Abstract
Sepsis is among the most common causes of death in hospitalized patients, and early recognition followed by immediate initiation of therapy is an important concept to improve survival in these patients. According to the definition of sepsis, diagnosis of sepsis requires the recognition of the systemic inflammatory response syndrome (SIRS) caused by infection as well as recognition of possible infection-related organ dysfunctions for diagnosis of severe sepsis or septic shock. Both SIRS and organ dysfunctions may occur frequently in hospitalized patients for various reasons. However, the fast recognition of acute infection as a cause of SIRS and newly developed organ dysfunction may be a demanding task since culture-based results of microbiological samples will be available only days after onset of symptoms. Biomarkers and PCR-based pathogen detection may help the physician in differentiating SIRS from sepsis. Procalcitonin (PCT) is the best investigated biomarker for this purpose. Furthermore, the current data support the usage of PCT for guidance of antimicrobial therapy. C-reactive protein (CRP) may be used to monitor the course of infection but has only limited discriminative capabilities. Interleukin-6 is widely used for its fast response to the infectious stimulus, but conclusive data for the application of this biomarker are missing. None of the available biomarkers can by itself reliably differentiate SIRS from sepsis but can aid and shorten the decision process. PCR-based pathogen detection can theoretically shorten the recognition of the underlying pathogen to about 8 h. However, this technique is expensive and requires additional staff in the laboratory; controlled prospective studies are missing. Although current studies suggest that PCR-based pathogen detection may be useful to shorten time to adequate antimicrobial therapy and diagnose invasive Candida infections, no general recommendations about the application of PCR for the diagnosis of sepsis can be given.
Access this chapter
Tax calculation will be finalised at checkout
Purchases are for personal use only
Similar content being viewed by others
References
Angus DC, Linde-Zwirble WT, Lidicker J, Clermont G, Carcillo J, Pinsky MR (2001) Epidemiology of severe sepsis in the United States: analysis of incidence, outcome, and associated costs of care. Crit Care Med 29(7): 1303–1310
Levy MM, Artigas A, Phillips GS, Rhodes A, Beale R, Osborn T, Vincent JL, Townsend S, Lemeshow S, Dellinger RP (2012) Outcomes of the surviving sepsis campaign in intensive care units in the USA and Europe: a prospective cohort study. Lancet Infect Dis 12(12): 919–924
Engel C, Brunkhorst FM, Bone HG, Brunkhorst R, Gerlach H, Grond S, Gruendling M, Huhle G, Jaschinski U, John S et al (2007) Epidemiology of sepsis in Germany: results from a national prospective multicenter study. Intensive Care Med 33(4):606–618
Harrison DA, Welch CA, Eddleston JM (2006) The epidemiology of severe sepsis in England, Wales and Northern Ireland, 1996 to 2004: secondary analysis of a high quality clinical database, the ICNARC Case Mix Programme Database. Crit Care 10(2):R42
van Gestel A, Bakker J, Veraart CP, van Hout BA (2004) Prevalence and incidence of severe sepsis in Dutch intensive care units. Crit Care 8(4):R153–R162
Rohde JM, Odden AJ, Bonham C, Kuhn L, Malani PN, Chen LM, Flanders SA, Iwashyna TJ (2013) The epidemiology of acute organ system dysfunction from severe sepsis outside of the intensive care unit. J Hosp Med 8(5): 243–247
Hranjec T, Rosenberger LH, Swenson B, Metzger R, Flohr TR, Politano AD, Riccio LM, Popovsky KA, Sawyer RG (2012) Aggressive versus conservative initiation of antimicrobial treatment in critically ill surgical patients with suspected intensive-care-unit-acquired infection: a quasi-experimental, before and after observational cohort study. Lancet Infect Dis 12(10):774–780
Dellinger RP, Levy MM, Rhodes A, Annane D, Gerlach H, Opal SM, Sevransky JE, Sprung CL, Douglas IS, Jaeschke R et al (2013) Surviving sepsis campaign: international guidelines for management of severe sepsis and septic shock, 2012. Intensive Care Med 39(2):165–228
Bone RC, Fisher CJ Jr, Clemmer TP, Slotman GJ, Metz CA, Balk RA (1989) The methylprednisolone severe sepsis study group: sepsis syndrome—a valid clinical entity. Crit Care Med 17(5):389–393
ACCP/SCCM Consensus Conference Committee (1992) Definition for sepsis and organ failure and guidelines for the use of innovative therapies in sepsis. Crit Care Med 20(6): 864–874
Marshall JC (2010) Principles of source control in the early management of sepsis. Curr Infect Dis Rep 12(5):345–353
Rangel-Frausto MS, Pittet D, Costigan M, Hwang T, Davis CS, Wenzel RP (1995) The natural history of the systemic inflammatory response syndrome (SIRS). A prospective study. JAMA 273(2):117–123
Vincent JL (1997) Dear SIRS, I’m sorry to say that I don’t like you. Crit Care Med 25(2): 372–374
Larche J, Azoulay E, Fieux F, Mesnard L, Moreau D, Thiery G, Darmon M, Le Gall JR, Schlemmer B (2003) Improved survival of critically ill cancer patients with septic shock. Intensive Care Med 29(10):1688–1695
Kumar A, Roberts D, Wood KE, Light B, Parrillo JE, Sharma S, Suppes R, Feinstein D, Zanotti S, Taiberg L et al (2006) Duration of hypotension before initiation of effective antimicrobial therapy is the critical determinant of survival in human septic shock. Crit Care Med 34(6):1589–1596
Levy MM, Dellinger RP, Townsend SR, Linde-Zwirble WT, Marshall JC, Bion J, Schorr C, Artigas A, Ramsay G, Beale R et al (2010) The surviving sepsis campaign: results of an international guideline-based performance improvement program targeting severe sepsis. Crit Care Med 38(2):367–374
Gaieski DF, Mikkelsen ME, Band RA, Pines JM, Massone R, Furia FF, Shofer FS, Goyal M (2010) Impact of time to antibiotics on survival in patients with severe sepsis or septic shock in whom early goal-directed therapy was initiated in the emergency department. Crit Care Med 38(4):1045–1053
Ferrer R, Artigas A, Suarez D, Palencia E, Levy MM, Arenzana A, Perez XL, Sirvent JM (2009) Effectiveness of treatments for severe sepsis: a prospective multicenter observational study. Am J Respir Crit Care Med 180(9): 861–866
Shapiro NI, Wolfe RE, Moore RB, Smith E, Burdick E, Bates DW (2003) Mortality in Emergency Department Sepsis (MEDS) score: a prospectively derived and validated clinical prediction rule. Crit Care Med 31(3): 670–675
Lee CC, Chen SY, Tsai CL, Wu SC, Chiang WC, Wang JL, Sun HY, Chen SC, Chen WJ, Hsueh PR (2008) Prognostic value of mortality in emergency department sepsis score, procalcitonin, and C-reactive protein in patients with sepsis at the emergency department. Shock 29(3):322–327
Zhao Y, Li C, Jia Y (2013) Evaluation of the Mortality in Emergency Department Sepsis score combined with procalcitonin in septic patients. Am J Emerg Med 31(7): 1086–1091
Ghanem-Zoubi NO, Vardi M, Laor A, Weber G, Bitterman H (2011) Assessment of disease-severity scoring systems for patients with sepsis in general internal medicine departments. Crit Care 15(2):R95
Bastani A, Galens S, Rocchini A, Walch R, Shaqiri B, Palomba K, Milewski AM, Falzarano A, Loch D, Anderson W (2012) ED identification of patients with severe sepsis/septic shock decreases mortality in a community hospital. Am J Emerg Med 30(8):1561–1566
Calandra T, Cohen J (2005) The international sepsis forum consensus conference on definitions of infection in the intensive care unit. Crit Care Med 33(7):1538–1548
Levy MM, Fink MP, Marshall JC, Abraham E, Angus D, Cook D, Cohen J, Opal SM, Vincent JL, Ramsay G (2003) 2001 SCCM/ESICM/ACCP/ATS/SIS international sepsis definitions conference. Crit Care Med 31(4):1250–1256
Gabay C, Kushner I (1999) Acute-phase proteins and other systemic responses to inflammation. N Engl J Med 340(6):448–454
van Vugt SF, Broekhuizen BD, Lammens C, Zuithoff NP, de Jong PA, Coenen S, Ieven M, Butler CC, Goossens H, Little P et al (2013) Use of serum C reactive protein and procalcitonin concentrations in addition to symptoms and signs to predict pneumonia in patients presenting to primary care with acute cough: diagnostic study. BMJ 346:f2450
Eberhard OK, Haubitz M, Brunkhorst FM, Kliem V, Koch KM, Brunkhorst R (1997) Usefulness of procalcitonin for differentiation between activity of systemic autoimmune disease (systemic lupus erythematosus/systemic antineutrophil cytoplasmic antibody-associated vasculitis) and invasive bacterial infection. Arthritis Rheum 40(7):1250–1256
Meisner M, Adina H, Schmidt J (2006) Correlation of procalcitonin and C-reactive protein to inflammation, complications, and outcome during the intensive care unit course of multiple-trauma patients. Crit Care 10(1):R1
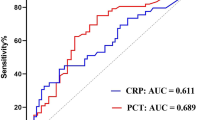
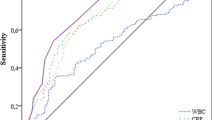
Simon L, Gauvin F, Amre DK, Saint-Louis P, Lacroix J (2004) Serum procalcitonin and C-reactive protein levels as markers of bacterial infection: a systematic review and meta-analysis. Clin Infect Dis 39(2):206–217
Su L, Han B, Liu C, Liang L, Jiang Z, Deng J, Yan P, Jia Y, Feng D, Xie L (2012) Value of soluble TREM-1, procalcitonin, and C-reactive protein serum levels as biomarkers for detecting bacteremia among sepsis patients with new fever in intensive care units: a prospective cohort study. BMC Infect Dis 12:157
Schmit X, Vincent JL (2008) The time course of blood C-reactive protein concentrations in relation to the response to initial antimicrobial therapy in patients with sepsis. Infection 36(3): 213–219
Hoeboer SH, Groeneveld AB (2013) Changes in circulating procalcitonin versus C-reactive protein in predicting evolution of infectious disease in febrile, critically ill patients. PLoS One 8(6):e65564
Povoa P, Teixeira-Pinto AM, Carneiro AH (2011) C-reactive protein, an early marker of community-acquired sepsis resolution: a multi-center prospective observational study. Crit Care 15(4):R169
Becker K, Müller B, Nylen ES (2001) Calcitonin gene family of peptides. In: Becker K (ed) Principles and practice of endocrinology and metabolism, 3rd edn. J.B. Lippincott Co., Philadelphia, PA, pp 520–534
Bloos F, Marshall JC, Dellinger RP, Vincent JL, Gutierrez G, Rivers E, Balk RA, Laterre PF, Angus DC, Reinhart K et al (2011) Multinational, observational study of procalcitonin in ICU patients with pneumonia requiring mechanical ventilation: a multicenter observational study. Crit Care 15:R88. doi:10.1186/cc10087
Brunkhorst FM, Heinz U, Forycki ZF (1998) Kinetics of procalcitonin in iatrogenic sepsis. Intensive Care Med 24(8):888–889
Wacker C, Prkno A, Brunkhorst FM, Schlattmann P (2013) Procalcitonin as a diagnostic marker for sepsis: a systematic review and meta-analysis. Lancet Infect Dis 13(5): 426–435
Reinhart K, Meisner M (2011) Biomarkers in the critically ill patient: procalcitonin. Crit Care Clin 27(2):253–263
Dou YH, Du JK, Liu HL, Shong XD (2013) The role of procalcitonin in the identification of invasive fungal infection-a systemic review and meta-analysis. Diagn Microbiol Infect Dis 76:464–469
Karlsson S, Heikkinen M, Pettila V, Alila S, Vaisanen S, Pulkki K, Kolho E, Ruokonen E, Finnsepsis Study Group (2010) Predictive value of procalcitonin decrease in patients with severe sepsis: a prospective observational study. Crit Care 14(6):R205
Charles PE, Tinel C, Barbar S, Aho S, Prin S, Doise JM, Olsson NO, Blettery B, Quenot JP (2009) Procalcitonin kinetics within the first days of sepsis: relationship with the appropriateness of antibiotic therapy and the outcome. Crit Care 13(2):R38
Schuetz P, Maurer P, Punjabi V, Desai A, Amin D, Gluck E (2013) Procalcitonin decrease over 72 hours in US critical care units predicts fatal outcome in sepsis patients. Crit Care 17(3): R115
Christ-Crain M, Jaccard-Stolz D, Bingisser R, Gencay MM, Huber PR, Tamm M, Muller B (2004) Effect of procalcitonin-guided treatment on antibiotic use and outcome in lower respiratory tract infections: cluster-randomised, single-blinded intervention trial. Lancet 363 (9409):600–607
Christ-Crain M, Stolz D, Bingisser R, Muller C, Miedinger D, Huber PR, Zimmerli W, Harbarth S, Tamm M, Muller B (2006) Procalcitonin guidance of antibiotic therapy in community-acquired pneumonia: a randomized trial. Am J Respir Crit Care Med 174(1): 84–93
Schuetz P, Briel M, Christ-Crain M, Stolz D, Bouadma L, Wolff M, Luyt CE, Chastre J, Tubach F, Kristoffersen KB et al (2012) Procalcitonin to guide initiation and duration of antibiotic treatment in acute respiratory infections: an individual patient data meta-analysis. Clin Infect Dis 55(5):651–662
Heyland DK, Johnson AP, Reynolds SC, Muscedere J (2011) Procalcitonin for reduced antibiotic exposure in the critical care setting: a systematic review and an economic evaluation. Crit Care Med 39(7):1792–1799
Nobre V, Harbarth S, Graf JD, Rohner P, Pugin J (2008) Use of procalcitonin to shorten antibiotic treatment duration in septic patients: a randomized trial. Am J Respir Crit Care Med 177(5):498–505
Sponholz C, Sakr Y, Reinhart K, Brunkhorst F (2006) Diagnostic value and prognostic implications of serum procalcitonin after cardiac surgery: a systematic review of the literature. Crit Care 10(5):R145
Schuetz P, Affolter B, Hunziker S, Winterhalder C, Fischer M, Balestra GM, Hunziker P, Marsch S (2010) Serum procalcitonin, C-reactive protein and white blood cell levels following hypothermia after cardiac arrest: a retrospective cohort study. Eur J Clin Invest 40(4):376–381
Giovanella L, Verburg FA, Imperiali M, Valabrega S, Trimboli P, Ceriani L (2013) Comparison of serum calcitonin and procalcitonin in detecting medullary thyroid carcinoma among patients with thyroid nodules. Clin Chem Lab Med 51(7):1477–1481
Song M, Kellum JA (2005) Interleukin-6. Crit Care Med 33(12 Suppl):S463–S465
Miguel-Bayarri V, Casanoves-Laparra EB, Pallas-Beneyto L, Sancho-Chinesta S, Martin-Osorio LF, Tormo-Calandin C, Bautista-Rentero D (2012) Prognostic value of the biomarkers procalcitonin, interleukin-6 and C-reactive protein in severe sepsis. Med Intensiva 36(8):556–562
Pettila V, Hynninen M, Takkunen O, Kuusela P, Valtonen M (2002) Predictive value of procalcitonin and interleukin 6 in critically ill patients with suspected sepsis. Intensive Care Med 28(9):1220–1225
Tschaikowsky K, Hedwig-Geissing M, Braun GG, Radespiel-Troeger M (2011) Predictive value of procalcitonin, interleukin-6, and C-reactive protein for survival in postoperative patients with severe sepsis. J Crit Care 26(1): 54–64
Oberhoffer M, Russwurm S, Bredle D, Chatzinicolaou K, Reinhart K (2000) Discriminative power of inflammatory markers for prediction of tumor necrosis factor-alpha and interleukin-6 in ICU patients with systemic inflammatory response syndrome (SIRS) or sepsis at arbitrary time points. Intensive Care Med 26(Suppl 2):S170–S174
Harbarth S, Holeckova K, Froidevaux C, Pittet D, Ricou B, Grau GE, Vadas L, Pugin J (2001) Diagnostic value of procalcitonin, interleukin-6, and interleukin-8 in critically ill patients admitted with suspected sepsis. Am J Respir Crit Care Med 164(3):396–402
Tsalik EL, Jaggers LB, Glickman SW, Langley RJ, van Velkinburgh JC, Park LP, Fowler VG, Cairns CB, Kingsmore SF, Woods CW (2012) Discriminative value of inflammatory biomarkers for suspected sepsis. J Emerg Med 43(1): 97–106
Reinhart K, Bauer M, Riedemann NC, Hartog CS (2012) New approaches to sepsis: molecular diagnostics and biomarkers. Clin Microbiol Rev 25(4):609–634
Bouchon A, Facchetti F, Weigand MA, Colonna M (2001) TREM-1 amplifies inflammation and is a crucial mediator of septic shock. Nature 410(6832):1103–1107
Gibot S, Kolopp-Sarda MN, Bene MC, Cravoisy A, Levy B, Faure GC, Bollaert PE (2004) Plasma level of a triggering receptor expressed on myeloid cells-1: its diagnostic accuracy in patients with suspected sepsis. Ann Intern Med 141(1):9–15
Jeong SJ, Song YG, Kim CO, Kim HW, Ku NS, Han SH, Choi JY, Kim JM (2012) Measurement of plasma sTREM-1 in patients with severe sepsis receiving early goal-directed therapy and evaluation of its usefulness. Shock 37(6):574–578
Wu Y, Wang F, Fan X, Bao R, Bo L, Li J, Deng X (2012) Accuracy of plasma sTREM-1 for sepsis diagnosis in systemic inflammatory patients: a systematic review and meta-analysis. Crit Care 16(6):R229
Guha M, Mackman N (2001) LPS induction of gene expression in human monocytes. Cell Signal 13(2):85–94
Wright SD, Ramos RA, Tobias PS, Ulevitch RJ, Mathison JC (1990) CD14, a receptor for complexes of lipopolysaccharide (LPS) and LPS binding protein. Science 249(4975):1431–1433
Sakr Y, Burgett U, Nacul FE, Reinhart K, Brunkhorst F (2008) Lipopolysaccharide binding protein in a surgical intensive care unit: a marker of sepsis? Crit Care Med 36(7):2014–2022
Prucha M, Herold I, Zazula R, Dubska L, Dostal M, Hildebrand T, Hyanek J (2003) Significance of lipopolysaccharide-binding protein (an acute phase protein) in monitoring critically ill patients. Crit Care 7(6):R154–R159
Tschaikowsky K, Hedwig-Geissing M, Schmidt J, Braun GG (2011) Lipopolysaccharide-binding protein for monitoring of postoperative sepsis: complemental to C-reactive protein or redundant? PLoS One 6(8):e23615
Chang SS, Hsieh WH, Liu TS, Lee SH, Wang CH, Chou HC, Yeo YH, Tseng CP, Lee CC (2013) Multiplex PCR system for rapid detection of pathogens in patients with presumed sepsis: a systemic review and meta-analysis. PLoS One 8(5):e62323
Bloos F, Hinder F, Becker K, Sachse S, Mekontso Dessap A, Straube E, Cattoir V, Brun-Buisson C, Reinhart K, Peters G et al (2010) A multicenter trial to compare blood culture with polymerase chain reaction in severe human sepsis. Intensive Care Med 36(2): 241–247
Bloos F, Sachse S, Kortgen A, Pletz MW, Lehmann M, Straube E, Riedemann NC, Reinhart K, Bauer M (2012) Evaluation of a polymerase chain reaction assay for pathogen detection in septic patients under routine condition: an observational study. PLoS One 7(9): e46003
Avni T, Leibovici L, Paul M (2011) PCR diagnosis of invasive candidiasis: systematic review and meta-analysis. J Clin Microbiol 49(2): 665–670
Bloos F, Bayer O, Sachse S, Straube E, Reinhart K, Kortgen A (2013) Attributable costs of patients with candidemia and potential implications of polymerase chain reaction-based pathogen detection on antifungal therapy in patients with sepsis. J Crit Care 28(1):2–8
Hebart H, Klingspor L, Klingebiel T, Loeffler J, Tollemar J, Ljungman P, Wandt H, Schaefer-Eckart K, Dornbusch HJ, Meisner C et al (2009) A prospective randomized controlled trial comparing PCR-based and empirical treatment with liposomal amphotericin B in patients after allo-SCT. Bone Marrow Transplant 43(7): 553–561
Pletz MW, Wellinghausen N, Welte T (2011) Will polymerase chain reaction (PCR)-based diagnostics improve outcome in septic patients? A clinical view. Intensive Care Med 37(7): 1069–1076
Bouadma L, Luyt CE, Tubach F, Cracco C, Alvarez A, Schwebel C, Schortgen F, Lasocki S, Veber B, Dehoux M et al (2010) Use of procalcitonin to reduce patients’ exposure to antibiotics in intensive care units (PRORATA trial): a multicentre randomised controlled trial. Lancet 375(9713):463–474
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer Science+Business Media New York
About this protocol
Cite this protocol
Bloos, F. (2015). Clinical Diagnosis of Sepsis and the Combined Use of Biomarkers and Culture- and Non-Culture-Based Assays. In: Mancini, N. (eds) Sepsis. Methods in Molecular Biology, vol 1237. Humana Press, New York, NY. https://doi.org/10.1007/978-1-4939-1776-1_19
Download citation
DOI: https://doi.org/10.1007/978-1-4939-1776-1_19
Published:
Publisher Name: Humana Press, New York, NY
Print ISBN: 978-1-4939-1775-4
Online ISBN: 978-1-4939-1776-1
eBook Packages: Springer Protocols