Abstract
This chapter discusses the emerging field of vector-mediated antibody gene transfer as an alternative vaccine for infectious disease, with a specific focus on HIV. However, this methodology need not be confined to HIV-1; the general strategy of vector-mediated antibody gene transfer can be applied to other difficult vaccine targets like hepatitis C virus, malaria, respiratory syncytial virus, and tuberculosis. This approach is an improvement over classical passive immunization strategies that administer antibody proteins to the host to provide protection from infection. With vector-mediated gene transfer, the antibody gene is delivered to the host, via a recombinant adeno-associated virus (rAAV) vector; this in turn results in long-term endogenous antibody expression from the injected muscle that confers protective immunity. Vector-mediated antibody gene transfer can rapidly move existing, potent broadly cross-neutralizing HIV-1-specific antibodies into the clinic. The gene transfer products demonstrate a potency and breadth identical to the original product. This strategy eliminates the need for immunogen design and interaction with the adaptive immune system to generate protection, a strategy that so far has shown limited promise.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Monoclonal antibodies as therapeutics have rapidly become a powerful new class of biologically based drugs. There are at least 25 antibodies that are approved for clinical use, with approximately ten times that number in development [1]. The essentially infinite number of possible antibody targets has given rise to antibody products for treatment of autoimmunity, cancer, inflammation, and infectious diseases, to name a few. Antibody therapy involves injecting highly purified antibody proteins to provide an immediate treatment for illnesses and diseases. Specific antibodies can also be passively administered to healthy people in the form of a vaccine, or immunoprophylactic. This strategy essentially bypasses the adaptive immune response by engendering the host with protective antibodies to prevent infection. While these methods hold tremendous promise for the treatment of many diseases, they are less applicable for a large-scale human prophylactic vaccine approach. Injections of antibodies every few weeks to potentially millions of people are not practical or cost effective. In this chapter, we will discuss the emerging field of vector-mediated antibody gene transfer as an alternative vaccine for infectious disease, with a specific focus on HIV-1. However, this methodology need not be confined to HIV-1. The general strategy of vector-mediated antibody gene transfer can be applied to other difficult vaccine targets like hepatitis C virus, malaria, respiratory syncytial virus, and tuberculosis. This approach is an improvement over classical passive immunization strategies that administer antibody proteins to the host to provide protection from infection. With vector-mediated gene transfer, the antibody gene is delivered to the host resulting in long-term endogenous antibody expression from the injected muscle that confers protective immunity.
Finding Potent Broadly Neutralizing Antibodies for HIV-1
The need for a safe and effective HIV-1 vaccine is undisputed. In 2012 alone, 1.6 million people died from AIDS related causes, while 2.3 million people were newly infected with HIV [2]. Two HIV-1 Envelope (Env) subunit vaccines tested in Phase 3 clinical trials (Vax003 and Vax004) failed to protect vaccine recipients from infection, and neither diminished viral replication after infection [3, 4]. A similar lack of efficacy was also seen from the Step Study, which used recombinant adenovirus vectors (rAd) that expressed multiple HIV-1 proteins [5, 6]. The RV144 trial in Thailand tested a canary pox vector prime/Env protein boost strategy and showed modest efficacy (31 %) [7]. Detailed analyses of the RV144 study results revealed two significant correlations with infection among vaccine recipients. The presence of IgG antibodies against V1/V2 loop of Env may have contributed to protection against HIV-1 infection, whereas high levels of Env-specific IgA antibodies correlated virus acquisition [8]. More recently, the HVTN 505 trial was stopped for futility, dealing yet another blow to HIV vaccine efforts [9]. The HVTN 505 trial, which used a DNA prime/rAd boost, showed no difference in HIV-1 infections between those recipients who received the vaccine and those receiving placebo [10]. Vaccine recipients did generate IgG antibodies to Env; however, the majority were non-neutralizing with low reactivity to the V1/V2 loop [10]. These observations underscore the tremendous hurdles that must be overcome to develop an effective HIV-1 vaccine. Foremost is figuring out how to induce antibodies that neutralize a wide array of HIV-1 field isolates. It was initially believed that potent, broadly neutralizing antibodies (bNAbs) to HIV-1 were extremely rare and difficult to elicit. In fact for some time, only four such antibodies had been identified, known as b12, 2F5, 2G12, and 4E10 [11–14]. These antibodies provided valuable information as to what regions of HIV-1 envelope were potentially sensitive to neutralization, which could aid in better vaccine antigen design. More recently, a large number of new, significantly more potent bNAbs have been identified using improved screening and sequencing techniques. These newer antibodies were isolated by high throughput screening of sera from healthy HIV-1-infected individuals categorized as “elite neutralizers” based on their neutralization breadth and potency [15–23]. Detailed analyses of these antibodies indicated they are approximately 10- to 100-fold more potent and have an increased breadth compared to the original four isolates. Furthermore, this new class of antibodies can neutralize HIV-1 through binding to a variety of envelope domains including the CD4 binding site (VRC01, NIH45-46, and PGV04) [18, 21, 24], glycan containing regions in the variable loops (PG9, PG16, PGT121, and PGT128) [16, 17], and the membrane-proximal external region (MPER) on gp41 (10E8) [19].
Epitope mapping of these new, potent antibodies has invigorated the vaccine field by providing precise regions to target when designing new protein or subunit vaccine antigens to induce bNAbs [25]. For example, highly stable Env trimers have been generated that bind to most of the known neutralizing antibodies, but generally do not bind non-neutralizing antibodies, and could potentially be used as a next-generation immunogen [26]. However, even with this new wealth of information at hand, generating bNAbs with improved, redesigned antigens may still prove to be problematic. Extensive sequence analysis of these potent, broadly neutralizing antibodies reveal that high levels of somatic mutations (as much as 30 %) can occur in the generation of the mature antibody [16, 18, 21, 23, 27]. Furthermore, the maturation may have involved repeated rounds of antibody selection through interactions with the HIV-1 antigen. In light of this, several groups have developed novel immunogens, such as glycopeptides or computation-derived multimerized nanoparticles that are designed to induce bNAbs [28, 29]. These immunogens can bind to both mature bNAbs as well as the receptors on their germ-line (naïve) B-cells, which can trigger their activation and maturation into plasma cells that are able to produce the bNAb.
Passive Immunization Strategies for HIV
While induction of bNAbs by various next-generation immunization strategies holds promise, the question remains as to the best use the human monoclonals that have already been isolated and characterized. One obvious option is passive immunization. Passive immunization using neutralizing monoclonal antibodies has protected monkeys from simian–human immunodeficiency virus (SHIV) challenge infections [30–36]. In a recent study by Moldt et al. [36] they showed that passively administered PGT121 can mediate sterilizing immunity against SHIV in monkeys at serum concentrations that were significantly lower than those observed in previous studies. Sterilizing immunity was achieved in all animals administered 5 and 1 mg/kg and three of five animals administered 0.2 mg/kg PGT121, with corresponding average antibody serum concentrations of 95 μg/mL, 15 μg/mL, and 1.8 μg/mL, respectively. The results suggested that a protective serum concentration for PGT121 was in the single-digit μg/mL amount. While this study demonstrates the potential for passive immunization with the new class of bNAbs, unfortunately, an injection of antibodies every few weeks is not practical or cost effective as a large-scale human prophylactic vaccine approach.
Vector-Mediated Antibody Gene Transfer to Bypass Adaptive Immune System
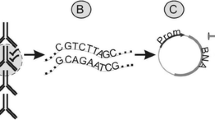
Given the difficulties of using the classic concept of passive immunization as a vaccine, we developed a second option: isolate the representative antibody gene and use gene transfer technology to endow a target host with the gene. In this way, the antibody gene directs endogenous expression of the antibody molecule, and the host (in theory) will now have the antibody in its circulation. Thus, after a single injection, the muscle now serves as a depot to synthesize the bNAbs that are passively distributed through the circulatory system (Fig. 1). The host is now armed with a potent bNAb against HIV-1 that effectively bypasses the adaptive immune system. This is in contrast to the traditional idea of passive immunization whereby the purified antibodies are injected intravenously into the host to provide protection from infection. However, due to the antibody half-life (approximately 6 days for PGT121 [36]), the levels decline requiring repeated injections. The obvious advantage is that antibody gene transfer engenders the host with long-term antibody persistence from a single injection due to endogenous antibody expression.
Immunoprophylaxis by antibody gene transfer. Passive immunization involves intravenous delivery of purified antibodies to engender the host with short-lived immunity in serum and mucosa. In contrast, vector mediated antibody gene transfer uses a viral vector to deliver the antibody gene to the host via intramuscular injection. The antibody is produced endogenously in the muscle and secreted into the circulatory system and mucosa providing long-term protection from infection
Choosing the Right Gene Transfer Vector
A popular antibody gene delivery vector is the recombinant adeno-associated virus (rAAV) vector, which is derived from wild-type AAV. AAV is a dependovirus with a 4.7 kb single strand DNA genome that contains only two genes (rep and cap) flanked by inverted terminal repeats (ITRs). AAV natural infection is common and has not been associated with any disease. Multiple AAV serotypes have been identified with different transduction efficiencies in different tissues, offering flexibility for gene transfer targets such as muscle or liver [37]. rAAV vectors have an established record of high-efficiency gene transfer in a variety of model systems [38, 39]. Following injection, the rAAV vector genome can form stable non-integrating circular episomes that can persist in non-dividing cells [40–42]. Because of these features, rAAV vectors have become popular gene delivery vehicles for use in clinical studies for the treatment of diseases such as alpha1-antitrypsin deficiency, cystic fibrosis, hemophilia B, Leber’s congenital amaurosis, lipoprotein lipase (LPL) deficiency, Parkinson’s disease, and muscular dystrophy [43].
rAAV gene transfer vectors are devoid of the endogenous rep and cap genes, and consist of the antibody gene expression cassette flanked by the AAV ITRs (Fig. 2). The ITRs (145 bp each), which are necessary for rAAV vector genome replication and packaging, are the only part of the AAV genome present in the rAAV vectors. One method for antibody expression utilizes a two-promoter system whereby the heavy and light chain genes are transcribed independently using two different promoters and polyadenylation signals within the same rAAV vector genome (Fig. 2) [44]. Another method uses a single promoter for expression of both the heavy and light chains, which are separated by the foot-and-mouth-disease virus (FMDV) 2A peptide, which undergoes self-cleavage to produce separate heavy and light chain proteins (Fig. 2) [45]. The advantage of this system is that the heavy and light chains can potentially be expressed in a 1:1 ratio using a single promoter, which may translate to more efficient expression. However, a potential disadvantage is that the FMDV-2A peptide is derived from a viral sequence and may be immunogenic in the host causing immune clearance of cells expressing the antibody.
rAAV vectors for antibody gene transfer. (a) The wild-type AAV (wtAAV) genome consists of the rep and cap genes flanked by inverted terminal repeats (ITR). For rAAV vectors, the rep and cap genes are removed and replaced by an antibody expression cassette flanked by ITRs, which are necessary for rAAV vector genome replication and packaging. (b) Immunoadhesins contain the antibody variable domains (VL variable light, VH variable heavy) usually joined by a flexible protein linker. The variable domains are connected to the hinge and constant heavy chain domains (CH2 and CH3). The immunoadhesins can form dimers through disulfide bonding in the hinge region. (c) Full antibodies can be expressed using either a dual promoter of single promoter system. For dual promoter expression, the antibody heavy and light chains are each expressed separately from their own promoter. For the single promoter system, the heavy and light chains are expressed as a single polypeptide separated by the foot-and-mouth-disease virus 2A peptide (FMDV-2A). The FMDV-2A peptide can undergo self-cleavage to give rise to separate heavy and light chains
Antibody Gene Transfer for an HIV-1 Vaccine
We first tested the concept of rAAV-mediated antibody gene transfer in animals by using one of the first bNAb isolated, IgG1b12. The human monoclonal IgG1b12 heavy and light chains were cloned independently into an rAAV genome using the two promoter system. The resulting vector was injected into the quadriceps muscles of immunodeficient mice (to avoid immune responses to human IgG). IgG1b12 was expressed in mouse muscle (confirmed by histochemical staining), and biologically active antibody was found in sera for over 6 months [44]. Characteristic biologic activity was determined by HIV-1 neutralization assays against IgG1b12 sensitive/resistant viruses. This study provided the first evidence that: (1) rAAV vectors transferred antibody genes to muscle; (2) myofibers produced antibodies; (3) antibodies were distributed to the circulation; and (4) such antibodies were biologically active.
Our next objective was to test the gene transfer concept in monkeys in a challenge study. In pilot experiments using the rAAV-IgG1b12 vector, macaques developed antibody responses to the human-derived transgene that effectively shut down expression. We turned to using rhesus-derived antibodies by taking advantage of native macaque SIV gp120-specific Fab molecular clones that had been derived directly from SIV-infected macaques [46]. When designing the antibody gene transfer vectors, we chose to express the Fabs as immunoadhesins, which in pilot experiments in mice were superior to single-chain (scFv) or whole-antibody (IgG) molecules with respect to steady-state serum concentrations (unpublished data). Immunoadhesins are chimeric, antibody-like molecules that combine the functional domain of a binding protein like a scFv or CD4 extracellular domains 1 and 2 (D1D2) with an immunoglobulin constant domain [47] (Fig. 2). They have been shown to be effective in disease models including HIV, SIV, and influenza [48–50]. A typical immunoadhesin lacks the constant light chain domain and the constant heavy domain 1 (CH1); however, it can be expressed as a single polypeptide from a single promoter, and forms dimers through disulfide bonding in the hinge region. While immunoadhesins have many attractive features such as efficient expression/secretion in vivo, they also have some drawbacks. Immunoadhesins may not exhibit the same neutralization breadth and potency as the native antibody. While we have seen cases where a specific immunoadhesin functions identically to its native antibody counterpart, we have also seen an immunoadhesin become tenfold less potent at neutralizing HIV-1 (unpublished observation). Thus, each immunoadhesin must be fully characterized and compared to the native antibody from which they were derived before it can be considered as a vaccine. Another drawback to using immunoadhesins is possible immunogenicity. Immunoadhesins are not naturally occurring proteins and may contain amino acid linkers connecting the variable domains (Fig. 2), which could trigger an immune response leading to loss of expression. However, it should be noted that Enbrel (etanercept), an immunoadhesin consisting of the TNF receptor fused to IgG1-Fc, was well tolerated in patients for long-term treatment (10 years) of rheumatoid arthritis [51].
For the macaque experiments, we constructed immunoadhesins derived from two different SIV Fab fragments (4L6 and 5L7), as well as a third immunoadhesin containing the rhesus CD4 D1D2, which was modeled after CD4-Ig fusion proteins [52]. All of the constructs neutralized in vitro the proposed SIV challenge stock (SIVmac316), indicating that the immunoadhesins were functioning like the original Fab clones [49]. The three immunoadhesins were injected into three monkeys each (for nine total), followed by an intravenous SIVmac316 challenge 4 weeks later, including six naïve controls. Immunoadhesin expression levels were as high as 190 μg/mL at the time of challenge (4 weeks post injection) and peaked around 6 months with levels reaching 400 μg/mL in some animals [49]. Overall, six of the nine monkeys receiving the immunoadhesins were completely protected from SIV infection while all six naïve controls became infected. Analysis of the three monkeys from the immunoadhesin group that became infected revealed that these specific animals had developed an immune response to the immunoadhesin by 3 weeks post injection, suggesting a correlation between an immune response to the immunoadhesin and failure to protect from infection. We have performed longitudinal studies of the protected monkeys, which are now over 6 years post injection. Immunoadhesin levels dropped to a stable level of approximately 20 μg/mL, which has persisted for over the last 4 years. The monkeys have remained negative for SIV infection and have not developed an immune response to the immunoadhesins (unpublished observation). Thus, this crucial study was instrumental in proving the concept of vector mediated gene transfer as a viable HIV vaccine.
More recently other investigators performed rAAV vector-mediated gene transfer expression/challenge studies, which they called vectored immunoprophylaxis (VIP) [53]. They expressed the native, full antibodies of 2G12, IgG1b12, 2F5, 4E10, and VRC01 using the single promoter FMDV-2A system. Following intramuscular rAAV injection in mice, antibody expression levels greater than 100 μg/mL were observed for at least 12 months. Using a humanized mouse model, they further showed that these rAAV vectors provided protection following HIV-1 challenge, with antibody serum levels as low as 8.3 μg/mL (antibody VRC01). These encouraging results reinforce the efficacy of the antibody gene transfer approach, especially when potent antibodies such as VRC01 are used. Taken together, these murine and primate studies show that vector-mediated antibody gene transfer can bypass the adaptive immune response and engender the host with antibodies that provide protection from infection. Furthermore, antibody expression can persist several years following a single injection, suggesting long-term protection is possible.
Antibody Gene Transfer for HIV-1 Therapy
While antibody gene transfer shows great promise for providing protection from HIV-1 infection, one obvious question is whether this strategy can also be used for antibody therapy in HIV-1 positive individuals. Several recent studies have demonstrated that it may be possible. One group of experiments was done using a humanized mouse model [54, 55]. Humanized mice were generated by injecting immunodeficient mice with human fetal liver-derived CD34+ hematopoietic stem cells, resulting in mice with a complete human immune system. The advantage here is that the mice will not generate an immune response to the presence of human antibodies, which is a problem when trying to express human antibodies in nonhuman primates.
For these studies, HIV-1-infected humanized mice were passively administered several bNAbs either singly or in combination. The mice showed sustained decreases in plasma viral loads starting a few days after antibody delivery. Furthermore, these mice also exhibited reduced cell-associated viral DNA, suggesting the antibodies played a role in killing infected cells expressing HIV gp120 on their surface through antibody-dependent cell-mediated cytotoxicity (ADCC). Viral loads tended to rebound over time, which correlated with the loss of the bNAbs due to the antibody half-life in the serum. Not surprisingly, some mice developed viral escape mutants. These escape mutants, predominantly from groups that were passively administered a single bNAb, were further analyzed and, as one would predict, they had developed mutations at sites that conferred resistance to the respective antibody. The level of viral escape mutants was dramatically reduced in mice that were passively administered multiple bNAbs at once. These antibody mixtures targeted different regions of gp120 and suggested that the viruses were unable to escape the broad selective pressure provided by using antibodies targeting multiple epitopes.
To answer the question as to whether vector mediated antibody gene transfer could be used for HIV-1 therapy, one of these studies [54] included a group of mice that received an intravenous injection of a rAAV (serotype 8) vector expressing bNAb 10-1074, which targets the base of the V3 stem of gp120 [56]. These mice maintained a high level of antibody 10-1074 expression of around 200 μg/mL for the entire length of the 67-day observation period. During this time, six of the seven mice in the group were able to control HIV-1 plasma viral loads, whereas one mouse exhibited viral escape. As seen with the escape mutants from the passive immunization studies, sequence analysis of the gp120 of these escape virus revealed mutations in the 10-1074 binding site that conferred resistance to the antibody. It remains to be seen if simultaneously administering rAAV vectors expressing multiple bNAbs could dramatically reduce or even possibly eliminate the generation of escape mutants. Furthermore, long-term studies will be required to see if escape mutants could arise over time, even in the presence of multiple antibodies.
Similar passive antibody therapy studies have been performed in SHIV-infected rhesus monkeys [57, 58]. SHIV is a virus composed of both HIV and SIV, and allows researchers to study antiviral compounds against HIV-1 Env in a nonhuman primate model. As seen in the humanized mice studies, SHIV-infected monkeys demonstrated a dramatic drop in plasma viral load as well as reduced proviral DNA in peripheral blood following intravenous infusions of bNAbs, either administered alone, or in combination. SHIV virus levels rebounded when serum bNAb titers declined to undetectable levels at around day 60. However, some animals maintained long-term SHIV control (>100 days) in the absence of additional bNAb infusions [57]. Some groups of monkeys that received only a single infused bNAb went on to develop neutralization-resistant escape mutant variants, which was also observed in the humanized mouse studies. In contrast, monkeys receiving only the single bNAb PGT121 [57] did not give rise to escape mutants, which may be reflective of the overall potency and breadth of the bNAb used in the studies, or may be due to duration of the bNAb in the serum. One caveat here is that long-term studies with repeated infusions of these human monoclonal antibodies in monkeys are not possible. The monkeys will recognize the human antibodies as foreign and generate anti-human IgG immune responses to eliminate the infused antibodies. Thus, the effects of long-term selective pressure on the generation of escape mutants cannot be properly addressed here.
Neither of these immunotherapy studies in monkeys used vector-mediated gene transfer to deliver the bNAbs to SHIV infected monkeys. However, for reasons described above, the human antibodies would very likely not be expressed long-term in these monkeys due to species incompatibility with a human antibody. A study using bNAbs isolated from monkeys would be required, as was done in the nonhuman primate immunoprophylactic study [49]. Those issues notwithstanding, the antibody immunotherapy studies done in humanized mice and monkeys suggest that using vector-mediated gene transfer to deliver bNAbs to HIV-1 infected individuals could be a viable option, possibly even used in conjunction with standard antiretroviral therapy (ART). An overriding theme is that multiple bNAbs would be required to provide the selective pressure to avoid viral escape mutants. Multiple antibodies could target different gp120 domains such as the exterior loops, CD4 binding site and MPER. Furthermore, multiple antibodies could be used that target different stages of viral entry including CD4 binding, CCR5 binding, and membrane fusion. Of course this strategy of the simultaneous use of multiple antibodies against multiple viral targets or stages of entry could also be applicable and in a prophylactic vaccine approach for maximum efficacy.
Antibody Gene Transfer for Respiratory Tract Infections
The use of vector-mediated antibody gene transfer has not been limited to just HIV-1 (Table 1). Respiratory syncytial virus (RSV) is a major cause severe respiratory infection in high-risk populations (such as infants) for which a vaccine is not yet available. Currently, the only way to prevent infection is through the passive administration of anti-RSV antibodies, such as palivizumab (also known as Synagis, manufactured by MedImmune). This antibody can be administered intramuscularly once each month during the RSV season (winter and spring) to prevent RSV infection. While this treatment is effective, it is costly and limited to high-risk individuals, which are attributes that make it a prime candidate for antibody gene transfer. Instead of repeated monthly injections of the purified antibody, the antibody could be endogenously expressed from a single injection using antibody gene transfer and provide a constant level of protective anti-RSV antibodies in the host.
The study used different vector systems to deliver antibodies against RSV infection [59]. They compared expression and efficacy of a mouse version of palivizumab in a mouse model system when delivered by either a rAAV vector (serotype rh.10) or adenovirus (Ad) vector. Adenovirus vectors have the capacity for high-level gene transfer with rapid and robust transgene expression. However, Ad vectors are highly immunogenic, and transduced cells are quickly cleared by the immune system resulting in rapid loss of transgene expression. In contrast, rAAV vectors have very low immunogenicity and can give rise to long-term gene (antibody) expression for potentially the life of the individual. The Ad-palivizumab vector was administered intravenously, with palivizumab detected in the lungs by day 3 post-administration. Following an intranasal RSV challenge 7 days post administration, the mice showed >5-fold decrease in RSV titers in the lung compared to control animals. Long-term antibody expression and challenge studies were done using the rAAVrh.10-palivizumab vector via intrapleural administration. Palivizumab was detected in the serum of these animals by 8 weeks post administration that started to peak by week 20. These rAAVrh.10-palivizumab mice were intranasally challenged with RSV at 7 and 21 weeks post-administration. They showed a 14.3-fold and 10.6-fold lower numbers of RSV pfu in the lungs, indicating that protection against RSV infection can be sustained at least 21 weeks post delivery of a rAAV vector.
Antibody gene transfer studies using rAAV vectors have also been done to prevent influenza. Although traditional vaccination strategies for influenza are quite effective, they may not be adequate for a possible zoonotic strain that could lead to a pandemic (such as the 2009 H1N1). In this case, the time needed to develop a traditional vaccine may not be rapid enough. The rationale is that vector-mediated antibody gene transfer could quickly deliver a bNAb that is effective against multiple strains of influenza that would provide protection against a pandemic. One study looked at delivering the bNAb antibody FI6 [60] as an immunoadhesin using rAAV serotype 9 via intranasal delivery in mice and ferrets [50]. FI6 immunoadhesin expression was detected in the nasal and lung lavage fluids of mice 14 days post vector administration at concentrations ranging from 0.5 to 2.0 μg/mL. Animals challenged as early as 3 days after rAAV9-FI6 administration could be protected. Furthermore, this strategy was able to protect both mice and ferrets from exposure of lethal doses of various clinical isolates of H5N1 and H1N1. An additional study [61] also demonstrated that rAAV9-FI6 administration showed partial efficacy in mice challenged with the newly emergent avian H7N9, which is believed to be transmitted from poultry to humans.
A separate study used a similar strategy but with intramuscular administration of the rAAV antibody vector in mice [62]. They expressed antibodies F10 [63] and CR6261 [64] in a rAAV serotype 8 vector using the FMDV-2A expression system. Antibody expression levels in the serum reached 200 μg/mL at 5 weeks post intramuscular injection, with levels still around 10 μg/mL out to at least 11 months after a single injection. These treated mice were protected from diverse strains of H1N1 influenza when challenged at either of these time points (5 weeks and 11 months), demonstrating once again the incredible potential for this strategy as a vaccine. The results from both the intranasal [50] and intramuscular [62] routes of vector administration reinforce the flexibility of vector-mediated gene transfer and provide important proof-of-concept studies that could lead to translation into humans.
Other Applications for Antibody Gene Transfer
Up to this point, we have discussed the use of vector-mediated antibody gene transfer for the prevention and possible treatment of infectious diseases such as HIV-1, RSV, and influenza. However, this strategy can be expanded for use in noninfectious disease applications where antibodies still play a critical role, such as cancer treatment. In a study by Fang et al. [45], they examined the efficacy of an antitumor antibody to reduce tumor growth in a mouse model system. They used a rAAV8 vector that expressed antibody DC101 by the FMDV-2A system. Antibody DC101 is an antiangiogenic monoclonal antibody that targets vascular endothelial cell growth factor receptor-2 (VEGFR2). Mice given an intravenous injection of rAAV8-DC101 could express high levels (>1 mg/mL) of the antibody in the serum for the length of the 5-month monitoring period. Mice receiving this rAAV vector exhibited shrinkage of tumors and prolonged survival time compared to untreated control animals. These encouraging results set the stage for combining antibody gene transfer technology with the ever increasing number of antibody-based therapies for cancers that include such antibodies as Herceptin and Avastin (Genentech), to name a few.
Perhaps a less conventional use of vector-mediated antibody gene transfer is a potential role in the treatment of substance addiction. Antibodies exist that can bind to these substances in the blood and prevent their transfer to the brain, which leads to their addictive properties. Antibody therapy for addiction would require routine, costly injections, which once again makes this a prime candidate for antibody gene transfer. NIC9D9 is an anti-nicotine antibody that was delivered intravenously (targeting the liver) to mice using a rAAVrh.10 vector [65]. NIC9D9 antibody was detected in the serum for the length of the 18-week study. Following intravenously nicotine delivery, the rAAV-NIC9D9 mice had 83 % of the nicotine bound to the NIC9D9 antibody in serum, which drastically reduced the amount of serum delivered to the brain. Furthermore, these mice had reduced cardiovascular effects compared to control animals. These results indicate that this strategy may hold promise as an effective preventative therapy for nicotine addiction.
Along the same line, GNC92H2 is a mouse monoclonal antibody with high affinity for cocaine. This antibody was also delivered to mice using the rAAVrh.10 vector via intravenous injection [66]. GNC92H2 was detected in the serum for the entire duration of the 24-week study. The GNC92H2 antibody was able to sequester intravenously administered cocaine in the blood, thereby protecting the brain from the effects of cocaine. Furthermore, these mice showed suppressed cocaine-induced hyperactivity derived from weekly cocaine exposure (12–17 weeks post rAAVrh.10 vector administration). These findings offer an alternative intervention to cocaine addiction therapy. High affinity cocaine antibodies could be maintained long-term in the serum following a single administration. This strategy could be coupled with traditional behavioral therapies for a combined approach for the treatment of cocaine addiction.
Limitations of rAAV Gene Transfer
When using rAAV vectors to deliver antibodies, there are several factors that could limit their effectiveness. These considerations pertain to the antibody transgene, as well as the rAAV vector itself. Given the fact that AAV infection is common in the human population, plus AAV capsid sequences contain highly conserved regions, many people have circulating neutralizing antibodies to AAV capsids of multiple serotypes [67]. The presence of preexisting neutralizing antibodies, with titers as low as 1:5 to 1:10, can have a negative impact on vector transduction [68–70]. Furthermore, neutralizing antibodies may prevent repeated administrations [69], which would impede rAAV delivery of potentially more potent antibodies at a later time. Potential solutions to the AAV neutralization conundrum involve using rare AAV capsids, or capsids that have been reengineered to remove or alter neutralization epitopes [37].
Another immune obstacle to rAAV vectors is capsid-specific T cell responses. The leading hypothesis is that prior exposure to AAV gives rise to AAV-specific memory T cells that are activated following rAAV vector gene transfer [71]. Results from clinical trials using both hepatic and muscular delivery indicate T cell responses occur within 30 days after administration, which is associated with reduced or lost transgene expression [72, 73]. A more recent clinical study using intramuscular delivery of a rAAV vector for α-1 antitrypsin (AAT) deficiency did observe an early capsid-specific T cell response and associated decline in transgene expression [74]. However, AAT transgene expression did not completely disappear. In fact, AAT levels persisted for more than a year after administration despite the persistence of anti capsid T cells [74]. Clearly more studies will be required to elucidate the mechanism behind T cell responses and their effects on transgene expression.
With regard to limitations of the antibody transgene, essentially any therapeutic or immunoprophylactic protein can be expressed using rAAV vector gene transfer, as long as it fits within the vector packaging limit. However, one must be careful that the expressed protein is not immunogenic in the host. However, this is also the same concern for all exogenously (passively) administered proteins, including monoclonal antibodies and other biologics. Most, if not all, of the 25 monoclonal antibodies that have been approved as therapeutics have exhibited some level of immunogenicity [75, 76]. Several factors may contribute to immunogenicity including antibody structure, dosing regime, and the recipient’s genetic background. Also, it remains to be determined if an antibody that was endogenously expressed in the host via gene transfer will be more or less immunogenic than when passively administered as an exogenously produced protein. The big question is what effect would an immune response to the transgene have in the host? In the simplest scenario, as was seen in the nonhuman primate studies [49], the appearance of anti-antibody responses would limit the vaccine efficiency through loss of transgene expression, with no adverse events observed. Ultimately, at this stage it is difficult to predict with any certainty, which, if any, of the candidates would be immunogenic, and what the consequences would be. Human clinical trials will be the best predictor.
Perhaps of greater concern is the risk that the antibody will bind off target causing an unanticipated adverse event. Preclinical testing, such as passive administration and GLP human tissue binding studies, can help avert most of these issues. However, if off-target effects occur in vivo, there is currently no efficient method to stop antibody gene expression. As the data shows from animal models, antibodies are expressed for potentially the life of the host following a single intramuscular administration. A few studies have attempted to regulate gene expression from rAAV gene transfer vectors in mice and monkeys [77–79], but these schemes are transient and require continuous exogenous drug administration to maintain a constant level of gene expression. Clearly, identifying an efficient method to permanently eliminate antibody gene expression in the host is a top priority if rAAV vector-mediated antibody gene transfer is to become applicable for wide-scale use.
References
Chan AC, Carter PJ. Therapeutic antibodies for autoimmunity and inflammation. Nat Rev Immunol. 2010;10:301–16.
(UNAIDS) U. N. P. o. H. A. 2012. Getting to zero. The global AIDS epidemic.
Flynn NM, Forthal DN, Harro CD, Judson FN, Mayer KH, Para MF. Placebo-controlled phase 3 trial of a recombinant glycoprotein 120 vaccine to prevent HIV-1 infection. J Infect Dis. 2005;191:654–65.
Pitisuttithum P, Gilbert P, Gurwith M, Heyward W, Martin M, van Griensven F, Hu D, Tappero JW, Choopanya K. Randomized, double-blind, placebo-controlled efficacy trial of a bivalent recombinant glycoprotein 120 HIV-1 vaccine among injection drug users in Bangkok, Thailand. J Infect Dis. 2006;194:1661–71.
Buchbinder SP, Mehrotra DV, Duerr A, Fitzgerald DW, Mogg R, Li D, Gilbert PB, Lama JR, Marmor M, Del Rio C, McElrath MJ, Casimiro DR, Gottesdiener KM, Chodakewitz JA, Corey L, Robertson MN. Efficacy assessment of a cell-mediated immunity HIV-1 vaccine (the Step Study): a double-blind, randomised, placebo-controlled, test-of-concept trial. Lancet. 2008;372:1881–93.
McElrath MJ, De Rosa SC, Moodie Z, Dubey S, Kierstead L, Janes H, Defawe OD, Carter DK, Hural J, Akondy R, Buchbinder SP, Robertson MN, Mehrotra DV, Self SG, Corey L, Shiver JW, Casimiro DR. HIV-1 vaccine-induced immunity in the test-of-concept Step Study: a case-cohort analysis. Lancet. 2008;372:1894–905.
Rerks-Ngarm S, Pitisuttithum P, Nitayaphan S, Kaewkungwal J, Chiu J, Paris R, Premsri N, Namwat C, de Souza M, Adams E, Benenson M, Gurunathan S, Tartaglia J, McNeil JG, Francis DP, Stablein D, Birx DL, Chunsuttiwat S, Khamboonruang C, Thongcharoen P, Robb ML, Michael NL, Kunasol P, Kim JH. Vaccination with ALVAC and AIDSVAX to prevent HIV-1 infection in Thailand. N Engl J Med. 2009;361:2209–20.
Haynes BF, Gilbert PB, McElrath MJ, Zolla-Pazner S, Tomaras GD, Alam SM, Evans DT, Montefiori DC, Karnasuta C, Sutthent R, Liao HX, DeVico AL, Lewis GK, Williams C, Pinter A, Fong Y, Janes H, DeCamp A, Huang Y, Rao M, Billings E, Karasavvas N, Robb ML, Ngauy V, de Souza MS, Paris R, Ferrari G, Bailer RT, Soderberg KA, Andrews C, Berman PW, Frahm N, De Rosa SC, Alpert MD, Yates NL, Shen X, Koup RA, Pitisuttithum P, Kaewkungwal J, Nitayaphan S, Rerks-Ngarm S, Michael NL, Kim JH. Immune-correlates analysis of an HIV-1 vaccine efficacy trial. N Engl J Med. 2012;366:1275–86.
von Bubnoff, A. HVTN 505: “a hard blow”. In: Initiative IAV, editor. IAVIReport, 2013.
Hammer SM, Sobieszczyk ME, Janes H, Karuna ST, Mulligan MJ, Grove D, Koblin BA, Buchbinder SP, Keefer MC, Tomaras GD, Frahm N, Hural J, Anude C, Graham BS, Enama ME, Adams E, DeJesus E, Novak RM, Frank I, Bentley C, Ramirez S, Fu R, Koup RA, Mascola JR, Nabel GJ, Montefiori DC, Kublin J, McElrath MJ, Corey L, Gilbert PB. Efficacy trial of a DNA/rAd5 HIV-1 preventive vaccine. N Engl J Med. 2013;369:2083–92.
Burton DR, Pyati J, Koduri R, Sharp SJ, Thornton GB, Parren PW, Sawyer LS, Hendry RM, Dunlop N, Nara PL, et al. Efficient neutralization of primary isolates of HIV-1 by a recombinant human monoclonal antibody. Science. 1994;266:1024–7.
Muster T, Steindl F, Purtscher M, Trkola A, Klima A, Himmler G, Ruker F, Katinger H. A conserved neutralizing epitope on gp41 of human immunodeficiency virus type 1. J Virol. 1993;67:6642–7.
Trkola A, Purtscher M, Muster T, Ballaun C, Buchacher A, Sullivan N, Srinivasan K, Sodroski J, Moore JP, Katinger H. Human monoclonal antibody 2G12 defines a distinctive neutralization epitope on the gp120 glycoprotein of human immunodeficiency virus type 1. J Virol. 1996;70:1100–8.
Zwick MB, Labrijn AF, Wang M, Spenlehauer C, Saphire EO, Binley JM, Moore JP, Stiegler G, Katinger H, Burton DR, Parren PW. Broadly neutralizing antibodies targeted to the membrane-proximal external region of human immunodeficiency virus type 1 glycoprotein gp41. J Virol. 2001;75:10892–905.
Burton DR, Poignard P, Stanfield RL, Wilson IA. Broadly neutralizing antibodies present new prospects to counter highly antigenically diverse viruses. Science. 2012;337:183–6.
Walker LM, Huber M, Doores KJ, Falkowska E, Pejchal R, Julien JP, Wang SK, Ramos A, Chan-Hui PY, Moyle M, Mitcham JL, Hammond PW, Olsen OA, Phung P, Fling S, Wong CH, Phogat S, Wrin T, Simek MD, Koff WC, Wilson IA, Burton DR, Poignard P. Broad neutralization coverage of HIV by multiple highly potent antibodies. Nature. 2011;477:466–70.
Walker LM, Phogat SK, Chan-Hui PY, Wagner D, Phung P, Goss JL, Wrin T, Simek MD, Fling S, Mitcham JL, Lehrman JK, Priddy FH, Olsen OA, Frey SM, Hammond PW, Kaminsky S, Zamb T, Moyle M, Koff WC, Poignard P, Burton DR. Broad and potent neutralizing antibodies from an African donor reveal a new HIV-1 vaccine target. Science. 2009;326:285–9.
Wu X, Yang ZY, Li Y, Hogerkorp CM, Schief WR, Seaman MS, Zhou T, Schmidt SD, Wu L, Xu L, Longo NS, McKee K, O’Dell S, Louder MK, Wycuff DL, Feng Y, Nason M, Doria-Rose N, Connors M, Kwong PD, Roederer M, Wyatt RT, Nabel GJ, Mascola JR. Rational design of envelope identifies broadly neutralizing human monoclonal antibodies to HIV-1. Science. 2010;329:856–61.
Huang J, Ofek G, Laub L, Louder MK, Doria-Rose NA, Longo NS, Imamichi H, Bailer RT, Chakrabarti B, Sharma SK, Alam SM, Wang T, Yang Y, Zhang B, Migueles SA, Wyatt R, Haynes BF, Kwong PD, Mascola JR, Connors M. Broad and potent neutralization of HIV-1 by a gp41-specific human antibody. Nature. 2012;491:406–12.
Simek MD, Rida W, Priddy FH, Pung P, Carrow E, Laufer DS, Lehrman JK, Boaz M, Tarragona-Fiol T, Miiro G, Birungi J, Pozniak A, McPhee DA, Manigart O, Karita E, Inwoley A, Jaoko W, Dehovitz J, Bekker LG, Pitisuttithum P, Paris R, Walker LM, Poignard P, Wrin T, Fast PE, Burton DR, Koff WC. Human immunodeficiency virus type 1 elite neutralizers: individuals with broad and potent neutralizing activity identified by using a high-throughput neutralization assay together with an analytical selection algorithm. J Virol. 2009;83:7337–48.
Scheid JF, Mouquet H, Ueberheide B, Diskin R, Klein F, Oliveira TY, Pietzsch J, Fenyo D, Abadir A, Velinzon K, Hurley A, Myung S, Boulad F, Poignard P, Burton DR, Pereyra F, Ho DD, Walker BD, Seaman MS, Bjorkman PJ, Chait BT, Nussenzweig MC. Sequence and structural convergence of broad and potent HIV antibodies that mimic CD4 binding. Science. 2011;333:1633–7.
Zhou T, Georgiev I, Wu X, Yang ZY, Dai K, Finzi A, Kwon YD, Scheid JF, Shi W, Xu L, Yang Y, Zhu J, Nussenzweig MC, Sodroski J, Shapiro L, Nabel GJ, Mascola JR, Kwong PD. Structural basis for broad and potent neutralization of HIV-1 by antibody VRC01. Science. 2010;329:811–7.
Bonsignori M, Hwang KK, Chen X, Tsao CY, Morris L, Gray E, Marshall DJ, Crump JA, Kapiga SH, Sam NE, Sinangil F, Pancera M, Yongping Y, Zhang B, Zhu J, Kwong PD, O’Dell S, Mascola JR, Wu L, Nabel GJ, Phogat S, Seaman MS, Whitesides JF, Moody MA, Kelsoe G, Yang X, Sodroski J, Shaw GM, Montefiori DC, Kepler TB, Tomaras GD, Alam SM, Liao HX, Haynes BF. Analysis of a clonal lineage of HIV-1 envelope V2/V3 conformational epitope-specific broadly neutralizing antibodies and their inferred unmutated common ancestors. J Virol. 2011;85:9998–10009.
Falkowska E, Ramos A, Feng Y, Zhou T, Moquin S, Walker LM, Wu X, Seaman MS, Wrin T, Kwong PD, Wyatt RT, Mascola JR, Poignard P, Burton DR. PGV04, an HIV-1 gp120 CD4 binding site antibody, is broad and potent in neutralization but does not induce conformational changes characteristic of CD4. J Virol. 2012;86:4394–403.
Kwong PD, Mascola JR, Nabel GJ. Broadly neutralizing antibodies and the search for an HIV-1 vaccine: the end of the beginning. Nat Rev Immunol. 2013;13:693–701.
Sanders RW, Derking R, Cupo A, Julien JP, Yasmeen A, de Val N, Kim HJ, Blattner C, de la Pena AT, Korzun J, Golabek M, de Los Reyes K, Ketas TJ, van Gils MJ, King CR, Wilson IA, Ward AB, Klasse PJ, Moore JP. A next-generation cleaved, soluble HIV-1 Env Trimer, BG505 SOSIP.664 gp140, expresses multiple epitopes for broadly neutralizing but not non-neutralizing antibodies. PLoS Pathog. 2013;9:e1003618.
Zhou T, Zhu J, Wu X, Moquin S, Zhang B, Acharya P, Georgiev IS, Altae-Tran HR, Chuang GY, Joyce MG, Do Kwon Y, Longo NS, Louder MK, Luongo T, McKee K, Schramm CA, Skinner J, Yang Y, Yang Z, Zhang Z, Zheng A, Bonsignori M, Haynes BF, Scheid JF, Nussenzweig MC, Simek M, Burton DR, Koff WC, Mullikin JC, Connors M, Shapiro L, Nabel GJ, Mascola JR, Kwong PD. Multidonor analysis reveals structural elements, genetic determinants, and maturation pathway for HIV-1 neutralization by VRC01-class antibodies. Immunity. 2013;39:245–58.
Alam SM, Dennison SM, Aussedat B, Vohra Y, Park PK, Fernandez-Tejada A, Stewart S, Jaeger FH, Anasti K, Blinn JH, Kepler TB, Bonsignori M, Liao HX, Sodroski JG, Danishefsky SJ, Haynes BF. Recognition of synthetic glycopeptides by HIV-1 broadly neutralizing antibodies and their unmutated ancestors. Proc Natl Acad Sci U S A. 2013;110:18214–9.
Jardine J, Julien JP, Menis S, Ota T, Kalyuzhniy O, McGuire A, Sok D, Huang PS, MacPherson S, Jones M, Nieusma T, Mathison J, Baker D, Ward AB, Burton DR, Stamatatos L, Nemazee D, Wilson IA, Schief WR. Rational HIV immunogen design to target specific germline B cell receptors. Science. 2013;340:711–6.
Baba TW, Liska V, Hofmann-Lehmann R, Vlasak J, Xu W, Ayehunie S, Cavacini LA, Posner MR, Katinger H, Stiegler G, Bernacky BJ, Rizvi TA, Schmidt R, Hill LR, Keeling ME, Lu Y, Wright JE, Chou TC, Ruprecht RM. Human neutralizing monoclonal antibodies of the IgG1 subtype protect against mucosal simian-human immunodeficiency virus infection. Nat Med. 2000;6:200–6.
Mascola JR, Stiegler G, VanCott TC, Katinger H, Carpenter CB, Hanson CE, Beary H, Hayes D, Frankel SS, Birx DL, Lewis MG. Protection of macaques against vaginal transmission of a pathogenic HIV-1/SIV chimeric virus by passive infusion of neutralizing antibodies. Nat Med. 2000;6:207–10.
Parren PW, Marx PA, Hessell AJ, Luckay A, Harouse J, Cheng-Mayer C, Moore JP, Burton DR. Antibody protects macaques against vaginal challenge with a pathogenic R5 simian/human immunodeficiency virus at serum levels giving complete neutralization in vitro. J Virol. 2001;75:8340–7.
Hessell AJ, Poignard P, Hunter M, Hangartner L, Tehrani DM, Bleeker WK, Parren PW, Marx PA, Burton DR. Effective, low-titer antibody protection against low-dose repeated mucosal SHIV challenge in macaques. Nat Med. 2009;15:951–4.
Hessell AJ, Rakasz EG, Poignard P, Hangartner L, Landucci G, Forthal DN, Koff WC, Watkins DI, Burton DR. Broadly neutralizing human anti-HIV antibody 2G12 is effective in protection against mucosal SHIV challenge even at low serum neutralizing titers. PLoS Pathog. 2009;5:e1000433.
Willey R, Nason MC, Nishimura Y, Follmann DA, Martin MA. Neutralizing antibody titers conferring protection to macaques from a simian/human immunodeficiency virus challenge using the TZM-bl assay. AIDS Res Hum Retroviruses. 2010;26:89–98.
Moldt B, Rakasz EG, Schultz N, Chan-Hui PY, Swiderek K, Weisgrau KL, Piaskowski SM, Bergman Z, Watkins DI, Poignard P, Burton DR. Highly potent HIV-specific antibody neutralization in vitro translates into effective protection against mucosal SHIV challenge in vivo. Proc Natl Acad Sci U S A. 2012;109:18921–5.
Asokan A. Reengineered AAV vectors: old dog, new tricks. Discov Med. 2010;9:399–403.
Coura Rdos S, Nardi NB. The state of the art of adeno-associated virus-based vectors in gene therapy. Virol J. 2007;4:99.
Daya S, Berns KI. Gene therapy using adeno-associated virus vectors. Clin Microbiol Rev. 2008;21:583–93.
Nowrouzi A, Penaud-Budloo M, Kaeppel C, Appelt U, Le Guiner C, Moullier P, von Kalle C, Snyder RO, Schmidt M. Integration frequency and intermolecular recombination of rAAV vectors in non-human primate skeletal muscle and liver. Mol Ther. 2012;20:1177–86.
Penaud-Budloo M, Le Guiner C, Nowrouzi A, Toromanoff A, Cherel Y, Chenuaud P, Schmidt M, von Kalle C, Rolling F, Moullier P, Snyder RO. Adeno-associated virus vector genomes persist as episomal chromatin in primate muscle. J Virol. 2008;82:7875–85.
Schnepp BC, Clark KR, Klemanski DL, Pacak CA, Johnson PR. Genetic fate of recombinant adeno-associated virus vector genomes in muscle. J Virol. 2003;77:3495–504.
Aalbers CJ, Tak PP, Vervoordeldonk MJ. Advancements in adeno-associated viral gene therapy approaches: exploring a new horizon. F1000 Med Rep. 2011;3:17.
Lewis AD, Chen R, Montefiori DC, Johnson PR, Clark KR. Generation of neutralizing activity against human immunodeficiency virus type 1 in serum by antibody gene transfer. J Virol. 2002;76:8769–75.
Fang JM, Qian JJ, Yi SY, Harding TC, Tu GH, VanRoey M, Jooss K. Stable antibody expression at therapeutic levels using the 2A peptide. Nat Biotechnol. 2005;23:584–90.
Johnson WE, Sanford H, Schwall L, Burton DR, Parren PW, Robinson JE, Desrosiers RC. Assorted mutations in the envelope gene of simian immunodeficiency virus lead to loss of neutralization resistance against antibodies representing a broad spectrum of specificities. J Virol. 2003;77:9993–10003.
Ashkenazi A, Chamow SM. Immunoadhesins as research tools and therapeutic agents. Curr Opin Immunol. 1997;9:195–200.
Capon DJ, Chamow SM, Mordenti J, Marsters SA, Gregory T, Mitsuya H, Byrn RA, Lucas C, Wurm FM, Groopman JE, et al. Designing CD4 immunoadhesins for AIDS therapy. Nature. 1989;337:525–31.
Johnson PR, Schnepp BC, Zhang J, Connell MJ, Greene SM, Yuste E, Desrosiers RC, Clark KR. Vector-mediated gene transfer engenders long-lived neutralizing activity and protection against SIV infection in monkeys. Nat Med. 2009;15:901–6.
Limberis MP, Adam VS, Wong G, Gren J, Kobasa D, Ross TM, Kobinger GP, Tretiakova A, Wilson JM. Intranasal antibody gene transfer in mice and ferrets elicits broad protection against pandemic influenza. Sci Transl Med. 2013;5:187ra172.
Weinblatt ME, Bathon JM, Kremer JM, Fleischmann RM, Schiff MH, Martin RW, Baumgartner SW, Park GS, Mancini EL, Genovese MC. Safety and efficacy of etanercept beyond 10 years of therapy in North American patients with early and longstanding rheumatoid arthritis. Arthritis Care Res (Hoboken). 2011;63:373–82.
Allaway GP, Ryder AM, Beaudry GA, Maddon PJ. Synergistic inhibition of HIV-1 envelope-mediated cell fusion by CD4-based molecules in combination with antibodies to gp120 or gp41. AIDS Res Hum Retroviruses. 1993;9:581–7.
Balazs AB, Chen J, Hong CM, Rao DS, Yang L, Baltimore D. Antibody-based protection against HIV infection by vectored immunoprophylaxis. Nature. 2012;481:81–4.
Horwitz JA, Halper-Stromberg A, Mouquet H, Gitlin AD, Tretiakova A, Eisenreich TR, Malbec M, Gravemann S, Billerbeck E, Dorner M, Buning H, Schwartz O, Knops E, Kaiser R, Seaman MS, Wilson JM, Rice CM, Ploss A, Bjorkman PJ, Klein F, Nussenzweig MC. HIV-1 suppression and durable control by combining single broadly neutralizing antibodies and antiretroviral drugs in humanized mice. Proc Natl Acad Sci U S A. 2013;110:16538–43.
Klein F, Halper-Stromberg A, Horwitz JA, Gruell H, Scheid JF, Bournazos S, Mouquet H, Spatz LA, Diskin R, Abadir A, Zang T, Dorner M, Billerbeck E, Labitt RN, Gaebler C, Marcovecchio PM, Incesu RB, Eisenreich TR, Bieniasz PD, Seaman MS, Bjorkman PJ, Ravetch JV, Ploss A, Nussenzweig MC. HIV therapy by a combination of broadly neutralizing antibodies in humanized mice. Nature. 2012;492:118–22.
Mouquet H, Scharf L, Euler Z, Liu Y, Eden C, Scheid JF, Halper-Stromberg A, Gnanapragasam PN, Spencer DI, Seaman MS, Schuitemaker H, Feizi T, Nussenzweig MC, Bjorkman PJ. Complex-type N-glycan recognition by potent broadly neutralizing HIV antibodies. Proc Natl Acad Sci U S A. 2012;109:E3268–77.
Barouch DH, Whitney JB, Moldt B, Klein F, Oliveira TY, Liu J, Stephenson KE, Chang HW, Shekhar K, Gupta S, Nkolola JP, Seaman MS, Smith KM, Borducchi EN, Cabral C, Smith JY, Blackmore S, Sanisetty S, Perry JR, Beck M, Lewis MG, Rinaldi W, Chakraborty AK, Poignard P, Nussenzweig MC, Burton DR. Therapeutic efficacy of potent neutralizing HIV-1-specific monoclonal antibodies in SHIV-infected rhesus monkeys. Nature. 2013;503:224–8.
Shingai M, Nishimura Y, Klein F, Mouquet H, Donau OK, Plishka R, Buckler-White A, Seaman M, Piatak M, Lifson JD, Dimitrov D, Nussenzweig MC, Martin MA. Antibody-mediated immunotherapy of macaques chronically infected with SHIV suppresses viraemia. Nature. 2013;503:277–80.
Skaricic D, Traube C, De B, Joh J, Boyer J, Crystal RG, Worgall S. Genetic delivery of an anti-RSV antibody to protect against pulmonary infection with RSV. Virology. 2008;378:79–85.
Corti D, Voss J, Gamblin SJ, Codoni G, Macagno A, Jarrossay D, Vachieri SG, Pinna D, Minola A, Vanzetta F, Silacci C, Fernandez-Rodriguez BM, Agatic G, Bianchi S, Giacchetto-Sasselli I, Calder L, Sallusto F, Collins P, Haire LF, Temperton N, Langedijk JP, Skehel JJ, Lanzavecchia A. A neutralizing antibody selected from plasma cells that binds to group 1 and group 2 influenza A hemagglutinins. Science. 2011;333:850–6.
Limberis MP, Racine T, Kobasa D, Li Y, Gao GF, Kobinger G, Wilson JM. Vectored expression of a broadly neutralizing antibody (FI6) in mouse airway provides partial protection against a new avian influenza A (H7N9) virus. Clin Vaccine Immunol. 2013;20:1836–7.
Balazs AB, Bloom JD, Hong CM, Rao DS, Baltimore D. Broad protection against influenza infection by vectored immunoprophylaxis in mice. Nat Biotechnol. 2013;31:647–52.
Sui J, Hwang WC, Perez S, Wei G, Aird D, Chen LM, Santelli E, Stec B, Cadwell G, Ali M, Wan H, Murakami A, Yammanuru A, Han T, Cox NJ, Bankston LA, Donis RO, Liddington RC, Marasco WA. Structural and functional bases for broad-spectrum neutralization of avian and human influenza A viruses. Nat Struct Mol Biol. 2009;16:265–73.
Throsby M, van den Brink E, Jongeneelen M, Poon LL, Alard P, Cornelissen L, Bakker A, Cox F, van Deventer E, Guan Y, Cinatl J, ter Meulen J, Lasters I, Carsetti R, Peiris M, de Kruif J, Goudsmit J. Heterosubtypic neutralizing monoclonal antibodies cross-protective against H5N1 and H1N1 recovered from human IgM+ memory B cells. PLoS One. 2008;3:e3942.
Hicks MJ, Rosenberg JB, De BP, Pagovich OE, Young CN, Qiu JP, Kaminsky SM, Hackett NR, Worgall S, Janda KD, Davisson RL, Crystal RG. AAV-directed persistent expression of a gene encoding anti-nicotine antibody for smoking cessation. Sci Transl Med. 2012;4:140ra187.
Rosenberg JB, Hicks MJ, De BP, Pagovich O, Frenk E, Janda KD, Wee S, Koob GF, Hackett NR, Kaminsky SM, Worgall S, Tignor N, Mezey JG, Crystal RG. AAVrh.10-mediated expression of an anti-cocaine antibody mediates persistent passive immunization that suppresses cocaine-induced behavior. Hum Gene Ther. 2012;23:451–9.
Boutin S, Monteilhet V, Veron P, Leborgne C, Benveniste O, Montus MF, Masurier C. Prevalence of serum IgG and neutralizing factors against adeno-associated virus (AAV) types 1, 2, 5, 6, 8, and 9 in the healthy population: implications for gene therapy using AAV vectors. Hum Gene Ther. 2010;21:704–12.
Jiang H, Couto LB, Patarroyo-White S, Liu T, Nagy D, Vargas JA, Zhou S, Scallan CD, Sommer J, Vijay S, Mingozzi F, High KA, Pierce GF. Effects of transient immunosuppression on adenoassociated, virus-mediated, liver-directed gene transfer in rhesus macaques and implications for human gene therapy. Blood. 2006;108:3321–8.
Manno CS, Pierce GF, Arruda VR, Glader B, Ragni M, Rasko JJ, Ozelo MC, Hoots K, Blatt P, Konkle B, Dake M, Kaye R, Razavi M, Zajko A, Zehnder J, Rustagi PK, Nakai H, Chew A, Leonard D, Wright JF, Lessard RR, Sommer JM, Tigges M, Sabatino D, Luk A, Jiang H, Mingozzi F, Couto L, Ertl HC, High KA, Kay MA. Successful transduction of liver in hemophilia by AAV-Factor IX and limitations imposed by the host immune response. Nat Med. 2006;12:342–7.
Scallan CD, Jiang H, Liu T, Patarroyo-White S, Sommer JM, Zhou S, Couto LB, Pierce GF. Human immunoglobulin inhibits liver transduction by AAV vectors at low AAV2 neutralizing titers in SCID mice. Blood. 2006;107:1810–7.
Mingozzi F, High KA. Immune responses to AAV in clinical trials. Curr Gene Ther. 2011;11:321–30.
Mingozzi F, Maus MV, Hui DJ, Sabatino DE, Murphy SL, Rasko JE, Ragni MV, Manno CS, Sommer J, Jiang H, Pierce GF, Ertl HC, High KA. CD8(+) T-cell responses to adeno-associated virus capsid in humans. Nat Med. 2007;13:419–22.
Mingozzi F, Meulenberg JJ, Hui DJ, Basner-Tschakarjan E, Hasbrouck NC, Edmonson SA, Hutnick NA, Betts MR, Kastelein JJ, Stroes ES, High KA. AAV-1-mediated gene transfer to skeletal muscle in humans results in dose-dependent activation of capsid-specific T cells. Blood. 2009;114:2077–86.
Mueller C, Chulay JD, Trapnell BC, Humphries M, Carey B, Sandhaus RA, McElvaney NG, Messina L, Tang Q, Rouhani FN, Campbell-Thompson M, Fu AD, Yachnis A, Knop DR, Ye GJ, Brantly M, Calcedo R, Somanathan S, Richman LP, Vonderheide RH, Hulme MA, Brusko TM, Wilson JM, Flotte TR. Human Treg responses allow sustained recombinant adeno-associated virus-mediated transgene expression. J Clin Invest. 2013;123:5310–8.
Keizer RJ, Huitema AD, Schellens JH, Beijnen JH. Clinical pharmacokinetics of therapeutic monoclonal antibodies. Clin Pharmacokinet. 2010;49:493–507.
Kessler M, Goldsmith D, Schellekens H. Immunogenicity of biopharmaceuticals. Nephrol Dial Transplant. 2006;21 Suppl 5:9–12.
Fang J, Yi S, Simmons A, Tu GH, Nguyen M, Harding TC, VanRoey M, Jooss K. An antibody delivery system for regulated expression of therapeutic levels of monoclonal antibodies in vivo. Mol Ther. 2007;15:1153–9.
Rivera VM, Gao GP, Grant RL, Schnell MA, Zoltick PW, Rozamus LW, Clackson T, Wilson JM. Long-term pharmacologically regulated expression of erythropoietin in primates following AAV-mediated gene transfer. Blood. 2005;105:1424–30.
Nguyen M, Huan-Tu G, Gonzalez-Edick M, Rivera VM, Clackson T, Jooss KU, Harding TC. Rapamycin-regulated control of antiangiogenic tumor therapy following rAAV-mediated gene transfer. Mol Ther. 2007;15:912–20.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 American Society of Gene and Cell Therapy
About this chapter
Cite this chapter
Schnepp, B.C., Johnson, P.R. (2015). Vector-Mediated Antibody Gene Transfer for Infectious Diseases. In: Berkhout, B., Ertl, H., Weinberg, M. (eds) Gene Therapy for HIV and Chronic Infections. Advances in Experimental Medicine and Biology(), vol 848. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-2432-5_8
Download citation
DOI: https://doi.org/10.1007/978-1-4939-2432-5_8
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-2431-8
Online ISBN: 978-1-4939-2432-5
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)