Abstract
Obesity causes significant changes in lung function, many of which are secondary to the reduction in operating lung volume caused by a stiffening of the respiratory system. In addition, reductions in the volume of the intrathoracic cavity, due to the presence of adipose tissue and changes in other structures, may also contribute to an overall reduction in lung volume. Thus, the primary effects of obesity on lung function arise from the mechanical effects of adipose tissue on the respiratory system. However, some studies have reported changes in airway function associated with obesity that appear to be independent of lung volumes, though the causes of these abnormalities are unknown. It is unclear whether the mechanical effects of obesity on lung function can increase the risk of respiratory symptoms in otherwise healthy individuals. However, in respiratory disease, a reduction in operating lung volume may increase symptoms during bronchoconstriction in asthma and protect against symptoms during exercise in COPD.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Adiposity
- Respiratory compliance
- Lung volumes
- Expiratory flow limitation
- Ventilation distribution
- Gas exchange
- Breathlessness
Objectives
-
Evaluate the effects adiposity on respiratory mechanics
-
Assess the mechanism by which obesity leads to impairment in lung function
-
Evaluate how obesity may impact clinical presentation and physiology of obstructive and restrictive lung diseases
-
Examine the impact of obesity on pulmonary function testing interpretation
Introduction
The accumulation of adipose tissue, leading to the development of obesity, has a profound effect on human physiology, including significant effects on respiratory function due to the mechanical effects of excess adipose tissue on the balance of forces that normally act on the lung. In addition, adipose tissue produces hormones and other mediators, collectively termed adipokines, which are associated with low-grade systemic inflammation that can act indirectly on the respiratory system. However, at present it is unclear whether this causes any measurable impairment in respiratory function. The changes in lung function associated with obesity can lead to respiratory symptoms in otherwise healthy people, which are accentuated in those with respiratory disease, as a result of interaction between disease pathophysiology and the direct and indirect effects of obesity. The outcomes of this interaction are complex and differ according to the disease and the outcome of interest. The major effects of obesity on lung function are summarized in Fig. 1.1 and suggest that many of the changes in lung function result from changes in respiratory system mechanics and subsequent reduction in operating lung volume, whereas others may be associated with reduced thoracic volume, or may be due to other non-volume-related factors. In this chapter, the effects of obesity on lung function and the relationships summarized in Fig. 1.1 will be reviewed along with the effects of these impairments on respiratory symptoms.
The effects of obesity on lung function, illustrating likely mechanisms. Question marks indicate mechanisms for which further research evidence is needed. See text for more detailed discussion. TLC total lung capacity, FRC functional residual capacity, Rrs respiratory system resistance, EFL expiratory flow limitation
Adipose Tissue and Respiratory Mechanics
Obesity is defined as a body mass index >30 kg/m2. However, body mass index is a non-specific measure of body mass that includes both fat and lean mass, without any account of differences in fat distribution. Central obesity is associated with increased adipose tissue in the anterior chest and abdominal walls and visceral organs, whereas peripheral obesity reflects adiposity located peripherally on limbs, or in subcutaneous tissue. The effect of obesity on respiratory function is likely to be determined by the distribution of fat mass. Abdominal and thoracic fat are likely to have direct effects on the downwards movement of the diaphragm and on chest wall properties, while subcutaneous fat on the hips and limbs is unlikely to have any direct mechanical effect on the lungs. In addition, visceral fat is more metabolically active than subcutaneous fat and may therefore make a greater contribution to low-grade systemic inflammation in obesity. Because central obesity is more common in men than in women, the effect of obesity on respiratory function is also influenced by gender. Adipose tissue is also found inside the thoracic cavity, predominantly as pericardial fat, which, when combined with obesity-associated increase in the volume of the heart and major blood vessels, can reduce the volume of the thoracic cavity [1].
Intra-abdominal and Intrathoracic Pressures
Obesity is associated with chronic increases in intra-abdominal pressure that may affect the pleural space by altering pressure across the diaphragm. Intra-abdominal pressure is increased in obese subjects compared to non-obese [2, 3] and is greater in men than women [3], likely due to the greater prevalence of central obesity in men. Indeed, intra-abdominal pressure correlates with markers of central obesity, such as the sagittal abdominal diameter [2, 3]. Although pleural pressures are also increased in obese subjects compared to non-obese and may exceed atmospheric pressure at FRC in some patients [2], there were no gender related differences observed. In addition, in contrast to intra-abdominal pressure, studies in supine anaesthetized subjects [2] have shown that abdominal obesity, measured by waist circumferences and by sagittal abdominal diameter, was not correlated with pleural pressures. Since the relationship between abdominal pressure and pleural pressure is mediated by the diaphragm, the lack of correlation between the two may be due to compensatory increase in passive tension in the diaphragm in response to increased intra-abdominal pressure in the obese. Alternatively, factors other than increased abdominal pressures, such as changes in the properties of the chest wall, may also contribute to the altered respiratory system mechanics associated with obesity. Imaging studies of abdominal and thoracic fat have shown that both regions make a significant contribution to impairments of lung function in the obese [4].
Respiratory System Compliance
Obesity has consistently been associated with a reduction in the compliance of the total respiratory system [2, 5], likely due to reduction in the compliance of the chest wall and lungs. However, despite numerous studies of the compliance of the chest wall and lungs in obese subjects, the mechanisms that lead to a stiffening of the respiratory system in the obese remain poorly understood.
Measurement of chest wall compliance is challenging since the respiratory muscles must be relaxed and inactive to allow for accurate measurement. Studies of conscious, spontaneously breathing subjects, in which changes in lung volumes were induced using externally applied changes in pressures in a plethysmograph, suggest that there is a reduction in chest wall compliance in obesity [5, 6]. However, since respiratory muscle relaxation was assessed using EMG measurements, this may not adequately reflect muscle relaxation across the whole of the chest wall. In contrast, normal chest wall compliance has been reported in studies of supine anaesthetized, paralysed subjects with mild [7] or severe [2, 8] obesity, as well as in studies of upright conscious subjects [9]. Alteration in chest wall mechanics from being in the supine position [10] may account for some of the differences in findings between studies. However, a definitive understanding of the effect of obesity on chest wall mechanics remains elusive.
Although some studies have reported that lung compliance, measured by full P-V curves to TLC, is normal in some obese subjects [11], there is more consistent evidence that lung compliance is decreased in obese individuals [6–8, 12], and lung compliance appears to be exponentially related to BMI [7]. The mechanism for decreased lung compliance in obesity remains unclear; however, increased pulmonary blood volume [13], closure of dependent airways resulting in small areas of atelectasis [8], and increased alveolar surface tension due to a reduction in functional residual capacity (FRC) have been implicated as potential contributors to increased stiffness of the lung tissue.
An alternative hypothesis for altered respiratory mechanics in the obese has been proposed by Behazin et al. [2], who suggest that the apparent stiffening of the chest wall may simply reflect the mass loading of the chest wall due to an increased volume of intra-abdominal and mediastinal fat [1]. This hypothesis is consistent with findings from an experimental study by Sharp et al. [14], which showed that mass loading of the thorax in normal weight conscious or anaesthetized/paralysed subjects produced a parallel rightward shift of the chest wall pressure-volume curve without any effect on compliance. Furthermore, Behazin et al. [2] suggest that high pleural pressures, which are often above atmospheric pressure at FRC, would lead to closure of small airways. As a result, there would be an apparent reduction in lung compliance at FRC since the pressure-volume relationship would reflect both lung stiffness and the opening pressures of small airways. Thus, obesity could be associated with apparent changes in chest wall and lung compliance without actually causing any changes in the stiffness of either the chest wall or lung tissue. Figure 1.2 shows compliance curves for the chest wall (CCW), lung (CL) and respiratory system (CRS) in normal weight and obese individuals. In the obese, although the shape of the CCW curve is normal, it is shifted to the right, consistent with the effect of an inspiratory threshold load. The CL curve has an inflection point reflecting the increased pressure required to open airways that are closed just below FRC. As a result, the CRS curve, which is the summation of the CCW and CL curves, is flattened, indicating reduced compliance of the respiratory system in the obese. The volume at which the CRS curve crosses zero on the pressure axis (i.e. where there is a balance between inflationary and deflationary pressures) is FRC and occurs at a lower volume in the obese.
Consequences of Altered Respiratory Mechanics in Obesity
Alterations in respiratory mechanics in the obese, leading to an overall stiffening of the respiratory system, lead directly to changes in breathing pattern and resting lung volumes (Fig. 1.1).
Breathing Pattern
Increased stiffness of the respiratory system is likely to induce a rapid shallow pattern of tidal breathing, which is a typical response to an elastic load [15]. Indeed, previous studies have shown that tidal volumes are often reduced in severe obesity, and breathing follows a rapid, shallow pattern [16]. This alteration to breathing pattern is most apparent during exercise, when obese subjects preferentially increase their breathing frequency more, and tidal volumes less, than non-obese subjects [17, 18]. During bronchoconstriction, there is a greater decrease in tidal volumes in overweight or obese subjects than in normal weight subjects [19]. However, in mild-moderate obesity, tidal volumes at rest are often in the normal range [18, 20–22], and the frequency and magnitude of regular sighs and deep inspirations appear similar to that in normal weight subjects [20, 22]. Thus, increased respiratory system stiffness has a minor effect on breathing pattern and is only seen in severe obesity or when the system is under stress, such as during exercise or bronchoconstriction.
Resting Lung Volume
Aside from its effect on breathing pattern, increased respiratory system stiffness also has a major effect on resting lung volume, causing a reduction lung volume at relaxation, when the recoil pressures of the lung and chest wall are equal and opposite (Fig. 1.2). The relaxation volume of the lung usually equates to the functional residual capacity (FRC), which is very commonly reduced in obesity [7, 23]. FRC is exponentially related to BMI [7, 23], with reduction in FRC being detected even in overweight individuals [23]. This is illustrated in Fig. 1.3, which shows the relationship between BMI and FRC in a study of young adults, aged 28–30 years [24]. The reduction in FRC is also manifested by an increase in inspiratory capacity (IC). With increasing severity of obesity, the reduction in FRC may become so marked that the FRC approaches residual volume (RV), leaving the individual with a negligible expiratory reserve volume (ERV) [23]. In fact, in many studies, the reduction in ERV is one of the earliest and most marked changes in lung function that occurs with increasing weight [25]. In contrast, the effects of obesity on the upper and lower limits of lung volumes, total lung capacity (TLC) and RV are modest. Increasing body weight is associated with only small decrease in TLC [23, 26, 27], and RV is usually well preserved [16, 26, 28–30]. As a result, the RV/TLC ratio remains normal or slightly increased in obese individuals [23, 29].
The relationship between BMI and FRC, shown in Fig. 1.3, is steeper in men than in women. This difference in slope is likely to result from differences in the prevalence of central obesity between men and women. Central obesity, associated with greater fat deposition on the trunk and abdomen, is likely to have a greater effect on respiratory system compliance than peripheral fat distribution. Reductions in lung volumes are associated with both abdominal fat, measured by waist circumference [31], waist to hip ratio [32] or abdominal height [33], and thoracic or upper body fat, measured by sub-scapular skinfold thickness [34] or biceps skinfold thickness [26]. Several studies have used dual-energy X-ray absorptiometry (DXA) to quantify fat and lean mass in different regions of the body and relate these findings to lung function [4, 35]. Sutherland et al. [4] used a wide range of body fat variables to determine the effect of fat distribution on lung volumes in healthy adults. Lung volumes were only loosely associated with BMI; however, both DXA and non-DXA-derived measures of upper body fat showed highly significant negative correlations with FRC and ERV in both men and women. Both abdominal obesity and thoracic fat mass were similarly correlated with lung volumes, making it difficult to differentiate between the effects of abdominal and thoracic fat. Similarly, improvements in lung volumes such as FVC, FRC and ERV, following moderate weight loss, were related to the cumulative loss of fat from areas impinging on the chest wall, such as chest, subcutaneous abdominal or visceral fat, rather than from any specific region [36].
Consequences of Reduced FRC
In the causal pathway shown in Fig. 1.1, low operating lung volume due to reduced respiratory system compliance leads to effects on airway resistance, expiratory flow limitation, ventilation distribution and gas exchange.
Airway Resistance and Reactance
Since airway calibre is related to lung volume, reduction in FRC in the obese has significant effects on the mechanical properties of the airway and on expiratory flows during tidal breathing. Respiratory system resistance and airway resistance are increased in the obese [37], indicating that airway calibre is reduced throughout the breathing cycle. However, measurement of specific airway resistance in obese subjects, which is adjusted for lung volume, is in the normal range [30, 37–39], suggesting that the reduction in airway calibre at FRC in the obese is attributable to the reduction in lung volumes rather than to airway obstruction. Respiratory system reactance is also abnormal in the obese [21], but the mechanism for this is not clear.
Similarly, expiratory flows also decrease with increasing weight [29, 38] in proportion to changes in lung volumes [30]. As such, decrease in expiratory flows in an obese individual is unlikely to indicate bronchial obstruction unless the flow measurements have been normalized for the reduction in vital capacity. In a large sample of obese and normal weight non-smokers, reductions in expiratory flows at 50% (V′50) and 25% (V′25) of vital capacity were found in obese men, but not in obese women [38]. Although the difference between obese and normal weight men in V′50 disappeared after normalization for vital capacity, the difference in V′25 persisted after normalization, suggesting the presence of peripheral airway obstruction in obese men. It is not clear why this was only detected in men in this study, but increased peripheral airway obstruction in obesity is consistent with findings from other studies, in both men and women, showing that obesity is associated with increased frequency dependence of resistance [30] and increased frequency dependence of compliance [11].
Expiratory Flow Limitation During Tidal Breathing
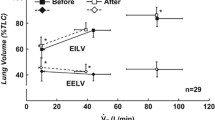
Expiratory flow rates are closely related to lung volumes, so that maximal flow decreases rapidly as expired volume approaches RV. As shown in Fig. 1.4, the predicted maximal flow, shown in the dashed line, is maintained well above the flows generated during tidal expiration at normal FRC, but the obese subject, breathing tidally at very low FRC, has very little expiratory flow reserve available during tidal breathing. For the obese individual, breathing at low lung volume places the tidal flow volume loop in a region where it may encroach on the maximal flow, thus increasing the risk of tidal expiratory flow limitation. It is not clear whether tidal expiratory flow limitation is a common occurrence in the obese. Two studies [40, 41], using the negative expiratory pressure technique, have found evidence of expiratory flow limitation in only 20% of severely obese subjects when upright. However, both expiratory flow limitation and breathlessness substantially increased when the subjects were placed supine. Quantification of expiratory flow limitation from the flow volume loop, as the percentage of the tidal volume that encroached on the maximal flow envelope, shows highly significant differences between obese and normal weight women when seated at rest [18]. However, the accuracy of comparisons of tidal and maximal flow volume curves may be limited by effects of dynamic compression of the airways during maximal forced expiratory manoeuvres. New techniques are available for measuring expiratory flow limitation during tidal breathing, based on the forced oscillation technique [42], that would allow larger studies to determine the extent of expiratory flow limitation in obese populations.
Flow volume loop from a healthy, obese individual (BMI = 43). The dashed lines show the predicted normal flow volume and tidal loops. There is minimal airway obstruction, but because FRC is low, the tidal loop encroaches onto the maximal loop, putting this individual at risk of expiratory flow limitation during tidal breathing
Intrinsic PEEP and Dynamic Hyperinflation
The presence of expiratory flow limitation during tidal breathing promotes the development of intrinsic positive end-expiratory pressure (PEEPi) and dynamic hyperinflation in obstructive airway disease, where it is an important determinant of respiratory symptoms. Pankow et al. [40] were able to detect PEEPi in all six severely obese subjects in whom they were able to make the measurement, even in the absence of expiratory flow limitation. The mechanism for PEEPi in the absence of EFL is unknown, but could be due to persistent post-inspiratory activity of the diaphragm, which has previously been observed in severely obese subjects [16]. PEEPi is a potential cause of respiratory symptoms in the obese since it is an additional elastic load that must be overcome at the beginning of each inspiration.
Although dynamic hyperinflation is usually closely associated with expiratory flow limitation and PEEPi, it might be expected that the decrease in respiratory system compliance associated with obesity would reduce the risk of dynamic hyperinflation in the obese. Indeed, the relationship between BMI and FRC is curvilinear and tends to flatten at high BMI (Fig. 1.3). We can speculate that the development of expiratory flow limitation and PEEPi in severely obese individuals might counteract, at least to a small degree, the effects of the stiffened respiratory system on lung volumes.
Airway Closure and Ventilation Distribution
It has been postulated that breathing at low lung volume, particularly in the setting of marked reduction in ERV seen in obesity, could lead to closure of peripheral airways in dependent lung zones [2, 11]. However, indicators of gas trapping and airway closure, such as RV [16, 28] and closing capacity [43], are not usually noted to be increased in obesity at rest. On the other hand, there is consistent evidence that if the FRC is very low, closing capacity exceeds the FRC and airway closure can occur within the tidal breaths [43–46]. Closing capacity, and particularly the extent to which closure occurs within the range of tidal breathing, has been correlated with arterial PO2 [43, 46] raising the possibility that airway closure during tidal breathing may be associated with under-ventilation of some regions of the lung.
Abnormalities of regional ventilation have been observed in obese individuals using lung imaging to determine the distribution of ventilation [47–49]. Holley et al. [47] found that in obese subjects with marked reductions in ERV to around 20% predicted, ventilation was preferentially distributed to the upper zones of the lung, leaving the lower, dependent zones relatively under-ventilated. Similarly, Demedts [49] found that ventilation was significantly lower in the lung bases and tended to be higher in the apical regions in obese subjects compared to normal weight controls. The findings were consistent with a reduced expansion of the basal zone, possibly due to limitations in chest wall and diaphragm movements. However, global measures of ventilation heterogeneity, measured by the slope of phase III from single-breath washouts or by lung clearance index, are normal even in severely obese individuals [43].
Gas Exchange
Mild hypoxemia and increased alveolar-arterial oxygen difference are frequently reported, even in eucapnic obese individuals [7, 8, 43, 50, 51], and have been associated with abdominal obesity in the morbidly obese [52]. Reduction in oxygenation is unlikely to be due to abnormalities of gas transfer since most studies suggest that DlCO is normal [6, 17, 27, 53], even in morbid obesity [29]. Indeed, some studies suggest that DlCO is increased in extremely obese subjects [27, 38], probably as a result of the increase in blood volume [27]. Regional ventilation-perfusion mismatch in the dependent zones of the lung is a potential determinant of hypoxemia in obese individuals. Although an increase in blood volume in the obese could improve the homogeneity of perfusion and increase perfusion in the apices of the lung, the distribution of perfusion is predominantly to the lower zones, and individuals with reduced ventilation in the lung bases are likely to be at risk of ventilation-perfusion mismatch [47]. The extent to which gas exchange abnormalities in the obese are reversible is unclear, since some weight loss studies show improvements in arterial oxygen tensions [51, 54] while others report no change [44, 55]. Hakala et al. [44] found no increase in oxygenation with weight loss, even though there were significant improvements in FRC and most subjects no longer had closing capacities above FRC.
Consequences of Reduced Intrathoracic Volume
The effect of obesity on lung function is often described in terms of a restrictive rather than obstructive pattern, characterized by reduction in total lung capacity and vital capacity. The mechanisms for the reduction in total lung capacity in the obese are not well understood, but, as proposed in Fig. 1.1, may be due to reduced intrathoracic volume, as outlined below, or decreased respiratory system compliance.
Total Lung Capacity
The magnitude of the reduction in TLC with increasing weight is proportionally smaller than the effect on FRC, at least until BMI exceeds 35 kg/m2 [23], with TLC usually maintained above the lower limit of normal even in severe obesity [23, 26, 28]. Lung restriction of the magnitude associated with restrictive lung disease, defined as TLC below the lower limit of normal, is not commonly associated with obesity in the absence of other disease. Nonetheless, evidence from prospective studies showing increases in TLC with weight loss in both mild [55] and morbidly obese [51] subjects, and decreases in vital capacity with weight gain [56], is consistent with the development of mild restrictive patterns of lung function in obesity.
The reasons for the reduction in TLC in the obese are unknown. It may be due to a reduction in the downwards movement of the diaphragm, due to increased abdominal mass, which could decrease TLC by limiting the room for lung expansion on inflation. Alternatively, deposition of fat in sub-pleural spaces [57] or elsewhere in the intrathoracic cavity might directly reduce lung volume by reducing the volume of the chest cavity. An exploratory study to investigate the mechanism for reduced TLC in obesity used MRI to measure intrathoracic volumes in obese and non-obese men and found increased mediastinal volume in the obese due to an increase in the volume of intrathoracic fat, the heart and major blood vessels [1]. At full inflation, the proportion of the intrathoracic volume occupied by inflated lungs was only 78% of the total in the obese compared with 88% in the controls, suggesting that the increased mediastinal volume may prevent full lung expansion in the obese, and may therefore explain the slight loss of TLC with increasing BMI. However, the marked loss of TLC in obese subjects with lung restriction (TLC < 80% predicted) was not explained by increased mediastinal volume, suggesting that other factors, such as reduced expansion of the thoracic cage, may also be important in this subgroup [1]. Since respiratory muscle strength and maximum inspiratory and expiratory pressures have been shown to be intact in obesity [16, 37, 58], it is unlikely that these would be an important determinant of obesity-related reduction in TLC.
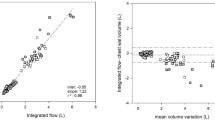
Spirometry
A reduction in total lung capacity, in the absence of any change in residual volume, indicates a reduction in vital capacity (VC). Consistent with a mild restrictive pattern of lung function in the obese, there is a progressive linear decrease in VC with increasing BMI that parallels the decrease in TLC [23]. Similarly, increasing BMI is also associated with a decrease in both FEV1 and FVC [30, 59, 60]. However, this effect is small and both FEV1 and FVC are usually within the normal range in healthy obese adults [59, 60] and children [61]. As a result, the FEV1/FVC ratio, which is a marker of airway obstruction, is usually well preserved or increased [30, 34, 38, 59, 60], even in morbid obesity [29]. Figure 1.5 shows data from a population of 1,971 adults aged between 17 and 73 years [60] based on per cent of predicted values. Although FVC is affected to a greater extent than FEV1 as BMI increases, FEV1/FVC ratio remains normal across the weight groups, even in the severely obese group. Studies looking at the effect of body fat distribution on spirometry have shown that abdominal obesity is a stronger predictor than either weight or BMI of reductions in FEV1 and FVC [33, 62], with one very large study of over 130,000 people suggesting that abdominal obesity may also be a risk for reduced FEV1/FVC ratio [62]. Moreover, weight gain following smoking cessation [63] or with increasing age [56] is associated with reductions in both FEV1 and FVC; the effect is greater on FVC than on FEV1 and greater in men than women, presumably because men gain more abdominal fat than women.
Mean spirometric values, according to weight category, in adults (Adapted from data in Schachter et al. [60]). FEV1 (diamonds) and FVC (triangles), as percent predicted, and FEV1/FVC (squares) as a percentage
Volume-Independent Effects on Airway Function
Although many of the effects of obesity on airway function can be attributed to the mechanical effects of breathing at low lung volume, as illustrated in Fig. 1.1, some studies have reported effects that appear to be independent of lung volume. In a population study of young adults, King et al. [24] found that obesity was associated with a persistent decrease in airway calibre, measured by respiratory system conductance, even after adjustment for lung volumes. This effect was present in men, but not in women. Another study by Watson et al. [28] comparing obese and control subjects sitting and supine found that differences in lung volume could only partly explain the differences in airflow resistance between obese and controls [28] or the increase in resistance associated with recumbency [28, 37]. Also, as discussed above, in the studies by Rubinstein et al. [38], although adjustment for vital capacity normalized V′50, there were significant differences in V′25 which persisted after normalization. Lastly, the effect of obesity on spirometry increases with increasing duration of obesity, independent of the severity of obesity [64].
The cause of these volume-independent abnormalities of airway function is unknown. In addition, it is unclear whether there are any structural changes in the airways of the obese. It is possible that airway structures could be remodelled by chronic exposure to pro-inflammatory adipokines or systemic inflammation, or damaged by the continual opening and closing of small airways throughout the breathing cycle [45]. However, it is unlikely that fat is present in the airways of obese people or has any direct effect on airway structure, but studies of diet-induced obesity in rats have reported changes in lipid deposition in the lungs [65] which may affect surfactant function [66]. There are no reports of biopsy, pathological or imaging studies of the airway walls of obese subjects to indicate whether there are any cellular or structural abnormalities of the airways that might explain abnormal airway function.
Effects of Altered Ventilatory Mechanics on Symptoms, Performance and Clinical Presentation
Breathlessness at Rest and During Exercise
Breathlessness at rest is usually regarded as uncommon in healthy obese subjects, particularly in those with mild to moderate obesity. One study found that 15 of 23 mildly obese men reported breathing difficulties at rest associated with lower maximum voluntary ventilation and maximal expiratory flows at low lung volumes. However, the dyspnoeic group included a greater proportion of smokers, which may account for some of the symptoms and differences in lung function [67]. In morbidly obese subjects (BMI > 40 kg/m2) [68], dyspnoea scores at rest correlate with both inspiratory muscle endurance and lung function.
In contrast, breathlessness during exercise is a common complaint among obese individuals. In population studies, subjects with the highest BMI quintile have the greatest risk of dyspnoea with exertion, despite being at least risk of airway obstruction [59]. Standardized weight-bearing exercise tests, such as the 6-minute walk test, show that exercise capacity is reduced in obese adults [69, 70] and children [71] compared to normal weight controls. However, increased exertional symptoms in the obese are most likely due to the increased metabolic cost of the energy needed to move heavy limbs and drive the respiratory muscles [18, 72, 73], rather than to deconditioning or to abnormalities of airway or lung mechanics. Studies using weight-supported exercise, such as with a cycle ergometer, show that peak exercise capacity, in terms of both peak work rate and oxygen consumption, is normal in healthy obese subjects suggesting that they are not deconditioned [18, 72, 74]. The ventilatory response to inhaled CO2 [17] and the relationships between oxygen consumption and minute ventilation, and between breathlessness and both oxygen consumption and minute ventilation are all normal in the obese [18]. Breathing at low lung volume could increase exertional breathlessness by preventing obese subjects from decreasing their end-expiratory volume during exercise [75, 76], but, in fact, because they breathe at low lung volumes, obese subjects have enough inspiratory reserve to increase their end-expiratory lung volume, to minimize expiratory flow limitation, but still increase tidal volumes to meet ventilatory demands [18]. Taken together, these observations suggest that the ability of the obese to increase ventilation in response to increasing metabolic demand is not impaired and that changes in lung volumes or airway mechanics due to obesity make little contribution to respiratory discomfort during exercise.
Effects of Obesity on Respiratory Function in Disease
The detrimental effects of obesity on lung function may have an impact on the outcomes of respiratory disease, although the effects are complex. In asthma, obesity is associated with greater prevalence and incidence of the disease [60, 61, 77] and may also be associated with worse clinical outcomes [78, 79], particularly in mild [80] or well-controlled [81] disease. In COPD, increasing BMI is associated with a reduced risk of death in patients with more severe disease, but not in those with mild COPD [82]. Although these relationships appear paradoxical, the mechanical effects of obesity on lung function are likely to be important contributing factors to many of the effects of obesity in respiratory disease.
How could the mechanical effects of obesity on lung function modify asthma pathophysiology? Asthma is characterized by airway obstruction, airway inflammation and airway hyperresponsiveness. One hypothesis suggests that breathing at reduced tidal volumes could affect the modulation of airway smooth muscle contractility by regular tidal stretching and deep inspirations [83], and increase the responsiveness of the muscle. Tidal volumes are not usually abnormal in mild to moderate obesity [18, 20–22]. However, breathing at low lung volumes means that airway calibre, and thus the length of airway smooth muscle, is reduced throughout the breathing cycle. It is not clear whether this leads to clinically meaningful increases in airway hyperresponsiveness in the obese. In studies of asthmatic subjects, there is little evidence that the severity of AHR is systematically increased in the obese [39, 80, 84, 85]. Moreover, there is inconsistent evidence of an association between BMI and airway responsiveness in studies of random populations [60, 61, 86]. An alternative hypothesis is that the reduction in operating lung volume in the obese has the potential to amplify the symptoms associated with bronchoconstriction. Bronchoconstriction in the obese is associated with increased airway closure compared to non-obese controls [87] and thus could increase gas trapping and alter ventilation distribution. Bronchoconstriction at low lung volume increases the risk of expiratory flow limitation and causes greater dynamic hyperinflation in obese asthmatic [84] and non-asthmatic [21] subjects, which may increase the severity of dyspnoea [88]. Nicolacakis et al. [39] suggest that obesity and asthma have additive, rather than synergistic effects, on outcomes such as spirometry and lung volumes. We can speculate that, in more severe or uncontrolled asthma, symptoms are likely to be dominated by the effects of uncontrolled airway inflammation and airway hyperresponsiveness. However, as these effects diminish with treatment and better asthma control, the effects of obesity on the development of airway closure, expiratory flow limitation and dynamic hyperinflation during episodes of mild bronchoconstriction may become more apparent. The occurrence of these additional elastic loads during bronchoconstriction, reflected by greater changes in respiratory system reactance in obese than non-obese subjects [21, 22], are often not well reflected by spirometry and may explain why some obese asthmatics have more severe symptoms than their lean counterparts, despite similar spirometry [89].
In COPD, it has been proposed that reduced operating lung volumes in obese patients may provide a mitigating influence on the intensity of exertional dyspnoea, by counterbalancing the negative mechanical consequences of severe lung hyperinflation [90, 91]. Because the obese COPD patients start from a much reduced FRC, dynamic hyperinflation during exercise does not result in such severe loss of inspiratory reserve as in non-obese COPD patients. The interactions between obesity and respiratory disease are discussed in detail in later chapters.
In restrictive lung disease, there are few available data about the effects of obesity on lung function. However, one study suggests increased BMI is associated with better survival in patients with idiopathic pulmonary fibrosis [92].
Impact of Obesity on the Interpretation of Pulmonary Function Tests
Obesity modifies many aspects of pulmonary function, even in people without respiratory disease, so the interpretation of pulmonary function tests in obese individuals can present problems. As outlined in this chapter, obesity in people without respiratory disease is typically associated with marked reductions in expiratory reserve volume and FRC, and modest reductions in TLC, VC, FEV1 and FVC. However, reductions in FEV1/FVC ratio, indicating airway obstruction, are not typical and would require further investigation. Measurements of expiratory flows and airway resistance may be abnormal and must be adjusted for lung volume before interpretation. The effect of obesity on pulmonary function tests in people at the extremes of age and height, where predicted values are less reliable, may be difficult to interpret.
In restrictive lung disease, TLC is, by definition, below the lower limit of normal. Although obesity is associated with a mild restrictive pattern of lung function, reductions of TLC of this magnitude are uncommon, even in severe obesity, and causes other than obesity should be sought for this restrictive pattern. Furthermore, in diseases such as idiopathic pulmonary fibrosis, diffusing capacity is reduced and both hypoxia and hypercapnia may be present. Some obese subjects have mild hypoxia on blood gas analysis, despite normal diffusing capacity. However, the presence of hypercapnia is uncommon and would suggest obesity hypoventilation syndrome (discussed in Chap. 5).
References
Watson RA, Pride NB, Thomas EL, et al. Reduction of total lung capacity in obese men: comparison of total intrathoracic and gas volumes. J Appl Physiol. 2010;108:1605–12.
Behazin N, Jones SB, Cohen RI, Loring SH. Respiratory restriction and elevated pleural and esophageal pressures in morbid obesity. J Appl Physiol. 2010;108:212–8.
Sugerman H, Windsor A, Bessos M, Wolfe L. Intra-abdominal pressure, sagittal abdominal diameter and obesity comorbidity. J Intern Med. 1997;241:71–9.
Sutherland TJT, Goulding A, Grant AM, et al. The effect of adiposity measured by dual-energy x-ray absorptiometry on lung function. Eur Respir J. 2008;32:85–91.
Naimark A, Cherniack RM. Compliance of the respiratory system and its components in health and obesity. J Appl Physiol. 1960;15:377–82.
Sharp JT, Henry JP, Swaeny SK, Meadows WR, Pietras RJ. The total work of breathing in normal and obese men. J Clin Invest. 1964;43:728–39.
Pelosi P, Croci M, Ravagnan I, et al. The effects of body mass on lung volumes, respiratory mechanics, and gas exchange during general anesthesia. Anesth Analg. 1998;87:654–60.
Hedenstierna G, Santesson J. Breathing mechanics, dead space and gas exchange in the extremely obese, breathing spontaneously and during anaesthesia with intermittent positive pressure ventilation. Acta Anaesthesiol Scand. 1976;20:248–54.
Suratt PM, Wilhoit SC, Hsiao HS, Atkinson RL, Rochester DF. Compliance of chest wall in obese subjects. J Appl Physiol. 1984;57:403–7.
Steier J, Jolley CJ, Seymour J, et al. Neural respiratory drive in obesity. Thorax. 2009;64: 719–25.
Douglas FG, Chong PY. Influence of obesity on peripheral airways patency. J Appl Physiol. 1972;33:559–63.
Pelosi P, Croci M, Ravagnan I, Vicardi P, Gattinoni L. Total respiratory system, lung, and chest wall mechanics in sedated-paralyzed postoperative morbidly obese patients. Chest. 1996;109:144–51.
Rochester DF, Enson Y. Current concepts in the pathogenesis of the obesity hypoventilation syndrome. Mechanical and circulatory factors. Am J Med. 1974;57:402–20.
Sharp JT, Henry JP, Swaeny SK, Meadows WR, Pietras RJ. Effects of mass loading the respiratory system in man. J Appl Physiol. 1964;19:959–66.
Axen K, Haas SS, Haas F, Gaudino D, Haas A. Ventilatory adjustments during sustained mechanical loading in conscious humans. J Appl Physiol. 1983;55:1211–8.
Sampson MG, Grassino AE. Load compensation in obese patients during quiet tidal breathing. J Appl Physiol. 1983;55:1269–76.
Dempsey JA, Reddan W, Rankin J, Balke B. Alveolar-arterial gas exchange during muscular work in obesity. J Appl Physiol. 1966;21:1807–14.
Ofir D, Laveneziana P, Webb KA, O’Donnell DE. Ventilatory and perceptual responses to cycle exercise in obese women. J Appl Physiol. 2007;102:2217–26.
Mansell AL, Walders N, Wamboldt MZ, et al. Effect of body mass index on response to methacholine bronchial provocation in healthy and asthmatic adolescents. Pediatr Pulmonol. 2006;41:434–40.
Boulet L-P, Turcotte H, Boulet G, Simard B, Robichaud P. Deep inspiration avoidance and airway response to methacholine: influence of body mass index. Can Respir J. 2005;12: 371–6.
Salome CM, Munoz PA, Berend N, et al. Effect of obesity on breathlessness and airway responsiveness to methacholine in non-asthmatic subjects. Int J Obes. 2008;32:502–9.
Torchio R, Gobbi A, Gulotta C, et al. Mechanical effects of obesity on airway responsiveness in otherwise healthy humans. J Appl Physiol. 2009;107:408–16.
Jones RL, Nzekwu M-MU. The effects of body mass index on lung volumes. Chest. 2006;130:827–33.
King GG, Brown NJ, Diba C, et al. The effects of body weight on airway calibre. Eur Respir J. 2005;25:896–901.
Sin DD, Sutherland ER. Obesity and the lung: 4. Obesity and asthma. Thorax. 2008;63:1018–23.
Collins LC, Hoberty PD, Walker JF, Fletcher EC, Peiris AN. The effect of body fat distribution on pulmonary function tests. Chest. 1995;107:1298–302.
Ray CS, Sue DY, Bray G, Hansen JE, Wasserman K. Effects of obesity on respiratory function. Am Rev Respir Dis. 1983;128:501–6.
Watson RA, Pride NB. Postural changes in lung volumes and respiratory resistance in subjects with obesity. J Appl Physiol. 2005;98:512–7.
Biring M, Lewis M, Liu JT, Mohsenifar Z. Pulmonary physiologic changes of morbid obesity. Am J Med Sci. 1999;318:293–7.
Zerah F, Harf A, Perlemuter L, et al. Effects of obesity on respiratory resistance. Chest. 1993;103:1470–6.
Chen Y, Rennie D, Cormier YF, Dosman JA. Waist circumference is associated with pulmonary function in normal-weight, overweight, and obese subjects. Am J Clin Nutr. 2007;85:35–9.
Canoy D, Luben R, Welch A, et al. Abdominal obesity and respiratory function in men and women in the EPIC-Norfolk Study, United Kingdom. Am J Epidemiol. 2004;159:1140–9.
Ochs-Balcom HM, Grant BJ, Muti P, et al. Pulmonary function and abdominal obesity in the general population. Chest. 2006;129:853–62.
Lazarus R, Sparrow D, Weiss ST. Effects of obesity and fat distribution on ventilatory function. Chest. 1997;111:891–8.
De Lorenzo A, Maiolo C, Mohamed EI, et al. Body composition analysis and changes in airways function in obese adults after hypocaloric diet. Chest. 2001;119:1409–15.
Babb TG, Wyrick BL, Chase PJ, et al. Weight loss via diet and exercise improves exercise breathing mechanics in obese men. Chest. 2011;140:454–60.
Yap JC, Watson RA, Gilbey S, Pride NB. Effects of posture on respiratory mechanics in obesity. J Appl Physiol. 1995;79:1199–205.
Rubinstein I, Zamel N, DuBarry L, Hoffstein V. Airflow limitation in morbidly obese, nonsmoking men. Ann Int Med. 1990;112:828–32.
Nicolacakis K, Skowronski ME, Coreno AJ, et al. Observations on the physiological interactions between obesity and asthma. J Appl Physiol. 2008;105:1533–41.
Pankow W, Podszus T, Gutheil T, et al. Expiratory flow limitation and intrinsic positive end-expiratory pressure in obesity. J Appl Physiol. 1998;85:1236–43.
Ferretti A, Giampiccolo P, Cavalli A, Milic-Emili J, Tantucci C. Expiratory flow limitation and orthopnea in massively obese subjects. Chest. 2001;119:1401–8.
Dellaca RL, Santus P, Aliverti A, et al. Detection of expiratory flow limitation in COPD using the forced oscillation technique. Eur Respir J. 2004;23:232–40.
Hedenstierna G, Santesson J, Norlander O. Airway closure and distribution of inspired gas in the extremely obese, breathing spontaneously and during anaesthesia with intermittent positive pressure ventilation. Acta Anaesthesiol Scand. 1976;20:334–42.
Hakala K, Mustajoki P, Aittomaki J, Sovijarvi AR. Effect of weight loss and body position on pulmonary function and gas exchange abnormalities in morbid obesity. Int J Obes. 1995;19:343–6.
Milic-Emili J, Torchio R, D’Angelo E. Closing-volume: a reappraisal (1967–2007). Eur J Appl Physiol. 2007;99:567–83.
Farebrother MJB, McHardy GJR, Munro JF. Relation between pulmonary gas exchange and closing volume before and after substantial weight loss in obese subjects. Br Med J. 1974;3: 391–3.
Holley HS, Milic-Emili J, Becklake MR, Bates DV. Regional distribution of pulmonary ventilation and perfusion in obesity. J Clin Invest. 1967;46:475–81.
Hurewitz A, Susskind H, Harold W. Obesity alters regional ventilation in lateral decubitus position. J Appl Physiol. 1985;59:774–83.
Demedts M. Regional distribution of lung volumes and of gas inspired at residual volume: influence of age, body weight and posture. Bull Eur Physiopathol Respir. 1980;16:271–85.
Jenkins SC, Moxham J. The effects of mild obesity on lung function. Respir Med. 1991;85: 309–11.
Thomas PS, Milledge JS. Respiratory function in the morbidly obese before and after weight loss. Thorax. 1989;44:382–6.
Zavorsky GS, Murias JM, Kim DJ, et al. Waist-to-hip ratio is associated with pulmonary gas exchange in the morbidly obese. Chest. 2007;131:362–7.
Sutherland TJT, Cowan JO, Young S, et al. The association between obesity and asthma: interactions between systemic and airway inflammation. Am J Respir Crit Care Med. 2008;178:469–75.
Refsum HE, Holter PH, Lovig T, Stadaas JO. Pulmonary function and energy expenditure after marked weight loss in obese women: observations before and one year after gastric banding. Int J Obes. 1990;14:175–83.
Womack CJ, Harris DL, Katzel LI, et al. Weight loss, not aerobic exercise, improves pulmonary function in older obese men. J Gerontol A Biol Sci Med Sci. 2000;55:M453–7.
Chen Y, Horne SL, Dosman JA. Body weight and weight gain related to pulmonary function decline in adults: a six year follow up study. Thorax. 1993;48:375–80.
Sargent EN, Boswell Jr WD, Ralls PW, Markovitz A. Subpleural fat pads in patients exposed to asbestos: distinction from non-calcified pleural plaques. Radiology. 1984;152:273–7.
Kelly TM, Jensen RL, Elliott CG, Crapo RO. Maximum respiratory pressures in morbidly obese subjects. Respiration. 1988;54:73–7.
Sin DD, Jones RL, Man SF. Obesity is a risk factor for dyspnea but not for airflow obstruction. Arch Intern Med. 2002;162:1477–81.
Schachter LM, Salome CM, Peat JK, Woolcock AJ. Obesity is a risk for asthma and wheeze but not airway hyperresponsiveness. Thorax. 2001;56:4–8.
Schachter LM, Peat JK, Salome CM. Asthma and atopy in overweight children. Thorax. 2003;58:1031–5.
Leone N, Courbon D, Thomas F, et al. Lung function and metabolic syndrome: the critical role of abdominal obesity. Am J Respir Crit Care Med. 2008;179:509–16.
Wise RA, Enright PL, Connett JE, et al. Effect of weight gain on pulmonary function after smoking cessation in the Lung Health Study. Am J Resp Crit Care Med. 1998;157:866–72.
Santamaria F, Montella S, Greco L, et al. Obesity duration is associated to pulmonary function impairment in obese subjects. Obesity (Silver Spring). 2011;19:1623–8.
Inselman LS, Spencer H. Obesity-induced hyperplastic lung growth. Am Rev Respir Dis. 1987;135:613–6.
Inselman LS, Chander A, Spitzer AR. Diminished lung compliance and elevated surfactant lipids and proteins in nutritionally obese young rats. Lung. 2004;182:101–17.
Sahebjami H. Dyspnea in obese healthy men. Chest. 1998;114:1373–7.
Collett F, Mallart A, Bervar JF, et al. Physiologic correlates of dyspnea in patients with morbid obesity. Int J Obes. 2007;31:700–6.
Larsson UE, Reynisdottir S. The six-minute walk test in outpatients with obesity: reproducibility and known group validity. Physiother Res Int. 2008;13:84–93.
Beriault K, Carpentier AC, Gagnon C, et al. Reproducibility of the 6-minute walk test in obese adults. Int J Sports Med. 2009;30:725–7.
Morinder G, Mattsson E, Sollander C, Marcus C, Larsson UE. Six-minute walk test in obese children and adolescents: reproducibility and validity. Physiother Res Int. 2009;14:91–104.
Babb TG, Ranasinghe KG, Comeau LA, Semon TL, Schwartz B. Dyspnea on exertion in obese women. Association with increased oxygen cost of breathing. Am J Respir Crit Care Med. 2008;178:116–23.
Kress JP, Pohlman AS, Alverdy J, Hall JB. The impact of morbid obesity on oxygen cost of breathing (VO2RESP) at rest. Am J Respir Crit Care Med. 1999;160:883–6.
Babb TG, DeLorey DS, Wyrick BL, Gardner PP. Mild obesity does not limit change in end-expiratory lung volume during cycling in young women. J Appl Physiol. 2002;92: 2483–90.
Babb TG, Buskirk ER, Hodgson JL. Exercise end-expiratory lung volumes in lean and moderately obese women. Int J Obes. 1989;13:11–9.
DeLorey DS, Wyrick BL, Babb TG. Mild-to-moderate obesity: implications for respiratory mechanics at rest and during exercise in young men. Int J Obes. 2005;29:1039–47.
Beuther DA, Sutherland ER. Overweight, obesity, and incident asthma: a meta-analysis of prospective epidemiologic studies. Am J Respir Crit Care Med. 2007;175:661–6.
Mosen DM, Schatz M, Magid DJ, Camargo Jr CA. The relationship between obesity and asthma severity and control in adults. J Allergy Clin Immunol. 2008;122:507–11. e6.
Vortmann M, Eisner MD. BMI and health status among adults with asthma. Obesity (Silver Spring). 2008;16:146–52.
Raviv S, Dixon AE, Kalhan R, Shade D, Smith LJ. Effect of obesity on asthma phenotype is dependent upon asthma severity. J Asthma. 2011;48:98–104.
Farah CS, Kermode JA, Downie SR, et al. Obesity is a determinant of asthma control, independent of inflammation and lung mechanics. Chest. 2011;140:659–66.
Landbo C, Prescott E, Lange P, Vestbo J, Almdal TP. Prognostic value of nutritional status in chronic obstructive pulmonary disease. Am J Respir Crit Care Med. 1999;160:1856–61.
Fredberg J, Inouye D, Mijailovich M, Butler J. Perturbed equilibrium of myosin binding in airway smooth muscle and its implications in bronchospasm. Am J Resp Crit Care Med. 1999;159:959–67.
Sutherland TJT, Cowan JO, Taylor DR. Dynamic hyperinflation with bronchoconstriction: differences between obese and nonobese women with asthma. Am J Respir Crit Care Med. 2008;177:970–5.
van Veen IH, ten Brinke A, Sterk PJ, Rabe KF, Bel EH. Airway inflammation in obese and non-obese patients with difficult-to-treat asthma. Allergy. 2008;63:570–4.
Chinn S, Jarvis D, Burney P. Relation of bronchial responsiveness to body mass index in the ECRHS. Thorax. 2002;57:1028–33.
Chapman DG, Berend N, King GG, Salome CM. Increased airway closure is a determinant of airway hyperresponsiveness. Eur Respir J. 2008;32:1563–9.
Lougheed MD, Lam M, Forkert L, Webb KA, O’Donnell DE. Breathlessness during acute bronchoconstriction in asthma. Am Rev Respir Dis. 1993;148:1452–9.
Thomson CC, Clark S, Camargo Jr CA. Body mass index and asthma severity among adults presenting to the emergency department. Chest. 2003;124:795–802.
Guenette JA, Jensen D, O’Donnell DE. Respiratory function and the obesity paradox. Curr Opin Clin Nutr Metab Care. 2010;13:618–24.
Ora J, Laveneziana P, Wadell K, et al. Effect of obesity on respiratory mechanics during rest and exercise in COPD. J Appl Physiol. 2011;111:10–9.
Alakhras M, Decker PA, Nadrous HF, Collazo-Clavell M, Ryu JH. Body mass index and mortality in patients with idiopathic pulmonary fibrosis. Chest. 2007;131:1448–53.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2013 Springer Science+Business Media New York
About this chapter
Cite this chapter
Salome, C.M., King, G.G., Berend, N. (2013). Effects of Obesity on Lung Function. In: Dixon, A., Clerisme-Beaty, E. (eds) Obesity and Lung Disease. Respiratory Medicine, vol 19. Humana Press, Totowa, NJ. https://doi.org/10.1007/978-1-62703-053-3_1
Download citation
DOI: https://doi.org/10.1007/978-1-62703-053-3_1
Published:
Publisher Name: Humana Press, Totowa, NJ
Print ISBN: 978-1-62703-052-6
Online ISBN: 978-1-62703-053-3
eBook Packages: MedicineMedicine (R0)