Abstract
We recently hypothesized that across the range of normoxia to severe hypoxia the major determinant of central motor drive (CMD) during endurance exercise switches from a predominantly peripheral origin to a hypoxic-sensitive central component of fatigue. We found that peripheral locomotor muscle fatigue (pLMF) is the prevailing factor limiting central motor drive and therefore exercise performance from normoxia to moderate hypoxia (SaO2 > 75 %). In these levels of arterial hypoxemia, the development of pLMF is confined to a certain limit which varies between humans—pLMF does not develop to this limit in more severe hypoxia (SaO2 < 70 %) and exercise is prematurely terminated presumably to protect the brain from insufficient O2 supply. Based on the observations from normoxia to moderate hypoxia, we outlined a model suggesting that group III/IV muscle afferents impose inhibitory influences on the determination of CMD of working humans during high-intensity endurance exercise with the purpose to regulate and restrict the level of exercise-induced pLMF to an “individual critical threshold.” To experimentally test this model, we pharmacologically blocked somatosensory pathways originating in the working limbs during cycling exercise in normoxia. After initial difficulties with a local anesthetic (epidural lidocaine, L3–L4) and associated loss of locomotor muscle strength we switched to an intrathecally applied opioid analgesic (fentanyl, L3–L4). These experiments were the first ever to selectively block locomotor muscle afferents during high-intensity cycling exercise without affecting maximal locomotor muscle strength. In the absence of opioid-mediated neural feedback from the working limbs, CMD was increased and end-exercise pLMF substantially exceeded, for the first time, the individual critical threshold of peripheral fatigue. The outcome of these studies confirm our hypothesis claiming that afferent feedback inhibits CMD and restricts the development of pLMF to an individual critical threshold as observed from normoxia up to moderate hypoxia.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
It is critical to recognize that this manuscript was written in 2009 and therefore does not consider the more recent literature. Whole-body endurance exercise is impaired in hypoxia. The reduction in aerobic performance of humans stems from the diminished alveolar partial pressure of O2 and the resulting curtailment in arterial oxygenation affecting O2 transport to various organ systems including two of the key determinants of endurance performance—the skeletal muscles and the brain. The heart has also been identified as a significant contributor to compromise aerobic exercise in hypoxia. It was proposed that the myocardium is sensitive to arterial oxygenation and that exercise intensity—and the associated pumping activity of the heart—is regulated/limited to ensure proper myocardial oxygenation and to avoid severe myocardial hypoxia [51]. However, not only the lack of evidence supporting this hypothesis, but especially the finding that the myocardium appears to work adequately even in very severe hypoxia equivalent to the summit of Mt. Everest [53, 63], speak against the theory of hypoxia-induced myocardial dysfunctions limiting endurance exercise.
Aerobic exercise capacity is highly sensitive to even small reductions in arterial oxygenation. This statement is supported by observations made at sea level, namely, exercise-induced arterial hypoxemia [23] deteriorates whole-body endurance exercise [6, 36] and accelerates the rate of development of locomotor muscle fatigue [56] of trained humans. These phenomenon are exacerbated in hypoxia [2, 25, 41, 42], but the extent of the effects of hypoxia on aerobic capacity are not uniform amongst humans. Well-trained endurance athletes seem to be affected at lower degrees of hypoxia and the decrease is more rapid at more severe levels of arterial hypoxemia as compared to untrained or moderately trained humans whose aerobic capacity suffers by about ~1 % for each 100 m ascended above ~1500 m above sea level [16, 25, 27, 31, 54, 69]. In contrast, anaerobic exercise capacity (i.e., Wingate performance, sprint efforts, maximal muscle contractile force) is not, or much less, affected by hypoxia [2, 18, 42, 54].
Of fundamental importance in the discussion on hypoxia limiting endurance exercise is not only the degree of arterial hypoxemia , but also whether certain observations were made during acute (<1–2 days) or chronic (>2 days) altitude exposure since the latter is known to evoke adaptations, like increases in hemoglobin concentration promoting convective O2 transport, which partially compensate for exercise impairments as observed in acute hypoxia. The focus of this evaluation is on acute normobaric hypoxia and I discuss, based on data from experiments in normoxia and hypoxia, the role of locomotor muscles and brain in limiting endurance exercise under conditions of reduced convective O2 transport.
2 Effects of Hypoxia-Exposure on the Development of Peripheral Locomotor Muscle Fatigue
Alterations in O2 delivery to the working muscles affect the development of peripheral fatigue during whole body endurance exercise. Its rate of development is mediated by the rate of accumulation of intracellular metabolites known to cause failure of excitation–contraction coupling within the muscle fiber (e.g., H+, phosphates) [26, 47, 70]. Since the rate of accumulation of protons [1, 39] and the hydrolysis of phosphocreatine and concomitant cytoplasmic inorganic phosphate (Pi) accumulation [37, 39] are faster under conditions of reduced—and slower under conditions of increased—O2 delivery to the working muscle, both metabolites are considered as major determinant of the rate of development of peripheral fatigue in conditions of altered muscle O2 delivery [61].
The effect of altitude-exposure on oxygen delivery to the locomotor muscles is twofold. First, reductions in the inspiratory partial pressure of oxygen (PIO2; hypobaric hypoxia, i.e., exposure to altitude) or inspiratory oxygen fraction (FIO2) (normobaric hypoxia) cause a reduction in arterial hemoglobin saturation (SaO2) and arterial partial pressure of oxygen (PaO2) which combined result in a lower arterial oxygen content (CaO2) compared to sea level conditions. Although various compensatory mechanisms—like increases in limb blood flow and/or oxygen extraction fraction [14, 44, 45]—are available to reduce these forfeits in limb O2 transport at lower exercise intensities, cardiac output and leg blood flow at high intensities of exercise approach their peak values and are no longer capable of compensating for the reduced CaO2. And second, hyperventilation of heavy sustained exercise (>85 % VO2max) causes substantial increases in respiratory muscle work leading to respiratory muscle fatigue [22]. Accumulation of metabolites in these muscles activates unmyelinated group IV phrenic afferents which, in turn, increase sympathetic vasoconstrictor activity in the working limb via a supra-spinal reflex [22]. The result is a work of breathing-induced reduction in limb blood flow and a corresponding reduction in O2 delivery to the working muscles—even at sea level [35]. Now, hypoxia not only reduces CaO2 compared to normoxia but also substantially increases respiratory muscle work during exercise compared to the identical exercise performed in normoxia [8, 21]. These two factors lead to a faster and more severe development of respiratory muscle fatigue [66] which potentiates the metaboreflex described above. Amann et al. have previously shown that both of these factors, namely the reduction in CaO2 and the increased respiratory muscle work, significantly and independently contribute to the accelerated rate of development of peripheral locomotor muscle fatigue in hypoxia (Fig. 22.1) [8].
Individual (solid symbols) and group mean (open symbols) effects of cycling exercise in acute moderate hypoxia (FIO2 0.15) on quadriceps muscle fatigue expressed as a percent reduction in 1 Hz potentiated twitch force (Q tw,pot) from pre- to 2-min post-exercise. All trials were conducted at identical work rate (273 ± 6 W) and identical duration (8.6 ± 0.2 min). The figure illustrates the independent effects of inspiratory muscle work (W b) and hemoglobin saturation (SaO2) on peripheral locomotor muscle fatigue. A proportional assist ventilator (PAV) was used to reduce W b. By comparing conditions of (1) identical levels of reduced SaO2 in combination with significantly different levels of W b (Hypoxia-CTRL vs Hypoxia-PAV, Panel a) and (2) identical levels of reduced W b in combination with significantly different levels of SaO2 (Normoxia-PAV vs Hypoxia-PAV, Panel b), we were able to isolate the two main effects of hypoxia on peripheral locomotor muscle fatigue. Panel (a) shows the isolated effects of W b in hypoxia on quadriceps fatigue. W b was reduced by about 70 % whereas SaO2 (~82 %) was unchanged from Hypoxia-CTRL to Hypoxia-PAV. Panel (b) shows the isolated effects of SaO2 on quadriceps fatigue. SaO2 was reduced from ~95 % to ~82 % whereas W b was unchanged from Normoxia-PAV to Hypoxia-PAV. Panel (c) shows the exacerbating effects of reductions in SaO2 (~14 %) combined with increases in W b (~36 %) on peripheral fatigue when exercising in hypoxia vs normoxia. From Amann et al. [8]
3 Effects of Peripheral Locomotor Muscle Fatigue and Hypoxia on Muscle Afferent Activity
With the onset of exercise, but especially when peripheral fatigue develops, mechanical and chemical stimuli change the activity of various intramuscular receptors (metaboceptive/nociceptive) which is reflected in the firing frequency of the respective large- and small diameter afferents (group I/II and group III/IV, respectively) [30]. Group III/IV muscle afferents have also been shown to be stimulated by intra-arterial injections of metabolic byproducts of muscle contraction/peripheral muscle fatigue [30, 43, 48, 49, 57, 58, 62]. Furthermore, during prolonged maximal efforts and especially during contractile fatigue characterized by the intramuscular accumulation of metabolic byproducts, muscle afferent feedback is thought to cause a reflex inhibition of the α-motoneuron pool of the working muscles at spinal, but especially via supraspinal levels [28, 29].
In addition, small diameter muscle afferents are also sensitive to reductions in arterial oxygenation, per se. Acute arterial hypoxemia increases baseline discharge frequency of group III, and especially of group IV muscle afferents in resting cats [38, 46] and rabbits [12]. Furthermore, during muscle contraction, the net firing frequency of group III/IV muscle afferents is higher in hypoxia compared to normoxia. Hill et al. directly recorded from group III and IV fibers of triceps surae muscles of barbiturate-anesthetized cats and found potentiated responses of these afferents to electrically induced static muscle contraction in acute hypoxia vs normoxia (PaO2 ~23 mmHg vs. ~108 mmHg, respectively) [38]. This increased net discharge results from the higher resting firing frequency plus the increase in discharge frequency evoked by the hypoxia-induced exaggerated accumulation of metabolites [39] known to stimulate small diameter afferents.
4 Effects of Hypoxia-Exposure on Brain
Insufficient O2 transport to the brain depresses electrical activity of cerebral neurons. Blunted activity and excitability of cortical neurons result not only from a hypoxia-induced disturbance of ionic homeostasis of cerebral nerve cells [33], but also from the extracellular release of neurotransmitter affecting the postsynaptic membrane [32]. This derangement of the turnover of several CNS neurotransmitters (i.e., dopamine, norepinephrine, serotonin) might affect the limbic-to-motor link within the basal ganglia [50], motivation [60], preparation and execution of movement [20], and cognitive functions [34] involving both the prefrontal cortex and the basal ganglia [20].
Indirect evidence suggests that cerebral oxygenation as seen during high intensity whole body endurance exercise is unlikely to play an important limiting role for endurance exercise performance in normoxia and acute moderate hypoxia (SaO2 > 80 %) [11, 67], whereas severe hypoxia might impose cerebral hypoxia of sufficient severity to limit whole body exercise [11]. This postulate is based on various classical “reoxygenation” studies. For example, Amann et al. had subjects perform the identical strenuous constant-load cycling exercise to task failure (pedal frequency drops below 70 % of self selected cadence for ≥5 s) in normoxia (FIO2 0.21, SaO2 ~ 93 %), acute moderate hypoxia (FIO2 0.15, SaO2 ~ 82 %), and acute severe hypoxia (FIO2 0.10, SaO2 ~ 66 %) [11]. At task failure, arterial oxygenation was surreptitiously increased via switching the inspirate to a hyperoxic gas mixture (FIO2 0.30) and the subjects, unaware of the gas switch, continued to exercise to exhaustion (pedal frequency drops below 60 % of self selected cadence for ≥5 s). Frontal cerebral cortex oxygenation was continuously measured throughout the trials via near-infrared spectroscopy. At task failure, just prior to the increase in FIO2 to 0.30, cerebral oxygenation in the normoxic trial was slightly below resting values (~6 %, not significant), whereas in acute moderate and severe hypoxia, cerebral cortex oxygenation was substantially reduced below resting normoxic baseline levels (by 18 % and 24 %, respectively). Following the increase in FIO2 to 0.30, CaO2 in the normoxic and moderate hypoxic trial increased towards resting normoxic levels within seconds and cerebral tissue oxygenation substantially increased. However, despite the increase in brain O2 delivery, the subjects were not able to maintain or further increase central neural drive to continue the exercise suggesting that cerebral oxygenation might not have limited performance [11]. In contrast, following reoxygenation at task failure in severe hypoxia, CaO2 increased to resting normoxic baseline levels within seconds, cerebral oxygenation immediately and significantly rose, and the subjects were able to continue the exercise for an additional ~3.4 min until exhaustion was reached in hyperoxia (Fig. 22.2a). These findings are supported by other experiments in acute and chronic hypoxia [15, 17, 42, 64, 65].
5 What Determines the Regulation of Central Motor Drive and the Voluntary Cessation of Endurance Exercise in Normoxia and Hypoxia? The Development of a Hypothesis
Previous findings in humans showed that during incremental cycling exercise to voluntary exhaustion in normoxia and moderate normobaric hypoxia (FIO2 0.14, SaO2 ~ 81 %), changes in sarcoplasmic reticulum Ca2+ cycling [24] and Na+-K+-ATPase [59] determined from muscle biopsies obtained at voluntary exhaustion were identical, despite marked differences in time to exhaustion (~13 %) and peak work rate (~19 %). Furthermore, magnetic resonance imaging measurements during incremental plantar flexion exercise to voluntary exhaustion showed hypoxia-induced (FIO2 0.10, PaO2 ~ 45 mmHg) acceleration and hyperoxia-induced (FIO2 1.00, PaO2 ~ 600 mmHg) slowing of intra-cellular Pi and H+ accumulation in calf muscle and identical levels of these muscle metabolites, which are known to cause peripheral fatigue, were achieved at end-exercise—despite markedly different peak work rates and exercise times [39]. In a different study, Hogan and Welch [40] had subjects cycling at the same absolute workload and for the same duration but breathing different FIO2s (0.16 or 0.60) during exercise. By doing so, the authors induced different levels of [H+] and [La−] and investigated these effects on subsequent (4 min break) cycling performance trials in normoxia. Blood [H+] and [La−] at the beginning of these constant workload performance trials were significantly higher following the hypoxic vs hyperoxic “pretreatment” and resulted in a significantly shorter time to exhaustion for the subsequent constant load exercise trial. Nevertheless, [H+] and [La−] at exhaustion were not significantly different between trials despite the marked differences in exercise performance time [40]. Combined, these experiments suggest that exercise is regulated to preserve a certain intramuscular metabolic milieu.
Based on these findings and knowing that endurance exercise performance and the rate of exercise-induced fatigue development critically depend on convective O2 transport [2] (see above), Amann et al. conducted a study in which four different 5-km cycling time trials (power output voluntarily adjustable, [7]) were performed at different levels of CaO2 —from moderate hypoxia (FIO2 0.15, SaO2 ~ 78 %) to hyperoxia (FIO2 1.00, SaO2 100 %) [6]. Central motor drive and power output were upregulated with increased and downregulated with reduced CaO2; however, the magnitude of peripheral locomotor muscle fatigue developed at end-exercise was identical. Since the rate of accumulation of peripheral fatigue (i.e., fatigue causing metabolites) is enhanced with reduced CaO2 and slowed with increased CaO2, the downregulation of central neural drive and consequently power output in the presence of reduced CaO2 ensured that the rate of development of peripheral locomotor muscle fatigue was slowed and prevented from exceeding a certain limit. Hence, end-exercise peripheral locomotor muscle fatigue was identical between the time trials of various levels of CaO2 and limited to an “individual critical threshold” [6]. The existence of this individual critical threshold of peripheral fatigue that is never exceeded during high intensity whole body endurance exercise was confirmed in various other investigations [4, 8, 11, 55, 59] and the idea of peripheral locomotor muscle fatigue as a sensed and regulated variable in normoxia and moderate hypoxia was introduced [3, 5, 19].
The postulate claims that peripheral locomotor muscle fatigue develops only up to a threshold unique for each individual and endurance exercise is either voluntarily terminated once peripheral fatigue has reached this critical threshold (in case of constant workload trials) or the exercise intensity is drastically reduced once a critical rate of fatigue development is reached (in case of time trial exercise where power output is voluntarily adjustable). We interpreted existing correlative evidence to mean that the rate of development of peripheral fatigue is associated with increasing sensory feedback (i.e., group III/IV muscle afferents which are sensitive to fatigue metabolites) from locomotor muscles to the central nervous system (CNS) . In turn this feedback influences the regulation of central motor drive—and consequently locomotor muscle power output—in order to limit the level of peripheral fatigue development and thereby avoid intolerable levels of effort/“pain” perception and/or excessive muscle dysfunction as presumably associated with peripheral fatigue beyond the individual critical threshold (Fig. 22.3).
In other words, our fatigue theorem claims that neural afferent feedback associated with peripheral locomotor muscle fatigue exerts an inhibitory influence on the central motor drive resulting in a centrally mediated limitation of exercise in normoxic and moderately hypoxic (SaO2 > 76 %) exercise [6, 11]. To be very explicit here, I distinctively emphasize that peripheral locomotor muscle fatigue and/or its rate of development might only be one of many potential mechanisms [52] available to consciously and/or subconsciously influence the determination of central motor output and performance during high intensity whole body endurance exercise.
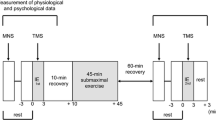
However, what happens if humans are exposed to more severe levels of arterial hypoxemia ? Is the exercise-induced magnitude of peripheral locomotor muscle fatigue and/or the rate of development of fatigue of these muscles still as important a regulated variable at extreme altitudes/arterial hypoxemia? Or does the priority change and other organ systems, like the brain, take over the hierarchy of regulated variables due to the increased threat associated with severe systemic hypoxemia induced by exercise beyond moderate hypoxia (SaO2 < 76 %)? We have suggested that the relative effects of centrally vs peripherally originating impairments of central motor drive (and consequently limitations in exercise performance) change with the level of convective O2 transport as affected by acute hypoxia [2, 11]. In a carefully designed study, subjects were instructed to pedal against a heavy intensity fixed workload to exhaustion in normoxia, and moderate and severe hypoxia (FIO2/SaO2: 0.21/94 %, 0.15/82 %, and 0.10/67 %, respectively). Clear criteria for task failure (drop in pedal cadence below 70 % of self-selected target cadence for ≥5 s) and exhaustion (drop in pedal cadence below 60 % of self-selected target cadence for ≥5 s) were established prior to the study. When the subjects, unaware of the procedure, reached task failure in each condition, arterial hypoxemia was rapidly removed by surreptitiously switching to an FIO2 of 0.3 (reoxygenation). A significant prolongation of exercise time to exhaustion was not achieved following reoxygenation at task failure in normoxia (SaO2 ~ 94 %, time to task failure ~660 s) and moderate hypoxia (SaO2 ~ 82 %, time to task failure ~280 s). However, in severe hypoxia (SaO2 ~ 67 %, time to task failure ~130 s), reoxygenation at task failure elicited a significant prolongation (~170 %) of time to exhaustion (Fig. 22.2a).
The subjects performed constant-load cycling exercise (333 ± 9 W) in normoxia (FIO2 0.21, SaO2 ~ 93 %) and two levels of hypoxia (FIO2 0.15/SaO2 ~ 82 % and FIO2 0.10/SaO2 ~ 66 %). The target pedal frequency was individually chosen but had to be held constant throughout exercise. At task failure (pedal frequency drops below 70 % of self selected cadence for ≥5 s), arterial and cerebral oxygenation was surreptitiously increased via switching the inspirate to a slightly hyperoxic gas mixture (FIO2 0.30) and the subjects, unaware of the gas switch, continued to exercise to exhaustion (pedal frequency drops below 60 % of self selected cadence for ≥5 s). (a) Time to task failure and additional time to exhaustion. Note that the subjects were not able to significantly prolong exercise following reoxygenation at task failure in normoxia and moderate hypoxia. In contrast, exercise was significantly prolonged after reoxygenation at task failure in severe hypoxia. (b) Exercise-induced quadriceps fatigue assessed via changes in potentiated quadriceps twitch force (Q tw,pot) as measured pre- vs post-exercise in response to supramaximal femoral nerve stimulation. On separate days, peripheral fatigue was assessed following task failure (left bar of the respective condition) and following exhaustion (right bar). Note that peripheral fatigue at task failure and exhaustion were identical in normoxia and moderate hypoxia; whereas at task failure in severe hypoxia, the locomotor muscles were significantly less fatigued. Following reoxygenation, peripheral fatigue continued to increase during the additional 205 s of cycling to reach the similar level at exhaustion as seen in normoxia and moderate hypoxia. #P < 0.05. Modified from Amann et al. [11]
Schematic illustration of our proposed fatigue theorem. The solid line indicates efferent nerve activity (central motor drive), the dashed line indicates afferent nerve activity. This regulatory mechanism suggests that the cortical projection of muscle afferents (inhibitory feedback) affects the determination of the magnitude of central motor drive which in turn determines power output of the locomotor muscles. The magnitude of power output determines the metabolic milieu within the working muscles which in turn determines the magnitude of the inhibitory afferent feedback. Based on our data, the purpose of this feedback loop is apparently to restrict peripheral locomotor muscle fatigue to an individual threshold and/or sensory tolerance limit which is never exceeded
Why this difference with severe hypoxia? At task failure in normoxia and moderate hypoxia peripheral locomotor muscle fatigue—assessed via changes in quadriceps twitch force as measured pre- versus post-exercise in response to supramaximal femoral nerve stimulation—was identical (despite different exercise performances) and presumably reached the individual critical threshold. As expected, the magnitude of peripheral fatigue did not change further within the additional few seconds of exercise to exhaustion following reoxygenation in normoxia or moderate hypoxia (Fig. 22.2b) [11]. This is consistent with the literature indicating that reoxygenation has no instant alleviating effect on the already induced magnitude of peripheral muscle fatigue. Interestingly however, at task failure in severe hypoxia peripheral muscle fatigue was significant but only about two-thirds of the level of fatigue measured at task failure in normoxia and moderate hypoxia and therefore far below the individual critical threshold. Following reoxygenation in severe hypoxia, subjects continued to exercise and peripheral fatigue continued to develop to the same level (individual critical threshold) as observed at exhaustion in normoxia and moderate hypoxia (Fig. 22.2b) [11].
So, what limits endurance exercise in normoxia and moderate hypoxia vs severe hypoxia and why was there significantly less locomotor muscle fatigue at task failure in severe hypoxia? The data indicate that exercise- and altitude-induced arterial hypoxemia and the associated reduction in cerebral oxygenation as experienced at sea level and up to moderate hypoxia, per se, might not be severe enough to impose an inhibitory influence on central motor drive in healthy humans [2, 11, 64, 65]. The CNS at these levels of hypoxemia/cerebral oxygenation “allows” the development of peripheral locomotor muscle fatigue until the individual critical threshold is reached, which then in turn curtails central motor drive presumably via strong inhibitory neural feedback to the brain as proposed above. The roles seem to be reversed in severe hypoxia (SaO2 < 68 %). The level of arterial hypoxemia during exercise at those extreme altitudes might impose a severe threat to cerebral oxygenation. Accordingly, central motor output might be constrained largely independent from any inhibitory afferent feedback originating in the periphery. This central inhibitory effect of severe hypoxia probably serves to avoid severe cerebral dysfunction far in advance of reaching the individual critical threshold of peripheral muscle fatigue.
6 Experimental Challenge and Verification of Hypothesis Under Normoxic Conditions
Again, based on strong correlative evidence as partly outlined above [4, 6, 8, 11, 39, 55], we have formulated a hypothesis. Namely, somatosensory feedback from the fatiguing locomotor muscles exerts inhibitory influence on central motor drive to modulate and/or limit the development of peripheral muscle fatigue during high intensity whole body endurance exercise (SaO2 > ~70 %), presumably to avoid a severe disturbance of locomotor muscle homeostasis—and this postulate had to be challenged experimentally. As a reminder, the key component of our proposed “regulatory mechanism ” (Fig. 22.3) is the afferent arm consisting of both myelinated (group III) and unmyelinated (group IV) nerve fibers which increase their spontaneous discharge—and therefore their cortical projection—in the presence of metabolic byproducts of fatigue.
As a first step in testing our hypothesis experimentally, we blocked the cortical projection of locomotor muscle afferent feedback during a 5 km cycling time trial via the lumbar epidural injection of a local anesthetic (0.5 % lidocaine, vertebral interspace L3–L4) [9]. However, lidocaine also affected efferent motor nerves leading to a significant loss in resting locomotor muscle strength (~22 %). These confounding effects did not allow us to adequately test the role of afferent feedback effects, per se, on exercise performance. And indeed, power output during the time trial performed with the local anesthetic was lower as compared to the control trial. However, several lines of evidence were observed which support a higher central neural drive during the time trial performed with blocked afferent feedback from the locomotor muscles. For example, electromyographic (EMG) activity (relative to the maximal EMG measured during pre-race maximal voluntary muscle contractions—which was lower with vs without epidural lidocaine) obtained from the vastus lateralis suggests that on average and over time the “drive” to race averaged about 9 % stronger when neural feedback was blocked [9]. Furthermore, cardiorespiratory variables (minute ventilation, heart rate, blood pressure) are well known to reliably reflect increases in central motor drive [13, 68]. A substantially increased central command during the time trial with impaired neural feedback was reflected by the similar or even greater cardiorespiratory response to exercise despite the significantly lower workload and metabolic rate during the lidocaine vs the control time trial. In other words, heart rate and mean arterial blood pressure were nearly identical and minute ventilation was even significantly increased despite the lower power output and metabolic rate during lidocaine vs control 5 km time trial [9] (Fig. 22.4).
Power output and physiological responses during a 5 km cycling time trial without (control, solid symbols) and with (experimental, lumbar epidural anesthesia, open symbols) blocked somatosensory neural feedback from the fatiguing locomotor muscles. The subjects were required to reach an individual target power output before the race was launched. Group mean performance was significantly reduced from the control trial (7.35 ± 0.10 min) to the experimental trial (7.66 ± 0.17 min). Mean iEMG of the vastus lateralis was normalized to the iEMG obtained from pre-exercise MVC maneuvers performed either without or with epidural lidocaine. Each point represents the mean iEMG of the preceding 0.5 km section. Despite the substantially lower power output during the experimental trial, central neural drive was higher during the experimental trial vs the control trial. This is indicated by (1) the increased relative integrated EMG (iEMG), (2) ventilation (VE) increased out of proportion to the metabolic rate (VE/VCO2), and (3) similar heart rate and blood pressure (not shown) despite the higher power output during the control trial. From Amann et al. [9]
To circumvent the lidocaine-induced forfeit of locomotor muscle force generating capacity and to adequately determine the effect of neural feedback from exercising muscle on power output and the development of peripheral fatigue during high intensity whole body endurance exercise, Amann et al. then used fentanyl (intrathecally, L3–L4) an opioid analgesic, to selectively block the cortical projection of ascending sensory pathways without affecting motor nerve activity or maximal force output [10]. Again, the subjects had to perform a 5 km cycling time trial either with (fentanyl) or without (placebo) opioid-mediated neural feedback from the locomotor muscles. Blocking these fibers attenuated the centrally mediated reflex inhibition and central motor drive during the fentanyl time trial was less restricted and significantly higher as normally chosen by the athlete, i.e., in the placebo time trial (Fig. 22.5). This higher central neural drive resulted in a substantially higher power output during the first half of the race and the CNS “allowed” or “tolerated” the exercise-induced development of peripheral locomotor muscle fatigue drastically beyond levels as observed following the same exercise but with an intact neural feedback system (Figs. 22.5 and 22.6) [10]. In the absence of afferent feedback, the magnitude of central neural drive was thus uncoupled from the intramuscular metabolic milieu of the locomotor muscles. As a consequence, the “naïve” CNS did not limit the development of excessive peripheral fatigue beyond the individual critical threshold which caused ambulatory problems like short-term difficulties with upright standing and walking. Nevertheless, the resulting metabolic and respiratory acidosis eventually prevented the performance to be improved during the fentanyl vs placebo time trial .
Effect of modified somatosensory feedback on neural drive and power output during a 5 km cycling time trial. All subjects raced with no intervention (Control), with a placebo injection (Placebo; interspinous ligament injection of sterile normal saline, L3–L4), and with intrathecal fentanyl (Fentanyl, L3–L4). (a) Effects of opioid analgesic (fentanyl) on group mean integrated EMG (iEMG) of vastus lateralis. Mean iEMG of the vastus lateralis was normalized to the iEMG obtained from pre-exercise MVC maneuvers performed either without (Placebo and Control) or with (Fentanyl) intrathecal fentanyl. Each point represents the mean iEMG of the preceding 0.5 km section. (b) Group mean power output during the 5 km time trial with and without impaired afferent feedback. The subjects were required to reach an individual target power output before the race was launched. *P < 0.05 (Fentanyl vs Placebo). From Amann et al. [10]
Individual (solid symbols) and group mean (open symbols) effects of 5 km time trial without (control trial, placebo trial) and with intrathecal fentanyl (fentanyl trial) on quadriceps twitch force (Q tw,pot). Exercise performance was similar between Control and Placebo (~7.49 min, P = 0.75) which was also reflected in similar exercise-induced reductions in Q tw,pot from before to 3-min after the time trial. Despite a similar overall exercise performance (7.51 ± 0.13 min), end-exercise quadriceps fatigue was significantly exacerbated following the Fentanyl vs Placebo trial (P < 0.001). From Amann et al. [10]
7 Summary
We have formulated and tested a model with the intent to provide an alternative approach to the “traditional” way of explaining hypoxia-induced endurance exercise limitations in terms of reduced O2 transport into the muscle cell or changes in relative exercise intensity. Our model suggests that exercise- and hypoxia-induced alterations of the metabolic milieu (and associated peripheral fatigue) of locomotor muscles affect, in a dose-dependent manner, the firing rate—and thus the cortical projection—of muscle afferents providing inhibitory feedback to the determination of central motor drive during high intensity whole-body endurance exercise. The purpose of this proposed feedback-loop might be to regulate and restrict the level of exercise-induced peripheral locomotor muscle fatigue to an “individual critical threshold” and ultimately to prevent an excessive disturbance of muscle homeostasis. We believe that this regulatory mechanism is applicable during strenuous endurance exercise at sea level and up to moderate hypoxia (SaO2 > ~75 %), whereas in acute severe hypoxia (SaO2 < ~70 %), a critical level of CNS hypoxia presumably precedes the development of significant peripheral muscle fatigue and dominates the decision to reduce central motor drive and/or to terminate the exercise.
References
Adams RP, Welch HG. Oxygen uptake, acid-base status, and performance with varied inspired oxygen fractions. J Appl Physiol. 1980;49:863–8.
Amann M, Calbet JA. Convective oxygen transport and fatigue. J Appl Physiol. 2008;104:861–70.
Amann M, Dempsey JA. The concept of peripheral locomotor muscle fatigue as a regulated variable. J Physiol. 2008;586:2029–30.
Amann M, Dempsey JA. Locomotor muscle fatigue modifies central motor drive in healthy humans and imposes a limitation to exercise performance. J Physiol. 2008;586(1):161–73.
Amann M, Dempsey JA. Peripheral muscle fatigue from hyperoxia to moderate hypoxia - a carefully regulated variable? Physiology News. 2007;66:28–9.
Amann M, Eldridge MW, Lovering AT, Stickland MK, Pegelow DF, Dempsey JA. Arterial oxygenation influences central motor output and exercise performance via effects on peripheral locomotor muscle fatigue. J Physiol. 2006;575(3):937–52.
Amann M, Hopkins WG, Marcora SM. Similar sensitivity of time to exhaustion and time trial to changes in endurance. Med Sci Sports Exerc. 2008;40:574–8.
Amann M, Pegelow DF, Jacques AJ, Dempsey JA. Inspiratory muscle work in acute hypoxia influences locomotor muscle fatigue and exercise performance of healthy humans. Am J Physiol Regul Integr Comp Physiol. 2007;293:R2036–45.
Amann M, Proctor LT, Sebranek JJ, Eldridge MW, Pegelow DF, Dempsey JA. Somatosensory feedback from the limbs exerts inhibitory influences on central neural drive during whole body endurance exercise. J Appl Physiol. 2008;105:1714–24.
Amann M, Proctor LT, Sebranek JJ, Pegelow DF, Dempsey JA. Opioid-mediated muscle afferents inhibit central motor drive and limit peripheral muscle fatigue development in humans. J Physiol. 2008;587:271–83.
Amann M, Romer LM, Subudhi AW, Pegelow DF, Dempsey JA. Severity of arterial hypoxaemia affects the relative contributions of peripheral muscle fatigue to exercise performance in healthy humans. J Physiol. 2007;581:389–403.
Arbogast S, Vassilakopoulos T, Darques JL, Duvauchelle JB, Jammes Y. Influence of oxygen supply on activation of group IV muscle afferents after low-frequency muscle stimulation. Muscle Nerve. 2000;23:1187–93.
Asmussen E, Johansen SH, Jorgensen M, Nielsen M. On the nervous factors controlling respiration and circulation during exercise. Experiments with curarization. Acta Physiol Scand. 1965;63:343–50.
Barclay JK. A delivery-independent blood flow effect on skeletal muscle fatigue. J Appl Physiol. 1986;61:1084–90.
Boushel R, Calbet JA, Radegran G, Sondergaard H, Wagner PD, Saltin B. Parasympathetic neural activity accounts for the lowering of exercise heart rate at high altitude. Circulation. 2001;104:1785–91.
Buskirk ER, Kollias J, Akers RF, Prokop EK, Reategui EP. Maximal performance at altitude and on return from altitude in conditioned runners. J Appl Physiol. 1967;23:259–66.
Calbet JA, Boushel R, Radegran G, Sondergaard H, Wagner PD, Saltin B. Why is VO2 max after altitude acclimatization still reduced despite normalization of arterial O2 content? Am J Physiol Regul Integr Comp Physiol. 2003;284:R304–16.
Calbet JA, De Paz JA, Garatachea N, Cabeza De Vaca S, Chavarren J. Anaerobic energy provision does not limit Wingate exercise performance in endurance-trained cyclists. J Appl Physiol. 2003;94:668–76.
Calbet JAL. The rate of fatigue accumulation as a sensed variable. J Physiol. 2006;575:688–9.
Chaudhuri A, Behan PO. Fatigue and basal ganglia. J Neurol Sci. 2000;179:34–42.
Cibella F, Cuttitta G, Romano S, Grassi B, Bonsignore G, Milic-Emili J. Respiratory energetics during exercise at high altitude. J Appl Physiol. 1999;86:1785–92.
Dempsey JA, Romer L, Rodman J, Miller J, Smith C. Consequences of exercise-induced respiratory muscle work. Respir Physiol Neurobiol. 2006;151:242–50.
Dempsey JA, Wagner PD. Exercise-induced arterial hypoxemia. J Appl Physiol. 1999;87:1997–2006.
Duhamel TA, Green HJ, Sandiford SD, Perco JG, Ouyang J. Effects of progressive exercise and hypoxia on human muscle sarcoplasmic reticulum function. J Appl Physiol. 2004;97:188–96.
Ferretti G, Moia C, Thomet JM, Kayser B. The decrease of maximal oxygen consumption during hypoxia in man: a mirror image of the oxygen equilibrium curve. J Physiol. 1997;498(Pt 1):231–7.
Fitts RH. The cross-bridge cycle and skeletal muscle fatigue. J Appl Physiol. 2008;104:551–8.
Fulco CS, Rock PB, Cymerman A. Maximal and submaximal exercise performance at altitude. Aviat Space Environ Med. 1998;69:793–801.
Gandevia SC. Spinal and supraspinal factors in human muscle fatigue. Physiol Rev. 2001;81:1725–89.
Gandevia SC, Macefield G, Burke D, McKenzie DK. Voluntary activation of human motor axons in the absence of muscle afferent feedback. The control of the deafferented hand. Brain. 1990;113(Pt 5):1563–81.
Garland SJ, Kaufman MP. Role of muscle afferents in the inhibition of motoneurons during fatigue. In: Gandevia SC, Enoka RM, McComas AJ, Stuart DG, Thomas CK, editors. Fatigue: neural and muscular mechanisms. New York, NY: Plenum Press; 1995. p. 271–8.
Gore CJ, Hahn AG, Scroop GC, Watson DB, Norton KI, Wood RJ, Campbell DP, Emonson DL. Increased arterial desaturation in trained cyclists during maximal exercise at 580 m altitude. J Appl Physiol. 1996;80:2204–10.
Haddad GG, Jiang C. O2 deprivation in the central nervous system: on mechanisms of neuronal response, differential sensitivity and injury. Prog Neurobiol. 1993;40:277–318.
Hansen AJ. Effect of anoxia on ion distribution in the brain. Physiol Rev. 1985;65:101–48.
Harik SI, Busto R, Martinez E. Norepinephrine regulation of cerebral glycogen utilization during seizures and ischemia. J Neurosci. 1982;2:409–14.
Harms CA, Babcock MA, McClaran SR, Pegelow DF, Nickele GA, Nelson WB, Dempsey JA. Respiratory muscle work compromises leg blood flow during maximal exercise. J Appl Physiol. 1997;82:1573–83.
Harms CS, McClaran S, Nickele GA, Pegelow DF, Nelson WB, Dempsey JA. Effect of exercise-induced arterial O2 desaturation on VO2max in women. Med Sci Sports Exerc. 2000;32:1101–8.
Haseler LJ, Richardson RS, Videen JS, Hogan MC. Phosphocreatine hydrolysis during submaximal exercise: the effect of FIO2. J Appl Physiol. 1998;85:1457–63.
Hill JM, Pickar JG, Parrish MD, Kaufman MP. Effects of hypoxia on the discharge of group III and IV muscle afferents in cats. J Appl Physiol. 1992;73:2524–9.
Hogan MC, Richardson RS, Haseler LJ. Human muscle performance and PCr hydrolysis with varied inspired oxygen fractions: a 31P-MRS study. J Appl Physiol. 1999;86:1367–73.
Hogan MC, Welch HG. Effect of varied lactate levels on bicycle ergometer performance. J Appl Physiol. 1984;57:507–13.
Kayser B. Why is endurance performance decreased at high altitude? Schweizerische Zeitschrift für Sportmedizin und Sporttraumatologie. 2005;53:54–60.
Kayser B, Narici M, Binzoni T, Grassi B, Cerretelli P. Fatigue and exhaustion in chronic hypobaric hypoxia: influence of exercising muscle mass. J Appl Physiol. 1994;76:634–40.
Kniffki KD, Mense S, Schmidt RF. Responses of group IV afferent units from skeletal muscle to stretch, contraction and chemical stimulation. Exp Brain Res. 1978;31:511–22.
Koskolou MD, Calbet JA, Radegran G, Roach RC. Hypoxia and the cardiovascular response to dynamic knee-extensor exercise. Am J Physiol. 1997;272:H2655–63.
Koskolou MD, Roach RC, Calbet JA, Radegran G, Saltin B. Cardiovascular responses to dynamic exercise with acute anemia in humans. Am J Physiol. 1997;273:H1787–93.
Lagier-Tessonnier F, Balzamo E, Jammes Y. Comparative effects of ischemia and acute hypoxemia on muscle afferents from tibialis anterior in cats. Muscle Nerve. 1993;16:135–41.
Lannergren J, Westerblad H. Force decline due to fatigue and intracellular acidification in isolated fibres from mouse skeletal muscle. J Physiol. 1991;434:307–22.
Mense S. Nervous outflow from skeletal muscle following chemical noxious stimulation. J Physiol. 1977;267:75–88.
Mense S. Sensitization of group IV muscle receptors to bradykinin by 5-hydroxytryptamine and prostaglandin E2. Brain Res. 1981;225:95–105.
Nauta WJH. The relationship of basal ganglia to the limbic system. In: Vinken PJ, Bruyn GW, editors. Handbook of clinical neurology. Amsterdam: Elsevier Science; 1986. p. 19–32.
Noakes TD, Peltonen JE, Rusko HK. Evidence that a central governor regulates exercise performance during acute hypoxia and hyperoxia. J Exp Biol. 2001;204:3225–34.
Nybo L, Secher NH. Cerebral perturbations provoked by prolonged exercise. Prog Neurobiol. 2004;72:223–61.
Reeves JT, Groves BM, Sutton JR, Wagner PD, Cymerman A, Malconian MK, Rock PB, Young PM, Houston CS. Operation Everest II: preservation of cardiac function at extreme altitude. J Appl Physiol. 1987;63:531–9.
Roach RC, Maes D, Sandoval D, Robergs RA, Icenogle M, Hinghofer-Szalkay H, Lium D, Loeppky JA. Exercise exacerbates acute mountain sickness at simulated high altitude. J Appl Physiol. 2000;88:581–5.
Romer LM, Haverkamp HC, Amann M, Lovering AT, Pegelow DF, Dempsey JA. Effect of acute severe hypoxia on peripheral fatigue and endurance capacity in healthy humans. Am J Physiol Regul Integr Comp Physiol. 2007;292:R598–606.
Romer LM, Haverkamp HC, Lovering AT, Pegelow DF, Dempsey JA. Effect of exercise-induced arterial hypoxemia on quadriceps muscle fatigue in healthy humans. Am J Physiol Regul Integr Comp Physiol. 2006;290:R365–75.
Rotto DM, Kaufman MP. Effect of metabolic products of muscular contraction on discharge of group III and IV afferents. J Appl Physiol. 1988;64:2306–13.
Rybicki KJ, Waldrop TG, Kaufman MP. Increasing gracilis muscle interstitial potassium concentrations stimulate group III and IV afferents. J Appl Physiol. 1985;58:936–41.
Sandiford SD, Green HJ, Duhamel TA, Schertzer JD, Perco JD, Ouyang J. Muscle Na-K-pump and fatigue responses to progressive exercise in normoxia and hypoxia. Am J Physiol Regul Integr Comp Physiol. 2005;289:R441–9.
Schultz W, Dayan P, Montague PR. A neural substrate of prediction and reward. Science. 1997;275:1593–9.
Stary CM, Hogan MC. Impairment of Ca(2+) release in single Xenopus muscle fibers fatigued at varied extracellular PO(2). J Appl Physiol. 2000;88:1743–8.
Steinhagen C, Hirche HJ, Nestle HW, Bovenkamp U, Hosselmann I. The interstitial pH of the working gastrocnemius muscle of the dog. Pflugers Arch. 1976;367:151–6.
Suarez J, Alexander JK, Houston CS. Enhanced left ventricular systolic performance at high altitude during Operation Everest II. Am J Cardiol. 1987;60:137–42.
Subudhi AW, Dimmen AC, Roach RC. Effects of acute hypoxia on cerebral and muscle oxygenation during incremental exercise. J Appl Physiol. 2007;103:177–83.
Subudhi AW, Lorenz MC, Fulco CS, Roach RC. Cerebrovascular responses to incremental exercise during hypobaric hypoxia: effect of oxygenation on maximal performance. Am J Physiol Heart Circ Physiol. 2008;294:H164–71.
Vogiatzis I, Georgiadou O, Koskolou M, Athanasopoulos D, Kostikas K, Golemati S, Wagner H, Roussos C, Wagner PD, Zakynthinos S. Effects of hypoxia on diaphragmatic fatigue in highly trained athletes. J Physiol. 2007;581:299–308.
Volianitis S, Fabricius-Bjerre A, Overgaard A, Stromstad M, Bjarrum M, Carlson C, Petersen NT, Rasmussen P, Secher NH, Nielsen HB. The cerebral metabolic ratio is not affected by oxygen availability during maximal exercise in humans. J Physiol. 2008;586:107–12.
Waldrop TG, Eldridge FL, Iwamoto GA, Mitchell JH. Central neural control of respiration and circulation during exercise. In: Rowell LB, Shepherd JT, editors. Handbook of physiology. Section 12: Exercise: Regulation and Integration of Multiple Systems. New York, NY: Oxford University Press; 1996. p. 333–80.
Wehrlin JP, Hallen J. Linear decrease in VO2max and performance with increasing altitude in endurance athletes. Eur J Appl Physiol. 2006;96:404.
Westerblad H, Allen DG, Lannergren J. Muscle fatigue: lactic acid or inorganic phosphate the major cause? News Physiol Sci. 2002;17:17–21.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2016 Springer Science+Business Media New York
About this chapter
Cite this chapter
Amann, M., Dempsey, J.A. (2016). Ensemble Input of Group III/IV Muscle Afferents to CNS: A Limiting Factor of Central Motor Drive During Endurance Exercise from Normoxia to Moderate Hypoxia. In: Roach, R., Hackett, P., Wagner, P. (eds) Hypoxia. Advances in Experimental Medicine and Biology, vol 903. Springer, Boston, MA. https://doi.org/10.1007/978-1-4899-7678-9_22
Download citation
DOI: https://doi.org/10.1007/978-1-4899-7678-9_22
Published:
Publisher Name: Springer, Boston, MA
Print ISBN: 978-1-4899-7676-5
Online ISBN: 978-1-4899-7678-9
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)