Abstract
Beta-lactam antibiotics (BLs) are the most frequent cause of hypersensitivity reactions mediated by specific immunological mechanisms, with two main types, IgE reactions or T-cell-dependent responses. From a practical point of view, these reactions can be classified into immediate, for those appearing within 1 h after drug intake, and non-immediate, for those appearing at least 1 h after and usually within 24 h of BL administration. The clinical symptoms differ according to this classification. Urticaria and anaphylaxis are the most frequently recorded symptoms in immediate reactions and maculopapular exanthema and delayed urticaria in non-immediate reactions. Although the exact diagnostic approach differs depending on the underlying mechanism, it is based on the performance of skin testing, laboratory tests, and drug provocation tests.
T cells are a key factor in all types of hypersensitivity reactions to BLs, regulating both IgE production or acting as effector cells, with a different profile of cytokine production. A Th1 pattern is observed in both CD4+ and CD8+ peripheral T cells in non-immediate reactions, whereas a Th2 pattern is expressed in CD4+ T cells in immediate reactions.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
11.1 Introduction
Drug hypersensitivity includes reactions mediated by immunological mechanisms, the most frequent of which are those induced by specific IgE antibodies or by T-cell-dependent mechanisms (Blanca et al. 2009; Torres et al. 2003). The drugs most often involved in these immunological reactions are the beta-lactam antibiotics (BLs), which have therefore become the best studied model. Other hypersensitivity reactions are non-immunologically mediated—the most frequent of these being cross intolerance to nonsteroidal anti-inflammatory drugs. This type of reaction is not induced by BLs, and it does not therefore come within the scope of this review.
According to the time interval between the drug administration and the development of the symptoms, hypersensitivity reactions to BLs can be classified as immediate (appearing within 1 h of drug intake) or non-immediate reactions (appearing more than 1 h after drug intake) (Blanca et al. 2009). The former are mediated by specific IgE antibodies and the latter mainly by a T-cell-dependent mechanism.
Although all BLs, including those more recently introduced on the market, can induce hypersensitivity reactions, the particular BL involved depends on the patterns of prescription and consumption in the population evaluated (Blanca 1995). Benzylpenicillin (BP) was the first BL identified as responsible for allergic reactions, but it has progressively been replaced by amoxicillin (AX) (Blanca 1995). Other BLs, such as cephalosporins (Blanca 1995) and more recently clavulanic acid, also contribute to inducing hypersensitivity reactions, most of them immediate (Torres et al. 2010a). This tendency will probably change over the next few decades as patterns of consumption are modified (Blanca 1995; Torres et al. 2010a).
The prevalence and incidence of hypersensitivity to BLs is unknown, with data differing depending on the study (Rebelo-Gomes and Demoly 2005). Surveys carried out in large series of patients with cutaneous symptoms showed that 19 % of all the patients evaluated with a history of hypersensitivity reactions to BLs were finally allergic (Rebelo-Gomes and Demoly 2005), with lower values when children were evaluated (Caubet et al. 2011).
The immunological mechanisms involved in hypersensitivity reactions to BLs follow the classification of hypersensitivity reactions described by Gell and Coombs (1968), although further complexity has been added (Pichler 2003):
-
Type I or immediate reactions, mediated by drug-specific IgE antibodies.
-
Type II or cytotoxic reactions, responsible for immune hemolytic anemia and thrombocytopenia as classical representatives.
-
Type III reactions, also known as cytotoxic and immune complex reactions. These are now considered rather rare and are mediated by drug-specific, complement-fixing IgG or IgM antibodies. The classical entity seen in this group is serum sickness.
-
Type IV or delayed-type hypersensitivity reactions, where different T lymphocyte subpopulations participate as well as other immune system cells.
In this review we will analyze in detail the general characteristics of hypersensitivity reactions to BLs, focusing on the mechanisms in both IgE-mediated (Type 1) and T-cell-dependent (Type IV) reactions.
11.2 Skin as a Target of Hypersensitivity Reactions
The skin is generally the target organ in hypersensitivity reactions to BLs (Blanca et al. 2009; Torres et al. 2003). In the case of IgE-mediated reactions, symptoms can be limited to the skin, as happens in urticaria with transient pruriginous wheals occurring simultaneously at different sites of the body. This may or may not be accompanied by angioedema, consisting of inflammation of the subcutaneous tissue. IgE-mediated reactions also include anaphylaxis, which involves generalized pruritus, erythema, and angioedema: difficulty breathing; upper/lower airway obstruction; and, in more severe cases, cardiovascular collapse leading to anaphylactic shock. The reasons why some persons develop urticaria while others develop anaphylaxis are currently not well understood.
The symptoms in T-cell-mediated reactions usually appear after 24–48 h, although they can develop as soon as 1 h after drug administration leading to a full expression in a few hours (Padial et al. 2008; Blanca-Lopez et al. 2009; Warrington et al. 1993). The most frequent entities are usually mild, such as MPE and delayed urticaria (Blanca et al. 2009; Romano et al. 1995; Terrados et al. 1995; Garcia et al. 1997), but other more severe manifestations can also appear. These latter include acute generalized exanthematous pustulosis; drug hypersensitivity syndrome with eosinophilia and systemic symptoms/drug-induced hypersensitivity syndrome (DRESS/DIHS); bullous eruptions such as erythema multiform, Stevens–Johnson syndrome (SJS), and toxic epidermal necrolysis (TEN) (Doña et al. 2009); localized or generalized fixed drug eruption (FDE) and contact dermatitis (de San et al. 1999); and serum sickness-like syndrome (Clark et al. 2006). It is important to note that it is difficult to differentiate these symptoms from those induced by viral or autoimmune diseases, especially in children where viral infections are frequent (Mayorga et al. 2009).
The reasons why BLs, which are usually administered by oral or parenteral routes, induce symptoms mainly affecting the skin are not completely understood. In immediate reactions the release of histamine and other inflammatory mediators produces the typical skin effects of wheals and erythema as well as pruritus. In non-immediate reactions induced by drugs that require metabolism, there is presence in the skin of an incomplete metabolic system that does not totally detoxify drugs. This is more difficult to explain in non-immediate reactions induced by BLs where no metabolic pathway is needed.
Although classically the skin has been considered just a physical and biochemical barrier of the organism, its importance as an immunological organ has been stressed in recent years. The skin contains different cells related with the immunological response, including mast cells, macrophages, dermal dendritic cells, keratinocytes, and Langerhans cells; these have been denominated the static skin components that produce proinflammatory cytokines (Metz and Maurer 2009; Fernandez et al. 2009; Ramirez-Gonzalez et al. 2009). These cytokines induce the recruitment of cells from peripheral blood as antigen-presenting cells (APC), such as Langerhans cells, dendritic cells (DCs), monocytes and macrophages, as well as T lymphocytes expressing skin-homing receptors like the cutaneous lymphocyte antigen (CLA) and different chemokine receptors (CCR10, CCR4, CCR6,) representing the cellular basis of the immunological memory in the skin (Fernandez et al. 2009; Blanca et al. 2000; Bos and Kapsenberg 1993). These cells form the dynamic component of the cutaneous immunological system.
11.3 Beta-Lactams as Haptens
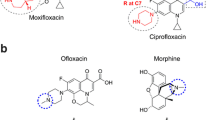
The chemical structure of BLs is formed by a four-member ring, the so-called BL ring. In penicillins it is bound to a five-member thiazolidine ring and in cephalosporins a six-member dihydrothiazine ring (Fig. 11.1). Penicillins have only one side chain at the R1 position and cephalosporins two, one at the R1 and the other at the R2 position. The chemical substitutions at the different side chains produce a wide range of BLs with different antibacterial activity and spectra that are also differentially recognized by the immunological system (Blanca et al. 1994).
BLs are haptens that cannot be recognized by the immunological system and bind spontaneously to exogenous or endogenous proteins that can later be processed and recognized by the immunological system (Burke et al. 1991; Levine and Ovary 1961). This binding with the lysine residues produces the opening of the BL ring inducing, in the case of BP, the benzylpenicilloyl (BPO) structure, the first antigenic determinant identified (Burke et al. 1991; Levine and Ovary 1961) (Fig. 11.2). This has been used for skin test diagnosis by conjugating with PLL as a carrier in what has been called the major determinant, analogous to what occurs with protein allergens, because it was the most frequent structure recognized (Adkinson et al. 1971). Human serum albumin is the candidate carrier protein and BP and benzylpenicillenic acid selectively target different residues, Lys199 and Lys525, respectively (Meng et al. 2011). In the degradation pathway of BP, other metabolites can appear, such as benzylpenicilloic or benzylpenilloic, that can also induce positive responses in the skin; these are commercialized as a minor determinants mixture (MDM) (Parker et al. 1962; Levine and Redmond 1969). Similar determinants are also generated from AX, such as amoxicilloic acid and diketopiperazine (Torres et al. 2010b).
The contribution to the antigenic determinant and the way the BL molecule is recognized by IgE antibodies depend on the chemical structure. Using murine monoclonal antibodies to BP three epitopes have been identified: the side chain, the structure formed by the binding of the carbonyl of the BL to the amino group of proteins, and the thiazolidine ring (De Haan et al. 1985). Another study generating a complete panel of antibodies of different isotypes to AX (Mayorga et al. 1995) showed that the side chain was the most important part of the molecule contributing to the epitope, with the whole structure necessary for optimal recognition. Studies carried out using human IgE antibodies showed that although differences in the side chain structure were important for IgE recognition, the whole structure including the protein carrier plus the BL was also necessary for the constitution of the complete antigenic determinant (Perez-Inestrosa et al. 2005; Sánchez-Sancho et al. 2003; Moreno et al. 1995).
These in vitro studies agree with clinical evidence that selective responses to AX occur in a considerable number of cases as well as with varying degrees of cross-reactivity between the different BLs (Moreno et al. 1995; Blanca et al. 1988, 1990). Up to 30 % of allergic patients react with AX but have good tolerance to BP, though this percentage is tending to increase over the years (Blanca et al. 1988, 1990). IgE antibodies from selective responders to AX mainly recognize the AX side chain structure, whereas those patients with cross-reactive responses to BP do not differentiate between the AX and BP side chain structures and also recognize the nuclear part of the BL structure (Moreno et al. 1995).
The situation with cephalosporins is more complex, as there are four generations of chemical structures and many more molecules with differences in the degradation pathway and generation of metabolites (Perez-Inestrosa et al. 2005). With these drugs the opening of the BL ring by nucleophilic attack of proteins and other reagents generates an intermediate cephalosporoyl (CPO) determinant which is chemically unstable, suffering multiple fragmentation reactions (Fig. 11.3). Those cephalosporins that have a good R2 leaving group undergo the process of expulsion when they conjugate to carrier proteins by the opening of the BL ring. For these cephalosporins the unstable dihydrothiazine moiety is enough to undergo further degradation processes. As a result, conjugation of cephalosporins by the BL ring leads to loss of the R2 side chain and to fractionation of the dihydrothiazine ring, and this does not therefore form part of the epitope presented in the hapten–carrier conjugate. Only the R1 side chain and a fragment of the BL ring remain bound to the carrier protein, constituting the epitope resulting from these conjugates. The presence of an R2 side chain that may act as a good leaving group is closely related to enhanced reactivity of the BL ring for nucleophilic attack (Perez-Inestrosa et al. 2005).
In depth studies of IgE, recognition to these resultant structures has involved the synthesis of well-defined structures comprising the entire acyl side chain of different cephalosporins and the aminoacidic residue included in the BL moiety of the cephalosporins studied, linked as amide functions to an aliphatic (n-butyric) chain (Sánchez-Sancho et al. 2003; Montañez et al. 2011). The results showed that the proposed skeleton epitopes involving the appropriate functionality and R1 side chain were selectively recognized by IgE from patients allergic to cephalosporins with the same or similar side chain structures.
11.4 Immunological Mechanisms Involved
Although Gell and Coombs described four main mechanisms of hypersensitivity, the two mechanisms mainly involved in BLs are specific IgE antibodies and T-cell mediation. However, T cells have an essential role in all types of hypersensitivity reactions to drugs, regulating both IgE production or effector cells, depending on the profile of cytokine production (Mosmann et al. 1986). Differences in the cytokines and transcription factors have been detected in immediate and non-immediate reactions, with a Th1 pattern with T-bet expression in both CD4+ and CD8+ T cells in non-immediate reactions, and a Th2 pattern with c-Maf expression in CD4+ T cells in immediate reactions (Cornejo-Garcia et al. 2007).
11.4.1 IgE-Mediated Reactions
In the sensitization phase BLs are taken up by the DCs, processed, and presented to T cells in a Th2 microenvironment. These will proliferate and interact by two signals (CD40–CD40L and the Th2 cytokines) with B cells, inducing the corresponding switching to produce specific IgE antibodies to the hapten–carrier conjugate which binds to high affinity Fcε-RI on the surface of mast cells and basophils. After a drug reexposure, this conjugate is recognized by specific IgE antibodies at the cell surface, and after cross-linking the activation of a calcium-dependent protein kinase cascade occurs with a subsequent release of inflammatory mediators such as histamine, prostaglandin D2, sulphidoleukotrienes, tryptase, and many cytokines. These mediators induce the symptoms of IgE-mediated reactions.
11.4.2 T-Cell-Dependent Responses
The skin is the target organ in the majority of hypersensitivity reactions to BLs. This type of reaction can be monitored during the acute episode and the resolution period in the affected skin and the peripheral blood in order to provide clues concerning the pathophysiological mechanisms involved. This process parallels the skin lesion involvement, and it is thought that after an antigenic stimulus originated in the skin, the specific immunological process is triggered, with the arrival of lymphocytes via the peripheral circulation with the interplay of different ligands and receptors, including adhesion molecules and chemokine receptors (Mayorga et al. 2009).
The involvement of T cells in allergic drug reactions has mostly been studied in non-immediate reactions, where the presence has been shown of activated T cells expressing the CLA during the acute response that normalize when the clinical reaction subsides (Picker et al. 1993; Leyva et al. 2000) as well as increased production of the IFN-γ, TNF-α, IL-2 and transcription factor, T-bet, and cytotoxic markers perforin and granzyme B (Mayorga et al. 2009).
Considering the specific subpopulations involved, although in general there is a predominant HLADR+ activation in the CD8+ cells in circulating cells in patients with severe skin symptoms with CD4+ cells in weak maculopapular eruptions (Hari et al. 2001), specific differences nevertheless exist depending on the exact entity induced. This has been confirmed by immunohistochemical studies performed in the skin, showing a mononuclear cell infiltrate composed mainly of T cells, expressing activation markers (CD25, CD69, and HLADR) and the skin-homing receptor CLA in both CD4+ and CD8+ subsets, with CD4+ cells generally predominating over CD8+ cells (Pichler 2003; Rozieres et al. 2009; Torres et al. 2004). Other cells such as neutrophils, eosinophils, macrophages, or keratinocytes can take part, as in MPE where increased numbers of eosinophils have been found in the papillary dermis (Mayorga et al. 2009).
Data from different studies show a parallelism between the results found in the skin and those in the peripheral blood, with a higher participation of CD4+ cells in the more severe reactions (Torres et al. 2006). The trafficking of T cells is regulated by differential cell-surface expression of chemokine and tissue homing receptors to the skin, varying between entities (Foster 2001). In addition to high CLA expression, other receptors are involved, with chemokines playing a fundamental role (Kunkel and Butcher 2002). Some reports have shown that most CLA+ T cells express other skin-homing chemokine receptors such as CCR4 and CCR10 (Tapia et al. 2004; Homey et al. 2002; Soler et al. 2003) and a parallel increase in chemokine CCL27 (CCR10 ligand) production in keratinocytes (Mizukawa et al. 2002). In MPE, during the acute phase of the reaction, the presence of Th1 (CXCR9 and CXCR10) and skin-homing (CCL20 and CCL27) chemokines has been identified in the skin, and their corresponding receptors (CXCR3, CCR6, and CCR10, respectively) in peripheral blood, which demonstrates the complexity of lymphocyte recruitment (Fernandez et al. 2008). With respect to the cytokines and cytotoxic marker expression in the skin, we found significant increases in TNF-α (Fernandez et al. 2008), which can be related with the expression of CCL27 by keratinocytes (Homey et al. 2002), and in IFN-γ, which is the stimulus for keratinocytes to produce CXCL9 and CXCL10 (Flier et al. 2001) (Fig. 11.4).
It is clear that immunological cellular mechanisms are responsible for the non-immediate reactions to BLs (Pichler et al. 1998). This group includes a variety of clinical entities formerly classified as Type IV reactions according to Gell and Coombs and that have now been divided into four separate subgroups (Type IV a–d) (Pichler 2003). These are elicited by different subsets of T cells, with distinctive functions leading to tissue damage. BLs are involved in all four Type IV reactions: Type IVa (Th1) reactions with macrophage activation, eosinophil-rich exanthemas (Type IVb); bullous skin diseases (Type IVc); and neutrophil-rich inflammations like AGEP (Type IVd).
Although most information about non-immediate reactions to BLs concerns the specific effector T-cell response as described above, other cells, like DCs, also participate. These are professional APCs essential for initiating T-cell responses, the activities of which depend on the maturational status and which will modulate the tolerant or the effector immune responses mediated by different subtypes of T lymphocytes (Banchereau and Steinman 1998), with immature DCs (imDCs) and semimature DCs related to tolerant immunologic responses and mature DCs (matDC) to effector responses (Lutz and Schuler 2002). Several studies have supported the role of DCs in the response to haptens (Enk et al. 1993; Arrighi et al. 2001; Enk and Katz 1992), especially in contact dermatitis induced by low-molecular-weight compounds, such as nickel (Boisleve et al. 2004) in which the hapten by itself is able to produce DC maturation (Arrighi et al. 2001; Boisleve et al. 2004). Although there is little information regarding the involvement of DCs in non-immediate hypersensitivity reactions to BL, some studies indicate that BLs interact differently with DCs in drug-allergic and nonallergic patients by the modification of the maturational level of imDCs. AX increases the expression of DC maturation and activation markers and decreases their endocytosis (Rodriguez-Pena et al. 2006). Furthermore, AX-treated imDCs from patients with delayed hypersensitivity induced an increased proliferation of allogenic T cells (Rodriguez-Pena et al. 2006). However, AX was unlikely to induce full maturation of DCs because after 72 h of treatment, compared with other agents that interact directly with receptors (LPS and TNF-a), it just induced a semi-maturation status (Lutz and Schuler 2002; Granucci et al. 2001).
The immune response involves a tight interaction between the innate and the adaptive immune systems, in which the NK–dendritic cell cross-talk has an important role (Walzer et al. 2005; Marcenaro et al. 2005). As has been shown, DCs can activate NK cells (Ferlazzo et al. 2004) and vice versa, and activated NK cells can induce DC maturation or the death of imDC through the production of either cytokines or cytotoxic factors (Vitale et al. 2004; Zhang et al. 2006), which can be a mechanism for DC homeostasis to maintain the balance between tolerant and immunologic responses (Walzer et al. 2005). In this sense, in non-immediate reactions to AX, this drug is able to activate NK-producing cytotoxic markers (perforin and granzyme B) mainly in the CD56dim subpopulation and a Th1 cytokine (IFNγ) in CD56bright cells (Chaves et al. 2010). The increase in the inflammatory NK subpopulation is mainly observed in the presence of AX-matured DCs. Moreover, AX only increases the NK cytotoxic effect in allergic patients, by an increase in annexin V binding to DC, preferentially imDC (Cahves et al. 2010).
Several studies have reported the bidirectional modulation induced by NK/DC cross-talk that includes maturation of DC and activation of NK cells (Marcenaro et al. 2005; Moretta 2002; Ferlazzo et al. 2002; Gerosa et al. 2002). Data in allergic patients show that the cytotoxic activity and cytokine release are well-differentiated processes in NK cells and depend on the status of the DC present in the culture, with imDC involved in NK cytotoxicity, whereas matDC are involved in cytokine production. All these data support the hypothesis that the cross-talk between both the innate and the adaptive immune systems, represented by NK cells and DCs, is critical in the immunopathology of adverse drug reactions, having as a consequence the amplification of the harmful effects observed in these reactions to drugs.
11.5 Clinical Approach to Hypersensitivity Reactions to BLs
The clinical symptoms and the diagnostic approach differ between patients with immediate reactions and those with non-immediate reactions. Table 11.1 lists the clinical entities of the patients with hypersensitivity reactions to BLs as well as the diagnostic methods currently used.
11.5.1 Diagnostic Workup
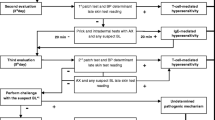
The diagnostic approach to patients with hypersensitivity reactions to BLs is based on the performance of a clinical history followed by skin testing and a drug provocation test (DPT) when indicated. In some cases laboratory tests can also help with the diagnosis.
Skin testing is recommended to be done using benzylpenicilloyl-poly-l-lysine (PPL) and MDM, consisting of BP and benzylpenilloic acid (Blanca et al. 2009) and AX (Blanca et al. 2009; Torres et al. 2003). When the BLs involved in the reaction are different to BP and AX and skin tests to PPL, MDM, and AX are negative, skin testing with the culprit BL, such as cephalosporins or clavulanic acid, should be done (Blanca et al. 2009; Torres et al. 2003, 2010a).
Depending on the type of reactions to be explored, skin tests can be done by prick, intradermal, or patch testing. In IgE-mediated reactions the sensitivity of skin testing is lower than previously thought, with the number of patients reacting to penicillin decreasing and those reacting to AX increasing (Blanca et al. 2009; Torres et al. 2003). In T-cell-dependent reactions, sensitivity of the order of 50–60 % has been reported although recent studies have shown lower figures, with 10–20 % or even lower in children where most cases tolerate the BL implicated in the reaction (Blanca et al. 2009; Torres et al. 2003; Caubet et al. 2011; Padial et al. 2008; Blanca-Lopez et al. 2009; Terrados et al. 1995). In these reactions aminopenicillins are the drugs most frequently implicated, followed to a lesser extent by cephalosporins, with most patients tolerating BP (Blanca et al. 2009; Torres et al. 2003; Caubet et al. 2011; Padial et al. 2008; Blanca-Lopez et al. 2009; Terrados et al. 1995).
In subjects with negative skin tests, a DPT can be done to confirm the diagnosis, especially in mild reactions. This approach consists of an increasing administration of the suspected drug to confirm the reaction or assess tolerance. This is contraindicated in severe IgE and T-cell reactions but is mainly done in urticarial reactions and MPE. This is particularly important in children with skin rashes attributed to BL administration, where penicillin allergy is overdiagnosed and symptoms are only reproducible in less than 7 % of the children studied by DPT (Caubet et al. 2011).
Laboratory methods widely used to detect BL-specific IgE antibody include immunoassays with different determinants such as BP, AX, and cephalosporins conjugated to carrier molecules (human serum albumin, aliphatic spacers or PLL) and then bound to solid phases (sepharose, cellulose discs) (Garcia et al. 1997; Blanca et al. 1992). A commercial assay for routine analysis is the CAP System FEIA method (Phadia, Uppsala, Sweden), which has a high surface capacity solid-phase assay using a secondary fluoro-labeled antibody. The specificity of this method ranges from 83.3 to 100 % with a sensitivity varying from 12.5 to 25 %, depending on the study (Blanca et al. 2001; Sanz et al. 2009).
Another procedure that is increasingly used is the basophil activation test (BAT). This is based on the capacity of basophils to upregulate activation markers like CD63 or CD203c after the interaction of the drug with specific IgE antibodies at their cell surface. It has a sensitivity of 48.6 % and a specificity of 93 % (Garcia et al. 1997; Blanca et al. 2001; Sanz et al. 2009). In general, in vitro tests, although less sensitive than skin testing, are complementary for the diagnosis of immediate reactions to BLs, with some cases being skin test negative but in vitro test positive (Torres et al. 2002).
The lymphocyte transformation test (LTT), although not routinely used, can be used for the evaluation of non-immediate reactions to BLs (Nyfeler and Pichler 1997; Luque et al. 2001). In our experience, 57 % of patients have a positive LTT to at least one of the penicillins tested, although when different BLs are used in the stimulation, a heterogeneous response is observed (Luque et al. 2001). Moreover, a study showed that the inclusion of autologous DCs as APC increases the sensitivity of the LTT to AX with no changes in the specificity (Rodriguez-Pena et al. 2006), properties that have been confirmed with other drugs (Lopez et al. 2009; Torres et al. 2008) (Table 11.2).
11.5.2 Cross-Reactivity
Patients with specific IgE antibodies to one BL can recognize a different BL due to similarities in their chemical structure and may therefore experience an allergic response. This has been described more often between penicillins and first-generation cephalosporins, although it can appear between any BL. Indeed, cross-reactivity has been described between penicillins and cloxacillin, ampicillin, methicillin, and AX (Blanca et al. 2009; Moreno et al. 1995; Torres et al. 1999, 2001; Co Minh et al. 2006).
The pattern of response varies between patients, and patients with a selective response to AX have a reaction after AX administration or even with AX skin testing while having good tolerance after BP administration. Similar patterns have been detected in patients allergic to cloxacillin or penicillin V (Padial et al. 2008; Blanca-Lopez et al. 2009; Romano et al. 1995; Terrados et al. 1995). Moreover, this recognition is maintained over time independently of the BL administered (Fernandez et al. 2005). This has recently been shown with clavulanic acid (Torres et al. 2010a) where patients developing an IgE response to AX–clavulanic acid administration responded to BP, AX, or clavulanic acid depending on their age. Cross-reactivity with carbapenems and monobactams in penicillin-allergic patients seems to be very low, less than 1 % with imipenem (Romano et al. 2006) and none with aztreonam (Vega et al. 1991).
Considering cephalosporins, cross-reactivity in patients who had an IgE response to penicillin was around 10 % (Romano et al. 2004). As mentioned above, the degradation pathway of cephalosporins is quite different from that of penicillins, and they are rapidly degraded and just the side chain at the R1 position remains, with this part of the molecule being critical for recognition and therefore for inducing cross-reactivity (Mosmann et al. 1986). This is the reason why first-generation cephalosporins have higher cross-reactivity with penicillins than those newly introduced into the market. Cross-reactivity is higher when the side chain is identical, increasing to 30 % in cases of selective responders to AX when cefadroxil is administered (Miranda et al. 1996). Similar results are found in patients with immediate allergic reactions to cephalosporins that may or may not cross-react with penicillin, and even tolerate other cephalosporins with different side chains. A high degree of cross-reactivity has been detected between cephalosporins with similar or identical side chains at the R1 position, as is the case of ceftriaxone, cefotaxime, or cefepime (Romano et al. 2000; Antúnez et al. 2006a).
Finally, cross-reactivity in non-immediate hypersensitivity reactions seems to be very low between penicillins and cephalosporins and even within the penicillins where cross-reactivity to other penicillins with different side chains is infrequent (Padial et al. 2008; Blanca-Lopez et al. 2009; Romano et al. 1995; Terrados et al. 1995).
11.5.3 Natural Evolution
Patients with IgE-mediated responses to BLs experience a decrease in the production of the antibodies over time that results in the negativization of skin and laboratory tests like the radioallergosorbent test (RAST) and BAT (Blanca et al. 1999; Fernández et al. 2009). This was first observed in patients with clear anaphylactic reactions but who were skin test negative when a long time had passed between the reaction and the allergological work-up (Blanca et al. 1999). The rate of negativization of the skin test depended on the BL inducing the reaction, with those cases involving IgE recognition of BP decreasing more slowly than those with selective responses to AX (Romano et al. 2004). Whether this decrease in sensitivity is accompanied by good tolerance or not is still not clearly known. Moreover, after new exposure a booster effect can appear and resensitization occurs, as has been detected in both skin tests and laboratory tests (Antúnez et al. 2006b). This is the reason why it is recommended to repeat the study in those cases with a clear reaction and a negative allergological work-up before confirming that patients are nonallergic (Blanca et al. 2009). Additionally, after a new contact a booster response occurs to the original sensitizer independently of the BL administered, such that IgE antibodies can increase to BP although the new contact was with AX, for example (Antúnez et al. 2006b).
In the case of T-cell responses, although the possibility of a decrease in the response also exists, sensitivity is maintained longer with the presence of drug-reactive T cells, even many years after the avoidance of contact with the culprit drug (Padial et al. 2008; Blanca-Lopez et al. 2009; Romano et al. 1995; Terrados et al. 1995; Beeler et al. 2006).
11.6 Concluding Remarks
T cells have an essential role in hypersensitivity reactions to BLs, in the case of immediate reactions by regulating IgE production and in the case of non-immediate reactions by acting as effector cells. The monitoring of the acute hypersensitivity response in non-immediate reactions showed that both CD4+ and CD8+ T cells are involved, with the expression of a number of cell-surface markers that enable them to migrate to the skin. Furthermore, the expression of the different markers is related with the different entities induced and their severity. Exploration of the T-cell function can be used as a diagnostic tool.
New insights into the interaction of T cells with dendritic cells and NK cells show that the development of the reaction involves an interaction between the innate and the acquired immune systems.
Abbreviations
- AGEP:
-
Acute generalized exanthematous pustulosis
- APC:
-
Antigen-presenting cells
- AX:
-
Amoxicillin
- BAT:
-
Basophil activation test
- BLs:
-
Beta-lactam antibiotics
- BP:
-
Benzylpenicillin
- BPO:
-
Benzylpenicilloyl
- CLA:
-
Cutaneous lymphocyte antigen
- CPO:
-
Cephalosporoyl
- DC:
-
Dendritic cells
- DIHS:
-
Drug-induced hypersensitivity syndrome
- DPT:
-
Drug provocation test
- DRESS:
-
Drug hypersensitivity syndrome with eosinophilia and systemic symptoms
- FDE:
-
Fixed drug eruption
- LTT:
-
Lymphocyte transformation test
- MDM:
-
Minor determinants mixture
- MPE:
-
Maculopapular exanthema
- PLL:
-
Poly-l-lysine
- PPL:
-
Benzylpenicilloyl-poly-l-lysine
- RAST:
-
Radioallergosorbent test
- SJS:
-
Stevens–Johnson syndrome
- TEN:
-
Toxic epidermal necrolysis
References
Adkinson NF Jr, Thompson WL, Maddrey WC, Lichtestein L (1971) Routine use of penicillin skin testing on an inpatient service. N Engl J Med 285:22–4
Antúnez C, Blanca-López N, Torres MJ, Mayorga C, Pérez-Inestrosa E, Montanez MI et al (2006a) Immediate allergic reactions to cephalosporins: evaluation of cross-reactivity with a panel of penicillins and cephalosporins. J Allergy Clin Immunol 117:404–10
Antúnez C, Fernández T, Blanca-Lopez N, Torres MJ, Mayorga C, Canto G et al (2006b) IgE antibodies to betalactams: relationship between the triggering hapten and the specificity of the immune response. Allergy 61:940–6
Arrighi JF, Rebsamen M, Rousset F, Kindler V, Hauser C (2001) A critical role for p38 mitogen-activated protein kinase in the maturation of human blood-derived dendritic cells induced by lipopolysaccharide, TNF-a, and contact sensitizers. J Immunol 166:3837–45
Banchereau J, Steinman RM (1998) Dendritic cells and the control of the immunity. Nature 392:245–52
Beeler A, Engler O, Gerber BO, Pichler WJ (2006) Long-lasting reactivity and high frequency of drug-specific T cells after severe systemic drug hypersensitivity reactions. J Allergy Clin Immunol 117:455–62
Blanca M (1995) Allergic reactions to penicillins. A changing world? Allergy 50:777–82
Blanca M, Perez EC, Garcia J, Miranda A, Femandez J, Vega JM, Terrados S, Avila S, Suau R (1988) Anaphylaxis to amoxicillin but good tolerance for benxylpenicillin. Allergy 43:508–10
Blanca M, Vega JM, Carmona MJ, Terrados S, Avila MJ, Miranda A, Juarea C (1990) Allergy to amoxicillin with good tolerance to other penicillins. Study of the incidence in patients allergic to & lactams. Clin Exp Allergy 20:475–81
Blanca M, Mayorga C, Perez E, Suau R, Juarez C, Vega JM et al (1992) Determination of IgE antibodies to the benzylpenicilloyl determinant. A comparison between poly-L-lysine and human serum albumin as carriers. J Immunol Methods 153:99–105
Blanca M, Vega JM, García J, Miranda A, Carmona MJ, Juárez C (1994) New aspects of allergic reactions to betalactams. Cross-reactions and unique specificities. Clin Exp Allergy 24:407–15
Blanca M, Torres MJ, García JJ, Romano A, Mayorga C, de Ramon E et al (1999) Natural evolution of skin test sensitivity in patients allergic to beta-lactam antibiotics. J Allergy Clin Immunol 103:918–24
Blanca M, Posadas S, Torres MJ, Leyva L, Mayorga C, Gonzalez L et al (2000) Expression of the skin-homing receptor in peripheral blood lymphocytes from subjects with non immediate cutaneous allergic drug reactions. Allergy 55:998–1004
Blanca M, Mayorga C, Torres MJ, Reche M, Moya MC, Rodriguez JL et al (2001) Clinical evaluation of Pharmacia CAP System RAST FEIA amoxicilloyl and benzylpenicilloyl in patients with penicillin allergy. Allergy 56:862–70
Blanca M, Romano A, Torres MJ, Férnandez J, Mayorga C, Rodriguez J, Demoly P, Bousquet PJ, Merk HF, Sanz ML, Ott H, Atanasković-Marković M (2009) Update on the evaluation of hypersensitivity reactions to betalactams. Allergy 64(2):183–93
Blanca-Lopez N, Zapatero L, Alonso E, Torres MJ, Fuentes V, Martinez-Molero MI et al (2009) Skin testing and drug provocation tests in the diagnosis of non immediate reactions to aminopenicillins in children. Allergy 64:229–33
Boisleve F, Kerdine-Romer S, Rougier-Larzat N, Pallardy M (2004) Nickel and DNCB induce CCR7 expression on human dendritic cells through different signalling pathways: role of TNF-alpha and MAPK. J Invest Dermatol 123:494–502
Bos JD, Kapsenberg ML (1993) The skin immune system: progress in cutaneous biology. Immunol Today 14:75–8
Burke AP, Saenger J, Mullick F, Virmani R (1991) Hypersensitivity myocarditis. Arch Pathol Lab Med 115:764–9
Caubet JC, Kaiser L, Lemaître B, Fellay B, Gervaix A, Eigenmann PA (2011) The role of penicillin in benign skin rashes in childhood: a prospective study based on drug rechallenge. J Allergy Clin Immunol 127(1):218–22
Chaves P, Torres MJ, Aranda A et al (2010) Natural killer-dendritic cell interaction in lymphocyte responses in hypersensitivity reactions to betalactams. Allergy 65:1600–8
Clark BM, Kotti GH, Shah AD, Conger NG (2006) Severe serum sickness reaction to oral and intramuscular penicillin. Pharmacotherapy 26:705–8
Co Minh HB, Bousquet PJ, Fontaine C, Kvedariene V, Demoly P (2006) Systemic reactions during skin tests with betalactams: a risk factor analysis. J Allergy Clin Immunol 117:466–8
Coombs PRA, Gell PGH (1968) Classification of allergic reactions responsible for clinical hypersensitivity and disease. In: Gell RRA (ed) Clinical aspects of immunology. Oxford University Press, Oxford, pp 575–96
Cornejo-Garcia JA, Fernandez TD, Torres MJ, Carballo M, Hernan I, Antunez C, Blanca M, Mayorga C (2007) Differential cytokine and transcription factor expression in patients with allergic reactions to drugs. Allergy 62:1429–38
De Haan P, Jonge AJ, Verbrugge E, Borrsma DM (1985) Three epitope-specific monoclonal antibodies against the hapten penicillin. Int Arch Allergy Appl Immunol 76:42–6
de San S, Pedro Morera B, Enriquez JQ, López JF (1999) Fixed drug eruptions due to betalactams and other chemically unrelated antibiotics. Contact Dermatitis 40:220–1
Doña I, Chaves P, Gómez E, Torres MJ, Cantó LG, Blanca M (2009) Drug rash with eosinophilia and systemic symptoms after penicillin V administration in a patient with acquired C1 inhibitor acquired deficiency. J Investig Allergol Clin Immunol 19:325–7
Enk AH, Katz SI (1992) Early molecular events in the induction phase of contact sensitivity. Proc Natl Acad Sci U S A 89:1398–402
Enk AH, Angeloni VL, Udey MC, Katz SI (1993) An essential role for Langerhans cell-derived IL-1 in the initiation of primary immune responses in skin. J Immunol 150:3698–704
Ferlazzo G, Tsang ML, Moretta L, Melioli G, Steinman RM, Munz C (2002) Human dendritic cells activate resting natural killer (NK) cells and are recognized via the NKp30 receptor by activated NK cells. J Exp Med 195:343–51
Ferlazzo G, Pack M, Thomas D et al (2004) Distinct roles of IL-12 and IL-15 in human natural killer cell activation by dendritic cells from secondary lymphoid organs. Proc Natl Acad Sci U S A 101:16606–11
Fernandez T, Torres MJ, R-Pena R, Fuentes MS, Robles S, Mayorga C, Blanca M (2005) Decrease of selective immunoglobulin E response to amoxicillin despite repeated administration of benzylpenicillin and penicillin V. Clin Exp Allergy 35(12):1645–50
Fernandez TD, Mayorga C, Torres MJ, Cornejo-Garcia JA, López S, Chaves P, Rondon C, Blanca M (2008) Cytokine and chemokine expression in the skin from patients with maculopapular exanthema to drugs. Allergy 63:712–9
Fernandez TD, Canto G, Blanca M (2009) Molecular mechanisms of maculopapular exanthema. Curr Opin Infect Dis 22:272–8
Fernández TD, Torres MJ, Blanca-López N, Rodríguez-Bada JL, Gomez E, Canto G et al (2009) Negativization rates of IgE radioimmunoassay and basophil activation test in immediate reactions to penicillins. Allergy 64:242–8
Flier J, Boorsma DM, van Beek PJ, Nieboer C, Stoof TJ, Willemze R et al (2001) Differential expression of CXCR3 targeting chemokines CXCL10, CXCL9, and CXCL11 in different types of skin inflammation. J Pathol 194:398–405
Foster JR (2001) The functions of cytokines and their uses in toxicology. Int J Exp Pathol 82:171–92
Garcia JJ, Blanca M, Moreno F, Vega JM, Mayorga C, Fernandez J et al (1997) Determination of IgE antibodies to the benzylpenicilloyl determinant: a comparison of the sensitivity and specificity of three radio allergo sorbent test methods. J Clin Lab Anal 11:251–7
Gerosa F, Baldani-Guerra B, Nisii C, Marchesini V, Carra G, Trinchieri G (2002) Reciprocal activating interaction between natural killer cells and dendritic cells. J Exp Med 195:327–33
Granucci F, Vizzardelli C, Virzi E, Rescigno M, Ricciardi-Castagnoli P (2001) Transcriptional reprogramming of dendritic cells by differentiation stimuli. Eur J Immunol 31:2539–46
Hari Y, Frutig-Schnyder K, Hurni M, Yawalkar N, Zanni MP, Schnyder B et al (2001) T cell involvement in cutaneous drug eruptions. Clin Exp Allergy 31:1398–408
Homey B, Alenius H, Muller A et al (2002) CCL27-CCR10 interactions regulate T cell mediated skin inflammation. Nat Med 8:157–65
Kunkel EJ, Butcher EC (2002) Chemokines and the tissue-specific migration of lymphocytes. Immunity 16:1–4
Levine BB, Ovary Z (1961) Studies of the mechanism of the formation of the penicillin antigen III: The N (D (Benzylpenicilloyl) group as an antigenic determinant responsible for hypersensitivity to penicillin G. J Exp Med 114:875–904
Levine BB, Redmond AP (1969) Minor haptenic determinant specific reagins of penicillin hypersensitivity in man. Int Arch Allergy Appl Immunol 35:445–55
Leyva LMJ, Torres S, Posadas M, Blanca G, Besso F, O’Valle RG et al (2000) Anticonvulsant-induced toxic epidermal necrolysis. Monitoring of the immunologic response. J Allergy Clin Immunol 105:157–65
Lopez S, Torres MJ, Rodríguez-Pena R, Blanca-Lopez N, Fernandez TD, Antunez C, Canto G, de Luque V, Mayorga C (2009) Lymphocyte proliferation response in patients with delayed hypersensitivity reactions to heparins. Br J Dermatol 160:259–65
Luque I, Leyva L, Torres MJ, Rosal M, Mayorga C, Segura JM et al (2001) In vitro T lymphocyte responses to betalactam drugs in immediate and nonimmediate allergic reactions. Allergy 56:611–8
Lutz MB, Schuler G (2002) Immature, semimature and fully mature dendritic cells: which signals induce tolerance or immunity? Trends Immunol 23:445–9
Marcenaro E, Ferranti B, Moretta A (2005) NK-DC interaction: on the usefulness of auto-aggression. Autoimmun Rev 4:520–5
Mayorga C, Obispo T, Jimeno L, Blanca M, Moscoso J, Carreira J, Juárez C (1995) Epitope mapping of betalactam antibiotics with the use of monoclonal antibodies. Toxicology 97:225–34
Mayorga C, Torres MJ, Fernandez J, Canto G, Blanca M (2009) Cutaneous symptoms in drug allergy: what have we learnt? Curr Opin Allergy Clin Immunol 9:431–6
Meng X, Jenkins RE, Berry NG, Maggs JL, Farrell J, Lane CS, Stachulski AV, French NS, Naisbitt DJ, Pirmohamed M, Park BK (2011) Direct evidence for the formation of diastereoisomeric benzylpenicilloyl haptens from benzylpenicillin and benzylpenicillenic acid in patients. J Pharmacol Exp Ther 338(3):841–9
Metz M, Maurer M (2009) Innate immunity and allergy in the skin. Curr Opin Allergy Clin Immunol 21:687–93
Miranda A, Blanca M, Vega JM, Moreno F, Carmona MJ, Garcıa JJ et al (1996) Cross-reactivity between a penicillin and a cephalosporin with the same side chain. J Allergy Clin Immunol 98:671–7
Mizukawa Y, Yamazaki Y, Teraki Y et al (2002) Direct evidence for interferon production by effector-memory-type intraepidermal T cells residing at an effector site of immunopathology in Fixed Drug Eruption. Am J Pathol 161:1337–47
Montañez MI, Mayorga C, Torres MJ, Ariza A, Blanca M, Perez-Inestrosa E (2011) Synthetic approach to gain insight into antigenic determinants of cephalosporins: in vitro studies of chemical structure-IgE molecular recognition relationships. Chem Res Toxicol 24:706–17
Moreno F, Blanca M, Mayorga C, Terrados S, Moya C, Pérez E et al (1995) Studies of the specificities of IgE antibodies found in sera from subjects with allergic reactions to penicillins. Int Arch Allergy Appl Immunol 108:74–81
Moretta A (2002) Natural killer cells and dendritic cells: rendezvous in abused tissues. Nat Rev Immunol 2:957–64
Mosmann TR, Cherwinski H, Bond MW, Giedlin MA, Coffman RL (1986) Two types of murine helper T cell clone. I. Definition according to profiles of lymphokine activities and secreted proteins. J Immunol 136:2348–57
Nyfeler B, Pichler WJ (1997) The lymphocyte transformation test for the diagnosis of drug allergy: sensitivity and specificity. Clin Exp Allergy 27:175–81
Padial A, Antunez C, Blanca-Lopez N, Fernandez TD, Cornejo-Garcia JA, Mayorga C et al (2008) Non-immediate reactions to beta-lactams: diagnostic value of skin testing and drug provocation test. Clin Exp Allergy 38:822–8
Parker CW, de Weck AL, Shapiro J, Kern M, Eisen HN (1962) The preparation and some properties of penicillenic acid derivatives relevant to penicillin hypersensitivity. J Exp Med 115:803–19
Perez-Inestrosa E, Suau R, Montañez MI, Rodriguez R, Mayorga C, Torres MJ, Blanca M (2005) Cephalosporin chemical reactivity and its immunological implications. Curr Opin Allergy Clin Immunol 5:323–30
Pichler WJ (2003) Delayed drug hypersensitivity reactions. Ann Intern Med 39:683–93
Pichler WJ, Scheyder B, Zanni M, Hari Y, von Greyerz S (1998) Role of T cells in drug allergies. Allergy 53:225–32
Picker LJ, Treer JR, Ferguson-Darnell B, Collins PA, Bergstresser PR, Terstappen LW II (1993) Differential regulation of the cutaneous lymphocyte-associated antigen, a tissue-selective homing receptor for skin-homing T cells. J Immunol 150:1122–36
Ramirez-Gonzalez MD, Herrera-Enriquez M, Villanueva-Rodriguez LG, Castell-Rodriguez AE (2009) Role of epidermal dendritic cells in drug-induced cutaneous adverse reactions. Handb Exp Pharmacol 188:137–62
Rebelo-Gomes E, Demoly P (2005) Epidemiology of hypersensitivity drug reactions. Curr Opin Allergy Clin Immunol 5:309–16
Rodriguez-Pena R, Lopez S, Mayorga C, Antunez C, Fernandez TD, Torres MJ, Blanca M (2006) Potential involvement of dendritic cells in delayed-type hypersensitivity reactions to beta-lactams. J Allergy Clin Immunol 118:949–56
Romano A, Di Fonso M, Papa G, Pietroantonio F, Federico F, Fabrizi G et al (1995) Evaluation of adverse cutaneous reactions to aminopenicillins with emphasis on those manifested by maculopapular rashes. Allergy 50:113–8
Romano A, Mayorga C, Torres MJ, Artesani MC, Suau R, Pérez E et al (2000) Immediate allergic reactions to cephalosporins: cross-reactivity and selective responses. J Allergy Clin Immunol 106:1177–83
Romano A, Gueant-Rodriguez RM, Viola M, Pettinato R, Gueant JL (2004) Cross-reactivity and tolerability of cephalosporins in patients with immediate hypersensitivity to penicillins. Ann Intern Med 141:16–22
Romano A, Viola M, Gueant-Rodriguez RM, Gaeta F, Pettinato R, Gueant JL (2006) Imipenem in patients with immediate hypersensitivity to penicillins. N Engl J Med 354:2835–7
Rozieres A, Vocanson M, Saïd BB, Nosbaum A, Nicolas JF (2009) Role of T cells in nonimmediate allergic drug reactions. Curr Opin Allergy Clin Immunol 9:305–10
Sánchez-Sancho F, Perez-Inestrosa E, Suau R, Montañez MI, Mayorga C, Torres MJ, Romano A, Blanca M (2003) Synthesis, characterization and immunochemical evaluation of cephalosporin antigenic determinants. J Mol Recognit 16(3):148–56
Sanz ML, Gamboa PM, Mayorga C (2009) Basophil activation test in the evaluation of immediate drug hypersensitivity. Curr Opin Allergy Clin Immunol 9:298–304
Soler D, Humphreys TL, Spinola SM, Campbell JJ (2003) CCR4 versus CCR10 in human cutaneous TH lymphocyte trafficking. Blood 101:1677–82
Tapia B, Padial A, Sanchez-Sabate E et al (2004) Involvement of CCL27-CCR10 interactions in drug-induced cutaneous reactions. J Allergy Clin Immunol 114:335–40
Terrados S, Blanca M, Garcia J, Vega JM, Torres MJ, Carmona MJ et al (1995) Non-immediate reactions to betalactams: prevalence and role of the different penicillins. Allergy 50:563–7
Torres MJ, Mayorga C, Pamies R, Rodriquez JL, Juarez C, Romano A, Blanca M (1999) Immunologic response to different determinants of benzylpenicillin, amoxicillin, and ampicillin. Comparison between urticaria and anaphylactic shock. Allergy 54:936–43
Torres MJ, Romano A, Mayorga C, Moya MC, Guzman AE, Reche M et al (2001) Diagnostic evaluation of a large group of patients with immediate allergy to penicillins: the role of skin testing. Allergy 56:850–6
Torres MJ, Mayorga C, Cornejo-García JA, Romano A, Blanca M (2002) IgE antibodies to penicillin in skin test negative patients. Allergy 57:965
Torres MJ, Blanca M, de Weck A, Fernandez J, Demoly P, Romano A et al (2003) Diagnosis of immediate allergic reactions to betalactam antibiotics. Allergy 58:854–63
Torres MJ, Sanchez-Sabate E, Alvarez J, Mayorga C, Fernandez J, Padial A et al (2004) Skin test evaluation in non-immediate allergic reactions to penicillins. Allergy 59:219–24
Torres MJ, Mayorga C, Fernaández TD, Cornejo-García JA, Antúnez C, Valenzuela M et al (2006) T cell assessment in allergic drug reactions during the acute phase according to the time of occurrence. Int J Immunopathol Pharmacol 19:119–30
Torres MJ, Mayorga C, Cornejo-Garcia JA, Lopez S, Chaves P, Rondon C, Fernandez T, Blanca M (2008) Monitoring non-immediate allergic reactions to iodine contrast media. Clin Exp Immunol 152(2):233–8
Torres MJ, Ariza A, Mayorga C, Doña I, Blanca-Lopez N, Rondon C, Blanca M (2010a) Clavulanic acid can be the component in amoxicillin-clavulanic acid responsible for immediate hypersensitivity reactions. J Allergy Clin Immunol 125:502–5
Torres MJ, Ariza A, Fernández J, Moreno E, Laguna JJ, Montañez MI, Ruiz-Sanchez AJ, Blanca M (2010b) Role of minor determinants of amoxicillin in the diagnosis of immediate allergic reactions to amoxicillin. Allergy 65(5):590–6
Vega JM, Blanca M, Garcıa JJ, Miranda A, Carmona MJ, Garcıa A et al (1991) Tolerance to aztreonam in patients allergic to beta-lactam antibiotics. Allergy 46:196–202
Vitale M, Della Chiesa M, Carlomagno S et al (2004) The small subset of CD56brightCD16- natural killer cells is selectively responsible for both cell proliferation and interferon-gamma production upon interaction with dendritic cells. Eur J Immunol 34:1715–22
Walzer T, Dalod M, Robbins SH et al (2005) Natural-killer cells and dendritic cells: ‘l’union fait la force’. Blood 106:2252–8
Warrington RJ, Silviu-Dan F, Magro C (1993) Accelerated cell-mediated immune reactions in penicillin allergy. J Allergy Clin Immunol 92:626–8
Zhang C, Zhang J, Tian Z (2006) The regulatory effect of natural killer cells: do ‘NK-reg cells’ exist? Cell Mol Immunol 3:241–54
Conflict of Interest
None of the authors have any conflict of interest nor have they received any money for the present study. Research is part of their daily activities. All the authors had full access to all the data and can take responsibility for the integrity of the data and the accuracy of the data analysis. The study was funded by FIS-Thematic Networks and Co-operative Research Centres (RIRAAF/RD07/0064), Junta de Andalucia (CTS 06603, PI-0545-2010), and FIS (09/01768, PS09/00966).
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Basel
About this chapter
Cite this chapter
Torres, M.J., Mayorga, C., Blanca-López, N., Blanca, M. (2014). Hypersensitivity Reactions to Beta-lactams. In: Martin, S. (eds) T Lymphocytes as Tools in Diagnostics and Immunotoxicology. Experientia Supplementum, vol 104. Springer, Basel. https://doi.org/10.1007/978-3-0348-0726-5_11
Download citation
DOI: https://doi.org/10.1007/978-3-0348-0726-5_11
Published:
Publisher Name: Springer, Basel
Print ISBN: 978-3-0348-0725-8
Online ISBN: 978-3-0348-0726-5
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)