Abstract
Glycolipids and gangliosides play important roles in maintaining the functional integrity of the nervous system. However, surprisingly little is known about how glycolipids and gangliosides in particular participate in various neurodegenerative processes. For example, it has been known for a long time that administration of gangliosides and in particular, GM1 ganglioside, can ameliorate damage to the central and peripheral nervous systems and can mitigate effects of a variety of neurodegenerative processes. What is not known is the extent to which dysfunctional biosynthesis or metabolism of gangliosides may be involved in various neurodegenerative disorders and if alterations observed reflect an intrinsic disease-related process or represent the response of the brain to a degenerative process. This chapter briefly reviews recent advances in the study of glycolipids and gangliosides and their potential participation in a variety of neurodegenerative disorders including Parkinson’s disease, Alzheimer’s disease, Huntington’s disease and the potential link between Gaucher disease and Parkinson’s disease.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
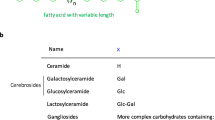
Glycolipids are broadly defined as lipids with a carbohydrate attached. There are a wide variety of glycolipids found in biological systems. Of particular relevance for the nervous system is a subset of glycolipids known as glycosphingolipids that contain sphingosine. A further subset of glycosphingolipids of particular relevance to the structure and function of the nervous system are cerebrosides and gangliosides. Glycosphingolipids are present on cell surface membranes and are particularly abundant in the brain (Hirabayashi 2012). Cerebrosides comprise a group of glycosphingolipids consisting of ceramide and sugar residues, the major forms being glucocerebrosides and galactocerebrosides. Gangliosides are sialic acid-containing glycosphingolipids that are integral components of cell surface membranes and are highly enriched in the central nervous system. The major ganglioside species in brain are a- and b-series gangliosides and consist of the major gangliosides GM1, GD1a, GD1b, and GT1b. GM1 ganglioside, a main component of membrane signaling domains (lipid rafts), is particularly important in the central nervous system (CNS) as it plays important roles in neuronal development and survival and modulates a wide variety of cellular functions through modulation of cell signaling mechanisms. GM1 has been shown to exert neurotrophic or neuroprotective effects under a variety of circumstances and influences numerous cellular activities mediated at the level of the plasma membrane as well as intracellularly, where it influences Ca2+ homeostasis, mitochondrial function, and lysosomal integrity, among other processes (Hakomori and Igarashi 1993; Allende and Proia 2002; Shield et al. 2006; Wei et al. 2009).
This brief review focuses on recent advances in the description and understanding of the role of glycolipids and in particular, gangliosides and glucocerebrosides, in neurodegenerative disorders. This review focuses on Parkinson’s disease, Alzheimer’s disease, and Huntington’s Disease and the accumulating evidence for a link between Parkinson’s disease and Gaucher disease.
20.1 Gangliosides and Parkinson’s Disease
GM1 ganglioside has long been suggested as a potential agent for the treatment of Parkinson’s disease, although the precise reasons for the efficacy of GM1 in animal models of Parkinson’s disease and in Parkinson’s disease patients is still unclear. Toffano et al. (1983) first described the ability of GM1 ganglioside to enhance recovery of the nigrostriatal projection system. In this initial study, administration of GM1 ganglioside (30 mg/kg, beginning the second day after surgery) to rats that received unilateral hemitransections of ascending nigrostriatal dopaminergic fibers significantly increased striatal tyrosine hydroxylase (TH) activity, homovanillic acid (HVA) content, TH immunohistochemical staining ipsilateral to the hemitransection and reduced apomorphine-induced rotations. These data were the first demonstration of improvement of biochemical, morphological, and behavioral parameters associated with damage to the nigrostriatal pathway with GM1 treatment (Toffano et al. 1983). Over the next couple of decades, numerous studies were performed showing that administration of GM1 ganglioside at least partially reversed detrimental effects of various types of insults to the nigrostriatal dopamine system including mechanical transection (Agnati et al. 1983; Toffano et al. 1983, 1984), 1-methyl-4-phenyl, 1,2,3,6-tetrahydropyridine (MPTP) toxin-induced lesions (Hadjiconstantinou et al. 1986; Schneider and Yuwiler 1989; Hadjiconstantinou and Neff 1988), and, 6-hydroxydopamine-induced lesions (Tilson et al. 1988) to the nigrostriatal dopamine system, as well as ameliorate age-related dopaminergic changes in brain. Results in normal aged animals are particularly interesting in that GM1 administration restored a variety of dopaminergic markers in the striatum and substantia nigra to levels approximate to those seen in young animals (Goettl et al. 1999, 2003). Although GM1 administration had little effect on several measures of motor function assessed in aged animals (Goettl et al. 2001), improvements in cognitive functioning (i.e., spatial learning and memory) were described (Fong et al. 1997). Although relatively few papers have examined age-related changes in ganglioside content in brain, in rats, GM1 levels in whole brain were reported to be fairly consistent between 3 and 24 months of age, while GD1a and GT1b levels decreased (Aydin et al. 2000). These data need to be viewed cautiously as there are significant regional differences in ganglioside content in brain that might be obscured by examining whole brain expression. Regional expression of gangliosides examined in human brain showed variation by region and age (between 4 months and 80/90 years of age), with GM1 levels significantly decreased with advanced age in the frontal cortex and moderately decreased in hippocampus (Kracun et al. 1992b), with a possible shift in expression from the a- to b-series gangliosides with aging (see Chap. 19).
While most of the experimental work with GM1 and Parkinson’s disease models was performed with rodents, studies using nonhuman primate models of Parkinson’s disease also showed significant improvements with GM1 treatment. In MPTP-treated monkeys, GM1 treatment resulted in improved motor and cognitive functioning, compared to saline-treated lesion control animals, and also resulted in small but statistically significant increases in striatal dopamine levels and increased density of tyrosine hydroxylase (TH)-positive fibers (Schneider et al. 1992). Other studies showed that GM1 treatment resulted in significant increases in TH protein levels in residual dopaminergic neurons in the substantia nigra of MPTP-treated monkeys (Herrero et al. 1993).
These promising preclinical research findings led to clinical studies of GM1 treatment in Parkinson’s disease patients. All clinical studies using GM1 were approved by the appropriate institutional ethics committees, performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki, and written informed consent was obtained from all subjects prior to enrollment. Following a small phase I safety study (Schneider et al. 1995b), a randomized, double-blind, placebo-controlled trial was conducted with 45 Parkinson’s disease patients (N = 22 GM1; N = 23 placebo) over a 16-week study period (Schneider et al. 1998). At the study initiation visit, subjects received intravenous infusion of 1,000 mg GM1 or placebo and then received two subcutaneous injections per day (GM1 100 mg/2 ml per injection or placebo) for the remainder of the 16 week study period. The primary efficacy measure was change from baseline in the Unified Parkinson’s Disease Rating Scale (UPDRS) motor score, assessed during a practically defined off period (that is, in the morning after at least 12 h from the last dose of any anti-Parkinson medication). The GM1-treated group showed significant improvements in UPDRS motor scores compared to subjects receiving placebo (Schneider et al. 1998). The treatment effect size at week 16 was −6.79 ± 1.24 (p < 0.0002). Secondary measures of activities of daily living and performance of timed motor tests also showed significant effects in favor of the GM1-treated subjects (Schneider et al. 1998). GM1 was well tolerated and no serious adverse effects were noted. This brief duration study suggested that GM1 could have a symptomatic effect in Parkinson’s disease patients. Although the precise mechanisms underlying this response are not known, the effects observed in this study are consistent with preclinical data demonstrating an ability of GM1 to enhance TH expression and dopamine synthesis in residual neurons in animal models of Parkinson’s disease (Herrero et al. 1993; Schneider et al. 1995a).
A group of subjects who completed the study described above consented to continue to receive GM1 and to be followed clinically for up to 5 years (Schneider et al. 2010). In this open extension study (26 subjects at start; 13 from the prior placebo group and 13 from the prior GM1-treated group), subjects were administered a total daily dose of 200 mg GM1 by subcutaneous injection (two injections of 100 mg GM1 per day). Subjects were evaluated during practically defined off periods at 6 month intervals over the course of the study. Changes in UPDRS motor scores and activities of daily living scores were assessed as were timed tests of motor function. In subjects who received GM1 during the previous randomized study, regression modeling showed a slow linear increase of the average UPDRS motor score over time, with an estimated annual rate of increase of approximately 1.2 points (95 % confidence interval, CI: −0.1 to 2.5, p = 0.06) (Schneider et al. 2010). However, at the end of 5 years of continuous GM1 use, the estimated average UPDRS motor score (for the ten subjects who continued through the entire 5 year period) was still lower than that at baseline prior to randomization into the main randomized trial, suggesting that improvements achieved during the initial study were maintained during the open extension period. In subjects previously randomized to receive placebo but who received GM1 during the open-extension study, regression modeling also showed a change in the average UPDRS motor scores over time. Over the first 2 years of the extension study, motor scores decreased by about 3–4 points per year on average while in later years, the scores increased slightly and approached pre-randomization levels by the fifth year. However, for nine of the ten subjects followed for the full 5 year period, no appreciable progression of motor symptoms was observed. This relatively small open label study suggested that chronic use of GM1 in PD patients was safe (no serious adverse events reported over the course of the study) and may be beneficial in Parkinson’s disease patients. However, without a control group, it is not possible to come to any firm conclusions regarding the long-term efficacy of GM1 as a potential disease modifying agent in Parkinson’s disease.
In order to better assess efficacy of GM1 as a potential disease modifying therapy for Parkinson’s disease, a randomized, controlled, delayed start trial of GM1 in Parkinson’s disease was conducted (Schneider et al. 2013). Due to the complex nature of Parkinson’s disease, there are several challenges in the clinical assessment of disease progression and the demonstration of disease modification, since many drugs with potential disease modifying effects may also exert symptomatic effects. Since we had previously shown that GM1 may potentially have both symptomatic and disease modifying effects on Parkinson’s disease, a study design, the delayed start study, previously suggested to possibly differentiate between these aspects of drug response (Olanow et al. 2008, 2009; D’Agostino 2009) was used. In the delayed start trial design, subjects are initially randomized to either an early start group (i.e., randomized to receive GM1 and to continue to receive GM1 for the duration of the trial (out to week 120)) or a delayed start group (randomized to receive placebo but switched to GM1 after 24 weeks). In addition, a separate group of standard-of-care subjects (“Comparison group”) was recruited according to the same criteria used for recruitment of the treatment groups and these subjects were assessed longitudinally to provide descriptive information regarding disease progression. The primary outcome measure in this study was change from baseline UPDRS motor scores assessed during a practically defined off period. Subjects were also evaluated during their best on period (i.e., typically at least 1 h. after taking their standard anti-Parkinson medication). At week 24, the early-start (GM1) group showed significant improvement in UPDRS motor scores compared to a significant worsening of scores in the delayed-start (placebo) group (Fig. 20.1). The early-start group also showed a sustained benefit compared to the delayed-start group at the end of the study (week 120) (Fig. 20.1). Following an initial improvement in UPDRS motor scores in the early-start group, this measure of symptom severity changed little over the course of the study and by the end of the observation period, these scores were still lower (i.e., improved) than they were at study baseline (Schneider et al. 2013). The standard-of-care comparison group showed a pattern of symptom progression different from both the early-start subjects who received GM1 throughout the study and the delayed-start subjects after they started receiving GM1 after week 24 (Schneider et al. 2013). Both early-start and delayed-start groups showed significant symptom worsening during washout (assessed at 1–2 years after the last use of GM1) (Fig. 20.1). The results of this study supported the previous report that GM1 use for a relatively short period of time was superior to placebo for improving motor symptoms and showed that extended GM1 use (up to 120 weeks) resulted in a lower than expected rate of symptom progression (also suggested in the previous open label study). Thus, the data from this relatively small study suggested that GM1 may have symptomatic and potentially disease modifying effects on Parkinson’s disease.
Changes in unified Parkinson’s disease rating scale (UPDRS) motor subsection scores. (a) The mean (±SE) change from baseline (observed scores) in Early-start and Delayed-start study subjects and in the standard-of-care Comparison group, assessed in the practically defined “off” condition. The dashed vertical line at week 24 indicates the end of study Phase I. The dashed vertical line at week 120 indicates the end of study Phase II. The horizontal dashed line indicates baseline level. An increase of score indicates symptom worsening; a decrease in score indicates symptom improvement. *p < 0.0001 Early-start vs. Delayed-start; ^p < 0.05 Early-start vs. Delayed-start. (b) The mean (±SE) change from baseline in Early-start and Delayed-start study subjects and in the standard-of-care Comparison group, assessed in the best “on” condition. The dashed vertical line at week 24 indicates the end of study Phase I. The dashed vertical line at week 120 indicates the end of study Phase II. The horizontal dashed line indicates baseline level. *p < 0.01 Early-start vs. Delayed-start. [Reprinted from Schneider JS, Gollomp SM, Sendek S, Colcher A, Cambi F, and Du W (2013) A randomized, controlled, delayed start trial of GM1 ganglioside in treated Parkinson’s disease patients. Journal of the Neurological Sciences 324:140–148
Despite the positive effects of GM1 on preclinical models of Parkinson’s disease and positive effects of GM1 in Parkinson’s disease patients, the mechanisms underlying these effects remain somewhat obscure. We have suggested that at least in part, the apparent neuroprotective/neurorestorative effects of GM1 may involve modulation of lipid raft structure/function by altering the GM1 content of the rafts that could exert significant influence on a variety of signaling pathways (Schneider et al. 2013). Further, several Parkinson’s disease-relevant proteins such as alpha synuclein, LRRK2, parkin, and PINK1 associate with lipid rafts and co-localize with GM1, potentially influencing neurodegeneration in Parkinson’s disease (Martinez et al. 2007; Fallon et al. 2002; Hatano et al. 2007). One reason why GM1 may seemingly work so well in Parkinson’s disease is that administration of GM1 to Parkinson’s disease patients may represent GM1 replacement therapy, that is, restores a deficiency in GM1 levels (see Chap. 15). This would only be true if there is in fact a decrease in GM1 levels in the Parkinson’s disease brain, and specifically, in the nigrostriatal dopamine system. Recent data from our lab (Kidd et al. 2012) and others (Wu et al. 2012) suggest that GM1 levels may be lower than normal in the substantia nigra of Parkinson’s disease patients compared to age matched controls. This may be due to lower levels of GM1 in residual neurons. Additionally, we have made the novel observation that expression of key glycosyltransferase genes B3Galt4 (the gene encoding the glycosyltransferase necessary for conversion of GM2 into GM1) and St3gal2 (the gene encoding the sialyltransferase necessary for conversion of GM1 into GD1A) are decreased in the substantia nigra in Parkinson’s disease brains compared with age-matched controls (Kidd et al. 2012). We have also recently observed increases in gene expression in Parkinson’s disease substantia nigra for at least some of the enzymes responsible for the production of both a- and b-series gangliosides (i.e. St3Gal5, St8sia3, see Chap. 9 for metabolic pathways), compared to samples from neurologically intact, age-matched controls (Mettil et al. 2013). These findings together suggest that in addition to a loss of GM1 in the Parkinson’s disease substantia nigra, there may also be an imbalance between a- and b-series gangliosides. More work is needed in order to understand the extent to which there is indeed a defect in GM1 expression in the Parkinson’s disease brain and if so, the extent to which this defect is specific to the nigrostriatal dopamine system.
20.2 Gangliosides in Alzheimer’s Disease
Several lines of evidence have linked Alzheimer’s disease (AD) with aberrant lipid homeostasis and with abnormal expression of gangliosides. There have been a number of reports of decreased ganglioside concentrations in various regions of the AD brain dating back to the late 1960s, but some of these findings have been contradictory and lacked experimental consistency in the way in which gangliosides were measured and in the pathological confirmation of AD and AD subtypes. Gottfries et al. (1983) described a decreased expression of brain gangliosides in AD brain but the pattern of ganglioside expression was not evaluated. Kalanj et al. (1991) and Kracun et al. (1992a) reported that in AD brain, all ganglio-series gangliosides (i.e., GM1, GD1a, GD1b, and GT1b) were decreased in temporal and frontal cortices as well as in the nucleus basalis of Meynert, while gangliosides GM2, GD3, and GM3 were elevated in frontal and parietal cortex. Svennerholm and Gottfries (1994) described significant decreases in gangliosides in frontal and temporal cortices, caudate nucleus, and hippocampus in AD type I cases (early onset form) and more restricted loss of gangliosides in temporal cortex, hippocampus and frontal white matter in AD type II (late onset) cases. These authors suggested that based on a diminished yield of synaptosomes in AD type I brains that there was marked loss of synapses and neuronal processes in the AD type I brain. Studies examining CSF from AD patients showed increased GM1 in CSF in early onset AD compared to late onset AD, suggested by the authors to indicate more severe neurodegeneration in type I vs. type II AD patients (Blennow et al. 1991).
Recent evidence, however, suggests that more than simple measurement of ganglioside levels in AD brain may be needed to better appreciate the role that gangliosides might play in the pathophysiology of AD. More complex alterations in the lipid profile in brain may be associated with AD, with region-specific lipid anomalies potentially linked to AD pathogenesis (Chan et al. 2012). Aberrant lipid homeostasis has been suggested to play a role in AD as the neuronal lipid composition regulates activity of key proteins such as APP, BACE1 and presenilin that control Aβ levels (Chan et al. 2012). Gangliosides (GM1 in particular) have been suggested to modulate the pathogenic potential of Aβ by influencing its aggregation properties. A number of studies have suggested that the interaction of Aβ with GM1 results in GM1-bound Aβ that acts as a seed for the Aβ fibrillogenesis in the AD brain (Yanagisawa 2007). Recent data further suggest that Aβ is preferentially incorporated into GM1-rich membrane regions (i.e., lipid rafts) where the peptides undergo a conformational shift that disrupts membrane stability and promotes peptide–peptide interaction and oligomer formation (Haughey et al. 2010). Although the precise role of gangliosides and other lipids in AD remains to be determined, it is clear that alterations in sphingolipid metabolism and expression likely play an important role in the pathological processes contributing to AD. The role of GM1 ganglioside in particular in AD remains to be elucidated as some reports suggest that GM1 administration may be at least partially neuroprotective in model systems (Kreutz et al. 2011) and in humans (Svennerholm et al. 2002).
20.3 Gangliosides and Huntington’s Disease
Desplats et al. (2007) reported abnormal expression levels of various genes encoding glycosyltransferases and sialyltransferases that are involved in the biosynthesis of various gangliosides in the striatum of Huntington’s disease transgenic mice (R6/1 mice) and in postmortem caudate nucleus tissue from Huntington’s disease patients. In particular, increased expression of St8sia1 (encoding GD3 synthase) and decreased expression of St8sia2, St8sia3 (GD3 synthase) and B4galnt1 (GM2/GD2 synthase) was found in the striatum of R6/1 transgenic Huntington’s disease mice. The mRNA expression levels of St3gal5 (encoding GM3 synthase), St3gal2 (encoding GM1b/GD1a/GT1b synthase), and St6galnac5 (SiaT7e) were not affected in the R6/1 transgenic mice (Desplats et al. 2007). Ganglioside analysis showed a significant decrease in GM1 levels in striatum from R6/1 transgenic mice (Desplats et al. 2007). The gene expression of St3gal5, St8sia3, B4galnt1, and St3gal2 were significantly decreased in the caudate nucleus from HD patients. However, in human Huntington’s disease caudate, an overall decrease in ganglioside levels was reported, compared to control subjects with the exception of a specific increase in GD3 levels (Desplats et al. 2007). This could be significant as GD3 may be an apoptogenic ganglioside (Scorrano et al. 1999) and increased levels of GD3 in Huntington’s disease caudate could contribute to apoptotic neurodegeneration. Although these data are from a very small sample of Huntington’s patients (i.e., three cases), they do suggest altered ganglioside biosynthesis and expression associated with Huntington’s disease.
Following up on these data, Maglione et al. (2010) described decreased expression of B3galt4 (GM1/GD1b synthase) mRNA and reduced levels of GM1 ganglioside in cell and animal models of Huntington’s disease as well as in fibroblasts isolated from Huntington’s disease patients (Maglione et al. 2010). They further reported that the presence of mutant huntingtin protein affected ganglioside metabolism in a transgenic mouse Huntington’s disease model, with reduced GM1, GD1a, and GT1b levels noted in striatum and cortex (Maglione et al. 2010). Administration of GM1 to a knock-in cell model of Huntington’s disease restored GM1 levels and protected cells from apoptosis. GM1 administration also promoted AKT activation and resulted in phosphorylation of mutant huntingtin protein which may support neuroprotection and perhaps decrease toxicity of the mutant protein (Maglione et al. 2010). Importantly, this study demonstrated that relatively small alterations of GM1 content in the plasma membrane could cause significant changes in cell susceptibility to apoptosis.
As a follow up to the findings that levels of GM1 may be decreased in the HD brain (as well as in HD models), Di Pardo et al. (2012) demonstrated that administering GM1 by intraventricular infusion in a mouse HD model ((YAC)128 mice) restored normal motor behavior, increased striatal expression of DARP-32, a protein highly enriched in intrinsic striatal neurons, and increased phosphorylation of huntingtin at serine 13 and serine 16, suggested a potential role for GM1 in the treatment of HD.
20.4 Role of Glycolipids in the Link Between Parkinson’s Disease and Gaucher Disease
A possible connection between Gaucher disease and Parkinson’s disease has recently been suggested, although the molecular link between the two diseases is still somewhat obscure (Goldin 2010) (see also Chap. 19). The occurrence of Parkinson’s disease in some type 1 (non-neuronopathic) Gaucher disease individuals and their first degree relatives suggested GBA1 mutations might be a genetic risk factor for idiopathic Parkinson’s (Bultron et al. 2010). It has recently been shown that compared to the general population, there is an approximate 20-fold increase in lifetime risk of developing Parkinson’s disease in patients with type 1 Gaucher disease (Bultron et al. 2010). Gaucher disease is caused by mutations in the GBA1 gene that encodes the enzyme glucocerebrosidase which degrades glycosphingolipids to ceramide and glucose (Beutler and Grabowski 2001). GBA1 mutations result in lysosomal accumulation of glucocerebroside (glucosylceramide). In type II Gaucher disease, increased levels of ganglioside GD3 have been reported in brain and in cerebrospinal fluid (Gornati et al. 2002); some studies have reported increases in expression of gangliosides GM2, GM3, GM1, and GD3 in the CNS in Gaucher disease while others have indicated either no change or decreases in gangliosides (Gonzalez-Sastre et al. 1974; Gornati et al. 2002; Conradi et al. 1984; Kaye et al. 1986). However, most of the reports of altered ganglioside expression were in association with type II or infantile forms of Gaucher disease. The extent to which CNS ganglioside expression is altered in type I Gaucher is unclear. However, ganglioside GM3 is reported to be strikingly elevated in plasma of type 1 Gaucher disease patients (Ghauharali-van der Vlugt et al. 2008).
A further link between Gaucher disease and Parkinson’s disease is the presence of α-synuclein inclusions in brains of patients with type I Gaucher disease and Parkinsonism. Such patients also have Lewy body pathology and loss of substantia nigra dopaminergic neurons (Wong et al. 2004). Brain samples from patients with Gaucher disease or from Gaucher disease carriers with Parkinsonism all showed GBA1 mutations and Lewy body pathology, with α-synuclein and glucocerebrosidase detected in Lewy body inclusions (Shachar et al. 2011; Goker-Alpan et al. 2010). It has also recently been shown that increased intracellular glucosylceramide (GlcCer) levels (GlcCer accumulates in affected tissues in Gaucher disease due to glucocerebrosidase deficiency) enhance the formation of toxic α-synuclein assemblies which may lead to neurodegeneration (Mazzulli et al. 2011).
20.5 Concluding Remarks
Although there have been tremendous advances in the understanding of the pathophysiology of numerous neurodegenerative disorders, there is still much that is not known about the mechanisms that initiate and drive neurodegeneration. This is particularly true in Parkinson’s disease and Alzheimer’s disease. Recent data though suggest that alterations in ganglioside biosynthesis and/or metabolism may be involved in numerous neurodegenerative disorders. Further research is now needed in order to better understand the nature of the changes in brain gangliosides in these disorders and to understand the extent to which these changes are either the cause or effect of neurodegenerative processes.
Abbreviations
- AD:
-
Alzheimer’s disease
- CNS:
-
Central nervous system
- Ca:
-
Calcium
- mg/kg:
-
Milligram per kilogram
- TH:
-
Tyrosine hydroxylase
- HVA:
-
Homovanillic acid
- MPTP:
-
1-Methyl-4-phenyl 1,2,3,6-tetrahydropyridine
- UPDRS:
-
Unified Parkinson’s Disease Rating Scale
- APP:
-
Amyloid precursor protein
- Aβ:
-
Amyloid-beta
- BACE1:
-
Beta-secretase 1
- DARP-32:
-
Dopamine- and cAMP-regulated neuronal phosphoprotein
- GBA1:
-
Beta-glucosidase 1
References
Agnati LF, Fuxe K, Calza L, Benfenati F, Cavicchioli L, Toffano G, Goldstein M. Gangliosides increase the survival of lesioned nigral dopamine neurons and favour the recovery of dopaminergic synaptic function in striatum of rats by collateral sprouting. Acta Physiol Scand. 1983;119:347–63.
Allende ML, Proia RL. Lubricating cell signaling pathways with gangliosides. Curr Opin Struct Biol. 2002;12:587–92.
Aydin M, Cengiz S, Agachan B, Yilmaz H, Isbir T. Age-related changes in GM1, GD1a, GT1b components of gangliosides in Wistar albino rats. Cell Biochem Funct. 2000;18:41–5.
Beutler E, Grabowski G. Gaucher disease. In Scriver CR, Beaudet AL, Sly WS, Valle D (eds). The Metabolic and Molecular Bases of Inherited Disease. New York: McGraw-Hill. 2001; pp. 3635–3668.
Blennow K, Davidsson P, Wallin A, Fredman P, Gottfries CG, Karlsson I, Mansson JE, Svennerholm L. Gangliosides in cerebrospinal fluid in ‘probable Alzheimer’s disease’. Arch Neurol. 1991;48:1032–5.
Bultron G, Kacena K, Pearson D, Boxer M, Yang R, Sathe S, Pastores G, Mistry PK. The risk of Parkinson’s disease in type 1 Gaucher disease. J Inherit Metab Dis. 2010;33:167–73.
Chan RB, Oliveira TG, Cortes EP, Honig LS, Duff KE, Small SA, Wenk MR, Shui G, Di Paolo G. Comparative lipidomic analysis of mouse and human brain with Alzheimer disease. J Biol Chem. 2012;287:2678–88.
Conradi NG, Sourander P, Nilsson O, Svennerholm L, Erikson A. Neuropathology of the Norrbottnian type of Gaucher disease. Morphological and biochemical studies. Acta Neuropathol. 1984;65:99–109.
D’Agostino Sr RB. The delayed-start study design. N Engl J Med. 2009;361:1304–6.
Desplats PA, Denny CA, Kass KE, Gilmartin T, Head SR, Sutcliffe JG, Seyfried TN, Thomas EA. Glycolipid and ganglioside metabolism imbalances in Huntington’s disease. Neurobiol Dis. 2007;27:265–77.
Di Pardo A, Maglione V, Alpaugh M, Horkey M, Atwal RS, Sassone J, Ciammola A, Steffan JS, Fouad K, Truant R, Sipione S. Ganglioside GM1 induces phosphorylation of mutant huntingtin and restores normal motor behavior in Huntington disease mice. Proc Natl Acad Sci U S A. 2012;109:3528–33.
Fallon L, Moreau F, Croft BG, Labib N, Gu WJ, Fon EA. Parkin and CASK/LIN-2 associate via a PDZ-mediated interaction and are co-localized in lipid rafts and postsynaptic densities in brain. J Biol Chem. 2002;277:486–91.
Fong TG, Neff NH, Hadjiconstantinou M. GM1 ganglioside improves spatial learning and memory of aged rats. Behav Brain Res. 1997;85:203–11.
Ghauharali-van der Vlugt K, Langeveld M, Poppema A, Kuiper S, Hollak CE, Aerts JM, Groener JE. Prominent increase in plasma ganglioside GM3 is associated with clinical manifestations of type I Gaucher disease. Clin Chim Acta. 2008;389:109–13.
Goettl VM, Wemlinger TA, Duchemin AM, Neff NH, Hadjiconstantinou M. GM1 ganglioside restores dopaminergic neurochemical and morphological markers in aged rats. Neuroscience. 1999;92:991–1000.
Goettl VM, Wemlinger TA, Colvin AE, Neff NH, Hadjiconstantinou M. Motoric behavior in aged rats treated with GM1. Brain Res. 2001;906:92–100.
Goettl VM, Zhang H, Burrows AC, Wemlinger TA, Neff NH, Hadjiconstantinou M. GM1 enhances dopaminergic markers in the brain of aged rats. Exp Neurol. 2003;183:665–72.
Goker-Alpan O, Stubblefield BK, Giasson BI, Sidransky E. Glucocerebrosidase is present in alpha-synuclein inclusions in Lewy body disorders. Acta Neuropathol. 2010;120:641–9.
Goldin E. Gaucher disease and parkinsonism, a molecular link theory. Mol Genet Metab. 2010;101:307–10.
Gonzalez-Sastre F, Pampols T, Sabater J. Infantile Gaucher’s disease: a biochemical study. Neurology. 1974;24:162–7.
Gornati R, Berra B, Montorfano G, Martini C, Ciana G, Ferrari P, Romano M, Bembi B. Glycolipid analysis of different tissues and cerebrospinal fluid in type II Gaucher disease. J Inherit Metab Dis. 2002;25:47–55.
Gottfries CG, Adolfsson R, Aquilonius SM, Carlsson A, Eckernas SA, Nordberg A, Oreland L, Svennerholm L, Wiberg A, Winblad B. Biochemical changes in dementia disorders of Alzheimer type (AD/SDAT). Neurobiol Aging. 1983;4:261–71.
Hadjiconstantinou M, Neff NH. Treatment with GM1 ganglioside restores striatal dopamine in the 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine-treated mouse. J Neurochem. 1988;51:1190–6.
Hadjiconstantinou M, Rossetti ZL, Paxton RC, Neff NH. Administration of GM1 ganglioside restores the dopamine content in striatum after chronic treatment with MPTP. Neuropharmacology. 1986;25:1075–7.
Hakomori S, Igarashi Y. Gangliosides and glycosphingolipids as modulators of cell growth, adhesion, and transmembrane signaling. Adv Lipid Res. 1993;25:147–62.
Hatano T, Kubo S, Imai S, Maeda M, Ishikawa K, Mizuno Y, Hattori N. Leucine-rich repeat kinase 2 associates with lipid rafts. Hum Mol Genet. 2007;16:678–90.
Haughey NJ, Bandaru VV, Bae M, Mattson MP. Roles for dysfunctional sphingolipid metabolism in Alzheimer’s disease neuropathogenesis. Biochim Biophys Acta. 2010;1801:878–86.
Herrero MT, Perez-Otano I, Oset C, Kastner A, Hirsch EC, Agid Y, Luquin MR, Obeso JA, Del Rio J. GM-1 ganglioside promotes the recovery of surviving midbrain dopaminergic neurons in MPTP-treated monkeys. Neuroscience. 1993;56:965–72.
Hirabayashi Y. A world of sphingolipids and glycolipids in the brain—novel functions of simple lipids modified with glucose. Proc Jpn Acad Ser B Phys Biol Sci. 2012;88:129–43.
Kalanj S, Kracun I, Rosner H, Cosovic C. Regional distribution of brain gangliosides in Alzheimer’s disease. Neurol Croat. 1991;40:269–81.
Kaye EM, Ullman MD, Wilson ER, Barranger JA. Type 2 and type 3 Gaucher disease: a morphological and biochemical study. Ann Neurol. 1986;20:223–30.
Kidd SK, Mettil W, Anderson DW, Schneider JS. Ganglioside regulation in the human substantia nigra and its relation to Parkinson’s disease. Program No. 754.16. 2012 Neuroscience Meeting Planner. New Orleans, LA: Society for Neuroscience, Online; 2012.
Kracun I, Kalanj S, Talan-Hranilovic J, Cosovic C. Cortical distribution of gangliosides in Alzheimer’s disease. Neurochem Int. 1992a;20:433–8.
Kracun I, Rosner H, Drnovsek V, Vukelic Z, Cosovic C, Trbojevic-Cepe M, Kubat M. Gangliosides in the human brain development and aging. Neurochem Int. 1992b;20:421–31.
Kreutz F, Frozza RL, Breier AC, de Oliveira VA, Horn AP, Pettenuzzo LF, Netto CA, Salbego CG, Trindade VM. Amyloid-beta induced toxicity involves ganglioside expression and is sensitive to GM1 neuroprotective action. Neurochem Int. 2011;59:648–55.
Maglione V, Marchi P, Di Pardo A, Lingrell S, Horkey M, Tidmarsh E, Sipione S. Impaired ganglioside metabolism in Huntington’s disease and neuroprotective role of GM1. J Neurosci. 2010;30:4072–80.
Martinez Z, Zhu M, Han S, Fink AL. GM1 specifically interacts with alpha-synuclein and inhibits fibrillation. Biochemistry. 2007;46:1868–77.
Mazzulli JR, Xu YH, Sun Y, Knight AL, McLean PJ, Caldwell GA, Sidransky E, Grabowski GA, Krainc D. Gaucher disease glucocerebrosidase and alpha-synuclein form a bidirectional pathogenic loop in synucleinopathies. Cell. 2011;146:37–52.
Mettil W, Kidd SK, Anderson DW, Schneider JS. Decreased GM1 ganglioside expression and altered ganglioside biosynthetic pathways in the brain of Parkinson’s disease patients. Program No. 806.09. 2013 Neuroscience Meeting Planner. San Diego, CA: Society for Neuroscience, Online; 2013.
Olanow CW, Hauser RA, Jankovic J, Langston W, Lang A, Poewe W, Tolosa E, Stocchi F, Melamed E, Eyal E, Rascol O. A randomized, double-blind, placebo-controlled, delayed start study to assess rasagiline as a disease modifying therapy in Parkinson’s disease (the ADAGIO study): rationale, design, and baseline characteristics. Mov Disord. 2008;23:2194–201.
Olanow CW, Rascol O, Hauser R, Feigin PD, Jankovic J, Lang A, Langston W, Melamed E, Poewe W, Stocchi F, Tolosa E. A double-blind, delayed-start trial of rasagiline in Parkinson’s disease. N Engl J Med. 2009;361:1268–78.
Schneider JS, Yuwiler A. GM1 ganglioside treatment promotes recovery of striatal dopamine concentrations in the mouse model of MPTP-induced parkinsonism. Exp Neurol. 1989;105:177–83.
Schneider JS, Pope A, Simpson K, Taggart J, Smith MG, DiStefano L. Recovery from experimental parkinsonism in primates with GM1 ganglioside treatment. Science. 1992;256:843–6.
Schneider JS, Kean A, DiStefano L. GM1 ganglioside rescues substantia nigra pars compacta neurons and increases dopamine synthesis in residual nigrostriatal dopaminergic neurons in MPTP-treated mice. J Neurosci Res. 1995a;42:117–23.
Schneider JS, Roeltgen DP, Rothblat DS, Chapas-Crilly J, Seraydarian L, Rao J. GM1 ganglioside treatment of Parkinson’s disease: an open pilot study of safety and efficacy. Neurology. 1995b;45:1149–54.
Schneider JS, Roeltgen DP, Mancall EL, Chapas-Crilly J, Rothblat DS, Tatarian GT. Parkinson’s disease: improved function with GM1 ganglioside treatment in a randomized placebo-controlled study. Neurology. 1998;50:1630–6.
Schneider JS, Sendek S, Daskalakis C, Cambi F. GM1 ganglioside in Parkinson’s disease: results of a five year open study. J Neurol Sci. 2010;292:45–51.
Schneider JS, Gollomp SM, Sendek S, Colcher A, Cambi F, Du W. A randomized, controlled, delayed start trial of GM1 ganglioside in treated Parkinson’s disease patients. J Neurol Sci. 2013;324:140–8.
Scorrano L, Petronilli V, Di Lisa F, Bernardi P. Commitment to apoptosis by GD3 ganglioside depends on opening of the mitochondrial permeability transition pore. J Biol Chem. 1999;274:22581–5.
Shachar T, Lo Bianco C, Recchia A, Wiessner C, Raas-Rothschild A, Futerman AH. Lysosomal storage disorders and Parkinson’s disease: Gaucher disease and beyond. Mov Disord. 2011;26:1593–604.
Shield AJ, Murray TP, Board PG. Functional characterisation of ganglioside-induced differentiation-associated protein 1 as a glutathione transferase. Biochem Biophys Res Commun. 2006;347:859–66.
Svennerholm L, Gottfries CG. Membrane lipids, selectively diminished in Alzheimer brains, suggest synapse loss as a primary event in early-onset form (type I) and demyelination in late-onset form (type II). J Neurochem. 1994;62:1039–47.
Svennerholm L, Brane G, Karlsson I, Lekman A, Ramstrom I, Wikkelso C. Alzheimer disease—effect of continuous intracerebroventricular treatment with GM1 ganglioside and a systematic activation programme. Dement Geriatr Cogn Disord. 2002;14:128–36.
Tilson HA, Harry GJ, Nanry K, Hudson PM, Hong JS. Ganglioside interactions with the dopaminergic system of rats. J Neurosci Res. 1988;19:88–93.
Toffano G, Savoini G, Moroni F, Lombardi G, Calza L, Agnati LF. GM1 ganglioside stimulates the regeneration of dopaminergic neurons in the central nervous system. Brain Res. 1983;261:163–6.
Toffano G, Savoini G, Aporti F, Calzolari S, Consolazione A, Maura G, Marchi M, Raiteri M, Agnati LF. The functional recovery of damaged brain: the effect of GM1 monosialoganglioside. J Neurosci Res. 1984;12:397–408.
Wei J, Fujita M, Nakai M, Waragai M, Sekigawa A, Sugama S, Takenouchi T, Masliah E, Hashimoto M. Protective role of endogenous gangliosides for lysosomal pathology in a cellular model of synucleinopathies. Am J Pathol. 2009;174:1891–909.
Wong K, Sidransky E, Verma A, Mixon T, Sandberg GD, Wakefield LK, Morrison A, Lwin A, Colegial C, Allman JM, Schiffmann R. Neuropathology provides clues to the pathophysiology of Gaucher disease. Mol Genet Metab. 2004;82:192–207.
Wu G, Lu ZH, Kulkarni N, Ledeen RW. Deficiency of ganglioside GM1 correlates with Parkinson’s disease in mice and humans. J Neurosci Res. 2012;90:1997–2008.
Yanagisawa K. Role of gangliosides in Alzheimer’s disease. Biochim Biophys Acta. 2007;1768:1943–51.
Ethics Statement
Some of the research reported in this chapter was supported by NIH grant NS038681. The author declares that he has no conflict of interest.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
Schneider, J.S. (2014). Gangliosides and Glycolipids in Neurodegenerative Disorders. In: Yu, R., Schengrund, CL. (eds) Glycobiology of the Nervous System. Advances in Neurobiology, vol 9. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-1154-7_20
Download citation
DOI: https://doi.org/10.1007/978-1-4939-1154-7_20
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-1153-0
Online ISBN: 978-1-4939-1154-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)