Abstract
The search for a completely noninvasive intracranial pressure (ICPni) monitoring technique capable of real-time digitalized monitoring is the Holy Grail of brain research. If available, it may facilitate many fundamental questions within the range of ample applications in neurosurgery, neurosciences and translational medicine, from pharmaceutical clinical trials, exercise physiology, and space applications. In this work we compare invasive measurements with noninvasive measurements obtained using the proposed new noninvasive method. Saline was infused into the spinal channel of seven rats to produce ICP changes and the simultaneous acquisition of both methods was performed. The similarity in the invasive and noninvasive methods of ICP monitoring was calculated using Pearson’s correlation coefficients (r). Good agreement between measures < r > = 0.8 ± 0.2 with a range 0.28–0.96 was shown.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Intracranial pressure (ICP) is the pressure inside the cranial cavity and is directly associated with three components of this space: the parenchymal component consisting of the brain structures, the cerebrospinal fluid (CSF) component consisting of the CSF of the ventricles and the subarachnoid space, and the vascular component characterized by the circulating blood in the brain. The ratio of pressure among these three components is constantly adjusted to maintain a balance in the intracranial system, and ICP maintenance within its normal values depends on the preservation of intracranial volume. ICP monitoring is a very important topic in neurology and neurosurgery and can be used in the diagnosis and prognosis of various disorders, for example, stroke, hydrocephalus, tumors, and trauma.
In the case of hydrocephalus, for instance, which is a pathological process that interferes with the production, circulation and absorption of CSF, with serious consequences, such as intracranial hypertension [1], the main difficulty is the late diagnosis of the disease, since the symptoms of brain degeneration (mainly manifested by symptoms of dementia) can be similar to those of Alzheimer’s disease. However, normal-pressure hydrocephalus is a treatable disease and virtually reversible, if diagnosed early. The use of an ICP monitor can facilitate medical decisions in these and other cases.
In the 1960s, Lundberg introduced continuous intraventricular pressure monitoring in the neurointensive clinic. This method, based on an intraventricular catheter connected to a pressure transducer at the level of the external auditory meatus, has remained the gold standard ever since [2]. The main limitation of this method is the risk of infection, which increases over time and is within the range of 6–11 % [3, 4]. Owing to the traumatic nature of the method, difficulties concerning the surgical procedure, especially when the cerebral ventricles are compressed, and the relatively high infection rate, other methods have been introduced. These include an epidural transducer, a subdural bolt via a burr hole, a subdural catheter, preoperative placement of a subdural needle, and intraparenchymal transducer, lumbar spinal fluid pressure, and lumbar epidural pressure [2]. The idea of a noninvasive method of measuring ICP is captivating, as complications seen in relation to the invasive methods of ICP measurement, that is, hemorrhage and infection, are avoidable [5].
The search for a completely noninvasive intracranial pressure (ICPni) monitoring technique capable of real-time digitalized monitoring is the Holy Grail of brain research. If available, the range of ample applications in neurosurgery, neurosciences, and translational medicine, from pharmaceutical clinical trials, exercise physiology, and space applications, are some of the unique challenges in this field. This study is aimed at measuring the correlation coefficient between invasive and noninvasive measurements of ICP in rats. The new noninvasive monitoring method consists of a strain gauge fixed on a mechanical device that touches the surface of the scalp in the parietal region lateral to the sagittal suture. The equipment is able to detect small changes in the dimensions of the skull resulting from pressure changes inside, without the need for surgery or shaving the patient’s head. This new noninvasive sensor opens new avenues in the field of ICP and brain monitoring, mainly in clinical pictures where ICP monitoring had been previously impossible owing to the invasiveness of the current methods.
Materials and Methods
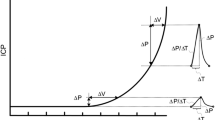
The ICPni system (Braincare Corp.) associates the skull deformation with ICP detection and changes [6], and it includes a signal amplifier and an analog-to-digital converter. The noninvasive sensor (Fig. 1) consists of a support for a sensor bar for the detection of local skull bone deformations, adapted with strain sensors. Detection of these deformations is obtained by a cantilever bar modeled by finite elements calculations. To this bar, strain gauges are attached for strain detection. Noninvasive contact with the skull is obtained by adequate pressure directly on the scalp by a pin.
Changes in ICP cause deformations in the skull bone detected by the sensor bar. Variations in ICP lead to deformations in the bar, which are captured by the strain sensors. The equipment filters, amplifies, and digitalizes the signal from the sensor, and sends the data to a computer.
To induce dynamic changes for a direct comparison of the time series response for the invasive (intraparenchymatous – Codman) and ICPni methods, 0.9 % saline infusions into the spinal channel were performed. The animals (n = 7, 300–350 g) were anesthetized with ketamine (95 mg/kg) and xylasine (12 mg/kg) and the noninvasive sensor was positioned on the skin of the animals, in the parietal region opposite the invasive sensor. The baseline was monitored and then saline bolus injection was started until the invasive sensor presented substantial changes in ICP (20–40 mmHg). The number of infusions for each animal is shown in (Table 1).
Time series were obtained with the acquisition rate of 200 Hz. Data smoothing was implemented with a 10-s moving average window. Data analysis was performed using the ICM+ (Cambridge Enterprises) and MatLab® software.
Results
To measure the similarity in the responses of the invasive and noninvasive methods to the increase in ICP, Pearson’s correlation coefficients (r) were calculated. Figures 2 and 3 present typical time series for the two methods. Mean r value results showed good agreement, <r > = 0.8 ± 0.2 with a range 0.28–0.96. The values of the noninvasive measure (mV) are related to the invasive measure (mmHg) according to the slopes and intercepts of regression lines between ICPi and ICPni. The values obtained ranged from 25 to 1073 (mmHg/mV), showing some variability owing to noninvasive sensor installation. Regarding infusion procedures, because of the variable experimental conditions among the animals (mainly movement artifacts due to the short anesthesia time), it was not possible to perform the same infusion protocol in all experiments. The last column of (Table 1) shows the number of infusions for each animal.
Discussion
It has been reported in the literature that one of the main disadvantages of noninvasive techniques is the lack of accuracy compared with their invasive counterparts. Additionally, another marked disadvantage is that noninvasive ICP monitoring cannot be carried out on a large percentage of patients owing to anatomical variations, leading us to conclude that current noninvasive techniques cannot be used as alternatives to the invasive techniques [5]. However, from the above results, we were able to demonstrate experimentally that this novel ICPni method is capable of monitoring with good sensitivity and agreement the mean value dynamics of ICP when simultaneously compared with an invasive technique. Nevertheless, other aspects such as calibration methodology for ICPni measurement and clinical applications of this method still need to be developed in further studies.
References
Machado ABM (2004) Neuroanatomia Funcional, 2nd edn. Atheneu, São Paulo
Kolsen-Petersen JA, Dahl BL, Cold GE (2008) Monitoring of intracranial pressure (ICP): a review. In: Monitoring of cerebral and spinal haemodynamics during neurosurgery. Springer Berlin Heidelberg, Denmark pp 1–58
Mayhall CG, Archer NH, Lamb VA et al (1984) Ventriculostomy-related infections. A prospective epidemiological study. N Eng J Med 310:553–559
Aucoin PJ, Kotilainen HR, Gantz NM et al (1986) Intracranial pressure monitors. Epidemiologic study of risk factors and infections. Am J Med 80:369–376
Raboel PH, Bartek Jr J, Andresen M, Bellander BM, Romner B et al (2012) Intracranial pressure monitoring: invasive versus non-invasive methods — A review. Crit Care Res Pract 2012:950393, doi:10.1155/2012/950393
Mascarenhas S, Vilela GHF (2013) Noninvasive intracranial pressure system. Patent No. WO/2013/041973. United States Patent and Trademark Office
Acknowledgments
Conselho Nacional de Desenvolvimento e Pesquisa (CNPq), Fundação de Amparo a Pesquisa do Estado de São Paulo (FAPESP), Brazilian Ministry of Health, Pan American Health Organization – World Health Organization (PAHO-WHO), and Sapra Corp for financial support.
Conflict of interest
ICM+ is a software program for brain monitoring in clinical/experimental neurosciences, licensed by Cambridge Enterprise Ltd (www.neurosurg.cam.ac.uk/icmplus). MC has an interest in part of the licensing fee. The remaining authors declare that they have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Cabella, B. et al. (2016). Validation of a New Noninvasive Intracranial Pressure Monitoring Method by Direct Comparison with an Invasive Technique. In: Ang, BT. (eds) Intracranial Pressure and Brain Monitoring XV. Acta Neurochirurgica Supplement, vol 122. Springer, Cham. https://doi.org/10.1007/978-3-319-22533-3_18
Download citation
DOI: https://doi.org/10.1007/978-3-319-22533-3_18
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-22532-6
Online ISBN: 978-3-319-22533-3
eBook Packages: MedicineMedicine (R0)