Abstract
sub-Saharan Africa is home to almost three-quarters of all individuals living with HIV/AIDS in the world. Yet, sub-Saharan Africa also has one of the most severe shortages of trained medical and behavioral health care workers in the world to tackle the needs of the huge epidemic. This gap between HIV-related treatment needs and staff resources has presented the need for “task shifting” or “task sharing,” defined as delegating tasks to less specialized health care workers, and/or considering ways of sharing tasks across a clinical team. Task shifting has been a key implementation strategy for increasing access to antiretroviral therapy (ART) to treat HIV/AIDS across sub-Saharan Africa. For behavioral medicine, task shifting can be used for the delivery of behavioral health interventions for HIV medication adherence and co-occurring mental health problems. In this chapter, we aim to demonstrate how the efforts to use task shifting for rolling out ART programs in sub-Saharan Africa can inform behavioral medicine task shifting efforts to expand access to evidence-based ART adherence counseling and mental health interventions in HIV care in sub-Saharan Africa. We focus specifically on examples of task shifting cognitive behavioral therapy (CBT) for ART adherence, depression, and substance use among individuals living with HIV/AIDS in sub-Saharan Africa. Although there have been few examples to date of task shifting CBT in the context of HIV care in sub-Saharan Africa, we use these promising early examples to inform future considerations for adapting and implementing CBT using a task shifting model in this population.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Cognitive Behavioral Therapy
- Behavioral Medicine
- Cognitive Behavioral Therapy Intervention
- Adherence Counseling
- Task Shifting
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Task shifting is defined by the World Health Organization (WHO) as the “process of delegation whereby tasks are moved, where appropriate, to less specialized health workers” [1]. This allows, for example, for qualified nurses to prescribe and dispense medications when doctors are not available, and for community workers (who are in greater supply compared to nurses and physicians in resource-limited settings) to deliver a wide range of clinical services that would normally have been delivered by nurses or other professionals. More recently, task shifting models have been re-conceptualized to be instead a “task sharing” approach, as a way to avoid overburdening and over-relying on lower level cadres of workers. Task sharing (vs. shifting) involves delineating specific roles and responsibilities for each provider within a clinical team, as well as considering other ways of task sharing with family members and patients themselves [2]. As tasks are shifted and shared across the team, it is also essential to consider the changing roles of the physicians and higher level nurses, particularly focusing their attention on complex, treatment resistant patients and also ensuring ongoing supervision and management of the lower level providers [2].
Within the global context of HIV/AIDS and behavioral medicine interventions, task shiftingFootnote 1 is important because of the lack of specialized professionals relative to the epidemiology of the epidemic. To expand access to biomedical treatment, task shifting has been employed to deliver HIV care and HIV medication because of the shortage of trained physicians. For behavioral medicine, task shifting can be used to deliver psychosocial interventions to improve adherence to HIV medication, as well as to deliver evidence-based mental health interventions [2].
In this chapter, we aim to demonstrate how the use of task shifting for delivering biomedical HIV care in sub-Saharan Africa can inform efforts to use task shifting models to deliver behavioral medicine interventions for individuals living with HIV/AIDS in this setting. In doing so, we first describe the widespread HIV/AIDS epidemic in sub-Saharan Africa and the shortage of trained health care providers to meet the needs of the epidemic. We describe task shifting efforts for expanding access to HIV medication in sub-Saharan Africa, and then illustrate how this approach to task shifting can be used to inform a similar approach for evidence-based behavioral medicine interventions among individuals living with HIV/AIDS in sub-Saharan Africa. We move from a broad overview of task shifting in HIV care in sub-Saharan Africa to specific examples of task shifting efforts to deliver evidence-based cognitive behavioral therapy (CBT) among individuals living with HIV/AIDS in sub-Saharan Africa. These efforts to task shift CBT address HIV medication adherence and commonly co-occurring psychological symptoms that interfere with successful HIV/AIDS outcomes, including depression and substance use. Although at the time of writing there have been few examples of task shifting of CBT to address psychosocial and behavioral medicine issues among individuals living with HIV/AIDS in sub-Saharan Africa, there have been a few promising early examples, including in the treatment of depression in Zimbabwe [3], the treatment of alcohol use in Kenya [4, 5], and integrated interventions for depression and HIV medication adherence in South Africa [6]. From these in-depth examples of task shifting CBT for alcohol use, depression, and integrated adherence interventions, we discuss considerations when adapting and implementing CBT using a task shifting model in this population. Finally, we discuss future directions and novel methodologies, for instance using multimedia-based interventions to promote standardization of task shifting delivery of CBT interventions and/or facilitate the use of these techniques by live interventionists. We also discuss the need to move from efficacy and effectiveness designs to more implementation science focused methods to promote sustainable integration of CBT for behavioral medicine in HIV care in sub-Saharan Africa.
This chapter focuses on HIV/AIDS and task shifting in HIV/AIDS care given its global prevalence, the need for behavioral medicine interventions for HIV medication adherence, self-care, and secondary prevention, and a rich prior history of using task shifting for expanding access to HIV medication in sub-Saharan Africa. Yet, HIV is just one example of a global disease burden that has benefitted from biomedical and behavioral task shifting efforts. This model and clinical examples provided in the remainder of this chapter are relevant for other diseases that require significant self-care that have increasing prevalence in sub-Saharan Africa, such as cancer and diabetes [7, 8].
1.1 HIV/AIDS Epidemic in sub-Saharan Africa
Nearly 71 % (24.7 million) of the total number of people living with HIV/AIDS in the world live in sub-Saharan Africa [9]. In sub-Saharan Africa, nearly 1 in every 25 adults is living with HIV [9]. In this region, ten countries (Ethiopia, Kenya, Malawi, Mozambique, Nigeria, South Africa, Uganda, Tanzania, Zambia, and Zimbabwe) account for 81 % of all individuals living with HIV/AIDS. Collectively, South Africa (SA) (25 %) and Nigeria (13 %) account for half of the HIV-infected population. Between 2005 and 2013, there has been a significant decline (39 %) in AIDS-related deaths in the region as a result of the rapid increase in number of people on HIV treatment [9].
1.2 Shortage of Trained Health Care Workers in sub-Saharan Africa
Sub-Saharan Africa has the lowest density of physicians, nurses, and midwives in the world, at 1.33 health workers per 1000 population (3 % of the global health workforce), with large variations between and within countries [10, 11]. Only 8 out of the 49 countries in sub-Saharan Africa have a health force density above the recommendations put forth by the World Health Organization [12]. The density of health workers tends to increase with improved economic status, although this is not always the case (see Ahmat et al. [10] for greater discussion of the relationship between higher economic status and health workforce). Further, in more specialized training areas, such as psychology and behavioral health, there are shortages in all countries in sub-Saharan Africa [13].
1.3 Gap Between HIV Treatment Needs and Staff Resources in sub-Saharan Africa
The HIV/AIDS epidemic in sub-Saharan Africa has compounded the need for health providers and has placed additional strain on the health sector that is already facing professional health worker shortages; for example, an estimated minimum of one to two doctors, up to seven nurses, and approximately three pharmacy staff are required per 1000 people for effective provision of HIV treatment [14]. As illustrated above, the reality falls far short of the requirements. These low numbers are further exacerbated by health workers themselves being vulnerable to disease, death, burnout and fatigue [15, 16], and the brain drain, or loss of doctors, nurses, and other health professionals by emigration to other, usually better resourced countries ([17, 18]). In addition, many African countries lack institutions and the capacity to train sufficient numbers of doctors [19].
1.4 Need for Task Shifting to Address Provider Shortage
WHO noted in 2006 that it was crucial for drastic action to be taken to address the human resource crises in the face of the HIV/AIDS epidemic in sub-Saharan Africa and launched a “Treat, Train, Retrain” plan to upscale and expand the health workforce [1]. WHO aims to get HIV medication to all persons living with HIV/AIDS worldwide. Although in sub-Saharan Africa HIV treatment is now available to approximately 37 % of people, there are significant differences between countries [9]. Universal access to HIV treatment and care services will require health systems capable of delivering quality interventions on a vastly expanded scale, relying heavily on task shifting models [20].
1.5 Task Shifting in HIV Care in sub-Saharan Africa
As stated above, in HIV care in sub-Saharan Africa, nurses and/or community health workers can successfully perform tasks such as provision and management of HIV medication, and counseling and screening to facilitate enrollment of HIV-infected patients eligible for treatment [21–23]. For instance, nurses have been successfully used to identify HIV treatment eligible patients, while physicians continued to initiate HIV treatment and prioritize time with HIV treatment eligible patients and those with more complex treatment needs [24]. Community health workers have also proved to contribute to service delivery and human resource capacity in sub-Saharan Africa. By serving as an entry point into HIV care, support, and treatment services, community health workers reduced waiting times, streamlined patient flow, and reduced workload of health workers, thus enhancing reach, uptake, and overall quality of HIV services [23].
1.6 Task Shifting HIV Medication Adherence Counseling
After initiating HIV medication, treatment requires lifelong adherence [25], which proves challenging for many; a prior meta-analysis indicated that approximately 23 % of patients in sub-Saharan Africa did not achieve optimal HIV medication adherence [26]. Implications of HIV medication nonadherence are heightened in sub-Saharan Africa where available HIV medication regimens are limited, and developing drug resistance may further eliminate availability of treatment regimens [27]. Task shifting HIV medication adherence counseling to lay health workers aims to increase access to adherence counseling, support, and psychoeducation [21–23]. Lay counselor-delivered HIV medication adherence counseling in HIV care aims to provide treatment preparation and ongoing adherence support to people enrolled in HIV clinic services [28, 29]. Lay counselors frequently remain outside the formal health system and are generally instructed, employed, and managed through nongovernmental intermediaries [29]. Educational requirements for lay health workers differ from country to country, and requirements may also change over time. Lay counselors, like other community health workers, do not have any formal professional or paraprofessional qualifications [30] for the field that they work in and they are generally trained by nongovernmental intermediaries.
1.7 Outcomes of Task Shifting
Prior research has suggested the effectiveness of task shifting in the delivery of HIV treatment in Africa, specifically substantial cost savings [21] and physician time savings [21–23, 31]. In settings where tasks have shifted to nurses, there is less loss to follow-up in the nurse-managed groups (vs. physician-managed) with no difference in mortality and equal survival rates at 12 months [32]. Many patients appear to prefer nurse-managed care because of friendlier service, better patient examination and education, and the closer proximity of services to their homes. This result was however not found universally, and some patients feared stigmatization and inadequate care [33] and preferred care from primary health clinics and district management units because of better relationships with providers, friendlier and more supportive care, and better patient education [34, 35].
The presence of community health workers also appears to improve retention in care and the quality of life of people living with HIV/AIDS [23, 36]. However, community health worker programs have not always been successful, and, in particular, larger programs tend to present with sustainability and quality of care challenges [23, 37–39]. In a South African study assessing the impact of a community-based adherence support program on HIV outcomes in government HIV treatment sites, patients with community health worker adherence support more consistently collected their medication and attained a treatment pickup rate of 95 % vs. 67 % of those who did not have community health workers adherence support [40]. Retention in care and adherence are two of the most important issues for long-term success of HIV treatment programs, and both appear to benefit from task shifting and community health worker involvement [23]. As has been suggested by prior researchers, we must leverage the lessons learned from task shifting in HIV care in sub-Saharan Africa for other noncommunicable diseases [41]. More specifically, in this chapter, we will discuss how these lessons can inform efforts to implement other evidence-based behavioral medicine interventions for individuals living with HIV/AIDS in sub-Saharan Africa.
2 Applications of Task Shifting for Behavioral Medicine Interventions in HIV Care in sub-Saharan Africa
In addition to the behavioral health needs related to managing HIV/AIDS, such as HIV medication adherence and retention in care, comorbid psychiatric conditions are also common among HIV-infected individuals in sub-Saharan Africa. Two of the most common psychiatric disorders among individuals living with HIV/AIDS in sub-Saharan Africa are depression and substance abuse [42]. Elevated depressive symptom rates are approximately 31 %, and a pooled estimate of major depression is 18 % according to a meta-analysis in sub-Saharan Africa [42]. Alcohol is the most common drug used in sub-Saharan Africa [43], and rates of alcohol use disorders range from 7 to 31 % [42]. When untreated, depression and substance use are significantly associated with poor antiretroviral adherence across multiple studies, which ultimately leads to worse HIV/AIDS treatment outcomes [42].
Unfortunately, similar to the shortage of trained medical providers in sub-Saharan Africa, there is also a shortage of trained mental health providers. In general, low income countries have between 0.05 psychiatrists and 0.16 psychiatric nurses per 100,000 people [13]. Only half of the countries in Africa have any type of community-based mental health care [13]. Countries with the largest shortage of mental health care workers in the world are Chad, Eritrea, and Liberia, each only have one psychiatrist in the entire country [13]. Much of sub-Saharan Africa has less than five mental health care workers per 100,000 individuals, and South Africa is the only country in sub-Saharan Africa with more than 25 mental health care workers per 100,000 people [13]. As such, there are clear needs for task shifting of mental health care for individuals with HIV/AIDS.
2.1 Task Shifting CBT in sub-Saharan Africa
Cognitive behavioral therapy (CBT) can be used to address a range of behavioral health needs among individuals living with HIV/AIDS, including to improve symptoms of depression, reduce HIV medication nonadherence, and reduce substance use [44, 45]. Although the majority of empirical support for CBT interventions among individuals living with HIV/AIDS is from the US and other developed countries, there is accumulating empirical support for CBT interventions in sub-Saharan Africa using task shifting models. In particular, CBT’s structured, time limited approach has been viewed as particularly suitable for the demands of task shifting (i.e., to improve ease of training, supervision). See Table 14.1.
In this section, we will discuss examples of task shifting of evidence-based CBT interventions to address psychosocial and behavioral medicine issues among individuals living with HIV/AIDS in sub-Saharan Africa. These examples are highlighted in detail below in the Case Illustrations section. From these examples, we discuss considerations for future efforts when adapting and implementing CBT using a task shifting model in this population.
3 Cognitive Behavioral Therapy for Adherence
As indicated above, although adherence counseling is routinely delivered in HIV clinic settings in South Africa it is not clear if this counseling is evidence-based, as there have been few efforts to describe or evaluate routine adherence counseling in this setting [51]. As such, despite efforts to use task shifting models to deliver adherence counseling in sub-Saharan Africa, continued efforts are needed to use task shifting to deliver evidence-based HIV medication adherence interventions in these settings. For instance, there is a substantial evidence base for cognitive behavioral interventions to improve HIV medication adherence, largely in developing countries. Simoni et al. [52] conducted a meta-analytic review of published randomized clinical trials (RCTs) that had evaluated a behavioral HIV medication adherence intervention. In this review (with most trials being US-based; 74 %), the majority of interventions (79 %) included CBT components, such as psychoeducation, motivational interviewing, healthy coping strategies, and some form of cognitive restructuring. Eighty-four percent of studies included behavioral CBT strategies (i.e., cue dosing, activity scheduling). The majority of studies (58 %) included three of the aforementioned CBT components. Further, interventions that included CBT components (compared to those that did not include CBT components) tended to show greater improvements in HIV medication nonadherence. Across studies, the most common providers were well-trained health care providers (i.e., physicians, nurses in 47 % of studies) or trained psychologists (in 26 % of studies). Over half of studies (53 %) used research staff (not clinic staff) to provide the intervention.
There are clear implications when we consider extending these research findings to LMICs, and sub-Saharan Africa in particular, where task shifting with other levels of providers is essential. There has been a similar review of RCTs of HIV medication adherence interventions in sub-Saharan Africa [53]. Although this review categorized interventions based on the use of behavioral and cognitive techniques, none of the identified interventions used a theory-driven CBT approach to address adherence, nor did the review discuss who was implementing the interventions to ascertain whether a task shifting model has been used to implement CBT for adherence in sub-Saharan Africa. Although there are few published examples of using task shifting to deliver CBT interventions for HIV medication adherence in HIV clinic settings, there are examples in progress that integrate evidence-based CBT interventions for adherence with other CBT interventions for co-occurring psychiatric symptoms that we discuss in more depth below.
4 Task Shifting of CBT for Co-occurring Psychiatric Symptoms Among HIV-Infected Individuals in sub-Saharan Africa
There have been few efforts to use task shifting models to deliver CBT specifically in sub-Saharan Africa for HIV populations; however, some preliminary work has been done to task shifting efficacious CBT interventions for depression and substance use among HIV-infected individuals in sub-Saharan Africa. The examples listed in this section are described in more detail in the Case Illustrations section, and then followed by specific considerations from this process that may affect future implementation and scalability.
4.1 CBT for Alcohol Use in HIV/AIDS
At the time of writing, perhaps the clearest example of systematically adapting and evaluating a task shifting delivery model of CBT in an HIV population in sub-Saharan Africa is that of Papas et al. [4, 5]. This team adapted CBT to reduce alcohol use among HIV-infected outpatients in Edloret, Kenya and conducted a preliminary pilot trial to examine initial feasibility and acceptability of paraprofessional delivery [5] and subsequently published a Stage 1 RCT evaluating its efficacy [4]. CBT was initially selected for this work because of its strong empirical support in Western settings, and prior application in sub-Saharan Africa (i.e., Zambia [54]). Additionally, and central to task shifting models, it was also selected given its highly structured format, which was seen to be feasible for training paraprofessionals with limited formal education.
4.2 Integrated CBT Intervention for Alcohol Use and HIV Medication Adherence
One limitation of the work of Papas et al. [4, 5] in Kenya was a lack of a dual focus on HIV outcomes (e.g., HIV medication adherence). Given the prevalence of alcohol use disorders and its powerful effects on HIV medication adherence in sub-Saharan Africa [55], efforts to develop an integrated CBT intervention to address alcohol use and HIV medication adherence are also necessary. Preliminary work in this area has begun to be conducted in South Africa, where rates of alcohol consumption are also among the highest in the world [43]. This work in South Africa [56] is developing a lay adherence counselor-delivered CBT intervention to address hazardous alcohol use and HIV medication nonadherence in the public HIV clinic setting in South Africa.
4.3 CBT for Depression in HIV/AIDS
As an example of task shifting a CBT intervention for depression in HIV care in sub-Saharan Africa, Chibanda et al. [3] adapted problem-solving therapy for depression to be delivered by lay health workers in a Harare, Zimbabwe primary care setting. In this setting, lay health workers typically have at least primary school education, have lived locally for an extended period of time, and are intended to support HIV medication adherence and other psychological counseling in the HIV care setting. Although patients did not have to disclose their HIV status to enter into the trial, over half of all patients in the trial had an HIV-related problem, and the study was conducted at primary care clinic sites that see a large percentage of HIV-infected patients in this region. Up to six sessions of problem-solving therapy were offered either at the “Friendship bench,” located adjacent to the HIV clinic setting, or in the patient’s home.
4.4 Integrated CBT Intervention for Depression and HIV Medication Adherence
Although still in progress, there are initial efforts to integrate CBT for depression with an evidence-based CBT intervention for adherence (Life-Steps) [57, 58]. Andersen et al. [6] evaluated a nurse-delivered CBT intervention for depression and HIV medication adherence. The intervention was a six to eight session intervention based on cognitive behavioral therapy for adherence and depression [6]. Primary modifications to the original intervention included streamlining session content, and removing the cognitive restructuring module due to its complexity. Treatment modules included psychoeducation, motivational interviewing, problem-solving, activity scheduling, and relaxation training. Initial evidence suggests the intervention approach is acceptable to patients and associated with significant improvements in depression, functioning, and modest improvements in HIV medication adherence. Implementation was challenging, requiring extensive weekly supervision, initial training (88 h), supplemented with regular ongoing training. Additional research is needed in this area to determine whether a nurse- or lay counselor-delivered CBT intervention is feasible and sustainable for delivery in this setting, and whether the treatment is associated with long-term improvements in key health and psychological outcomes.
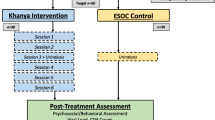
Bere and colleagues are evaluating a lay counselor-delivered CBT intervention for depression and HIV medication adherence in Zimbabwe [50]. The intervention combines Life-Steps for HIV medication adherence [57, 58] with an integrated behavioral activation and problem-solving therapy approach to depression, delivered in public HIV care in Harare, Zimbabwe by four trained lay adherence counselors. The study will determine whether the implementation strategy was feasible, acceptable, and associated with improvements in depression, HIV medication adherence, and HIV-related health outcomes. Descriptions of the formative qualitative work [59] and preliminary work to culturally adapt Life-Steps for this setting [50] provide important details regarding the necessary steps for adapting CBT for this resource-limited HIV care setting.
5 Case Illustrations of Task Shifting CBT in sub-Saharan Africa
5.1 Case 1: Task Shifting CBT for Alcohol Use Among HIV-Infected Patients in Kenya
As mentioned briefly above, Papas et al. [5] adapted CBT to be delivered by paraprofessionals in Kenya to address alcohol use among HIV-infected patients. The adaptation process began with initial formative qualitative work, followed by systematic treatment adaptation and pilot trial, and then a subsequent efficacy trial. Below the specific steps and details regarding the process of adaptation and implementation are highlighted.
5.1.1 Formative Phase
The first step in adapting CBT to address alcohol use among HIV-infected patients in Kenya consisted of formative qualitative work with patients, providers, and staff, as well as observation of local alcohol peer support groups [5]. Initial qualitative analysis found that the CBT model for alcohol use fit with the Kenyan culture; however, it was recommended in formative work that exercises be adapted to the local setting, for instance unique cultural contexts for drinking, as well as adapting language used to be appropriate for local idioms, and including culturally appropriate visual aids and metaphors. Cultural myths and misinformation about alcohol use and HIV outcomes in this population were incorporated into the CBT protocol. A focus on income-generating activities, particularly among female patients, was also incorporated. It was also decided that groups would be stratified by gender to allow for discussion of sensitive issues. Group format was selected given focus on social networks as key in Kenyan culture, and also because of implications for cost-effectiveness [60]. Selection of the primary treatment target—alcohol vs. other HIV-related behaviors—was decided upon locally. Assessments were also adapted to be fitting to local culture; for instance, breathalyzers were highly stigmatized given that they were used by Kenyan police and as such saliva tests were seen as more discrete and less stigmatized and thus were used instead to assess the primary outcome. Finally, the original CBT protocol was reduced to six sessions due to feasibility concerns.
5.1.2 Interventionist Selection, Training, and Supervision
Given the lack of trained mental health professionals providing substance use treatment in Kenya [60], two paraprofessionals with no prior CBT experience (one with a high school diploma and no counseling experience and one with a two-year post high school counseling diploma and minimal counseling experience) were hired to deliver the intervention. One of the providers was HIV-infected. Selection procedures included discussing case examples and conducting behavioral role plays, and the team aimed to select those with natural talents (empathy, emotional perceptiveness, good communication and analytical skills). The counselors received 175–300 h of training and supervision prior to the trial. Training in CBT included classroom work, role plays, videotaped feedback, and training in ethics and basic health education. Counselors conducted role plays with medical students as simulated patients, which were supervised and rated for use of CBT skills. Once counselors met a minimum threshold on adherence to the CBT manual, they then conducted pilot groups, which were videotaped.
5.1.3 Pilot Trial Results
Results from the initial pilot trial with 27 patients showed that the two lay providers were able to deliver CBT with modest fidelity and competence [5]. Pilot patient outcomes were favorable, including treatment attendance, acceptability, and reductions in alcohol use [5]. Additionally, although treatment attendance was fairly high (overall attendance was 77 %), numerous efforts were made to reduce barriers to attendance, such as text and phone call appointment reminders, reimbursement for transportation, and in some cases, transportation to the first CBT session [5].
5.1.4 Stage 1 Efficacy Trial
Subsequently, this team conducted a Stage 1 RCT to evaluate the efficacy of the adapted, paraprofessional intervention (delivered in Kiswahili) compared to usual care among HIV-infected HIV treatment eligible patients who reported hazardous/binge drinking (n = 75) [4]. The primary outcome as indicated above was alcohol use (assessed using a timeline follow back and alcohol saliva tests). Results demonstrated large effect sizes between the conditions at the 30-day follow-up in reducing alcohol use (d = 0.95). At a 90-day follow-up, abstinence from alcohol was 69 % in the CBT condition and 38 % in usual care. Participants randomized to CBT attended 93 % of the six sessions offered (M = 5.6, SD = 0.66). Ratings of counselor adherence and competence were conducted using a standardized rating scale [61]. Adherence and competence were found to be equivalent to bachelors-level therapists delivering CBT in the US. Although the results are promising, one noted limitation is the lack of attention to HIV outcomes in the trial, limiting the treatment to a single target. Although integrated CBT treatments have been developed and largely tested in the US to address HIV-related behaviors and co-occurring substance use [62, 63], it is unclear whether this is feasible for paraprofessional delivery in a resource constrained setting.
5.2 Case 2: Task Shifting an Integrated Intervention for Alcohol Use and HIV Medication Adherence in South Africa
To improve health outcomes alongside efforts to reduce alcohol use among HIV-infected patients, efforts are underway in South Africa to adapt an integrated CBT intervention for alcohol use and HIV medication adherence. The intervention was adapted for paraprofessional delivery in HIV care. Below the formative phase is described and the ongoing plan for evaluating the adapted intervention in an efficacy trial.
5.2.1 Formative Phase
Formative research was conducted in South Africa to examine the appropriateness and acceptability of an intervention delivered in HIV care to address both alcohol use and alcohol-related HIV medication nonadherence [55]. The formative phase was conducted at two HIV clinics in Tshwane, South Africa among 304 HIV-infected adults. Feedback was solicited on who would be optimal to deliver the intervention, the preferred quantity, duration, format, and settings of the sessions, specific skills to focus on, and potential involvement of friends and family. Regarding specific skills, patients were asked to assess the perceived utility of potential CBT skills (although not labeled as such), including non-alcohol related healthy coping strategies, relapse prevention, advantages and disadvantages of not drinking, and brainstorming ways to reduce frequency and quantity of alcohol consumption. Results from the formative work indicated that 95 % of patients surveyed felt there was a need for an intervention to address alcohol-related HIV medication adherence. Suggestions included two clinic-based sessions 1 h in length in a group format to be led by a peer (a fellow HIV treatment recipient) or an adherence counselor (typically a high school level paraprofessional trained to deliver standard adherence counseling in South Africa). Further, individuals with low levels of HIV medication adherence in particular strongly preferred paraprofessional interventionists. There was a strong preference for “strategies for coping that do not involve alcohol” to be a primary component of intervention, as well as discussing pros and cons of drinking. Authors suggested that this evidence points to the relevance of a CBT type intervention, including using motivational interviewing and relapse prevention strategies, to address alcohol-related nonadherence by paraprofessionals in the HIV clinic setting [55].
5.2.2 Protocol for Evaluating Intervention Delivery and Patient Outcomes
In response [56], this team has developed a protocol to evaluate a CBT intervention to address alcohol and HIV medication nonadherence in the HIV clinic setting in South Africa. This team is adapting a blended motivational interviewing/problem-solving therapy intervention that has been developed to address alcohol use among individuals in South Africa [49] for the needs of HIV-positive alcohol using patients. The blended motivational interviewing/problem intervention for adherence/alcohol use aims to increase motivation to reduce alcohol use and promote HIV medication adherence. Feedback will be provided on levels of substance use, and psychoeducation will be provided on how alcohol use impacts HIV treatment outcomes. Motivational interviewing strategies will increase readiness to change and build rapport, and readiness change will be assessed using a “readiness ruler.” Other CBT techniques include a motivational interviewing decisional balance exercise, problem-solving skills to cope with triggers, acceptance, and coping with negative thoughts. A motivational interviewing style is emphasized throughout the intervention.
Adaptation of the intervention followed four initial focus groups and results of the formative phase [55]. Lay adherence counselors (i.e., high school diploma level, often HIV positive) are being trained to deliver the intervention. Patients are being recruited from the public hospital-based HIV clinics in Tshwane, South Africa where the pilot work took place, specifically patients who are HIV positive, on HIV medication, and categorized as “harmful/hazardous drinkers” using the Alcohol Use Disorders Identification Test (AUDIT) [64]. Participants are randomized to one of three conditions, a motivational interviewing/problem-solving alcohol and adherence intervention, a time matched motivational interviewing/problem-solving “wellness” intervention, and treatment as usual. Alcohol use and HIV medication adherence will be assessed at baseline, three-, six-, and 12 months using interviews and biological specimens. Finally, a process evaluation will assess counselors’ and participants’ perceptions of acceptability and effectiveness.
This trial will provide important evidence regarding the effectiveness and feasibility of using a lay counselor-delivered integrated intervention to address alcohol use and HIV medication nonadherence. Additionally, if the intervention is effective, authors indicate they will offer training to other staff at the clinics and other interested health workers on how to screen and deliver the intervention. This has important implications for sustainability of the intervention. When this stage of implementation is reached, ongoing evaluation is needed as to when clinic-based counselors, as opposed to lay counselors hired for research purposes, are feasibly and competently able to deliver the CBT intervention.
5.3 Case 3: Task Shifting CBT for Depression in HIV Primary Care in Zimbabwe—the “Friendship Bench”
Chibanda et al. [3] trained lay health workers in HIV primary care in Harare, Zimbabwe in problem-solving therapy for depression. Although not focused on HIV specifically, over half of all patients in the trial (52 %) presented with an HIV-related problem, and the treatment was implemented at primary care clinic sites that treat a large percentage of HIV-infected patients in this region. This case illustration describes the process of training and supervising the lay health workers and implementing the “Friendship Bench” intervention in Harare, Zimbabwe. We present results from the initial implementation trial for the Case Illustration, although the Friendship bench continues to be ongoing in these clinic settings. Current priorities include scaling up the Friendship bench to other clinic settings, particularly in rural Zimbabwe, and integrating with evidence-based ART adherence counseling [50].
5.3.1 Interventionist Training
In the pilot implementation trial (Chibanda et al. [3]), 20 lay health workers were trained in a locally adapted problem-solving therapy intervention. Lay health workers in this setting are intended to support nurses in primary care and are locally called “ambuya utano” or “grandmother health provider.” The lay health workers support individuals living with HIV/AIDS and TB, provide psychological counseling and HIV medication adherence counseling, and promote community health education in designated geographic areas. In the setting where the trial took place, the lay workers were female, literate, had at least primary school education, and had lived locally for at least 15 years. An eight-day training was conducted by two psychologists with expertise in problem-solving therapy, a general nurse, and a psychiatrist. The training included education on common mental disorders, including a locally defined depressive disorder (“kufungisisa,” or thinking too much; [65]), skills to identify common mental disorders using a local, standardized screener (Shona Symptom Questionnaire; [66]), and how to deliver the locally adapted problem-solving therapy. For the study, 10 lay health workers were randomly selected to participate in the pilot trial. These individuals received ongoing training every two weeks for the first six months and then monthly.
5.3.2 Interventionist Supervision
Supervision for the lay health workers included a weekly, one hour long group supervision led by a general nurse with prior counseling training. Group supervision was also conducted by a clinical psychologist one hour every two weeks, and by a psychiatrist monthly for 45 minutes. The lay workers also participated in a daily peer support group facilitated by one of the lay health workers.
5.3.3 Friendship Bench Approach
At the clinic settings, clients can be referred or can self-refer to the “Friendship bench”—a large wooden bench located under a tree adjacent to the clinic setting—which was available daily from 9 am to 12 pm. During the implementation trial, one lay worker was responsible for the bench daily and would approach the bench after a client sat on it to deliver a problem-solving therapy session. The problem-solving therapy intervention included basic problem-solving strategies (i.e., identifying problems, brainstorming practical and feasible solutions, and selecting and implementing a solution). Patients received feedback on their symptoms on the Shona Symptom Questionnaire, including psychoeducation on kufungisisa. The intervention was locally adapted for lay health worker delivery. Up to six sessions of problem-solving therapy were offered either at the Friendship bench or in the patient’s home. Home visits included prayer with family, which was seen as an essential component for appropriateness of the intervention in the local Zimbabwean culture. For patients with kufungisisa or extreme poverty, problem-solving therapy was also enhanced with activity scheduling and local income-generating activities (peanut butter making, recycling).
5.3.4 Implementation Trial Results
The lay health workers evaluated the problem-solving therapy intervention (i.e., rated the “ease with which they learned the problem-solving therapy approach, delivered it, and proportion of patients who appeared to benefit from it”). Focus groups were also conducted following implementation of the Friendship Bench. These groups pointed to successes of the program, including a view that the providers were trustworthy and wise, that patients received motivation and support from home visits, and that the approach minimized stigma associated with mental health treatment. The lay health workers also reported that the structure of the therapy approach supported them in monitoring progress, in particular the step of problem-solving therapy of breaking down problems into specific/manageable steps. Over the course of the research study, 320 patients used the Friendship bench. All patients completed a minimum of three sessions over six weeks, with 30 % completing all six sessions. After a minimum of three sessions, there was a meaningful clinical reduction in clinical symptoms (on the SSQ). This approach using peer- and nurse-led supervision, with an option for specialist referral, which was utilized very infrequently, was seen as a potentially sustainable model for task shifting in this community, and continues to be ongoing, with intended efforts for larger scale-up in rural areas.
6 Summary and Considerations for Task Shifting CBT in Resource-Poor Settings
Across these examples of task shifting CBT for behavioral health needs among HIV-infected individuals in sub-Saharan Africa, although still in early phases, it seems that task shifting CBT across the examples provided was feasible, appropriate, and acceptable to patients. In some cases, paraprofessional delivery, as illustrated in formative qualitative work in South Africa to develop an alcohol/adherence intervention [55], may even be preferable (i.e., using a peer or fellow HIV treatment recipient as the provider). This may not be so surprising considering the leading addiction programs across the world are peer-led [67]. Whether lay counselors are able to deliver a more complicated integrated intervention [51, 56] will answer important questions on the types of interventions paraprofessionals are most well suited to deliver. These decisions will likely need to consider the advantages and disadvantages of incorporating multiple treatment targets in an integrated treatment protocol (i.e., improved efficiency yet also potentially added complexity that may reduce feasibility or acceptability for training, supervision, and long-term therapist skill acquisition).
As indicated above, the primary CBT techniques that have been used in sub-Saharan Africa among HIV-infected patients have been problem-solving therapy, motivational interviewing, and activity scheduling. Although a bit outside the scope of this chapter, there has also been extensive work evaluating trauma focused CBT (TF-CBT) in Zambia and Tanzania [68, 69] among youth, as well as adapting interpersonal psychotherapy to treat depression in Uganda [70]. Interpersonal psychotherapy has also been delivered by lay counselors to address depression among HIV-infected individuals in South Africa [71].Across these studies, when adapting CBT techniques for resource-limited settings, often the key consideration in the adaptation is cultural modification and adapting for paraprofessional delivery while also maintaining the core components of the intervention. Given that many CBT manuals are initially tested and developed using masters- or doctoral-level therapists in high income countries, considering changes to the treatment manual and training procedures for lay counselors or health care workers with no background in psychology or counseling is essential. Often these modifications include (1) focusing on how training is conducted; (2) simplifying terms and avoiding clinical jargon; and (3) adapting the structure of supervision. Regarding cultural adaptations, changes may include ensuring appropriate delivery within a local context, linguistic modifications, and including local idioms, metaphors, and stories, as well as adapting for low literacy populations. For instance, while there is no empirical support for home-based prayer with family in the treatment of depression, providers in Zimbabwe felt that it was inappropriate to remove, and that the treatment would no longer be acceptable to patients or families if not included [3]. Another example of the importance of community buy-in when selecting and adapting the intervention approach was in Papas et al. [5] in which the primary treatment target (alcohol as opposed to other HIV-related health behaviors) was decided upon locally and that the community urged for this to be the focus. These adaptations reflect a larger literature on community-based participatory research (CBPR) that identifies the need to have the community dictate research- and clinical priorities [72, 73].
It is interesting to note that across the aforementioned clinical examples of task shifting, CBT was selected or deemed to be appropriate in process evaluations for paraprofessional delivery given its structured format. Although easier for training purposes, the structured format may be challenging at times for lay counselor providers not familiar with structured CBT type approaches in learning how to maintain a primary focus on the key intervention target (e.g., adherence), particularly when patients may also request addressing other health behaviors in the context of the intervention. Ongoing considerations when adapting CBT in this type of setting should consider maintaining a structured, manual format and assessing what types of manuals are most easy to use by counselors (e.g., workbooks, flip manuals; [6, 74]). That being said, dissemination and implementation research models have indicated that the more flexible the delivery of an intervention the greater the likelihood for ultimate adoption in clinical settings [75–77]. As such, finding a balance between providing structure and allowing for some flexibility in delivery, for instance using a modular approach [78, 79], may be necessary.
7 Novel Approaches Using Technology
Technology-based platforms to support the delivery of evidence-based behavioral HIV care have emerged in resource-limited settings, for instance using text messaging (SMS) reminders support for adherence [80] and using multimedia-based interventions to standardize the delivery of evidence-based interventions. One example of using a computer-, multimedia-based intervention as a means to support task shifting of adherence counseling in South Africa is the “Masivukeni” (“let’s wake up”) intervention. Currently being evaluated in a randomized clinical trial in South Africa [46], the intervention is a six-session lay counselor-delivered intervention that uses multimedia to help counselors track delivery of specific intervention components and to explain complex concepts to patients in a straightforward, visual way. The computer program includes scripted text, imagery, animations, audio, and video to delivery information and provides a structured agenda for each session. The intervention program only requires basic computer familiarity (e.g., how to use a mouse and keyboard, open and close programs). The intervention is based on social action theory (SAT; [48]) and utilizes some CBT strategies (i.e., problem-solving barriers to adherence, social support). Each 45 min session includes interactive multimedia components to provide psychoeducation on HIV medication adherence and problem solve barriers to adherence (for greater description of the intervention, see Remien et al. [46]). The program tracks activities, time spent on activities and sessions, and patient responses. These built-in features of activity tracking allow for supervision that is not human resource-intensive and thereby addresses the problem of limited resources for supervision. The program also allows for easy printing of personalized patient data that can be used by counselors and patients, and can save information/questions session to session to enable reviewing at subsequent sessions. A screener for mental health and substance use is incorporated in the program and gives automated scoring and referral scripts to the counselor, enabling counselors with modest training to make critical referral for mental health and substance use problems that may compromise medical adherence [46]. Although the intervention is still being tested, recently published pilot data (n = 55) indicate that the Masivukeni intervention was associated with improvements in HIV medication adherence (measured as clinic-based pill count data), more positive attitudes towards disclosure and medication social support, and better clinic–patient relationships compared to treatment as usual adherence counseling [47]. In formative work, the intervention was also found to be feasible and acceptable for lay counselor delivery [46]. If it proves effective, feasible, and acceptable in the larger trial, multimedia-based platforms may be a potentially useful strategy to promote sustainable implementation of task shifting models delivering CBT in HIV care in sub-Saharan Africa.
8 Moving from Effectiveness to Implementation Research for Task Shifting CBT
Alongside the promising results of effectiveness trials of CBT using task shifting models, clear implementation challenges emerge from these examples of task shifting CBT in this setting. Primary implementation challenges include poor role definition or clarity on scope of work for lay counselors, lack of standardized training, and inadequate supervision, support, and compensation. For long-term sustainability, a primary consideration is whether activities would be feasible if conducted in a clinic-based setting without any additional research resources. For instance, the amount of training and supervision described in each of the examples may likely not be sustainable in a real-world clinical setting. For instance, in the Papas et al. [4, 5] studies, counselors received 175–300 h of training and supervision prior to starting to see patients for the trial that included not only didactics, but also role plays, videotaped feedback, and supervised sessions with rated CBT skill use. Indeed, in that study, transitioning supervision and training to local supervisors was not attained, and the US-based lead investigator remained on-site throughout the course of the study to maintain her responsibilities of in-person supervision.
The model for supervision seemed to fully embody a task shifting approach in the Friendship Bench, as it was a tiered approach using daily peer supervision, weekly nurse-led supervision, and supervision with a clinical psychologist and psychiatrist once every two weeks and monthly, respectively [3]. Although this is likely also more intensive than would be feasible in a non-research context, it is a good example of a task shifting model of supervision for this intervention. Additionally, in one study [5], numerous efforts were made to reduce barriers to attendance that may not be feasible in non-research contexts, such as text and phone call appointment reminders, reimbursement for transportation, and in some cases, transportation to the first CBT session. When a later stage of implementation is reached outside the context of a research study, ongoing evaluation is needed as to when clinic-based counselors, as opposed to lay counselors hired for research purposes, are feasibly and competently able to deliver the CBT intervention. Another important consideration when considering efforts to implement CBT in clinical settings outside of a research context will be how to standardize selection of paraprofessional counselors. Papas et al. [4, 5] aimed to hire for natural talents (empathy, emotional perceptiveness, good communication and analytical skills) assessed using case conceptualizations and behavioral role plays. It remains an empirical question whether this selection approach is effective and feasible in a real-world clinical setting. If task shifting CBT for behavioral medicine conditions proves to be feasible and effective in the ongoing work, it may be a particularly appealing approach to meet the needs for integrating behavioral health interventions into HIV care in sub-Saharan Africa [81].
9 Conclusions and Resources
In conclusion, task shifting behavioral medicine CBT interventions for ART adherence and co-occurring mental health problems for individuals living with HIV/AIDS is a promising and essential strategy for meeting the treatment needs in the context of a specialized provider shortage in sub-Saharan Africa. Addressing ART adherence concerns and the co-occurring mental health problems which disrupt ART adherence are key to the success of biomedical treatment as prevention efforts to curbing the HIV/AIDS epidemic in sub-Saharan Africa. In many ways task shifting of biomedical ART programs can only succeed in the context of also task shifting evidence-based CBT interventions to promote ART adherence and viral suppression. For readers interested in more details on task shifting efforts for behavioral medicine in sub-Saharan Africa, please visit these resources:
-
1.
Africa Focus on Intervention Research for Mental Health (AFFIRM) http://www.affirm.uct.ac.za/affirm-aims: A research and capacity development hub in six sub-Saharan African countries: Ethiopia, Ghana, Malawi, South Africa, Uganda, and Zimbabwe—evaluating task shifting/sharing interventions for mental health disorders delivered by community health workers in South Africa and Ethiopia.
-
2.
Programme for Improving Mental health carE (PRIME) http://www.prime.uct.ac.za/: An initiative focused on implementing and scaling up of treatment programs for mental disorders, with a focus on community involvement, and health service and system strengthening.
-
3.
Emerging Mental Health Systems in Low- and Middle-Income Countries (EMERALD) http://www.emerald-project.eu: An initiative focused on strengthening the health system (training/resources/infrastructure etc.) to lay the groundwork for universal mental health care coverage at the primary care level.
Notes
- 1.
Throughout the chapter we use the term “task shifting” to refer to both task shifting and task sharing.
References
World Health Organization. Task shifting: Rational redistribution of tasks among health workforce teams: global recommendations and guidelines. Geneva, Switzerland: WHO Press; 2008.
Padmanathan P, De Silva MJ. The acceptability and feasibility of task-sharing for mental healthcare in low and middle income countries: a systematic review. Soc Sci Med. 2013;97:82–6.
Chibanda D, Mesu P, Kajawu L, Cowan F, Araya R, Abas MA. Problem-solving therapy for depression and common mental disorders in Zimbabwe: piloting a task-shifting primary mental health care intervention in a population with a high prevalence of people living with HIV. BMC Public Health. 2011;11:828. doi:10.1186/1471-2458-11-828.
Papas RK, Sidle JE, Gakinya BN, et al. Treatment outcomes of a stage 1 cognitive-behavioral trial to reduce alcohol use among human immunodeficiency virus-infected out-patients in western Kenya. Addiction. 2011;106(12):2156–66. doi:10.1111/j.1360-0443.2011.03518.x.
Papas RK, Sidle JE, Martino S, et al. Systematic cultural adaptation of cognitive-behavioral therapy to reduce alcohol use among HIV-infected outpatients in western Kenya. AIDS Behav. 2010;14(3):669–78. doi:10.1007/s10461-009-9647-6.
Andersen LS, Magidson JF, O’Cleirigh C, Remmert JE, Kagee A, Leaver M, Stein DJ, Safren SA, Joska J. A pilot study of a nurse-delivered cognitive behavioral therapy intervention (Ziphamandla) for adherence and depression in HIV in South Africa. Journal of Health Psychology. 2016.
American Cancer Society. Cancer in Africa. Atlanta: American Cancer Society Inc; 2011.
Diabetes Leadership Forum. Diabetes: the hidden pandemic and its impact on Sub-Saharan Africa. 2010. http://www.changingdiabetesbarometer.com/docs/Diabetes%20in%20sub-saharan%20Africa.pdf.
UNAIDS. The Gap report. 2014. http://www.unaids.org/sites/default/files/en/media/unaids/contentassets/documents/unaidspublication/2014/UNAIDS_Gap_report_en.pdf.
Ahmat A, Bilal N, Herbst H, Weber S. How many health workers? In: Soucat A, Scheffler R, Ghebreyesus TA, editors. The labor market for health workers in Africa: a new look at the crisis. Washington, DC: World Bank; 2013.
Maddison AR, Schlech WF. Will universal access to antiretroviral therapy ever be possible? The health care worker challenge. Can J Infect Dis Med Microbiol. 2010;21(1):e64–9.
World Health Organization. Achieving the health-related MDGs. It takes a workforce! Geneva: World Health Organization; 2015.
Saxena S, Thornicroft G, Knapp M, Whiteford H. Resources for mental health: scarcity, inequity, and inefficiency. Lancet. 2007;370(9590):878–89. doi:10.1016/S0140-6736(07)61239-2.
WHO Int. Taking Stock. Task shifting to tackle health worker shortages. 2006. http://www.who.int/healthsystems/task_shifting_booklet.pdf.
Harries AD, Hargreaves NJ, Gausi F, Kwanjana JH, Salaniponi FM. High death rates in health care workers and teachers in Malawi. Trans R Soc Trop Med Hyg. 2002;96(1):34–7.
Huddart J, Picazo O. The health sector human resource crisis in Africa: an issues paper. Washington, DC: United States Agency for International Development; 2003.
Naicker S, Eastwood JB, Plange-Rhule J, Tutt RC. Shortage of healthcare workers in Sub-Saharan Africa: a nephrological perspective. Clin Nephrol. 2010;74 Suppl 1:S129–33.
Mills EJ, Kanters S, Hagopian A, et al. The financial cost of doctors emigrating from Sub-Saharan Africa: human capital analysis. BMJ. 2011;343, d7031.
Mullan F, Frehywot S, Omaswa F, et al. Medical schools in Sub-Saharan Africa. Lancet. 2011;377(9771):1113–21. doi:10.1016/S0140-6736(10)61961-7.
WHO. Working together for health: the world health report 2006. 2006. http://www.who.int/whr/2006/whr06_en.pdf?ua=1.
Mdege ND, Chindove S, Ali S. The effectiveness and cost implications of task-shifting in the delivery of antiretroviral therapy to HIV-infected patients: a systematic review. Health Policy Plan. 2013;28(3):223–36. doi:10.1093/heapol/czs058.
Callaghan M, Ford N, Schneider H. A systematic review of task- shifting for HIV treatment and care in Africa. Hum Resour Health. 2010;8:8. doi:10.1186/1478-4491-8-8.
Mwai GW, Mburu G, Torpey K, Frost P, Ford N, Seeley J. Role and outcomes of community health workers in HIV care in Sub-Saharan Africa: a systematic review. J Int AIDS Soc. 2013;16:18586.
Gimbel-Sherr SO, Micek MA, Gimbel-Sherr KH, et al. Using nurses to identify HAART eligible patients in the Republic of Mozambique: results of a time series analysis. Hum Resour Health. 2007;5:7. doi:10.1186/1478-4491-5-7.
Bangsberg DR, Perry S, Charlebois ED, Clark RA, Roberston M, Zolopa AR, Moss A. Non-adherence to highly active antiretroviral therapy predicts progression to AIDS. Aids. 2001;15(9):1181–3.
Mills EJ, Nachega JB, Buchan I, et al. Adherence to antiretroviral therapy in Sub-Saharan Africa and North America: a meta-analysis. JAMA. 2006;296(6):679–90. doi:10.1001/jama.296.6.679.
Palombi L, Marazzi MC, Guidotti G, et al. Incidence and predictors of death, retention, and switch to second-line regimens in antiretroviral- treated patients in Sub-Saharan African Sites with comprehensive monitoring availability. Clin Infect Dis. 2009;48(1):115–22.
Schneider H, Hlophe H, van Rensburg D. Community health workers and the response to HIV/AIDS in South Africa: tensions and prospects. Health Policy Plan. 2008;23(3):179–87. doi:10.1093/heapol/czn006.
Schneider H, Lehmann U. Lay health workers and HIV programmes: implications for health systems. AIDS Care. 2010;22 Suppl 1:60–7. doi:10.1080/09540120903483042.
Lewin SA, Dick J, Pond P, et al. Lay health workers in primary and community health care. Cochrane Database Syst Rev. 2005;1, CD004015. doi:10.1002/14651858.CD004015.pub2.
Price J, Binagwaho A. From medical rationing to rationalizing the use of human resources for AIDS care and treatment in Africa: a case for task shifting. Dev World Bioeth. 2010;10(2):99–103. doi:10.1111/j.1471-8847.2010.00281.x.
Iwu EN, Holzemer WL. Task shifting of HIV management from doctors to nurses in Africa: clinical outcomes and evidence on nurse self-efficacy and job satisfaction. AIDS Care. 2014;26(1):42–52. doi:10.1080/09540121.2013.793278.
Mukora R, Charalambous S, Dahab M, Hamilton R, Karstaedt A. A study of patient attitudes towards decentralisation of HIV care in an urban clinic in South Africa. BMC Health Serv Res. 2011;11:205. doi:10.1186/1472-6963-11-205.
Assefa Y, Kiflie A, Tekle B, Mariam DH, Laga M, Van Damme W. Effectiveness and acceptability of delivery of antiretroviral treatment in health centres by health officers and nurses in Ethiopia. J Health Serv Res Policy. 2012;17(1):24–9. doi:10.1258/jhsrp.2011.010135.
Boyer S, Protopopescu C, Marcellin F, et al. Performance of HIV care decentralization from the patient’s perspective: health-related quality of life and perceived quality of services in Cameroon. Health Policy Plan. 2012;27(4):301–15. doi:10.1093/heapol/czr039.
Ledikwe JH, Kejelepula M, Maupo K, et al. Evaluation of a well-established task-shifting initiative: the lay counselor cadre in Botswana. PLoS One. 2013;8(4), e61601. doi:10.1371/journal.pone.0061601.
Hermann K, Van Damme W, Pariyo GW, et al. Community health workers for ART in Sub-Saharan Africa: learning from experience—capitalizing on new opportunities. Hum Resour Health. 2009;7:31. doi:10.1186/1478-4491-7-31.
Berman PA, Gwatkin DR, Burger SE. Community-based health workers: head start or false start towards health for all? Soc Sci Med. 1987;25(5):443–59.
Gilson L, Walt G, Heggenhougen K, et al. National community health worker programs: how can they be strengthened? J Public Health Policy. 1989;10(4):518–32.
Igumbor JO, Scheepers E, Ebrahim R, Jason A, Grimwood A. An evaluation of the impact of a community-based adherence support programme on ART outcomes in selected government HIV treatment sites in South Africa. AIDS Care. 2011;23(2):231–6. doi:10.1080/09540121.2010.498909.
Rabkin M, El-Sadr WM. Why reinvent the wheel? Leveraging the lessons of HIV scale-up to confront non-communicable diseases. Glob Public Health. 2011;6(3):247–56. doi:10.1080/17441692.2011.552068.
Nakimuli-Mpungu E, Bass JK, Alexandre P, et al. Depression, alcohol use and adherence to antiretroviral therapy in Sub-Saharan Africa: a systematic review. AIDS Behav. 2012;16(8):2101–18. doi:10.1007/s10461-011-0087-8.
Shield KD, Rylett M, Gmel G, Gmel G, Kehoe-Chan TAK, Rehm J. Global alcohol exposure estimates by country, territory and region for 2005—a contribution to the comparative risk assessment for the 2010 global burden of disease study. Addiction. 2013;108(5):912–22. doi:10.1111/add.12112.
Labbe A, Yeterian J, Wilner J, Kelly J. Cognitive and behavioral approaches for treating substance use disorders among behavioral medicine patients. In: Vranceau A, Safren S, Greer J, editors. Massachusetts general hospital handbook of behavioral medicine. New York: Springer; 2016.
Blashill A, Dale S, Jampel J, Safren S. HIV. In: Vranceaunu A, Greer J, Safren S, editors. Massachusetts general hospital handbook of behavioral medicine. New York: Springer; 2016.
Remien RH, Mellins CA, Robbins RN, et al. Masivukeni: development of a multimedia based antiretroviral therapy adherence intervention for counselors and patients in South Africa. AIDS Behav. 2013;17(6):1979–91. doi:10.1007/s10461-013-0438-8.
Robbins RN, Mellins CA, Leu C-S, et al. Enhancing lay counselor capacity to improve patient outcomes with multimedia technology. AIDS Behav. 2015;19:163–76. doi:10.1007/s10461-014-0988-4.
Ewart CK. Social action theory for a public health psychology. Am Psychol. 1991;46(9):931–46.
Sorsdahl K, Myers B, Ward CL, et al. Adapting a blended motivational interviewing and problem-solving intervention to address risky substance use amongst South Africans. Psychother Res. 2014;25:435–44. doi:10.1080/10503307.2014.897770.
Bere T, Nyamayaro P, Magidson J, et al. Cultural adaptation of a cognitive-behavioral intervention to improve adherence to antiretroviral therapy among people living with HIV/AIDS in Zimbabwe: “Nzira Itsva.” J Health Psychol. In press.
Dewing S, Mathews C, Schaay N, Cloete A, Louw J, Simbayi L. “It’s important to take your medication everyday okay?” An evaluation of counselling by lay counsellors for ARV adherence support in the Western Cape, South Africa. AIDS Behav. 2013;17(1):203–12. doi:10.1007/s10461-012-0211-4.
Simoni JM, Pearson CR, Pantalone DW, Marks G, Crepaz N. Efficacy of interventions in improving highly active antiretroviral therapy adherence and HIV-1 RNA viral load. J Acquir Immune Defic Syndr. 2006;43 Suppl 1:S23–35. doi:10.1097/01.qai.0000248342.05438.52.
Bärnighausen T, Chaiyachati K, Chimbindi N, Peoples A, Haberer J, Newell M-L. Interventions to increase antiretroviral adherence in Sub-Saharan Africa: a systematic review of evaluation studies. Lancet Infect Dis. 2011;11(12):942–51. doi:10.1016/S1473-3099(11)70181-5.
Jones DL, Ross D, Weiss SM, Bhat G, Chitalu N. Influence of partner participation on sexual risk behavior reduction among HIV-positive Zambian women. J Urban Health 2005;82(3 Suppl 4):iv92–iv100.
Kekwaletswe CT, Morojele NK. Alcohol use, antiretroviral therapy adherence, and preferences regarding an alcohol-focused adherence intervention in patients with human immunodeficiency virus. Patient Prefer Adherence. 2014;8:401–13. doi:10.2147/PPA.S55547.
Parry CD, Morojele NK, Myers BJ, et al. Efficacy of an alcohol-focused intervention for improving adherence to antiretroviral therapy (ART) and HIV treatment outcomes—a randomised controlled trial protocol. BMC Infect Dis. 2014;14:500. doi:10.1186/1471-2334-14-500.
Safren SA, Otto MW, Worth JL. Life-steps: applying cognitive-behavioral therapy to patient adherence in HIV medication treatment. Cogn Behav Pract. 1999;6:332–41.
Safren S, Gonzalez J, Soroudi N. Coping with chronic illness: a cognitive-behavioral therapy approach for adherence and depression. Therapist guide. New York: Oxford University Press; 2008.
Kidia K, Machando D, Bere T, et al. “I was thinking too much”: experiences of HIV-positive adults with common mental disorders and poor adherence to antiretroviral therapy in Zimbabwe. Trop Med Int Health. 2015;20(7):903–13. doi:10.1111/tmi.12502.
Braithwaite RS, Nucifora KA, Kessler J, et al. Impact of interventions targeting unhealthy alcohol use in Kenya on HIV transmission and AIDS-related deaths. Alcohol Clin Exp Res. 2014;38(4):1059–67. doi:10.1111/acer.12332.
Carroll KM, Nich C, Sifry RL, et al. A general system for evaluating therapist adherence and competence in psychotherapy research in the addictions. Drug Alcohol Depend. 2000;57(3):225–38.
Parsons JT, Rosof E, Punzalan JC, Maria LD. Integration of motivational interviewing and cognitive behavioral therapy to improve HIV medication adherence and reduce substance use among HIV-positive men and women: Results of a pilot project. AIDS Patient Care STDS. 2005;19(1):31–9. doi:10.1089/apc.2005.19.31.
Mimiaga MJ, Reisner SL, Pantalone DW, O’Cleirigh C, Mayer KH, Safren SA. A pilot trial of integrated behavioral activation and sexual risk reduction counseling for HIV-uninfected men who have sex with men abusing crystal methamphetamine. AIDS Patient Care STDS. 2012;26(11):681–93. doi:10.1089/apc.2012.0216.
Barbor TF, de la Fuente JR, Sunder J, Grant M. AUDIT: the alcohol use disorders identification test. Guidelines for use in primary health care. Geneva: World Health Organization; 1992.
Patel V, Araya R, Bolton P. Treating depression in the developing world. Trop Med Int Health. 2004;9(5):539–41. doi:10.1111/j.1365-3156.2004.01243.x.
Patel V, Simunyu E, Gwanzura F, Lewis G, Mann A. The Shona symptom questionnaire: the development of an indigenous measure of common mental disorders in Harare. Acta Psychiatr Scand. 1997;95(6):469–75.
Alcoholics anonymous. 2001. http://www.aa.org/.
O’Donnell K, Dorsey S, Gong W, Ostermann J, Whetten R, Cohen JA, Itemba D, Manongi R, Whetten K. Treating maladaptive grief and posttraumatic stress symptoms in orphaned children in Tanzania: Group‐based trauma‐focused cognitive–behavioral therapy. Journal of traumatic stress. 2014;27(6):664–71.
Murray LK, Familiar I, Skavenski S, et al. An evaluation of trauma focused cognitive behavioral therapy for children in Zambia. Child Abuse Negl. 2013;37(12):1175–85. doi:10.1016/j.chiabu.2013.04.017.
Bolton P, Bass J, Neugebauer R, et al. Group interpersonal psychotherapy for depression in rural Uganda: a randomized controlled trial. JAMA. 2003;289(23):3117–24. doi:10.1001/jama.289.23.3117.
Petersen I, Bhana A, Baillie K, MhaPP Research Programme Consortium. The feasibility of adapted group-based interpersonal therapy (IPT) for the treatment of depression by community health workers within the context of task shifting in South Africa. Community Mental Health J. 2012;48(3):336–41.
Tapp H, White L, Steuerwald M, Dulin M. Use of community-based participatory research in primary care to improve healthcare outcomes and disparities in care. J Comp Eff Res. 2013;2(4):405–19. doi:10.2217/cer.13.45.
Stacciarini J-MR, Shattell MM, Coady M, Wiens B. Review: community-based participatory research approach to address mental health in minority populations. Community Ment Health J. 2011;47(5):489–97. doi:10.1007/s10597-010-9319-z.
Andersen L, Joska J, Safren S. Life steps for ART adherence. 2013. http://hivmentalhealth.co.za/wp-content/uploads/2013/05/Life-Steps-ART-Adherence1.pdf.
Glasgow RE, Vogt TM, Boles SM. Evaluating the public health impact of health promotion interventions: the RE-AIM framework. Am J Public Health. 1999;89(9):1322–7.
Thorpe KE, Zwarenstein M, Oxman AD, et al. A pragmatic–explanatory continuum indicator summary (PRECIS): a tool to help trial designers. CMAJ. 2009;180(10):E47–57. doi:10.1503/cmaj.090523.
Damschroder LJ, Aron DC, Keith RE, Kirsh SR, Alexander JA, Lowery JC. Fostering implementation of health services research findings into practice: a consolidated framework for advancing implementation science. Implement Sci. 2009;4:50. doi:10.1186/1748-5908-4-50.
Safren S, O’Cleirigh C, Tan JY, et al. A randomized controlled trial of cognitive behavioral therapy for adherence and depression (CBT-AD) in HIV-infected individuals. Health Psychol. 2009;28(1):1–10. doi:10.1037/a0012715.
Safren S, O’Cleirigh CM, Bullis JR, Otto MW, Stein MD, Pollack MH. Cognitive behavioral therapy for adherence and depression (CBT-AD) in HIV-infected injection drug users: a randomized controlled trial. J Consult Clin Psychol. 2012;80(3):404–15. doi:10.1037/a0028208.
Pop-Eleches C, Thirumurthy H, Habyarimana JP, et al. Mobile phone technologies improve adherence to antiretroviral treatment in a resource-limited setting: a randomized controlled trial of text message reminders. AIDS. 2011;25(6):825–34. doi:10.1097/QAD.0b013e32834380c1.
Kaaya S, Eustache E, Lapidos-Salaiz I, Musisi S, Psaros C, Wissow L. Grand challenges: improving HIV treatment outcomes by integrating interventions for co-morbid mental illness. PLoS Med. 2013;10(5), e1001447. doi:10.1371/journal.pmed.1001447.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer Science+Business Media New York
About this chapter
Cite this chapter
Magidson, J.F., Gouse, H., Psaros, C., Remmert, J.E., O’Cleirigh, C., Safren, S.A. (2017). Task Shifting and Delivery of Behavioral Medicine Interventions in Resource-Poor Global Settings: HIV/AIDS Treatment in sub-Saharan Africa. In: Vranceanu, AM., Greer, J., Safren, S. (eds) The Massachusetts General Hospital Handbook of Behavioral Medicine. Current Clinical Psychiatry. Humana Press, Cham. https://doi.org/10.1007/978-3-319-29294-6_14
Download citation
DOI: https://doi.org/10.1007/978-3-319-29294-6_14
Published:
Publisher Name: Humana Press, Cham
Print ISBN: 978-3-319-29292-2
Online ISBN: 978-3-319-29294-6
eBook Packages: MedicineMedicine (R0)