Abstract
Mesenchymal Stem Cells (MSC) are non-hematopoietic adult stromal cells that reside in a perivascular niche in close association with pericytes and endothelial cells and possess self-renewal and multi-lineage differentiation capacity. The origin, unique properties, and therapeutic benefits of MSC are under intensive investigation worldwide. Several challenges with regard to the proper source of clinical-grade MSC and the efficacy of MSC-based treatment strategies need to be addressed before MSC can be routinely used in the clinic. Here, we discuss three areas that can potentially facilitate the translation of MSC into clinic: Generation of MSC-like cells from human pluripotent stem cells, strategies to enhance homing of MSC to injured tissues, and targeting of MSC in vivo.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Mesenchymal stem cells (MSC) are multipotent cells that were first identified by Friedenstein as bone marrow osteogenic stem cells [1]. The term “mesenchymal stem cell” was coined by Caplan to describe a population of cells that are involved in the formation of bone and cartilage during embryonic development, bone turnover, and repair throughout adulthood [2]. However, the term “mesenchymal” is contentious and not generally accepted [3]. Other names also exist for MSC including multipotent mesenchymal stromal cells, skeletal stem cells, adult stromal stem cells, and bone marrow stromal cells [4, 5]. MSC are defined as non-hematopoietic, plastic adherent multipotent stem cells that are present in the bone marrow stroma and can differentiate into cells of mesodermal lineage including osteoblasts, adipocytes, and chondrocytes. In ex vivo culture, MSC are positive for a number of CD markers: CD105, CD106, CD90, CD73, CD140b, CD166 and negative for CD31, CD45, CD34, CD14, CD133 and the major histocompatibility complex (MHC) class II markers [4, 6]. In addition to their presence in bone marrow, MSC-like cell populations have been isolated from the stromal compartment of adipose tissue, umbilical cord, dental pulp, skeletal muscle, synovium, and periodontal ligament [7–13]. While MSC-like cell populations share a common molecular signature with bone marrow MSC, they exhibit differences in their molecular phenotype and differentiation potential characteristic for their tissue of origin [14]. A common in vivo location of MSC in the bone marrow and in other tissues is in a perivascular niche in close association with pericytes and endothelial cells [15].
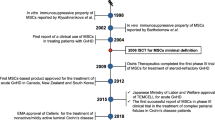
2 Towards Clinical Use
MSC hold a great promise for clinical use in tissue regeneration in a large number of clinical conditions. 379 clinical trials, worldwide, are currently undergoing investigations into the therapeutic benefits of MSC (http://clinicaltrials.gov). These range from enhancing hematopoiesis following hematopoietic stem cell transplantation to enhancing tissue regeneration for cardiomyopathies, nerve tissue, bone and cartilage repair following injury and chronic disease.
Several factors limit the clinical use of MSC [16], including the inability to obtain the large number of MSC required for clinical transplantation due to in vitro replicative senescence [17], heterogeneity of ex vivo cultured MSC with respect to their differentiation capacity, and lack of specific markers that identify MSC prospectively and are predictive of their in vivo phenotype. In the current review, we will discuss progress in studies related to three areas that received a lot of attention due to their possible use to facilitate clinical use of MSC: (1) use of human pluripotent stem cells as a source for generation of an unlimited number of MSC, (2) development of approaches to enhance in vivo migration of MSC into injured tissues, and (3) novel strategies for targeting MSC in vivo with the aim of enhancing bone formation.
3 Generation of MSC-Like Cells from Human Pluripotent Stem Cells
Human pluripotent stem cells (hPSC) are a group of specialized cells that have the unique ability to differentiate into cells of the mesoderm, endoderm, and ectoderm lineages and are thus termed pluripotent. There are two major sources of hPSC: human embryonic stem cells (hESC) and induced pluripotent stem cells (iPSC). hESC are generated through isolation of the inner cell mass (ICM) from a 5- to 6-day-old human blastocyst [18]. Since the derivation of hESC by Thomson in 1998 [18] much effort has been focused to develop protocols for differentiation of hESC into lineage-specific cell types [19]. The creation of induced pluripotent stem cells (iPSC) from adult somatic cells [20–22] has added a new dimension to the field of regenerative medicine by offering the possibility of generating autologous pluripotent stem cells [23]. ESC and iPSC are similar in their expression of the self-renewal markers and ability to differentiate into the three basic cell lineages: ectoderm, endoderm, and mesoderm [20–22, 24, 25]. Pluripotent stem cells offer much promise within the field of regenerative medicine due to their unlimited proliferation ability, scalability, and differentiation capacity.
A number of methods have been reported for derivation of functional MSC-like cells from PSC, using embryoid body formation (EB), monolayer differentiation, coculture, selective isolation of spontaneously differentiated cells, and cultures using biomaterials [23, 26–29].
EB Formation:
Standard methods demonstrate that EBs can be formed spontaneously from small clumps of pluripotent cells that are passaged either mechanically or using enzymatic methods and cultured in suspension using low adhesion plastic vessels. This method allows spontaneous nondirected differentiation or directed differentiation of PSC, through addition of growth factors/morphogens/cytokines. EBs imitate the structure of the early embryo and recapitulate many of the early embryonic developmental events like gastrulation, polarization, and primitive streak formation [26, 30]. However, a disadvantage of the EB method is that it provides heterogeneous populations of MSC-like cells. In an attempt to reduce cellular heterogeneity, a number of alternative approaches have been developed including methods of synchronized growth and differentiation through forced aggregation by centrifugation [31], bioreactor cultures [32], and stirred suspension cultures [33] and recently Son et al. [34] published data demonstrating a simple method using periodic passaging of hEBs to maintain uniformity on size and proliferation whilst preserving their differentiation potential.
Monolayer Differentiation:
2-D PSC cultures have an advantage over EB-based differentiation as it is possible to visualize the progression of ex vivo differentiation. However, this technique fails to recapitulate the gastrulation-like processes apparent in EB formation. Development of MSC-like cells has been obtained by using induction media that allows synchronized differentiation, e.g. adding Rock inhibitor Y27632 [35], by selection by continuous subculture over a number of weeks to select for stromal (MSC-like) cells [36, 37], or by cell sorting based on specific surface markers, e.g., the selection of a CD105+/CD24− cell population [38].
Coculture:
A number of groups have used coculture of hESC with differentiated cells to induce differentiation into an MSC-like phenotype. Barberi et al. employed coculture with murine OP9 cells followed by sorting for CD73+ MSC-like cells [39]. This method of induced differentiation presupposes that secreted factors from the differentiated cells can supply microenvironmental cues necessary for differentiation, but the nature of these factors is not known.
Spontaneous Differentiation:
Spontaneous differentiation into MSC-like cells often occurs at the edges of the hPSC colonies, obtained when hPSC are cultured in a feeder-free system. In the “raclure” method, the cells at the edges of the colonies are manually scrapped [40, 41], or cells can be enriched through adherence to selective extracellular matrix components such as hyaluronic acid (HA)-coated plates [28], or through forced differentiation through overgrowth of cultures [42]. In our laboratory, we found that selection of MSC-like cells based on selective adherence to HA-coated culture plates resulted in obtaining a morphologically homogeneous cell population with a similar phenotype to bone marrow-derived MSC [28]. In addition, Liu et al. demonstrated that hESC and iPSC differentiated into MSC-like cells through plating of single cells on a fibrillar type 1 collagen matrix [29].
The MSC-like cells derived from hESC or iPSC using the above-mentioned approaches exhibit a phenotypic profile comparable to MSC as defined by CD markers and differentiation ability into one or more of the osteoblastic, chondrocytic, or adipocytic lineages. While most of the reported differentiation capacities are based on in vitro data, a number of groups have demonstrated the ability of hPSC-derived MSC-like cells to form bone in vivo following osteogenic induction ex vivo or through direct implantation of the cells in osteoinductive scaffolds [28, 43, 44].
4 Concerns of Using hPSC-Derived MSC-Like Cells in Cellular Therapy
For clinical use, hPSC-derived MSC-like cells should be obtained from GMP (good manufacture practice) compliant hPSC lines. There have been an increasing number of reported hESC lines [45–48] and iPSC lines [49] derived under GMP standards. Additionally, clinical-grade derivation protocols for MSC-like cells have been reported [50]. The necessity for extensive ex vivo culture, which would be required for clinical therapy, has raised concerns about the possibility of genetic changes and the development of a transformed phenotype. A number of reports have highlighted the issue of karyotypic stability during routine maintenance of hESC cultured ex vivo where gains in chromosomes 12, 17, and X have been reported [51–55]. Of additional concern is the unintentional transplantation of undifferentiated hPSC in conjunction with their differentiated progeny that may lead to teratoma formation upon transplantation. As the purity of hPSC differentiated cultures is variable, attempts are being made to deplete undifferentiated hPSC within the cultures either by using cytotoxic agents, mechanically removing undifferentiated cells [56, 57], or separating out undifferentiated cells using fluorescent tags which identify undifferentiated cells [58, 59]. Thus, before hPSC-derived MSC are considered for cellular therapy safety criteria are needed to be instituted [60, 61].
MSC-like cells derived from iPS cells should be compatible with their recipient and thus will not elicit an immunological rejection reaction. Interestingly, differentiated cells derived from hESC may be hypoimmunegenic. Drukker et al. [62] demonstrated absence of the MHC class II molecules and the presence of low levels of class I molecules in hESC. Additionally, normal irradiated mice transplanted with bone marrow from immune compromised (SCID) mice were transfused with human peripheral blood mononuclear cells to test the possible immunological reaction or rejection of transplanted hESC. Over the course of a month, transplanted hESC did not demonstrate significant rejection [62]. More recently Araki et al. demonstrated limited or no immune response in differentiated mouse ESC and iPSC [63].
It is envisaged that off-the-shelf MSC-like cells should be available in stem cell banks that contain hPSC lines that cover the majority of the Western European population tissue types. It has been estimate that 150 hESC cell lines in Europe [64] and 170 cell lines for the Japanese population [65] would be needed to obtain an acceptable degree of HLA matching which would only require a minimum of immune suppressor therapy.
iPSC were initially derived using a combination of four transcription factors (OCT4, SOX2, KLF4, and cMyc) to reprogram the somatic cells to their pluripotent status [20]. Whilst the success of reprogramming was a huge step forward towards generation of cells for therapy, standard methods used to generate iPSC may result in cells not suitable for therapy due to the use of viral vectors. New strategies are being developed to overcome these concerns using plasmids [66], recombinant proteins [67], or RNA molecules [68, 69].
5 Directing MSC to Injured Tissues
Current thinking vis-a-vis the clinical use of MSC in therapy is modeled on the hematopoietic stem cell transplantation model where HSC are infused intravenously and consequently home to the bone marrow where they establish hematopoiesis [70]. Although homing of MSC to sites of injury and their involvement in healing and/or regeneration of defected tissues is a natural repair mechanism, it was observed that this endogenous ability can be further enhanced by exogenously administered MSC [71, 72]. Systemic infusion of MSC for treatment of tissue injury represents a more attractive procedure for clinical applications. In addition, studies on MSC migration to injured tissues have been shaped by concepts related to leukocyte recruitment from the circulation to inflammation sites, through a coordinated multistep biological process termed “cell homing” that includes infused cell rolling/adhering onto sinusoidal endothelial cells followed by their firm adhesion preventing their back movement to circulation, resulting in transmigration to their destined tissues [73]. Employing this model for MSC has been supported by evidence for the presence of osteoprogenitors or MSC-like cells in the circulation that can home to bone marrow or inflammatory sites [74].
Following injury, damaged cells secrete a number of chemokines that act as attractants to cells participating in tissue repair [75]. However, one of the major challenges facing MSC-based cell therapy is the observed low and inefficient homing of systemically infused MSC to non-injured tissues [76]. Several groups have demonstrated successful but limited homing after systemic delivery to ischemic, irradiated, or otherwise injured skeletal tissues in which only a small fraction of transplanted MSC can be found in the target tissue [77–79].
5.1 Novel Approaches to Enhance Homing of MSC into Injured Tissues
It is well known that adhesion and integrin molecules are important key players in determining the potential of cellular homing [80]. For example, the CD44 antigen is a cell surface glycoprotein involved in cell adhesion and migration [81]. A specialized glycoform of CD44 called hematopoietic cell E-/L-selectin ligand (HCELL) is an E-selectin ligand expressed on human cells [82]. Using real-time confocal microscopy cell trafficking was monitored in immune-compromised mouse calvaria. These results indicated that overexpression of HCELL E-selectin on MSC caused, within hours, enhanced osteotropic migration to the bone marrow [83]. Recently, modification of MSC cell surface integrins to enhance homing of MSC to bone surfaces was achieved by attaching a synthetic ligand (LLP2A) against integrin α4β1 on the MSC surface to a bisphosphonate (alendronate, Ale). Upon administration in in vivo animal models the LLP2A-ALE-modified MSC showed enhanced homing to bone surfaces with improved bone formation at the endo-cortical, trabecular, and periosteal surfaces when compared to non-modified MSC [84]. In another study, cell adhesion molecules were chemically attached to the cell surface to improve rolling efficiency of MSC. This chemical approach involved introduction of biotin groups to the cell surface by treatment with sulfonated biotinyl-N-hydroxy-succinimide, the addition of streptavidin, and attachment of a biotinylated cell rolling ligand (sialyl Lewisx (SLeX)) found on the surface of leukocytes [85]. This approach can be used to potentially target P-selectin expressing endothelium in the bone marrow or at sites of inflammation [86].
Another hypothesized explanation for the poor homing capacity of MSC is their inadequate expression of homing-associated chemokines. For example, CXCR4, a homing signaling molecule known for its interaction with its cognate ligand Stromal cell-derived factor-1 (SDF-1α), is expressed at low levels on the MSC cell surface [87, 88]. In a number of in vivo studies, homing of transplanted MSC to tumors [89], myocardium [90], and bone marrow [78] has been improved by overexpression of CXCR4 on the MSC surface. For example, MSC overexpressing CXCR4 were infused intravenously 24 h after coronary occlusion in a rat model of AMI and were found to home to the infarcted myocardium resulting in better recovery of left ventricular function as compared to rats infused with control (low CXCR4 expressing) cells [87]. In another study, C3H10T1/2 cells, a multipotent mouse stem cell line, overexpressing CXCR4 were injected intravenously in immune-competent glucocorticoid-induced osteoporotic mice. These cells had enhanced homing efficiency to the bone marrow and increased bone mass in the osteoporotic mice [79]. Another member of the chemokine family is the C-C chemokine receptor type 1 (CCR1), known to be involved in the recruitment of immune cells to sites of inflammation, e.g., injured myocardium [91]. Mouse bone marrow MSC, overexpressing CCR1, were injected intra-myocardially in a mouse model of AMI. One hour post coronary artery ligation, MSC overexpressing CCR1 had accumulated in the infarcted myocardium at significantly higher levels than control MSC. This led to significant reduction in infarct size, reduced cardio-myocyte apoptosis, increased capillary density, and restoration of cardiac function via enhancement of transplanted cells’ viability and engraftment [92].
All these studies demonstrate work in progress towards developing a clinically relevant protocol for intravenous infusion of the MSC to patients in need of enhanced tissue regeneration.
6 Targeting of MSC In Vivo
Therapeutic strategies that employ ex vivo cultured cells are associated with some limitations such as the need for substantial number of cells requiring extensive ex vivo cell expansion, the need for GMP facilities, as well as development of robust methods for differentiation induction [16]. Targeting of the endogenous MSC populations, using small molecules, small-interfering RNA (siRNA), or MicroRNA (miRNA), is an attractive alternative and is suitable for treatment of diseases where the mature cell populations, which are to be targeted by the drug, are depleted or do not respond to standard treatment. An example of such a clinical setting is the use of osteoblast-targeting anabolic therapies for treatment of bone loss, in which osteoblasts are decreased in number and activity [93].
Small molecules are very attractive agents to be used in clinical applications, due to the opportunity of fine-tuning their chemical structure using traditional chemistry techniques, high stability, adaptability to large-scale production leading to substantial reduction of the treatment costs, and a potential for oral delivery [39, 94, 95]. Some examples of these approaches have been recently reported.
Bortezomib (Bzb) is a small molecule proteasome inhibitor that is used in the clinic for treatment of multiple myeloma [96]. It has been shown that Bzb targets bone marrow MSC in vivo and induces their differentiation toward the osteoblastic lineage through regulation of runt-related transcription factor 2 (Runx2), known as a master regulator of osteogenesis [97, 98]. Intraperitoneal (i.p.) administration of Bzb to mice for 3 weeks increased bone mass, trabecular bone connectivity, trabecular number, serum osteocalcin, as well as bone formation rate demonstrating enhanced in vivo osteoblastic bone formation activity. Moreover, it was shown that in contrast to MSC, osteoprogenitors and osteoclasts did not respond to Bzb treatment [98].
siRNA can specifically silence the synthesis of any desired protein by base paring to its mRNA sequence [99]. To date, more than 20 siRNA-based drugs are under clinical investigation for treatment of a variety of conditions including solid tumors, acute kidney injury, age-related macular degeneration (AMD), diabetic macular edema, hepatitis C, AIDS-associated lymphoma, and respiratory syncytial virus infection [100]. Administration of siRNA and silencing the synthesis of a gene of interest can be used to alter the differentiation fate of MSC in vivo [101]. However, the large therapeutic doses of systematically administered siRNA that is needed to exert the desired clinical outcome may lead to activation of immune response, as well as adverse effects on other tissues. Thus, the development of novel systems that deliver siRNA specifically to the cell population of interest is highly desirable. Recently, a novel targeting system has been developed that delivers siRNA to the bone-forming surfaces enriched for MSC and osteoprogenitors [102]. This system involves dioleoyl trimethylammonium propane (DOTAP)-based cationic liposomes attached to six repetitive sequences of aspartate, serine, serine ((AspSerSer)6). This system has been used for in vivo systemic delivery of siRNA targeting Plekho1 (a negative regulator of bone formation) in rats and led to significant enhancement of bone formation, enhanced the bone micro-architecture, and increased the bone mass in both healthy and osteoporotic rats [102]. In addition to siRNA, miRNAs have potential use in therapy. miRNAs are endogenous, short, noncoding RNAs that regulate diverse biological processes mostly through translational repression of their target genes [103]. miRNAs can be employed to modulate the differentiation fate of MSC in vitro and in vivo [103]. Exogenous supplementation or ectopic expression of miRNAs as well as using anti-miRs to antagonize the effect of miRNAs are promising strategies to be employed for treatment of different clinical conditions [104]. In our group, we have demonstrated that miR-138 negatively regulates in vitro osteoblast differentiation and in vivo bone formation of MSC, by targeting focal adhesion kinase (FAK), a kinase playing a central role in promoting osteoblast differentiation [105]. Using a preclinical in vivo bone formation model, we showed that pharmacological inhibition of miR-138 by antimiR-138 increased ectopic bone formation and thus it is possible to develop antimiR-138 into a novel strategy for treatment of bone loss conditions [105].
7 Conclusions and Future Perspectives
Regenerative medicine holds promise to restore normal tissue functions in the body using stem cell transplantation or ex vivo grown tissues and organs generated through a combination of stem cells and biomaterials, i.e., tissue engineering approaches. The transition from the laboratory to the clinic has proven to be difficult and currently there is no standard stem cell-based therapy for non-cancer indications. Conversely, a large number of clinical trials testing the ability of different types of stem cells including MSC in a number of disease conditions are being conducted and include conditions such as nonunion fractures, ulcerative colitis, type 1 diabetes mellitus, liver cirrhosis, idiopathic dilated cardiomyopathy, multiple sclerosis, spinal cord injury, acute and chronic graft-versus-host disease, middle cerebral artery infarct, osteoarthritis, relapsed/refractory severe acquired aplastic anemia, chronic critical limb ischemia, Parkinson’s disease, acute myocardial infarction, hematological malignancies, Crohn’s disease, acute leukemia, lupus nephritis, and non-healing wounds (please see: http://clinicaltrials.gov). It is hoped that these trials will establish the efficacy of stem cells and MSC in therapy and their place among other current treatment modalities.
Abbreviations
- AMD:
-
Age-related macular degeneration
- AMI:
-
Acute myocardial infarction
- Bzb:
-
Bortezomib
- CCR1:
-
C-C Chemokine receptor type 1
- CXCR4:
-
C-X-C Chemokine receptor type 4
- EB:
-
Embryoid body
- FAK:
-
Focal adhesion kinase
- GMP:
-
Good manufacturing practice
- hESC:
-
Human embryonic stem cells
- HLA:
-
Human leukocyte antigen
- hPSC:
-
Human pluripotent stem cells
- ICM:
-
Inner cell mass
- iPSC:
-
Induced pluripotent stem cells
- MHC:
-
Major histocompatibility complex
- miRNA:
-
MicroRNA
- MSC:
-
Mesenchymal stem cells
- Runx2:
-
Runt-related transcription factor 2
- SCID:
-
Severe combined immunodeficiency
- SDF-1α:
-
Stromal cell-derived factor-1
- siRNA:
-
Small-interfering RNA
References
Friedenstein AJ, Chailakhyan RK, Gerasimov UV (1987) Bone marrow osteogenic stem cells: in vitro cultivation and transplantation in diffusion chambers. Cell Tissue Kinet 20(3):263–272
Caplan AI (1991) Mesenchymal stem cells. J Orthop Res 9(5):641–650
Bianco P, Cao X, Frenette PS, Mao JJ, Robey PG, Simmons PJ et al (2013) The meaning, the sense and the significance: translating the science of mesenchymal stem cells into medicine. Nat Med 19(1):35–42
Garcia-Gomez I, Elvira G, Zapata AG, Lamana ML, Ramirez M, Castro JG et al (2010) Mesenchymal stem cells: biological properties and clinical applications. Expert Opin Biol Ther 10(10):1453–1468
Bianco P, Robey PG, Simmons PJ (2008) Mesenchymal stem cells: revisiting history, concepts, and assays. Cell Stem Cell 2(4):313–319
Sivasubramaniyan K, Lehnen D, Ghazanfari R, Sobiesiak M, Harichandan A, Mortha E et al (2012) Phenotypic and functional heterogeneity of human bone marrow- and amnion-derived MSC subsets. Ann N Y Acad Sci 1266:94–106
Akiyama K, Chen C, Gronthos S, Shi S (2012) Lineage differentiation of mesenchymal stem cells from dental pulp, apical papilla, and periodontal ligament. Methods Mol Biol 887:111–121
Asakura A, Komaki M, Rudnicki M (2001) Muscle satellite cells are multipotential stem cells that exhibit myogenic, osteogenic, and adipogenic differentiation. Differentiation 68(4–5):245–253
De Bari C, Dell’Accio F, Tylzanowski P, Luyten FP (2001) Multipotent mesenchymal stem cells from adult human synovial membrane. Arthritis Rheum 44(8):1928–1942
Seo BM, Miura M, Gronthos S, Bartold PM, Batouli S, Brahim J et al (2004) Investigation of multipotent postnatal stem cells from human periodontal ligament. Lancet 364(9429):149–155
Bianco P, Riminucci M, Gronthos S, Robey PG (2001) Bone marrow stromal stem cells: nature, biology, and potential applications. Stem Cells 19(3):180–192
Zuk PA, Zhu M, Mizuno H, Huang J, Futrell JW, Katz AJ et al (2001) Multilineage cells from human adipose tissue: implications for cell-based therapies. Tissue Eng 7(2):211–228
Kermani AJ, Fathi F, Mowla SJ (2008) Characterization and genetic manipulation of human umbilical cord vein mesenchymal stem cells: potential application in cell-based gene therapy. Rejuvenation Res 11(2):379–386
Al-Nbaheen M, Vishnubalaji R, Ali D, Bouslimi A, Al-Jassir F, Megges M et al (2013) Human stromal (mesenchymal) stem cells from bone marrow, adipose tissue and skin exhibit differences in molecular phenotype and differentiation potential. Stem Cell Rev 9(1):32–43
Crisan M, Yap S, Casteilla L, Chen CW, Corselli M, Park TS et al (2008) A perivascular origin for mesenchymal stem cells in multiple human organs. Cell Stem Cell 3(3):301–313
Aldahmash A, Zaher W, Al-Nbaheen M, Kassem M (2012) Human stromal (mesenchymal) stem cells: basic biology and current clinical use for tissue regeneration. Ann Saudi Med 32(1):68–77
Stenderup K, Justesen J, Clausen C, Kassem M (2003) Aging is associated with decreased maximal life span and accelerated senescence of bone marrow stromal cells. Bone 33(6):919–926
Thomson JA, Itskovitz-Eldor J, Shapiro SS, Waknitz MA, Swiergiel JJ, Marshall VS et al (1998) Embryonic stem cell lines derived from human blastocysts. Science 282(5391):1145–1147
Odorico JS, Kaufman DS, Thomson JA (2001) Multilineage differentiation from human embryonic stem cell lines. Stem Cells 19(3):193–204
Takahashi K, Tanabe K, Ohnuki M, Narita M, Ichisaka T, Tomoda K et al (2007) Induction of pluripotent stem cells from adult human fibroblasts by defined factors. Cell 131(5):861–872
Wernig M, Meissner A, Foreman R, Brambrink T, Ku M, Hochedlinger K et al (2007) In vitro reprogramming of fibroblasts into a pluripotent ES-cell-like state. Nature 448(7151):318–324
Yu J, Vodyanik MA, Smuga-Otto K, Antosiewicz-Bourget J, Frane JL, Tian S et al (2007) Induced pluripotent stem cell lines derived from human somatic cells. Science 318(5858):1917–1920
Lian Q, Zhang Y, Zhang J, Zhang HK, Wu X, Lam FF et al (2010) Functional mesenchymal stem cells derived from human induced pluripotent stem cells attenuate limb ischemia in mice. Circulation 121(9):1113–1123
Park IH, Zhao R, West JA, Yabuuchi A, Huo H, Ince TA et al (2008) Reprogramming of human somatic cells to pluripotency with defined factors. Nature 451(7175):141–146
Zhao XY, Li W, Lv Z, Liu L, Tong M, Hai T et al (2009) iPS cells produce viable mice through tetraploid complementation. Nature 461(7260):86–90
Mahmood A, Harkness L, Abdallah BM, Elsafadi M, Al-Nbaheen MS, Aldahmash A et al (2012) Derivation of stromal (skeletal and mesenchymal) stem-like cells from human embryonic stem cells. Stem Cells Dev 21(17):3114–3124
Inanc B, Elcin AE, Elcin YM (2007) Effect of osteogenic induction on the in vitro differentiation of human embryonic stem cells cocultured with periodontal ligament fibroblasts. Artif Organs 31(11):792–800
Harkness L, Mahmood A, Ditzel N, Abdallah BM, Nygaard JV, Kassem M (2011) Selective isolation and differentiation of a stromal population of human embryonic stem cells with osteogenic potential. Bone 48(2):231–241
Liu Y, Goldberg AJ, Dennis JE, Gronowicz GA, Kuhn LT (2012) One-step derivation of mesenchymal stem cell (MSC)-like cells from human pluripotent stem cells on a fibrillar collagen coating. PLoS One 7(3):e33225
ten Berge D, Koole W, Fuerer C, Fish M, Eroglu E, Nusse R (2008) Wnt signaling mediates self-organization and axis formation in embryoid bodies. Cell Stem Cell 3(5):508–518
Ng ES, Davis RP, Azzola L, Stanley EG, Elefanty AG (2005) Forced aggregation of defined numbers of human embryonic stem cells into embryoid bodies fosters robust, reproducible hematopoietic differentiation. Blood 106(5):1601–1603
Yirme G, Amit M, Laevsky I, Osenberg S, Itskovitz-Eldor J (2008) Establishing a dynamic process for the formation, propagation, and differentiation of human embryoid bodies. Stem Cells Dev 17(6):1227–1242
Abbasalizadeh S, Larijani MR, Samadian A, Baharvand H (2012) Bioprocess development for mass production of size-controlled human pluripotent stem cell aggregates in stirred suspension bioreactor. Tissue Eng Part C Methods 18(11):831–851
Son MY, Kim HJ, Kim MJ, Cho YS (2011) Physical passaging of embryoid bodies generated from human pluripotent stem cells. PLoS One 6(5):e19134
Wu R, Gu B, Zhao X, Tan Z, Chen L, Zhu J et al (2013) Derivation of multipotent nestin+/CD271-/STRO-1- mesenchymal-like precursors from human embryonic stem cells in chemically defined conditions. Hum Cell 26(1):19–27
Arpornmaeklong P, Brown SE, Wang Z, Krebsbach PH (2009) Phenotypic characterization, osteoblastic differentiation, and bone regeneration capacity of human embryonic stem cell-derived mesenchymal stem cells. Stem Cells Dev 18(7):955–968
Karlsson C, Emanuelsson K, Wessberg F, Kajic K, Axell MZ, Eriksson PS et al (2009) Human embryonic stem cell-derived mesenchymal progenitors – potential in regenerative medicine. Stem Cell Res 3(1):39–50
Lian Q, Lye E, Suan Yeo K, Khia Way Tan E, Salto-Tellez M, Liu TM et al (2007) Derivation of clinically compliant MSCs from CD105+, CD24- differentiated human ESCs. Stem Cells 25(2):425–436
Aravamudhan A, Ramos DM, Nip J, Subramanian A, James R, Harmon MD et al (2013) Osteoinductive small molecules: growth factor alternatives for bone tissue engineering. Curr Pharm Des 19(19):3420–3428
Olivier EN, Rybicki AC, Bouhassira EE (2006) Differentiation of human embryonic stem cells into bipotent mesenchymal stem cells. Stem Cells 24(8):1914–1922
Olivier E, Bouhassira E (2011) Differentiation of human embryonic stem cells into mesenchymal stem cells by the raclure method. In: Nieden NI (ed) Embryonic stem cell therapy for osteo-degenerative diseases. Humana, New York, pp 183–193
Trivedi P, Hematti P (2008) Derivation and immunological characterization of mesenchymal stromal cells from human embryonic stem cells. Exp Hematol 36(3):350–359
Mahmood A, Harkness L, Schroder HD, Abdallah BM, Kassem M (2010) Enhanced differentiation of human embryonic stem cells to mesenchymal progenitors by inhibition of TGFb/activin/nodal signaling using SB-431542. J Bone Miner Res 25(6):1216–1233
Tremoleda JL, Forsyth NR, Khan NS, Wojtacha D, Christodoulou I, Tye BJ et al (2008) Bone tissue formation from human embryonic stem cells in vivo. Cloning Stem Cells 10(1):119–132
Crook JM, Peura TT, Kravets L, Bosman AG, Buzzard JJ, Horne R et al (2007) The generation of six clinical-grade human embryonic stem cell lines. Cell Stem Cell 1(5):490–494
Sidhu KS, Walke S, Tuch, BE (2008) Derivation and Propagation of hESC Under a Therapeutic Environment. Current Protocols in Stem Cell Biology 6:1A.4.1–1A.4.31
Skottman H, Dilber MS, Hovatta O (2006) The derivation of clinical-grade human embryonic stem cell lines. FEBS Lett 580(12):2875–2878
Unger C, Skottman H, Blomberg P, Sirac Dilber M, Hovatta O (2008) Good manufacturing practice and clinical-grade human embryonic stem cell lines. Hum Mol Genet 17(R1):R48–R53
Ohmine S, Dietz A, Deeds M, Hartjes K, Miller D, Thatava T et al (2011) Induced pluripotent stem cells from GMP-grade hematopoietic progenitor cells and mononuclear myeloid cells. Stem Cell Res Ther 2(6):46
Han G, Jing Y, Zhang Y, Yue Z, Hu X, Wang L et al (2010) Osteogenic differentiation of bone marrow mesenchymal stem cells by adenovirus-mediated expression of leptin. Regul Pept 163(1–3):107–112
Draper JS, Smith K, Gokhale P, Moore HD, Maltby E, Johnson J et al (2004) Recurrent gain of chromosomes 17q and 12 in cultured human embryonic stem cells. Nat Biotechnol 22(1):53–54
Maitra A, Arking DE, Shivapurkar N, Ikeda M, Stastny V, Kassauei K et al (2005) Genomic alterations in cultured human embryonic stem cells. Nat Genet 37(10):1099–1103
Mitalipova MM, Rao RR, Hoyer DM, Johnson JA, Meisner LF, Jones KL et al (2005) Preserving the genetic integrity of human embryonic stem cells. Nat Biotechnol 23(1):19–20
Pera MF (2004) Unnatural selection of cultured human ES cells? Nat Biotechnol 22(1):42–43
Spits C, Mateizel I, Geens M, Mertzanidou A, Staessen C, Vandeskelde Y et al (2008) Recurrent chromosomal abnormalities in human embryonic stem cells. Nat Biotechnol 26(12):1361–1363
Bieberich E, Silva J, Wang G, Krishnamurthy K, Condie BG (2004) Selective apoptosis of pluripotent mouse and human stem cells by novel ceramide analogues prevents teratoma formation and enriches for neural precursors in ES cell-derived neural transplants. J Cell Biol 167(4):723–734
Schriebl K, Satianegara G, Hwang A, Tan HL, Fong WJ, Yang HH et al (2012) Selective removal of undifferentiated human embryonic stem cells using magnetic activated cell sorting followed by a cytotoxic antibody. Tissue Eng Part A 18(9–10):899–909
Tang C, Lee AS, Volkmer JP, Sahoo D, Nag D, Mosley AR et al (2011) An antibody against SSEA-5 glycan on human pluripotent stem cells enables removal of teratoma-forming cells. Nat Biotechnol 29(9):829–834
Wang YC, Nakagawa M, Garitaonandia I, Slavin I, Altun G, Lacharite RM et al (2011) Specific lectin biomarkers for isolation of human pluripotent stem cells identified through array-based glycomic analysis. Cell Res 21(11):1551–1563
Fong CY, Gauthaman K, Bongso A (2010) Teratomas from pluripotent stem cells: a clinical hurdle. J Cell Biochem 111(4):769–781
Knoepfler PS (2009) Deconstructing stem cell tumorigenicity: a roadmap to safe regenerative medicine. Stem Cells 27(5):1050–1056
Drukker M (2008) Immunological considerations for cell therapy using human embryonic stem cell derivatives. In: StemBook [Internet]. Cambridge (MA): Harvard Stem Cell Institute. Available from: http://www.ncbi.nlm.nih.gov/books/NBK27031/
Araki R, Uda M, Hoki Y, Sunayama M, Nakamura M, Ando S et al (2013) Negligible immunogenicity of terminally differentiated cells derived from induced pluripotent or embryonic stem cells. Nature 494(7435):100–104
Taylor CJ, Bolton EM, Pocock S, Sharples LD, Pedersen RA, Bradley JA (2005) Banking on human embryonic stem cells: estimating the number of donor cell lines needed for HLA matching. Lancet 366(9502):2019–2025
Isomoto S, Hattori K, Ohgushi H, Nakajima H, Tanaka Y, Takakura Y (2007) Rapamycin as an inhibitor of osteogenic differentiation in bone marrow-derived mesenchymal stem cells. J Orthop Sci 12(1):83–88
Okita K, Nakagawa M, Hyenjong H, Ichisaka T, Yamanaka S (2008) Generation of mouse induced pluripotent stem cells without viral vectors. Science 322(5903):949–953
Lin T, Ambasudhan R, Yuan X, Li W, Hilcove S, Abujarour R et al (2009) A chemical platform for improved induction of human iPSCs. Nat Methods 6(11):805–808
Anokye-Danso F, Trivedi CM, Juhr D, Gupta M, Cui Z, Tian Y et al (2011) Highly efficient miRNA-mediated reprogramming of mouse and human somatic cells to pluripotency. Cell Stem Cell 8(4):376–388
Judson RL, Babiarz JE, Venere M, Blelloch R (2009) Embryonic stem cell-specific microRNAs promote induced pluripotency. Nat Biotechnol 27(5):459–461
Magnon C, Frenette PS (2008) Hematopoietic stem cell trafficking. StemBook. Cambridge, MA
Grauss RW, Winter EM, van Tuyn J, Pijnappels DA, Steijn RV, Hogers B et al (2007) Mesenchymal stem cells from ischemic heart disease patients improve left ventricular function after acute myocardial infarction. Am J Physiol Heart Circ Physiol 293(4):H2438–H2447
Chapel A, Bertho JM, Bensidhoum M, Fouillard L, Young RG, Frick J et al (2003) Mesenchymal stem cells home to injured tissues when co-infused with hematopoietic cells to treat a radiation-induced multi-organ failure syndrome. J Gene Med 5(12):1028–1038
Lawrence MB, Springer TA (1991) Leukocytes roll on a selectin at physiologic flow rates: distinction from and prerequisite for adhesion through integrins. Cell 65(5):859–873
Pignolo RJ, Kassem M (2011) Circulating osteogenic cells: implications for injury, repair, and regeneration. J Bone Miner Res 26(8):1685–1693
Wu Y, Zhao RC (2012) The role of chemokines in mesenchymal stem cell homing to myocardium. Stem Cell Rev 8(1):243–250
Bentzon JF, Stenderup K, Hansen FD, Schroder HD, Abdallah BM, Jensen TG et al (2005) Tissue distribution and engraftment of human mesenchymal stem cells immortalized by human telomerase reverse transcriptase gene. Biochem Biophys Res Commun 330(3):633–640
Bobis-Wozowicz S, Miekus K, Wybieralska E, Jarocha D, Zawisz A, Madeja Z et al (2011) Genetically modified adipose tissue-derived mesenchymal stem cells overexpressing CXCR4 display increased motility, invasiveness, and homing to bone marrow of NOD/SCID mice. Exp Hematol 39(6):686–696
Devine MJ, Mierisch CM, Jang E, Anderson PC, Balian G (2002) Transplanted bone marrow cells localize to fracture callus in a mouse model. J Orthop Res 20(6):1232–1239
Lien CY, Chih-Yuan HK, Lee OK, Blunn GW, Su Y (2009) Restoration of bone mass and strength in glucocorticoid-treated mice by systemic transplantation of CXCR4 and cbfa-1 co-expressing mesenchymal stem cells. J Bone Miner Res 24(5):837–848
Frenette PS, Subbarao S, Mazo IB, von Andrian UH, Wagner DD (1998) Endothelial selectins and vascular cell adhesion molecule-1 promote hematopoietic progenitor homing to bone marrow. Proc Natl Acad Sci U S A 95(24):14423–14428
Zhu H, Mitsuhashi N, Klein A, Barsky LW, Weinberg K, Barr ML et al (2006) The role of the hyaluronan receptor CD44 in mesenchymal stem cell migration in the extracellular matrix. Stem Cells 24(4):928–935
Sackstein R (2012) Glycoengineering of HCELL, the human bone marrow homing receptor: sweetly programming cell migration. Ann Biomed Eng 40(4):766–776
Sackstein R, Merzaban JS, Cain DW, Dagia NM, Spencer JA, Lin CP et al (2008) Ex vivo glycan engineering of CD44 programs human multipotent mesenchymal stromal cell trafficking to bone. Nat Med 14(2):181–187
Guan M, Yao W, Liu R, Lam KS, Nolta J, Jia J et al (2012) Directing mesenchymal stem cells to bone to augment bone formation and increase bone mass. Nat Med 18(3):456–462
Sarkar D, Vemula PK, Teo GS, Spelke D, Karnik R, Wee lY et al (2008) Chemical engineering of mesenchymal stem cells to induce a cell rolling response. Bioconjug Chem 19(11):2105–2109
Sarkar D, Zhao W, Gupta A, Loh WL, Karnik R, Karp JM (2011) Cell surface engineering of mesenchymal stem cells. Methods Mol Biol 698:505–523
Cheng Z, Ou L, Zhou X, Li F, Jia X, Zhang Y et al (2008) Targeted migration of mesenchymal stem cells modified with CXCR4 gene to infarcted myocardium improves cardiac performance. Mol Ther 16(3):571–579
Wynn RF, Hart CA, Corradi-Perini C, O’Neill L, Evans CA, Wraith JE et al (2004) A small proportion of mesenchymal stem cells strongly expresses functionally active CXCR4 receptor capable of promoting migration to bone marrow. Blood 104(9):2643–2645
Song C, Li G (2011) CXCR4 and matrix metalloproteinase-2 are involved in mesenchymal stromal cell homing and engraftment to tumors. Cytotherapy 13(5):549–561
Zhang D, Fan GC, Zhou X, Zhao T, Pasha Z, Xu M et al (2008) Over-expression of CXCR4 on mesenchymal stem cells augments myoangiogenesis in the infarcted myocardium. J Mol Cell Cardiol 44(2):281–292
Hodgkinson CP, Gomez JA, Mirotsou M, Dzau VJ (2010) Genetic engineering of mesenchymal stem cells and its application in human disease therapy. Hum Gene Ther 21(11):1513–1526
Huang J, Zhang Z, Guo J, Ni A, Deb A, Zhang L et al (2010) Genetic modification of mesenchymal stem cells overexpressing CCR1 increases cell viability, migration, engraftment, and capillary density in the injured myocardium. Circ Res 106(11):1753–1762
Kassem M, Marie PJ (2011) Senescence-associated intrinsic mechanisms of osteoblast dysfunctions. Aging Cell 10(2):191–197
Sachsenmaier C (2001) Targeting protein kinases for tumor therapy. Onkologie 24(4):346–355
Via MC (2011) Kinase-targeted therapeutics: development pipelines, challenges, and opportunities, August. http://www.insightpharmareports.com/Kinase-Targeted-Therapeutics-Report.aspx
Field-Smith A, Morgan GJ, Davies FE (2006) Bortezomib (Velcadetrade mark) in the treatment of multiple myeloma. Ther Clin Risk Manag 2(3):271–279
Lee B, Thirunavukkarasu K, Zhou L, Pastore L, Baldini A, Hecht J et al (1997) Missense mutations abolishing DNA binding of the osteoblast-specific transcription factor OSF2/CBFA1 in cleidocranial dysplasia. Nat Genet 16(3):307–310
Mukherjee S, Raje N, Schoonmaker JA, Liu JC, Hideshima T, Wein MN et al (2008) Pharmacologic targeting of a stem/progenitor population in vivo is associated with enhanced bone regeneration in mice. J Clin Invest 118(2):491–504
Andersen MO, Nygaard JV, Burns JS, Raarup MK, Nyengaard JR, Bunger C et al (2010) siRNA nanoparticle functionalization of nanostructured scaffolds enables controlled multilineage differentiation of stem cells. Mol Ther 18(11):2018–2027
Burnett JC, Rossi JJ, Tiemann K (2011) Current progress of siRNA/shRNA therapeutics in clinical trials. Biotechnol J 6(9):1130–1146
Takayama K, Suzuki A, Manaka T, Taguchi S, Hashimoto Y, Imai Y et al (2009) RNA interference for noggin enhances the biological activity of bone morphogenetic proteins in vivo and in vitro. J Bone Miner Metab 27(4):402–411
Zhang G, Guo B, Wu H, Tang T, Zhang BT, Zheng L et al (2012) A delivery system targeting bone formation surfaces to facilitate RNAi-based anabolic therapy. Nat Med 18(2):307–314
Taipaleenmaki H, Bjerre Hokland L, Chen L, Kauppinen S, Kassem M (2012) Mechanisms in endocrinology: micro-RNAs: targets for enhancing osteoblast differentiation and bone formation. Eur J Endocrinol 166(3):359–371
Lares MR, Rossi JJ, Ouellet DL (2010) RNAi and small interfering RNAs in human disease therapeutic applications. Trends Biotechnol 28(11):570–579
Eskildsen T, Taipaleenmaki H, Stenvang J, Abdallah BM, Ditzel N, Nossent AY et al (2011) MicroRNA-138 regulates osteogenic differentiation of human stromal (mesenchymal) stem cells in vivo. Proc Natl Acad Sci U S A 108(15):6139–6144
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
Jafari, A., Harkness, L., Zaher, W., Kassem, M. (2014). Adult Stromal (Skeletal, Mesenchymal) Stem Cells: Advances Towards Clinical Applications. In: Turksen, K. (eds) Adult Stem Cells. Stem Cell Biology and Regenerative Medicine. Humana Press, New York, NY. https://doi.org/10.1007/978-1-4614-9569-7_15
Download citation
DOI: https://doi.org/10.1007/978-1-4614-9569-7_15
Published:
Publisher Name: Humana Press, New York, NY
Print ISBN: 978-1-4614-9568-0
Online ISBN: 978-1-4614-9569-7
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)