Abstract
Timely and accurate assessment of skeletal remains is integral to the progression of medicolegal death investigations, including cases involving child maltreatment. These cases have legal implications that could potentially send the innocent to prison or set the guilty free if the assessment is not made correctly. The skeleton can provide useful information regarding an individual’s health and disease and evidence of trauma. The juvenile skeleton is characterized by nutrition-dependent rapid growth. It differs from the adult skeleton in several ways including anatomy and morphology, physiology, and biomechanics. Since the juvenile skeleton is in a constant state of change, bone morphology will vary depending on the age and phase of development. Integral to investigating child maltreatment is the ability to recognize abnormalities. Since the juvenile skeleton is very different from that of an adult, an investigator who is not well trained in juvenile skeletal anatomy may overlook important evidence or misdiagnose. Therefore, it is essential for researchers investigating the juvenile skeleton to have an understanding of skeletal growth and development and juvenile skeletal anatomy to accurately and efficiently locate and evaluate a set of remains.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
3.1 Introduction
In 2008, the U.S. Department of Health and Human Services reported that 772,000 children were victims of maltreatment. Of these, 71% were classified as victims of neglect, 16% as victims of physical abuse, 9% as victims of sexual abuse, and 7% as victims of emotional abuse [1, 2]. In 2008, an estimated 1,740 children died as a result of neglect and abuse [1, 2]. Of these, 80% of the deaths occurred among children younger than 4 years of age, 10% in children between 4 and 7 years, 4% in children between 8 and 11 years, and 2% in children between 16 and 17 [1, 2]. Since the human skeleton is capable of providing information about what happened to a person during their life, the skeleton can yield crucial information regarding child maltreatment. For example, it can tell us about a child’s health, disease, whether trauma occurred to the bone, and the timing of trauma. In order for an investigator to recognize vital information regarding the health and welfare of a child, one must first have a complete understanding of the juvenile skeleton, what is considered normal, and how juvenile remains differ from the adult skeleton.
The human skeleton serves a number of functions including providing shape, support, and protection for vital soft tissue organs. In addition, it allows movement, produces blood cells, and stores vital vitamins and minerals that are important for bodily function. The human skeleton can also provide a wealth of information about the person to whom they belong. It can provide important evidence in medicolegal death investigations including the identification of unknown remains and child abuse. It holds information regarding an individual’s biological sex, age-at-death, ancestral origins, health and disease, and evidence of trauma. Forensic investigations involving juvenile remains are very sensitive, especially when child abuse is suspected as misdiagnosis may send innocent caregivers to prison or, conversely, allow the guilty to walk free. Understanding the juvenile skeleton is essential for proper and timely recovery, identification, analyses of remains, and case resolution in child abuse–related investigations. For example, recovery of juvenile remains can prove difficult if those employed to search for the remains cannot recognize the features and bones that make up the juvenile skeleton. They may become confused if confronted with nonhuman remains, or disregard the remains altogether.
Baker et al. [3] have noted that many osteology courses lack training in juvenile skeletal identification. Rang and Wenger [4] stated it perfectly with their book chapter titled “Children Are Not Just Small Adults.” Therefore, having been trained in the identification and methods associated only with the adult skeleton will leave an investigator ill-equipped to accurately assess remains belonging to a child. When investigating juvenile remains, it is important to remember that children’s bone react to stresses differently than adult bones because the anatomy, biomechanics, and physiology of a child’s skeleton are very different from that of an adult [4]. In addition, identification of the various elements may prove difficult for an individual with little knowledge of the juvenile skeleton since it is morphologically different from the adult skeleton and throughout early development is composed of numerically more elements that are held together by dense connective tissues. This chapter will discuss the differences between juvenile and adult skeletons and provide the reader with an overview of human bone growth and development, juvenile anatomy, and bone health. It is intended to supplement the reading found throughout the rest of this book and provides the reader with a basic understanding of the various concepts that will be discussed in later chapters. However, it is beyond the scope of this chapter to provide a complete treatment of human bone growth and development, juvenile and adult osteology, and bone health as each topic has easily comprised entire textbooks. Therefore, a list of supplemental readings is suggested at the end of this chapter.
3.2 Anatomical Terminology
To efficiently describe the human skeleton and share data, the human skeleton is referred to in terms of anatomical direction. First and foremost, the human skeleton is oriented in what is called “standard anatomical position.” This position is characterized by the human body facing forward with the arms lying near the side of the body, the palms facing up, the legs extended together, and the toes pointing forward [5] (Fig. 3.1). This ensures that no bones are crossed over one another. For example, the palms are oriented facing up so that the radius and ulna lie parallel to each another.
The body is then divided into three planes of reference. These include the sagittal, coronal, and transverse planes. The sagittal plane divides the body into left and right halves. The sagittal plane runs along the midline of the body and allows us to refer to features and structures that lie medially (toward the center of the body) or laterally (away from the midline of the body). The coronal plane divides the body into front and back halves. The front half of the coronal plane is referred to as anterior and the back half as posterior. Lastly, the transverse plane divides the body into upper and lower halves and passes perpendicular to the sagittal and frontal planes. With reference to the transverse plane, the term “superior” is used to describe features or elements that lie toward the head, while inferior refers to body parts that lie away from the head. The terms proximal and distal are generally used in association with the limb bones. Proximal refers to the portion of bone that is nearest to the axial skeleton, or articulation point. Conversely, distal refers to the portion of bone that is furthest away from the axial skeleton or articulation point. Lastly, the term “cranial” refers to the bones of the skull, and the term “postcranial” refers to all of the bones located below the skull. For an illustration of these descriptions, please see Fig. 3.1.
The figure depicts “standard anatomical position” with the body facing forward, arms extended along the side of the body, palms facing up, legs extended, and toes pointing forward. Also illustrated are the three planes of reference and anatomical directional terminology.
At birth the juvenile skeleton is comprised of roughly 450 ossification centers or elements. Extending from fetal life, these elements continue to mature and grow throughout childhood and fuse together to eventually become the 206 bones found in a typical adult skeleton. These centers include both primary and secondary centers of ossification. The primary centers are the initial sites of ossification, and the majority appear during the embryonic and fetal periods [6]. In some cases, secondary centers of ossification develop, including the proximal and distal ends of the long bones and rib tubercles. These centers appear later, most often after birth [6]. The long limb bones and the tubular bones of the hands and feet form from both primary and secondary centers of ossification. The primary and secondary centers are separated by an organized region of rapid growth that includes the growth plate, epiphyseal plate, and physis, and eventually fuse together to form the whole bone [6]. Many bones such as the cranial bones and the bones of the wrists and ankles form from one or several primary centers of ossification.
Bones are comprised of different types of bones (Fig. 3.2). The smooth, hard, outer portion of bone is known as cortical or compact bone. Sponge-like bone is located within the interior of bone and occurs at the ends of long bones and the vertebral bodies, and between the inner and outer layers of the cranial bones. This type of bone is collectively referred to as cancellous or trabecular bone, and within the cranial vault, it is called the diplöe. Living bone is covered by a layer of vascularized tissue called the periosteum. The inner surface of bones is lined with a cellular membrane call the endosteum. The periosteum and endosteum are osteogenic tissues that contain bone-forming cells and work together to allow bone to grow appositionally. The periosteum is thicker during childhood as the bone-forming cells are numerous and active because of the growing and developing bones [4, 6]. In adulthood, these cells reduce in number but remain active for remodeling and maintenance [4].
Three structures that characterize long bones include the diaphysis, epiphyses, and metaphyses (Fig. 3.2). The diaphysis is considered the shaft and is the portion that comprises the majority of the total length of the long bone. At either end of the diaphysis are the metaphyses. Finally, the epiphyses cap both ends of the diaphysis at the site of the metaphyses. During growth, the diaphysis is considered the primary center of ossification (largely because, in long bones, it is the first structure to appear). The epiphyses that cap either end of the diaphysis are considered secondary centers of ossification, because they form later. Throughout growth, these elements slowly grow together at the site of the growth plate, epiphyseal plate, and physis to form the final element recognized in the adult skeleton [6]. It should be noted that some elements cannot be identified through these three structures (diaphysis, metaphyses, and epiphyses). For example, the bones of the cranial vault form from their own separate primary ossification centers and eventually join the other cranial bones at junctions called sutures.
3.3 Overview of Bone Growth and Development
All bone growth is the result of bone deposition and replacement on a preexisting connective tissue [5]. Osteogenesis, the process of laying down new bone, occurs in two distinct phases in the developing skeleton through intramembranous and endochondral ossification. The bones of the cranial vault, in particular the frontal and parietal bones and the clavicle in the postcrania, are formed by apposition on a primitive mesenchymal tissue, which is an embryonic connective tissue. Most skeletal elements form through endochondral ossification, which is a cartilaginous precursor or model. Essentially, whether bones are formed intramembranously or endochondrally, they are formed on a preexisting “blue print.” During the early phase of development, in utero, the skeleton is flexible being composed mostly of a cartilage precursor, which is best for rapid growth and as a rigid frame is unnecessary during this phase of development.
3.3.1 Embryology
At the time of conception, the fertilized egg, or zygote, undergoes a series of mitotic divisions and eventually becomes known as a blastocyst. During this period, the zygote travels down the fallopian tube and, by the end of the first week, has converted into a blastocyst and has begun embedding itself into the uterine lining [7]. By the second week after fertilization, the blastocyst is completely implanted and cell division occurs that gives rise to the embryonic disc that is characterized by the formation of the primitive streak, notochord, and three primary germ layers from which all the structures of the body eventually develop. These three germ layers include the ectoderm, mesoderm, and endoderm. The ectoderm is the outer layer from which the epidermis (hair, nails, and skin), the sensory organs, and the brain and spinal cord arise. The middle layer is the mesoderm, from which the bones, muscles, connective tissues, and circulatory system arise. Lastly, the endoderm is the inner layer from which the epithelial linings of the digestive tract and respiratory passages arise. All major organs and systems of the body form from these three germ layers [7]. Ultimately, the skeletal system forms from the mesoderm.
The establishment of the germ layers begins with a band called the primitive streak. Shortly after the primitive streak appears, cells from within the primitive streak form mesenchyme, a loose network of embryonic connective tissue. Mesenchymal cells leaving the primitive streak eventually migrate to the various sites of osteogenesis where they proliferate and differentiate into various cell types, including fibroblasts, chondroblasts, and osteoblasts [7]. At the beginning of the third week, the notochord, a cellular rod that defines the primitive axis of the embryo and provides support, develops from mesenchymal cells released by the primitive streak. The notochord forms the central axis from which the vertebral column and the neural tube will form.
On both sides of the notochord is a column of mesoderm that becomes divided into cuboidal segments called somites. Somites develop throughout the third week of gestation and are prominent during the fourth and fifth weeks and eventually form the vertebrae, head, and trunk (the bones of the axial skeleton).
Models of the bones are initially formed by condensations of mesenchymal cells. Some bones develop directly from the mesenchyme through intramembranous bone formation, while other bones develop from the transformation of mesenchyme into cartilage bone models that are eventually ossified through the process of endochondral ossification. The mesoderm of the developing embryo condenses and gives rise to the mesenchyme, the embryonic connective tissue that ultimately forms all other connective tissues, including cartilage and eventually bone. These mesenchymal cells migrate to sites of future osteogenesis and differentiate into bone (intramembranously) or into cartilage (endochondrally) and ultimately form the “blue print” or ossification centers from which bone growth commences.
3.3.1.1 Intramembranous Ossification
Bones formed through intramembranous ossification do not begin with a cartilaginous precursor. Bones formed this way include the flat cranial bones, the mandible, and the clavicle. As the mesenchyme condenses, the first sign of ossification is the penetration of a blood vessel. At this time, cells differentiate into osteoblasts (bone-forming cells) and are deposited to form a network of spicules around which collagen fibers are deposited [8, 9]. Calcium salts, phosphates, and other inorganic salts then accumulate around the spicules. These fibers continue to form frameworks of spicules and calcify. As the calcification continues, the framework forms spongy bone. Some osteoblasts become trapped within the matrix and transform into osteocytes (bone cells) and help make up the spongy framework. Meanwhile the remaining osteoblasts stay on the periphery and continue laying new bone, creating layers around vascular channels that become the Haversian systems [6, 8, 9]. Osteoblasts work together with osteoclasts (bone-removing cells) to shape the growing bone tissue through bone deposition and removal.
3.3.1.2 Chondrification
Bones that form from a cartilaginous precursor must first go through chondrification, the process of transforming the mesenchyme bone model into cartilage. Cartilage develops when mesenchyme condenses and the cells proliferate and become rounded. As the cells differentiate, they form two layers, an outer one composed of fibroblasts and an inner one capable of differentiating into cartilage [8]. Together these layers form the perichondrium that covers the surface of the cartilage bone model. Chondroblasts, which are responsible for appositional growth, are found within the inner layer of the perichondrium [6].
Cartilage grows by both interstitial and appositional growth. The cells within the newly developed mass continue to divide and lay down more cartilaginous matrix through the process of interstitial growth. Appositional growth occurs when cells within the perichondrium differentiate and deposit layer after layer of cartilage on the outer surface of the model.
3.3.1.3 Endochondral Ossification
Endochondral ossification is characterized by bone formation that occurs from a preexisting cartilaginous precursor. Initially, the perichondrium of the cartilage model thickens, gives rise to osteoblasts (bone-forming cells), and eventually transforms into the periosteum of the ensuing bone [6]. The osteoblasts initially released by the perichondrium form a bone collar around the midshaft. Next, ossification within the core of the cartilage model begins as the chondrocytes (cartilage cells) swell up and calcium salts are deposited, ultimately forming calcified cartilage [6, 8]. The cartilaginous bone model continues to calcify, is invaded by a system of blood vessels, and then is occupied by osteoblasts and osteoclasts that eventually remodel the mineralized cartilage to form cancellous bone [6]. The osteoblasts deposited on the outer portion of bone form the hard surface known as cortical bone. For an illustration of endochondral ossification, please see Fig. 3.3.
As short bone develops (particularly those that form from a primary center of ossification, i.e., bones of the wrist and ankle), the core of the cartilaginous template ossifies through osteoclast and mineral salt deposition, while at the same time the cartilage continues to grow appositionally [8]. Eventually, the bone formation occurring at the core of the bone will consume the cartilage and form the adult bone.
Endochondral ossification begins on a preexisting cartilage model. The perichondrium produces osteoblasts that form a bone collar and transforms into the periosteum. Cartilage within the center of the cartilage model begins to calcify, becoming the primary center of ossification. Blood vessels then penetrate the bone collar and the secondary centers begin to calcify. Osteoclasts found in the endosteum remove the calcified cartilage to form the medullary cavity as osteoblasts in the periosteum deposit bone on the outside.
3.3.1.4 Fusion of Ossification Centers
As mentioned earlier, the initial site of ossification is the primary center. The primary center (diaphysis) does not always extend the entire cartilaginous precursor, and in some regions, separate secondary centers of ossification (epiphyses) will develop. At the site of the periosteum on the diaphysis, osteoblasts cause the shaft to grow in thickness. At the same time, a cavity is formed in the center of the bone by osteoclasts. This cavity eventually becomes the medullary cavity within which blood-forming cells and fat are stored (see Fig. 3.3). The shaft of the bone continues to grow larger in diameter through appositional growth on the outside of the shaft and removal of bone within the center.
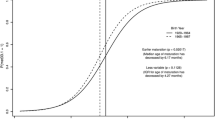
At the ends of the diaphysis, the cartilage continues to grow appositionally, while other centers of ossification (secondary) appear at the ends of the future bone. These secondary centers are referred to as epiphyses. A zone of cartilage known at the epiphyseal plate (growth plate) separates the metaphysis of the diaphysis from the epiphysis. This region allows the long bone to increase in length [6]. During childhood the cartilage of the epiphyseal plate continues to grow in thickness, while at the same time ossification proceeds outward from the diaphysis. Eventually, the ossification proceeding from the diaphysis will overcome and consume the cartilage of the epiphyseal plate and form a union between the diaphysis and the epiphysis [6, 8] (see Fig. 3.4). The union or closure of the epiphysis and diaphysis marks the end of growth in length of that bone.
The overall timing of epiphyseal fusion and closure varies in different parts of the skeleton and aids in determining the age of an individual. The reader should consult books such as Baker et al. (2005), Scheuer and Black (2000), and Scheuer et al. (2008) for exact timing.
The growth plate that separates the epiphysis from the diaphysis is a zone of cartilage that grows in thickness throughout childhood. Bone maturing from the direction of the diaphysis eventually consumes the thickening cartilage and forms a union between the diaphysis and the epiphysis. This growth allows long bones to increase in length.
3.4 Major Differences Between the Adult and Juvenile Skeleton
Anatomically and morphologically speaking, the juvenile skeleton is very different from the adult skeleton because it is in a constant state of change. At birth, there are about 450 centers of ossification present. These centers eventually ossify and fuse to form the 206 bones that are typically found in the adult human. This process of bone growth and development begins during the fetal life and does not finish roughly until the mid-20s. The juvenile skeleton is different from the adult skeleton in terms of morphology primarily because the young skeleton has not fully fused. At various developmental stages, the juvenile skeleton will have different numbers of elements as the appearance and ossification of the centers change.
The physiology of the juvenile skeleton also differs greatly from that of an adult. This is primarily because the bone is still forming and growing. The juvenile skeleton is characterized by a thick periosteum. The periosteum is the connective tissue covering the outside of bone and aids in bone formation and repair. It bridges the gap between broken segments of bone after a fracture occurs by producing cartilage and/or bone-forming cells. Since the periosteum is responsible for growth and for aiding in the repair of fractures, the juvenile skeleton heals a great deal faster than that of an adult because the actions associated with fracture repair are already present in excessive amounts in the developing skeleton [4].
It is also important to note that the biomechanics are also different. Young bone is more porous and more flexible than adult bone. This is because the Haversian canals occupy a greater portion of the cortex [4]. Because of its construction, a child’s bone can withstand a great deal more pressure than an adult bone before breaking. In fact, the bones in a child’s forearm can be bent up to 45 degrees before the sound of a fracture is heard [4]. This is due to the greater thickness and strength of the periosteum in the growing juvenile skeleton. In addition, the young bone is composed of more collagen, which allows it to be more flexible and elastic. Additionally, the cartilaginous composition of the growing bone also helps withstand outside pressures as the cartilaginous matrices hold together large volumes of fluid, making it resistant to compression [10]. Once fully developed, the adult skeleton loses its elasticity and turns to a state of remodeling and maintenance where a thick periosteum is no longer needed [8].
3.5 Environmental and Nutritional Factors Influencing Growth
Growth is the product of genetic potential, the environment, and the interaction between the two. At the time of conception, the embryo contains the genetic blueprint that includes a person’s potential for achieving a particular adult size and shape; the environment alters this potential [10, 12–14]. As such, a growing child can be adversely affected by diet, socioeconomic resources, and/or poisons in the atmosphere. While poor nutrition may have an adverse effect on growth, one must keep in mind that there are numerous factors that can impair growth that may not necessarily be due to child maltreatment including disease and infection [13].
Proper nutrition is essential for individuals to achieve a normal growth pattern and maximize their potential as adults [11–13]. According to Sinclair and Dangerfield [8], in the first year of life, a baby requires about twice as many calories per unit weight as an adult male engaged in moderately heavy work. Nutritional needs during adolescence may be higher than at any other time during life, and malnourished children may exhibit delayed growth and puberty [13]. However, the growth response will vary depending on the type, intensity, and duration of the nutritional insult [13]. Undernourishment can lead to a cycle in which an undernourished child becomes more susceptible to infection and illness, and once ill, requires more nourishment, and if it is not received, becomes a downward spiral [13]. One of the earliest responses to limited food is growth retardation [13]. When a child is undernourished, the development of the teeth takes precedence over the growth of the bones [8]. Since the teeth are an accurate indicator of age, comparison of the teeth and bone development may yield information regarding the health of a child. A balanced diet that includes vitamins and minerals is essential during childhood to support health bone growth.
A balanced diet includes a variety of foods containing minerals and vitamins including calcium, vitamin D, phosphorus, magnesium, vitamin C, as well as proteins [9]. Calcium is important for several bodily systems, makes up approximately 70% of the composition of bone, and is essential for bone formation [9]. Therefore, consuming foods with calcium is important for the growth and maintenance of bone tissue and for proper functions of the heart, muscles, and nervous system. Bones are the storage vaults from which the body draws calcium. If the body does not have enough calcium for other systems in the body, the body will leach calcium from bone and over time will cause the bones to become thin and weak. Phosphorus works with calcium to strengthen and maintain bone and teeth. In addition, phosphorus aids in the conversion of food into energy [9].
Vitamin D works with calcium and phosphorus. It improves the rate of calcium and phosphorus absorption from the intestine and essentially increases their amounts in the bloodstream, making calcium readily available to perform bodily functions [9]. Therefore, if vitamin D is deficient, so may be calcium. An inadequate supply of calcium in the bloodstream will cause the body to leach out the calcium stored within bone. If vitamin D is deficient, bone will fail to mineralize and, as a result, children may develop rickets. It ultimately causes distorted growth of the epiphyseal plate. If persistent, it will ultimately lead to softened bones that become bent under the weight of the body [8].
Magnesium stimulates the production of calcitonin, a hormone that works with other hormones in the body to raise calcium levels in the bones and prevent calcium from being absorbed into other parts of the body. In addition, magnesium also reduces acid levels in the blood. Bone loss occurs more severely when blood is more acidic [9].
Vitamin C aids in the growth and maintenance of healthy bones, teeth, gums, ligaments, and blood vessels. Vitamin C deficiency causes the intercellular substance of bone to become inadequately formed and can eventually form scurvy [8]. It may cause a decreased growth rate at the epiphyseal plates and deficient bone formation elsewhere.
Protein-energy malnutrition can ultimately lead to conditions known as kwashiorkor and marasmus [13], which are characterized by slowed skeletal growth and maturation. In fact, epiphyseal union may be delayed as much as a year compared with that in properly nourished children [8].
3.6 Summary
This chapter has provided a brief overview of juvenile skeletal anatomy and growth and development. The juvenile skeleton is characterized as a nutrition-dependent and rapidly growing phase. Children’s bones are different from adult bones, and those having taken courses only in adult human osteology may have difficulty distinguishing juvenile human remains from nonhuman remains, may have difficulty identifying the various structures and bones of the juvenile skeleton, and may not accurately assess the remains. Since the juvenile skeleton is different from the adult skeleton, it is essential for investigators of child maltreatment to become familiar with juvenile skeletal anatomy and understand what is considered normal variation.
Suggested Reading
Baker BJ, Dupras TL, Tocheri MW. The Osteology of Infants and Children. College Station, TX: Texas A&M University Press, 2005
Scheuer L, Black S, Schaefer MC. Juvenile Osteology: A Laboratory and Field Manual. San Diego, CA: Academic, 2008
Scheuer L, Black S. The Juvenile Skeleton. San Diego, CA: Elsevier Academic Press, 2004
References
Center for Disease Control, National Center for Injury Prevention and Control. Child Maltreatment: Facts at a Glance. 2010 http://www.cdc.gov/violencePrevention/childmaltreatment/
U.S. Department of Health and Human Services, Administration for Children and Families, Administration on Children, Youth and Families, Children’s Bureau. Child Maltreatment. 2008 http://www.acf.hhs.gov/programs/cb/stats_research/index.htm#can
Baker BJ, Dupras TL, Tocheri MW. The Osteology of Infants and Children. College Station, TX: Texas A&M University Press, 2005
Rang M, Wenger D. Children Are Not Just Small Adults. In: Rang M, Wenger DR, Pring ME, editors. Rang’s Children’s Fractures, 3rd Ed. Philadelphia, PA: Lippincott Williams & Wilkins, 2005; 1–10
White TD. Human Osteology, 2nd Ed. San Diego, CA: Academic, 2000
Scheuer L, Black S. Developmental Juvenile Osteology. San Diego, CA: Academic, 2000
Moore KL, Persaud TVN. The Developing Human, 5th Ed. Philadelphia, PA: W.B. Saunders Company, 1993
Sinclair D, Dangerfield P. Human Growth after Birth, 6th Ed. Oxford: Oxford University Press, 1998
Kelly E. The Skeletal System. Westport, CT: Greenwood Press, 2004
Hall BK. Bones and Cartilage: Developmental and Evolutionary Skeletal Biology. San Diego, CA: Elsevier Academic Press, 2005
Cameron N. Human Growth Curve, Canalization, and Catch-Up Growth. In: Cameron N, editor. Human Growth and Development. Amsterdam: Academic, 2006; 1–20
Lejarraga H. Growth in Infancy and Childhood: A Pediatric Approach. In: Cameron N, editor. Human Growth and Development. Amsterdam: Academic, 2006; 21–44
Norgan NG. Nutrition and Growth. In: Cameron N, editor. Human Growth and Development. San Diego, CA: Academic, 2006; 139–164
Schell LM, Knutson KL. Environmental Effects on Growth. In: Cameron N, editor. Human Growth and Development. San Diego, CA: Academic, 2006; 165–195
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2011 Springer Science+Business Media, LLC
About this chapter
Cite this chapter
Humphries, A.L. (2011). Basic Juvenile Skeletal Anatomy and Growth and Development. In: Ross, A., Abel, S. (eds) The Juvenile Skeleton in Forensic Abuse Investigations. Humana Press. https://doi.org/10.1007/978-1-61779-255-7_3
Download citation
DOI: https://doi.org/10.1007/978-1-61779-255-7_3
Published:
Publisher Name: Humana Press
Print ISBN: 978-1-61779-254-0
Online ISBN: 978-1-61779-255-7
eBook Packages: MedicineMedicine (R0)