Abstract
For decades, school-based programs have constituted the primary approach for addressing the childhood obesity epidemic at the population level. School programs have the potential to reach many children and affect many factors in the causal path to obesity (i.e., diet, physical activity, knowledge, and other psychosocial factors); in theory, they have great promise for long-term sustainability through institutionalization of intervention components.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Key Words
Introduction
For decades, school-based programs have constituted the primary approach for addressing the childhood obesity epidemic at the population level. School programs have the potential to reach many children and affect many factors in the causal path to obesity (i.e., diet, physical activity, knowledge, and other psychosocial factors); in theory, they have great promise for long-term sustainability through institutionalization of intervention components (1–4).
On the other hand, the effectiveness of school-based interventions has for the most part been disappointing. Most school programs have been associated with only modest impacts on childhood behavior and weight gain (5–8). Some success has been observed in school intervention trials that have had strong program champions, but the beneficial effects in children are often reversed if staff members who championed the program leave the school (9,10). These findings have led us and other investigators to question the school-centered approach to child obesity prevention (11–15). One of the primary critiques has been that school-centered programs are unlikely to be successful if not heavily reinforced by strong interventions in the community.
Children are influenced by the wide range of choices and factors that constitute the food and physical activity environments outside of schools; these include the presence and proximity of retail food stores, the availability of prepared and “fast” foods, the variety and quantity of foods available and served within the home, and the accessibility of parks and recreation centers. Parents and other caregivers can influence greatly the foods consumed by their children, particularly at a young age (16,17). In recent years, a growing number of school-based intervention trials have sought to expand beyond the confines of the school to engage the broader community. We term these interventions “school–community programs.” In addition to school-based interventions, they include community and family components that invoke community involvement, nutrition environment intervention near schools, and family education and participation. Here we review the literature on “school–community” intervention trials to answer three questions:
-
(1)
What types of “school–community intervention trials” are found in the literature? How do these programs vary in terms of program components, emphasis on school versus community, strategies, and study size, etc?
-
(2)
How successful have “school–community” programs been? What components appear to be most successful overall?
-
(3)
What are future directions for school-based and school–community programs to prevent childhood obesity?
To identify the relevant literature for school–community programs, we conducted a literature search for the years from 1990 to 2009 using Medline, PubMed, PsycINFO, and the Cochrane Database of Systematic Reviews. The following inclusion criteria were used to select articles for the review: (1) selected studies should have both school-based intervention programs and substantial components outside the school aimed at preventing childhood obesity; (2) the overall goal of studies should be preventing unhealthy weight gain or obesity among children through increased physical activity, better nutrition, and/or environmental policy changes in schools and communities; (3) evaluation outcomes must include obesity, physical activity, and/or energy intake to be included in this review. We excluded studies that sent home materials and/or had activities within the school for family members as their primary form of community engagement (e.g., Pathways (18), CATCH (19)). In addition, recent review articles (2000–2007) on school-based and community-based childhood obesity prevention program were manually checked to be sure that any studies mentioned in the reviews would meet the inclusion criteria for this study. A total of eight intervention studies were found matching these criteria and 22 articles were reviewed. Additional searches were performed to identify the relevant literature for school–community-based diabetes prevention studies. Two additional studies were reviewed and included in the tables.
Therefore, a total of ten intervention studies were reviewed. In addition to reference to published articles, we contacted the lead authors when information was missing and included the information provided by the authors to provide a more complete description of the studies.
Summary of the Literature
Summary of Articles of School–Community Programs for Obesity Prevention
Tables 1 and 2 summarize our findings from the review of the literature. Table 1 describes the background, target population, and intervention approach of each program. Table 2 outlines the methods of evaluation used and the primary results and recommendations.
General Description of the Intervention Trials
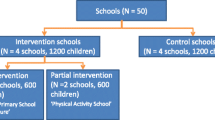
Of ten studies reviewed, six were implemented in the USA, one in Canada, one in Australia, one in New Zealand, and one in France. The intervention periods ranged from 1 to 3 years, with two exceptions (9,28). With the exception of one study by Perman and colleagues (27), all interventions were controlled trials with comparison groups; three of the studies (TAAG (10), SNPI (34), Switch (38)) randomly assigned schools as intervention and control.
One study conducted in France, titled Fleurbaix-Laventie Ville Santé (FLVS (26)), has a different approach than others included here. Unlike the other studies, which were designed as school–community interventions, the French study was initiated in 1992 as a school-based nutrition education intervention and evolved into a school–community intervention beginning in 1999. The program was still ongoing in 2007 when the evaluation paper was published; the reviewed paper summarized the intervention effect through 2004.
Target Populations
Most of the studies reviewed here targeted elementary school students, most of whom ranged from 4 to 12 years of age. SNPI study targeted 4th–6th graders, whereas, SUS mainly focused on 1st–3rd graders. TAAG worked mainly with middle school girls and ZDPP study targeted high school students.
The trials included in this review included children from a wide range of ethnic groups. Many of the studies focused on low-income populations; for example, the two studies designed to reduce diabetes risk factors were conducted in American Indian and First Nation children (9,29). Of the remaining seven investigations, two specifically targeted populations with relatively lower socio-economic status. Jumpin’ Jaguars worked with one elementary school in a community in which 57% of households earned less than $10,000 annually; among participating children, 80% were either African-American or Hispanic (27). Similarly, more than 50% of the SNPI participants were eligible for federally subsidized, free, or reduced-price meals. The majority were ethnic minorities: 44% African-American, 17% Asian, and 22% Hispanic children (34). On the other hand, the BAEW study population (Australia) and the Switch population were mostly white (25,39).
Theoretical and Participatory Approaches
Not surprisingly, all ten studies mentioned community engagement as a key component of the formative phase of the intervention. The TAAG study obtained detailed information on formative research with community and school members as well as youth and family members (40–44). The SUS and the SNPI formed advisory councils to assist in assessing community needs and designing the program (34,35). The community-based intervention components in the FLVS study were proposed by community members and organizations that had previously participated in an earlier school-based nutrition education intervention in the community. The communities themselves suggested and organized events for increasing physical activity levels targeting whole communities (26). Lastly, all the diabetes prevention studies in native communities emphasized partnership between research teams and community leaders for a successful intervention; this is well documented in KSDPP (28,30,49).
Intervention Components Inside and Outside Schools
All the studies included in this review have both school-based and out-of-school components (Table 3). While studies that solely emphasized family materials/workshops were not considered sufficient for inclusion, most investigations included parent outreach programs and events (except TAAG (10)). Most of the studies (7/10) included policy and environmental changes as components of school-based programs. For example, the SNPI study (34) used a coalition of community-based organizations to focus on changing food and nutrition environments in schools. After-school programs were incorporated to increase physical activity levels [BAEW (25), SUS (35), TAAG (10), and APPLE (20)] and to target overweight or obese children by collaborating with other local agencies [Jumpin’ Jaguars (27)].
The types and intensities of community programs varied considerably (Table 3). However, more than half of the studies (6/10) endeavored to change the food environments in their communities. For example, the SUS study devoted a substantial part of the intervention to developing community gardens and farmers’ markets and recruiting SUS “approved” restaurants in the city (35). SNPI also worked with local food stores to help customers identify healthier food options by providing point of purchase information (34). Half of the studies (5/10) focused on environmental factors that encourage physical activity in communities. With the support of the town councils, the FLVS study led to the construction of new sporting facilities; new sport educators were employed as a part of the intervention (26). The KSDPP study held various promotional events on increasing physical activities targeting the whole community (28). The SUS study worked closely with the city government to increase walkability and bikeability in the community (35).
Most of the interventions (8/10) worked closely with various local stakeholders. The TAAG study implemented intervention components for increasing physical activity among girls both on and off school property, working with small advisory groups of school staff and community organizations and members. Community organizations, such as the YMCA or YWCA, local health clubs, and community recreation centers, were identified in intervention schools and invited to plan and implement programs and events. Moreover, the study recruited and trained Program Champions from intervention schools and communities to take ownership of the program for the purpose of sustainability after researchers from outside the community leave the study (10). The Jumpin’ Jaguars study enlisted the support of various local community-based organizations (e.g. YMCA, Community Trust Bank, and God’s pantry) for their after-school program (27). Lastly, the SNPI study worked with local food stores to promote intake of healthy foods (34). The SUS trained local physicians and clinic staff to increase awareness of childhood obesity and formed collaborations with ethnic-minority group in the community (35). The Zuni Diabetes Prevention Program (ZDPP) developed supportive social networks by forming a Teen Task Force, which helped to recruit youth participants into the study and served as peer mentors for other students (9). Three of ten studies included collaboration with local health offices or support from government organizations. For example, the BAEW strategies were incorporated into the Municipal Public Health Plan and Integrated Health Promotion Plan (25). Most studies (7/10) reported that the intervention attempted to reach the whole community in order to increase awareness of the programs through various mass media campaigns.
Process Evaluation
Most of the studies (8/10) collected process evaluation data [except (27,26)], with great variation in methods and documentation. Process evaluation measures included changes in schools’ and in communities’ environments as well as dose, reach, and fidelities of intervention activities (28,35,45). Two papers from the SUS study presented the results of food environment modification efforts in the community, focusing on food service at schools and local restaurants (36,37).
Psychosocial Measures and Behavioral Impacts
We compared the forms of evaluation used by the different trials. Psychosocial factors were measured in more than half of the studies reviewed. The BAEW (25) and the SNPI (34) studies administered body dissatisfaction questionnaires to monitor adverse effects of the interventions. The KSDPP (28), Switch (39), TAAG (46), and ZDPP (9) studies measured psychosocial factors such as self-efficacy, outcome expectations, knowledge, perceptions, and/or attitudes.
Seven studies measured both dietary intake and physical activity. The TAAG study measured only physical activity levels among participating girls using accelerometers and observations (10). FLVS and Jumpin’ Jaguars did not include behavioral assessments (27,26). Most of the studies of physical activity level and dietary intake used self-reported questionnaires. Some specific behaviors, such as intake of fruits and vegetables or screen time, were reported separately in some studies [KSDPP (29), Switch (39), and ZDPP (9)].
Health Outcomes
BMI and BMI z-scores were the most common health outcomes measured. In addition, some studies included other anthropometric measures such as waist–hip ratio, percent body fat, and physiological measures such as blood pressure and pulse rate. Overweight or obesity prevalence and incidence were also reported in some studies [FLVS (26), SNPI (34)].
Community Measures
Impacts at the community level were assessed in some trials. One study measured sustainability of the program effect after 2 years of program completion by interviewing school principals [APPLE (22)]. Other studies (28,45,36) mentioned environmental and policy changes as a measure of the impact of intervention. The Switch study performed community surveys before and after the intervention to measure the changes on community awareness of the study’s target healthy behaviors (38). The SUS study team described efforts to change food environments in restaurants and schools. The compliance rate of restaurants that followed approval criteria was not high (∼50%); however, school food environments improved after implementation, with increased availability of fruits, vegetables, whole grains, and low fat dairy products (36,37).
Study Results
Impact on Psychosocial Factors and Behavior
Three studies assessed the psychosocial impacts of intervention: two studies found no increase in body dissatisfaction or eating disorders among participants [BAEW (25), SNPI (34)], and one study reported that participants perceived positive changes in their behaviors (39).
Among five studies that reported nutrition-related behavioral changes, three had positive results (9,20,39) while two found no changes in dietary intake (34,29). The APPLE project documented lower consumption of carbonated beverages and higher consumption of fruit among intervention children and the ZDPP noted lower consumption of sugared beverages. Lastly, the parents of children from the Switch intervention communities reported higher consumption of fruits and vegetables (39). Only one study reported dietary results at the nutrient level (KSDPP); no significant impacts were observed.
Among five studies that reported effects on physical activity, four had a positive impact. The APPLE intervention increased physical activity level (20), SNPI and Switch reduced sedentary behavior (34,39), and the TAAG study increased the activity levels of adolescent girls (10). The KSDPP study showed increases in physical activity during the initial study period (1994–1999); however, these changes were not sustained in a 3-year follow-up (29).
Impact on BMI and Anthropometric Measures
Six of the ten studies demonstrated positive albeit small impacts on BMI and related anthropometric measures (Table 4). Children undergoing the BAEW intervention gained less weight and had smaller increases in waist circumference, BMI z-score, and waist–hip ratio than children in the comparison group. Even though the program did not analyze changes in the prevalence and incidence of overweight and obesity between intervention and comparison groups, the changes in BMI and other anthropometric measures are encouraging (25). The SUS (35) and the APPLE project also showed promising outcomes (20,22): mean BMI z-scores were reduced. Moreover, BMI z-scores and the prevalence of overweight remained lower in the APPLE intervention group for 2 years. The SNPI program (34), which focuses on changing nutrition environment at schools, showed that the predicted odds of incidence and prevalence of overweight were lower for the intervention group. The KSDPP showed some early positive effects on skinfold thickness but not on BMI or fitness (29). Glucose/insulin ratios were increased in the ZDPP study; the significance of this finding is unclear without proper comparison groups and without controlling for other factors in the analysis (9).
Impact on Community
Most of the studies sought to work with community groups to reduce unhealthy weight gain or diabetes risk factors; however, little information on how the intervention changed communities was found in the papers. One follow-up study of APPLE explicitly addressed sustainability issues: whether the intervention components in schools and communities were still in place 2 years after program cessation (50). Some studies mentioned that they followed environmental and policy changes in communities as part of process evaluation but results were not documented [e.g., KSDPP (38), TAAG (26)].
Discussion
Our review of the literature identified a limited number of school-based obesity prevention programs that had a substantial community component. It is clear that a great deal of work remains to expand this area of intervention research as a means of addressing the child obesity epidemic. Some large-scale interventions with extensive community involvement are underway: the SUS study is being replicated in six urban communities in the USA (renamed BALANCE) and is being adapted and implemented in eight rural communities in the USA (renamed CHANGE) (51). We expect to see more evaluation results in a few years; this should provide more definitive information regarding the effectiveness of school–community intervention programs. Nevertheless, on the basis of the work reviewed, some limited conclusions can be drawn.
In general, the school–community trials reviewed in this chapter have had a limited but significant impact in reducing BMI z-scores or obesity rates in children. Limited success has also been achieved with efforts to change food and physical activity environments in order to increase the choices available to children and their caregivers, such as working with food stores to increase the availability of healthy foods. However, more work needs to be done to tie these school-external changes to those that have been made to curriculum and to activities within the schools so that children and their adult caregivers are aware of the changes made.
It should be noted that eight of the ten studies we reviewed were conducted in elementary school children; the two studies of teenagers found no effect on weight gain or fat mass, although the TAAG intervention increased activity levels in adolescent girls. The preferential responses of prepubertal children to a lifestyle intervention likely reflect greater parental supervision and tighter control of food intake and selection. Other studies have noted the difficulty in changing weight-related behaviors in obese adolescents (50,52,53).
Changing the environment around schools and in communities is enormously challenging and requires a great deal of focused effort and community support and engagement. Community engagement and participatory approaches are central features of the successful “school–community” intervention trials reviewed in this chapter. No single approach appears to have been highly effective, and in fact the level of engagement ranged considerably.
Many of the programs reviewed stressed and incorporated policy changes both inside and outside schools (34,25,35,20). Policy changes may be viewed as another form of community engagement. Policy changes would lead to institutionalization of program activities in schools and community settings, which may lead to long-term sustainability.
Serious deficiencies exist for most of the intervention trials reviewed in terms of evaluation methodologies. While the studies included community intervention components, there is significant room for improvement in assessing change at the community and environmental levels pre- and post-intervention. A further weakness is the lack of substantial process evaluation of each component of the intervention implemented in the community. These are major gaps that should be addressed in future trials of school–community programs. Furthermore, most of the studies did not provide data on the impact of their programs on dietary intake at the nutrient level. Behavioral outcomes like diet and physical activity are required to explain the mechanisms for change in weight status or lack thereof.
In addition, it is important to document and disseminate information regarding costs for future assessment of trials in this area. Only one study conducted a cost analysis (23); a second mentioned the total cost of intervention implementation (27). We contacted the original authors of the studies to gather more information on cost (Table 5). Due to the complex nature of school–community-based interventions, including variation in study size, geographical differences, and evaluation methods, it was challenging to make any comprehensive comparisons using the data provided by the authors. The variation that we observed was substantial: costs of intervention ranged from 2 euro (∼ 2.9 USD) to 429 USD per child per year. This can be explained by program differences. One was an intensive 2-year intervention beginning with building partnership with other stakeholders in the community to working with school cafeterias to alter food choices (23); the other capitalized on an established collaboration with the community and did not require many external resources (26).
Two studies found no adverse effects on children’s psychological health. Stigmatization of children in school-based programs is a potential concern and led to the termination of one reportedly successful approach that targeted overweight children (54,55). Only one of the ten studies reported here (Jumpin’ Jaguars) included a specific intervention for overweight children. On the one hand, the inclusion of the entire school population represents a strength of school–community programs. On the other hand, the lack of targeting may limit the effectiveness of school-based obesity interventions for overweight or high-risk children. More detailed investigation will be required to resolve this conundrum.
An additional challenge lies in the area of study design. We emphasized intervention strategy as the primary criterion by which we selected studies for this review; this enabled us to include many studies with various forms of school–community interventions. However, limitations in design of some of the studies (such as lack of a control group) weaken our ability to draw firm conclusions. In addition, many school-based studies, such as CATCH (19) and Pathways (18), took the unit of analysis and randomization as the school itself. This is not possible when extensive community engagement and changes become an additional focus of the intervention. Instead the unit of analysis becomes the community. Rigorous statistical analytical methods are needed to capture the unique aspects of community involvement and social engagement.
As noted, the reductions in mean BMI z observed in these studies were modest and variable, and the interventions are time consuming and, in some cases, expensive. Should we then abandon our efforts with school and communities and focus on targeting families and children at the highest risk for obesity and its complications? Strong evidence indicates that these targeted efforts can be effective (56,57). We would argue, however, that the sheer size, scope, and progression of the obesity epidemic will not permit us to focus our efforts solely on the small number at greatest risk.
To conclude, the experience with school-based interventions has been discouraging, and an emerging body of literature reveals strong associations between the obesogenic environment and the prevalence of childhood obesity. Our findings suggest that school–community interventions provide one possible solution to the problem. Ongoing studies with strong design and evaluation plans will provide more information regarding the efficacy and costs of school–community programs for prevention (and management) of childhood obesity. In the meantime, the positive trends noted in our review provide support for continued and expanded research trials that intervene in both schools and the communities that surround them.
References
Pyle S, Sharkey J, Yetter G, Felix E, Furlong M. Fighting an epidemic: the role of schools in reducing childhood obesity. Psychol Sch. 2006;43(3):361.
Caballero B. Obesity prevention in children: opportunities and challenges. Int J Obes Relat Metab Disord. Nov 2004;28(Suppl 3):S90–5.
Budd GM, Volpe SL. School-based obesity prevention: research, challenges, and recommendations. J Sch Health. Dec 2006;76(10):485–95.
Naylor PJ, McKay HA. Prevention in the first place: schools a setting for action on physical inactivity. Br J Sports Med. Jan 2009;43(1):10–3.
Brown T, Summerbell C. Systematic review of school-based interventions that focus on changing dietary intake and physical activity levels to prevent childhood obesity: an update to the obesity guidance produced by the National Institute for Health and Clinical Excellence. Obes Rev. Jan 2009;10(1):110–41.
Kropski JA, Keckley PH, Jensen GL. School-based obesity prevention programs: an evidence-based review. Obesity (Silver Spring). May 2008;16(5):1009–18.
Shaya FT, Flores D, Gbarayor CM, Wang J. School-based obesity interventions: a literature review. J Sch Health. Apr 2008;78(4):189–96.
Sharma M. School-based interventions for childhood and adolescent obesity. Obes Rev. Aug 2006;7(3):261–9.
Teufel NI, Ritenbaugh CK. Development of a primary prevention program: insight gained in the Zuni Diabetes Prevention Program. Clin Pediatr (Phila). Feb 1998;37(2):131–41.
Webber LS, Catellier DJ, Lytle LA, Murray DM, Pratt CA, Young DR, et al. Promoting physical activity in middle school girls: trial of activity for adolescent girls. Am J Prev Med. Mar 2008;34(3):173–84.
Gittelsohn J, Kumar MB. Preventing childhood obesity and diabetes: is it time to move out of the school? Pediatr Diabetes. Dec 2007;8(Suppl 9):55–69.
Peterson KE, Fox MK. Addressing the epidemic of childhood obesity through school-based interventions: what has been done and where do we go from here? J Law Med Ethics. Spring 2007;35(1):113–30.
Thomas H. Obesity prevention programs for children and youth: why are their results so modest? Health Educ Res. Dec 2006;21(6):783–95.
Lytle LA. School-based interventions: where do we go next? Arch Pediatr Adolesc Med. Apr 2009;163(4):388–9.
Lee A. Health-promoting schools: evidence for a holistic approach to promoting health and improving health literacy. Appl Health Econ Health Policy. 2009;7(1):11–7.
Savage JS, Fisher JO, Birch LL. Parental influence on eating behavior: conception to adolescence. J Law Med Ethics. Spring 2007;35(1):22–34.
Arcan C, Neumark-Sztainer D, Hannan P, van den Berg P, Story M, Larson N. Parental eating behaviours, home food environment and adolescent intakes of fruits, vegetables and dairy foods: longitudinal findings from Project EAT. Public Health Nutr. Nov 2007;10(11):1257–65.
Caballero B, Clay T, Davis SM, Ethelbah B, Rock BH, Lohman T, et al. Pathways: a school-based, randomized controlled trial for the prevention of obesity in American Indian schoolchildren. Am J Clin Nutr. Nov 2003;78(5):1030–8.
Edmundson E, Parcel GS, Feldman HA, Elder J, Perry CL, Johnson CC, et al. The effects of the Child and Adolescent Trial for Cardiovascular Health upon psychosocial determinants of diet and physical activity behavior. Prev Med. Jul–Aug 1996;25(4):442–54.
Taylor RW, McAuley KA, Barbezat W, Strong A, Williams SM, Mann JI. APPLE Project: 2-year findings of a community-based obesity prevention program in primary school age children. Am J Clin Nutr. Sept 2007;86(3): 735–42.
Taylor RW, Mcauley KA, Williams SM, Barbezat W, Nielsen G, Mann JI. Reducing weight gain in children through enhancing physical activity and nutrition: the APPLE project. Int J Pediatr Obes. 2006;1(3): 146–52.
Taylor RW, McAuley KA, Barbezat W, Farmer VL, Williams SM, Mann JI, et al. Two-year follow-up of an obesity prevention initiative in children: the APPLE project. Am J Clin Nutr. Nov 2008;88(5):1371–7.
Williden M, Taylor RW, McAuley KA, Simpson JC, Oakley M, Mann JI. The APPLE project: an investigation of the barriers and promoters of healthy eating and physical activity in New Zealand children aged 5–12 years. Health Educ J. 2006;65(2):135–48.
McAuley KA, Taylor RW, Farmer VL, Hansen P, Williams SM, Booker CS, et al. Economic evaluation of a community-based obesity prevention program in children: the APPLE project. Obesity (Silver Spring). Jan 2010;18(1):131–6.
Sanigorski AM, Bell AC, Kremer PJ, Cuttler R, Swinburn BA. Reducing unhealthy weight gain in children through community capacity-building: results of a quasi-experimental intervention program, Be Active Eat Well. Int J Obes (London). Jul 2008;32(7):1060–7.
Romon M, Lommez A, Tafflet M, Basdevant A, Oppert JM, Bresson JL, et al. Downward trends in the prevalence of childhood overweight in the setting of 12-year school- and community-based programmes. Public Health Nutr. Dec 2008;23:1–8.
Perman JA, Young TL, Stines E, Hamon J, Turner LM, Rowe MG. A community-driven obesity prevention and intervention in an elementary school. J Ky Med Assoc. Mar 2008;106(3):104–8.
Macaulay AC, Paradis G, Potvin L, Cross EJ, Saad-Haddad C, McComber A, et al. The Kahnawake Schools Diabetes Prevention Project: intervention, evaluation, and baseline results of a diabetes primary prevention program with a native community in Canada. Prev Med. Nov–Dec 1997;26(6):779–90.
Paradis G, Levesque L, Macaulay AC, Cargo M, McComber A, Kirby R, et al. Impact of a diabetes prevention program on body size, physical activity, and diet among Kanien’keha:ka (Mohawk) children 6–11 years old: 8-year results from the Kahnawake Schools Diabetes Prevention Project. Pediatrics. Feb 2005;115(2):333–9.
Potvin L, Cargo M, McComber AM, Delormier T, Macaulay AC. Implementing participatory intervention and research in communities: lessons from the Kahnawake Schools Diabetes Prevention Project in Canada. Soc Sci Med. Mar 2003;56(6):1295–305.
McComber AM, Macaulay AC, Kirby R, Desrosiers S, Cross EJ, Saad-Haddad C. The Kahnawake Schools Diabetes Prevention Project: community participation in a diabetes primary prevention research project. Int J Circumpolar Health. 1998;57(Suppl 1):370–4.
Jimenez MM, Receveur O, Trifonopoulos M, Kuhnlein H, Paradis G, Macaulay AC. Comparison of the dietary intakes of two different groups of children (grades 4–6) before and after the Kahnawake Schools Diabetes Prevention Project. J Am Diet Assoc. Sept 2003;103(9):1191–4.
Levesque L, Guilbault G, Delormier T, Potvin L. Unpacking the black box: a deconstruction of the programming approach and physical activity interventions implemented in the Kahnawake Schools Diabetes Prevention Project. Health Promot Pract. Jan 2005;6(1):64–71.
Foster GD, Sherman S, Borradaile KE, Grundy KM, Vander Veur SS, Nachmani J, et al. A policy-based school intervention to prevent overweight and obesity. Pediatrics. Apr 2008;121(4):e794–802.
Economos CD, Hyatt RR, Goldberg JP, Must A, Naumova EN, Collins JJ, et al. A community intervention reduces BMI z-score in children: shape Up Somerville first year results. Obesity (Silver Spring). May 2007;15(5):1325–36.
Economos CD, Folta SC, Goldberg J, Hudson D, Collins J, Baker Z, et al. A community-based restaurant initiative to increase availability of healthy menu options in Somerville, Massachusetts: shape Up Somerville. Prev Chronic Dis. Jul 2009;6(3):A102.
Goldberg JP, Collins JJ, Folta SC, McLarney MJ, Kozower C, Kuder J, et al. Retooling food service for early elementary school students in Somerville, Massachusetts: the Shape Up Somerville experience. Prev Chronic Dis. Jul 2009;6(3):A103.
Eisenmann JC, Gentile DA, Welk GJ, Callahan R, Strickland S, Walsh M, et al. SWITCH: rationale, design, and implementation of a community, school, and family-based intervention to modify behaviors related to childhood obesity. BMC Public Health. Jun 2008;29(8):223.
Gentile DA, Wlk G, Eisenmann JC, Reimer RA, Walsh DA, Russell DW, Callahan R, Walsh M, Strickland S, Fritz K. Evaluation of a multiple ecological level child obesity prevention program: switch what you Do, View, and Chew. BMC Med. Sept 2009;7(18):49.
Gittelsohn J, Steckler A, Johnson CC, Pratt C, Grieser M, Pickrel J, et al. Formative research in school and community-based health programs and studies: “state of the art” and the TAAG approach. Health Educ Behav. Feb 2006;33(1): 25–39.
Moe SG, Pickrel J, McKenzie TL, Strikmiller PK, Coombs D, Murrie D. Using school-level interviews to develop a Multisite PE intervention program. Health Educ Behav. Feb 2006;33(1):52–65.
Saunders RP, Moody J. Community agency survey formative research results from the TAAG study. Health Educ Behav. Feb 2006;33(1):12–24.
Vu MB, Murrie D, Gonzalez V, Jobe JB. Listening to girls and boys talk about girls’ physical activity behaviors. Health Educ Behav. Feb 2006;33(1):81–96.
Young DR, Johnson CC, Steckler A, Gittelsohn J, Saunders RP, Saksvig BI, et al. Data to action: using formative research to develop intervention programs to increase physical activity in adolescent girls. Health Educ Behav. Feb 2006;33(1):97–111.
Young DR, Steckler A, Cohen S, Pratt C, Felton G, Moe SG, et al. Process evaluation results from a school- and community-linked intervention: the Trial of Activity for Adolescent Girls (TAAG). Health Educ Res. Dec 2008;23(6):976–86.
Stevens J, Murray DM, Catellier DJ, Hannan PJ, Lytle LA, Elder JP, et al. Design of the Trial of Activity in Adolescent Girls (TAAG). Contemp Clin Trials. Apr 2005;26(2):223–33.
Treuth MS, Baggett CD, Pratt CA, Going SB, Elder JP, Charneco EY, et al. A longitudinal study of sedentary behavior and overweight in adolescent girls. Obesity (Silver Spring). May 2009; 17(5):1003–8.
McKenzie TL, Catellier DJ, Conway T, Lytle LA, Grieser M, Webber LA, et al. Girls’ activity levels and lesson contexts in middle school PE: TAAG baseline. Med Sci Sports Exerc. Jul 2006;38(7):1229–35.
Cargo M, Levesque L, Macaulay AC, McComber A, Desrosiers S, Delormier T, et al. Community governance of the Kahnawake Schools Diabetes Prevention Project, Kahnawake Territory, Mohawk Nation, Canada. Health Promot Int. Sept 2003;18(3):177–87.
Whitlock EA, O’Connor EP, Williams SB, Beil TL, Lutz KW. Effectiveness of weight management programs in children and adolescents. Evid Rep Technol Assess (Full Rep). Sept 2008;170:1–308.
Children in Balance. Research and Projects. Available at: http://www.childreninbalance.org (2009). Accessed 20 Aug 2009.
Oude Luttikhuis H, Baur L, Jansen H, Shrewsbury VA, O’Malley C, Stolk RP, et al. Interventions for treating obesity in children. Cochrane Database Syst Rev. 21 Jan 2009;1:CD001872.
Summerbell CD, Waters E, Edmunds LD, Kelly S, Brown T, Campbell KJ. Interventions for preventing obesity in children. Cochrane Database Syst Rev. 20 Jul 2005;3:CD001871.
Toh CM, Cutter J, Chew SK. School based intervention has reduced obesity in Singapore. BMJ. 16 Feb 2002;324(7334):427.
Agence France Presse. Schools making fat students thin, but emotional burden is heavy. Feb 2005.
Brandou F, Savy-Pacaux AM, Marie J, Bauloz M, Maret-Fleuret I, Borrocoso S, et al. Impact of high- and low-intensity targeted exercise training on the type of substrate utilization in obese boys submitted to a hypocaloric diet. Diabetes Metab. Sept 2005;31(4 Pt 1):327–35.
Reinehr T, Widhalm K, l’Allemand D, Wiegand S, Wabitsch M, Holl RW, et al. Two-year follow-up in 21,784 overweight children and adolescents with lifestyle intervention. Obesity (Silver Spring). Jun 2009;17(6):1196–9.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2010 Springer Science+Business Media, LLC
About this chapter
Cite this chapter
Gittelsohn, J., Park, S. (2010). School- and Community-Based Interventions. In: Freemark, M. (eds) Pediatric Obesity. Contemporary Endocrinology. Humana Press, New York, NY. https://doi.org/10.1007/978-1-60327-874-4_22
Download citation
DOI: https://doi.org/10.1007/978-1-60327-874-4_22
Published:
Publisher Name: Humana Press, New York, NY
Print ISBN: 978-1-60327-873-7
Online ISBN: 978-1-60327-874-4
eBook Packages: MedicineMedicine (R0)