Abstract
Infertility is one of the major health problems that affect human sociocultural life. It affects 8–15 % of couples around the world, and about 50 % of infertility cases are attributed to male factors (WHO 1991; Cui 2010; Hamada et al. 2011). Among the factors that cause male infertility are exposures to environmental toxicants (Akingbemi et al. 2004). Bisphenol A ([2,2-bis(4-hydroxyphenyl)propane]: BPA) is among the most prominent of toxic environmental contaminants worldwide. The original synthesis of BPA is attributed to two scientists: Dianin, who is thought to have been the first to design the molecule in 1891, and Zincke, who reportedly synthesized the molecule in 1905 (Huang et al. 2011). Since then, BPA has been widely produced and used as a common ingredient in the manufacture of plastics. Plastics are broadly integrated into today’s lifestyle and make a major contribution to almost all product areas (Olea et al. 1996; Völkel et al. 2011; Hammer et al. 2012). The wide and heavy use of plastics has contributed to BPA having been spread throughout the environment.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Infertility is one of the major health problems that affect human sociocultural life. It affects 8–15% of couples around the world, and about 50% of infertility cases are attributed to male factors (WHO 1991; Cui 2010; Hamada et al. 2011). Among the factors that cause male infertility are exposures to environmental toxicants (Akingbemi et al. 2004). Bisphenol A ([2,2-bis(4-hydroxyphenyl)propane]: BPA) is among the most prominent of toxic environmental contaminants worldwide. The original synthesis of BPA is attributed to two scientists: Dianin, who is thought to have been the first to design the molecule in 1891, and Zincke, who reportedly synthesized the molecule in 1905 (Huang et al. 2011). Since then, BPA has been widely produced and used as a common ingredient in the manufacture of plastics. Plastics are broadly integrated into today’s lifestyle and make a major contribution to almost all product areas (Olea et al. 1996; Völkel et al. 2011; Hammer et al. 2012). The wide and heavy use of plastics has contributed to BPA having been spread throughout the environment.
Humans are mainly exposed to BPA through food ingestion (Yamada et al. 2002), and increasing evidence supports its association with impairment of male reproductive function, as well as other health problems and diseases; such diseases include diabetes, obesity, cardiovascular diseases, and cancer (Li et al. 2010a, 2011; Salian et al. 2011; Batista et al. 2012; Shankar and Teppala 2012; Lee et al. 2012; Wang et al. 2012a). BPA acts primarily by mimicking the effect of estrogen hormones, modifying DNA methylation, and modulating enzyme activities in utero and in vivo, resulting in metabolic diseases, spermatogenesis defects, and/or infertility in males. The deleterious effect of BPA on male reproductive function may occur during embryonic, pubertal, and/or adult life. The fact that BPA is a causal agent in such effects is supported by its repeated detection in human biological samples (Sun et al. 2004; He et al. 2009a; Li et al. 2010a).
In this review, we address the topic of BPA effects on male reproductive function and emphasize its effects on testicular steroidogenesis, spermatogenesis, and sperm function.
2 Sources and Routes of Bisphenol A Exposure
BPA is a man-made industrial chemical that is used as a component of plastics. The USA, Japan, and Europe are the areas in which the majority of BPA is produced. BPA’s annual production capacity now exceeds six billion pounds, and this high production level is sustained and encouraged by the widespread use of plastics to manufacture food containers, water bottles, medical devices, and other objects that must be made of materials that are both flexible and durable. More than 100 t of the annual BPA production volume is released into the atmosphere (Vandenberg et al. 2009; Cao et al. 2011). This volume of release has made BPA environmentally ubiquitous; BPA residues are found in air, drinking water, lakes, the seas, sewage sludge, soil, house dust, foodstuffs, paper currency, among other objects and media (Ignatius et al. 2010; Liao and Kannan 2011; Geens et al. 2012; Hammer et al. 2012; Liao et al. 2012; Molina-García et al. 2012; Rudel et al. 2011; Wang et al. 2012b; Rocha et al. 2013).
BPA enters the human body mainly via consuming contaminated food and drinking water, although exposure via environmental (from polluted air and water), domestic (household products, cosmetics), medical (from contaminated equipment and devices), and occupational sources (inhalation, dermal contact, and ingestion during manufacturing processes or industrial use) also occurs (Toppari et al. 1996; Demierre et al. 2012; Cho et al. 2012). Intake by the oral route may be enhanced when certain food preparation practices are used, such as wrapping food in plastic bags prior to thermal treatment or cooking—processes that enhance leakage of BPA from the bag into the food. BPA is known to be used in the manufacture of microwave oven ware, from which it may be released to food (EFSA 2006; Geens et al. 2012). Oral exposure to BPA may also be enhanced from the presence in the mouth of dental composites (Olea et al. 1996; Doerge et al. 2012), or from using epoxy resin-based food cans, water bottles, or plastic baby bottles (Cao et al. 2011; Kang et al. 2011; Völkel et al. 2011; Cho et al. 2012).
Absorption of BPA may also be indirect, as occurs when the fetus absorbs the chemical from maternal blood plasma (after maternal exposure). Indeed, BPA is transported across the human placenta (Mørck et al. 2010), and BPA’s effect on the fetus may be exacerbated, because the production of toxic effects is inversely correlated with age (Kline and Ruhter 2012). Transdermal BPA exposure and inhalation are of greater concern because such exposure routes avoid the first-pass metabolic effect that occurs with oral intake (Welshons et al. 2006; Mørck et al. 2010; Demierre et al. 2012).
Occupational exposure to BPA occurs in those countries where the compound is manufactured. Although most intake occurs from ingestion, people who are engaged in the manufacturing or use of BPA (or related chemicals) can easily absorb it through the skin, or take it up via inhalation (He et al. 2009b; Kaddar et al. 2009; Geens et al. 2012).
Absorption or uptake of BPA into the human body is ascertained by analyzing for the presence of the chemical or its metabolites in biological fluids such as blood, breast milk, urine, etc. (Zhang et al. 2011; Geens et al. 2012). For instance, a study conducted in a reference human population of the United States showed the presence of BPA in ≥95% of urinary samples collected from urban and rural residents (Calafat et al. 2005). Similarly, BPA was detected in spot samples of urine collected from both urban and rural girls in Egypt (Nahar et al. 2012). Urinary levels of BPA, detected in children and adolescents, were reported to be higher than in adults (Calafat et al. 2009; Zhang et al. 2011).
High levels of BPA have been measured in human placental tissue, in maternal urine, and in maternal and fetal plasma. Maternal BPA levels were positively correlated with BPA concentrations detected in the fetal umbilical cord (Schönfelder et al. 2002; Lee et al. 2008; Callan et al. 2012; Ünüvar and Büyükgebiz 2012). In utero exposure appears to be more harmful in humans, since BPA accumulates in amniotic fluid of pregnant women (Schönfelder et al. 2002; Sun et al. 2004). BPA concentrations in maternal plasma were found to be fivefold lower than levels measured in amniotic fluid (Ikezuki et al. 2002), indicating that the fetus is more highly exposed than is the mother. These observations suggest that BPA exposure is higher during fetal life, and diminishes as age increases.
Urinary BPA levels detected in workers were also consistent with degree of occupational exposure to the chemical. He et al. (2009b) reported high levels of BPA in urine and blood of people working in epoxy-resin and BPA manufacturing factories in China.
Several researchers have noted that BPA produces estrogenic and antiandronenic activity, thus emphasizing the importance of its potential harmful effects on human health upon entry into the organism (Olea et al. 1996; Lee et al. 2003; Wetherill et al. 2002, 2007; Alonso-Magdalena et al. 2012). In males, such endocrine disruption may also affect the regulation of the hypothalamic–pituitary–gonadal axis, resulting in reproductive disorders and infertility.
3 Effects of In Utero Exposure to Bisphenol A on Male Reproductive Function
The harmful effects of BPA on male reproductive function, following in utero exposure, have been widely studied in laboratory animals such as rodents. vom Saal et al. (1998) studied prenatal BPA exposure on male mice and found increased size for preputial glands and reduced epididymides size, as well as decreased efficiency of sperm production (daily sperm production). A decrease in fertility, daily sperm production, sperm count and motility in BPA-exposed male offspring during adulthood was also reported (Salian et al. 2009a, 2011). Oral administration of 2–20 ng BPA/g body weight (bwt) to female mice on gestational day (GD) 11–17 resulted in a significant decrease of relative testis weight of male pups at 8 and 12 weeks of age (Kawai et al. 2003). When female mice were concomitantly administered BPA and di(2-ethylhexyl)phthalate (another plastic component), the expression level of Anti-Müllerian hormone (AMH) and Steroidogenic Acute Regulatory Protein (StAR) was reduced in the testes of the exposed male pups, and the pups’ testicular size was reduced. Importantly, the adverse effects were persistent in the sexually mature pups at postnatal day (PND) 42, and were consistent with significant reductions of epididymal sperm counts (Xi et al. 2012). Analysis of RNA samples from the hypothalamus, testes, and epididymides of rat fetuses, exposed to BPA in utero from GD 11–20, or GD 6–21, revealed modification of the gene expression profile, including hypothalamic estrogen receptors (ERs), testicular luteinizing hormone receptor (LHR), cholesterol side chain cleavage enzyme (Cyp11a1), and StAR (Naciff et al. 2005; Cao et al. 2013). BPA exposure affects hypothalamic development in the embryo. This was evidenced by enhanced dendritic and synaptic development in cultured hypothalamic cells from fetal rats, as manifested by increases in the area of dot-like staining of synapsin I and MAP2-positive area (Iwakura et al. 2010). Treatment of Ishikawa cell cultures with BPA also modulated the expression of the INSIG1 and FOS genes, which are implicated in regulating transcription and steroid metabolic processes, respectively (Naciff et al. 2010).
In pregnant female rats exposed to BPA from GD 1 throughout parturition, serum testosterone levels were decreased in male fetuses and pups (Tanaka et al. 2006). Exposures of the dams from GD 12 to PND 21 also resulted in decreased testosterone levels in the testicular interstitial fluid of male pups in adulthood (Akingbemi et al. 2004). The testosterone inhibition is probably induced by the BPA-suppressive effect on testicular Leydig cell steroidogenic proteins. In fact, BPA inhibits expression of the StAR protein, and the 17-β-hydroxysteroid dehydrogenase enzyme (17β-HSD) (Horstman et al. 2012; Nanjappa et al. 2012). Protein expression of the LHR is also compromised following BPA exposure, and may lead to decreasing androgen secretion by testicular Leydig cells (Nanjappa et al. 2012). The testosterone concentration increased in 9-week-old male pups exposed to BPA in utero and through lactation (Watanabe et al. 2003), and this could be attributed to in utero BPA-induced proliferative activity (mitogenic effect) on testosterone-producing Leydig cells (Nanjappa et al. 2012). In addition to modulating the Leydig cells, BPA also induced down-regulation of several genes associated with Sertoli cell function (Msi1h, Ncoa1, Nid1, Hspb2, and Gata6) in 6-week-old male mice after prenatal exposure (Tainaka et al. 2012), thereby disrupting the blood–testis barrier (BTB) and impairing spermatogenesis (Cheng et al. 2011; Su et al. 2011). Perturbation of BTB (reduction in the expression of Connexin 43 and increases in the expression of N-cadherin and Zona Occludin-1) and spermatogenesis were also observed in 45/90-day-old rats neonatally exposed to BPA (≥400 μg/kg bwt/day, during PND 1–5) (Salian et al. 2009b).
The biological effect of thyroid hormones that act on male reproductive function by modulating germ cell development (Krassas and Pontikides 2004) can also be compromised by BPA exposure during fetal life. BPA affects the expression of thyroid specific genes that have been implicated in thyroid development, as well as control of gene expression in rat thyroid cells and zebra fish embryos in vitro (Gentilcore et al. 2013). BPA antagonizes triiodothyronine (T3) action at the transcriptional level in human TSA201 cells, through displacement of T3 from the hormone receptor (TSH) and recruitment of a transcriptional repressor (a T3- negatively regulated TSHalpha promoter), resulting in gene suppression (Moriyama et al. 2002). A BPA antithyroid effect in rats was also observed in vivo. In fact, feeding pregnant Sprague-Dawley rats a BPA-containing diet during pregnancy and lactation caused an increase in serum total thyroxin in male pups on PND 15, with up-regulation of the expression of the thyroid hormone-responsive gene RC3/neurogranin in the dentate gyrus. This suggests a thyroid-hormone antagonist effect of BPA on the beta-thyroid receptor, which mediates the negative feedback effect of the hormone on the pituitary gland (Zoeller et al. 2005). In utero exposure of CD-1 pregnant mice to BPA (50 μg BPA/kg/day, during GD 16–18) also resulted in increasing the anogenital distance (AGD: distance from the center of the anus to the anterior base of the penis, an androgen-dependent variable, used as a sensitive marker of androgenic and antiandrogenic effects of in utero chemical exposure) in male pups (Gupta 2000; Foster and McIntyre 2002). This contrasted with studies of Talsness et al. (2000), who reported shortening of the AGD, following prenatal BPA exposure. Notwithstanding, these two studies indicated that BPA has the ability to modulate AGD during prenatal life.
These in utero effects are likely to also occur in BPA exposed human males. Such evidence has been derived from a recent epidemiological study conducted by Braun et al. (2012), who detected BPA in urine samples of pregnant women, suggesting gestational exposure. Moreover, Miao et al. (2011a) demonstrated an association between parental occupational BPA exposure during pregnancy and shortened AGD in male offspring. The latter association was stronger for maternal exposure, and the authors found a dose–response relationship between increased BPA levels in pregnancy and greater magnitude of shortened AGD. In Table 1, we summarize data from selected studies that addressed BPA’s male reproductive effects.
Because of its accumulation in amniotic fluid of pregnant women, BPA exposure appears to be more harmful in utero (Schönfelder et al. 2002; Sun et al. 2004), a critical hormonally dependent step in development of the individual. BPA acts as an endocrine disruptor (estrogenic, antiandrogenic, or antithyroid). It has been shown to reduce total blood T4 levels in pregnant women, with associated decreased TSH in their respective male neonates (Olea et al. 1996; Moriyama et al. 2002; Lee et al. 2003; Zoeller et al. 2005; Wetherill et al. 2007; Chevrier et al. 2013). BPA binds to ERs, inhibits androgen-induced androgen receptor (AR) transcriptional activity and androgen (dihydroxytestosterone) binding to AR (Lee et al. 2003; Alonso-Magdalena et al. 2012). However, recent findings support an additional BPA action mechanism, through a non-genomic pathway, initiated at membrane receptors, including classical ERs and/or G protein-coupled receptor 30 (reviewed by Iwakura et al. 2010). The estrogenicity of BPA can also prevent AMH action on the Müllerian ducts in the male (Pryor et al. 2000), leading to the feminization of male fetus (Hutson et al. 1994). Such feminization may be triggered by up-regulation of genes required for ovary development (Foxl2 and Wnt4), with concomitant repression of genes responsible for testis development (Sox9 and Fgf9) in the embryo, as reported elsewhere (Aoki and Takada 2012). By disrupting hormone levels or receptor activity, the detrimental effect of BPA may be to alter male reproductive-organ development during fetal life (Miao et al. 2011a, b). Moreover, the BPA effect may be more pronounced and irreversible during this development stage, unlike in adults, who have a matured and functional sex-specific physiology, in which the deleterious effect is potentially reversible once exposure ends (Kline and Ruhter 2012).
4 Effects of Bisphenol A on Spermatogenesis and Sperm Function Following Postnatal Exposure
4.1 Effects on the Hypothalamic–Pituitary–Testicular Axis
The spermatogenesis process in mammals is coordinated by the hypothalamic–pituitary–testicular axis and the thyroid gland (Zoeller et al. 2005; Moriyama et al. 2002). Dysfunction of the axis, triggered by endocrine disruptors such as BPA, may result in arrest or alteration of spermatogenesis (Table 1).
One adverse effect attributable to BPA is atrophy of the testes, as reported to have occurred in adult male Swiss mice treated with BPA glycerolate dimethacrylate (BISGMA, 100 μg/kg/day) for 60 days (Al-Hiyasat and Darmani 2006). White Leghorn male chicks treated with BPA (2 μg-200 m/kg/day) from 2 to 25 weeks of age also showed decreased testes size, and growth inhibition of androgen-dependent organs such as comb and wattle. The chicks receiving a higher BPA dose (≥20 μg/kg) showed inhibition of seminiferous tubuli development and spermatogenesis (Furuya et al. 2006), conditions more likely attributed to inhibition of testosterone synthesis. BPA’s modulatory effect on testosterone synthesis has been reported in several studies (Table 2).
Oral administration of BPA to young mice for 4–8 weeks resulted in a dramatic decrease of plasma free-testosterone levels (Takao et al. 1999). BPA exposure also decreased the serum testosterone level in adult male rats, and suppressed human chorionic gonadotropin (hCG)-induced testosterone release by the testis (Tohei et al. 2001; El-Beshbishy et al. 2012; D’Cruz et al. 2012a). This antiandrogenic activity results from the BPA inhibitory effect on testicular Leydig cell StAR protein and steroidogenic enzymes, such as 3-β-hydroxysteroid dehydrogenase (3β-HSD), and 17β-HSD (D’Cruz et al. 2012a; Hatef et al. 2012a).
Decreased activity of 3β-HSD and 17β-HSD, following BPA exposure, was also observed in both rat and human testis microsomes, together with inhibition of 17α-hydroxylase/17,20-lyase (CYP17A1) (Ye et al. 2011). Similarly, Akingbemi et al. (2004) reported that BPA inhibited Leydig cell CYP17A1. The inhibitory effect of BPA on CYP17 is likely a competitive-type inhibition, as demonstrated in Escherichia coli that expressed steroidogenic CYP17 (Niwa et al. 2001). Aromatase (CYP19) catalyzes conversion of androgens (testosterone) to estrogens (Carreau and Hess 2010; Carreau et al. 2010), and BPA exposure increased its expression in testes of male chicks, or in rat testicular Leydig cells (Furuya et al. 2006; Kim et al. 2010). This induction of testicular aromatase by BPA may thus contribute to decreased serum levels of androgens. However, Akingbemi et al. (2004) reported that postnatal BPA exposure of rats resulted in inhibited Leydig cell CYP19 expression and decreased serum 17β-estradiol levels. The latter authors exposed Long-Evans rats to BPA during perinatal period (PND 21–35) and noticed that serum estradiol was inhibited in the animals treated with the lower doses of BPA (0.2 μg–100 mg/kg bwt/day). The inhibitory effect was not observed at the highest dose (100 mg BPA/kg bwt/day), suggesting a dose-dependent effect of BPA on aromatase.
The fact that BPA causes an antisteroidogenic effect is further sustained by its ability to inhibit cAMP formation by preventing adenylate cyclase coupling to the luteinizing hormone (LH) receptor in vitro in mLTC-1 Leydig tumor cells (Nikula et al. 1999). Secretion of LH was also compromised in male animals exposed to BPA (Nakamura et al. 2010). The suppressed serum LH was associated with decreased LHbeta, decreased hypothalamic KiSS1 mRNA levels, and increased pituitary and testicular estrogen receptor (ER) mRNA levels (Akingbemi et al. 2004; Furuya et al. 2006; Navarro et al. 2009; Bai et al. 2011; Hatef et al. 2012a). An increased excretion (vs. matched controls) of BPA and decreased plasma follicle-stimulating hormone (FSH) was reported in men occupationally exposed to epoxy-resin hardening agents containing BPA diglycidyl ether (Hanaoka et al. 2002), suggesting inhibition of FSH release by the chemical (Salian et al. 2011). In contrast, Tohei et al. (2001) reported increased plasma LH, following treatment of adult male rats of the Wistar-Imamichi strain (300–350 g) with BPA (1 mg/rat/day for 2 weeks). The LH stimulatory effect was associated with decreased plasma concentrations of testosterone and prolactin, as well as testicular contents of inhibin, suggesting that BPA directly inhibits testicular functions. The increased level of plasma LH was probably due to a reduction in the negative feedback regulation of the hypothalamic–pituitary axis by testosterone. Discrepancies in modulation of LH secretion by BPA (stimulation, or inhibition) as demonstrated by Tohei et al. (2001) and Nakamura et al. (2010), emphasize that the BPA endocrine-disrupting effect may be affected by the age of the animal at the onset of exposure.
Inhibin is synthesized in adult rat testes by Sertoli cells. Any reduction of inhibin’s concentration in plasma, or in the testis (Tohei et al. 2001), therefore, suggests a dysfunction of the Sertoli cells. BPA-induced apoptosis of rat Sertoli cell was reported by Iida et al. (2003), and may result from an induction of caspase-3 by BPA (Mørck et al. 2010). BPA also promotes contact between harmful substances and developing sperm cells, by inducing inter-Sertoli cell BTB impairment (Toyama and Yuasa 2004; Salian et al. 2009b; Cheng et al. 2011). Sertoli cell function is pivotal in spermatogenesis, because it coordinates the differentiation of spermatogonia to mature spermatozoa, under stimulation of the FSH. Modulation of the Sertoli cells by BPA, directly or indirectly via inhibition of FSH synthesis (Hanaoka et al. 2002), may impair reproductive function in exposed males.
4.2 Effects of Bisphenol A on Spermatogenesis
The antiandrogenic and estrogenic effects of BPA that have been described in male goldfish (Carassius auratus) were associated with impairment of their spermatogenesis, as illustrated by the altered sperm parameters that were observed (viz., reduction in total sperm number, volume, density, motility, and velocity) (Hatef et al. 2012a, b). Lower semen quality was also observed in brown trout exposed to 1.75–2.40 μg/L BPA during the late prespawning and spawning periods (Lahnsteiner et al. 2005). Similarly, Haubruge et al. (2000) demonstrated declines in total sperm counts in adult male guppies exposed to BPA (274–549 μg/L) for 21 days. Such adverse effects of BPA on fish spermatogenesis have been documented to occur in rodents following the postnatal and pubertal periods, and in adulthood.
In mice, BPA induced the formation of morphologically multinucleated giant cells in testicular seminiferous tubules, having greater than three nuclei each (Takao et al. 1999). Similarly, a decrease of sperm count and motility was observed, and an increase of sperm morphological abnormalities, following 2 weeks of BPA administration (10–40 mg/kg bwt) (Dobrzyńska and Radzikowska 2013). The latter sperm parameters were also affected by a BPA derivative, BPA glycerolate dimethacrylate; this derivative induced decreased male mouse fertility (Al-Hiyasat and Darmani 2006). Administration of BPA (≥20 μg/kg bwt/day) to adult rats for 6 days decreased daily sperm production (Sakaue et al. 2001). Similarly, Chitra et al. (2003a) reported a reduction in epididymal sperm motility in adult rats exposed to BPA for 60 days.
The antispermatogenic effect of BPA demonstrated in experimental animals has been confirmed by several epidemiological studies conducted among groups of BPA-exposed human males. Examples include a study carried out in China in 2008, in which it was revealed that male factory workers exposed to high levels of BPA at work experienced a sexual dysfunction, characterized by reduced sexual desire, and greater erectile and ejaculatory difficulties (Li et al. 2010b). During a cross-sectional pilot study, Xiao et al. (2009) analyzed blood BPA and semen quantity in workers exposed to BPA, and compared results to a control group. The sperm density of exposed workers was significantly lower than that of the control group, which had a lower blood BPA concentration. Furthermore, there was a negative correlation between blood BPA concentration and the percentage of normal sperm, indicating the negative influence of BPA on the semen quality.
Meeker et al. (2010) found a positive association, though not statistically significant, between BPA exposure (urinary BPA concentration) and altered sperm parameters (viz., decreased sperm count, altered morphology and motility, and increased sperm DNA damage) among infertile men. In a study carried out in fertile men, the correlation of urinary BPA concentration with semen quality was suggestive of an inverse association with sperm count and sperm motility (Mendiola et al. 2010). The urinary BPA concentration of the subjects was inversely associated with the free androgen index (FAI) and the FAI/LH ratio, and positively correlated to sex hormone-binding globulin (SHBG), indicating a deregulation of spermatogenesis. Similarly, Wang et al. (2012c) reported an association between higher urinary BPA concentrations and clinically abnormal thyroid hormones (elevated serum free T3 levels) that also influence spermatogenesis.
Although a three-generation reproductive toxicity study of BPA exposure in CD Sprague-Dawley rats showed no treatment-related effects from BPA exposure on reproductive organs/parameters (Tyl et al. 2002), other adverse effects appeared to be consistent with those caused by BPA in previous studies. Furthermore, Tyl et al. (2002) investigated physiological parameters, but did not assess biochemical changes. Other authors have studied BPA and have reported that it caused various effects, including genotoxicity and clastogenicity in blood cells (Ulutaş et al. 2010; Dobrzyńska and Radzikowska 2013; Tiwari et al. 2012), increased susceptibility to chemically induced mammary carcinogenesis (Jenkins et al. 2012), and induced meiotic aneuploidy in oocytes (Hunt et al. 2003), suggesting possible modification of the DNA in male germ cells that may be transmitted to the next generation (Salian et al. 2011).
Further evidence that BPA causes adverse effects is provided by the results of an in vitro binding assay involving proteins that transport sex hormones (Déchaud et al. 1999). BPA is a xenoestrogen that binds to SHBG (a steroid transporter in human plasma), with a reversible and competitive binding activity for both testosterone and estradiol, and produces a dose-dependent increase in concentrations of hSHBG-unbound testosterone and/or estradiol. BPA may thus displace endogenous sex steroid hormones from hSHBG binding sites and disrupt the androgen-to-estrogen balance that is required for normal spermatogenesis (Déchaud et al. 1999; Carreau and Hess 2010).
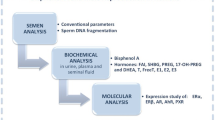
4.3 Effects of Bisphenol A on the Testicular and Epididymal Antioxidant System
Another important mechanism by which environmental toxicants exert their adverse effects on male reproductive function is to disturb the pro-oxidant–antioxidant balance of the testis, resulting in impairment of testicular function (Mathur et al. 2008). Testicular function is associated with production of reactive oxygen species (ROS) that are regulated by an antioxidant system, under normal physiologic conditions. Exposure to environmental toxicants such as BPA aggravates the production of ROS, leading to testicular oxidative stress (see Fig. 1). El-Beshbishy et al. (2012), orally administered BPA to male rats at a dose of 10 mg/kg bwt for 14 days, and observed a decrease of testicular antioxidant enzymes such as glutathione reductase, glutathione peroxidase, superoxide dismutase, and catalase. The levels of hydrogen peroxide (H2O2) and lipid peroxidation were also increased in testes and spermatozoa of BPA-treated animals. In another study, testicular antioxidant enzymes were impaired by a very low-dose (viz., 0.005 mg/kg bwt/day) of BPA following 45 days of exposure (De Flora et al. 2011; D’Cruz et al. 2012a, b). BPA also decreased antioxidant enzyme activities and induced lipid peroxidation in both epididymides and sperm cells (Chitra et al. 2003a) (Fig. 1). The latter antioxidant enzymes were negatively affected in liver (Bindhumol et al. 2003), the organ that synthesizes steroid transport proteins such as hSHBG (Pugeat et al. 2010).
A schematic diagram showing the main effects and action sites of BPA on male reproductive function: This schematic drawing depicts the hypothalamic–pituitary–testicular axis, and accessory organs. It also summarizes the spermatogenesis and sperm maturation processes. The main action sites where BPA modulates male reproductive function are indicated in the chart. The positive and negative signs indicate the following: (−): BPA disrupts cell function, reduces the weight of accessory organs, or inhibits hormone levels; (+): BPA induces increased hormone levels or reactive oxygen species (ROS), or stimulates enlargement of the prostate; (+/−): BPA exposure results in either induction (+) or inhibition (−) of hormone production. The numbers 1 to 7 refer to germ cells, at different developmental/maturation stages, viz. 1: spermatogonium; 2: preleptotene spermatocyte; 3: pachytene spermatocyte; 4: round spermatid; 5: elongated spermatid; 6 and 7: spermatozoa, before and after capacitation, respectively. Abbreviations: BTB blood–testis barrier, E2 estradiol, LC Leydig cell, FSH follicle-stimulating hormone, GnRH gonadotropin-releasing hormone, SC Sertoli cell, T testosterone
BPA acts to significantly disturb the pro-oxidant–antioxidant balance; therefore, reinforcing the ROS scavenging activity in the reproductive organs may represent a promising strategy to mitigate the BPA-related disturbances. To illustrate, in a recent study, Fang et al. (2013) reported that adolescent male mice, whose diet was supplemented with vitamin E during BPA exposure, showed an enhanced antioxidant response (i.e., increased SOD activity), and vitamin E protected against the reproductive inhibition normally caused by BPA.
4.4 Effects of Bisphenol A on Sperm Function
Whether BPA directly affects spermatozoa is still unclear. Luconi et al. (2001) incubated human spermatozoa in the presence of 1 μM BPA, and the results revealed no significant modification in calcium influxes and acrosome reaction in the spermatozoa. Similarly, the DNA integrity of sperm cells, as assessed using the Comet and TUNEL assays, and redox activity were not affected by BPA treatment in vitro (Bennetts et al. 2008). This suggests that the adverse effects on male reproductive function caused by BPA are mediated in vivo by other mechanisms, such as alteration of the hypothalamic–pituitary–gonadal axis and thyroid function (Akingbemi et al. 2004; Zoeller et al. 2005). Other examples of the effects caused by in vivo BPA exposure include altered sperm motility and velocity in goldfish (i.e., following 20–90 days exposure to 0.2 and 20 μg BPA/L) (Hatef et al. 2012a, b), and enhanced fragility of spermatozoa (i.e., as revealed by DNA fragmentation or sperm chromatin dispersion) in rats, following 10 days of administration of 200 mg BPA/kg bwt (De Flora et al. 2011). Meeker et al. (2010) also studied human male partners of subfertile couples seeking treatment from the Vincent Andrology Lab at Massachusetts General Hospital, and observed increased DNA damage in sperm, and reduced semen quality that were associated with BPA exposure (Fig. 1).
5 Effects of Bisphenol A on Accessory Reproductive Organs
Secretions of male reproductive accessory organs have been implicated in the maturation, motility, and vitality of spermatozoa in the female tract. These organs represent potential targets for antifertility compounds, such as BPA. When female rats were orally dosed to 2 and 20 μg BPA/kg bwt/day on GD 11–17, their male offspring showed enlargement of the prostate in adulthood (Nagel et al. 1997). The latter effect was also reported by Gupta (2000) in CD-1 mice, whose female progenitors received 50 μg BPA/kg/day, during GD 16–18. In addition, the pups showed reduced AGD and decreased epididymal weight (Gupta 2000; Talsness et al. 2000). Exposure of rats to low doses of BPA (≥0.2 μg BPA/kg/day for 45 days) during pubertal and adult life also induced decreased epididymal and testicular weights, as well as increased weight of ventral prostate (Chitra et al. 2003a, b). BPA also affected the prostate epigenome during development, and thereby promoted prostate cancer (Ho et al. 2006). Mitogenic effects in the prostatic gland have been further affirmed by in vitro studies on human prostatic adenocarcinoma (LNCaP). In fact, BPA initiated both an androgen-independent (inappropriate proliferation, through activation of the tumor-derived androgen receptor, AR-T877A) and an estrogen/androgen-dependent proliferation signalling pathway in LNCaP (Wetherill et al. 2002; Lee et al. 2012). Moreover, treatment of Ishikawa cell cultures with BPA modulated several genes implicated in regulation of transcription (SUZ12, HES2, FST, ATF3) (Naciff et al. 2010). The increased size of the preputial glands and atrophy of epididymides were also reported in mice prenatally exposed to BPA (vom Saal et al. 1998).
6 Effects of Bisphenol A Derivatives on Male Reproduction
Because of concerns for the effects of BPA, Canada was the first country to regulate the products in which BPA could be used. Canada banned the use of BPA in baby bottles in 2008. Since this occurred, other developed countries (e.g., Japan and the USA) have also acted to restrict the use of BPA in baby bottles, and to some degree, the manufacture or production of BPA. These countries have also promoted the development of alternative BPA isomers, such as Bisphenol S ((BPS; 4,4′-sulfonyldiphenol), Bisphenol F (BPF; 4,4′-dihydrox-ydiphenylmethane), Bisphenol AF (BPAF; 4,4′-(hexa fluoroisopropylidene)diphenol), and Bisphenol B (BPB; 2,2-bis(4-hydroxyphenyl)butane), all of which are thought to be safer (Health Canada 2008; Liao et al. 2012). Unfortunately, the biological activity (genotoxicity and estrogenicity) of these derivatives appears to be similar to that of BPA (Liao et al. 2012). BPAF acts as an agonist or antagonist to estrogen receptor alpha (ERα) or estrogen receptor beta (ERβ) (Matsushima et al 2010), and its administration to adult male rats for 14 days induced dysregulation of the hypothalamic–pituitary–testicular axis, characterized by increased LH and FSH levels, reduced serum testosterone, and a decline in testicular mRNA levels of inhibin B, ERα, and LHR (Feng et al. 2012).
7 Implications of Updated Data for Bisphenol A Exposure in Risk Assessment Studies
Human exposure to BPA is now of great concern, because of how widespread the chemical has become in the environment and because it is detected in human biological fluids. The harmful effects of BPA on male reproductive function have been clearly illustrated in animal-based studies, and the effects it produces appear to be more pronounced during fetal life (Lagos-Cabré and Moreno 2012). The reported data were essentially gathered from investigations that used rodents (rats and mice) as the animal model. However, BPA’s kinetics within rodent and primate (chimpanzee and monkey) systems are similar (Taylor et al. 2011), and support a conclusion that BPA effects observed in rodents may well be expected to occur in humans. Moreover, although glucuronidation of BPA (prior to urinary elimination) occurs both in rat and human liver microsomes, human liver microsomes do this less efficiently than do those of rats (Elsby et al. 2001), and this can lead to BPA bioaccumulation in humans, as recently suggested by Stahlhut et al. (2009). It is also of concern that human fetal testes are more sensitive to the deleterious effects (inhibition of testosterone secretion and insulin-like 3 mRNA levels in Leydig cells) of BPA than are testes of rodents (N’Tumba-Byn et al. 2012).
Therefore, we believe that regulators should reinforce actions to prevent exposures to BPA and BPA-related products, with particular emphasis on reducing exposures during fetal life (pregnancy) and babyhood, since these are the stages that are most sensitive to toxicity by this chemical. BPA also preferentially attacks the developing (rather than adult) testis during the puberty stage.
The current BPA tolerable daily intake values (TDI) proposed by the European Food Safety Authority and by Health Canada are 0.025 and 0.05 mg/kg bwt/day, respectively (EFSA 2010; Cao et al. 2011; Hengstler et al. 2011; Geens et al. 2012). These values are respectively based on animal studies, in which the lowest-observed-effect-level (LOEL) for BPA is 0.025 μg/kg bwt and 0.05 μg/kg bwt. These TDIs were derived from LOEL values using an uncertainty factor of 1,000 (10 for interspecies differences, 10 for interindividual differences, and 10 for LOEL to no-observed-effect-level or TDI). However, recent studies included in this review have provided evidence that harmful or adverse effects result from administering very low doses of BPA. D’Cruz et al. (2012a, b) showed that administering 0.005 μg BPA/kg bwt/day for 45 days inhibited rat testicular steroidogenic and antioxidant enzymes. This indicates that a more appropriate LOEL for BPA may be 0.005 μg/kg bwt in rats. Hence, we suggest a proper TDI to be 5 μg/kg bwt/day, instead of 25 or 50 μg/kg bwt/day (with an uncertainty factor of 1,000). Establishing a lower TDI that is more appropriate will assist in guiding authorities to limit human BPA exposure, and reduce the risk burden it places on health, and particularly on male reproductive function.
8 Summary
BPA is a ubiquitous environmental contaminant, resulting mainly from manufacturing, use or disposal of plastics of which it is a component, and the degradation of industrial plastic-related wastes. Growing evidence from research on laboratory animals, wildlife, and humans supports the view that BPA produces an endocrine-disrupting effect and adversely affects male reproductive function. To better understand the adverse effects caused by exposure to BPA, we performed an up-to-date literature review on the topic, with particular emphasis on in utero exposure, and associated effects on spermatogenesis, steroidogenesis, and accessory organs.
BPA studies on experimental animals show that effects are generally more detrimental during in utero exposure, a critical developmental stage for the embryo. BPA has been found to produce several defects in the embryo, such as feminization of male fetuses, atrophy of the testes and epididymides, increased prostate size, shortening of AGD, disruption of BTB, and alteration of adult sperm parameters (e.g., sperm count, motility, and density). BPA also affects embryo thyroid development.
During the postnatal and pubertal periods and adulthood, BPA affects the hypothalamic–pituitary–testicular axis by modulating hormone (e.g., LH and FSH, androgen and estrogen) synthesis, expression and function of respective receptors (ER, AR). These effects alter sperm parameters. BPA also induces oxidative stress in the testis and epididymis, by inhibiting antioxidant enzymes and stimulating lipid peroxidation. This suggests that employing antioxidants may be a promising strategy to relieve BPA-induced disturbances.
Epidemiological studies have also provided data indicating that BPA alters male reproductive function in humans. These investigations revealed that men occupationally exposed to BPA had high blood/urinary BPA levels, and abnormal semen parameters. BPA-exposed men also showed reduced libido and erectile ejaculatory difficulties; moreover, the overall BPA effects on male reproduction appear to be more harmful if exposure occurs in utero.
The regulation of BPA and BPA-related products should be reinforced, particularly where exposure during the fetal period can occur. The current TDI for BPA is proposed as 25 and 50 μg/kg bwt/day (European Food Safety Authority and Health Canada, respectively). Based on the evidence available, we believe that a TDI value of 5 μg/kg bwt/day is more appropriate (the endpoint is modulation of rat testicular function). Certain BPA derivatives are being considered as alternatives to BPA. However, certain of these related products display adverse effects that are similar to those of BPA. These effects should be carefully considered before using them as final alternatives to BPA in plastic production.
References
Akingbemi BT, Sottas CM, Koulova AI, Klinefelter GR, Hardy MP (2004) Inhibition of testicular steroidogenesis by the xenoestrogen bisphenol A is associated with reduced pituitary luteinizing hormone secretion and decreased steroidogenic enzyme gene expression in rat Leydig cells. Endocrinology 145:592–603
Al-Hiyasat AS, Darmani H (2006) In vivo effects of BISGMA-a component of dental composite-on male mouse reproduction and fertility. J Biomed Mater Res A 78:66–72
Alonso-Magdalena P, Ropero AB, Soriano S, García-Arévalo M, Ripoll C, Fuentes E, Quesada I, Nadal Á (2012) Bisphenol-A acts as a potent estrogen via non-classical estrogen triggered pathways. Mol Cell Endocrinol 355:201–207
Aoki T, Takada T (2012) Bisphenol A modulates germ cell differentiation and retinoic acid signaling in mouse ES cells. Reprod Toxicol 34(3):463–470
Bai Y, Chang F, Zhou R, Jin PP, Matsumoto H, Sokabe M, Chen L (2011) Increase of anteroventral periventricular kisspeptin neurons and generation of E2-induced LH-surge system in male rats exposed perinatally to environmental dose of bisphenol-A. Endocrinology 152(4):1562–1571
Batista TM, Alonso-Magdalena P, Vieira E, Amaral MEC, Cederroth CR, Nef S, Quesada I, Carneiro EM, Nadal A (2012) Short-term treatment with Bisphenol- A leads to metabolic abnormalities in adult male mice. PLoS One 7(3):e33814. doi:10.1371/journal.pone.0033814)
Bennetts LE, De Iuliis GN, Nixon B, Kime M, Zelski K, McVicar CM, Lewis SE, Aitken RJ (2008) Impact of estrogenic compounds on DNA integrity in human spermatozoa: evidence for cross-linking and redox cycling activities. Mutat Res 641(1–2):1–11
Bindhumol V, Chitra KC, Mathur PP (2003) Bisphenol A induces reactive oxygen species generation in the liver of male rats. Toxicology 188(2–3):117–124
Braun JM, Smith KW, Williams PL, Calafat AM, Berry K, Ehrlich S, Hauser R (2012) Variability of urinary phthalate metabolite and bisphenol A concentrations before and during pregnancy. Environ Health Perspect 120:739–745
Calafat AM, Kuklenyik Z, Reidy JA, Caudill SP, Ekong J, Needham LL (2005) Urinary concentrations of bisphenol A and 4-nonylphenol in a human reference population. Environ Health Perspect 113:391–395
Calafat AM, Weuve J, Ye X, Jia LT, Hu H, Ringer S, Huttner K, Hauser R (2009) Exposure to bisphenol A and other phenols in neonatal intensive care unit premature infants. Environ Health Perspect 117:639–644
Callan AC, Hinwood AL, Heffernan A, Eaglesham G, Mueller J, Odland JO (2012) Urinary bisphenol A concentrations in pregnant women. Int J Hyg Environ Health (in press). doi:10.1016/j.ijheh.2012.10.002
Cao XL, Perez-Locas C, Dufresne G, Clement G, Popovic S, Beraldin F, Dabeka RW, Feeley M (2011) Concentrations of bisphenol A in the composite food samples from the 2008 Canadian total diet study in Quebec City and dietary intake estimates. Food Addit Contam Part A Chem Anal Control Expo Risk Assess 28(6):791–798
Cao J, Rebuli ME, Rogers J, Todd KL, Leyrer SM, Ferguson SA, Patisaul HB (2013) Prenatal bisphenol A exposure alters sex-specific estrogen receptor expression in the neonatal rat hypothalamus and amygdala. Toxicol Sci 133(1):157–173
Carreau S, Hess RA (2010) Oestrogens and spermatogenesis. Phil Trans R Soc B 365:1517–1535
Carreau S, Wolczynski S, Galeraud-Denis I (2010) Aromatase, oestrogens and human male reproduction. Phil Trans R Soc B 365:1571–1579
Cheng CY, Wong EW, Lie PP, Li MW, Su L, Siu ER, Yan HH, Mannu J, Mathur PP, Bonanomi M, Silvestrini B, Mruk DD (2011) Environmental toxicants and male reproductive function. Spermatogenesis 1(1):2–13
Chevrier J, Gunier RB, Bradman A, Holland NT, Calafat AM, Eskenazi B, Harley KG (2013) Maternal urinary bisphenol a during pregnancy and maternal and neonatal thyroid function in the CHAMACOS study. Environ Health Perspect 121(1):138–144
Chitra KC, Latchoumycandane C, Mathur PP (2003a) Induction of oxidative stress by bisphenol A in the epididymal sperm of rats. Toxicology 185(1–2):119–127
Chitra KC, Rao KR, Mathur PP (2003b) Effect of bisphenol A and co-administration of bisphenol A and vitamin C on epididymis of adult rats: a histological and biochemical study. Asian J Androl 5(3):203–208
Cho S, Choi YS, Luu HM, Guo J (2012) Determination of total leachable bisphenol A from polysulfone membranes based on multiple consecutive extractions. Talanta 101:537–540
Cui W (2010) Mother or nothing: the agony of infertility. Bull World Health Organ 88:881–882
D’Cruz SC, Jubendradass R, Jayakanthan M, Rani SJ, Mathur PP (2012) Bisphenol A impairs insulin signaling and glucose homeostasis and decreases steroidogenesis in rat testis: an in vivo and in silico study. Food Chem Toxicol 50:1124–1133
De Flora S, Micale RT, La Maestra S, Izzotti A, D’Agostini F, Camoirano A, Davoli SA, Troglio MG, Rizzi F, Davalli P, Bettuzzi S (2011) Upregulation of clusterin in prostate and DNA damage in spermatozoa from bisphenol A–treated rats and formation of DNA adducts in cultured human prostatic cells. Toxicol Sci 122:45–51
Déchaud H, Ravard C, Claustrat F, de la Perrière AB, Pugeat M (1999) Xenoestrogen interaction with human sex hormone-binding globulin (hSHBG). Steroids 64(5):328–334
Demierre AL, Peter R, Oberli A, Bourqui-Pittet M (2012) Dermal penetration of bisphenol A in human skin contributes marginally to total exposure. Toxicol Lett 213(3):305–308
Dobrzyńska MM, Radzikowska J (2013) Genotoxicity and reproductive toxicity of bisphenol A and X-ray/bisphenol A combination in male mice. Drug Chem Toxicol 36(1):19–26
Doerge DR, Twaddle NC, Vanlandingham M, Fisher JW (2012) Pharmacokinetics of bisphenol A in serum and adipose tissue following intravenous administration to adult female CD-1 mice. Toxicol Lett 211(2):114–119
El-Beshbishy HA, Aly HA, El-Shafey M (2012) Lipoic acid mitigates bisphenol A-induced testicular mitochondrial toxicity in rats. Toxicol Ind Health (in press). doi:10.1177/0748233712446728
Elsby R, Maggs JL, Ashby J, Park BK (2001) Comparison of the modulatory effects of human and rat liver microsomal metabolism on the estrogenicity of bisphenol A: implications for extrapolation to humans. J Pharmcol Exp Ther 297:103–113
Fang Y, Zhou Y, Zhong Y, Gao X, Tan T (2013) Effect of vitamin E on reproductive functions and anti-oxidant activity of adolescent male mice exposed to bisphenol A. (Article in Chinese). Wei Sheng Yan Jiu 42(1):18–22
Feng Y, Yin J, Jiao Z, Shi J, Li M, Shao B (2012) Bisphenol AF may cause testosterone reduction by directly affecting testis function in adult male rats. Toxicol Lett 211:201–209
EFSA (European Food Safety Authority) (2006) Opinion of the scientific panel on food additives, flavourings, processing aids and materials in contact with food on a request from the commission related to 2,2-bis(4-hydroxyphenyl) propane (Bisphenol A). Question number EFSA-Q-2005-100. EFSA J 428:1–75. http://www.efsa.europa.eu/fr/scdocs/scdoc/428.htm. Accessed 31 Jan 2013
EFSA (European Food Safety Authority) (2010) Scientific opinion on Bisphenol A: evaluation of a study investigating its neurodevelopmental toxicity, review of recent scientific literature on its toxicity and advice on the Danish risk assessment of Bisphenol A of the EFSA Panel on Food Contact Materials, Enzymes, Flavourings and Processing Aids (CEF) on request from the European Commission, Questions No. EFSA-Q-2009-00864, EFSA-Q-2010-01023 and EFSA-Q-2010-00709, adopted on 23rd September 2010. EFSA J 8:1829, 1–116. http://www.efsa.europa.eu/en/scdocs/scdoc/1829.htm. Accessed 31 Jan 2013
Foster PM, McIntyre BS (2002) Endocrine active agents: implications of adverse and non-adverse changes. Toxicol Pathol 30(1):59–65
Furuya M, Adachi K, Kuwahara S, Ogawa K, Tsukamoto Y (2006) Inhibition of male chick phenotypes and spermatogenesis by Bisphenol-A. Life Sci 78:1767–1776
Geens T, Aerts D, Berthot C, Bourguignon JP, Goeyens L, Lecomte P, Maghuin-Rogister G, Pironnet AM, Pussemier L, Scippo ML, Van Loco J, Covaci A (2012) A review of dietary and non-dietary exposure to bisphenol-A. Food Chem Toxicol 50(10):3725–3740
Gentilcore D, Porreca I, Rizzo F, Ganbaatar E, Carchia E, Mallardo M, De Felice M, Ambrosino C (2013) Bisphenol A interferes with thyroid specific gene expression. Toxicology 304:21–31
Gupta C (2000) Reproductive malformation of the male offspring following maternal exposure to estrogenic chemicals. Proc Soc Exp Biol Med 224:61–68
Hamada A, Esteves SC, Agarwal A (2011) The role of contemporary andrology in unraveling the mystery of unexplained male infertility. Open Reprod Sci J 4:27–41
Hammer J, Kraak MH, Parsons JR (2012) Plastics in the marine environment: the dark side of a modern gift. Rev Environ Contam Toxicol 220:1–44
Hanaoka T, Kawamura N, Hara K, Tsugane S (2002) Urinary bisphenol A and plasma hormone concentrations in male workers exposed to bisphenol A diglycidyl ether and mixed organic solvents. Occup Environ Med 59(9):625–628
Hatef A, Alavi SM, Abdulfatah A, Fontaine P, Rodina M, Linhart O (2012a) Adverse effects of bisphenol A on reproductive physiology in male goldfish at environmentally relevant concentrations. Ecotoxicol Environ Saf 76:56–62
Hatef A, Zare A, Alavi SM, Habibi HR, Linhart O (2012b) Modulations in androgen and estrogen mediating genes and testicular response in male goldfish exposed to bisphenol A. Environ Toxicol Chem 31(9):2069–2077
Haubruge E, Petit F, Gage MJ (2000) Reduced sperm counts in guppies (Poecilia reticulata) following exposure to low levels of tributyltin and bisphenol A. Proc Biol Sci 267(1459):2333–2337
He Y, Miao M, Herrinton LJ, Wu C, Yuan W, Zhou Z, Li DK (2009a) Bisphenol A levels in blood and urine in a Chinese population and the personal factors affecting the levels. Environ Res 109:629–633
He Y, Miao M, Wu C, Yuan W, Gao E, Zhou Z, Li DK (2009b) Occupational exposure levels of bisphenol A among Chinese workers. J Occup Health 51:432–436
Health Canada (2008) Government of Canada takes action on another chemical of concern: bisphenol A, April 18, 2008. http://www.marketwire.com/printer_friendly?id=845680. Accessed 31 Jan 2013
Hengstler JG, Foth H, Gebel T, Kramer PJ, Lilienblum W, Schweinfurth H, Völkel W, Wollin KM, Gundert-Remy U (2011) Critical evaluation of key evidence on the human health hazards of exposure to bisphenol A. Crit Rev Toxicol 41:263–291
Ho SM, Tang WY, Belmonte de Frausto J, Prins GS (2006) Developmental exposure to estradiol and bisphenol A increases susceptibility to prostate carcinogenesis and epigenetically regulates phosphodiesterase type 4 variant 4. Cancer Res 66:5624–5632
Horstman KA, Naciff JM, Overmann GJ, Foertsch LM, Richardson BD, Daston GP (2012) Effects of transplacental 17-α-ethynyl estradiol or bisphenol A on the developmental profile of steroidogenic acute regulatory protein in the rat testis. Birth Defects Res B Dev Reprod Toxicol 95:318–325
Huang YQ, Wong CKC, Zheng JS, Bouwman H, Barra R, Wahlström B, Neretin L, Wong MH (2011) Bisphenol A (BPA) in China: a review of sources, environmental levels, and potential human health impacts. Environ Int 42:91–99
Hunt PA, Koehler KE, Susiarjo M, Hodges CA, Ilagan A, Voigt RC, Thomas S, Thomas BF, Hassold TJ (2003) Bisphenol a exposure causes meiotic aneuploidy in the female mouse. Curr Biol 13:546–553
Hutson JM, Baker M, Terada M, Zhou B, Paxton G (1994) Hormonal control of testicular descent and the cause of cryptorchidism. Reprod Fertil Dev 6:151–156
Ignatius CM, Francis EE, Emeka EN, Elvis NS, Ebele JI (2010) BPA and environmental estrogen in potable water sources in Enugu municipality, South-East, Nigeria. Bull Environ Contam Toxicol 85:534–537
Iida H, Maehara K, Doiguchi M, Mōri T, Yamada F (2003) Bisphenol A-induced apoptosis of cultured rat Sertoli cells. Reprod Toxicol 17(4):457–464
Ikezuki Y, Tsutsumi O, Takai Y, Kamei Y, Taketani Y (2002) Determination of bisphenol A concentrations in human biological fluids reveals significant early prenatal exposure. Hum Reprod 17:2839–2841
Iwakura T, Iwafuchi M, Muraoka D, Yokosuka M, Shiga T, Watanabe C, Ohtani-Kaneko R (2010) In vitro effects of bisphenol A on developing hypothalamic neurons. Toxicology 272:52–58
Jenkins S, Betancourt AM, Wang J, Lamartiniere CA (2012) Endocrine-active chemicals in mammary cancer causation and prevention. J Steroid Biochem Mol Biol 129:191–200
Kaddar N, Bendridi N, Harthé C, Rolland de Ravel M, Bienvenu AL, Cuilleron CY, Mappus E, Pugeat M, Déchaud H (2009) Development of a radioimmunoassay for the measurement of Bisphenol A in biological samples. Anal Chim Acta 645:1–4
Kang YG, Kim JY, Kim J, Won PJ, Nam JH (2011) Release of bisphenol A from resin composite used to bond orthodontic lingual retainers. Am J Orthod Dentofacial Orthop 140:779–789
Kawai K, Nozaki T, Nishikata H, Aou S, Takii M, Kubo C (2003) Aggressive behavior and serum testosterone concentration during the maturation process of male mice: the effects of fetal exposure to bisphenol A. Environ Health Perspect 111:175–178
Kim JY, Han EH, Kim HG, Oh KN, Kim SK, Lee KY, Jeong HG (2010) Bisphenol A-induced aromatase activation is mediated by cyclooxygenase-2 up-regulation in rat testicular Leydig cells. Toxicol Lett 193:200–208
Kline TR, Ruhter MC (2012) Alternatives analysis report for Bisphenol-A in infant formula cans and baby food jar lids. Prepared for Maine Department of Environmental Protection, Bureau of Remediation and Waste Management. http://www.maine.gov/dep/safechem/documents/AAR-Report-December2012.pdf. Accessed 31 Jan 2013
Krassas GE, Pontikides N (2004) Male reproductive function in relation with thyroid alterations. Best Pract Res Clin Endocrinol Metab 18(2):183–195
Lagos-Cabré R, Moreno RD (2012) Contribution of environmental pollutants to male infertily: a working model of germ cell apoptosis induced by plasticizers. Biol Res 45:5–14
Lahnsteiner F, Berger B, Kletzl M, Weismann T (2005) Effect of bisphenol A on maturation and quality of semen and eggs in the brown trout, Salmo trutta f. fario. Aquat Toxicol 75(3):213–224
Lee HJ, Chattopadhyay S, Gong EY, Ahn RS, Lee K (2003) Antiandrogenic effects of bisphenol A and nonylphenol on the function of androgen receptor. Toxicol Sci 75:40–46
Lee YJ, Ryu HY, Kim HK, Min CS, Lee JH, Kim E, Nam BH, Park JH, Jung JY, Jang DD, Park EY, Lee KH, Ma JY, Won HS, Im MW, Leem JH, Hong YC, Yoon HS (2008) Maternal and fetal exposure to bisphenol A in Korea. Reprod Toxicol 25:413–419
Lee HR, Hyun SH, Jeung EB, Choi KC (2012) 193 Bisphenol A and phthalate enhanced the growth of prostate cancer cells and altered TGF-β signaling molecules via an estrogen receptor or androgen receptor-dependent pathway in in vitro and in vivo models. Reprod Fertil Dev 25(1):245–246
Li D, Zhou Z, Qing D, He Y, Wu T, Miao M, Wang J, Weng X, Ferber JR, Herrinton LJ, Zhu Q, Gao E, Checkoway H, Yuan W (2010a) Occupational exposure to bisphenol-A (BPA) and the risk of self-reported male sexual dysfunction. Hum Reprod 25(2):519–527
Li DK, Zhou Z, Miao M, He Y, Qing D, Wu T, Wang J, Weng X, Ferber J, Herrinton LJ, Zhu Q, Gao E, Yuan W (2010b) Relationship between urine bisphenol-A level and declining male sexual function. J Androl 31:500–506
Li DK, Zhou Z, Miao M, He Y, Wang J, Ferber J, Herrinton LJ, Gao E, Yuan W (2011) Urine bisphenol-A (BPA) level in relation to semen quality. Fertil Steril 95:625–630
Liao C, Kannan K (2011) High levels of bisphenol A in paper currencies from several countries, and implications for dermalexposure. Environ Sci Technol 45:6761–6768
Liao C, Liu F, Kannan K (2012) Bisphenol S, a new bisphenol analogue, in paper products and currency bills and its association with bisphenol A residues. Environ Sci Technol 46:6515–6522
Luconi M, Bonaccorsi L, Forti G, Baldi E (2001) Effects of estrogenic compounds on human spermatozoa: evidence for interaction with anongenomic receptor for estrogen on human sperm membrane. Mol Cell Endocrinol 178:39–45
Mathur PP, Saradha B, Vaithinathan S (2008) Impact of environmental toxicants on testicular function. Immunol Endocr Metab Agents Med Chem 8:79–90
Matsushima A, Liu X, Okada H, Shimohigashi M, Shimohigashi Y (2010) Bisphenol AF is a full agonist for the estrogen receptor ERα but a highly specific antagonist for ERβ. Environ Health Perspect 118(9):1267–1272
Meeker JD, Ehrlich S, Toth TL, Wright DL, Calafat AM, Trisini AT, YE X, Hauser R (2010) Semen quality and sperm DNA damage in relation to urinary bisphenol A among men from an infertility clinic. Reprod Toxicol 30:532–539
Mendiola J, Jørgensen N, Andersson A-M, Calafat AM, Ye X, Redmon JB, Drobnis EZ, Wang C, Sparks A, Thurston SW, Liu F, Swan SH (2010) Are environmental levels of bisphenol associated with reproductive function in fertile men? Environ Health Perspect 118(9):1286–1291
Miao M, Yuan W, He Y, Zhou Z, Wang J, Gao E, Li G, Li DK (2011a) In utero exposure to bisphenol-A and anogenital distance of male offspring. Birth Defects Res A Clin Mol Teratol 91:867–872
Miao M, Yuan W, Zhu G, He X, Li DK (2011b) In utero exposure to bisphenol-A and its effect on birth weight of offspring. Reprod Toxicol 32:64–68
Molina-García L, Fernández-de Córdova ML, Ruiz-Medina A (2012) Analysis of Bisphenol A in milk by using a multicommuted fluorimetric sensor. Talanta 96:195–201
Mørck TJ, Sorda G, Bechi N, Rasmussen BS, Nielsen JB, Ietta F, Rytting E, Mathiesen L, Paulesu L, Knudsen LE (2010) Placental transport and in vitro effects of Bisphenol A. Reprod Toxicol 30(1):131–137
Moriyama K, Tagami T, Akamizu T, Usui T, Saijo M, Kanamoto N, Hataya Y, Shimatsu A, Kuzuya H, Nakao K (2002) Thyroid hormone action is disrupted by bisphenol A as an antagonist. J Clin Endocrinol Metab 87:5185–5190
N’Tumba-Byn T, Moison D, Lacroix M, Lecureuil C, Lesage L, Prud’homme SM, Pozzi-Gaudin S, Frydman R, Benachi A, Livera G, Rouiller-Fabre V, Habert R (2012) Differential effects of bisphenol A and diethylstilbestrol on human, rat and mouse fetal leydig cell function. PLoS One 7(12):e51579. doi:10.1371/journal.pone.0051579
Naciff JM, Hess KA, Overmann GJ, Torontali SM, Carr GJ, Tiesman JP, Foertsch LM, Richardson BD, Martinez JE, Daston GP (2005) Gene expression changes induced in the testis by transplacental exposure to high and low doses of 17{alpha}-ethynyl estradiol, genistein, or bisphenol A. Toxicol Sci 86:396–416
Naciff JM, Khambatta ZS, Reichling TD, Carr GJ, Tiesman JP, Singleton DW, Khan SA, Daston GP (2010) The genomic response of Ishikawa cells to bisphenol A exposure is dose- and time-dependent. Toxicology 270:137–149
Nagel SC, Vom Saal FS, Thayer KA, Dhar MG, Boechler M, Welshons WV (1997) Relative binding affinity-serum modified access (RBA-SMA) assay predicts the relative in vivo bioactivity of the xenoestrogens bisphenol A and octylphenol. Environ Health Perspect 105:70–76
Nahar MS, Soliman AS, Colacino JA, Calafat AM, Battige K, Hablas A, Seifeldin IA, Dolinoy DC, Rozek LS (2012) Urinary bisphenol A concentrations in girls from rural and urban Egypt: a pilot study. Environ Health 11:20. doi:10.1186/1476-069X-11-20
Nakamura D, Yanagiba Y, Duan Z, Ito Y, Okamura A, Asaeda N, Tagawa Y, Li C, Taya K, Zhang SY, Naito H, Ramdhan DH, Kamijima M, Nakajima T (2010) Bisphenol A may cause testosterone reduction by adversely affecting both testis and pituitary systems similar to estradiol. Toxicol Lett 194(1–2):16–25
Nanjappa MK, Simon L, Akingbemi BT (2012) The industrial chemical bisphenol A (BPA) interferes with proliferative activity and development of steroidogenic capacity in rat Leydig cells. Biol Reprod 86(5):135. doi:10.1095/biolreprod.111.095349, 1–12
Navarro VM, Sánchez-Garrido MA, Castellano JM, Roa J, García-Galiano D, Pineda R, Aguilar E, Pinilla L, Tena-Sempere M (2009) Persistent impairment of hypothalamic KiSS-1 system after exposures to estrogenic compounds at critical periods of brain sex differentiation. Endocrinology 150(5):2359–2367
Nikula H, Talonpoika T, Kaleva M, Toppari J (1999) Inhibition of hCG-stimulated steroidogenesis in cultured mouse Leydig tumor cells by bisphenol A and octylphenols. Toxicol Appl Pharmacol 157:166–173
Niwa T, Fujimoto M, Kishimoto K, Yabusaki Y, Ishibashi F, Katagiri M (2001) Metabolism and interaction of bisphenol A in human hepatic cytochrome P450 and steroidogenic CYP17. Biol Pharm Bull 24:1064–1067
Olea N, Pulgar R, Pérez P, Olea-Serrano F, Rivas A, Novillo-Fertrell A, Pedraza V, Soto AM, Sonnenschein C (1996) Estrogenicity of resin-based composites and sealants used in dentistry. Environ Health Perspect 104:298–305
Pryor JL, Hughes C, Foster W, Hales BF, Robaire B (2000) Critical windows of exposure for children’s health: the reproductive system in animals and humans. Environ Health Perspect 108(3):491–503
Pugeat M, Nader N, Hogeveen K, Raverot G, Déchaud H, Grenot C (2010) Sex hormone-binding globulin gene expression in the liver: drugs and the metabolic syndrome. Mol Cell Endocrinol 316(1):53–59
Rocha S, Domingues VF, Pinho C, Fernandes VC, Delerue-Matos C, Gameiro P, Mansilha C (2013) Occurrence of Bisphenol A, Estrone, 17b-Estradiol and 17a-Ethinylestradiol in Portuguese Rivers. Bull Environ Contam Toxicol 90(1):73–78
Rudel RA, Gray JM, Engel CL, Rawsthorne TW, Dodson RE, Ackerman JM, Rizzo J, Nudelman JL, Brody JG (2011) Food packaging and bisphenol A and bis(2-ethyhexyl) phthalate exposure: findings from a dietary intervention. Environ Health Perspect 119(7):914–920
Sakaue M, Ohsako S, Ishimura R, Kurosawa S, Kurohmaru M, Hayashi Y, Aoki Y, Yonemoto J, Tohyama C (2001) Bisphenol-A affects spermatogenesis in the adult rat even at a low dose. J Occup Health 43:185–190
Salian S, Doshi T, Vanage G (2009a) Neonatal exposure of male rats to Bisphenol A impairs fertility and expression of Sertoli cell junctional proteins in the testis. Toxicology 265(1–2):56–67
Salian S, Doshi T, Vanage G (2009b) Perinatal exposure of rats to Bisphenol A affects the fertility of male offspring. Life Sci 85:742–752
Salian S, Doshi T, Vanage G (2011) Perinatal exposure of rats to Bisphenol A affects fertility of male offspring–an overview. Reprod Toxicol 31(3):359–362
Schönfelder G, Wittfoht W, Hopp H, Talsness CE, Paul M, Chahoud I (2002) Parent bisphenol A accumulation in the human maternal-fetal-placental unit. Environ Health Perspect 110:A703–A707
Shankar A, Teppala S (2012) Urinary bisphenol A and hypertension in a multiethnic sample of US adults. J Environ Public Health 2012:481641. doi:10.1155/2012/481641
Stahlhut RW, Welshons WV, Swan SH (2009) Bisphenol A data in NHANES suggest longer than expected half-life, substantial nonfood exposure, or both. Environ Health Perspect 117(5):784–789
Su L, Mruk DD, Cheng CY (2011) Drug transporters, the blood–testis barrier, and spermatogenesis. J Endocrinol 208:207–223
Sun Y, Irie M, Kishikawa N, Wada M, Kuroda N, Nakashima K (2004) Determination of bisphenol A in human breast milk by HPLC with column-switching and fluorescence detection. Biomed Chromatogr 18(8):501–507
Tainaka H, Takahashi H, Umezawa M, Tanaka H, Nishimune Y, Oshio S, Takeda K (2012) Evaluation of the testicular toxicity of prenatal exposure to bisphenol A based on microarray analysis combined with MeSH annotation. J Toxicol Sci 37:539–548
Takao T, Nanamiya W, Nagano I, Asaba K, Kawabata K, Hashimoto K (1999) Exposure with the environmental estrogen bisphenol A disrupts the male reproductive tract in young mice. Life Sci 65:2351–2357
Talsness C, Fialkowski O, Gericke C, Merker H-J, Chahoud I (2000) The effects of low and high doses of bisphenol A on the reproductive system of female and male rat offspring. Congenit Anom 40:S94–S107
Tanaka M, Nakaya S, Katayama M, Leffers H, Nozawa S, Nakazawa R, Iwamoto T, Kobayashi S (2006) Effect of prenatal exposure to bisphenol A on the serum testosterone concentration of rats at birth. Hum Exp Toxicol 25:369–373
Taylor JA, Vom Saal FS, Welshons WV, Drury B, Rottinghaus G, Hunt PA, Toutain PL, Laffont CM, VandeVoort CA (2011) Similarity of bisphenol A pharmacokinetics in rhesus monkeys and mice: relevance for human exposure. Environ Health Perspect 119(4):422–430.
Tiwari D, Kamble J, Chilgunde S, Patil P, Maru G, Kawle D, Bhartiya U, Joseph L, Vanage G (2012) Clastogenic and mutagenic effects of bisphenol A: an endocrine disruptor. Mutat Res 743:83–90
Tohei A, Suda S, Taya K, Hashimoto T, Kogo H (2001) Bisphenol A inhibits testicular functions and increases luteinizing hormone secretion in adult male rats. Exp Biol Med (Maywood) 226(3):216–221
Toppari J, Larsen JC, Christiansen P, Giwercman A, Grandjean P, Guillette LJ Jr, Jegou B, Jensen TK, Jouannet P, Keiding N, Leffers H, McLachlan JA, Meyer O, MIlIer J, Rajpert-De Meyts E, Scheike T, Sharpe R, Sumpter J, Skakkebaekl NE (1996) Male reproductive health and environmental xenoestrogens. Environ Health Perspect 104:741–803
Toyama Y, Yuasa S (2004) Effects of neonatal administration of 17β-estradiol, β-estradiol 3-benzoate, or bisphenol A on mouse and rat spermatogenesis. Reprod Toxicol 19:181–188
Tyl RW, Myers CB, Marr MC, Thomas BF, Keimowitz AR, Brine DR, Veselica MM, Fail PA, Chang TY, Seely JC, Joiner RL, Butala JH, Dimond SS, Cagen SZ, Shiotsuka RN, Stropp GD, Waechter JM (2002) Three-generation reproductive toxicity study of dietary bisphenol A in CD Sprague-Dawley rats. Toxicol Sci 68:121–146
Ulutaş OK, Yildiz N, Durmaz E, Ahbab MA, Barlas N, Çok İ (2010) An in vivo assessment of the genotoxic potential of bisphenol A and 4-tert-octylphenol in rats. Arch Toxicol 85:995–1001
Ünüvar T, Büyükgebiz A (2012) Fetal and neonatal endocrine disruptors. J Clin Res Pediatr Endocrinol 4(2):51–60
Vandenberg LN, Maffini MV, Sonnenschein C, Rubin BS, Soto AM (2009) Bisphenol-A and the great divide: a review of controversies in the field of endocrine disruption. Endocr Rev 30(1):75–95
Völkel W, Kiranoglu M, Fromme H (2011) Determination of free and total bisphenol A in urine of infants. Environ Res 111(1):143–148
vom Saal FS, Cooke PS, Buchanan DL, Palanza P, Thayer KA, Nagel SC, Parmigiani S, Welshons WV (1998) A physiologically based approach to the study of bisphenol A and other estrogenic chemicals on the size of reproductive organs, daily sperm production, and behavior. Toxicol Ind Health 14:239–260
Wang HX, Zhou Y, Tang CX, Wu JG, Chen Y, Jiang QW (2012a) Association between bisphenol A exposure and body mass index in Chinese school children: a cross-sectional study. Environ Health 11:79. doi:10.1186/1476-069X-11-79
Wang B, Huang B, Jin W, Wang Y, Zhao S, Li F, Hu P, Pan X (2012b) Seasonal distribution, source investigation and vertical profile of phenolic endocrine disrupting compounds in Dianchi Lake, China. J Environ Monit 14(4):1275–1282
Wang F, Hua J, Chen M, Xia Y, Zhang Q, Zhao R, Zhou W, Zhang Z, Wang B (2012c) High urinary bisphenol A concentrations in workers and possible laboratory abnormalities. Occup Environ Med 69(9):679–684
Watanabe S, Wang RS, Miyagawa M, Kobayashi K, Suda M, Sekiguchi S, Honma T (2003) Imbalance of testosterone level in male offspring of rats perinatally exposed to bisphenol A. Ind Health 41:338–341
Welshons WV, Nagel SC, Vom Saal FS (2006) Large effects from small exposures. III. Endocrine mechanisms mediating effects of bisphenol A at levels of human exposure. Endocrinology 147:S56–S69
Wetherill YB, Petre CE, Monk KR, Puga A, Knudsen KE (2002) The xenoestrogen bisphenol A induces inappropriate androgen receptor activation and mitogenesis in prostatic adenocarcinoma cells. Mol Cancer Ther 1:515–524
Wetherill YB, Akingbemi BT, Kanno J, McLachlan JA, Nadal A, Sonnenschein C, Watson CS, Zoeller RT, Belcher SM (2007) In vitro molecular mechanisms of bisphenol A action. Reprod Toxicol 24:178–198
WHO (1991) Infertility. A tabulation of available data on prevalence of primary and secondary infertility. Geneva, WHO Programme on Maternal and Child Health and Family Planning, Division of Family Health, Geneva, p 72
Xi W, Wan HT, Zhao YG, Wong MH, Giesy JP, Wong CK (2012) Effects of perinatal exposure to bisphenol A and di(2-ethylhexyl)-phthalate on gonadal development of male mice. Environ Sci Pollut Res 19:2515–2527
Xiao GB, Wang RY, Cai YZ, He GH, Zhou ZJ (2009) Effect of bisphenol A on semen quality of exposed workers: a pilot study. (Article in Chinese). Zhonghua Lao Dong Wei Sheng Zhi Ye Bing Za Zhi 27:741–743
Yamada H, Furuta I, Kato EH, Kataoka S, Usuki Y, Kobashi G, Sata F, Kishi R, Fujimoto S (2002) Maternal serum and amniotic fluid bisphenol A concentrations in the early second trimester. Reprod Toxicol 16:735–739
Ye L, Zhao B, Hu G, Chu Y, Ge RS (2011) Inhibition of human and rat testicular steroidogenic enzyme activities by bisphenol A. Toxicol Lett 207:137–142
Zhang Z, Alomirah H, Cho HS, Li YF, Liao C, Minh TB, Mohd MA, Nakata H, Ren N, Kannan K (2011) Urinary bisphenol A concentrations and their implications for human exposure in several Asian countries. Environ Sci Technol 45:7044–7050
Zoeller RT, Bansal R, Parris C (2005) Bisphenol-A, an environmental contaminant that acts as a thyroid hormone receptor antagonist in vitro, increases serum thyroxine, and alters RC3/neurogranin expression in the developing rat brain. Endocrinology 146:607–612
Acknowledgements
This work was funded by the Federation of Indian Chambers of Commerce & Industry (FICCI), the Department of Science and Technology (DST), and Government of India, through CV Raman International Fellowship for African Researchers.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Manfo, F.P.T., Jubendradass, R., Nantia, E.A., Moundipa, P.F., Mathur, P.P. (2014). Adverse Effects of Bisphenol A on Male Reproductive Function. In: Whitacre, D. (eds) Reviews of Environmental Contamination and Toxicology Volume 228. Reviews of Environmental Contamination and Toxicology, vol 228. Springer, Cham. https://doi.org/10.1007/978-3-319-01619-1_3
Download citation
DOI: https://doi.org/10.1007/978-3-319-01619-1_3
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-01618-4
Online ISBN: 978-3-319-01619-1
eBook Packages: Earth and Environmental ScienceEarth and Environmental Science (R0)