health” refers to the promotion and maintenance of the highest degree of physical, mental, and social well-being of workers using information and communications technology.
Currently, major challenges for occupational medicine and occupational psychology concerning mental health include: (1) the prevention of ill health and sick leave (physical and mental) caused by adverse psychosocial work conditions (“work stress”); (2) provision of fast and adequate health service to employees who develop mental health problems that become apparent in the work-place; and (3) providing support for those who return to work after prolonged absences because of mental disorders. For prevention, the central tools are mental health risk assessment and subsequent interventions such as redesign of work organization and tasks or stress-management training; however, successfully achieving these requires considerable effort. Provision of fast and adequate health services to persons with mental health problems is a challenge to the entire health system and especially to responsible stakeholders in enterprises; prolonged illness without appropriate diagnosis and treatment may cause presenteeism, difficulties at work, unnecessarily long sick leave, and job losses, all of which can be heavy burdens for employers and employees. As for early treatment, successful return to work helps to prevent job loss and early retirement because of mental disorder, which are one of the most frequent reasons for prematurely quitting work life. The emerging resource of occupational e-mental health may provide solutions to these challenges.
2 Current Approaches and Upcoming Trends in Occupational e-Mental Health
The proposed definition of occupational e-mental health covers a wide variety of intervention approaches including Internet-based interventions; m-health or mobile health technologies; social media; serious gaming and gamification; v-health or virtual reality; and providing care via videoconferencing, telephone, or instant messaging (cf. Mohr et al. 2013). We will now describe these approaches in further detail (cf. Fig. 1).
2.1 Internet Interventions
So far, most research has been conducted in the field of Internet interventions targeting mental health outcomes. Ritterband and Thorndike (2006) described Internet interventions as “typically behaviorally or cognitive-behaviorally-based treatments that have been operationalized and transformed for delivery via the Internet. Usually, they are highly structured; self- or semi-self-guided; based on effective face-to-face interventions; personalized to the user; interactive; enhanced by graphics, animations, audio, and possibly video; and tailored to provide follow-up and feedback”. This definition provides an insight into the typical features employed in Internet interventions and differentiates Internet interventions from websites providing information and education. Guidance is usually provided by a health-care professional. Most Internet interventions are designed for desktop computers.
2.2 Mobile Technologies
Mobile technologies have the potential to introduce interventions into everyday life. Because most people carry mobile or smartphones with them and these devices are widely available, mobile technologies can deliver “ecological momentary interventions” under real-world and real-time conditions to individuals on a very large scale (Heron and Smyth 2010). Interventions using mobile technologies can be delivered as stand-alone programs or in combination with desktop-optimized Internet interventions. Combined or hybrid formats are particularly useful for the components of interventions that focus on ecological moment-to-moment assessment and interventions such as regular mood or behavior assessments, diaries, frequent exercises, or messages (e.g., reminding or encouraging messages). Moreover, built-in devices (e.g., cameras), sensors (e.g., GPS), or wearables (e.g., glasses, watches) connected to smartphones may also play roles in such interventions. Finally, traditional devices such as accelerometers, actigraphy devices, and blood pressure or heart rate monitors may also be connected indirectly to the Internet via smartphones. Moreover, such devices can also have direct Internet access, a phenomenon that has been described as the Internet of Things. While the dynamic in the development of mental health smartphone applications has been extraordinary, empirical evidence for its efficacy is very limited, although promising (Fiordelli et al. 2013). Notably, the distinction between Internet-based and mobile health interventions is not clear-cut and should be regarded as in a heuristic stage. We believe that interventions delivered via mobile devices that are connected to the Internet such as tablet computers or smartphones may also be labeled Internet-based interventions.
2.3 Social Media
Social media focus on the exchange of content created by its users in the context of social networks, discussions, or support groups. Social media can be a component of Internet-based interventions that enables participants to give each other feedback and provide encouragement. Although there is some evidence that support groups moderated by a health-care professional can be beneficial (Winzelberg et al. 2003), it is possible for non-moderated groups to have no or even negative effects because of social contagion (Takahashi et al. 2009). In addition to their use as a component of Internet-based interventions, social media (namely, Facebook, Twitter, WhatsApp) may also be useful tools for health communication and to increase the reach and efficiency of (occupational) health services (Capurro et al. 2014; Moorhead et al. 2013).
2.4 Serious Gaming and Gamification
Games for serious purposes or serious games related to e-health are “digital games with the purpose to improve an individual’s knowledge, skills, or attitudes in the ‘real’ world” (Graafland et al. 2014). This approach is based on the idea of using “entertaining games with non-entertainment-related goals” such as the promotion of mental health (Mohr et al. 2013). A related approach is to identify the ingredients that make games attractive and use these features to increase the enjoyableness, reach, and efficacy of Internet interventions or smartphone applications. Generally, gamification has been defined as “the use of game design elements in non-game contexts” (Deterding et al. 2011). Some of these design elements are rewards, badges, leaderboards, points and levels-systems, challenges and quests, specific goals, social engagement loops and onboarding, and the provision of cover-stories (Zichermann and Cunningham 2011).
2.5 V-Health or Virtual Reality
The potential of v-health approaches for mental health was first successfully investigated in virtual reality exposure therapy for anxiety disorders (e.g., social phobia, fear of flying) (Opriş et al. 2012). Virtual reality exposure has been defined by Parsons and Rizzo (2008) as a method “in which users are immersed within a computer-generated simulation or virtual environment (VE) that updates in a natural way to the user’s head and/or body motion.” When a user is immersed in a VE, they can be systematically exposed to specific “feared” situations and learn to apply new behavioral skills. Regarding occupational health, an avatar-based virtual environment “Family of Heroes” has been found to be an effective tool for helping family members to motivate their veterans to seek help from Veterans Administration when those veterans are exhibiting evidence of post-traumatic stress disorder, traumatic brain injury, depression, or suicidal ideation (Albright et al. 2012).
2.6 Videoconferencing, Telephone, and Instant Messaging
Real-time or synchronous communication is a shared characteristic of videoconferencing (e.g., Skype, Google Hangout), telephoning, or instant messaging. Compared with in-person or face-to-face settings, videoconferencing eliminates some elements of nonverbal communication (e.g., olfactory or haptic cues); however, it does provide restricted but similar visual information. Talking to someone on the telephone removes the visual channel from communication and instant messaging is restricted to written material. There is a growing body of evidence that videoconferencing is an effective mode of delivering psychotherapeutic care to patients in their own homes, which is particularly relevant for persons staying or living in remote areas (including military personnel and people in civil war zones or developing countries) or for providing support and expertise from specialized health-care professionals to remote clinics (Hilty et al. 2013; Richardson et al. 2009). Occupational health videoconferencing has successfully been used to treat mental disorders in veterans (Hilty et al. 2013). Telephone-delivered psychotherapy for treating veterans reportedly yields mixed results (Mohr et al. 2011); however, telephone-delivered psychotherapy is generally effective in other settings (Mohr et al. 2008).
Most research in the field of occupational e-mental health has been conducted with Internet-based trainings as defined by Ritterband and Thorndike (2006). Accordingly, the following sections will focus on this approach. As to the other approaches just described, the immediacy and wide reach of m-health and social media make their potential obvious; developing applications in this area is a popular topic and researchers have begun to employ stronger research designs. Likewise, the potential benefits of serious gaming and v-health are apparent; however, the high costs of developing virtual reality or high-quality games are currently a barrier to widespread research and implementation that may be overcome in the next few years with the development of more affordable solutions. Videoconferencing and telephone-delivered health-care have already proven their potential. However, for technical reasons it has only been in the last few years that video- and telephone conferencing has begun to be Internet-based and therefore to qualify as a form of e-mental health. In the future, the aforementioned approaches are expected to be increasingly combined and integrated. For example, incorporation of smartphone applications, social media features, or videoconferencing into Internet-based trainings is feasible and promising. Likewise, boundaries become blurred as responsive web design allows delivery of the same interventions via mobile devices such as smartphones and via desktop computers (e.g., Dagöö et al. 2014).
3 Characteristics of In-Person and Internet Interventions
In this section, we compare the characteristics of traditional stress-management trainings with those of Internet-based trainings for promoting mental health in workers (c.f. Lehr et al. 2014).
Stress-management trainings are often based on cognitive behavioral therapy, which is the most common intervention used in occupational health to promote psychological well-being. Several meta-analyses have demonstrated the effectiveness of stress-management trainings with regard to stress, depression, and anxiety (Martin et al. 2009; Richardson and Rothstein 2008; van der Klink et al. 2001; Bhui et al. 2012). As outlined in Sect. 2, most research in occupational e-mental health has targeted Internet-based interventions as opposed to other approaches. Accordingly, Internet-based and face-to-face training formats can be considered the standard approaches in the online and offline worlds, respectively.
Over the past decade, well-established training concepts have been adopted and converted into Internet-based formats. Internet-based trainings are usually based on the same theoretical background and offer the same content as traditional trainings. Moreover, traditional and Internet-based trainings both require investment of time and challenge working people to change their health behavior or stress-related cognitions in spite of their daily, sometimes heavy, workload. In addition to these shared fundamentals, both training formats have their own specific characteristics.
Traditional trainings are typically face-to-face or in-person interventions (Table 1) with groups of 10–20 participants led by one or two health-care professionals.
The trainings usually comprise between four and ten sessions. Although weekly sessions are usually recommended, trainings are often conducted in block courses as single events. Participation in traditional trainings requires participants to be willing to work in groups on their personal health issues. In groups aimed at addressing personal stress management, participants are expected to disclose personal information to other group members to enable them to work on their individual strengths and weaknesses. A group atmosphere can discourage some individuals, particularly those with social anxiety, from opening up or participating. However, groups can offer social support, which may increase motivation for participation, adherence, and effectiveness. The group setting provides opportunities for interactive training techniques for promoting social skills, such as role-playing. Additionally, group members can provide direct feedback. With emotionally demanding exercises such as imagination exercises, trainers can provide participants with immediate support. Verbal sharing of personal experiences in group settings also requires a certain degree of verbal competence and affinity. Regarding organizational factors, participation in group trainings requires fixed dates and times over several weeks or block seminars. Additionally, extra time for traveling by private or public transportation to the venue has to be taken into account. The availability of such trainings may be limited, especially in rural areas. Furthermore, trainings often take place in closed groups, which means that groups cannot be joined at any time and potential participants must wait for the next training course to begin.
In contrast with the group setting of traditional trainings, Internet trainings are usually conducted individually. The interventions characteristically comprise five to ten training modules that can be completed weekly. This procedure underlines the necessity of performing exercises repeatedly and regularly. Each module is usually designed to be completed in approximately 30–60 min; the exercises within a module may all be performed at once or distributed over some time. Some interventions are pure self-help trainings without any support from a health-care professional (unguided self-help training). Self-help trainings in particular have the potential to be disseminated on a large scale and to be available at any time. Hence, training can be started when desired and no waiting time is necessary. The training can be conducted anywhere that is convenient, with Internet access being the only precondition. Pure self-help trainings most appropriately compared with traditional self-help books whereas guided trainings provide the possibility of contacting a health-care professional, who is sometimes referred to as an e-coach, via email or a messaging system. The e-coach guides the participants through the training, answers questions, and provides support with the exercises. Typically, this support is provided for 15–30 min after every session. Alternatively, with coaching-on-demand formats, participants receive support only when requested. Formats that require a higher coaching intensity, similar to the amount of time needed in psychotherapy, may also be used. The greater the guidance provided, the more personnel resources are needed, which limits the reach and immediacy of access to Internet training.
Interactive elements such as audio and video clips are often included. Furthermore, online diaries offer participants the opportunity to monitor their own health and training progress. Despite the increased use of multimedia elements, Internet-based interventions are often characterized as being largely text-based. Written exercises require substantial reading and writing skills and also an affinity with these communication channels. The lack of nonverbal signals may cause misunderstandings in asynchronous communications that can only be dealt with after a time delay. Likewise, only delayed rather than immediate support may be available for emotional crises that are, for example, triggered by certain exercises. Unless monitoring is part of the training, the participants must initiate sharing of information on, for example, symptom deterioration; alternatively, the e-coach can ask for such information at regular intervals.
Another specific characteristic of Internet-based interventions is that participants can work at their own pace and review materials and relevant topics as often as they wish. Because their experiences with exercises are in written form, the participants can also easily access their previous responses. Individuals can decide according to their personal preferences or habits on the extent to which they will self-disclose and self-reflect during the training process. However, this may also lead to avoidance of certain topics.
In general, there is a low access threshold for participating in Internet-based trainings. However, easy-in also means easy-out; the threshold for dropping out is also low. Hence, specific measures for fostering adherence, such as gamification, may be required. Anonymity is an important characteristic of Internet-based trainings, especially regarding their low threshold for access. Anonymity is often regarded as an advantage of Internet trainings because it facilitates engagement in topics associated with feelings of shame or guilt (e.g., alcohol consumption for managing stress). Although Internet trainings may appear to be completely anonymous, the degree of anonymity actually depends on several factors. These include individual habits in handling personal data and ensuring data security, the provision of data security by the Internet or training provider or both, and legal or illegal activities by third parties who may read, save, or pass on data. These possibilities may elicit fear and discourage some individuals from participating.
Table 1 summarizes the characteristics of Internet and traditional trainings. However, because of the rapidity of technological developments, these characteristics are constantly changing and only reflect present circumstances. They should be regarded as an orientation to determining the best match between the preferences, needs, and skills of participants and training characteristics.
4 Internet Interventions for Workers: A Review of Concepts and Evidence of Efficacy
The efficacy of Internet-based interventions has so far mainly been investigated in the field of psychotherapy. Internet interventions have proven to be effective in the reduction of depression (Richards and Richardson 2012) and anxiety (Cuijpers et al. 2009; Haug et al. 2012), and have also demonstrated substantial effects in reducing sleep disorders (Cheng and Dizon 2012).
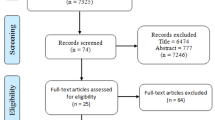
Several Internet interventions targeting mental health in workers have also been investigated in randomized controlled trials, which are regarded as the gold standard for investigating efficacy. We will now describe the content of those trainings and their basic results.
Ruwaard et al. (2007) evaluated an email-based training for stress reduction in the work-place in a sample of 342 individuals. The training consisted of the following seven modules: self-monitoring and perception of stress symptoms; relaxation; rumination, worrying, and coping with negative thoughts; positive self-verbalization; social competence training; time management; and relapse prevention. On average, each participant received 5 h of coaching. Compared with the wait-list control subjects, participants in the intervention group showed significantly greater improvements in stress, depression, anxiety, and burnout.
Hasson et al. (2005) evaluated a stress toolbox in 303 employees in the information technology and media sector. Participants in the control group had access to an online stress diary with feedback and received information concerning stress and health whereas the intervention group underwent a program that offered exercises covering relaxation, sleep enhancement, cognitive restructuring, time management, regulation of emotion, and self-esteem. Moreover, a chat was available to participants of the intervention group. These investigators used the following biological stress markers as indicators of efficacy: chromogranin A, dehydroepiandrosterone, neuropeptide Y, and tumor necrosis factor-α. The intervention group showed significantly better results for all biological markers.
Cook et al. (2007) investigated a comprehensive health promotion program that included stress management, nutrition/weight management, and fitness/physical activity. The participants were 419 employees of a human resources company. Information and guidance was provided on a website for 3 months. The web-based program was completely self-guided, highly interactive, and used videos, audio, and graphics. Participants in the web-condition were compared on a variety of outcome measures with an active control group that received high-quality print material on the same topics. The subjects in the web-condition improved more in the areas of diet and nutrition than did those in the print-condition; however, there were no significant differences between the groups in stress reduction and improvements related to physical activity. Adherence to the intervention was generally poor, particularly for stress management and physical activity. However, the authors identified a dose-response relationship: there was a significant relationship between the number of times participants accessed the web program and the strength of effect across the dependent measures.
A prevention program for stress, depression, anxiety, and substance abuse was examined by Billings et al. (2008) in a sample of 309 employees. The intervention group had 3 months’ access to a self-help program that was audio-narrated and incorporated videos and graphics. The training was based on different modules, such as goal setting, problem-solving, identification and restructuring of negative thoughts, and time management. Compared with a wait-list control group, the investigators found a small reduction in stress but no effects on depression or anxiety. However, the intervention group showed a more positive attitude toward seeking psychological help for crises.
Yamagishi et al. (2008) evaluated a training course for nursing staff based on the assumption that unfavorable occupational identity is a key source of stress. Its effectiveness was examined in nursing staff (N = 60). The training consisted of the following four modules: definition of occupational identity; assumptions regarding participants’ own occupational identity, characteristics of nursing staff, and alternative careers; and management and planning of occupational identity. They found no differences between the intervention and control groups regarding health benefits.
Abbott et al. (2009) developed a 10-week online resilience training and evaluated the intervention in 53 sales managers. The goal of the training was to learn the following seven core competences with the aim of improving resilience: regulation of emotion, impulse control, optimism, analysis of causality of problems, empathy, self-efficacy, and improvement in positive aspects of life such as close contact with other people or facing challenges. Only seven people completed the training, which may explain the absence of significant intervention effects.
Geraedts et al. (2014a, b) investigated the effects of the Happy@Work training in employees with symptoms of depression. The intervention consisted of six sessions and comprised a problem-solving training and additional features adopted from cognitive therapy. The study included 231 employees who received support from an e-coach. Although the training group showed considerable improvements in depressive symptoms, the investigators identified neither short- nor long-term effects (after 12 months) compared with care as usual (Geraedts et al. 2014a, b). Notably, an economic evaluation of this clinic trial showed that the majority of costs were attributable to presenteeism; however, the intervention was not considered to be cost-effective or cost-saving for the employer (Geraedts et al. 2015).
Ebert, Lehr et al. (2014) evaluated a similar problem-solving training in a study of 150 schoolteachers with symptoms of depression. The intervention comprised five sessions of problem-solving training and participants received guidance from an e-coach. Compared with a wait-list control group, participants showed a moderately greater reduction in depressive symptoms and this improvement remained stable over 6 months. Similar effects were observed in general self-efficacy and work-specific self-efficacy. Several predictors of training efficacy such as age, sex, weekly working hours, experience with therapy or training, emotional exhaustion, and general self-efficacy were tested; however, these variables did not predict change in severity of depression (Junge et al. 2015).
A recreation training designed to improve restorative sleep, mental detachment from work, and recreational activities was developed by Thiart, Lehr et al. (2015). The training consisted of six lessons and employed established methods from cognitive behavioral therapy for managing insomnia such as sleep restriction, stimulus control, and hygiene interventions, as well as techniques targeted at reducing rumination such as a gratitude diary and the promotion of recreational activities. In a study of 128 teachers receiving personal support from an e-coach, the investigators found that the training substantially reduced sleep problems and fostered recreational behavior and mental detachment from work. The beneficial effects were maintained over 6 months. Only 10 % of the participants had had prior experiences with other occupational mental health trainings, indicating that this training reached workers who had not been reached by traditional training formats. In a replication study Ebert et al. (2015) found similar effects for the unguided version of the recreation training. Moreover, Thiart et al. (in press) conducted the first economic evaluation of an internet intervention from an employer's perspective and found that the focusing on sleep improvement using the recreation training may be a cost-effective strategy in occupational health care.
Heber et al. (2016) evaluated a web-based and mobile stress-management training course for employees. The training consisted of seven sessions and was based on problem-solving and emotion-regulation techniques. The 256 participants were supported by an e-coach and could receive text messages on their mobile phones alongside a web-based intervention that introduced training exercises and motivational support in real life and real time. A considerable difference between the intervention and a wait-list control group was found for reduction of perceived stress post-test and at a 6-month follow-up as there is new evidence: Significant medium to large between-group effects were also found for relevant secondary outcomes concerning mental health (e.g., depression, anxiety), work-related health (e.g., emotional exhaustion), and stress-related skills (e.g., emotion-regulation competencies).
Wolever et al. (2012) developed a mindfulness-based training for employees that focused on work-related stress, work-life balance, and self-care. “Similar effects for primary and secondary outcomes were found in a replication study investigating the unguided self-help version of the same intervention (Ebert et al. 2016).” The training comprised 1-h sessions over 12 weeks and daily exercises. The same training was offered in two different formats; namely, a traditional local group training and a virtual group training over the Internet with real-time bidirectional communication. Ninety-six individuals took part in the study: the investigators found no differences between the virtual and in-person training formats. When they compared the Internet training group with a wait-list control group, they found a medium to large effect on stress reduction.
Feicht et al. (2013) evaluated a 7-week happiness intervention in 147 employees of a health insurance company. The intervention was based on principles of positive psychology and mindfulness and included components such as improving social relationships, mindfulness exercises, identification and use of personal strengths, and a happiness and gratitude diary. Participants received a weekly email at work explaining the intervention topic (10–15 min) and were asked to perform the exercises at home. Compared with a wait-list control group, the investigators found a moderate effect on reduction of subjective experience of stress post-test. They also found large between-group effects on happiness, satisfaction, and quality of life in favor of the intervention group at post-test and 4 weeks after completion of training. They found no differences between the groups on objective physiological measures (serum cortisol and alpha-amylase concentrations).
Bolier et al. (2014) examined the effects of a workers’ health surveillance module including tailored feedback and an online intervention in 366 nurses and allied health professionals. After an initial screening, they offered participants tailored advice about their mental health and an online intervention in the following areas: well-being and mental fitness, depression, stress, panic, and alcohol. Compared with a wait-list control group, positive mental health and psychological well-being were significantly enhanced in the intervention group at post-test and follow-up. No significant effects were found for work engagement. However, because the uptake of the interventions was lower than expected, the authors suggested that the positive effects may have been attributable to the increased awareness caused by the screening process and tailored, personalized advice.
Ly et al. (2014) evaluated the effectiveness of a smartphone-based training in a sample of 73 mid-level managers. The 6-week training was based on the principles of Acceptance Commitment Therapy and incorporated mindfulness exercises to help participants focus on the present and reduce multitasking, avoid equating thoughts about a situation with reality, learn to accept unpleasant thoughts and emotions without avoidance, and identify their own values and translate them into action goals. The investigators found moderate positive differences between the intervention and wait-list control groups.
Kawakami et al. (2006) developed an unguided online training for supervisors. The training comprised the following nine sessions: a general introduction; the importance of mental health in the work-place; official guidelines for promoting mental health in the work-place and the role of the supervisor; listening to and advising subordinate workers and the use of mental health services; support for workers who return to work after sick leave; improving the work environment regarding stress prevention; awareness of and coping with stress; knowledge about mental health; and a final summary. The investigators randomly assigned 46 supervisors to either training or non-training work-places. With regard to job stressors, social support received by distressed workers did not differ between trained (N = 81) and untrained (N = 108) supervisors. However, there were some small favorable effects for work autonomy and friendly atmosphere in the work-place in favor of work-places with trained supervisors.
Overall, Internet trainings for workers have been investigated using a variety of health outcomes ranging from biological stress markers to self-reported stress, depression, or expert-diagnosed insomnia. Participants have been recruited from within companies and from the general population. Some studies have applied almost none and others rigorous inclusion criteria; some have used a universal and others a selected or indicated approach to prevention. Some studies have focused on specific occupational groups or settings whereas others have been designed for a broader range of participants. Trainings have also differed in length, theoretical background, and the number of different skills or coping strategies addressed. Finally, support from a personal coach was provided in some trainings, whereas others were designed as pure self-help trainings.
In summary, it can be concluded that Internet trainings for workers are feasible. However, findings concerning efficacy are heterogeneous, varying from reportedly having small or non-significant effects through to significant effects. The availability of support and guidance from health-care experts appears to be one important explanation for differences in efficacy. However, there are currently far too few studies to identify the key factors associated with effective Internet trainings.
5 Agendas for Future Research
Occupational e-mental health is still in its infancy. This section outlines topics that might be important for accelerating its growth. Some of these refer to general challenges in e-mental health research (cf. Mohr et al. 2013), whereas others are specific with regard to the occupational field.
5.1 Creating a Critical Mass of Efficacy Research
Compared with the amount of research into, and experiences with, integration of psychotherapeutic interventions into routine health-care, particularly regarding the treatment of depression and anxiety, there is scant evidence for the efficacy of occupational e-mental health. Few randomized controlled trials investigating the efficacy of Internet interventions in this field have been conducted. Because a critical mass of research is needed to ascertain the potential of occupational e-mental health and identify blind alleys and fruitful routes, the number of studies employing strong research designs must increase substantially. The research described in Sect. 4 indicates that Internet interventions in particular have the potential to be effective; however, there is insufficient current evidence to draw general conclusions. In addition to investigating general efficacy, it is also importance to determine how these interventions work, and for whom. For example, research could focus on the identification of subgroups for which training is more successful (i.e. Junge et al. 2015). Comparison of Internet-based and traditional trainings to identify the characteristics that determine why traditional trainings work better for some people and Internet-based trainings work better for others would also be useful (Wolever et al. 2012).
5.2 Investigating Reach, Adoption, and Adherence
The potential reach and availability of Internet and m-health interventions is huge because increasing numbers of people own computers with Internet access or use smartphones, or both. This is often seen as a major advantage of e-mental health over traditional health-care. However, evidence concerning the actual reach of public health interventions via the Internet is very limited and less optimistic. Research is needed to better characterize the actual reach and investigate better strategies for increasing acceptance and utilization rates (Bennett and Glasgow 2009). Greater effort and more creative methods are needed to engage males and less educated people, these groups being characteristically under-represented. Especially regarding occupational health, it is important to recommend that companies adopt e-mental health and to investigate factors that influence its adoption. Moreover, even when workers have been reached, Internet interventions are often plagued by high attrition rates. The advantage of easy-in, particularly in self-help trainings, is counter-balanced by the problem of easy-drop-out. Several methods for improving adherence have been proposed, including managing expectations prior to commencing an intervention, tailoring the content to the users’ situations, enhancing usability, providing positive feedback, adding personal support (via email, phone, or other media), offering incentives, and applying gaming elements to make the intervention more engaging (Bennett and Glasgow 2009; Mohr et al. 2013).
5.3 Applying Theoretical Frameworks for Occupational Stress in Training Design
Traditional and third-wave cognitive behavioral therapies are often used as the theoretical background for the trainings described here, reflecting the clinical and therapeutic origins of practice and research in the field of Internet interventions. However, with few exceptions, these trainings have not been designed based on a theoretical framework for occupational stress. The recreation training (Thiart, Lehr et al. 2015) described in Sect. 4 is one example of a training whose content is based on a theoretical model of recreation proposed by Lehr et al. (2012). This model claims that recreational activities, mental detachment from work, and restorative sleep are the three core components of recovery from work-related stress. Designing interventions that incorporate the most prominent models of occupational stress would necessitate that such a training cover the topics of coping with effort–reward imbalance situations (Siegrist 2002) or dealing with work-places characterized by low decision latitude (i.e., autonomy and control) in combination with high work demands (Karasek and Theorell 1990). Applying other fruitful frameworks such as the “stress as offense to self” approach (Semmer et al. 2007) to the design of a training could result in trainings that focus on strengthening self-esteem (i.e. through success experiences) or protecting the self against offenses in the work-place such as disrespectful social interactions, illegitimate tasks (i.e., unreasonable or unnecessary tasks), and illegitimate stressors (i.e., pressure to use inadequate tools to accomplish work tasks). However, even traditional stress-management interventions have rarely been designed according to a well-established theory of occupational stress such as the effort–reward imbalance model (i.e., Limm et al. 2011). Applying theoretical frameworks of occupational stress can help to design trainings that specifically target problems that are relevant to participants, thus making the trainings more tailored and sensitive to their work situations. Moreover, application of evidence-based frameworks ensures that trainings focus on topics that have been proven to be associated with mental health.
5.4 Considering Environmental and Organizational Factors
Research on delivering psychotherapy using the Internet has focused almost exclusively on individual factors. However, occupational health has a much broader arena and should take into account the creation of healthy working conditions and the responsibility of employers to ensure workers’ health. As Semmer (2006, p. 515) has emphasized, “the promotion of health and the prevention of health problems should predominantly focus on creating a work environment that does not induce an undue amount of stress and that compensates for unavoidable stresses by characteristics such as high control and high rewards”. The above cited review of Richardson and Rothstein (2008) illustrates that this widely accepted claim often fails to be acknowledged by the economic world; whereas individual stress management interventions that target the individual factors of work life are effective, interventions targeting organizations have been found to have little or no effects. However, as Lamontagne et al. (2007) have shown in a comprehensive review, if changes in the work-place are actually implemented, their effects on workers’ mental health are positive. This finding has been corroborated in later trials (Bourbonnais et al. 2011; Weigl et al. 2013). Kawakami et al. (2006) were among the first to design an Internet intervention for worksite mental health promotion. More research is needed to clarify how to design effective Internet trainings aimed at improving the work environment and organizational factors. Such interventions could either focus on fostering individual skills in “job-crafting” or enable those who are responsible for the organization of work (i.e., supervisors, managers, personnel officers) to create a healthy work environment, or both. Social media in particular has the potential to increase participation, which is necessary for achieving accepted and meaningful organizational changes (Semmer 2006).
5.5 Combining Assessment and Intervention
In many countries, health risk assessment is demanded by the occupational safety and health authorities. The mental health risk component of health risk assessment has only recently received adequate attention and is now increasingly being implemented in the work-place. However, because both mental health and psychosocial work-place factors contributing to physical and mental health are much more difficult to measure precisely, interpret, and change than physical or chemical factors, substantial new expertise is required. Moreover, not only what is done but also how it is done, that is, the implementation process, is extremely important because many power groups within an enterprise must work together to achieve a health risk assessment (Weigl et al. 2015). Recently, the European Agency for Safety and Health at Work launched the OiRA: an online interactive risk assessment project. Internet-based assessment tools provide advantages such as being accessible on a large scale, easy to update, and providing the opportunity to link further information and interventions to an assessment. These assessments could focus on the work environment and organization of work (e.g., identifying hazards, stressors) or on the health status of the individual worker (e.g., level of perceived stress, health behavior), or both. Online health assessments were found to be preferred and well accepted by employees across six different public and private sector organizations in England, especially when highly stigmatized mental health problems such as unhealthy alcohol consumption are targeted (Khadjesari et al. 2015). First experiences from linking Internet-based assessments with personalized feedback on health behaviors has demonstrated the feasibility of delivering screening in combination with brief interventions in the work-place (Khadjesari et al. 2015). Similarly, Bolier et al. (2014) combined screening, tailored advice, and tailored choice of Internet interventions for promoting mental health in nurses in the Netherlands. However, more work is needed to identify successful strategies for engaging a larger proportion of employees in online health assessments (Khadjesari et al. 2014), and in doing so to attract those workers with unhealthy behaviors who would most benefit from the interventions (Khadjesari et al. 2015). Nevertheless, a very promising route seems to be the investigation of delivering Internet-based health assessments that provide valid individual feedback on yellow or red flags, thus helping workers prioritize their health issues and enhancing their motivation for change. Such feedback could be combined with immediate access to tailored interventions that are either Internet-based or in-person. Moreover, information and communications technology easily allows combining data from such worker-directed health assessments and work-place-directed assessments. This could enable the initiation of comprehensive and coordinated actions that are again both worker- and work-place-directed.
5.6 Fostering Implementation
Investigation of sound strategies for integrating occupational e-mental health into existing occupational care is required. Lessons could be learnt from the successful implementation of Internet-based treatments into routine psychiatric and psychotherapeutic care. Development of blended trainings (combining in-person and Internet-based training sessions) and integration of occupational e-mental health into a stepped-care approach are promising avenues. The mainstays of successful implementation are transparent ongoing communication and the participation of all groups in an enterprise (e.g., employer’s representatives, employees, health experts, staff representatives) from the very beginning. Moreover, embedding the interventions into existing structures, for example, within the occupational safety and health departments and their existing health promotion activities, is key to success.
Blending in-person and Internet-based training may be especially promising because they combine the virtues of both approaches and facilitate implementation of training in the complex setting of a work-place. Social support and immediate feedback as experienced in traditional interventions (so called health circles; Aust and Ducki 2004), or stress management interventions (Limm et al. 2011; Bourbonnais et al. 2011) are probably among the main factors that promote long-term benefits. In health circles that aim to identify stressors at work and at redesigning the work environment for better work design, exchanges in such groups and an atmosphere of mutual support contribute to creative solutions and broad acceptance of changes. The emotional exchanges that occur in stress-management groups create social support, mutual understanding, and the recognition that others also experience work-related stress. Regarding implementation, trust is of outmost importance. A combination of face-to-face meetings in the work-place with Internet-based interventions and its obvious advantages seems optimal for creating a framework of trust and social support.
Anonymity is often seen as an advantage of Internet interventions, especially with regard to stigmatized mental health issues. However, concerns about data security may pose a major threat for the broad incorporation of occupational e-mental health into routine occupational health-care. Illegal tracking of personal information is of concern, as is the employment by legal authorities of barely legal methods of surveillance. Khadjesari et al. (2015) found 27 % of workers to be concerned about the safety of health-related personal information on the Internet. Trust in data security is especially important because mental health problems are often stigmatized and accompanied by feelings of insufficiency, shame, and guilt.
Finally, from an ethical point of view, workers should be free to choose either a traditional or Internet-based intervention. Unfortunately, technological changes tend to enter a field as an additional opportunity and become obligatory with the passage of time. It is therefore important to emphasize freedom of choice as a paramount value from the birth of occupational e-mental health.
5.7 Capitalizing on Interdisciplinary Research
Research in e-mental health has so far been driven predominantly by research in clinical or health psychology and psychiatry. Especially with occupational e-mental health, there is a need for stronger cooperation with experts from work and organizational psychology and occupational medicine. Moreover, research in occupational e-mental health should go beyond health sciences such as medicine and psychology and capitalize on interdisciplinary research, namely computer science and economics.
Computer science and information systems research can contribute to occupational e-mental health in multiple ways: First, through Internet interventions and health risk assessments, a wealth of data (e.g. sensor data from smartphones, data from ecological assessments in the moment, and simple questionnaires) can be collected that can help to identify people at risk and improve the quality of interventions (Mohr et al. 2013). Application of techniques from machine learning to these data can not only derive informative features for enhancing and personalizing interventions but also contribute to a general understanding of workers’ behavior and mental health (cf. Both et al. 2008). Second, occupational e-mental health can learn from software engineering how to bridge the gap between the pilot studies currently being carried out in many research settings and their full implementation in practice. This may involve various aspects, including considering basic principles of software architecture, balancing the conflicting requirements of different stakeholders, and leveraging approaches like “privacy by design” (Gürses et al. 2011). Third, information systems research can shed some light on user acceptance of, and engagement in, occupational e-mental health interventions (cf. Kleine Stegemann et al. 2012).
Economic evaluations can provide valuable information on the economic costs and benefits of occupational e-mental health interventions (van Dongen et al. 2014). So far, little is known about the effects of Internet trainings on the costs of absenteeism and presenteeism (Geraedts et al. 2015). Additionally, future research should also consider the effects on costs of work-place accidents, staff turnover, work engagement, and organizational citizenship behavior. However, whether economic evaluations demonstrating occupational e-mental health interventions to be cost-beneficial from an employer’s perspective would lead to greater investments is an unanswered question. In his review, Semmer (2006) found little evidence that even sound cost–benefit analyses have an important impact on companies’ decisions regarding their investment in health-oriented interventions. Other factors appear to be more relevant to decision-making regarding investments in health promotion. For example, it seems particularly important for decision makers to perceive health as a distinct value, independently of financial interests. Moreover, trusting relationships in those who deliver such interventions appear decisive. Further research is needed to investigate the impact of economic evaluations and other factors on the willingness to invest in occupational e-mental health.
References
Abbott J, Klein B, Hamilton C et al (2009) The impact of online resilience training for sales managers on wellbeing and performance. E J Appl Psychol 5(1):89–95
Albright G, Goldman R, Shockley KM et al (2012) Using an avatar-based simulation to train families to motivate veterans with post-deployment stress to seek help at the VA. Game Health J 1(1):21–28
Andersson G, Riper H, Carlbring P (2014) Editorial: Introducing Internet interventions—a new open access journal. Internet Intervent 1:1–2
Aust B, Ducki A (2004) Comprehensive health promotion interventions at the workplace: experiences with health circles in Germany. J Occup Health Psychol 9(3):258–270
Bennett GG, Glasgow RE (2009) The delivery of public health interventions via the Internet: actualizing their potential. Annu Rev Public Health 30:273–292
Bhui KS, Dinos S, Stansfeld SA et al (2012) A synthesis of the evidence for managing stress at work: a review of the reviews reporting on anxiety, depression, and absenteeism. J Environ Public Health. doi:10.1155/2012/515874
Billings DW, Cook RF, Hendrickson A et al (2008) A web-based approach to managing stress and mood disorders in the workforce. J Occup Environ Med 50(8):960–968
Bolier L, Ketelaar SM, Nieuwenhuijsen K et al (2014) Workplace mental health promotion online to enhance well-being of nurses and allied health professionals: a cluster-randomized controlled trial. Internet Intervent 1:196–204
Both F, Hoogendoorn M, Klein M et al (2008) Modeling the dynamics of mood and depression. In: Proceedings of the 18th European conference on artificial intelligence, Amsterdam, pp 266–270
Bourbonnais R, Brisson C, Vézina M (2011) Long-term effects of an intervention on psychosocial work factors among healthcare professionals in a hospital setting. Occup Environ Med 68(7):479–486
Capurro D, Cole K, Echavarría MI et al (2014) The use of social networking sites for public health practice and research: a systematic review. J Med Internet Res 16(3):e79
Cheng SK, Dizon J (2012) Computerised cognitive behavioural therapy for insomnia: a systematic review and meta-analysis. Psychother Psychosom 81(4):206–216
Christensen H, Griffiths KM, Evans K (2002) E-mental health in Australia: implications of the internet and related technologies for policy. Information Strategy Committee discussion paper, vol 3. Commonwealth Department of Health and Ageing, Canberra
Cook RF, Billings DW, Hersch RK et al (2007) A field test of a web-based workplace health promotion program to improve dietary practices, reduce stress, and increase physical activity: randomized controlled trial. J Med Internet Res 9(2):e17
Cox T, Baldursson E, Rial-Gonzalez E (2000) Occupational health psychology. Work Stress 14(2):101–104
Cuijpers P, Marks IM, van Straten A et al (2009) Computer-aided psychotherapy for anxiety disorders: a meta-analytic review. Cogn Behav Ther 38(2):66–82
Dagöö J, Persson Asplund R, Andersson Bsenko H et al (2014) Cognitive behavior therapy versus interpersonal psychotherapy for social anxiety disorder delivered via smartphone and computer: a randomized controlled trial. J Anxiety Disord 28:410–417
Deterding S, Dixon D, Khaled R et al (2011) From game design elements to gamefulness: defining ‘gamification’. In: Proceedings of the 15th international academic MindTrek conference: envisioning future media environments, New York. ACM, New York, pp 9–15
Ebert DD, Lehr D, Boss L et al (2014) Efficacy of an internet-based problem-solving training for teachers: results of a randomized controlled trial. Scand J Work Environ Health 40(6):582–596
Ebert DD, Berking M, Thiart H et al (2015) Restoring depleted resources: efficacy and mechanisms of change of an internet-based unguided recovery training for better sleep and psychological detachment from work. Health Psychol 34:1240–1251
Ebert DD, Heber E, Berking M et al (2016) Self-guided internet-based and mobile-based stress management for employees: results of a randomised controlled trial. Occup Environ Med 73(5):315–323
Eng TR (2001) The eHealth landscape: a terrain map of emerging information and communication technologies in health and heath care. Robert Wood Johnson Foundation, Princeton
Eysenbach G (2001) What is e-health? J Med Internet Res 3(2):e20
Feicht T, Wittmann M, Jose G et al (2013) Evaluation of a seven-week web-based happiness training to improve psychological well-being, reduce stress, and enhance mindfulness and flourishing: a randomized controlled occupational health study. Evid Based Complement Alternat Med 2013:676953
Fiordelli M, Diviani N, Schulz PJ (2013) Mapping mHealth research: a decade of evolution. J Med Internet Res 15(5):e95
Geraedts AS, Kleiboer AM, Twisk J et al (2014a) Long-term results of a web-based guided self-help intervention for employees with depressive symptoms: randomized controlled trial. J Med Internet Res 16(7):e168
Geraedts AS, Kleiboer AM, Wiezer NM et al (2014b) Short-term effects of a web-based guided self-help intervention for employees with depressive symptoms: randomized controlled trial. J Med Internet Res 16(5):e121
Geraedts AS, van Dongen JM, Kleiboer AM et al (2015) Economic evaluation of a web-based guided self-help intervention for employees with depressive symptoms; results of a randomised controlled trial. J Occup Environ Med 57(6):666–675
Graafland M, Dankbaar M, Mert A et al (2014) How to systematically assess serious games applied to health care. JMIR Serious Games 2(2):e11
Gürses S, Troncoso C, Diaz C (2011) Engineering privacy by design. Available from https://www.cosic.esat.kuleuven.be/publications/article-1542.pdf. Accessed 7 Apr 2015
Hasson D, Anderberg U, Theorell T et al (2005) Psychophysiological effects of a web-based stress management system: a prospective, randomized controlled intervention study of IT and media workers. BMC Public Health 5(1):78
Haug T, Nordgreen T, Öst LG et al (2012) Self-help treatment of anxiety disorders: a meta-analysis and meta-regression of effects and potential moderators. Clin Psychol Rev 32(5):425–445
Heber E, Lehr D, Ebert DD et al (2016) Web-based and mobile stress management intervention for employees: a randomized controlled trial. J Med Internet Res 18(1), e21
Heron KE, Smyth JM (2010) Ecological momentary interventions: incorporating mobile technology into psychosocial and health behaviour treatments. Br J Health Psychol 15(1):1–39
Hilty DM, Ferrer DC, Parish MB et al (2013) The effectiveness of telemental health: a 2013 review. Telemed J E Health 19(6):444–454
Houdmont J, Leka S (2010) An introduction to occupational health psychology. In: Leka S, Houdmont J (eds) Occupational health psychology. Wiley-Blackwell, Chichester, pp 1–30
Junge M, Lehr D, Bockting CLH et al (2015) For whom are occupational e-mental health interventions effective? Predictors of internet-based problem-solving training outcome. Internet Intervent 2(1):39–47
Karasek R, Theorell T (1990) Healthy work: stress, productivity, and the reconstruction of working life. Basic Books, New York
Kawakami N, Takao S, Kobayashi Y et al (2006) Effects of web-based supervisor training on job stressors and psychological distress among workers: a workplace-based randomized controlled trial. J Occup Health 48(1):28–34
Khadjesari Z, Freemantle N, Linke S et al (2014) Health on the web: randomised controlled trial of online screening and brief alcohol intervention delivered in a workplace setting. PLoS One 9(11):e112553
Khadjesari Z, Newbury-Birch D, Murray E et al (2015) Online health check for reducing alcohol intake among employees: a feasibility study in six workplaces across England. PLoS One 10(3):e0121174
Kleine Stegemann S, Ebenfeld L, Thiart H et al (2012) Towards measuring user engagement in internet interventions for common mental disorders. In: Proceedings of HCI 2012, The 26th BCS conference on human computer interaction. Available from http://ewic.bcs.org/upload/pdf/ewic_hci12_pcp_paper7.pdf. Accessed 7 Apr 2015
Lamontagne AD, Keegel T, Louie AM et al (2007) A systematic review of the job-stress intervention evaluation literature, 1990−2005. Int J Occup Environ Health 13(3):268–280
Lehr D, Heber E, Thiart H (2012) Regeneration als Ressource: Erholungsverhalten als Antwort auf berufliche Herausforderungen [Regeneration as an major resource. Coping with occupation stress by fostering recreational behaviour]. PADUA 7:182–187 (in German)
Lehr D, Eckert M, Baum K et al (2014) Online-Trainings zur Stressbewältigung—eine neue Chance zur Gesundheitsförderung im Lehrerberuf? [Online stress-management-interventions—an effective approach to fostering mental health in school teachers?]. Lehrerbildung auf dem Prüfstand 1:191–212 (in German)
Limm H, Gündel H, Heinmüller M et al (2011) Stress management interventions in the workplace improve stress reactivity: a randomised controlled trial. Occup Environ Med 68(2):126–133
Ly KH, Asplund K, Andersson G (2014) Stress management for middle managers via an acceptance and commitment-based smartphone application: a randomized controlled trial. Internet Intervent 1(3):95–101
Martin A, Sanderson K, Cocker F (2009) Meta-analysis of the effects of health promotion intervention in the work place on depression and anxiety symptoms. Scand J Work Environ Health 35(1):7–18
Mohr DC, Vella L, Hart S et al (2008) The effect of telephone-administered psychotherapy on symptoms of depression and attrition: a meta-analysis. Clin Psychol Sci Pract 15(3):243–253
Mohr DC, Carmody T, Erickson L et al (2011) Telephone-administered cognitive behavioral therapy for veterans served by community-based outpatient clinics. J Consult Clin Psychol 79(2):261–265
Mohr DC, Burns MN, Schueller SM et al (2013) Behavioral intervention technologies: evidence review and recommendations for future research in mental health. Gen Hosp Psychiatry 35:332–338
Moorhead SA, Hazlett DE, Harrison L et al (2013) A new dimension of health care: systematic review of the uses, benefits, and limitations of social media for health communication. J Med Internet Res 15(4):e85
National Institute for Occupational Safety and Health (2005) Occupational health psychology. Available from http://www.cdc.gov/niosh/topics/ohp/. Accessed 18 Feb 2015
Oh H, Rizo C, Enkin M et al (2005) What is eHealth (3): a systematic review of published definitions. J Med Internet Res 7(1):e1
Opriş D, Pintea S, García-Palacios A et al (2012) Virtual reality exposure therapy in anxiety disorders: a quantitative meta-analysis. Depress Anxiety 29(2):85–93
Pagliari C, Sloan D, Gregor P et al (2005) What is eHealth (4): a scoping exercise to map the field. J Med Internet Res 7(1):e9
Parsons TD, Rizzo AA (2008) Affective outcomes of virtual reality exposure therapy for anxiety and specific phobias: a meta-analysis. J Behav Ther Exp Psychiatry 39(3):250–261
Richards D, Richardson T (2012) Computer-based psychological treatments for depression: a systematic review and meta-analysis. Clin Psychol Rev 32:329–342
Richardson KM, Rothstein HR (2008) Effects of occupational stress management intervention programs: a meta-analysis. J Occup Health Psychol 13:69–93
Richardson LK, Frueh BC, Grubaugh AL et al (2009) Current directions in videoconferencing tele-mental health research. Clin Psychol Sci Pract 16(3):323–338
Riper H, Andersson G, Christensen H et al (2010) Theme issue on e-mental health: a growing field in internet research. J Med Internet Res 12(5):e74
Ritterband LM, Thorndike F (2006) Internet interventions or patient education websites? J Med Internet Res 8(3):e18
Ruwaard J, Lange A, Bouwman M et al (2007) E-mailed standardized cognitive behavioural treatment of work-related stress: a randomized controlled trial. Cogn Behav Ther 36:179–192
Sauter SL, Hurrel JJ, Fox HR et al (1999) Occupational health psychology: an emerging discipline. Ind Health 37(2):199–211
Semmer NK (2006) Job stress interventions and the organization of work. Scand J Work Environ Health 32(6):515–527
Semmer NK, Jacobshagen N, Meier LL et al (2007) Occupational stress research: the “stress-as-offense-to-self” perspective. In: Houdmont J, McIntyre S (eds) Occupational health psychology: European perspectives on research, education and practice, vol 2. Nottingham University Press, Nottingham, pp 43–60
Siegrist J (2002) Effort-reward imbalance at work and health. In: Perrewe P, Ganster D (eds) Research in occupational stress and well-being, vol 2, Historical and current perspectives on stress and health. JAI Elsevier, New York, pp 261–291
Takahashi Y, Uchida C, Miyaki K et al (2009) Potential benefits and harms of a peer support social network service on the internet for people with depressive tendencies: qualitative content analysis and social network analysis. J Med Internet Res 11(3):e29
Thiart H, Ebert DD, Lehr D et al. (in press) Internet-based cognitive behavioral therapy for insomnia: a health economic evaluation. Sleep.
Thiart H, Lehr D, Ebert DD et al (2015) Log in and breathe out: internet-based recovery training for sleepless employees with work-related strain: results of a randomized controlled trial. Scand J Work Environ Health pii:3478. doi:10.5271/sjweh.3478 [Epub ahead of print]
van der Klink JJ, Blonk RW, Schene AH et al (2001) The benefits of interventions for work-related stress. Am J Public Health 91(2):270–276
van Dongen JM, van Wier MF, Tompa E et al (2014) Trial-based economic evaluations in occupational health: principles, methods, and recommendations. J Occup Environ Med 56(6):563–572
Weigl M, Hornung S, Angerer P et al (2013) The effects of improving hospital physicians working conditions on patient care: a prospective, controlled intervention study. BMC Health Serv Res 13:401
Weigl M, Herbig B, Bahemann A et al (2015) Empfehlungen zur Durchführung einer Gefährdungsbeurteilung psychischer Belastungen: Positionspapier der Deutschen Gesellschaft für Arbeitsmedizin und Umweltmedizin, erstellt von der AG Psychische Gesundheit in der Arbeit der DGAUM [Recommendations on developing and carrying out psychosocial risk evaluations at the workplace]. Arbmed Sozialmed Umweltmed 50:660–665 (in German)
Winzelberg AJ, Classen C, Alpers GW et al (2003) Evaluation of an internet support group for women with primary breast cancer. Cancer 97(5):1164–1173
Wolever RQ, Bobinet KJ, McCabe K et al (2012) Effective and viable mind-body stress reduction in the workplace: a randomized controlled trial. J Occup Health Psychol 17(2):246–258
Yamagishi M, Kobayashi T, Nakamura Y (2008) Effects of web-based career identity training for stress management among Japanese nurses: a randomized control trial. J Occup Health 50(2):191–193
Zichermann G, Cunningham C (2011) Gamification by design: implementing game mechanics in web and mobile apps. O’Reilly Media, Sebastopol, pp 35–67
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Lehr, D. et al. (2016). Occupational e-Mental Health: Current Approaches and Promising Perspectives for Promoting Mental Health in Workers. In: Wiencke, M., Cacace, M., Fischer, S. (eds) Healthy at Work . Springer, Cham. https://doi.org/10.1007/978-3-319-32331-2_19
Download citation
DOI: https://doi.org/10.1007/978-3-319-32331-2_19
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-32329-9
Online ISBN: 978-3-319-32331-2
eBook Packages: Business and ManagementBusiness and Management (R0)