Abstract
The body is colonized by a vast population of genetically diverse microbes, the majority of which reside within the intestines to comprise the intestinal microbiota. During periods of homeostasis, these microbes reside within stable climax communities, but exposure to physical, physiological, as well as psychological stressors can significantly impact the structure of the intestinal microbiota. This has been demonstrated in humans and laboratory animals, with the most consistent finding being a reduction in the abundance of bacteria in the genus Lactobacillus. Whether stressor exposure also changes the function of the microbiota, has not been as highly studied. The studies presented in this review suggest that stressor-induced disruption of the intestinal microbiota leads to increased susceptibility to enteric infection and overproduction of inflammatory mediators that can induce behavioral abnormalities, such as anxiety-like behavior. Studies involving germfree mice also demonstrate that the microbiota are necessary for stressor-induced increases in innate immunity to occur. Exposing mice to a social stressor enhances splenic macrophage microbicidal activity, but this effect fails to occur in germfree mice. These studies suggest a paradigm in which stressor exposure alters homeostatic interactions between the intestinal microbiota and mucosal immune system and leads to the translocation of pathogenic, and/or commensal, microbes from the lumen of the intestines to the interior of the body where they trigger systemic inflammatory responses and anxiety-like behavior. Restoring homeostasis in the intestines, either by removing the microbiota or by administering probiotic microorganisms, can ameliorate the stressor effects.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
The body is heavily colonized by microorganisms collectively referred to as the microbiota, and it is now realized that all surfaces of the body naturally harbor unique microbial communities. While archea, protists, and viruses are known to reside within these communities, the majority of the microbiota are bacteria that reside within the gastrointestinal tract. Proximal sections of the gastrointestinal (GI) tract, including the stomach and the duodenum, harbor low levels of microorganisms (typically between 100 and 1,000 colony forming units (CFU) per ml of contents), whereas distal sections of the GI tract, including the ileum and the colon, harbor high levels of microorganisms (typically between 106 and 1012 CFU/ml of contents). In the colon, the microbiota reside as a stable climax community due to the selection of microbes that are best adapted for their given niche [1]. Although this climax community is relatively resistant to change [2], it is well known that factors such as diet and antibiotics can cause transient alterations in microbial community structure [3–5]. This review will discuss the evidence that exposure to different types of stressors can also cause transient alterations in microbial community structure, and will discuss the evidence that even transient alterations in the microbiota may be associated with variations in host immune and behavioral responses.
The Modern Stress Concept
Stress is an intrinsic part of life, and successfully coping with aversive stimuli is essential for organism survival in an ever changing environment. While the concept of stress is intuitive, there is not a single, widely accepted definition of stress. In its simplest form, stress can be broken down into the stimulus that threatens organism homeostasis (called the stressor) and the behavioral and physiological response to this challenge (called the stress response). Thus, a stressor is any stimulus that disrupts internal homeostasis, and can involve psychological, physical, or physiological stimuli. This disruption to homeostasis elicits physiological responses that are aimed at reducing the threat and re-establishing internal homeostasis. Initiation of the stress response to physical or physiological stressors is typically subconscious, but additional cognitive processing occurs in response to psychological stressors. Psychological stressors that are perceived as exceeding available coping strategies set into motion coordinated behavioral and physiological responses that ultimately serve to help the organism adapt to the stressor. Interestingly, the physiological stress responses to physical, physiological, and psychological stressors have many similarities that can be generalized across host species.
Physiological Stress Response
There are two neuroendocrine pathways that are major contributors to the stress response, namely the hypothalamic-pituitary-adrenal (HPA) axis and the sympathetic nervous system (SNS). Activation of the HPA axis occurs through the release of corticotrophin release hormone (CRH) from neurosecretory cells found in the paraventricular nucleus of the hypothalamus. CRH travels a short distance from the hypothalamus to the anterior pituitary gland where it stimulates the release of adrenocorticotrophic hormone (ACTH). The ACTH then travels through the blood and stimulates the release of glucorticoid hormones, namely corticosterone in rodents and cortisol in humans, from the cortex of the adrenal glands. As the name suggests, glucorticoids are important for increasing the bioavailability of glucose via gluconeogenesis in the liver. The glucose is then used by the body to cope with and adapt to the stressful stimulus.
In addition to the HPA axis, the sympathetic branch of the autonomic nervous system becomes activated during stressor exposure. The sympathetic nervous system (SNS) originates in the brain stem from different brain nuclei, such as the locus coeruleus, pons, and medulla, which send projections along the spinal column. After exiting the spinal column, preganglionic SNS neurons synapse in prevertebral ganglia using acetylcholine as the neurotransmitter. The acetylcholine excites postganglionic neurons that innervate virtually every organ in the body using norepinephrine (NE) as the terminal neurotransmitter.
Activation of the SNS occurs very rapidly and is largely responsible for the well-known “fight-or-flight” stress response, that is dependent upon the effects the SNS has on the heart and lungs (i.e., increased heart rate and respiration), blood vessels (i.e., increased vasodilation in skeletal muscle), and internal organs (e.g., increased glycogenolysis in the liver and reduced digestive functions in the gut). Upon stressor termination, the parasympathetic branch of the autonomic nervous system becomes activated and releases the neurotransmitter acetylcholine to restore homeostasis and induce the “rest-and-digest” response.
Stress Exposure and the Gut
Stressor-induced activation of the SNS and the HPA axis are well known to affect the functioning of the gastrointestinal tract. This was first recognized when it was observed that a patient with a gastric fistula produced significantly less gastric acid during fearful periods [6]. Other stressors, including a cold pressure task and mental arithmetic [7, 8] can also reduce gastric acid secretion. Studies in laboratory animals indicate that these stressor effects are due to activation of the autonomic nervous system. Activation of the SNS tends to suppress whereas the PNS enhances gastric acid secretion [9].
Other components of gastrointestinal physiology such as gastrointestinal motility and mucous production are also known to be significantly changed by stressor exposure. For example, GI motility, can be either slowed or enhanced during stressor exposure depending upon the type of stressor and the section of the intestine that is investigated [10, 11]. Stressor exposure has also been shown to affect mucous secretion, depending upon the strength and duration of the stressor. Early life or short-lasting stressors tend to increase mucous secretion throughout the length of the gastrointestinal tract, whereas long-lasting stressors tend to deplete mucous stores and thus decrease mucous levels in the gut [12, 13].
Gastric acid secretion, gastrointestinal motility, and mucous levels can influence the ability of microbes to colonize within the gastrointestinal tract. For example, it is well known that microbes must be able to survive the low acidity in the stomach in order to colonize lower sections of the gut. Reducing acid secretion can in turn alter gut microbiota populations [14]. Similarly, motility has long been recognized as a primary factor controlling microbe levels the length of the GI tract [15]. Pharmacological manipulation of gastrointestinal motility is associated with altered microbial populations [16]. The mucous layer in the gut is also an important factor for the development of microbial community structure, because the mucins that comprise the mucous layer are glycosylated with O-glycans that are an important food source for mucoadherent microbes [17]. Moreover, some microbes, such as members in the genus Lactobacillus, contain mucous binding proteins that help them to bind to the intestinal mucous layer [18]. Thus, changing mucous secretion has the potential to change microbial populations.
Impact of the Stress Response on Gut Microbiota and Colonic Inflammation
Studies in this laboratory have been influenced by the findings that gastrointestinal physiological functions that are affected by stressor exposure can also impact gut microbes, because they reflect a possible biological/mechanistic link between stressor-exposure and alterations in the microbiota. However, alteration of gut physiological functioning is not the only potential mechanism by which stress could impact the gastrointestinal microbiota. Direct neurotransmitter/hormone-bacterial interactions might also mediate stressor effects on the gut microbiota.
Neuroendocrine-Bacterial Interactions
The growth of many types of bacteria, including both infectious and commensal organisms, have been shown to be significantly enhanced upon culture with catecholamines, such a norepinephrine (NE), as shown in multiple chapters in this book.
While the effects of neuroendocrine hormones on microbial growth have been amply demonstrated in both in vitro and ex vivo model systems (reviewed in [19]), demonstrating these interactions occur in vivo has been challenging. However, studies involving the use of a neurotoxin to lyse peripheral sympathetic neurons, and thus causing an increase in norepinephrine levels in vivo, indicate that elevated norepinephrine levels leads to bacterial overgrowth in the intestines [20]. The growth of commensal Gram-negative microbes, primarily Escherichia coli, was increased by nearly 10,000-fold after elevating NE levels through the use of the neurotoxin [20]. The effects of norepinephrine on bacterial growth was also evident in an ileal loop model, where growth of Salmonella enterica in the presence of NE prior to inoculation into an ileal loop was associated with significantly elevated pathogen levels in the ileal loop, and a more severe pathogen-induced disease progression [21].
As these studies demonstrate, there are multiple mechanisms by which host physiology can impact microbial populations in the intestines. And, exposure to stressors that are physical, physiological, or psychological in nature has the capacity to significantly change all of these host physiological processes. These findings have led to testing the general hypothesis that stressor exposure can significantly change microbial populations naturally residing within the gastrointestinal tract.
Culture-Based Findings of Stressor Effects on the Structure of the Microbiota
It has been recognized for over 30 years that changing an animal’s environment can lead to gut microbial dysbiosis. In 1974, Tannock and Savage [22] demonstrated that moving mice into a cage lacking bedding, food, and water reduced the number of lactobacilli that could be cultured from the small and large intestines, with the greatest reduction being found in the stomach. Although it was not possible to determine whether the reduction was due to the change in environment, rather than the lack of food and water, this was one of the earliest studies to demonstrate that external factors could impact the microbiota. Subsequent studies confirmed and extended the observation that environmental stimuli can impact the microbiota. For example, chronic sleep deprivation was found to cause a significant overgrowth of microbiota in the distal ileum and cecum [23]. This microbial overgrowth was associated with a translocation of the microbes to the spleen, liver, and regional lymph nodes in sleep-deprived animals [23].
It is becoming increasingly evident that physical and physiological stressor can impact gut microbial populations, but only a few studies have focused on the impact that psychological stressors can have on the microbiota. Data from early studies on the composition of the microbiota in Russian cosmonauts were among the first to suggest that psychological stimuli could impact the composition of the microbiota. The data demonstrated that the intestinal microbiota were significantly different during space flight as compared to training periods on Earth [24]. There are many environmental changes associated with space flight, and it was not clear whether the differences in the microbiota could be due to the stress associated with space flight. However, other studies tracking microbial populations during space training found that periods of emotional stress, such as the stress of confinement, was associated with periods of altered microbial profiles [25], thus suggesting that emotional stress could impact the stability of the intestinal microbiota.
The strongest evidence that stressor exposure can impact microbial populations has come from studies involving laboratory animals. For example, studies demonstrate that separating rhesus monkeys (Macaca mulatta) from their mothers was sufficient to significantly change the number of bacteria that could be cultured from the stool. Levels of total cultured bacteria tended to be significantly decreased by 3 days after separation [26], but the most consistent findings occurred when a single type of microbe was cultured. Levels of bacteria in the genus Lactobacillus were significantly reduced 3 days after maternal separation [26]. Of importance, this reduction in lactobacilli was significantly correlated with the expression of stress indicative behaviors. Those animals that displayed a larger number of stress-indicative behaviors (such as repetitive lip smacking and cooing) tended to have lower levels of lactobacilli. This effect lasted through 3 days post-separation. Interestingly, as the infant monkeys formed stable social groups by 1 week post-separation, the levels of lactobacilli returned to pre-separation values [26].
Members of the genus Lactobacillus are known to have protective effects in the intestines, with one protective effect being the production of proteins and other compounds that have the capacity to kill enteric pathogens. Two enteric pathogens, namely Shigella flexneri and Campylobacter jejuni, are endemic in monkey colonies. Exposure to maternal separation increased opportunistic infection with S. flexneri and C. jejuni, and pathogen levels tended to correlate with lactobacilli levels. In general, maternally separated infant monkeys that had high pathogen loads also had low levels of lactobacilli [26]. This study demonstrated that a naturally occurring stressor changed the levels of bacteria that could be cultured from the stool and also reduced the ability of the microbiota to exclude pathogen colonization.
The effects of stressor exposure on the microbiota also extend into the prenatal period. Exposing monkeys to an acoustical startle stressor during gestation significantly changes the development of the intestinal microbiota in the offspring [27]. This was manifest as a reduction in the levels of bifidobacteria and lactobacilli that could be cultured from the stool for the first 6 weeks of life. As with previous studies, this stressor-associated reduction in lactobacilli was associated with an increased incidence of opportunistic infection [27].
Culture-based studies in rodents have also demonstrated that stressor exposure reduces the number of lactobacilli cultured from the stool. Mice that were housed in cages lacking bedding, as well as mice that were exposed to horizontal shaking, for 3 consecutive days were found to have lower lactobacilli levels shed in the feces than did control mice [28]. This reduction in lactobacilli was consistent between the different stressors, and led the authors to suggest that reduction in the lactobacilli could be used as a marker for environmental stressor exposure [28]. A note of caution is needed, however, because one study has found that inbred female mice have low levels of Enterococcus and Lactobacillus spp., as determined using fluorescent in situ hybridization (FISH), but exposure to water avoidance stress during antibiotic administration causes an increase in this bacterial group, rather than a decrease [29].
The effects of stressor exposure on lactobacilli have primarily been studied in laboratory animals, but one study found that stressor exposure reduced the levels of lactobacilli cultured from humans. Fecal lactobacilli levels were assessed in college students during a low stress period (i.e., the first week of the semester) and a high stress period (i.e., final exam week) to determine whether the stressful period was associated with lower levels of lactobacilli. The final exam period was associated with higher levels of perceived stress, and consistent with results from animal studies, higher perceived stress resulted in lower levels of lactobacilli shed in the stool [30]. It should be noted that the exam period was also associated with significant differences in diet. Because diet can significantly impact microbial populations [31], it is possible that the reductions in lactobacilli were dependent upon changes in diet. However, given results demonstrating stressor-induced reductions in fecal lactobacilli in laboratory animals consuming a standardized laboratory diet [26, 27], it is likely that alterations in the human microbiome during the stress of the exam week were due to combined effects of the stressor on host physiology and changes in dietary habits.
Culture-Independent Studies of Stressor Effects on Gut Microbial Community Structure and Function
Most studies assessing the effects of stressor exposure on the gut microbiota have relied on culture-based enumeration of only a few types of microbes within a given sample. However, the vast majority of microbes in the gut cannot be cultured due to undefined culture conditions [32]. As a result, there are an increasing number of studies that have utilized culture-independent methods to demonstrate that stressor exposure can affect more than just a few gut microbes; community-wide alterations of the gut microbiota have been demonstrated to occur in response to multiple types of stressors. This was first realized in rats that were separated from their mothers for 3 h per day early in life (i.e., postnatal days 3–12). This maternal separation stressor resulted in significant community-wide alterations in the gut microbiota as assessed using denaturing gradient gel electrophoresis (DGGE) to assess microbial populations in the stool when the rats were 7–8 weeks of age [33]. Studies in this laboratory have also used culture-independent methods to assess the effects of stressor exposure on the intestinal microbiota [34, 35]. Next generation, high throughput 454 FLX pyrosequencing was first used to characterize the microbiota in mice exposed to a prolonged restraint stressor.
Studies Involving Prolonged Restraint
Prolonged restraint is a widely used murine stressor that has been extensively characterized in the literature and is the most commonly used murine stressor in biomedical and biobehavioral research [36]. This stressor involves both a physical component (i.e., physical confinement) and a psychological component that is thought to reflect the animal’s perception of burrow collapse and inescapability [36]. Exposure to the prolonged restraint stressor induces a physiological stress response that results in the elevation of endogenous corticosterone, epinephrine, and norepinephrine [36–39]. Thus, mice were exposed to the prolonged restraint stressor to determine the effects of the stress response on the stability of the intestinal microbiota.
In this initial experiment, approximately 100,000 sequences from the cecal contents of 32 mice (approximately 3,000 sequences per mouse) were analyzed to characterize microbial diversity within the cecum. Microbial diversity encompasses both the richness (i.e., the number of different types of bacteria in a community) and the evenness (i.e., the distribution of the individual bacteria). In microbial ecology, there are two primary measures of diversity, with α-diversity assessing diversity of species within samples and β-diversity assessing diversity between samples. Prolonged restraint affected both α- and β-diversity. Hierarchical clustering analyses indicated that the profile of the top ten most abundant bacterial types was significantly different in the mice exposed to 3, 5, or 7 days of restraint compared to profiles found in control animals [34]. Mice will not eat or drink while in restraining tubes, even if food and water is provided. Because changes in diet can have a profound impact on the microbiota [5, 40], a food and water deprived control group was included in the study. Mice that were restrained for one night had microbial profiles that were similar to food and water deprived control mice. However, as mice were exposed to repeated cycles of the restraint stressor (i.e., 3, 5, or 7 repeated nights of prolonged restraint) microbial profiles were distinct from those found in food and water deprived mice [34]. This indicates that at least some of the effects of the stressor on the microbiota are due to food and water deprivation, but that repeated cycles of the stressor had additional effects on the microbiota that were not accounted for by food and water deprivation.
In addition to changes in microbial community β-diversity, exposure to prolonged restraint also results in changes to α-diversity. Rarefaction analysis indicated that species diversity decreased with repeated cycles of restraint. This is important, because it is generally believed that loss of α-diversity leads to increased susceptibility to enteric infection [41]. Thus, it was hypothesized that mice exposed to the prolonged restraint stressor would have an increased susceptibility to enteric infection [34]. To test this hypothesis, mice were orally challenged with Citrobacter rodentium, which is a natural murine colonic pathogen, with pathogenesis and resulting colonic pathology that are nearly indistinguishable from that produced in humans infected with enteropathogenic E. coli, and some components of enterohemorrhagic E. coli [42–44]. As the infection progresses, the colonic inflammatory response resembles many aspects of the colitis found in patients with inflammatory bowel disease [44, 45].
Challenging mice with C. rodentium prior to, or during, exposing to the prolonged restraint stressor significantly increased C. rodentium colonization in the colon and increased pathogen-induced colitis marked by increases in inflammatory cytokine (e.g., TNF-α) mRNA levels and increased colonic histopathology [34, 46]. Interestingly, exposing mice to six consecutive nights of prolonged restraint prior to oral challenge with C. rodentium increased colonic pathogen levels and mildly increased pathogen-induced colitis [34]. However, exposing mice to the prolonged restraint stressor for 1 night prior to oral challenge with C. rodentium and then exposing mice to 6 more nights of prolonged restraint (i.e., through day 5 post-C. rodentium challenge) resulted in significantly greater colonic pathology [46]. Simultaneously administering the prolonged restraint stressor and the C. rodentium challenge caused outbred CD-1 mice, which are generally considered resistant to C. rodentium infection, to develop severe colitis with lesions containing inflammation, epithelial defects, hyperplasia, and dysplasia. In some cases, neutrophilic inflammation extended from the mucosa to the submucosa and was frequently associated with epithelial erosion and ulceration [46].
C. rodentium lack pathogenic mechanisms to cross the intestinal epithelial barrier, and thus are not considered an invasive pathogen. However, simply exposing mice to the prolonged restraint stressor during oral challenge with C. rodentium was sufficient to significantly increase the occurrence of C. rodentium in the spleen, and also increased circulating levels of IL-6 and anxiety-like behavior. This suggests that stressor exposure during C. rodentium challenge disrupted the tight junctions between intestinal epithelial cells that in healthy tissue prevent the passive transfer of non-invasive microbes, fluid, and nutrients form the lumen of the intestines to the interior of the body. Stressor exposure is well known to affect tight junctional protein expression and the permeability of intestinal tissue [47–49]. Our study involving a colonic pathogen suggests that pairing stressor exposure and colonic infection can further degrade colonic epithelial barrier integrity [46].
It is not yet known whether stressor-induced alterations in the intestinal microbiota contribute to the enhancive effects of stressor exposure on C. rodentium challenge. However, administering probiotic Lactobacillus reuteri (ATCC23272) has beneficial effects on stressor-exposed mice orally challenged with C. rodentium [46]. L. reuteri is widely recognized to limit inflammation, and in a study involving gnotobiotic mice orally challenged with enterohemorrhagic E. coli (which is closely related to C. rodentium), L. reuteri significantly reduced colonic inflammation [50]. In our studies, L. reuteri administration during prolonged restraint significantly enhanced gut barrier integrity. Providing L. reuteri to the stressor-exposed mice prevented the ability of C. rodentium to translocate from the lumen of the intestines to the spleen. Administering the L. reuteri also prevented the increase in circulating IL-6 and the development of anxiety-like behavior in mice exposed to the stressor during C. rodentium challenge [46].
Exposure to the prolonged restraint stressor reduces both relative and absolute levels of commensal L. reuteri that are associated with colonic tissue (Galley et al., under review). This was observed in a study involving 16s rRNA gene sequencing using the 454 FLX-Titanium pyrosequencing platform followed by real-time PCR to characterize colonic tissue-associated microbiota in mice exposed to the prolonged restraint stressor. Considering the finding that administering probiotic L. reuteri to stressor-exposed mice prevents some, but not all, effects of the stressor has led to the hypothesis that stressor-induced alterations in commensal tissue-associated microbiota result in an internal environment that is more conducive to pathogen-induced colonic inflammation. It is further hypothesized that this internal environment leads to increased epithelial permeability and the translocation of pathogenic (as well as commensal) microbes from the lumen of the intestines to the interior of the body where they stimulate increases in inflammatory cytokines that alter the behavior of the host (Fig. 12.1). Further studies are needed to confirm this hypothesis, and to determine whether commensal and probiotic microbes in addition to L. reuteri are involved with, or can prevent, stressor-induced increases in colonic inflammation.
Exposure to physical, physiological, or psychological stressors sets into motion a series of physiological responses that have the capacity to disrupt homeostatic interactions between the host and the gut microbiota. These disrupted homeostatic interactions lead to increases in susceptibility to intestinal infection and inflammation, and enhances epithelial barrier permeability and subsequent translocation from the lumen of the intestines to the interior of the body. The disruptions in epithelial barrier integrity lead to increases in circulating cytokines that have the capacity to change animal behavior and further stimulate the endocrine response. The hypothesis that alterations in the intestinal microbiota are responsible for these disrupted homeostatic interactions comes from data indicating that stressor exposure reduces beneficial microbes, such as bacteria in the genus Lactobacillus. Feeding mice lactobacilli to prevent the stressor-induced reduction in Lactobacillus spp. prevents the stressor-induced increase in susceptibility to colonic infection and inflammation and prevents disruptions to epithelial barrier integrity
Studies Involving Repeated Social Defeat
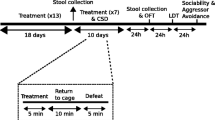
The effects of stress on colonic microbiota and inflammatory responses are also evident using a social stressor called social disruption (SDR). Social stressors often involve aggressive interactions between dominant and subordinate animals and are widely used to study the effects of stress on animal behavior and physiological functioning [51–54]. Social disruption involves aggressive interactions between a dominant intruder mouse (i.e., the aggressor) and resident subordinate mice (i.e., the experimental subjects). The aggressive interactions occur over a 2 h period at the beginning of the active cycle, when the aggressor is placed into the cage of the resident subordinate mice. The aggressor physically interacts with the residents for short periods of time until the residents display an upright defeat posture. Because the mice are housed together, the subordinate mice cannot escape and the aggressive intruder mouse will repeatedly attack and defeat the residents. Thus, the residents are exposed to repeated social defeat during the 2 h period.
The SDR stressor involves both physical and psychological components, and the defeated mice develop anxiety-like behaviors [55, 56] and a physiological stress response marked by elevated corticosterone [57, 58], epinephrine, and norepinephrine [59]. Importantly, exposure to the SDR stressor has well defined effects on systemic immune responses. For example, exposure to the SDR stressor is known to increase circulating levels of cytokines, such as IL-1 and IL-6, even in the absence of infectious challenge [60–62], which is also commonly evident in humans exposed to different types of stressors [63–65]. In addition, exposure to the SDR stressor reduces the sensitivity of splenic monocytes/macrophages to the suppressive effects of glucocorticoid hormones and increases the ability of these splenic monocytes/macrophages to kill target microbes [57, 58, 66–69].
Microbial populations in the cecums of mice exposed to the well-defined SDR stressor were assessed using 454 FLX pyrosequencing. Consistent with results obtained with prolonged restraint, exposure to the SDR stressor resulted in significant changes in both the α and β diversity of the cecal microbiota [35]. Alpha diversity indices, including OTU, ACE, and Chao all demonstrated statistically significant reductions in microbial diversity by 15 h after the last cycle of the SDR stressor. In addition, the relative abundance of 8 out of the top 25 most abundant microbes was significantly affected by exposure to the SDR stressor. These differences were evident immediately after the last cycle of stressor exposure, as well as the morning following the last cycle of the stressor [35] indicating that the effects of the stressor occur rapidly in response to stressor exposure and can persist for at least 15 h after termination of stressor exposure.
The conclusion that stressor exposure can enhance infectious colitis based on studies involving outbred CD-1 mice exposed to prolonged restraint during oral challenge with C. rodentium has been confirmed and extended in inbred mice exposed to a social stressor during oral challenge with C. rodentium. Inbred C57BL/6 mice were orally challenged with a low dose of C. rodentium, and in non-stressed control mice, little pathogen colonization and pathogen-induced colitis occurred with this low infectious dose. However, simply exposing the mice to the SDR stressor again increased both pathogen colonization and associated pathology (Galley et al., under review). Mice exposed to the social stressor during C. rodentium challenge had higher levels of mRNA for colonic inflammatory cytokines (e.g., TNF-α), chemokines (e.g., CCL2), and inflammatory mediators (e.g., inducible nitric oxide synthase (iNOS)). In addition, pathogen-induced colonic histopathology, which was mild in mice left undisturbed during oral challenge with C. rodentium, was significantly increased in mice exposed to the SDR stressor during challenge with the pathogen. Stressor exposed mice had increases in colonic epithelial cell hyperplasia and dysplasia, as well as epithelial defects, generalized edema and leukocyte infiltration. These effects were not evident in the mice that were not exposed to the stressor during pathogen challenge (Galley et al., under review).
Inflammatory monocytes are recruited to sites of inflammation in response to the chemokine CCL2 and are prolific producers of tissue-damaging TNF-α and iNOS in the colon [70]. Unpublished observations from our laboratory indicate that L. reuteri ATCC23272 can inhibit the ability of murine colonic epithelial cells (i.e., CMT-93 cells) to produce CCL2 (Mackos et al., unpublished observations), while others demonstrate that L. reuteri (strain 6475) can inhibit the ability of monocytes to produce TNF-α [71–73]. Thus, mice were administered L. reuteri to determine whether the commensal probiotic would attenuate stressor-induced colitis. Daily administration with 1 × 108 CFU of L. reuteri after exposure to the SDR stressor significantly reduced the effects of the stressor on C. rodentium induced colitis (Galley et al., under review); stressor-induced increases in TNF-α, iNOS, or CCL2 through the peak of C. rodentium infection, which occurs on day 12 post-challenge did not occur in probiotic-treated mice. In addition, colonic histopathology was not evident in any of the mice fed the L. reuteri, regardless of whether they were exposed to the stressor or not.
Much has been learned about the effects of probiotic microbes on host immune responses over the past 10 years, and it is tempting to speculate on the mechanisms by which L. reuteri attenuates stressor-induced colitis. L. reuteri has the capacity to limit pathogen growth and replication, particularly in vitro [74]. However, in all of the studies conducted in our laboratory utilizing C. rodentium [46], as well as other laboratories using a closely related pathogen (EHEC) [50], L. reuteri did not affect pathogen levels in vivo. Mice exposed to either the prolonged restraint stressor or the social stressor during oral challenge with C. rodentium had similar pathogen levels with or without being fed L. reuteri. These data demonstrate that L. reuteri does not attenuate pathogen-induced colitis by reducing pathogen load, and suggests that L. reuteri directly suppresses host inflammatory responses.
There are now multiple studies demonstrating that L. reuteri produces an immunomodulatory factor(s) when grown to stationary phase in vitro that reduces monocyte inflammatory cytokine production upon stimulation. Some of the effects of L. reuteri on stimulated monocytes are thought to be dependent upon bacterial production of histamine that when bound to H2 receptors reduces monocyte activity [73]. However, some strains of L. reuteri, such strain as ATCC23272 used in our studies, do not strongly reduce monocyte/macrophage activity, but rather have strong effects on colonic epithelial cells. Administering supernatants from overnight cultures of strain ATCC23272 reduced CCL2, TNF-α, and iNOS production by CMT-93 colonic epithelial cells, but not RAW264.7 macrophages or CD11b + splenic monocytes/macrophages stimulated with C. rodentium (Mackos and Bailey, Unpublished Observations). Thus, it is possible that some strains of L. reuteri reduce colonic inflammation through effects directly on inflammatory monocytes, whereas other strains might reduce colonic inflammation by reducing the ability of colonic epithelial cells to recruit and activate inflammatory cells, such as inflammatory monocytes and neutrophils.
It is also possible that L. reuteri has a more indirect effect on colonic inflammation in stressor-exposed mice. Studies demonstrate that intestinal microbes can impact the activation of the HPA axis and increase glucorticoid levels [75]. This could be of particular importance, because glucocorticoids produced by activation of the HPA axis potently suppress inflammatory responses [76], and reduced glucocorticoid production during stressor exposure as a result of adrenal insufficiency leads to intestinal inflammation during stressor exposure [77]. It is also possible that the production of immunomodulatory neuroendocrine mediators by L. reuteri, or by commensal microbes affected by L. reuteri, are responsible for effects on colonic inflammation in stressor-exposed mice. It has been shown that probiotic microbes can produce immunomodulatory neuroendocrine hormones, such as γ-amino butyric acid (GABA), norepinephrine, dopamine, and serotonin (reviewed in [78]), and it has been hypothesized that this hormone production can be responsible for influencing mucosal immune responses [78]. Thus, it is conceivable that L. reuteri does not directly impact host colonic inflammation, but rather stimulates host physiological responses that are known to have suppressive effects on the inflammatory response. Potential pathways by which stress, the microbiota, and probiotics impact colonic inflammation are illustrated in Fig. 12.1.
Microbiota and Stressor-Induced Immunomodulation in Systemic Compartments
Stressor exposure often results in increases in nonspecific inflammatory responses. For example, humans under the chronic stress of caring for a spouse with Alzheimer’s disease were found to have increases in circulating IL-6 [79], whereas exposure to acute laboratory stressors, such as different mental tasks, causes increases in IL-1 [80]. The mechanisms by which these stressor-induced increases in inflammatory cytokines occur in otherwise healthy individuals are not completely understood. But data from our laboratory, as well as others, suggest that the intestinal microbiota are involved [35, 81–83]. Mice exposed to the SDR stressor also show evidence of circulating cytokines, and cytokine levels directly correlate with microbiota levels [35]. For example, the relative abundance of three members of the microbiota (i.e., Coprococcus spp., Pseudobutyrivibrio spp., and Dorea spp.) were inversely correlated with the stressor-induced increases in circulating IL-6 [35]. This suggested that the microbiota were somehow involved in stressor-induced increases in circulating cytokines, but it was not until mice were given an oral cocktail of nonabsorbable antibiotics to reduce the microbiota that the link between the microbiota and circulating cytokines began to be clarified. Exposing antibiotic-treated mice to the stressor failed to increase circulating cytokines demonstrating a direct link between the microbiota and circulating cytokines [35]. This initial discovery led to additional studies to determine whether the microbiota are involved in stressor-induced modulation of macrophage microbicidal activity.
Phagocytes from mice lacking microbiota are deficient in their ability to kill target pathogens, including Streptococcus pneumoniae and Staphylococcus aureus [84]. Colonizing germ free mice by transplanting fecal bacteria from conventional mice in to the germ free mice led to effective bacterial killing by the phagocytes. Because reconstituted germfree mice had detectable levels of bacterial peptidoglycan in circulation, and because mice lacking the peptidoglycan receptor Nod1 were deficient in killing target microbes [84], it is likely that peptidoglycan from the microbiota is necessary to prime phagocytes for efficient microbicidal activity. This led us to question whether the microbiota are also necessary for the ability of the stress response to prime splenic macrophages for enhanced microbicidal activity.
Exposing conventional mice to the SDR stressor increases the ability of splenic macrophages to kill target microbes, such as E. coli, through an increased production of macrophage peroxynitrite [67, 85, 86]. This effect is dependent upon signaling through TLR4 [67] and the IL-1 receptor type 1 [86], and fails to occur in germfree mice that lack any microbiota [85]. Exposing germfree mice to the SDR stressor did not increase macrophage microbicidal activity or peroxynitrite production. However, reconstituting the germfree mice with microbiota allowed the effects of the stressor on splenic macrophage activity to again be manifest [85]. This demonstrates that the microbiota are necessary for stressor-induced increases in microbicidal activity to occur. Ongoing studies are determining the mechanisms by which the microbiota can impact splenic macrophage activity, but as shown in Fig. 12.2, data suggests that the microbiota exert their effects through IL-1R1 and TLR4 signaling.
Exposing conventional mice to a social stressor leads to the translocation of gut microbes and their products from the lumen of the intestines to the interior of the body, through a mast cell-dependent mechanism. It is hypothesized that this translocation is responsible for the stressor-induced increase in circulating cytokines, and subsequent enhancement of splenic macrophage microbicidal activity. The gut microbiota are hypothesized to be involved, because germfree mice exposed to the stressor have lower levels of circulating cytokines and macrophage microbicidal activity is not enhanced by stressor exposure
Conclusions
The dense populations of microbes that naturally colonize the body are well recognized to have beneficial effects on the host, and as microbiota research flourishes, we are becoming increasingly aware of the function of the microbiota in maintaining the health of the host. These functions are in part dependent upon the structure of the microbial communities, and it is thought that structure-function relationships have developed through the co-evolution of the host and its microbiota, such that alterations in one are associated with alterations in the other. This is well-illustrated in animals exposed to different types of stressors. During periods of quiescence, homeostatic interactions occur between the host and its microbiota to maintain beneficial microbial populations in the intestines and limit the induction of host inflammatory responses. As outlined in this chapter, exposing animals to experimental stressors significantly disrupts these homeostatic interactions; stressor-induced alterations in microbiota community structure are associated with increased host inflammatory responses.
There is now accumulating evidence that stressor-induced alterations in microbiota community structure are not just correlated with alterations in host inflammatory responses, but might actually be causally involved in stressor-induced immunomodulation. Exposure to psychological and physical stressors results in the reduction in commensal lactobacilli, with data in mice suggesting that the abundance of colonic tissue-associated Lactobacillus spp. are strongly reduced upon stressor exposure. The lactobacilli are known to have several beneficial effects on the health of the host, thus it is somewhat counterintuitive that the stress response, which has evolved to benefit the host in the face of environmental demands, would negatively impact commensal microbes. However, stressor-induced reductions in the lactobacilli might actually be reflective of gastrointestinal physiological responses that are meant to be protective against enteric pathogens. Stressor exposure increases colonic secretions, including the secretion of mucous, and colonic motility. Colonic mucous is a protective buffer that separates potential pathogens from adhering to colonic tissue. Thus, increased colonic mucous secretion, coupled with enhanced colonic motility, would help to flush potential pathogens from the colon. If, however, mucoadherent commensal microbes, such as members of the genus Lactobacillus, that naturally suppress colonic inflammation are also flushed from the intestines, it would result in a colonic environment that is conducive to overproduction of inflammatory mediators (Fig. 12.1).
Support for this notion comes from studies demonstrating that exposure to either prolonged restraint or the SDR stressor reduces the abundance of Lactobacillus spp., particularly of L. reuteri, and leads to increased colonic cytokine and chemokine production upon pathogen challenge. L. reuteri reduces colonic cytokine and chemokine production, and feeding stressor exposed mice L. reuteri to prevent stressor-induced reductions in L. reuteri prevents the exacerbating effects of the stressor on colonic cytokine and chemokine production. These findings support a causal role for stressor-induced alterations in lactobacilli in the stressor-induced exacerbation of infectious colitis (Fig. 12.1).
In addition to attenuating colonic inflammation, L. reuteri helped to reinforce the epithelial barrier. Mice exposed to either prolonged restraint or the SDR stressor during oral challenge with C. rodentium are more likely to have C. rodentium in the spleen than non-stressed control mice challenged with C. rodentium. This is important, because unlike invasive enteric pathogens, such as Salmonella spp., C. rodentium does not have mechanisms to invade its host [44]. C. rodentium and closely related EPEC stay within the digestive tract, attached to the apical surface of the colonic epithelium during infection of immunocompetent hosts [44]. However, C. rodentium can disrupt tight junctions found between colonic epithelial cells via the injection of effector proteins through a type III secretion system. L. reuteri are known to prevent inflammation-induced increases in colonic epithelial permeability [87], and can prevent the translocation of C. rodentium from the colon to the spleen in stressor-exposed mice, an effect that is associated with altered expression of genes encoding tight junction proteins [46]. These data indicate that an important function of the commensal microbiota is the regulation of tight junctional proteins, and stressor-induced alterations in the microbiota can allow for the loosening of tight junctions and the exacerbation of systemic manifestations of infectious colitis (Fig. 12.1).
Increased epithelial barrier permeability is also evident in uninfected stressor-exposed mice [48, 49, 85]. Several different types of stressors have been shown to increase the permeability of the intestinal barrier through mast cell-dependent mechanisms [47–49]. A defining characteristic of commensal microbes is their inability to invade through an epithelial barrier. Thus, commensal microbes can be maintained within their niche in the body by just a single layer of epithelial cells. However, it is known that stressor exposure can increase the ability of commensal microbes, and their products like lipopolysaccharide and peptidoglycan, to translocate from the lumen of the intestines to the interior of the body [85, 88, 89]. Because stressor-exposed germfree mice do not have increases in circulating cytokines, it is hypothesized that microbes that have translocated into circulation during stressor exposure cause an increase in circulating cytokines, such as IL-1. It is further hypothesized that this microbiota-dependent increase in IL-1 primes phagocytes for enhanced microbicidal activity through TLR4 signaling, because stressor-induced increases in microbicidal activity does not occur in TLR4-/- mice, IL-1R1-/- mice or in germfree mice (Fig. 12.2).
These studies demonstrate that the microbiota are interactively involved in stressor-induced immunomodulation at mucosal surfaces, as well as at systemic sites. Intestinal epithelial cells are important in mediating interactions between the microbiota and host immune responses. As interest in the microbiota continues to grow, it will be of importance to understand the molecular underpinnings through which microbiota, intestinal epithelial cells, and immune system activity are affected by stressor exposure.
Abbreviations
- ACTH:
-
Adrenocorticotrophic hormone
- CFU:
-
Colony forming units
- CRH:
-
Corticotrophin release hormone
- DGGE:
-
Denaturing gradient gel electrophoresis
- GABA:
-
γ-Amino butyric acid
- GI:
-
Gastrointestinal
- HPA:
-
Hypothalamic-pituitary-adrenal
- iNOS:
-
Inducible nitric oxide synthase
- mRNA:
-
Messenger ribonucleic acid
- NE:
-
Norepinephrine
- SDR:
-
Social disruption
- SNS:
-
Sympathetic nervous system
- TNF-α:
-
Tumor necrosis factor alpha
References
Huffnagle GB (2010) The microbiota and allergies/asthma. PLoS Pathog 6(5):e1000549
Allison SD, Martiny JB (2008) Colloquium paper: resistance, resilience, and redundancy in microbial communities. Proc Natl Acad Sci U S A 105(Suppl 1):11512–11519
Antonopoulos DA, Huse SM, Morrison HG, Schmidt TM, Sogin ML, Young VB (2009) Reproducible community dynamics of the gastrointestinal microbiota following antibiotic perturbation. Infect Immun 77(6):2367–2375
Dethlefsen L, Huse S, Sogin ML, Relman DA (2008) The pervasive effects of an antibiotic on the human gut microbiota, as revealed by deep 16S rRNA sequencing. PLoS Biol 6(11):e280
Turnbaugh PJ, Backhed F, Fulton L, Gordon JI (2008) Diet-induced obesity is linked to marked but reversible alterations in the mouse distal gut microbiome. Cell Host Microbe 3(4):213–223
Beaumont W (1838) Experiments and observations on the gastric juice and the physiology of digestion. Edinburgh, London
Badgley LE, Spiro HM, Senay EC (1969) Effect of mental arithmetic on gastric secretion. Psychophysiology 5(6):633–637
Holtmann G, Kriebel R, Singer MV (1990) Mental stress and gastric acid secretion. Do personality traits influence the response? Dig Dis Sci 35(8):998–1007
Yang H, Yuan PQ, Wang L, Tache Y (2000) Activation of the parapyramidal region in the ventral medulla stimulates gastric acid secretion through vagal pathways in rats. Neuroscience 95(3):773–779
Tache Y, Martinez V, Million M, Wang L (2001) Stress and the gastrointestinal tract III. Stress-related alterations of gut motor function: role of brain corticotropin-releasing factor receptors. Am J Physiol Gastrointest Liver Physiol 280(2):G173–G177
Tache Y, Perdue MH (2004) Role of peripheral CRF signalling pathways in stress-related alterations of gut motility and mucosal function. Neurogastroenterol Motil 16(Suppl 1):137–142
O’Malley D, Julio-Pieper M, Gibney SM, Dinan TG, Cryan JF (2010) Distinct alterations in colonic morphology and physiology in two rat models of enhanced stress-induced anxiety and depression-like behaviour. Stress 13(2):114–122
Shigeshiro M, Tanabe S, Suzuki T (2012) Repeated exposure to water immersion stress reduces the Muc2 gene level in the rat colon via two distinct mechanisms. Brain Behav Immun 26(7):1061–1065
Drasar BS, Shiner M, McLeod GM (1969) Studies on the intestinal flora. I. The bacterial flora of the gastrointestinal tract in healthy and achlorhydric persons. Gastroenterology 56(1):71–79
Berg RD (1996) The indigenous gastrointestinal microflora. Trends Microbiol 4(11):430–435
Stephen AM, Wiggins HS, Cummings JH (1987) Effect of changing transit time on colonic microbial metabolism in man. Gut 28(5):601–609
Sonnenburg JL, Xu J, Leip DD et al (2005) Glycan foraging in vivo by an intestine-adapted bacterial symbiont. Science 307(5717):1955–1959
Mackenzie DA, Jeffers F, Parker ML et al (2010) Strain-specific diversity of mucus-binding proteins in the adhesion and aggregation properties of Lactobacillus reuteri. Microbiology 156(Pt 11):3368–3378
Lyte M (2004) Microbial endocrinology and infectious disease in the 21st century. Trends Microbiol 12(1):14–20
Lyte M, Bailey MT (1997) Neuroendocrine-bacterial interactions in a neurotoxin-induced model of trauma. J Surg Res 70(2):195–201
Pullinger GD, Carnell SC, Sharaff FF et al (2010) Norepinephrine augments Salmonella enterica-induced enteritis in a manner associated with increased net replication but independent of the putative adrenergic sensor kinases QseC and QseE. Infect Immun 78(1):372–380
Tannock GW, Savage DC (1974) Influences of dietary and environmental stress on microbial populations in the murine gastrointestinal tract. Infect Immun 9(3):591–598
Everson CA, Toth LA (2000) Systemic bacterial invasion induced by sleep deprivation. Am J Physiol Regul Integr Comp Physiol 278(4):R905–R916
Lizko NN (1987) Stress and intestinal microflora. Nahrung 31(5–6):443–447
Holdeman LV, Good IJ, Moore WE (1976) Human fecal flora: variation in bacterial composition within individuals and a possible effect of emotional stress. Appl Environ Microbiol 31(3):359–375
Bailey MT, Coe CL (1999) Maternal separation disrupts the integrity of the intestinal microflora in infant rhesus monkeys. Dev Psychobiol 35(2):146–155
Bailey MT, Lubach GR, Coe CL (2004) Prenatal stress alters bacterial colonization of the gut in infant monkeys. J Pediatr Gastroenterol Nutr 38(4):414–421
Sakuma K, Funabashi H, Matsuoka H, Saito M (2013) Potential use of Lactobacillus cell density in feces as a non-invasive bio-indicator for evaluating environmental stress during mouse breeding. Biocontrol Sci 18(2):101–104
Aguilera M, Vergara P, Martinez V (2013) Environment-related adaptive changes of gut commensal microbiota do not alter colonic toll-like receptors but modulate the local expression of sensory-related systems in rats. Microb Ecol 66(1):232–243
Knowles SR, Nelson EA, Palombo EA (2008) Investigating the role of perceived stress on bacterial flora activity and salivary cortisol secretion: a possible mechanism underlying susceptibility to illness. Biol Psychol 77(2):132–137
Sartor RB (2006) Microbial and dietary factors in the pathogenesis of chronic, immune-mediated intestinal inflammation. Adv Exp Med Biol 579:35–54
Nocker A, Burr M, Camper AK (2007) Genotypic microbial community profiling: a critical technical review. Microb Ecol 54(2):276–289
O’Mahony SM, Marchesi JR, Scully P et al (2009) Early life stress alters behavior, immunity, and microbiota in rats: implications for irritable bowel syndrome and psychiatric illnesses. Biol Psychiatry 65(3):263–267
Bailey MT, Dowd SE, Parry NM, Galley JD, Schauer DB, Lyte M (2010) Stressor exposure disrupts commensal microbial populations in the intestines and leads to increased colonization by Citrobacter rodentium. Infect Immun 78(4):1509–1519
Bailey MT, Dowd SE, Galley JD, Hufnagle AR, Allen RG, Lyte M (2011) Exposure to a social stressor alters the structure of the intestinal microbiota: implications for stressor-induced immunomodulation. Brain Behav Immun 25(3):397–407
Buynitsky T, Mostofsky DI (2009) Restraint stress in biobehavioral research: recent developments. Neurosci Biobehav Rev 33(7):1089–1098
Dobbs CM, Vasquez M, Glaser R, Sheridan JF (1993) Mechanisms of stress-induced modulation of viral pathogenesis and immunity. J Neuroimmunol 48(2):151–160
Dobbs CM, Feng N, Beck FM, Sheridan JF (1996) Neuroendocrine regulation of cytokine production during experimental influenza viral infection: effects of restraint stress-induced elevation in endogenous corticosterone. J Immunol 157(5):1870–1877
Padgett DA, MacCallum RC, Sheridan JF (1998) Stress exacerbates age-related decrements in the immune response to an experimental influenza viral infection. J Gerontol A Biol Sci Med Sci 53(5):B347–B353
Sartor RB (2012) Gut microbiota: diet promotes dysbiosis and colitis in susceptible hosts. Nat Rev Gastroenterol Hepatol 9(10):561–562
Chang JY, Antonopoulos DA, Kalra A et al (2008) Decreased diversity of the fecal microbiome in recurrent Clostridium difficile-associated diarrhea. J Infect Dis 197(3):435–438
Borenshtein D, McBee ME, Schauer DB (2008) Utility of the Citrobacter rodentium infection model in laboratory mice. Curr Opin Gastroenterol 24(1):32–37
Luperchio SA, Schauer DB (2001) Molecular pathogenesis of Citrobacter rodentium and transmissible murine colonic hyperplasia. Microbes Infect 3(4):333–340
Mundy R, MacDonald TT, Dougan G, Frankel G, Wiles S (2005) Citrobacter rodentium of mice and man. Cell Microbiol 7(12):1697–1706
Eckmann L (2006) Animal models of inflammatory bowel disease: lessons from enteric infections. Ann N Y Acad Sci 1072:28–38
Mackos AR, Eubank TD, Parry NM, Bailey MT (2013) Probiotic Lactobacillus reuteri attenuates the stressor-enhanced severity of Citrobacter rodentium infection. Infect Immun 81:3253–3263
Cameron HL, Perdue MH (2005) Stress impairs murine intestinal barrier function: improvement by glucagon-like peptide-2. J Pharmacol Exp Ther 314(1):214–220
Santos J, Yang PC, Soderholm JD, Benjamin M, Perdue MH (2001) Role of mast cells in chronic stress induced colonic epithelial barrier dysfunction in the rat. Gut 48(5):630–636
Soderholm JD, Yates DA, Gareau MG, Yang PC, MacQueen G, Perdue MH (2002) Neonatal maternal separation predisposes adult rats to colonic barrier dysfunction in response to mild stress. Am J Physiol Gastrointest Liver Physiol 283(6):G1257–G1263
Eaton KA, Honkala A, Auchtung TA, Britton RA (2011) Probiotic Lactobacillus reuteri ameliorates disease due to enterohemorrhagic Escherichia coli in germfree mice. Infect Immun 79(1):185–191
Bohus B, Koolhaas JM, Heijnen CJ, de Boer O (1993) Immunological responses to social stress: dependence on social environment and coping abilities. Neuropsychobiology 28(1–2):95–99
de Groot J, van Milligen FJ, Moonen-Leusen BW, Thomas G, Koolhaas JM (1999) A single social defeat transiently suppresses the anti-viral immune response in mice. J Neuroimmunol 95(1–2):143–151
Korte SM, Smit J, Bouws GAH, Koolhaas JM, Bohus B (1990) Behavioral and neuroendocrine response to psychosocial stress in male rats: the effects of the 5-HT1A agonistic ipsapirone. Horm Behav 24:554–567
Sgoifo A, Stilli D, de Boer SF, Koolhaas JM, Musso E (1998) Acute social stress and cardiac electrical activity in rats. Aggress Behav 24:287–296
Kinsey SG, Bailey MT, Sheridan JF, Padgett DA, Avitsur R (2007) Repeated social defeat causes increased anxiety-like behavior and alters splenocyte function in C57BL/6 and CD-1 mice. Brain Behav Immun 21(4):458–466
Wohleb ES, Hanke ML, Corona AW et al (2011) beta-Adrenergic receptor antagonism prevents anxiety-like behavior and microglial reactivity induced by repeated social defeat. J Neurosci 31(17):6277–6288
Bailey MT, Avitsur R, Engler H, Padgett DA, Sheridan JF (2004) Physical defeat reduces the sensitivity of murine splenocytes to the suppressive effects of corticosterone. Brain Behav Immun 18(5):416–424
Engler H, Engler A, Bailey MT, Sheridan JF (2005) Tissue-specific alterations in the glucocorticoid sensitivity of immune cells following repeated social defeat in mice. J Neuroimmunol 163(1–2):110–119
Hanke ML, Powell ND, Stiner LM, Bailey MT, Sheridan JF (2012) Beta adrenergic blockade decreases the immunomodulatory effects of social disruption stress. Brain Behav Immun 26(7):1150–1159
Avitsur R, Kavelaars A, Heijnen C, Sheridan JF (2005) Social stress and the regulation of tumor necrosis factor-alpha secretion. Brain Behav Immun 19(4):311–317
Engler H, Bailey MT, Engler A, Stiner-Jones LM, Quan N, Sheridan JF (2008) Interleukin-1 receptor type 1-deficient mice fail to develop social stress-associated glucocorticoid resistance in the spleen. Psychoneuroendocrinology 33(1):108–117
Stark JL, Avitsur R, Hunzeker J, Padgett DA, Sheridan JF (2002) Interleukin-6 and the development of social disruption-induced glucocorticoid resistance. J Neuroimmunol 124(1–2):9–15
Brydon L, Edwards S, Mohamed-Ali V, Steptoe A (2004) Socioeconomic status and stress-induced increases in interleukin-6. Brain Behav Immun 18(3):281–290
Brydon L, Steptoe A (2005) Stress-induced increases in interleukin-6 and fibrinogen predict ambulatory blood pressure at 3-year follow-up. J Hypertens 23(5):1001–1007
Steptoe A, Hamer M, Chida Y (2007) The effects of acute psychological stress on circulating inflammatory factors in humans: a review and meta-analysis. Brain Behav Immun 21(7):901–912
Avitsur R, Stark JL, Dhabhar FS, Padgett DA, Sheridan JF (2002) Social disruption-induced glucocorticoid resistance: kinetics and site specificity. J Neuroimmunol 124(1–2):54–61
Bailey MT, Engler H, Powell ND, Padgett DA, Sheridan JF (2007) Repeated social defeat increases the bactericidal activity of splenic macrophages through a Toll-like receptor-dependent pathway. Am J Physiol Regul Integr Comp Physiol 293(3):R1180–R1190
Bailey MT, Kinsey SG, Padgett DA, Sheridan JF, Leblebicioglu B (2009) Social stress enhances IL-1beta and TNF-alpha production by Porphyromonas gingivalis lipopolysaccharide-stimulated CD11b + cells. Physiol Behav 98(3):351–358
Stark JL, Avitsur R, Padgett DA, Campbell KA, Beck FM, Sheridan JF (2001) Social stress induces glucocorticoid resistance in macrophages. Am J Physiol Regul Integr Comp Physiol 280(6):R1799–R1805
Platt AM, Bain CC, Bordon Y, Sester DP, Mowat AM (2010) An independent subset of TLR expressing CCR2-dependent macrophages promotes colonic inflammation. J Immunol 184(12):6843–6854
Jones SE, Versalovic J (2009) Probiotic Lactobacillus reuteri biofilms produce antimicrobial and anti-inflammatory factors. BMC Microbiol 9:35
Lin YP, Thibodeaux CH, Pena JA, Ferry GD, Versalovic J (2008) Probiotic Lactobacillus reuteri suppress proinflammatory cytokines via c-Jun. Inflamm Bowel Dis 14(8):1068–1083
Thomas CM, Hong T, van Pijkeren JP et al (2012) Histamine derived from probiotic Lactobacillus reuteri suppresses TNF via modulation of PKA and ERK signaling. PLoS One 7(2):e31951
Spinler JK, Taweechotipatr M, Rognerud CL, Ou CN, Tumwasorn S, Versalovic J (2008) Human-derived probiotic Lactobacillus reuteri demonstrate antimicrobial activities targeting diverse enteric bacterial pathogens. Anaerobe 14(3):166–171
Sudo N, Chida Y, Aiba Y et al (2004) Postnatal microbial colonization programs the hypothalamic-pituitary-adrenal system for stress response in mice. J Physiol 558(Pt 1):263–275
Padgett DA, Glaser R (2003) How stress influences the immune response. Trends Immunol 24(8):444–448
Reber SO, Peters S, Slattery DA et al (2011) Mucosal immunosuppression and epithelial barrier defects are key events in murine psychosocial stress-induced colitis. Brain Behav Immun 25(6):1153–1161
Lyte M (2011) Probiotics function mechanistically as delivery vehicles for neuroactive compounds: microbial endocrinology in the design and use of probiotics. Bioessays 33(8):574–581
Kiecolt-Glaser JK, Preacher KJ, MacCallum RC, Atkinson C, Malarkey WB, Glaser R (2003) Chronic stress and age-related increases in the proinflammatory cytokine IL-6. Proc Natl Acad Sci U S A 100(15):9090–9095
Brydon L, Edwards S, Jia H et al (2005) Psychological stress activates interleukin-1beta gene expression in human mononuclear cells. Brain Behav Immun 19(6):540–546
Maslanik T, Tannura K, Mahaffey L et al (2012) Commensal bacteria and MAMPs are necessary for stress-induced increases in IL-1beta and IL-18 but not IL-6, IL-10 or MCP-1. PLoS One 7(12):e50636
Maslanik T, Mahaffey L, Tannura K, Beninson L, Greenwood BN, Fleshner M (2013) The inflammasome and danger associated molecular patterns (DAMPs) are implicated in cytokine and chemokine responses following stressor exposure. Brain Behav Immun 28:54–62
Fleshner M (2013) Stress-evoked sterile inflammation, danger associated molecular patterns (DAMPs), microbial associated molecular patterns (MAMPs) and the inflammasome. Brain Behav Immun 27(1):1–7
Clarke TB, Davis KM, Lysenko ES, Zhou AY, Yu Y, Weiser JN (2010) Recognition of peptidoglycan from the microbiota by Nod1 enhances systemic innate immunity. Nat Med 16(2):228–231
Allen RG, Lafuse WP, Galley JD, Ali MM, Ahmer BM, Bailey MT (2012) The intestinal microbiota are necessary for stressor-induced enhancement of splenic macrophage microbicidal activity. Brain Behav Immun 26(3):371–382
Allen RG, Lafuse WP, Powell ND et al (2012) Stressor-induced increase in microbicidal activity of splenic macrophages is dependent upon peroxynitrite production. Infect Immun 80(10):3429–3437
Ahrne S, Hagslatt ML (2011) Effect of lactobacilli on paracellular permeability in the gut. Nutrients 3(1):104–117
Bailey MT, Engler H, Sheridan JF (2006) Stress induces the translocation of cutaneous and gastrointestinal microflora to secondary lymphoid organs of C57BL/6 mice. J Neuroimmunol 171(1–2):29–37
Ando T, Brown RF, Berg RD, Dunn AJ (2000) Bacterial translocation can increase plasma corticosterone and brain catecholamine and indoleamine metabolism. Am J Physiol Regul Integr Comp Physiol 279(6):R2164–R2172
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer New York
About this chapter
Cite this chapter
Bailey, M.T. (2014). Influence of Stressor-Induced Nervous System Activation on the Intestinal Microbiota and the Importance for Immunomodulation. In: Lyte, M., Cryan, J. (eds) Microbial Endocrinology: The Microbiota-Gut-Brain Axis in Health and Disease. Advances in Experimental Medicine and Biology(), vol 817. Springer, New York, NY. https://doi.org/10.1007/978-1-4939-0897-4_12
Download citation
DOI: https://doi.org/10.1007/978-1-4939-0897-4_12
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4939-0896-7
Online ISBN: 978-1-4939-0897-4
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)