Abstract
Recently, there has been a growing interest in the use of Parent-Child Interaction Therapy (PCIT) among preschoolers and school-age children with autism spectrum disorder (ASD). In this chapter, we describe two studies of PCIT and ASD: an open clinical trial and a randomized controlled trial. In both evaluations, we used the standard PCIT protocol to examine treatment efficacy with children 3–7 years of age and tested the traditional PCIT model without adaptations. However, tailoring the model to meet the unique needs of individual children was necessary. In a few cases, adapting the model was required to address persistent aggression in CDI and difficulty sitting for a length of 3 min during the discipline sequence. We discuss the considerable promise of PCIT as a treatment for children with ASD to reduce disruptive behavior severity and we highlight particular lessons learned through our clinical work with children with ASD and their families.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
- Randomized-controlled trial
- open-clinical trial
- Parent-Child Interaction Therapy
- Parent-Directed Interaction
- Child-Directed Interaction
- preschool
- early school age
The research summarized in this chapter was completed during two studies in which we examined the standard Parent-Child Interaction Therapy (PCIT) protocol with families of children with autism spectrum disorder (ASD) and disruptive behavior disorders. The initial study was an open clinical trial completed with our first ASD/PCIT cases with children ages 3–7 years. This served as a pilot for our subsequent randomized controlled trial (RCT) of PCIT with young children with ASD. Our RCT then randomized a total of 23 children ages 3–7 years to immediately receive 16 PCIT sessions or stay on a waiting list for 16 weeks prior to starting PCIT (Hoffman, Wong, & Handen, 2017; Scudder, Wong, & Handen, in press). This chapter will describe the clinic and clinical team, summarize initial study design and key findings, highlight lessons learned from both projects, and provide recommendations for future directions based on our work.
1 Description of Clinic and Team
The Merck Child Outpatient Clinic, Center for Autism and Developmental Disorders at the University of Pittsburgh Medical Center serves families with children ages preschool through young adulthood for diagnostic and treatment services. Families seen in the clinic come from across a wide region: western Pennsylvania as well as parts of West Virginia and Ohio. While families attend the Merck Clinic with a number of presenting concerns related to ASD and other developmental disorders, many families report problems associated with child disruptive behaviors . In 2012, the Merck Clinic first began offering PCIT to explore the utility of the intervention for children with ASD displaying early childhood disruptive and oppositional behaviors, as PCIT is well established as an evidence-based treatment for typically developing children. Since then, the clinic has continued to provide PCIT services over the last 5 years.
To establish and maintain strong clinical skills, the PCIT clinical team underwent a strict set of training and supervision guidelines. First, the team was trained and supervised by PCIT International-Certified trainers . Second, all PCIT clinicians received weekly clinical and research supervision which included case discussion, review of clinical assessments, and in-person and video-recorded supervision . The initial clinical team was composed of four doctoral-level licensed psychologists and one master’s level social worker . Following the initial cohort of clinicians, the program grew; to meet this demand, four master’s level clinicians were also trained according to the same standards as the previous cohort.
The work at the Merck Clinic is uniquely positioned as one of the first programs to provide PCIT with a clinical team who has primary expertise in neurodevelopmental disorders. For this reason, the clinic was a perfect setting to conduct one of the first RCTs of full-protocol PCIT (i.e., both Child-Direction Interaction [CDI] and Parent-Directed Interaction [PDI]) with ASD in preschool-aged children (Study 2). We describe our study designs, initial study findings, and lessons learned in the sections that follow.
2 Study 1: Open Clinical Trial
2.1 Study Design
Study 1 was an open clinical trial of PCIT with children with developmental disorders and disruptive behaviors (n = 8). Families of children enrolled in the program received services at the Merck Outpatient Clinic between 2012 and 2014. This examination of PCIT in our clinic was conducted retrospectively as program evaluation to assess outcomes of our first families in PCIT.
2.1.1 Measures
The following measures were obtained at baseline, mid-, and post-assessments.
2.1.1.1 Eyberg Child Behavior Inventory (ECBI ; Eyberg & Pincus, 1999)
A 36-item, parent-completed rating questionnaire used to assess disruptive behavior for children and adolescents ages 2–16 years. The ECBI comprises both an Intensity Scale and a Problem Scale. The Intensity Scale consists of a seven-point Likert scale to assess the frequency of behavior. Raw scores of 131 or higher are suggestive of clinically significant disruptive behavior. The tool has adequate internal consistency and test-retest reliability (Funderburk, Eyberg, Rich, & Behar, 2003; Robinson, Eyberg, & Ross, 1980) and good construct and discriminative validity (Baden & Howe, 1992; Boggs, Eyberg, & Reynolds, 1990). The ECBI was completed at baseline, mid-, and posttreatment assessments as well as at each treatment session.
2.1.1.2 Dyadic Parent-Child Interaction Coding System-IV (DPICS Eyberg, Nelson, Ginn, Bhuiyan, & Boggs, 2013)
A behavioral observation system designed to assess parent-child social interactions. Extensive normative data, reliability studies, and validity studies have shown the measure’s strong psychometric properties (Eyberg et al., 2013). During structured DPICS observations, “Do skills” (Labeled Praises, Reflections, Imitation, Behavioral Descriptions, Enjoyment; PRIDE skills) and “Don’t skills” (Negative Talk/Criticism, Commands, Questions) as well as child compliance are coded. The DPICS-IV was used to code a 5-min Child-Led Play observation, 5-min Parent-Led Play observation, and 5-min Clean-Up observation at baseline, mid-, and posttreatment. In addition, the DPICS was used for 5-min live coding of parent-child interactions prior to coaching during treatment sessions. This information was also used to provide feedback to the family and to tailor treatment. Mastery for CDI was reached for a parent who used 10 behavioral descriptions, 10 reflections, and 10 labeled praises and three or fewer “Don’t skills.”
2.1.2 Participants
As summarized in Table 24.1, participating children included 6 males (75%) and 2 females (25%), between the ages of 3 and 7 years (M = 5.13 years, SD = 1.55). The majority of children were White, Non-Hispanic (n = 5, 62.5%), while others were Asian (n = 1, 12.5%), Hispanic (n = 1, 12.5%), and multiracial (n = 1, 12.5%). All 8 children had been previously diagnosed with a pervasive developmental disorder: pervasive developmental disorder, not otherwise specified (PDD-NOS ; n = 6, 75%), Asperger’s disorder (n = 1, 12.5%), or autistic disorder (n = 1, 12.5%). In addition, many of the children were given a comorbid disruptive behavior disorder diagnosis: attention-deficit/hyperactivity disorder (ADHD; n = 5, 55.6%) and disruptive behavior disorder, not otherwise specified (DBD-NOS ; n = 2, 22.2%). Some children also had additional diagnoses such as anxiety disorder, not otherwise specified (n = 1, 11.1%) and generalized anxiety disorder (n = 1, 11.1%). Seven mothers and one father served as the primary parent participating in treatment, but both parents were trained in PCIT for half of the participating families.
2.1.3 PCIT sessions
All families were seen as part of standard clinical practice. PCIT was conducted in weekly one-hour sessions. Across sessions, as indicated in the PCIT protocol (Eyberg & Funderburk, 2011), an ECBI and a 5-min DPICS observation were administered. Treatment progression was based on parental skill mastery.
2.2 Results
2.2.1 Number of Sessions
As is shown in Table 24.1, the total number of sessions (i.e., CDI plus PDI) ranged from a low of 14 to as many as 31. Three mothers were able to meet PRIDE skills criteria in six or fewer CDI sessions; the remaining parents ranged from 10 to 16 sessions. One parent was unable to fully meet criteria before PDI sessions were initiated.
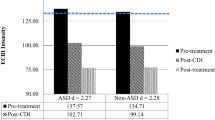
2.2.2 ECBI Scores
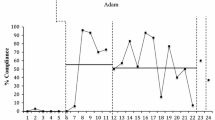
As shown in Table 24.2, the mean raw ECBI Intensity score across the eight families decreased from 139.4 to 123.8. Based upon a ≥ 20% decrease between the baseline and posttreatment ECBI Intensity score, four participants were found to be responders to PCIT. The remaining four families evidenced little change in ECBI Intensity scores. Mean raw ECBI Problem scores also decreased from 17.4 to 14.6 from baseline to posttreatment. Figure 24.1 depicts the session-by-session ECBI Intensity scores for Participant #3. The ECBI scores actually increased slightly during the course of the CDI sessions and did not start to decrease until after the PDI Coach 2 session . At that point, there was a 50-point decrease, which stayed stable for the remainder of treatment.
2.2.3 PRIDE skills
Table 24.3 summarizes the primary parent change in PRIDE skill use from baseline to mid- and posttreatment. As can be seen, all participating parents were able to significantly increase their use of “Do skills” and decrease their use of “Don’t skills” by the mid-treatment assessment. In addition, these skills were maintained (and in some cases continued to improve) at posttreatment. Only the mean rate of labeled praise dropped slightly at the end of treatment.
2.3 Discussion
This study captures outcomes of the clinicians’ very first PCIT cases. Clinically, we accepted families into the program who were reporting high levels of difficulty in managing their children’s disruptive behavior ; in two cases the reported behavioral intensity on the ECBI was slightly below the clinical cutoff (124 and 129 points). Four of eight participants were determined to be “PCIT responders .” Yet, even parents whose children’s ECBI Intensity scores failed to change appreciably were able to demonstrate consistent use of PRIDE skills across the course of treatment. Consequently, increased parental use of PRIDE skills alone may not always be associated with improved behavior for children with ASD. In fact, even in cases in which the children evidenced significant gains, it was not until a number of PDI sessions were completed before improvement on the ECBI Intensity score was noted.
A number of parents were able to demonstrate acquisition of PRIDE skills within a reasonably short number of sessions. However, the overall number of sessions required for treatment was rather long. It is possible that this was due to the fact that both parents were involved in four of the eight cases. It is also possible that children with ASD may require a greater number of sessions before gains are noted than among neurotypical children. Finally, there were many external factors that may have impacted outcome. For example, one family was undergoing a significant amount of interpersonal stress during the course of treatment, which likely affected their child’s behavior.
3 Study 2: A Randomized, Wait-List Control Trial
Our second study was a randomized, wait-list control trial of PCIT with children with ASD, ages 2.5–7 years (ClinicialTrial.gov identifier: NCT02088905). To our knowledge, this was one of the first randomized, controlled trials of PCIT among young children with ASD that included both CDI and PDI sessions . The study was conducted at two sites: The Merck Child Outpatient Clinic, Center for Autism and Developmental Disorders at the University of Pittsburgh Medical Center and Wesley Family Services. Data were collected between April 2014 and June 2016. A total of 25 families were enrolled and 23 randomized to either immediate treatment or a wait-list control.
All participants met criteria for a diagnosis of ASD, based upon the Diagnostic and Statistical Manual of Mental Disorders, fifth edition (DSM-5) criteria (American Psychiatric Association [APA], 2013) and the Autism Diagnostic Observation Schedule-2 (Lord, Rutter, DeLavore, & Risi, 2012), a semi-structured assessment of communication, social interaction, and play (or imaginative use of materials) which can be used to diagnose and differentiate individuals with and without autism or other pervasive developmental disorders . A minimum mental age of 30 months was required, based upon the Stanford-Binet V (Roid, 2003) or Mullen Scales of Early Learning (Mullen, 1995), which are each cognitive ability and intelligence tests used to diagnose developmental or intellectual deficiencies in young children. These criteria were established to ensure that children possessed enough expressive language to offer opportunities for the parents to learn “verbal reflection ” skills. In addition, receptive language skills of 30 months or greater were required, based upon performance on the Peabody Picture Vocabulary Test (PPVT , Dunn & Dunn, 2007). The receptive language criteria were established to ensure children could understand simple parental verbalizations.
Study participants continued to receive ongoing services, including preschool, individual therapies (e.g., speech, occupational therapy), and medication management throughout the course of participation. Treatment involved 8 CDI and 8 PDI sessions (including CDI and PDI Teach sessions). For all participants, study assessment visits occurred at baseline, mid-, and posttreatment; wait-list participants completed three additional assessment visits prior to beginning PCIT which occurred at the same time as the treatment group : an initial screen, 9-week visit, and 18-week visit. Outcome measures included the ECBI, the Parenting Stress Index (measuring parental stress levels; Abidin, 2012), the Social Responsiveness Scale-2 (identifying the presence or extent of social impairment in ASD; Constantino & Gruber, 2012), DPICS-IV, and the Therapy Attitude Inventory (assessing parental perspectives on therapy and their clinician; Brestan, Jacobs, Rayfield, & Eyberg, 1999). The results of that study were recently presented (Hoffman et al., 2017) and have been submitted for publication (Scudder et al., in press). Important lessons learned and future directions from the present study are described in detail below.
4 Lessons Learned and Future Directions
4.1 Differences in Parenting and Parent-Child Interactions in Families with ASD Compared to Typical Developing Children
Our experiences to date have strengthened our belief that parent-child interactions of families with children on the autism spectrum differ in some days from families of typically developing children. Furthermore, our work has reinforced the need to consider factors such as receptive language, behavioral severity, the function of challenging behaviors, and the influence of specific parent interaction strategies on child behavior in PCIT treatment of children with ASD, as they likely contribute to some of these differences. Reflecting on previously published findings, parents of young children with ASD tend to initiate play more frequently, give more suggestions and commands in the context of play, and more often respond at a level of play above the child’s abilities in comparison to parents of typically developing children (Freeman & Kasari, 2013). In our families, we found parents to frequently use verbal (e.g., suggestions and commands) and nonverbal strategies (e.g., gestures and physical touch) to engage their children in parent-child play. Often, parents in families of children with ASD are required to work harder to assess and match child play behaviors and abilities as children’s cognitive and adaptive levels are not the same as their chronological age and may vary from one type of activity to another. These differences and variations in the child’s cognitive and adaptive levels likely contribute to increases in child disruptive behavior (e.g., Simonoff et al., 2008), decreases in synchronized and cohesive parent-child behavior (e.g., Strid, Heimann, & Tjus, 2013), shorter duration of parent-child joint engagement (e.g., Freeman & Kasari, 2013; Maljaars, Boonen, Lambrechts, Van Leeuwen, & Noens, 2013), and decreases in parental consequences following child disruptive behaviors (e.g., Reese, Richman, & Belmont, 2005).
Behavior problems of children with ASD are also often perceived differently by their caregivers (e.g., Reese et al., 2005). For example, parents of children with ASD may more frequently look to antecedents of their child’s behavior or show and explain to the child how to behave, rather than implement consequences for their difficult behavior. We have found that at baseline, parents in our clinic commonly modify their communication towards their children using both strategies in line with PCIT (e.g., simplifying verbal instructions) as well as strategies that may maintain disruptive behaviors: modifying the child’s environment in ways that remove demands on the child or avoiding settings that seem to trigger problem behaviors (e.g., no longer taking the child to public places). As we have seen more families with ASD through PCIT, we take careful note of the interactional strategies used during our initial intake assessment and CDI sessions to optimize our coaching to individual family strengths.
Finally, the trajectory of which parenting skills are used across the age span may vary for parents of children with ASD compared to parents of typically developing children. For example, while mothers of younger, typically developing children report that they more often stimulate the development of their child than with older children, mothers of older children with ASD stimulate the development of their child even more compared to younger children with ASD (Maljaars et al., 2013). Consistent with this finding, parent-child interactions have been shown to more significantly influence social skills in children with ASD as they age than typically developing peers (Haven, Manangan, Sparrow, & Wilson, 2014; Meek, Robinson, & Jahromi, 2012). This may, in part, be due to increased difficulties for children and adolescents with ASD in developing other facilitative relationships. Regardless of some differences, an increase in behavior problems is directly related to increased negative, controlling parenting behaviors for families of both children with and without ASD (e.g., Maljaars et al., 2013).
4.2 Differences in Challenging Behaviors of Children with Autism
The challenging behaviors of children on the autism spectrum are substantial (Mayes et al., 2012) and although some behaviors may be accounted for solely by child noncompliance, some disruptive behaviors may in part be due to core features of ASD (e.g., restrictive and repetitive behaviors). Consistently, we found that behaviors such as stereotyped speech or movements, restricted interests or unusual sensory interests often influenced child behavior during play. For example, children in our clinic demonstrated a variety of stereotypic behaviors such as using repetitive verbalizations and rigid or repetitive play behaviors (e.g., lining up toys, sorting toys, verbalizing rigid rules during parent-child play interactions). This type of disruptive behavior is distinct from behaviors occurring due to noncompliance or defiance in typically developing children, and it has been hypothesized to, at times, serve as a self-regulatory coping strategy that helps regulate arousal levels or anxiety (Joosten, Bundy, & Einfeld, 2009). Some of the children we saw displayed frequent emotion dysregulation, which appeared to result in less persistence to continue tasks and less utilization of constructive coping strategies. Our clinical conceptualizations were that increasing alternative coping behaviors may be needed to fully address emotion dysregulation and the associated restrictive and repetitive behavior (e.g., Samson et al., 2014). We believe that additional empirical studies related to the process of developing alternative coping behaviors and emotion regulation skills in young children with ASD during evidence-based practices (e.g., PCIT) may be key to enhancing clinical practices.
4.3 Clinical Utility of PCIT with Children with Autism Spectrum Disorders: Tailoring, Adapting, and Modifying
Standard PCIT may not be effective for all children with ASD. Autism is a diagnosis which has great variability in clinical presentation and requires clinicians to have specialized knowledge and skill as well as be more expedient and flexible in repeatedly assessing and evaluating behavior during parent-child interactions. In addition, the clinician must be keenly aware of the influence of specific parenting strategies on child behavior, the function of challenging behaviors, and change in behavior over time. Anecdotally, this may be even more essential with a population with ASD and disruptive behaviors, because redirecting negative behavior patterns once they have started can be particularly demanding and time intensive. We also agree that children with ASD may more frequently have difficulty generalizing skills to other settings. Consequently, home (e.g., personal hygiene, completing household tasks, homework) and public (e.g., attending birthday parties, going to the grocery store) practice of skills is particularly important (Krasny, Williams, Provencal, & Ozonoff, 2003). In our opinion, additional clinician training is warranted to provide education and support in effectively tailoring specific aspects of the intervention to families of children with ASD.
When we first implemented PCIT for children with ASD, we utilized the standard protocol to determine the effectiveness of this strategy without adaptations . We found that for the majority of families, tailoring treatment in ways similar to that used in PCIT treatment with typically developing children was effective in the reduction of challenging behaviors. However, adaptations would likely benefit some children and families. Using Eyberg (2005) as a guide of tailoring, adapting, and modifying treatment, we are beginning to understand common ways the protocol may be tailored or adapted to families of children with ASD with specific clinical presentations (e.g., additional areas of emphasis in coaching, mastery criteria in CDI for children using few verbalizations [reflection criteria]). With this, we are also finding common presentations which may warrant further considerations of tailoring and adapting treatment, such as a child whose baseline assessment indicates significant language deficits; a large percentage of parent-child interactions characterized with persistent stimulation seeking, physicality, and aggression; frequent perseverative echolalia, repetitive play, or limited social responsivity; or any combination of these. Further examination of the adaptations to PCIT made by other authors studying PCIT and ASD (e.g., Masse, McNeil, Wagner, & Chorney, 2007; Solomon, Ono, Timmer, & Goodlin-Jones, 2008; see Chap. 16 from this handbook) as well as those made by others working in related areas, such as children with intellectual disabilities (Bagner & Eyberg, 2007) and toddlers (Dombrowski, Timmer, Blacker, & Urquiza, 2005), may also inform our approach.
4.4 Common Adjustments
4.4.1 Adjustment to the session environment and setup
Adjustments to the PCIT session environment are recommended as the first strategies to improving the effectiveness of PCIT for children with ASD. Careful consideration must be given to the types of toys used during treatment sessions, as many children with ASD have certain toys that are of extremely high interest to them. For example, iPads and electronics, cars, and superhero figurines were preferred play options for children in our studies. While including such toys may increase the child’s interest in coming to PCIT sessions, they also can make it very difficult for the parent to effectively interact with the child. In addition, a child’s preferred toy may not be conducive for a CDI session, as it may invoke increased aggressive behavior (e.g., light saber), the implementation of rules or structure (e.g., pogs or Harry Potter board game), or the increased likelihood of isolated play (e.g., iPad). Proactively addressing challenges (e.g., children arriving at the clinic with one of these favorite toys or activities) can prevent early difficulties. It may be helpful to discuss whether these items will be used in early sessions to engage children in play or left in the car or at home because they would likely require limit setting. In addition, if a child has a history of aggressive behavior, PCIT clinicians may need to have access to a number of soft, safe toy options, as aggressive behavior may persist longer and be more difficult to redirect initially than with typically developing children. Incorporating a child’s interests can also be helpful when first trying to engage children on the autism spectrum. If a child has an interest in a particular iPad game, rather than letting the child bring the iPad to session, we might coach the parent to try working the characters into play or have drawing paper with the characters on it. Since engaging children with ASD can be difficult, being creative in the ways to engage their interests may help reduce resistance stemming from removing their favorite activities entirely.
Small modifications to the physical session room and setup can also prevent unnecessary challenges. For example, children with ASD often have an interest in lights and switches. Having sat in the dark with more than one family when trying to conduct therapy, we quickly replaced our PCIT session room light switches with a key switch that cannot be operated by a child. Securing other doors, cabinets, and access to other areas in the clinic was also necessary to reduce elopement. In some cases, we found it necessary to remove all furniture in the session room. Similarly, a number of our children have pulled at the bug-in-the-ear wire or attempted to grab the device itself. We shifted to a wireless Bluetooth-like option, which is worth exploring. Prior to this, a few parents wore vests or other outer clothing to hide the device and associated wires. Lastly, the one-way mirror often intrigues both neurotypical and atypical young children; however, for several children with ASD, their interest in the mirror persisted for a longer duration (e.g., repeated saliva and mucus swirling on mirror). In these cases, we moved the dyad’s play interaction away from the mirror. Considering these slight adjustments prior to working with children with ASD may reduce the number of barriers to overcome while trying to regularly implement PCIT with this population. That being said, unique challenges will likely arise with individual clients and will require consistent patience, regular flexibility, and some ingenuity.
We commonly found that children in our studies had difficulty waiting and needed support and preparation for transitions. Minimizing the number of unnecessary or abrupt transitions for children, providing verbal transition statements , and positively attending to increases in flexibility throughout sessions can be ways to practice and model appropriate transitions with families, which will likely add ease during sessions. At times, clinicians may need to reconsider or adjust the regularly scheduled 5–10-min check-in with the parent used to obtain an update of the prior week’s activities and review of homework. During long check-ins, the child may engage in increased stereotypies or stimulation-seeking behaviors and, in turn, have difficulty transitioning into play. In particular, checking in with the parent by phone prior to the session, in-person while the child is playing in the waiting area, at the start of the session over the bug-in-the-ear, or at the end of the session may minimize preventable challenges early in treatment. As many of our participants required supervision at all times, clinicians may also need to interact with the child while providing the parent homework; in ideal circumstances , a second clinician might join to engage with the child while the primary clinician checks in with the parent and provides the homework assignment for the following week.
4.4.2 Adjustments in CDI
While “typical PCIT coaching” usually emphasizes child prosocial behaviors and parent support through the use of differential reinforcement, some additional education surrounding ASD behaviors was necessary to tailor the standardized protocol to the child and family’s specific needs (as would be done with typically developing children). For example, one child demonstrated repetitive behaviors and rigidity in allowing toys to mix. Coaching was tailored to include information about flexibility and rigidity in his play. Specifically, the use of selective attention principles during CDI to address rigid play behaviors and praising the child’s flexibility over time was a coaching focus. With his parents’ increased awareness of flexible play behavior, they were able to promote sharing, letting others have a turn or engage in the play, as well as creative child play behaviors.
In our work, we have been able to use the standard CDI mastery criteria for most parents of children with ASD. However, our most consistent challenge has been meeting mastery criteria for reflections. We have purposely limited PCIT enrollment to children with receptive/expressive language skills at or above 30 months to reduce this challenge. Regardless, we are finding that this does not necessarily mean that a given child will verbalize enough during a 5-min interaction period for parental mastery criteria for reflections (i.e., of child verbalizations) to be met. At times, we have adjusted the CDI parental mastery criteria from 10 or more reflections during a DPICS observation to reflecting >75% of the child’s verbalizations during the 5 min. This change capitalizes on opportunities for reflections rather than a direct frequency count. In cases that children have limited words, we would also encourage parents to reflect vocalizations . Therefore, in the case that a child only says five things during a given five-minute CDI observation, as long as the parent has reflected at least four verbalizations/vocalizations, he or she will have met the adapted reflection criteria.
Some of our children have displayed a range of sensory behaviors at various times during the sessions. These may include pacing, spinning, hand-waving, trailing their hands on the wall, and high-pitched screams. These types of behaviors are not typically socially mediated, so ignoring these behaviors does not always result in the child returning to the targeted activity. Occasionally, children with ASD simply engage in these behaviors for a brief period of time and will then begin interacting with their parent again. In cases that children are engaging in these behaviors for longer periods of time (e.g., child spinning a Lego over and over again saying “Woo!”, seemingly unaware of parent behavior or verbalizations), we may coach the parents to imitate or reflect and then redirect (e.g., say “Woo!” as they rotate the Lego. Then, once the child becomes engaged, we coach the parents to continue their own play by using the Lego in another way) as a way to engage attention back to the parent-child interaction in a manner that is interactive enough to disrupt the sensory self-stimulating behavior. Essentially, we coach the parent to briefly engage with the child and then expand the play. In most cases, this approach appeared to reduce the time spent in restrictive play, self-stimulation, and perseverative behavior across sessions.
Perseverative behaviors are also frequently observed among children with ASD in which a child seems to become “stuck” on a certain topic or appears overly focused on an item. For example, one participant wanted a particular toy to be in the session room. When he did not find it there, he repeatedly asked for it throughout the session (continued to focus on it, even when the parent did not respond to the questions and discussion). In our clinical discussions, we have focused on several potential parent responses. The clinician can either (a) continue to coach the parent to ignore the child’s perseverative behavior (which may limit what can be accomplished during the rest of the session), (b) provide a one-time answer and then move on (ignoring any further perseverative questioning), (c) immediately provide the child what he or she has been requesting (thereby, reinforcing initial requesting but prevent parents from reinforcing persistent and escalated requests), or (d) ignore and redirect such requests, but place the item in the session room at the next session so as to avoid continued perseveration across sessions. We have not created a specific response to this type of behavior as we have observed that the quality of the perseveration has varied across individual children. For example, one child who would unsafely climb on the table in the playroom continued to request the table at each appointment after it was removed. In another example, one child continuously requested a toy that was not in the room during one session . In this case, we chose to answer once, then ignore the repeated questions and redirect play throughout the session. When the toy was included in the session room during the next visit, the child did not engage with it.
Aggression was also an ongoing concern for some of our participants, particularly in CDI. In part, we found this to be due to deficits or delays in developmentally appropriate play, differences in functional and creative play, or ongoing parent-child interactions characterized by high levels of physical stimulation (e.g., parent and child initiated “rough housing,” such as child climbing on parent or parent frequently lifting the child). For example, a child may not easily be redirected or may even engage in increased disruptive behavior when the parent attempts to play in a manner different from the way the child was accustomed. In these cases, mild aggression could simply be ignored and redirected as outlined in the PCIT manual (Eyberg & Funderburk, 2011). However, we also observed more severe aggression and tantrums which were clearly unsafe, and in a few cases, persisted over multiple sessions.
We felt it was necessary to establish a clear discriminant of severe and persistent aggressive behavior in CDI. After attempting other recommended management strategies (see McNeil & Hembree-Kigin, 2010 for description), if aggression persisted, we moved to a “Swoop-and-Go” technique during CDI. This was introduced only in cases when the child displayed persistent aggression consisting of direct intentional harm towards the parent (e.g., repeatedly striking the parent, throwing toys with force at the parent’s head, pulling roughly at parent clothing). The parent simply told the child that he or she had to leave the room when the child hit (taking the toys as well). The parent remained out of the room (although still visible to the child) for 60 s, followed by 5 s of quiet. Once PDI sessions began with this group of aggressive children, the timeout sequence was used as a consequence for noncompliance just as it is in the standard protocol, beginning with an effective command. For these families, we taught the parent to give a quick incompatible command with any aggression, and, if needed, follow with a warning and use of timeout.
As a clinical team, we felt that this change in CDI was warranted for several reasons. In CDI, the children were primarily engaging with their parents in more physical ways than seen with same-aged typically developing kids. In many cases, a baseline assessment of behavior indicated that physical stimulation and communication were often functions of this physicality. Frequently, the parent was responding to the physical engagement (e.g., rough housing, allowing the child to climb on the parent’s back). For many reasons, these interactions were ineffective for dyads; however, they were central to how these dyads were interacting. In observing these interactions, an important focus of CDI treatment was helping the parents differentiate between positive and negative communication or stimulation behaviors. This distinction bolstered the parents’ use of more appropriate physical touch and alternative communication strategies (e.g., PRIDE skills), as well as supported effective selective attention. For these children, they were either (1) completely unresponsive to subtle redirection (e.g., the parent turning away and continuing to play) or (2) they became increasingly physical while the parent ignored and redirected the problem behaviors—extinction of the behavior did not occur in a period of time that appeared safe.
4.4.2.1 Examples
In Study 1, we had two children who fell in this category. For the first, we began with lower-level strategies (see McNeil & Hembree-Kigin, 2010), moving only to Swoop-and-Go after persistent aggression occurred (to adhere to the standard protocol). Although we eventually moved to our described Swoop-and-Go procedure, one child had already displayed in-session aggression for a number of CDI sessions; ultimately, this child demonstrated sporadic bouts of aggression throughout CDI. After this case, if child aggression persisted for more than one session, we moved to the Swoop-and-Go strategy to manage high levels of physicality and aggression. Importantly, we enforced a no tolerance rule for any physical aggression with these children. In these cases, aggression was managed much more quickly. We conceptualized this strategy as preventing the session room from becoming a discriminant stimulus for aggressive patterns of behavior. Ultimately, we found that we needed extremely clear consequences for aggressive behaviors with this group of children.
4.4.3 Adjustments in PDI
Similarly, to CDI, we found some changes were necessary when implementing PDI with children with ASD. Specifically, two primary challenges were included: child processing of a command and child ability to sit on the timeout chair for 3 min. These examples are detailed below.
One issue we continually faced while working in PDI with children on the autism spectrum was ensuring that parental commands were heard. For example, we have had a number of instances in which the child was engaging in sensory-seeking behaviors that distracted the child from processing the issued command. If it seemed that the child did not “hear” the command, we coached the parent to improve their location by moving closer, improve their positioning to be within the child’s view, and then restart the process by restating the command. Keeping to the standard PCIT protocol , we coached parents to avoid using an orienting command (e.g., calling the child’s name). However, many parents with a child with ASD have been taught (by other professionals) to engage the child by first using his/her child name prior to giving a directive. Therefore, additional rationale or focus was needed to adjust this behavior for families of children with ASD; for some, this was a particularly difficult behavior to change. We encouraged the parent to stand close to the child when commands were initially given and to point to enhance the clarity and saliency of what was said. The goal of this procedure was to increase the distance from the child at later sessions. As with typical children, parents may also be coached to remove or set aside items that may distract the child prior to giving the command. One study evaluating specific strategies to increase compliance in children with autism (Fischetti et al., 2012) highlights our clinical impression that effort reduction alone (providing less demanding instructions) may not be effective for increasing compliance. Further examination of gradually increasing task demands as well as the specific application of components of the discipline sequence may be useful when considering PDI coaching with families of children on the autism spectrum.
Some of our younger children or children with more severe ASD symptoms had difficulty fulfilling the three-minute timeout chair criteria. While the child may be able to remain seated and quiet for 1–2 min, by the second minute, some children began to engage in sensory behaviors or got out of the chair . In a few cases, it appeared that the child forgot that he or she was in timeout. As a result, we shortened the timeout period length for such children to 1–2 min plus quiet. We drew from our timed observations of how long the child was able to be seated during play in CDI and our baseline data of each child’s developmental level. In such cases, the shortened timeout period assisted in increasing compliance in a developmentally appropriate manner; this seemed to decrease frustration for both the parent and the child. Moreover, this change allowed the clinician to manage the session more effectively as well as more efficiently shape compliance across sessions.
5 Summary
Children with ASD often display high rates of disruptive behavior. We have found that utilizing PCIT to address these concerns has been successful. Across our two studies of PCIT and young children with ASD, we were able to follow the standard PCIT protocol with only slight adjustments. Our research suggests that parents of children with ASD can rapidly develop and consistently use PRIDE skills. Importantly, this does not necessarily mean that the clinician will observe a corresponding change in the rate of child’s disruptive behaviors; in fact, there may be a lag between parent acquisition of skills and decreases on ECBI scores. At times, some adaptations to the PCIT protocol will need to be considered when working with the ASD population. Specifically, there may be higher rates of aggression persisting across early sessions, as well as disruptive behaviors that relate to core features of ASD (e.g., stereotyped or repetitive motor movement, inflexible adherence to routines or ritualized behavior, restricted interests that interfere with parent-child interactions). Such behaviors may lower rates of child social reciprocity and verbalizations during parent-child interactions and lead to difficulty for some children in complying with parental instructions or sitting for the 3-min timeout required in the PDI sequence. In this chapter, we have provided some options for addressing such concerns and conclude that PCIT can be an appropriate treatment option for families of young children with ASD.
References
Abidin, R. (2012). Parenting stress index manual (4th ed.). Torrance, CA: Western Psychological Services.
American Psychiatric Association [APA]. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Arlington, VA: American Psychiatric Publishing.
Baden, A. D., & Howe, G. W. (1992). Mothers’ attributions and expectancies regarding their conduct disordered children. Journal of Abnormal Child Psychology, 20, 467–485.
Bagner, D., & Eyberg, S. M. (2007). Parent-child interaction therapy for disruptive behavior in children with mental retardation: A randomized controlled trial. Journal of Clinical Child & Adolescent Psychology, 36(3), 418–429.
Boggs, S. R., Eyberg, S. M., & Reynolds, L. (1990). Concurrent validity of the Eyberg child behavior inventory. Journal of Clinical Child Psychology, 19, 75–78.
Brestan, E., Jacobs, J., Rayfield, A., & Eyberg, S. M. (1999). A consumer satisfaction measure for parent-child treatments and its relationship to measures of child behavior change. Behavior Therapy, 30, 17–30.
Constantino, J. N., & Gruber, C. P. (2012). The social responsiveness scale-2 (SRS-2). Los Angeles, CA: Western Psychological Services.
Dombrowski, S. C., Timmer, S. G., Blacker, D. B., & Urquiza, A. J. (2005). A positive behavioural intervention for toddlers: Parent-child attunement therapy. Child Abuse Review, 14, 132–151.
Dunn, L. M., & Dunn, D. M. (2007). Peabody picture vocabulary test-IV (PPVT-IV). Circle Pines, MN: American Guidance Service.
Eyberg, S. M. (2005). Tailoring and adapting parent-child interaction therapy for new populations. Education and Treatment of Children, 28, 197–201.
Eyberg, S. M., & Funderburk, B. (2011). Parent-child interaction therapy protocol. Gainesville, FL: PCIT International Publishing. Retrieved from pcit.org
Eyberg, S. M., Nelson, M. M., Ginn, N. C., Bhuiyan, N., & Boggs, S. R. (2013). Dyadic Parent-Child Interaction Coding System (DPICS): Comprehensive manual for research and training (4th ed.). PCIT International: Gainesville, FL.
Eyberg, S. M., & Pincus, D. (1999). Eyberg child behavior inventory and Sutter-Eyberg student behavior inventory: Professional manual. Odessa, FL: Psychological Assessment Resources.
Fischetti, A. T., Wilder, D. A., Myers, K., Leon-Enriquez, Y., Sinn, S., & Rodriguez, R. (2012). An evaluation of evidence-based interventions to increase compliance among children with autism. Journal of Applied Behavior Analysis, 45, 859–863.
Freeman, S., & Kasari, C. (2013). Parent-child interactions in autism: Characteristics of play. Autism, 17, 147–161.
Funderburk, B. W., Eyberg, S. M., Rich, B., & Behar, L. (2003). Further psychometric evaluation of the Eyberg and Behar rating scales for parents and teachers of preschoolers. Early Education and Development, 14, 67–81.
Haven, E. L., Manangan, C. N., Sparrow, J. K., & Wilson, B. J. (2014). The relation of parent-child interaction qualities to social skills in children with and without autism spectrum disorders. Autism, 18, 292–300.
Hoffman, M., Wong, C., & Handen, B.L. (2017, September). Parent Child Interaction Therapy in children with autism spectrum disorder. Presented at the annual PCIT International Convention, Traverse City, MI.
Joosten, B.L., Bundy, A.C., & Einfeld, B.S. (2009). Journal of Autisn and Developmental Disorder, https//doi-org/10.1007/510803-008-0454-7.
Krasny, L., Williams, B. J., Provencal, S., & Ozonoff, S. (2003). Social skills interventions for the autism spectrum: Essential ingredients and a model curriculum. Child and Adolescent Psychiatric Clinics in North America, 12(1), 107–122.
Lord, C., Rutter, M., DeLavore, P. C., & Risi, S. (2012). Autism diagnostic observation Schedule-2. Los Angeles: Western Psychological Services.
Maljaars, J., Boonen, H., Lambrechts, G., Van Leeuwen, K., & Noens, I. (2013). Maternal parenting behavior and child behavior problems in families of children and adolescents with autism spectrum disorder. Journal of Autism and Developmental Disorders, 44, 501–512.
Masse, J., McNeil, C. B., Wagner, D., & Chorney, D. (2007). Parent-child interaction therapy and high functioning autism: A conceptual overview. Journal of Early and Intensive Behavior Intervention, 4(4), 714–735.
Mayes, S. D., Calhoun, S. L., Aggarwal, R., Baker, C., Mathapati, S., Anderson, R., & Petersen, C. (2012). Explosive, oppositional, and aggressive behavior in children with autism compared to other clinical disorders and typical children. Research in Autism Spectrum Disorders, 6, 1–10.
McNeil, C. B., & Hembree-Kigin, T. L. (2010). Parent-child interaction therapy (2nd ed.). New York: Springer.
Meek, S. E., Robinson, L. T., & Jahromi, L. B. (2012). Parent-child predictors of social competence with peers in children with and without autism. Research in Autism Spectrum Disorders, 6, 815–823.
Mullen, E. M. (1995). Mullen scales of early learning. Circle Pines, MN: American Guidance Service.
Reese, R. M., Richman, D. M., & Belmont, J. M. (2005). Functional characteristics of disruptive behavior in developmentally disabled children with and without autism. Journal of Autism & Developmental Disorders, 35(4), 419–428.
Robinson, E. A., Eyberg, S. M., & Ross, A. W. (1980). The standardization of an inventory of child conduct problem behaviors. Journal of Clinical Child Psychology, 9, 22–28.
Roid, G. (2003). Stanford-Binet intelligence scales (5th ed.). Rolling Meadows, IL: Riverside Publishing.
Samson, A. C., Phillips, J. M., Parker, K. J., Shah, S., Gross, J. J., & Hardan, A. Y. (2014). Emotion dysregulation and the core features of autism spectrum disorder. Journal of Autism and Developmental Disorders, 44, 1766–1772.
Scudder A.T., Wong, C. B., & Handen, B. L. (in press).
Simonoff, E., Pickles, A., Charman, T., Chandler, S., Loucas, T., & Baird, G. (2008). Psychiatric disorders in children with autism spectrum disorders: Prevalence, comorbidity, and associated factors in a population-derived sample. Journal of American Academy of Adolescent Psychiatry, 47(8), 921–929.
Solomon, M., Ono, M., Timmer, S. G., & Goodlin-Jones, B. (2008). The effectiveness of parent–child interaction therapy for families of children on the autism spectrum. Journal of Autism & Developmental Disorders, 38(1767–1776), 1767.
Strid, K., Heimann, M., & Tjus, T. (2013). Pretend play, deferred imitation and parent-child interaction in speaking and non-speaking children with autism. Scandinavian Journal of Psychology, 54, 26–32.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2018 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Scudder, A.T., Wong, C.B., Mendoza-Burcham, M., Handen, B. (2018). Summary of Lessons Learned from Two Studies: An Open Clinical Trial and a Randomized Controlled Trial of PCIT and Young Children with Autism Spectrum Disorders. In: McNeil, C., Quetsch, L., Anderson, C. (eds) Handbook of Parent-Child Interaction Therapy for Children on the Autism Spectrum. Springer, Cham. https://doi.org/10.1007/978-3-030-03213-5_24
Download citation
DOI: https://doi.org/10.1007/978-3-030-03213-5_24
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-03212-8
Online ISBN: 978-3-030-03213-5
eBook Packages: Behavioral Science and PsychologyBehavioral Science and Psychology (R0)