Abstract
A first generation of Coflex implant for non-rigid stabilization of lumbar spine was presented by Samani (Study of a semi-rigid interspinous U fixation system. Spinal Surgery, Child Orthopaedics: 1707, 2000).
We started to treat patients with this Coflex device in 2004 and since then more than 600 patients have been operated in our Neurosurgical Department. We are reporting 156 patients treated between December 2004 and 2006 with complete follow-up. The clinical trials of this and other implants provide evidence that this interspinous non-rigid stabilization is useful against low-back pain due to degenerative instability and without serious complications.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Degenerative lumbar disc
- Interspinous distractor
- Interspinous implant
- Low back pain
- Lumbar spinal stenosis
- Non-rigid fixation
Introduction
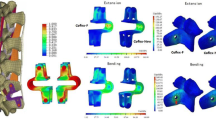
The Coflex interspinous implant is made of titanium having a U shaped form. It produces an interspinous and a discal distraction, dampening the antero-posterior forces and is compressible in extension, has some small reliefs that minimize expulsion, controls also rotation and spinal alignment.
This interspinous device is functionally dynamic: compressible in extension, allowing flexion and increase of rotational stability. Meanwhile the centre of rotation is close to the spinal canal. Coflex implant also protects the posterior elements performing stress reductions on facet joints with maintenance of foraminal height. Also it is easy to use because of the lesser invasiveness and tissue-sparing procedure.
Interspinous Coflex device stabilize intraoperative instability after decompression maneuver. Late instability may be prevented if projected. It is ideal in cases of facet arthrosis and all related decompressive procedures [1–10].
Material and Methods
From December 2004 to 2006, 156 patients with different lumbar problems were treated with a Coflex interspinous implant. These patients were controlled 6 months, 1 and 2 years after the operation.
The ethiologies of lumbar pathology were as follows:
The age of the patients in 9 cases were between 20 and 30 years old, 33 between 30 and 40, 36 between 40 and 50, 42 between 50 and 60, and 36 between 60 and 70 years old. Fifty-seven were male and 99 female.
Regarding the level, the Coflex was implanted in 26 patients at L3–L4 in 103 at L4–L5 and in 27 at L5–S1.
Degenerative disc disease (DDD) was diagnosed clinically when the patients had lumbar pain at least for 1 year and the MRI showed a decrease of disc height, loss due to hydration with image of black disk. Only in those cases we implanted the Coflex device. Degenerative spondylolisthesis was grade I, and in most cases patients were diagnosed with DDD. When there was a voluminous extrusion of the disc we also implanted a Coflex device since we only operated the fragment extruded without removing the rest of the disc, and we tried to avoid a recurrence of disc herniation. Vertebral instability is operated with Coflex when there is only one segment concerned to be clinically and radiologically confirmed. Recurrence of disc herniation is also treated with Coflex after removing the disc herniation, and lumbar canal stenosis is treated with foraminotomy, flavectomy and Coflex device.
Operative Technique
Under general anesthesia the patients were placed on a radiolucent table in decubitus prone position. After the operative level is confirmed through fluoroscopy, a middle sagittal incision of 4 cm is made over the spinous process of the level, paraspinal muscles are stripped off the laminae while preserving the facet capsules.
The interspinous ligament is sacrificed and any bony overgrowth of the spinous process that may interfere with insertion is resected. Ligamentum flavum is then also resected and microsurgical decompression is performed relieving all points of neural compression. Trials are utilized to define the appropriate implant size. Instruments are placed on trial to evaluate proper contact with the spinous process and the amount of interspinous distraction. Some bony resection of the spinous process may be needed to ensure proper contact of the implant. Distraction is considered to be appropriate if it prevents any setting of the interspinous distance after successful decompression in cases of spinal stenosis. The wings of the device may need to be opened slightly using bending pliers at the mid portion of the wing to ensure appropriate depth of insertion. The implant is introduced via impaction. If the wings are not having sufficient bony contact additional stability can be achieved by slightly crimping the wings. The incision was closed and the patients were allowed to return home the next day after surgery.
Clinical Results
In our stadistic there are different clinical groups. We are going to differentiate the results in order to ethiology.
Regarding lumbar canal stenosis (42 cases) we followed the criteria that the patient must be older than 50 years, have mild to moderate stenotic symptoms, have pain that is relieved when flexed and aggravated when extended. We have excluded patients with unremitting pain in any position, fixed motor deficit, severe symptomatic lumbar spinal canal stenosis at three or more levels and spinal instability. We used to score these patients with the Swiss Spinal Stenosis (SSS) Questionnaire [11, 12]. The mean follow-up was 24 months after surgery. The patients were 19 male and 8 female, the age of patients were between 58 and 80 years.
Patient satisfaction of SSS demonstrated that 80% of patients were satisfied with the outcome of their surgery, 40% of patients had a significant change in symptom severity and 10% showed a significant improvement in physical function.
The mean dural sac changed from 74 mm2 preoperatively to 90 mm2 postoperatively. The intervertebral foramina was increased from 60 to 80 mm2 and the interspinous distance increased from 4 to 9 mm.
We had 12 cases with voluminous disc herniation and recurrent disc herniation in six patients. Senegas [13] advises to treat cases of huge disc with removal of the extruded fragment plus interspinous spacer. The explanation for this is to avoid decrease of disc height and recurrence of disc herniation. In our 12 cases no recurrence of disc herniation happened and the disc height was similar as before the operation.
The recurrence of disc herniation was treated by removal of the fragment and insertion of the Coflex interspinous spacer. The goal was to avoid new surgery and also to avoid possible lumbar segmental instability, which, although they were a few cases, did not happen.
In the last group we could include altogether 42 cases of degenerative disc disease, nine cases of degenerative spondylolisthesis grade I, and 60 cases of single level segmental instability. They produce similar symptoms which are local lumbar pain when moving the lumbar region and decrease or disappearance of the pain when resting. Radiologically all of our nine cases of degenerative spondylolisthesis grade I had local segmental instability and degenerative disc disease.
It must be stressed that the 60 cases of single level local segmental instability had also degenerative disc disease.
The 42 cases with degenerative disc disease had radiologically a black disc principally and local lumbar pain.
In the group of 111 cases (60 lumbar local instability, 42 DDD and nine degenerative spondylolisthesis) we verified the improvement in low back pain in 80% of cases and the Oswestry functional score changed from 60 preoperatively to 16 postoperatively.
Postoperative analysis of MR images showed marked improvement in bony lesions on both sides of the disc. There were cases when the U device could not be inserted due to extensive weakness of the spinous process during the surgical procedure. In these cases, patients were unable to benefit from this technique and conventional fusion with pedicular screws was performed.
There were no late neurological complications related to the U and no cases of U penetration inside the canal or infection.
Discussion
We have treated with Coflex interspinous spacer a heterogeneous group of patients with lumbar problems, but the final results after operation have been excellent. This non-rigid stabilization has solved the problem of low back pain due to degenerative instability, and in our cases of lumbar stenosis has avoided a more aggressive operation such as laminectomy with or without fusion. The current results demonstrate that the dural sac increases with the Coflex interspinous implant, as we usually also performed foraminotomy plus flavectomy, but not laminectomy. Inufusa et al. [14] reported findings with X-Stop interspinous implant, based on the computed tomography data that showed that flexion increased the size of the central canal by 24 mm2 or 11% and extension decreased the size of the canal by 26 mm2 or 11%. Shönstron et al. [15] reported that the cross-sectorial area of the spinal canal is reduced by 40 mm2 and the mid-sagittal diameter of the canal is reduced by 2 mm when the lumbar spine moves from flexion to extension. Also the neural foramina dimensions were shown to be position dependent [16–20]. This technique is very favorable compared with laminectomy and fusion, since it is very easy and has no complications.
Regarding the other group of patients treated with the Coflex implant, they had significant resolution of low back pain. The functional improvement assessed using the Oswestry score was very clear.
Conclusion
In summary Coflex interspinous implant is a useful and easy technique in the management of some lumbar problems such as degenerative disc disease, lumbar segmental instability, grade I degenerative spondylolisthesis, mild lumbar canal stenosis and to prevent lumbar spinal instability after voluminous disc herniation or recurrent disc herniation.
References
Cho K-S (2005) Clinical outcome of interspinous-U (posterior distraction system) in the elderly lumbar spinal stenosis. 5th Annual Global Symposium on Motion Preservation Technology: Spine Arthroplasty Society.
Christie SD, Song KK, Fressler RG (2005) dynamic interspinous process technology. Spine 30 (16S): S73–S78.
Eif M, Schenke H (2005) The interspinous U – indications, experiences and results. 5th Annual Global Symposium on Motion Preservation Technology: Spine Arthroplasty Society, May: 73.
Kaech DL, Fernández C, Haninec P (2001) Preliminary experience with the interspinous U device. Rachis 13: 403–404.
Kaech DL, Fernández C, Lombardi-Weber D (2000) The Interspinous U: A new restabilization device for the lumbar spine. Spinal Restabil Proc 30: 355–362.
Kim W-K, Lee S-G, Yoo C-J, Park C-W, Park C-W (2005) Our experiences of interspinous U device in degenerative lumbar disease. 5th Annual Global Symposium on Motion Preservation Technology: Spine Arthroplasty Society, May.
Matge G (2002) Dynamic interspinous process “U” fixation. An alternative surgical treatment for degenerative lumbar instability. Scientific Session 2: 28.
Park C-K, Kim D-H, Cho K-S (2005) (Non-fusion technology) Therapeutic role of interspinous-U in the patients with degenerative lumbar spondylolisthesis. 5th Annual Global Symposium on Motion Preservation Technology: Spine Arthroplasty Society, May.
Tsai KJ, Murakami H, Lowery GL, Hutton WC (2006) A biomechanical evaluation of the stabilization effects of an interspinous device (coflex™). J Surg Orthop Adv 15(3): 167–172.
Vena P, Franzoso G, Gastaldi D, Contro R, Dallolio V (2005) A finite element model of the L4–L5 spinal motion segment: biomechanical compatibility of an interspinous device. Comput Methods Biomech Biomed Engin 8(1): 7–16.
Pratt RK, Fairbank JC, Virr A (2002) The reliability of the Shuttle Walking Test, the Swiss Spinal Stenosis Questionnaire, the Oxford Spinal Stenosis Score, and the Oswestry Disability Index in the assessment of patients with lumbar spinal stenosis. Spine 27: 84–91.
Strucki G, Daltroy L, Liang MH, et al. (1996) Measurement properties of a self-administered outcome measure in lumbar spinal stenosis. Spine 21: 796–803.
Sénégas J, Etchevers JP, Baulny D, Grenier F (1988) Widening of the lumbar vertebral canal as an alternative to laminectomy, in the treatment of lumbar stenosis. Fr J Orthop Surg 2: 93–99.
Inufusa A, An HS, Lim TH, et al. (1996) Anatomic changes of the spinal canal and intervertebral foramen associated with flexion-extension movement. Spine 21: 2412–2420.
Shönstrom N, Lindahl S, Willem J, et al. (1989) Dynamic changes in the dimensions of the lumbar spinal canal: an experimental study in vitro. J Orthop Res 7: 115–121
Lee J, Hida K, Seki T, et al. (2004) An interspinous process distractor (X Stop) for lumbar spinal stenosis in elderly patients. Preliminary experiences in 10 consecutives cases. J Spinal Disord Tech 17: 72–77.
Mayoux-Benhamou MA, Revel M, Aaron C, et al. (1989) A morphometric study of the lumbar foramen: influence of flexion-extension movements and of isolated disc collapse. Surg Radiol Anat 11: 97–102.
Nowicki BH, Yu S, Reinartz J, et al. (1990) Effect of axial loading on neural foramina and nerve roots in the lumbar spine. Radiology 176: 433–437.
Zamani AA, Moriarty R, Hsu L, et al. (1998) Functional MRI of the lumbar spine in erect position in a superconducting open configuration MR system: preliminary results. J Magn Res Imaging 8: 1329–1333.
Zucherman JF, Hsu KY, Hartjen CA, et al. (2004) A prospective randomized multi-center study for the treatment of lumbar spinal stenosis with the X STOP interspinous implant: 1-year results. Eur Spine J 13: 22–31.
Conflicts of Interest StatementWe declare that we have no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2011 Springer-Verlag/Wien
About this chapter
Cite this chapter
Villarejo, F., Carceller, F., de la Riva, A.G., Budke, M. (2011). Experience with Coflex Interspinous Implant. In: Alexandre, A., Masini, M., Menchetti, P. (eds) Advances in Minimally Invasive Surgery and Therapy for Spine and Nerves. Acta Neurochirurgica Supplementum, vol 108. Springer, Vienna. https://doi.org/10.1007/978-3-211-99370-5_25
Download citation
DOI: https://doi.org/10.1007/978-3-211-99370-5_25
Published:
Publisher Name: Springer, Vienna
Print ISBN: 978-3-211-99369-9
Online ISBN: 978-3-211-99370-5
eBook Packages: MedicineMedicine (R0)