Abstract
Based on continuous monitoring of the pressure reactivity index (PRx), we defined individualized intracranial pressure (ICP) thresholds by graphing the relationship between ICP and PRx. We hypothesized that an “ICP dose” based on individually assessed ICP thresholds might correlate more closely with 6-month outcome compared with ICP doses derived from the recommended universal thresholds of 20 and 25 mmHg. Data from 327 patients with severe traumatic brain injury (TBI) were analyzed. ICP doses were computed as the cumulative area under the curve above the defined thresholds in graphing ICP versus time. The term Dose 20 (D20) was used to refer to an ICP threshold of 20 mm Hg. The markers D25 and DPRx were calculated similarly. The discriminative ability of each dose with regard to mortality was assessed by receiver operating characteristics analysis using fivefold cross-validation (CV). DPRx was found to be the best discriminator of mortality, despite the fact that D20 was twice as large as DPRx. Individualized doses of intracranial hypertension were stronger predictors of mortality than doses derived from the universal thresholds of 20 and 25 mm Hg. The PRx could offer a method of individualizing the ICP threshold.
This work was performed in the Academic Neurosurgical Unit and the Neurosciences Critical Care Unit of Addenbrooke’s Hospital, University of Cambridge, Cambridge, UK
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Intracranial pressure
- Cerebrovascular pressure reactivity
- Neuromonitoring
- Clinical outcome
- Traumatic brain injury
Introduction
Intracranial hypertension has been closely linked to adverse outcomes after severe traumatic brain injury (TBI). Data from observational studies and noncontrolled series have suggested thresholds ranging from 15 to 25 mmHg [1, 8, 12, 14, 16]. The latest guideline of the Brain Trauma Foundation (BTF) identified a lack of level-1 evidence and recognized that, rather than accepting a generic, absolute intracranial pressure (ICP) threshold, an attempt should be made to individualize thresholds based on patient characteristics [3]. Cerebrovascular pressure reactivity is defined as the ability of vascular smooth muscle to respond to changes in transmural pressure and is one of the key mechanisms responsible for the autoregulation of cerebral blood flow [13]. Pressure reactivity can be determined by observing the response of ICP to changes in mean arterial pressure and is monitored via the pressure reactivity index (PRx), as suggested by Czosnyka et al. [6, 7, 17]. We defined patient-specific, pressure reactivity-guided ICP thresholds by graphing the relationship between ICP and PRx over the total monitoring time for each patient. We hypothesized that an “ICP dose” based on a disturbed pressure reactivity ICP threshold might correlate more closely with clinical outcome compared with an ICP dose calculated using the generic, recommended thresholds of 20 and 25 mmHg. The detailed findings of this study have been already published in the Journal of Neurosurgery. Here, we provide a synopsis of our work and make a further comment relating to previously unpublished findings on the absolute doses of intracranial hypertension.
Materials and Methods
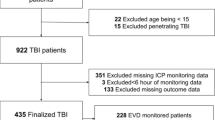
We retrospectively analyzed anonymized digital recordings of arterial blood pressure (ABP) and ICP waveforms from 327 consecutive patients with severe TBI who were admitted to the neurocritical care unit at Addenbrooke’s Hospital between 2003 and 2009. The clinical outcome at 6 months was assessed using the Glasgow Outcome Scale (GOS) [10]. Physiological signals were recorded using a laptop computer with ICM+ software (University of Cambridge, Cambridge Enterprise, Cambridge, UK, http://www.neurosurg.cam.ac.uk/icmplus) [15]. The PRx was calculated as a short-term moving Pearson correlation coefficient between changes in 30 consecutive 10-s averages of ABP, and corresponding ICP signals (with an 80 % overlap of data). Based on the continuous measurement and monitoring of PRx we defined patient-specific, individualized ICP thresholds. These thresholds were visually identified from graphs of PRx versus ICP over the total monitoring time for each patient individually. A cutoff of PRx > 0.2 was used; the value for the ICP threshold was accepted only if the graph showed a distinct change in PRx values from less than 0.2 to consistently exceeding 0.2. To quantify the physiological insult from intracranial hypertension, we computed “ICP dose” as the cumulative area under the curve (AUC) above a defined threshold. The trapezoidal method was used to calculate doses from graphs of ICP versus time; the ICP “dose” is measured in millimeters of mercury per hour (mm Hg*h) [18]. For an ICP threshold of 20 mmHg, we named this Dose 20 (D20). Using the same methodology we calculated D25 and DPRx. Identification of ICP thresholds and calculation of doses were blinded to clinical outcome.
The predictive ability of each dose on mortality was assessed. Receiver operating characteristic (ROC) curves were calculated and the AUC was used as a measure of discriminative ability and after adjusting for baseline Glasgow Coma Scale (GCS) score, age, and sex. Because the observed AUCs are “over fit” to the data, to determine how well the ICP doses would perform in terms of prediction, fivefold cross-validation (CV) of each covariate adjusted model was performed. Cross-validated results provide an estimate of how well the different ICP doses would predict mortality in a new data set. Statistical analyses were performed using SAS 9.3 and R 2.14.2.
Results
Only the results pertaining to ICP thresholds, doses, and ROC analysis are reported here. A clearly identifiable threshold, based on the set criteria, was possible in 224 patients (68 %). Mean, median, interquartile range (IQR), and standard deviation (SD) for the ICP threshold based on PRx were 25, 24, 20–32, and 10, respectively. Separate logistic regression models with mortality as the outcome and dose as the predictor (both alone and adjusted for covariates GCS score, age, and gender) were fitted. In the covariate adjusted logistic regression model, all doses calculated were significantly associated with mortality (D20 p < 0.0001, D25 p < 0.0001, and DPRx p < 0.0001). Further, DPRx (0.81, CI 0.74–0.87) was found to have the highest AUC over both D20 (0.75, CI 0.68–0.81) and D25 (0.77, CI 0.70–0.83), indicating that it has the best discriminative ability. Cross-validation confirmed the results of the observed AUCs; in the cross-validated model, DPRx was still the best predictor of mortality (DPRx AUC 0.77, 95 % CI 0.68–0.89; D20 0.72, 95 % CI 0.66–0.81; and D25 0.65, 95 % CI 0.56–0.73). Mean D20 was 1,055 mmHg*h vs 478 mmHg*h for DPRx (p < 0.0001). The relationship between ICP doses and mean ICP for all patients is shown in Fig. 1; Fig. 2 depicts the distribution of DPRx per GOS score, with a statistically significant higher dose sustained by patients who died.
Discussion
We explored the predictive ability of individualized ICP thresholds based on the PRx, compared with “standard” fixed ICP thresholds. We found that the ICP doses derived from an index describing the status of cerebrovascular pressure reactivity were stronger predictors of 6-month mortality than doses calculated based on the “suggested” ICP threshold of 20 mmHg and also from a second fixed threshold of 25 mmHg. Recent publications have challenged the traditional understanding of the monitoring and treatment of high ICP. The DECRA trial showed that decompressive craniectomy, despite effectively reducing ICP, did not translate into improved neurological outcomes [5]. Our findings are further pertinent in view of the recent publication of the randomized controlled trial (RCT) of ICP monitoring in severe TBI by Chesnut et al. [4] This was the first RCT to compare the management of intracranial hypertension based on the monitoring and treatment of ICP above the fixed threshold of 20 mmHg, versus a protocol based on clinical examination and neuroimaging. No benefit of one protocol over the other was found. An important aspect of interpreting the results should be the limitation of using fixed, universal ICP thresholds and thus disregarding patient-specific pathophysiology. We chose to quantify secondary brain injury due to intracranial hypertension by using a method that takes into account the cumulative extent and duration of these episodes. The method computes a “dose” of intracranial hypertension as the cumulative AUC above a defined threshold; it takes into account both the degree and the duration of ICP elevation [2, 9, 11, 18]. An additional advantage, as pointed out by Vik et al., is that the predictive power of doses for different thresholds can be explored. Here, we explored different thresholds by calculating doses based on pressure reactivity and comparing them against doses derived from the conventionally accepted threshold of 20 mmHg and from a second fixed threshold of 25 mmHg, as this is the recommended range in the BTF guidelines. To our knowledge, this is the first report to attempt the determination of individualized patient-specific ICP thresholds in patients with severe TBI, using these thresholds to quantify ICP dose per patient, and comparing these doses with those derived from the currently accepted generic thresholds of 20–25 mmHg. It should be noted that the mean dose, as calculated by the threshold of 20 mmHg, was significantly larger (double, in fact) than the mean dose derived based on disturbed PRx; nevertheless, DPRx was a better predictor of mortality, suggesting that it might not necessarily be the absolute dose that affects outcome, but intracranial hypertension in the face of ineffective pressure reactivity.
We were able to identify a PRx-based ICP threshold in two thirds of our patients; apart from technical limitations, an inability to identify a threshold could be physiologically interpreted as a state of dissociation between cerebrovascular pressure reactivity and mean ICP. We conclude that the predictive ability of individualized ICP thresholds based on the continuous monitoring of cerebrovascular pressure reactivity is stronger than the fixed thresholds of 20 and 25 mmHg, in a large single-center database of patients with severe TBI. Monitoring of the PRx could supplement ICP monitoring by offering patient-specific pathophysiological information.
References
Balestreri M, Czosnyka M, Hutchinson PJ, Steiner LA, Hiler M, Smielewski P, Pickard JD (2006) Impact of intracranial pressure and cerebral perfusion pressure on severe disability and mortality after head injury. Neurocrit Care 4:8–13
Barton CW, Hemphill JC, Morabito D, Manley G (2005) A novel method of evaluating the impact of secondary brain insults on functional outcomes in traumatic brain-injured patients. Acad Emerg Med 12:1–6
Bratton SL, Chestnut RM, Ghajar J, McConnell Hammond FF, Harris OA, Hartl R et al (2007) Guidelines for the management of severe traumatic brain injury. VIII. Intracranial pressure thresholds. J Neurotrauma 24(Suppl 1):S55–S58
Chesnut RM, Temkin N, Carney N, Dikmen S, Rondina C, Videtta W et al (2012) A trial of intracranial-pressure monitoring in traumatic brain injury. N Engl J Med 367(26):2471–2481
Cooper DJ, Rosenfeld JV, Murray L, Arabi YM, Davies AR, D'Urso P, DECRA Trial Investigators, Australian and New Zealand Intensive Care Society Clinical Trials Group et al (2011) Decompressive craniectomy in diffuse traumatic brain injury. N Engl J Med 364:1493–1502
Czosnyka M, Smielewski P, Kirkpatrick P, Laing RJ, Menon D, Pickard JD (1997) Continuous assessment of the cerebral vasomotor reactivity in head injury. Neurosurgery 41(1):11–17
Czosnyka M, Smielewski P, Kirkpatrick P, Piechnik S, Laing R, Pickard JD (1998) Continuous monitoring of cerebrovascular pressure-reactivity in head injury. Acta Neurochir Suppl 71:74–77
Eisenberg H, Frankowski R, Contant C, Marshall LF, Walker MD (1998) High-dose barbiturate control of elevated intracranial pressure in patients with severe head injury. J Neurosurg 69:15–23
Hemphill JC III, Barton CW, Morabito D, Manley GT (2005) Influence of data resolution and interpolation method on assessment of secondary brain insults in neurocritical care. Physiol Meas 26:373–386
Jennett B, Bond M (1975) Assessment of outcome after severe brain damage. Lancet 1:480–484
Kahraman S, Dutton RP, Hu P, Xiao Y, Aarabi B, Stein DM, Scalea TM (2010) Automated measurement of “pressure times time dose” of intracranial hypertension best predicts outcome after severe traumatic brain injury. J Trauma 69(1):110–118
Marmarou A, Anderson RL, Ward JD, Choi SC, Young HF, Eisenberg HM et al (1991) Impact of ICP instability and hypotension on outcome in patients with severe head trauma. J Neurosurg 75:S59–S66
Paulson OB, Strandgaard S, Edvinsson L (1990) Cerebral autoregulation. Cerebrovasc Brain Metab Rev 2:161–192
Schreiber MA, Aoki N, Scott B, Beck JR (2002) Determination of mortality in patients with severe blunt head injury. Arch Surg 137:285–290
Smielewski P, Lavinio A, Timofeev I, Radolovich D, Perkes I, Pickard JD, Czosnyka M (2008) ICM+, a flexible platform for investigations of cerebrospinal dynamics in clinical practice. Acta Neurochir Suppl 102:145–151
Sorrentino E, Diedler J, Kasprowicz M, Budohoski KP, Haubrich C, Smielewski P et al (2012) Critical thresholds for cerebrovascular reactivity after traumatic brain injury. Neurocrit Care 16(2):258–266
Steiner LA, Czosnyka M, Piechnik SK, Smielewski P, Chatfield D, Menon DK, Pickard JD (2002) Continuous monitoring of cerebrovascular pressure reactivity allows determination of optimal cerebral perfusion pressure in patients with traumatic brain injury. Crit Care Med 30(4):733–738
Vik A, Nag T, Fredriksli OA, Skandsen T, Moen KG, Schirmer-Mikalsen K, Manley GT (2008) Relationship of “dose” of intracranial hypertension to outcome in severe traumatic brain injury. J Neurosurg 109(4):678–684
Acknowledgments
The authors acknowledge great support from Addenbrooke’s Hospital Neurocritical Care Unit staff and Academic Neurosurgical Unit registrars, without whose help the collection of computerized data would never have succeeded. We also acknowledge Ming Yang MS for statistical assistance.
Conflicts of Interest and Source of Funding
The software for brain monitoring ICM+ (http://www.neurosurg.cam.ac.uk/icmplus) is licensed by the University of Cambridge (Cambridge Enterprise). Mr Czosnyka and Mr Smielewski have a financial interest in part of the licensing fee. Mr Hutchinson is supported by an Academy of Medical Sciences/Health Foundation Senior Scientist Fellowship and grants from the Medical Research Council/NIHR. Mr Menon is supported by funding from the Medical Research Council, the NIHR Cambridge Biomedical Centre, and an NIHR Senior Investigator award. Mr Pickard is a NIHR senior investigator awardee and a principal investigator within the NIHR Biomedical Research Centre (Cambridge University Hospital Foundation Trust) and lead principal investigator for the Medical Research Council “Acute Brain Injury Programme” grant. The remaining authors have not disclosed any potential conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Lazaridis, C., Smielewski, P., Menon, D.K., Hutchinson, P., Pickard, J.D., Czosnyka, M. (2016). Patient-Specific Thresholds and Doses of Intracranial Hypertension in Severe Traumatic Brain Injury. In: Ang, BT. (eds) Intracranial Pressure and Brain Monitoring XV. Acta Neurochirurgica Supplement, vol 122. Springer, Cham. https://doi.org/10.1007/978-3-319-22533-3_23
Download citation
DOI: https://doi.org/10.1007/978-3-319-22533-3_23
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-22532-6
Online ISBN: 978-3-319-22533-3
eBook Packages: MedicineMedicine (R0)