Summary
Background: The ‘optimal’ CPP (CPPopt) concept is based on the vascular pressure reactivity index (PRx). The feasibility and effectiveness of CPPopt guided therapy in severe traumatic brain injury (TBI) patients is currently being investigated prospectively in the COGiTATE trial. At the moment there is no clear evidence that certain admission and treatment characteristics are associated with CPPopt availability (yield).
Objective: To test the relation between patients’ admission and treatment characteristics and the average CPPopt yield.
Methods: Retrospective analysis of 230 patients from the CENTER-TBI high-resolution database with intracranial pressure (ICP) measured using an intraparenchymal probe. CPPopt was calculated using the algorithm set for the COGiTATE study. CPPopt yield was defined as the percentage of CPP monitored time (%) when CPPopt is available. The variables in the statistical model included age, admission Glasgow Coma Scale (GCS), gender, pupil response, hypoxia and hypotension at the scene, Marshall computed tomography (CT) score, decompressive craniectomy, injury severity score score and 24-h therapeutic intensity level (TIL) score.
Results: The median CPPopt yield was 80.7% (interquartile range 70.9–87.4%). None of the selected variables showed a significant statistical correlation with the CPPopt yield.
Conclusion: In this retrospective multicenter study, none of the selected admission and treatment variables were related to the CPPopt yield.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Cerebral autoregulation (CA) is defined as the ability of the cerebrovascular system to maintain adequate cerebral blood flow (CBF) despite fluctuations in cerebral perfusion pressure (CPP) [1]. In patients with severe traumatic brain injury (TBI), CA is often impaired and related to worse outcomes. Over the years, the new concept of personalized therapy based on a patient’s autoregulation has been introduced. Autoregulation-based individualized management of CPP promises to be a successful strategy, and it has already been proven from retrospective analysis that it might be related to outcome [2]. One of the methods created to estimate CA continuously at the bedside is the pressure reactivity index (PRx) [3]. PRx is calculated as the moving Pearson correlation between the slow waves of intracranial pressure (ICP) and mean arterial pressure (MAP) and it has proven to be able to detect the lower limit of autoregulation in animal models [4]. Several retrospective observations have shown correlations between average PRx and worse outcome when PRx values are above 0.2–0.3 [5,6,7]. In 2002, the CPPopt concept was introduced by plotting the values of PRx against CPP over the whole monitoring period for TBI patients [8]. The PRx/CPP relationship showed a U-shaped curve, with its nadir corresponding to the CPP at which PRx is the lowest and therefore the pressure reactivity is best preserved (CPPopt). Recent developments have made it possible to assess CPPopt automatically in individual patients and display it continuously at the bedside in real time (Fig. 1) [2, 9]. CPPopt guided therapy might therefore improve autoregulation, and its feasibility, safety, and effectiveness are currently being tested in a randomized controlled trial in four European centers (CPPOpt Guided Therapy: Assessment of Target Effectiveness, COGiTATE, www.cppopt.org) [10].
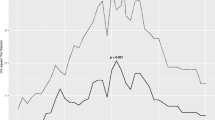
The CPP-PRx error bar over a certain period in a single patient with a fitted U-shaped curve (for more information about CPPopt and the fitting process, visit the website www.cppopt.org). In this example, the CPPopt would be around 92 mmHg
In the traditional CPPopt calculations based on a 4-h moving window, the yield was shown to be 50–60% of the total CPP monitored time [2]. With the weighted multiwindow approaches, the CPPopt availability improved to 94 ± 2.1% (mean ± SD) [9]. The importance of achieving high yield is crucial for the management of TBI patients in the light of future trials because it is important to know whether there are particular categories that are not likely to benefit from this approach, because CPPopt might not be readily available most of the time (Fig. 2a, b). This prompted our research question to investigate the relationship between demographic, clinical, and admission factors and the average CPPopt yield.
Examples of CPPopt time trends generated by continuous automated algorithm: CPPopt (thick line), CPP (thin line), PRx risk bar (with bold values indicating impaired autoregulation). PRx and CPP are selected for plotting the error bar chart. (a) An example when the (multiwindow and weighted) CPPopt time trend has several gaps limiting its use for CPP individualized management. Of note, the PRx/CPP relationship chart over this selected monitored period does not in fact form a proper U-shaped curve. (b) In this example, the CPPopt value is almost always available. Of note, the PRx/CPP plot over the selected period in this example shows a U-shaped curve
Material and Methods
This retrospective analysis was performed using ICP and ABP waveforms from the high-resolution cohort of the Collaborative European NeuroTrauma Effectiveness Research in TBI (CENTER-TBI) study. Patients in this cohort were not treated taking PRx or CPPopt information into account. The total cohort contained 271 TBI patients. After the exclusion of 41 patients who received ICP monitoring by an external ventricular drainage system with noisy or unreliable signals (due to continuous or intermittent Cerebrospinal fluid (CSF) drainage), 230 patients were left for analysis. CPPopt was calculated with ICM+ software (https://icmplus.neurosurg.cam.ac.uk) using a weighted multiwindow approach with the calculation criteria used in the COGiTATE study [10]. Several admission variables were selected: sex, age, hypoxia and hypotension at the trauma scene, Marshall computed tomography (CT) score, admission Glasgow Coma Scale (GCS), injury severity score (ISS), therapeutic intensity level (TIL) for the first 24 h, pupil reactivity, and decompressive craniectomy (DC) (Tables 1 and 2). The admission variables hypoxia, hypotension, and pupils were dichotomized into present or absent. Pupil reactivity was scored as bilateral reactive, bilateral unreactive, or unilateral unreactive. Pupils were then reclassified as a binary into normal if both pupils were reactive and pathological when one or both pupils were not reactive to light. The GCS at admission was divided into two groups, above and below 8, as an estimate of initial head trauma severity (mild/moderate if GCS > 8 and severe if GCS ≤ 8). CPPopt yield was considered as the percentage of monitored time (%) with CPPopt available given the presence of CPP. The TIL score was considered as an estimate of intracranial hypertension severity and the need for intensive treatment [11]. The aim of TIL is to produce a quantitative estimate of the interventions by assigning numerical scores to each TIL intervention and summing these. The maximum score is 38. DC was investigated as a contributing factor because there are worries that the pressure-volume characteristics necessary for reliable PRx calculations are violated [12]. In this cohort of patients, DC refers to both primary and secondary craniectomy. Statistical analysis was done with R Studio software (version 3.5.1). Nonparametric tests were used after testing the distribution of the variables through a Shapiro-Wilk test. Linear regression models were used comparing the CPPopt yield (%) to continuous variables (age, ISS, and 24-h TIL score for the first day). Mann-Whitney U and Kruskal-Wallis tests were used to compare CPPopt yield (%) for categorical and ordinal variables. A p-value <0.05 was considered for statistical significance.
Results
The patient characteristics are listed in Tables 1 and 2. The median CPPopt yield was 80.7% (interquartile range (IQR) 70.9–87.4) for the whole ICP/CPP monitoring period, suggesting the availability of CPPopt values during most of the recording period. All variables had a nonparametric distribution, showing the heterogeneity of the TBI population in this multicenter cohort. In the cohort analyzed, the median 24-h TIL score for the first day was 6 (IQR 4–9), and the median ISS score was 34 (IQR 25–43). No statistical relationship between any of the considered variables and CPPopt yield was found (Table 3).
Discussion
None of the admission demographic variables correlated with the CPPopt yield over the whole monitored period in a multicenter cohort of TBI patients. The importance of the CPPopt guided therapy concept lies in the fact that it might improve CA and, therefore, could improve the clinical outcome in TBI patients [13]. An important prerequisite of the application of the CPPopt concept at the bedside is the continuous availability of the automatically generated values of CPPopt, so that they could be used as clinical CPP targets. The first observation by Steiner et al. in 2002 about the CPPopt concept considered the total monitored time period identifying a single CPPopt value for all the patients and thus not ready for clinical use at the bedside [8]. Over the years the CPPopt algorithm and the bedside software interface have been modified using initially a 4-h moving single window [2] and later with a weighted multiwindow algorithm approach to improve the yield and stability of the CPPopt target [9, 10]. Weersink et al. investigated the relationship between the absence of a CPPopt curve and physiological and therapy variables in a two-center study [14]. Conditions related to the absence of a CPPopt curve were a high amount of sedative drugs, administration of high-dose vasopressors, using neuromuscular blockers, low variance in slow ABP waves, and status after DC. The absolute ICP values were also associated with an absence of CPPopt. CPPopt appeared more frequently in periods with higher ICP levels, perhaps owing to fact that a stronger association is present between slow fluctuations in ABP and ICP in the steep part of pressure-volume curves, thereby producing possibly more robust pressure reactivity values [3]. The multiwindow approach increased the yield considerably (reaching values above 90%) [9]. This algorithm was adapted to prospective bedside use within the COGiTATE study, introducing safety and stability measures that decreased the yield from the original multiwindow algorithm [10]. However, the retrospective analysis performed in this multicenter database showed that a high overall CPPopt yield was found (>80% of monitored time) with the algorithm suggested for prospective use by the COGiTATE study. Moreover, the yield was neither negatively influenced by admission criteria including demographic variables like sex and age or clinical variables like hypoxia and hypotension at the trauma scene, Marshall CT score, admission GCS, pupil reactivity, and DC. Furthermore, the 24-h ISS and TIL scores—as an estimate of (head) trauma severity—were not related to CPPopt yield.
Conclusions
This retrospective analysis showed no association between CPPopt yield and demographic, clinical, and management characteristics.
References
Lassen NA (1968) Autoregulation of cerebral blood flow. Circ Res 15(Suppl):201–204
Aries MJH et al (2012) Continuous determination of optimal cerebral perfusion pressure in traumatic brain injury. Crit Care Med 40(8):2456–2463
Czosnyka M et al (1997) Continuous assessment of the cerebral vasomotor reactivity in head injury. Neurosurgery 41(1):11–19
Brady KM, Lee JK, Kibler KK, Easley RB, Koehler RC, Shaffner DH (2008) Continuous measurement of autoregulation by spontaneous fluctuations in cerebral perfusion pressure: comparison of 3 methods. Stroke 39:2531–2537
Lavinio A et al (2008) Cerebrovascular reactivity and autonomic drive following traumatic brain injury. Acta Neurochir Suppl 102:3–7. https://doi.org/10.1007/978-3-211-85578-2_1
Petkus V, Krakauskait S, Preiksaitis A et al (2016) Association between the outcome of traumatic brain injury patients and cerebrovascular autoregulation, cerebral perfusion pressure, age, and injury grades. Medicina (Lithuania) 52(1):46–53
Sorrentino E, Diedler J, Kasprowicz M, Budohoski KP, Haubrich C, Smielewski P, Outtrim JG, Manktelow A, Hutchinson PJ, Pickard JD, Menon DK, Czosnyka M (2012) Critical thresholds for cerebrovascular reactivity after traumatic brain injury. Neurocrit Care 16(2):258–266
Steiner LA, Czosnyka M, Piechnik SK, et al. (2002) Continuous monitoring of cerebrovascular pressure reactivity allows determination of optimal cerebral perfusion pressure in patients with traumatic brain injury. Critical Care, 30(4):733–738
Liu X et al (2017) Monitoring of optimal cerebral perfusion pressure in traumatic brain injured patients using a multi-window weighting algorithm. J Neurotrauma 34:3081–3088
Beqiri E, Smielewski P, Robba C et al (2019) Feasibility of individualised severe traumatic brain injury management using an automated assessment of optimal cerebral perfusion pressure: the COGiTATE phase II study protocol. BMJ Open 9:e030727. https://doi.org/10.1136/bmjopen-2019-030727
Maset AL, Marmarou A, Ward JD, Choi S, Lutz HA, Brooks D, Moulton RJ, DeSalles A, Muizelaar JP, Turner H (1987) Pressure-volume index in head injury. J Neurosurg 67:832–840
Timofeev et al. (2008) “Effect of decompressive craniectomy on intracranial pressure and cerebrospinal compensation following traumatic brain injury”J Neurosurg; 108(1):66–73
Dias C et al (2015) Optimal cerebral perfusion pressure management at bedside: a single-center pilot study. NCC 23:92–102
Weersink C.S.A et al. (2015) Clinical and physiological events that contribute to the success rate of finding “Optimal” cerebral perfusion pressure in Severe Brain Trauma Patients Crit Care Med; 43(9):1952–63
Acknowledgements
The data used here were collected as part of a study supported by the European Union seventh Framework Programme (Grant 602150), Collaborative European NeuroTrauma Effectiveness Research in Traumatic Brain Injury (Center-TBI).
CENTER-TBI High-Resolution (HR ICU) Substudy Participants and Investigators : Audny Anke, Ronny Beer, BoMichael Bellander, Andras Buki, Marco Carbonara, Arturo Chieregato, Giuseppe Citerio, Endre Czeiter, Bart Depreitere, Shirin Frisvold, Raimund Helbok, Stefan Jankowski, Danile Kondziella, Lars-Owe Koskinen, Ana Kowark, David K. Menon, Geert Meyfroidt, Kirsten Moeller, David Nelson, Anna Piippo-Karjalainen, Andreea Radoi, Arminas Ragauskas, Rahul Raj, Jonathan Rhodes, Saulius Rocka, Rolf Rossaint, Juan Sahuquillo, Oliver Sakowitz, Nino Stocchetti, Nina Sundström, Riikka Takala, Tomas Tamosuitis, Olli Tenovuo, Peter Vajkoczy, Alessia Vargiolu, Rimantas Vilcinis, Stefan Wolf, Alexander Younsi.
Author information
Authors and Affiliations
Consortia
Editor information
Editors and Affiliations
Ethics declarations
Authors MC and PS have a financial interest in part of the licensing fees for ICM+ software.
MC is supported by NIHR, Biomedical Research Centre, Cambridge, UK.
Rights and permissions
Copyright information
© 2021 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Liberti, A. et al. (2021). Patient’s Clinical Presentation and CPPopt Availability: Any Association?. In: Depreitere, B., Meyfroidt, G., Güiza, F. (eds) Intracranial Pressure and Neuromonitoring XVII. Acta Neurochirurgica Supplement, vol 131. Springer, Cham. https://doi.org/10.1007/978-3-030-59436-7_34
Download citation
DOI: https://doi.org/10.1007/978-3-030-59436-7_34
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-59435-0
Online ISBN: 978-3-030-59436-7
eBook Packages: MedicineMedicine (R0)