Abstract
The musculoskeletal system is comprised of three distinct tissue categories: structural mineralized tissues, actuating muscular soft tissues, and connective tissues. Where connective tissues – ligament, tendon and cartilage – meet with bones, a graded interface in mechanical properties occurs that allows the transmission of load without creating stress concentrations that would cause tissue damage. This interface typically occurs over less than 1 mm and contains a three order of magnitude difference in elastic stiffness, in addition to changes in cell type and growth factor concentrations among others. Like all engineered tissues, the replication of these interfaces requires the production of scaffolds that will provide chemical and mechanical cues, resulting in biologically accurate cellular differentiation. For interface tissues however, the scaffold must provide spatially graded chemical and mechanical cues over sub millimetre length scales. Naturally, this complicates the manufacture of the scaffolds and every stage of their subsequent cell seeding and growth, as each region has different optimal conditions. Given the higher degree of difficulty associated with replicating interface tissues compared to surrounding homogeneous tissues, it is likely that the development of complex musculoskeletal tissue systems will continue to be limited by the engineering of connective tissues interfaces with bone.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
The interface between bone and soft tissues such as tendon, ligament or cartilage is characterized by a multiphasic interface containing spatial gradients in mechanical properties, structure and cell type. These gradients exist over a distance of less than 1 mm and serve to mediate load transfer between highly dissimilar tissues by minimizing stress concentrations. As mechanical mediators in the musculoskeletal system, the insertion sites of ligaments or tendons with bone, or the bone-cartilage (osteochondral) interface, have high incidences of acute and long-term injury respectively (United States Bone & Joint Initiative 2011). Principal sites of failure are the rotator cuff tendon (600,000 surgeries in the US per year (Yamaguchi 2011)), the anterior cruciate ligament (ACL) (100,000 surgeries in the US per year (AAOS 2014)), and osteoarthritis of the hip joint (580,000 surgeries in the US in 2013 (OECD 2013)). Additionally, current surgical repair techniques for many of these tissues are largely unsatisfactory as they do not regenerate the complex structure of the natural interface (Rodeo et al. 1993). Given the variety and prevalence of failures, repair or regeneration of interface tissues remains a significant clinical challenge.
This chapter begins by discussing the anatomy and materials involved in two distinct types of natural interface tissues: the ligament or tendon insertion site and the osteochondral interface. This will include a discussion of the challenges associated with determining the mechanical properties of these highly heterogeneous tissues. The bulk of the chapter contains an outline of specific strategies and methods employed when engineering interface tissues. Firstly, scaffold specific methods concerning manufacture, mechanics and composition will be considered. Secondly, exogenous factors in the system such as growth factors will be discussed. Thirdly, cellular factors concerning cell type and cell differentiation will be reviewed. Overall, the methods required and problems associated with generating biomimetic gradients will be considered for each of the factors influencing the tissue replication process.
2 Structure of Natural Interface Tissues
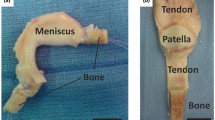
Connective tissues in the musculoskeletal system are subdivided into tendons (bone-muscle interactions in tension), ligaments (bone-bone interactions in tension) and cartilage (bone-bone interactions in compression). In this section we will discuss these tissues and their interface with mineralized tissue, primarily bone.
2.1 Ligament and Tendon Insertions
Bone is a stiff rigid connective tissue consisting of a highly organized extra cellular matrix (ECM) of type I collagen fibers, interconnected with stiffening hydroxyapatite (Ca10(PO4)6(OH)2) mineral deposits. Bone mineral is highly impure, containing 3 % by weight structural water (Yoder et al. 2012), and around 15 % substitution of carbonate (\( {\mathrm{CO}}_3^{2-} \)) ions for either OH− or PO4+ groups (Elliott 1994). This composite is maintained by an extensive vascular and nervous system along with the “osteo” group of cells: osteoclasts, osteoblasts and osteocytes. Bone’s primary function is to support and protect the soft tissues surrounding it, while the central marrow maintains and produces populations of the blood cells. Ligaments and tendons are compliant, hydrated, connective tissues whose primary function is to transmit tensile forces between either two bones, or a bone and a muscle respectively. They consist of 86 wt% (dry) highly aligned type I collagen, assembled into a hierarchical structure of fibrils (Amiel et al. 1984). The remainder of the ligament or tendon is a proteoglycan matrix surrounding rows of fibroblast cells. The insertion site (enthesis) of the ligament or tendon into bone can be between 100 μm and 1 mm across (Evans et al. 1990; Genin et al. 2009) with a structure that can vary from ligament to ligament and even between two ends of the same ligament. From an anatomical perspective the insertion of ligaments or tendons into SCB) is subdivided into two broad designations: direct (fibrocartilagenous) entheses and indirect (fibrous) entheses.
The medial collateral ligament (MCL) insertion into the femur and the supraspinatus tendon insertion into the humerus are both typical examples of a direct, fibrocartilaginous enthesis. At direct insertions the deep fibers of the ligament or tendon join perpendicular to the bone surface through a multi-tissue fibrocartilagenous transition of four distinct yet continuous zones (Fig. 11.1). These are pure ligament or tendon, unmineralized fibrocartilage, mineralized fibrocartilage and subchondral bone (Yahia and Newman 1970; Benjamin et al. 1986).
The structure of a direct insertion of a ligament or tendon enthesis with bone. Ligament and tendon contain highly aligned, hierarchical collagen fibrils containing elongated fibroblast cells. In the unmineralized fibrocartilage the degree of collagen organization and alignment goes down and the cells become rounder chondrocytes. In the mineralized fibrocartilage the organic structure remains unchanged but hydroxyapatite crystals begin to fill the interfibrillar space. Finally, the mineralized fibrocartilage forms an interdigitated interface with subchondral bone containing mature osteocytes and the canaliculi that interconnect them
Zone 1, ligament or tendon, consists of highly aligned collagen fibrils supporting fibroblasts with minimal vascularization and nerve supply as it approaches the enthesis. In zone 2, the tissue transforms into unmineralized fibrocartilage, where the cells become more rounded chondrocytes and the degree of collagen alignment lowers to 8° deviation from the tendon alignment (Genin et al. 2009). Zone 3, known as mineralized fibrocartilage, is histologically separated from zone 2 by the mineralization tidemark (Benjamin et al. 1986) but contains similar chondrocytic cell populations as in zone 2. Zone 4 is bone proper and hence is characterized by significant intrafibrillar mineral content, vascularization, a neural network, and the presence of the osteo group of cells to conduct bone remodelling.
The degree and location of mineralization across the two fibrocartilaginous regions of the enthesis is not completely conclusive. The classical view, stemming from histological staining, is that the mineral content increases abruptly at the clear visual mineralization tidemark. This is supported by SEM energy dispersive x-ray analysis (EDAX) of the bovine patellar tendon (Moffat et al. 2008), along with Fourier transform infrared spectroscopy imaging (FTIR-I) of the bovine (ACL) (Spalazzi et al. 2007). Conversely, Raman spectroscopy of the rat supraspinatus tendon insertion has shown a linearly increasing phosphate ion content, and hence mineral content, across the combined width of both fibrocartilaginous regions (Wopenka et al. 2008; Genin et al. 2009). Hence, a single rule governing mineral distribution across all entheses is not yet known, and the specific microstructure and composition must be considered on a tissue-by-tissue basis.
Indirect entheses differ from direct insertions in that the ligament or tendon fibres approach the bone surface at an acute angle where the outer fibers blend into the periosteum. The deep fibers penetrate directly into the outer SCB) via Sharpey’s fibers (Lui et al. 2010) with little to no fibrocartilaginous transition and often just a mineralization tidemark separating the two tissues under microscopy (Walsh 2007). This results in a characteristically less mechanically robust interface for indirect insertions (Benjamin and Ralphs 1998). An example of an indirect insertion would include the tibial insertion of the MCL.
2.2 The Osteochondral Interface
Cartilage is an avascular, aneural tissue that lines joints to aid in low friction movement and serves to resist compressive forces in the joint. Cartilage consists of a network of type II collagen, filled with a proteoglycan containing fluid phase, with a large internal osmotic pressure. Volume constraints imposed by the collagen network on the proteins that occupy the fluid filled space cause the tissue to swell and load the collagen fibrils in tension (Mow et al. 1992).
The bone-cartilage junction is characterized by a zone of calcified cartilage (ZCC) approximately 100–200 μm across (Hunziker et al. 2002). Thus giving an interface structure that is similar in size to, but less differentiated than, the four region ligament insertions. The ZCC forms during postnatal development via calcification of the basal layer of the overlaying hyaline cartilage. The calcification front is known as the tidemark and can be clearly seen on histological sections as an undulating line (Fig. 11.2). Types II and V collagen that make up hyaline cartilage, extend across the ZCC and remain highly hydrated in this region and hence less densely packed compared to the neighbouring subchondral bone (SCB) . It is the hydration, proteoglycans, collagen type and presence of hypertrophic chondrocytes that makes this region a calcified cartilage as opposed to bone that is lacking osteo group cells. Mineral particles in the ZCC are of a similar composition size and distribution to that found in bone (Zizak et al. 2003). The mineral content across the ZCC varies greatly from tissue to tissue. Because of the cartilage-like structure of this region, there is a large proportion of fluid filled interfibrillar space. When mineral is secreted from the SCB, some proportion of this fluid is displaced, allowing for large variations in the degree of mineralization, depending on the quantity of mineral secreted from SCB) . Many studies have shown that the mineral concentration increases across the ZCC as you progress from the bone towards the tidemark with cartilage proper (Reid and Boyde 1987; Ferguson et al. 2003; Gupta et al. 2005). These studies should be considered as a rebuttal to the commonly held belief that the mineral concentration forms a functional gradient across the ZCC. The width of the ZCC is limited on the bone side by the vascular front, beyond which bone remodelling by the group of osteo cells is limited, and on the cartilage side by the progression of the mineral tidemark into the unmineralized cartilage.
The osteochondral interface occurring at the medial femoral condyle of a human knee. The three regions of the osteochondral interface: Hyaline Cartilage (HC), Calcified Cartilage Zone (CCZ) and the Subchondral Bone (SB) can be seen. Von Kossa staining of this tissue shows the mineralization in each region of the interface (scale bar in CCZ region: 327 μm) (Reproduced with permission from Zhang (2012))
2.3 Mechanical Properties of Interface Tissues
Ligament or tendon entheses, or the osteochondral junction, serve to join two tissues with multiple orders of magnitude differences in mechanical properties. Ligament, tendon and cartilage have indentation moduli in the region 1–100 MPa (Hauch et al. 2009; McKee et al. 2011). Whereas the SCB) they anchor to has an indentation modulus three orders of magnitude larger, approximately 10 GPa (Bembey et al. 2006).
The challenge of mechanical integration of two materials with vastly disparate moduli arises in many engineering contexts. A common solution to this is to use functional gradients in microstructure and composition that give rise to similar functional gradients in mechanical properties. Thus, alleviating problems related to strength, stiffness and fracture at the material interface (Suresh and Mortenson 1998). Hence, a fundamental understanding of the structure-function relationships, and the mechanical properties they give rise to in the native tissue, is essential for successful tissue engineering solutions. Yet, direct measurement of the mechanical properties of either ligament or tendon entheses, or the osteochondral junction, is difficult due to their highly heterogeneous nature coupled with the small length scales involved.
Many of the issues associated with direct measurement of the interface have been bypassed with bulk compression or tensile experiments, where microscopic video analysis , or ultrasound scanning , was used to determine local strain across the different zones of the interface. Bulk compression of the enthesis of the bovine ACL showed a smooth and gradual increase in strain from the bone, through the mineralized and unmineralized fibrocartilage, to the pure ligament, suggesting a corresponding decrease in modulus over the same region (Moffat et al. 2008). Similar observations of the local strain distribution in the bovine ACL enthesis were obtained from ultrasound during cyclic tensile testing of a whole femur-ACL-tibia complex (Spalazzi et al. 2006b).
Direct measurement of mechanical properties of interface tissues at severely dehydrated conditions can be conducted using nanoindentation. Dehydrating the osteochondral region of human patellae (Gupta et al. 2005) caused the soft tissue to stiffen so significantly that nanoindentation mapping with sharp indenters (as would be conducted on a weld metal or ceramic composite) could be conducted. Their nanoindentation results, alongside quantitative backscattering SEM, revealed that the morphology of the gradients in mechanical properties closely match that of the mineral distribution. This is in accordance with the idea that the elastic properties of mineralized tissues can be predicted from the mineral volume fraction and will follow particulate composite bounds regardless of length scale (Oyen and Ko 2008; Ferguson 2009). Yet, the mechanism by which mineral concentration gives rise to tissue stiffening can be considered more complex than just a volume fraction composite bounds problem. It has also been suggested by theoretical analysis in Oyen et al. and simulations by Genin et al. that significant tissue stiffening occurs when the mineral concentration becomes sufficient that a mechanically continuous network of crystals has formed within the collagen fibers (Oyen et al. 2008; Genin et al. 2009).
In contrast to severely dehydrated tissues, direct measurement of mechanical properties at biologically relevant conditions is more challenging. Both Hauch et al. (2009) and Abraham and Haut Donahue (2013) conducted nanoindentation of hydrated meniscal attachment sites using a 150 μm radius spherical tip. Their line mapping suggests that the mechanical transition occurs over a wide 200 μm region spanning the mineralization tidemark. For this tissue, this is equivalent to approximately half way through the unmineralized fibrocartilage to half way through the mineralized fibrocartilage. However, these experimental conditions give an indenter-sample contact patch of 25–40 μm in diameter at SCB) and soft tissue respectively, thus inducing indentation specific artefacts in the results. Finite element simulations by this author show that indentation at length scales equivalent to material heterogeneities results in the transition region of modulus appearing wider than it actually is (Armitage and Oyen 2015). In Fig. 11.3, the dashed line shows an approximation of the stress field during indentation, for a material with a sharp transition in modulus. From this it can be seen that any indent close to the interface gives a modulus that is a non-uniform average of a region bridging the interface. Hence, when the indenter contact patch is of a similar size to, or larger than the material heterogeneity, the width of the transition region in the observed function of modulus appears much wider than the true function of modulus. As such, the true nature of the transition in mechanical properties of the ligament or tendon enthesis, or the osteochondral interface, remains inconclusive. This is due to a combination of lack of direct testing at native conditions and issues associated with testing heterogeneous materials with a probe of a similar size to the material heterogeneities.
The stress field occuring during indentation over a material containing a sharp transition in elastic modulus. The dark right hand side signifies the stiff material and the lighter left hand side the more compliant material. It can be seen that the stiffer side deforms out into the more compliant side during indentation. The dashed line represents a typical stress field under the indenter. It can be seen that if the contact patch is similar in size, or larger than the interface region, that the stress field extends outside the interface range being tested in a non-uniform manner
3 Engineering of Tissue Interfaces
As discussed above, the interfaces between ligaments and tendons with bone, or cartilage with bone, are a key site of injury or long-term degradation in the musculoskeletal system. Additionally, these interfaces are some of the most complex tissues to regenerate due to their small size and high degree of heterogeneity in mechanical properties, microstructure, composition and cell phenotype. Tissue engineering methods have already been implemented for replication of many of the homogenous tissues involved in these interfaces such as bone (Amini et al. 2012), ligament (Yilgor et al. 2012), tendon (Butler et al. 2008) and cartilage (Moutos and Guilak 2008). Yet, in the current state of the field, biomimetic fixation to bone of the homogeneous tissue engineered ligament or tendon graft is a key obstacle to successful clinical implementation. Natively, the variety of distinct tissues that are present at the interface, interact with one another to provide the physiological function of mediating load transfer between vastly different parts of the musculoskeletal system. Thus the aim of tissue engineering in this field is to replicate the structure-function relationships of the native tissue interfaces, and allow the engineered tissues to replicate the same physiological function. In this section we will discuss the strategies associated with replicating the natural structure-function relationships that allow this to happen. This includes material specific scaffold properties, cellular influences, and the application of external stimuli such as growth factors.
3.1 Scaffolds
Scaffolds in tissue engineering replace the function of the natural ECM and hence provide the medium through which cells, soluble proteins, mechanical cues and other external factors are delivered to the growing tissue. Additionally, the chemical, mechanical and topographical properties of the scaffold on a microscopic level, constitute a significant proportion of signalling in the cellular microenvironment, and hence have a large degree of control over cellular differentiation and growth. For the reproduction of an interface tissue the scaffold needs to mimic the gradient in structural organisation, biological factors and mechanical properties that are present in the natural tissue. There are two main approaches to the construction of scaffolds aiming to replicate the graduated properties of a natural interface tissue. The first is to create a number of discrete phases that each mimic a single region of the natural tissue, these can then be either chemically or mechanically joined to create an interface scaffold. The second option is to produce a single mass of scaffold material that is graded during manufacture to replicate an interface tissue.
Discrete scaffolds , made of a number of separate homogeneous scaffolds that are then joined together, are the easiest and most obvious option for multiphase scaffolds to replicate interface tissues. Examples of this for osteochondral interface reproduction include: (Schaefer et al. 2000), where seeded and cultured bone and cartilage scaffolds were sutured together to create an interface tissue; or (Niederauer et al. 2000) where polymer bone and cartilage scaffolds were glued together prior to culture. Yet, if significant care is not taken over the joining method then issues arise with scaffolds created in this way. The microstructure of the interface between regions of discretely joined scaffolds can result in a lack of interconnectivity between the two porous networks, inhibiting cellular infiltration, nutrient transport and cell-cell signalling between the two populations. Signalling between the cell populations in different regions of the growing tissue is known to be important for regulating tissue growth and viability in the ligament enthesis (Jiang et al. 2005; Wang et al. 2007). Furthermore, the primary in situ function of interface tissues is to mediate the joining of highly dissimilar materials. Hence, mechanical or chemical joining of discrete tissues in an abrupt manner results in a lack of mechanical integration at the interface, that is unlikely to adequately replace the natural biomechanical function in this region.
A gold standard example of a ligament enthesis scaffold, where distinct regions have been interconnected to give a graded structure, can be found in (Spalazzi et al. 2006a, 2008). In this work, three phases were individually synthesized as follows: a fibrous poly(lactic-co-glycolic acid) (PLGA) 10:90 knitted mesh for ligament fibroblast culture; a sintered network of PLGA 85:15 microspheres for chondrocyte culture of the fibrocartilaginous regions; and a sintered network of PLGA 85:15 and bioactive glass microspheres for osteoblast culture of a bony region. These three phases were sintered together to maintain a degree of similarity and structural continuity throughout the scaffold (PLA continuity at the ligament-fibrocartilaginous interface and PLGA continuity at the fibrocartilaginous-osseous interface). Subsequently the scaffold was tri-cultured in a subcutaneous rat model with fibroblast, chondrocyte and osteoblast cell lines pre-seeded in each region respectively. This resulted in mineralization localized to the osseous scaffold phase, and a distribution of collagen types that mimicked those found in natural tissue (Wang et al. 2006).
Continuously graded scaffolds, or those consisting of distinct regions that have been fully interconnected and integrated with one another prior to cell seeding, are more complex to produce but alleviate many of the issues with discrete scaffolds. Within these scaffolds gradients in pore size, mechanical properties and scaffold chemistry can all be used to influence region specific cell proliferation, or differentiation, to induce distinct localized tissue types. Yet, all of these factors are highly interdependent. Microscopic matrix stiffness, as felt in the immediate cellular environment is dependent on polymer choice, which affects surface chemistry. Pore size will affect macroscopic material properties and permeability, and hence influence fluid flow and cell-cell signalling within the scaffold. Hence, researchers must take significant care during scaffold design, as many symbiotic parameters must be prioritized simultaneously. Fabrication methods for continuously graded scaffolds will be discussed later.
3.1.1 Scaffold Properties
Pore size has been shown to be important for cell proliferation, with each of the primary cell types involved in interface tissues having an ideal range of pore sizes for optimal tissue growth. In general, fibroblasts and chondrocytes favour smaller pores compared to osteo group cells that favour larger pores. Specifically, fibroblasts and chondrocytes proliferate well on the surface of substrates with pores on the order of 10 μm but struggle to penetrate the bulk of the scaffold (Nehrer et al. 1997; Bhardwaj et al. 2001; Lowery et al. 2010). Scaffolds with pores in the range 70–120 μm have been observed to promote both chondrocyte and fibroblast proliferation throughout the scaffold pore structure (Salem et al. 2002; Griffon et al. 2006). In bone scaffolds the minimum pore size as determined by cell sizes is approximately 100 μm. Yet, pore size being approximately equal to cell size results in a lack of vascularization and hypoxic conditions, resulting in many papers concluding that osteogenesis is best served by pore sizes greater than 300 μm (Karageorgiou and Kaplan 2005; Murphy et al. 2010). However, an upper functional limit is also placed on pore size by the mechanical integrity of the scaffold, which is often desired to be stiffest in bony regions. Gradients in pore size through an interface scaffold can be achieved using a number of techniques such as freeze drying, graded hydrogels or functionally graded electrospinning, all of which will be discussed herein.
Mechanical properties of interface tissue engineering scaffolds are important factors that help to regulate cell phenotype expression (stem cells) or culture viability (bi or tri-culture of pre-differentiated cell lines). Scaffold mechanical properties can be considered on two length scales. On a microscopic scale (tens of microns in the immediate cellular microenvironment) the wall stiffness of foam-like porous scaffolds, or the individual fiber stiffness of fibrous scaffolds, heavily influences phenotype expression or culture viability. Cells attach to the ECM via mechanosensitive focal adhesion protein complexes (Chen 2008). These attachments allow them to probe their surroundings by actively pulling on the protein tethers, and subsequently sensing the resistance to the induced deformations up to a depth of 5 μm (Buxboim et al. 2010). For stem cells the mechanical response that they sense in this region is a determining factor regarding their differentiation into a range of cell types (Engler et al. 2006; Trappmann et al. 2012). On a macroscopic scale, the bulk mechanical properties of a scaffold must be sufficiently robust for pre-implantation culture and handling during surgery. While this is important for any tissue engineered scaffold, it provides additional complications for the higher loads and more aggressive surgical techniques associated with orthopaedic surgery. Moreover, once implanted, scaffolds must match the macroscale mechanical properties of the tissues surrounding them; implanted scaffolds are required to replace biomechanical function of the lost native tissue from the point of implantation, through to the completion of tissue remodelling. Scaffolds for interface tissues are hence required to simultaneously mimic the macroscale mechanical properties of the natural tissue, in both magnitude and distribution, whilst containing a gradient in microscale material stiffness to direct cellular differentiation. This has historically proven difficult, as scaffolds focused on replicating macroscale properties of bone or cartilage have failed to provide the high porosity or chemical cues required for successful tissue growth, causing them to fail in vivo (O’Brien 2011). An example of a scaffold that successfully recreated many of the macroscale mechanical properties of the ACL can be found in (Cooper et al. 2005; Freeman et al. 2007). These papers detail a fibrous scaffold produced from a combination of braided and twisted poly l-lactic acid (PLLA) where the tensile mechanical properties mimicked both the initial toeing in region of load (characteristic of collagen fiber uncrimping) followed by a linear region of approximately the correct stiffness. This fibrous scaffold was also shown to be biocompatible. An in vitro study and an in vivo rabbit model showed that the fibrous structure presented sufficient porosity for cellular ingrowth to the centre of the tissue engineered ligament by 12 weeks (Lu et al. 2005; Cooper et al. 2007). Yet, this scaffold was not designed to regenerate the multiphasic ligament-bone interface and was implanted by merely suturing into a bone tunnel. As such, this scaffold was observed to sufficiently replicate mechanical tensile function of the natural ligament in the bulk region but not regenerate the graded tissue interface characteristic of the ligament bone junction. A recent work (Chung et al. 2014) used a similarly braided PLL scaffold to replace tendon function but also integrated their braided scaffold into regions of porous HA nanocomposite bone scaffold at either end. This work showed good scaffold uptake in a rabbit model, attributed to the enhanced healing possibility of the bone scaffold to bone rather than a tendon scaffold to bone. This work did not seek to generate a multiphasic interface between the braided tendon scaffold and the nanocomposite bone scaffold and it remains to be seen if the lack of an enthesis like region will cause increased incidence of failure in scaffolds of this type.
The focal adhesion protein complexes that cells utilize to sense their mechanical microenvironment are composed of integrins , trans membrane receptor proteins that facilitate cell-ECM binding interactions (Chen 2008). Integrins bind with a family of molecules on the ECM, ligands, and the specificity of the pairing mediates many cell processes including gene expression, cell proliferation and cell differentiation (Langholz et al. 1995; Zandstra et al. 2000; Lutolf and Hubbell 2005). There are over 20 known integrin proteins (Ruoslahti 1996), each of which can bind with a number of ligand molecules. Yet, integrin specificity for the ligands present in the native ECM has been observed to be important in culture viability, while the misregulation of integrin-ligand binding has been linked with serious cellular diseases such as cancer metastasis (Logsdon et al. 2003). Hence, it has been concluded that both the density and type of integrin-ligand bonds that form between a cellular population and its ECM mediate much of the cells behaviour (Massia and Hubbell 1991; Asthagiri et al. 1999). Ligands occur naturally within the sequences of proteins that make up the natural ECM including collagen, fibronectin, hyaluronic acid and proteoglycans. This makes these molecules attractive options for tissue engineered scaffolds, as they will continue to present biologically relevant types and densities of ligands for cell-ECM binding. Conversely, synthetic polymers such as poly(esters), or natural ones occurring outside of the body, such as silk or alginate, need be functionalized with ligands to promote cell-ECM binding. For instance (Paxton et al. 2009), incorporated the RGD ligand into a poly ethylene glycol (PEG) hydrogel, showing increased attachment of primary tendon fibroblasts over unfunctionalized PEG gels. Given the important role of integrin-ligand binding in all aspects of the cellular life, it can be an important tool when designing interface tissue engineered scaffolds, where zonal differentiation is required. Use of ligands to control stem cell differentiation is discussed in (Saha et al. 2007) for neural, mesenchymal, epithelial and embryonic stem cells. While these principles have not as of yet been applied to gradient scaffolds for interface tissues, their potential for influencing localized differentiation is clear. Additionally, methods of gradient generation in ligand concentration or type have been developed in hydrogels for studying cell attachment or motility as a function of ligand density (Lühmann and Hall 2009; He et al. 2010; Sarvestani 2010). These gradient generation methods, alongside knowledge of specific integrin-ligand pairings that induce specific cell phenotypes, have the ability to assist guided differentiation of stem cells for interface tissue scaffolds.
Inorganic inclusions such as calcium phosphate , calcium carbonate and silicon dioxide have all been shown to promote osteoinduction in tissue engineered scaffolds for bone regeneration (Yuan et al. 1998; Xynos et al. 2001; Ripamonti et al. 2009; Poologasundarampillai et al. 2011). The mechanism by which inorganic mineral deposits promote osteoinduction is multifaceted. Firstly, the elastic stiffness of these materials is in the gigapascal range, promoting differentiation into osteoprogenitor cell types that naturally occupy stiff tissue environments. Secondly, these inorganic inclusions undergo cellular resorption and remodelling via ionic exchange at the mineral-cell boundary. This interaction promotes osteoblast proliferation and attachment by regulating cellular signalling pathways (Barrère et al. 2006). Additionally, during remodelling, the resorption of calcium phosphate , calcium carbonate or silicon dioxide inclusions does not induce abnormal or harmful levels of ions in the body (LeGeros 1993; Barrère et al. 2006; Rahaman et al. 2011). Their controllable deposition, and natural biocompatibility, makes inorganic inclusions a good option for promoting growth of bony tissue over fibrous tissue in regions of an enthesis or osteochondral scaffold. Multiple studies have employed this strategy, including: injecting calcium phosphate into a tendon graft to improve osteoinduction (Mutsuzaki et al. 2004); a 45S5 bioactive glass phase to promote a bony region in an ACL enthesis scaffold (Spalazzi et al. 2008); using calcium phosphate bone cement to simultaneously fixate a tendon graft in the bone tunnel and promote osteoinduction (Tien et al. 2004); inclusion of HA in a PEG hydrogel to assess interface formation with bone (Paxton et al. 2009); inclusion of HA particles within an alginate hydrogel to observe chondrocyte behaviour with different mineral concentrations (Khanarian et al. 2012); and graded deposition of HA using a varied incubation time in simulated body fluid (Li et al. 2009).
3.1.2 Scaffold Manufacturing Techniques
Freeze-drying is a widely used technique for the manufacture of highly interconnected porous scaffolds for tissue engineering. A range of materials can be freeze dried, including both organic and inorganic polymers such as collagen or polycaprolactone (Whang and Healy 2002; Maquet et al. 2003; Haugh et al. 2010) or stiff minerals such as HA (Macchetta et al. 2009). As a technique, freeze-drying offers a high degree of control over scaffold pore size, making it particularly apt for musculoskeletal scaffolds. Additionally, compared to other scaffold production techniques, freeze-drying eliminates the need for porogens that would later need to be leached away from the scaffold material. Graded structures of pore size or composition can also be manufactured. Gradients in pore size can be achieved by manipulating the thermodynamic conditions for ice crystal nucleation across the scaffold (Macchetta et al. 2009). Compositional gradients can be achieved by use of a graded proportion of two different precursor slurries (Weisgerber et al. 2013). A known disadvantage of freeze-dried scaffolds is cell encapsulation. Due to the inhospitable conditions associated with the freeze and sublimate steps, cells cannot be encapsulated within the scaffold during manufacture and must be infiltrated postproduction. In comparison to hydrogels this means that cells mount to the sidewalls of the foam rather than get encapsulated on all sides by the matrix, this often reduces the viability of their scaffold attachment. A freeze dried scaffold for osteochondral interface tissue engineering was described over a series of three papers (Harley et al. 2010a, b; Lynn et al. 2010). This scaffold was made from a collagen – glycosaminoglycan (collagen-GAG or CG) slurry and contained a gradient in both pore size and chemical composition. SEM images of this scaffold can be seen in Fig. 11.4 and show the graded transition from a dense cartilaginous scaffold to a more porous and mineralized osseous scaffold.
An SEM image of a CG scaffold designed for replication of an osteochondral interface tissue. Left and right images are the same scaffold at different magnifications. The red dashed line indicates the dense cartilaginous scaffold while the more porous area below is the osseous scaffold (Adapted with thanks and permission from Harley et al. (2010b))
Hydrogels are hydrophilic polymer networks that swell to many times their dry weight when exposed to water. In this way hydrogels mimic the ECM of cartilaginous tissues and hence have been considered as possible scaffolds for engineering of cartilage, among others (Suh and Matthew 2000). Hydrogels are prepared by either physical entanglement or chemical crosslinking of polymer chains. Polymer chain interconnectivity is brought about by either thermal settings or reversible bridging reactions in the case of physical entanglements, or by covalent bonding or photopolymerization in the case of chemical crosslinking (Oyen 2014). Additionally, it is simple to create interpenetrating double networks of two independent hydrogels. Double networks can be formed by mixing separate polymer solutions that are then cross-linked either in series or parallel, depending on the crosslinking techniques required for each network. Moreover, it is relatively simple to manufacture gradients in mechanical properties, pore size and chemistry within hydrogels. By generating a changing ratio of two polymers solutions the gel then contains a gradient in properties from that of purely one phase, to the properties of purely the other phase. For example, a mechanically and chemically graded collagen hydrogel was created using a microfluidics system for the study of matrix effects on hematopoietic stem cells (HSCs) (Mahadik et al. 2014). Alternatively, a homogenous polymer solution can be cross-linked in a graded manner to create a gradient in properties dependent on cross-linking density. Figure 11.5 shows examples of each of these methods of creating gradient hydrogels.
Methods of generating gradients in hydrogel properties for scaffold production. (a) Methods of mixing two solutions of different gel precursors solutions to generate a graded solid. (b) Methods of grading the crosslinking density of a gel precursor to produce graded solids (Figure reproduced with permission from Sant et al. (2010))
Electrospinning produces a mat of nanofibrous mesh from a large variety of organic and inorganic polymers. Electrospinning produces a fundamentally different structured scaffold compared to the open cell foam structures produced by freeze drying and other porogen based methods. By manipulating the process parameters of the experiment, fiber diameter, pore size and specimen thickness can be controlled. Furthermore, the morphology of the nanofibrous structure can be manipulated in a large variety of ways. Highly aligned fibers can be produced by spinning onto a rotating collector (Fennessey and Farris 2004), while a less dense and more 3D mesh can be produced by spinning into a fluid bath (Cai et al. 2013). Intricate collector geometries can also be used to produce complex patterned geometries of fibers (Zhang and Chang 2007). In addition to manipulating mesh morphology the fiber composition can be adapted to suit scaffold specific needs. Copolymer nanofibers can be formed by mixing two polymers in the precursor solution (Ma et al. 2005), or interpenetrating meshes of multiple distinct fibers can be formed from simultaneous spinning onto a single collector (Ifkovits et al. 2009). Furthermore, HA and bioactive glass inclusions can be incorporated into the fibers via sol-gel processes (Song et al. 2008; Poologasundarampillai et al. 2011).
Graded electrospun scaffolds with functional gradients in any of the parameters discussed above can hence be produced by temporal manipulation of the relevant experimental parameters. A hyaluronic acid mesh was electrospun containing both a mechanical gradient, by changing crosslinking density, and a chemical gradient, by changing RGD peptide concentration. Subsequent culture with avian aortic cells investigated the effect of the mechanical and chemical gradients on cell attachment and proliferation (Sundararaghavan and Burdick 2011). However, graded electrospun scaffolds have not as of yet been employed for regeneration of either the osteochondral interface or the bone-tendon enthesis.
3.2 External Factors
Gradients in concentration of signalling molecules in the cellular microenvironment affect all aspects of cell behaviour. Growth factors are one such class of signalling molecules and many growth factors (TGF-β, PDGF, bFGF and IGF-1) have been shown to have a positive role in culture viability for homogeneous cartilage, tendon or ligament tissues. This occurs by upregulation of both fibroblast proliferation and ECM production (Molloy et al. 2003; Thomopoulos et al. 2013). In a large number of studies, cocktails of these growth factors have been delivered with varying doses and release profiles into scaffolds, promoting tissue growth. Additionally, growth factor BMP-2 has been used to successfully promote healing of the tendon-bone interface within the bone tunnel after surgery (Chen et al. 2008). In one study, delivery of BMP-2 via a retroviral factor induced a juxtaposed tendon-bone replacement for the ACL to generate a graded, enthesis-like structure, 8 weeks after surgery (Martinek et al. 2002).
When considering scaffolds for graded interface tissues the different growth factor requirements of each tissue region must be considered. Additionally, the spatial arrangement, temporal release profile and interactions with one another must all be taken into account. Across the native tendon-bone interface the type of growth factors found varies greatly. For example, growth factors bFGF and GDF-5 are found in the native tendon, TGF-β3 and IGF-1 in the fibrocartilagenous transition and BMP-2 and VEGF in the bone (Galatz et al. 2006; Liu et al. 2008). However, the large numbers of growth factors present in situ, along with their relative quantities and spatial pattern within the complex enthesis tissue structure, means that an optimal distribution for tissue engineering has not yet been laid out. In one study, opposing gradients of TGF-β1 and BMP-2 growth factors were shown to induce patterning of cell phenotype differentiation, and subsequent tissue specific ECM composition (Dormer et al. 2010). Tactics like this, along with the knowledge of native growth factor distributions can allow for directed differentiation into the spatial distribution of cell phenotypes found in situ.
3.3 Cells
For interface tissue scaffolds the method of cell culture can be classified in two primary groups. Firstly, co-culture of two or more distinct cell lines where each population is characteristic of a distinct tissue region. Secondly, stem cell culture, where the mechanical, morphological and chemical properties of the scaffold direct stem cell differentiation into a range of phenotypes. In co-culture systems cell-cell signalling between populations is a key factor in influencing cell behaviour. A co-culture system consisting of a mass of bovine chondrocytes, covered in a monolayer of bovine osteoblasts, was used to investigate the co-culture effects for an osteochondral interface scaffold. Cross-sectioned staining from this study is shown in Fig. 11.6. This study showed that the co-culture method damped both the chondrocyte GAG expression compared to a chondrocyte control, and osteoblast mineralization compared to an osteoblast control (Jiang et al. 2005). In a further 3D study the co-culture system promoted formation of an interface region, similar to that of the ZCC, within a 3D osteochondral interface scaffold (Jiang et al. 2010). A different co-culture study cultured fibroblasts and osteoblasts in tissue wells split with a permeable hydrogel divider. Similar results regarding the damping of both fibroblast GAG production and osteoblast mineralization were observed (Wang et al. 2007). These studies show that co-culture may facilitate the formation of a fibrocartilaginous interface region by damping the characteristics that arise in mono-culture of either of the cell populations involved.
Cross sectioned images of osteoblast and chondrocyte co-culture with different staining. The “top” in both images is a monolayer of osteoblasts covering the mass of chondrocyte cells below it. (a) H&E staining of cell mass distribution showing how cells at the interface between populations became elongated compared to the more spherical cells in the centre of the mass. (b) Osteoblasts stained with CM-DiI (orange) and nuclei of both populations stained with DAPI (blue) (Figure reused with permission from Jiang et al. (2005))
A promising alternative to co-culture systems is to use multipotent or pluripotent progenitor stem cells, that are then directed to differentiate into the appropriate cell types for each region of the interface. Differentiation is directed by the graded mechanical, morphological and chemical factors of the scaffold that are discussed previously. Mesanchymal stem cells (MSCs) are a promising option for enthesis or osteochondral tissue engineering. MSCs can be harvested from adult bone marrow and have the ability to differentiate into osteoblasts, chondrocytes and fibroblasts, among others (Caplan 1991). A study to recreate the osteochondral interface using guided differentiation of MSCs has found recent success (Cheng et al. 2011). In this work MSCs were cultured within collagen microspheres into two sub populations: a chondrogenic population (Hui et al. 2008), and an osteogenic population (Chan et al. 2010). A layer of undifferentiated cells in collagen microspheres was placed between layers of the chondrogenic and osteogenic populations. The chemical cues received from the differentiated populations on either side, then prompted differentiation of the central layer into an interface region characterized by hypertrophic chondrocytes, as found in native tissue. In a different study, primary fibroblast cells, that have the ability to differentiate into osteoblasts, were cultured on collagen scaffolds in the presence of the osteogenic transcription factor Runx2/Cbfa1. The transcription factor was localized using immobilized retroviral deposits to create a gradient in transcription factor concentration. This resulted in a spatial gradient in differentiation of the primary fibroblasts into osteocytic and fibrocytic cell types, creating a corresponding gradient in cell-deposited matrix mineralization (Phillips et al. 2008).
4 Conclusions
Injuries to the soft tissues that connect the musculoskeletal system together are common. They include, sport-related acute tears of ligaments or tendons and age-related osteoarthritis of cartilage. Injuries such as these are significant problems clinically with largely unsatisfactory repair techniques. Tissue engineering has proven to be promising strategy for the reproduction of many homogeneous orthopaedic tissues such as bone, ligament and cartilage. However, even if fully biomimetic cartilage, ligament or tendon is produced then integrative clinical implantation is still challenging. Since, merely juxtaposing either cartilage with bone, or ligament with bone, does not result in the regeneration of the stratified natural interface. Consequently, tissue engineering efforts should focus on replication of the whole interface, from the soft tissue through to bone, and hence allow for a simpler bone-bone repair to occur post surgery.
Ligament or tendon entheses, and osteochondral interfaces, have unique and complex structures that are optimized to fulfil a niche biological role. Moreover, the exact distribution of some factors within the enthesis, including mineral content and mechanical response in each region, is under dispute. In order for tissue engineering efforts to be successful, these fundamental properties of the natural tissue must be understood in order for them to be recreated in scaffolds.
Scaffolds for interface tissue replication can be produced by either, joining a number of discrete homogeneous scaffolds, or, by fabrication of a single graded scaffold. Discrete scaffolds are easier to produce but significant care must be taken for full integration to be achieved at the interfaces. Regardless of the manufacturing method chosen, a number of scaffold properties must be controlled through the thickness. This is in order to ensure that either stem cell differentiation is appropriately directed, or, co-cultured distinct cell lines have the optimal properties for their viability. Pore size has a significant effect on different cell line viabilities, but also affects macroscale mechanical properties, and is itself dependent on the scaffold material and manufacturing method. Microscale mechanical properties of the scaffold are key in stem cell differentiation, while the macroscale mechanical properties allow the scaffold to replicate biomechanical function once implanted. Chemical properties of the scaffold such as: the availability of relevant ligands; degradation properties of the polymer backbone; and any external growth factors that are added, combine to control cellular activity. In summary, for successful interface tissue engineering this interdependent set of properties must be simultaneously controlled to achieve biomimetic, region specific, tissue types.
References
AAOS (2014) Anterior cruciate ligament injuries. http://orthoinfo.aaos.org/topic.cfm?topic=a00549
Abraham AC, Haut Donahue TL (2013) From meniscus to bone: a quantitative evaluation of structure and function of the human meniscal attachments. Acta Biomater 9:6322–6329
Amiel D, Frank C, Harwood F, Fronek J, Akeson W (1984) Tendons and ligaments: a morphological and biochemical comparison. J Orthop Res 1:257–265
Amini AR, Laurencin CT, Nukavarapu SP (2012) Bone tissue engineering: recent advances and challenges. Crit Rev Biomed Eng 40:363–408
Armitage OE, Oyen ML (2015) Indentation of tissue interfaces (in preparation)
Asthagiri AR, Nelson CM, Horwitz AF, Lauffenburger DA (1999) Quantitative relationship among integrin-ligand binding, adhesion, and signaling via focal adhesion kinase and extracellular signal-regulated kinase 2. J Biol Chem 274:27119–27127
Barrère F, van Blitterswijk CA, de Groot K (2006) Bone regeneration: molecular and cellular interactions with calcium phosphate ceramics. Int J Nanomedicine 1:317–332
Bembey A, Oyen M, Bushby A, Boyde A (2006) Viscoelastic properties of bone as a function of hydration state determined by nanoindentation. Phil Mag 86:5691–5703
Benjamin M, Ralphs JR (1998) Fibrocartilage in tendons and ligaments – an adaptation to compressive load. J Anat 193:481–494
Benjamin M, Evans EJ, Copp L (1986) The histology of tendon attachments to bone in man. J Anat 149:89–100
Bhardwaj T, Pilliar RM, Grynpas MD, Kandel RA (2001) Effect of material geometry on cartilagenous tissue formation in vitro. J Biomed Mater Res 57:190–199
Butler DL, Juncosa-Melvin N, Boivin GP, Galloway MT, Shearn JT, Gooch C, Awad H (2008) Functional tissue engineering for tendon repair: a multidisciplinary strategy using mesenchymal stem cells, bioscaffolds, and mechanical stimulation. J Orthop Res 26:1–9
Buxboim A, Rajagopal K, Brown AEX, Discher DE (2010) How deeply cells feel: methods for thin gels. J Phys Condens Matter 22:194116
Cai S, Xu H, Jiang Q, Yang Y (2013) 3D electrospun scaffolds with fibers oriented randomly and evenly in three dimensions to closely mimic the unique architectures of extracellular matrices in soft tissues. Langmuir 29:2311–2318
Caplan AI (1991) Mesenchymal stem cells. J Orthop Res 9:641–650
Chan BP, Hui TY, Wong MY, Yip KHK, Chan GCF (2010) Mesenchymal stem cell-encapsulated collagen microspheres for bone tissue engineering. Tissue Eng Part C Methods 16:225–235
Chen CS (2008) Mechanotransduction – a field pulling together? J Cell Sci 121:3285–3292
Chen C-H, Liu H-W, Tsai C-L, Yu C-M, Lin I-H, Hsiue G-H (2008) Photoencapsulation of bone morphogenetic protein-2 and periosteal progenitor cells improve tendon graft healing in a bone tunnel. Am J Sports Med 36:461–473
Cheng H, Luk KDK, Cheung KMC, Chan BP (2011) In vitro generation of an osteochondral interface from mesenchymal stem cell-collagen microspheres. Biomaterials 32:1526–1535
Chung EJ, Sugimoto MJ, Koh JL, Ameer GA (2014) A biodegradable tri-component graft for anterior cruciate ligament reconstruction. J Tissue Eng Regener Med. doi:10.1002/term.1966
Cooper JA, Lu HH, Ko FK, Freeman JW, Laurencin CT (2005) Fiber-based tissue-engineered scaffold for ligament replacement: design considerations and in vitro evaluation. Biomaterials 26:1523–1532
Cooper JA, Sahota JS, Gorum WJ, Carter J, Doty SB, Laurencin CT (2007) Biomimetic tissue-engineered anterior cruciate ligament replacement. Proc Natl Acad Sci U S A 104:3049–3054
Dormer NH, Singh M, Wang L, Berkland CJ, Detamore MS (2010) Osteochondral interface tissue engineering using macroscopic gradients of bioactive signals. Ann Biomed Eng 38:2167–2182
Elliott JC (1994) Structure and chemistry of the apatites and other calcium orthophosphates. Elsevier, Amsterdam
Engler AJ, Sen S, Sweeney HL, Discher DE (2006) Matrix elasticity directs stem cell lineage specification. Cell 126:677–689
Evans EJ, Benjamin M, Pemberton DJ (1990) Fibrocartilage in the attachment zones of the quadriceps tendon and patellar ligament of man. J Anat 171:155–162
Fennessey S, Farris R (2004) Fabrication of aligned and molecularly oriented electrospun polyacrylonitrile nanofibers and the mechanical behavior of their twisted yarns. Polymer (Guildf) 45:4217–4255
Ferguson VL (2009) Deformation partitioning provides insight into elastic, plastic, and viscous contributions to bone material behavior. J Mech Behav Biomed Mater 2:364–374
Ferguson VL, Bushby AJ, Boyde A (2003) Nanomechanical properties and mineral concentration in articular calcified cartilage and subchondral bone. J Anat 203:191–202
Freeman JW, Woods MD, Laurencin CT (2007) Tissue engineering of the anterior cruciate ligament using a braid-twist scaffold design. J Biomech 40:2029–2036
Galatz LM, Sandell LJ, Rothermich SY, Das R, Mastny A, Havlioglu N, Silva MJ, Thomopoulos S (2006) Characteristics of the rat supraspinatus tendon during tendon-to-bone healing after acute injury. J Orthop Res 24:541–550
Genin GM, Kent A, Birman V, Wopenka B, Pasteris JD, Marquez PJ, Thomopoulos S (2009) Functional grading of mineral and collagen in the attachment of tendon to bone. Biophys J 97:976–985
Griffon DJ, Sedighi MR, Schaeffer DV, Eurell JA, Johnson AL (2006) Chitosan scaffolds: interconnective pore size and cartilage engineering. Acta Biomater 2:313–320
Gupta HS, Schratter S, Tesch W, Roschger P, Berzlanovich A, Schoeberl T, Klaushofer K, Fratzl P (2005) Two different correlations between nanoindentation modulus and mineral content in the bone-cartilage interface. J Struct Biol 149:138–148
Harley BA, Lynn AK, Wissner-Gross Z, Bonfield W, Yannas IV, Gibson LJ (2010a) Design of a multiphase osteochondral scaffold. II. Fabrication of a mineralized collagen-glycosaminoglycan scaffold. J Biomed Mater Res A 92:1066–1077
Harley BA, Lynn AK, Wissner-Gross Z, Bonfield W, Yannas IV, Gibson LJ (2010b) Design of a multiphase osteochondral scaffold III: fabrication of layered scaffolds with continuous interfaces. J Biomed Mater Res A 92:1078–1093
Hauch KN, Oyen ML, Odegard GM, Haut Donahue TL (2009) Nanoindentation of the insertional zones of human meniscal attachments into underlying bone. J Mech Behav Biomed Mater 2:339–347
Haugh MG, Murphy CM, O’Brien FJ (2010) Novel freeze-drying methods to produce a range of collagen-glycosaminoglycan scaffolds with tailored mean pore sizes. Tissue Eng Part C Methods 16:887–894
He J, Du Y, Villa-Uribe JL, Hwang C, Li D, Khademhosseini A (2010) Rapid generation of biologically relevant hydrogels containing long-range chemical gradients. Adv Funct Mater 20:131–137
Hui TY, Cheung KMC, Cheung WL, Chan D, Chan BP (2008) In vitro chondrogenic differentiation of human mesenchymal stem cells in collagen microspheres: influence of cell seeding density and collagen concentration. Biomaterials 29:3201–3212
Hunziker EB, Quinn TM, Häuselmann HJ (2002) Quantitative structural organization of normal adult human articular cartilage. Osteoarthr Cartil 10:564–572
Ifkovits JL, Sundararaghavan HG, Burdick JA (2009) Electrospinning fibrous polymer scaffolds for tissue engineering and cell culture. J Vis Exp 32:629–629
Jiang J, Nicoll SB, Lu HH (2005) Co-culture of osteoblasts and chondrocytes modulates cellular differentiation in vitro. Biochem Biophys Res Commun 338:762–770
Jiang J, Tang A, Ateshian GA, Edward Guo X, Hung CT, Lu HH (2010) Bioactive stratified polymer ceramic-hydrogel scaffold for integrative osteochondral repair. Ann Biomed Eng 38:2183–2196
Karageorgiou V, Kaplan D (2005) Porosity of 3D biomaterial scaffolds and osteogenesis. Biomaterials 26:5474–5491
Khanarian NT, Jiang J, Wan LQ, Mow VC, Lu HH (2012) A hydrogel-mineral composite scaffold for osteochondral interface tissue engineering. Tissue Eng A 18:533–545
Langholz O, Röckel D, Mauch C, Kozlowska E, Bank I, Krieg T, Eckes B (1995) Collagen and collagenase gene expression in three-dimensional collagen lattices are differentially regulated by alpha 1 beta 1 and alpha 2 beta 1 integrins. J Cell Biol 131:1903–1915
LeGeros RZ (1993) Biodegradation and bioresorption of calcium phosphate ceramics. Clin Mater 14:65–88
Li X, Xie J, Lipner J, Yuan X, Thomopoulos S, Xia Y (2009) Nanofiber scaffolds with gradations in mineral content for mimicking the tendon-to-bone insertion site. Nano Lett 9:2763–2768
Liu Y, Ramanath HS, Wang DA (2008) Tendon tissue engineering using scaffold enhancing strategies. Trends Biotechnol 26:201–209
Logsdon C, Simeone D, Binkley C, Arumugam T, Greenson J, Giordano T, Misek D, Kuick R, Hanash S (2003) Molecular profiling of pancreatic adenocarcinoma and chronic pancreatitis identifies multiple genes differentially regulated in pancreatic cancer. Cancer Res 63:2649–2657
Lowery JL, Datta N, Rutledge GC (2010) Biomaterials effect of fiber diameter, pore size and seeding method on growth of human dermal fibroblasts in electrospun poly (3 -caprolactone) fibrous mats. Biomaterials 31:491–504
Lu HH, Cooper JA, Manuel S, Freeman JW, Attawia MA, Ko FK, Laurencin CT (2005) Anterior cruciate ligament regeneration using braided biodegradable scaffolds: in vitro optimization studies. Biomaterials 26:4805–4816
Lühmann T, Hall H (2009) Cell guidance by 3D-gradients in hydrogel matrices: importance for biomedical applications. Materials (Basel) 2:1058–1083
Lui P, Zhang P, Chan K, Qin L (2010) Biology and augmentation of tendon-bone insertion repair. J Orthop Surg Res 5:59–63
Lutolf MP, Hubbell JA (2005) Synthetic biomaterials as instructive extracellular microenvironments for morphogenesis in tissue engineering. Nat Biotechnol 23:47–55
Lynn AK, Best SM, Cameron RE, Harley BA, Yannas IV, Gibson LJ, Bonfield W (2010) Design of a multiphase osteochondral scaffold. I. Control of chemical composition. J Biomed Mater Res A 92:1057–1065
Ma M, Hill RM, Lowery JL, Fridrikh SV, Rutledge GC (2005) Electrospun poly(styrene-block-dimethylsiloxane) block copolymer fibers exhibiting superhydrophobicity. Langmuir 21:5549–5554
Macchetta A, Turner IG, Bowen CR (2009) Fabrication of HA/TCP scaffolds with a graded and porous structure using a camphene-based freeze-casting method. Acta Biomater 5:1319–1327
Mahadik BP, Wheeler TD, Skertich LJ, Kenis PJ, Harley B (2014) Microfluidic generation of gradient hydrogels to modulate hematopoietic stem cell culture environment. Adv Healthc Mater 3:449–458
Maquet V, Blacher S, Pirard R, Pirard J-P, Vyakarnam MN, Jérôme R (2003) Preparation of macroporous biodegradable poly(L-lactide-co-epsilon-caprolactone) foams and characterization by mercury intrusion porosimetry, image analysis, and impedance spectroscopy. J Biomed Mater Res A 66:199–213
Martinek V, Latterman C, Usas A, Abramowitch S, Woo SL-Y, Fu FH, Huard J (2002) Enhancement of tendon-bone integration of anterior cruciate ligament grafts with bone morphogenetic protein-2 gene transfer: a histological and biomechanical study. J Bone Joint Surg Am 84:1123–1131
Massia SP, Hubbell JA (1991) An RGD spacing of 440 nm is sufficient for integrin alpha V beta 3- mediated fibroblast spreading and 140 nm for focal contact and stress fiber formation. J Cell Biol 114:1089–1100
McKee CT, Last JA, Russell P, Murphy CJ (2011) Indentation versus tensile measurements of Young’s modulus for soft biological tissues. Tissue Eng Part B Rev 17:155–164
Moffat KL, Sun W-HS, Pena PE, Chahine NO, Doty SB, Ateshian GA, Hung CT, Lu HH (2008) Characterization of the structure-function relationship at the ligament-to-bone interface. Proc Natl Acad Sci U S A 105:7947–7952
Molloy T, Wang Y, Murrell GAC (2003) The roles of growth factors in tendon and ligament healing. Sport Med 33:381–394
Moutos FT, Guilak F (2008) Composite scaffolds for cartilage tissue engineering. Biorheology 45:501–512
Mow VC, Ratcliffe A, Poole AR (1992) Cartilage and diarthrodial joints as paradigms for hierarchical materials and structures. Biomaterials 13:67–97
Murphy C, Haugh M, O’Brien F (2010) The effect of mean pore size on cell attachment, proliferation and migration in collagen glycosaminoglycan scaffolds for bone tissue engineering. Biomaterials 31:461–466
Mutsuzaki H, Sakane M, Nakajima H, Ito A, Hattori S, Miyanaga Y, Ochiai N, Tanaka J (2004) Calcium-phosphate-hybridized tendon directly promotes regeneration of tendon-bone insertion. J Biomed Mater Res A 70:319–327
Nehrer S, Breinan HA, Ramappa A, Young G, Shortkroff S, Louie LK, Sledge CB, Yannas IV, Spector M (1997) Matrix collagen type and pore size influence behaviour of seeded canine chondrocytes. Biomaterials 18:769–776
Niederauer GG, Slivka MA, Leatherbury NC, Korvick DL, Harroff HH, Ehler WC, Dunn CJ, Kieswetter K (2000) Evaluation of multiphase implants for repair of focal osteochondral defects in goats. Biomaterials 21:2561–2574
O’Brien FJ (2011) Biomaterials & scaffolds for tissue engineering. Mater Today 14:88–95
OECD (2013) Hip and knee replacement. Health at a glance 2013: OECD indicators. Paris: OECD Publishing
Oyen ML (2014) Mechanical characterisation of hydrogel materials. Int Mater Rev 59:44–59
Oyen ML, Ko C-C (2008) Indentation variability of natural nanocomposite materials. J Mater Res 23:760–767
Oyen ML, Ferguson VL, Bembey AK, Bushby AJ, Boyde A (2008) Composite bounds on the elastic modulus of bone. J Biomech 41:2585–2588
Paxton JZ, Donnelly K, Keatch RP, Baar K (2009) Engineering the bone-ligament interface using polyethylene glycol diacrylate incorporated with hydroxyapatite. Tissue Eng Part A 15:1201–1209
Phillips JE, Burns KL, Le Doux JM, Guldberg RE, García AJ (2008) Engineering graded tissue interfaces. Proc Natl Acad Sci U S A 105:12170–12175
Poologasundarampillai G, Yu B, Jones JR, Kasuga T (2011) Electrospun silica/PLLA hybrid materials for skeletal regeneration. Soft Matter 7:10241–10251
Rahaman MN, Day DE, Sonny Bal B, Fu Q, Jung SB, Bonewald LF, Tomsia AP (2011) Bioactive glass in tissue engineering. Acta Biomater 7:2355–2373
Reid SA, Boyde A (1987) Changes in the mineral density distribution in human bone with age: image analysis using backscattered electrons in the SEM. J Bone Miner Res 2:13–22
Ripamonti U, Crooks J, Khoali L, Roden L (2009) The induction of bone formation by coral-derived calcium carbonate/hydroxyapatite constructs. Biomaterials 30:1428–1439
Rodeo SA, Arnoczky SP, Torzilli PA, Hidaka C, Warren RF (1993) Tendon-healing in a bone tunnel. A biomechanical and histological study in the dog. J Bone Joint Surg 75:1795–1803
Ruoslahti E (1996) RGD and other recognition sequences for integrins. Annu Rev Cell Dev Biol 12:697–715
Saha K, Pollock JF, Schaffer DV, Healy KE (2007) Designing synthetic materials to control stem cell phenotype. Curr Opin Chem Biol 11:381–387
Salem AK, Stevens R, Pearson RG, Davies MC, Tendler SJB, Roberts CJ, Williams PM, Shakesheff KM (2002) Interactions of 3T3 fibroblasts and endothelial cells with defined pore features. J Biomed Mater Res 61:212–217
Sant S, Hancock MJ, Donnelly JP, Iyer D, Khademhosseini A (2010) Biomimetic gradient hydrogels for tissue engineering. Can J Chem Eng 88:899–911
Sarvestani AS (2010) Cell adhesion on ligand gradient substrates: a thermodynamic study. Biotechnol Bioeng 105:172–183
Schaefer D, Martin I, Shastri P, Padera RF, Langer R, Freed LE, Vunjak-Novakovic G (2000) In vitro generation of osteochondral composites. Biomaterials 21:2599–2606
Song JH, Kim HE, Kim HW (2008) Electrospun fibrous web of collagen-apatite precipitated nanocomposite for bone regeneration. J Mater Sci Mater Med 19:2925–2932
Spalazzi JP, Doty SB, Moffat KL, Levine WN, Lu HH (2006a) Development of controlled matrix heterogeneity on a triphasic scaffold for orthopedic interface tissue engineering. Tissue Eng 12:3497–3508
Spalazzi JP, Gallina J, Fung-kee-fung SD, Konofagou EE, Lu HH (2006b) Elastographic Imaging of strain distribution in the anterior cruciate ligament and at the ligament – bone insertions. J Orthop Res 24:2001–2010
Spalazzi JP, Boskey AL, Lu HH (2007) Region-dependent variations in matrix collagen and mineral distribution across the femoral and tibial anterior cruciate ligament-to-bone insertion sites. Trans Orthop Res Soc 32:891
Spalazzi JP, Dagher E, Doty SB, Guo XE, Rodeo SA, Lu HH (2008) In vivo evaluation of a multiphased scaffold designed for orthopaedic interface tissue engineering and soft tissue-to-bone integration. J Biomed Mater Res A 86:1–12
Suh JK, Matthew HW (2000) Application of chitosan-based polysaccharide biomaterials in cartilage tissue engineering: a review. Biomaterials 21:2589–2598
Sundararaghavan HG, Burdick JA (2011) Gradients with depth in electrospun fibrous scaffolds for directed cell behavior. Biomacromolecules 12:2344–2350
Suresh S, Mortenson A (1998) Fundamentals of functionally graded materials: processing and thermomechanical behaviour of graded metals and metal-ceramic composites. IOM Communications, London
Thomopoulos S, Birman V, Genin G (2013) Structural interfaces and attachments in biology. New York: Springer-Verlag
Tien YC, Chih TT, Lin JHC, Ju CP, Lin SD (2004) Augmentation of tendon-bone healing by the use of calcium-phosphate cement. J Bone Joint Surg Br 86:1072–1076
Trappmann B, Gautrot JE, Connelly JT, Strange DGT, Li Y, Oyen ML, Cohen Stuart MA, Boehm H, Li B, Vogel V, Spatz JP, Watt FM, Huck WTS (2012) Extracellular-matrix tethering regulates stem-cell fate. Nat Mater 11:642–649
United States Bone & Joint Initiative (2011) The burden of musculoskeletal diseases in the United States, 2nd edn. American Academy of Orthopedic Surgeons, Rosemont
Walsh W (2007) Repair and regeneration of ligaments, tendons, and joint capsule. New York: Springer
Wang INE, Mitroo S, Chen FH, Lu HH, Doty SB (2006) Age-dependent changes in matrix composition and organization at the ligament-to-bone insertion. J Orthop Res 24:1745–1755
Wang I, Shan J, Choi R, Oh S, Kepler C, Chen F, Lu HH (2007) Role of osteoblast-fibroblast interactions in the formation of the ligament-to-bone interface. J Orthop Res 25:1609–1620
Weisgerber DW, Kelkhoff DO, Caliari SR, Harley BAC (2013) The impact of discrete compartments of a multi-compartment collagen-GAG scaffold on overall construct biophysical properties. J Mech Behav Biomed Mater 28:26–36
Whang K, Healy K (2002) Processing of polymer scaffolds: freeze – drying. In: Atala A, Anza RP (eds) Methods of tissue engineering. Houston: Academic Press, pp 697–702
Wopenka B, Kent A, Pasteris J (2008) The tendon-to-bone transition of the rotator cuff: a preliminary Raman spectroscopic study documenting the gradual mineralization across the insertion in rat tissue. Appl Spectrosc 62:1285–1294
Xynos ID, Edgar AJ, Buttery LDK, Hench LL, Polak JM (2001) Gene-expression profiling of human osteoblasts following treatment with the ionic products of Bioglass 45S5 dissolution. J Biomed Mater Res 55:151–157
Yahia H, Newman N (1970) Tendon and ligament insertion. A light and electron microscopic study. J Bone Joint Surg 52:664–674
Yamaguchi K (2011) New guideline on rotator cuff problems. AAOS Now
Yilgor C, Yilgor Huri P, Huri G (2012) Tissue engineering strategies in ligament regeneration. Stem Cells Int 2012:374676
Yoder C, Pasteris J, Worcester K, Schermerhorn D, Sternlieb M, Goldenberg J, Wilt Z (2012) Dehydration and rehydration of carbonated fluor- and hydroxylapatite. Minerals 2:100–117
Yuan H, Yang Z, Li Y, Zhang X, De Bruijn JD, De Groot K (1998) Osteoinduction by calcium phosphate biomaterials. J Mater Sci Mater Med 9:723–726
Zandstra PW, Lauffenburger DA, Eaves CJ (2000) A ligand-receptor signaling threshold model of stem cell differentiation control: a biologically conserved mechanism applicable to hematopoiesis. Blood 96:1215–1222
Zhang Y (2012) Analysis of the mineral composition of the human calcified cartilage zone. Int J Med Sci 9:353–360
Zhang D, Chang J (2007) Patterning of electrospun fibers using electroconductive templates. Adv Mater 19:3662–3667
Zizak I, Roschger P, Paris O, Misof BM, Berzlanovich A, Bernstorff S, Amenitsch H, Klaushofer K, Fratzl P (2003) Characteristics of mineral particles in the human bone/cartilage interface. J Struct Biol 141:208–217
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Armitage, O.E., Oyen, M.L. (2015). Hard-Soft Tissue Interface Engineering. In: Bertassoni, L., Coelho, P. (eds) Engineering Mineralized and Load Bearing Tissues. Advances in Experimental Medicine and Biology, vol 881. Springer, Cham. https://doi.org/10.1007/978-3-319-22345-2_11
Download citation
DOI: https://doi.org/10.1007/978-3-319-22345-2_11
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-22344-5
Online ISBN: 978-3-319-22345-2
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)