Abstract
Continuous innovation is one of the pharmaceutical industry’s most defining characteristics. New medications can be crucial for maintaining the quality of human life, and may even affect its duration. The sales potential is staggering: the global pharmaceutical market is expected to reach $1.1 trillion by 2015. The pressure to succeed is tremendous. Yet, pharmaceutical innovation is hardly an orderly, predictable process. It follows a technology-push model dependent on a meandering path of scientific breakthroughs with uneven timing and hard to foresee outcomes. Technological competency, decades of rigorous research, and profound understanding of unmet customer needs, while necessary, may prove insufficient for market success as the critical decision for commercialization remains outside the firm.
Drug innovation as a business process requires savvy strategic, organizational, and managerial decisions. It is already enjoying intensive research coverage, giving rise to abundant but relatively dispersed knowledge of the mechanisms driving drug discovery and development. In this chapter, we present a comprehensive overview of the process of drug innovation from a business and academic perspective. We discuss the evolving organizational forms and models for collaboration, summarize significant empirical regularities, and highlight differences in market positions related to firms’ strategic orientation, innovation emphasis, attitudes to risk, and specialized resources. As a guide to future research, critical drivers and modes for drug innovation are systematized in a unifying framework of characteristics and process decisions, and multiple areas in need of further scrutiny, analysis, and optimization are suggested. Because of its rich potential and high significance, research on drug innovation seems poised to gain increasing momentum in the years to come.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
2.1 Introduction
The pharmaceutical industry is essentially defined by innovation. Research on the forefront of science, the creation of new knowledge bases, the invention of new medicines, and the improvement of existing drugs constitute the fuel that propels the firms in this industry. The occasional triumph of creating a novel therapy in an area with no prior treatments counts among the pharmaceutical industry’s most defining hallmarks. This is the only industry whose output can make a difference by affecting the very molecules we are made of.
Modern era medications can influence the quality and the duration of human life in ways that were never possible before. As recently reported by the Pharmaceutical Research and Manufacturers of America (PhRMA), over the last 25 years prescription drugs have successfully improved the wellbeing of arthritis and Alzheimer’s sufferers around the world, and have significantly reduced deaths from heart disease, several types of cancer, and HIV/AIDS. The death rate for cardiovascular disease has fallen by a dramatic 28 % between 1997 and 2007, while the average life expectancy for cancer patients has increased by 3 years since 1980. Most of these gains are attributable to new medicines. In the USA, since the approval of antiretroviral treatments in 1995, the death rate from HIV/AIDS has dropped by more than 75 %. As predicted by IMS Health, innovative treatment options for stroke prevention, arrhythmia, melanoma, multiple sclerosis, breast cancer, prostate cancer, and hepatitis C are also imminent.
Successful and continuous new drug introductions constitute the source of sustainable competitive advantage for the firms in this industry. The sales potential is gigantic: the global pharmaceutical market was estimated at $837 billion in 2009 and was expected to reach $1.1 trillion by 2015. As reported by the IMS Institute for Healthcare Informatics (www.imshealth.com), in the USA alone, a total of $307 billion dollars, or $898 per capita, was spent on ethical drugs in 2010, representing 2.1 % of the GDP. The USA is poised to remain the single largest pharmaceutical market, with four billion dispensed prescriptions and a total revenue of $380 billion expected by 2015. Some estimates indicate that 46 % of the people living in the USA take at least one prescription drug.
Not only is the USA the largest market for ethical drugs, but it is also recognized as the world leader in drug discovery and development, as well as a global hub for scientific and medical research. The pharmaceutical sector is the second largest US export sector, just behind the aerospace industry. It is also a major employer, estimated to provide jobs to 655,000 people. In total, directly and indirectly, the sector supports over 3.1 million jobs nationwide. It is also one of the few industries that are projected to keep adding jobs in the years to come despite the recent slowdown in the economy (PhRMA and the Bureau of Labor Statistics).
Although innovation is the lifeblood of any industry, the discovery and development of new medicines is accompanied by a host of unique challenges, ethical implications, and social responsibilities. One will be hard pressed to think of another industry where meticulous research, rigorous testing, and stringent product standards (or the lack thereof) can have such a profound impact on human wellbeing. The fundamental role of the pharmaceutical industry in maintaining and enhancing human life is further reflected in the magnitude of its R&D activity. By some accounts, pharmaceutical R&D holds an impressive 19 % share of all business spending on R&D worldwide—an impressive financial commitment for a single industry. The USA is accountable for the lion’s share of pharmaceutical innovation as it finances about 36 % of the global expenses in pharmaceutical R&D.
In 2010, the US-based pharmaceutical firms had a total budget of about $67 billion designated for research. Another $31 billion was earmarked by the National Institutes of Health (NIH) to fund research in public sector institutions (primarily government labs and universities).Footnote 1 The total pharmaceutical R&D spending in the USA has been steadily rising at an average rate of about 12 % a year, not adjusting for inflation (Cockburn 2007).
PhRMA members allocate about 20 % of their domestic sales to R&D, which makes the pharmaceutical industry the most research-intensive one in the USA. The industry’s R&D spending per employee is estimated at $105,430, which is 40 % higher than the second highest research-intensive industry (communications equipment), and 60 % higher than other technology-driven industries such as semiconductors, computers, and electronics.
PhRMA companies currently boast rich pipelines of drug candidates. In the USA there are nearly 3,000 different medicines in various stages of product development, representing a whopping 45 % of all drugs in development worldwide. Of those 3,000 new drugs in the pipeline of the US-based firms, an assortment of anticancer drugs holds the lead with 861 medicines in development, followed by 334 for respiratory diseases, 300 for rare diseases, 299 for cardiovascular disorders, 252 for mental and behavioral disorders, 235 for diabetes, 100 for HIV/AIDS, 98 for Alzheimer’s disease and dementia, 74 for arthritis, and 25 for Parkinson’s disease.Footnote 2
Despite the ubiquitous presence of medications in our lives, to many of us laypersons, the actual drug innovation process seems arcane. As customers or patients, we tend to focus on the end outcomes, just like we do with other high-tech, increasingly complex and specialized fields of innovation. And yet, as human beings, we are often fascinated by the possibilities the latest advances in life sciences (e.g., genomics, molecular biology, neuroscience, biotechnology) open to us. Drug innovation converts these new opportunities into drugs that can directly impact our physiology. This realization prompts a closer examination of the methods, steps, and processes associated with the genesis of ethical drugs.
Surely, some aspects of the drug innovation process are well-known and widely discussed. The industry is perhaps less of an enigma these days due to the unfaltering attention given it in the media. But creating efficacious drugs is also a multibillion dollar business, and there is a need to integrate the abundant yet rather compartmentalized extant knowledge about drug innovation. Such synthesis can enable us to view the process systematically and discuss it in more depth, richer detail, and with a clear emphasis on its business aspects.
It is well known that drug creation finds itself on the leading edge of the latest scientific and technological breakthroughs. Revolutionary discoveries in various disciplines are often employed to assist in the selection among myriads of naturally occurring compounds, in the design of new ones, or in the transformation of existing ones. The economic aspects related to the colossal amounts of effort and dedication germane to drug innovation are no less deserving of attention.
Drug innovation emerges at the confluence of state-of-the-art discoveries in the life sciences, aided by cutting-edge advancements in other fields such as engineering, informatics, and optimization. Thriving in the wake of the latest achievements in these disciplines, it often brings them together to intersect and interact in a way geared to ultimately improve human health and extend human life. In the process of finding the most effective structures and the most efficient strategies, novel decision opportunities and challenges arise, and new organizational forms and arrangements emerge to address them.
Inventing novel drugs is ultimately a business process in need of strict fiscal discipline and effective strategic, organizational, and managerial decisions. Various aspects of pharmaceutical innovation have been the object of intense scrutiny in diverse fields such as economics, business strategy, and marketing. Still, the obtained findings and inferences have remained somewhat insular, limited to the originating discipline despite their broader applicability and significance. There are many areas that warrant further analysis and optimization. This is why a comprehensive overview of the business processes, strategies, and practices related to pharmaceutical innovation seems necessary and timely. A compilation of this kind can be a useful reference source for various future streams and areas of research.
Hence, the intention with this chapter is to present recent findings related to the organization and the outcomes of the innovation process in the pharmaceutical industry, and concisely yet systematically review them from a business perspective. We hope that a more integrated and informative picture of the currently dispersed fragments of knowledge will arise in this process. Such an outlook will be of interest to business students, fellow researchers, and pharmaceutical executives alike, as well as to anybody with a keen curiosity about the exciting domain of drug innovation.
We start by presenting some facts and figures related to the economics of drug innovation, and briefly describe the evolution of drug discovery from a historical perspective. We proceed with a comprehensive overview of the modern process of drug innovation. To highlight the nature and the sources of its inherent complexity, we provide succinct but hopefully informative descriptions of some of the latest technologies involved. Next, we discuss the mechanisms of intellectual property protection pertinent to the industry, and outline the distinction between patents and market exclusivity. Then we move on to discuss me-too and follow-on drugs. The foray of generic drugs, the market conditions most conducive to their entry, and the drastic market changes triggered by such entry are detailed next. This discussion is followed by a review of theoretical arguments and empirical findings related to economies of scale and scope in the pharmaceutical industry. We then proceed by presenting the fundamental types of organizations that operate in this industry and discuss the modes of collaboration that have emerged in drug innovation, with a particular focus on alliances. Next, we present a summary of recent findings and insights from the academic literature. We touch upon the precursors to the current industry structure in the USA, the synergistic and preemptive benefits of investing in own R&D, the implications of early and late timing for market entry, the dynamics of market adoption in the case of pent-up demand, and the key factors that affect the market diffusion of a new drug. Then we outline the most recent trends related to pharmaceutical innovation. We conclude the chapter by suggesting directions for future research.
2.2 An Overview of Innovation in the Pharmaceutical Industry
The nature of the pharmaceutical industry makes it a veritable standout compared to others. Profound understanding of market needs is necessary but woefully insufficient for a firm to succeed. Even when finding effective medications is vitally important for the wellbeing of millions of patients, decades of painstaking research may still fail to produce a satisfactory new product.
No other industry is expected to affect how long people can live or how fast they can recover from an illness. No other industry is focused on relieving the physical pain and other discomforts everyone gets to experience in life. Consequently, no other industry is under such tremendous pressures to innovate. Still, no other industry can burn through billions of dollars and man-hours only to end up empty-handed, with not much to show for its vast expenditure, dedication, and effort.
Unlike many other market-driven industries, the pharmaceutical industry follows the so-called technology-push model. Life sciences are at the center of its endeavors to alter or reverse the processes in the human body. The onus of creating value for patients is squarely dependent on a meandering path of scientific advances and technological breakthroughs with largely unpredictable results and uneven timing.
From a business perspective, the positive momentum created by successful innovation can have dramatic, long-lasting implications for the pharmaceutical firm. The impact of a new drug launch often goes beyond the hefty profits associated with patent protection and first-mover advantage. Incremental, follow-up improvements involving greater efficacy, fewer or less severe side effects, a more convenient dosage regimen, changes in the application method, modified formulations, or new indications can significantly expand the market potential for the firm by making the drug appropriate for new patients (e.g., patients who can benefit from different dosage protocols). Notably, more than half of the new brands of drugs introduced in 2010 were not novel chemical entities or biopharmaceuticals, but improved versions and altered formulations. Incremental drug modifications of this type can ensure improved treatment, may induce better patient compliance (by interfering less with the patients’ routines or lifestyle), or enable a more convenient drug delivery (e.g., weekly instead of daily regimen). Importantly, newly released improved versions of a drug can ensure cash-flow continuity, bring in additional streams of revenue for the firm, and increase shareholders’ returns.
Besides, the options for making incremental drug modifications or the chance to manufacture bioequivalent low-cost generics present coveted new opportunities to scores of eager industry rivals seeking to enter a new market. Thus, in addition to the creation of new product value affecting millions of patients, there is also the immense social and economic benefit from the thousands of new job positions created to handle the research, manufacturing, and marketing of novel drugs in multiple formulations and variations. This realization highlights the role of drug innovation as a powerful engine of economic progress.
But the creation of new drugs is hardly an orderly, predictable process. There are enormous difficulties associated with the making of a safe and efficacious drug. Despite unprecedented recent advances in science and technology, serendipity and chance still play a role in the discovery and synthesis of effective compounds. There is practically no way of ensuring that years upon years of intense R&D efforts and huge costs will pay off handsomely in the end as the rates of success in drug discovery remain steadily low. Importantly, the performance uncertainty is amplified by the presence of stringent regulations and intense scrutiny over the entire development process. The critical decision to go to market is essentially outside the control of the firm. The market approval for a new drug ultimately rests with the Food and Drug Administration (FDA), the government agency entrusted to exercise regulatory and control functions over the pharmaceutical industry. These idiosyncrasies combine to make the development and the life cycle of drugs different from the innovation process in any other technology-intensive industry.
2.2.1 The Economics of Pharmaceutical Innovation in Facts and Figures
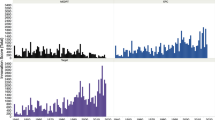
Creating new drugs is a complex, laborious, lengthy, and costly process with very uncertain outcomes. For instance, in the USA, the total number of new drugs approved between 2000 and 2010 was only 333, which seems surprisingly low given the colossal effort and cost expended by large pharmaceutical companies and numerous biotech firms alike. To explore the economics of drug innovation more closely and to size up the gravity of the issue, we will focus on the USA as the leading powerhouse in pharmaceutical research worldwide.Footnote 3
The odds of creating a marketable drug are minuscule: only 1 in every 5,000–10,000 potential compounds investigated by the US-based pharmaceutical companies is granted FDA approval. Even if the initial screening and testing have shown favorable indications, the chances of a promising drug candidate to make it through the sequential stages of the drug development process remain around one in five. About 30 % of the failures are associated with unacceptable toxicity. Another 30 % stem from lack of efficacy, while the remaining failures can be related to issues with the drug’s rate of action, the duration of its effects, or problems with the absorption, distribution, metabolism, or excretion of the drug by the human body.
On average, obtaining FDA approval and the rights to market a drug take about 15 years, with the majority of that time dedicated to clinical trials. In 2005, the average cost of a new drug successfully introduced in the USA was estimated to be $1.3 billion—a hefty 62 % increase over the last known estimate of $803 million in 2000. The opportunity cost of capital, related to the time the drug is winding its way through the discovery and development process, accounts for about 50 % of the total cost. Hence, the estimated out-of-pocket R&D expenditure for a new drug is approximately half of the amount mentioned above (DiMasi et al. 2003). Also, it must be noted that these frequently cited cost estimates are the fully capitalized cost per approved drug, which includes the cost of investigating compounds that fail to make the cut.
2.2.2 A Brief Historical Perspective on Drug Innovation
Before WWII, the link between the pharmaceutical industry and the life sciences was relatively tenuous. Most new drugs were derived from natural sources (herbs) or were based on existing compounds, mostly of organic origin. Little formal testing was done to ensure their safety or efficacy. The war instigated an extraordinary need for antibiotics worldwide. Fueled by surging market demands, pharmaceutical firms invested in unprecedented R&D programs that changed forever the process of drug discovery and development. In addition to acquiring technical and managerial experience along with the organizational capabilities to produce massive drug volumes, pharmaceutical firms emerged from the war with the clear realization how highly profitable drug development could be. Large-scale investments in R&D followed suit.
After the war, the industry faced a vast set of diseases and disorders with no known cures. There was little detailed knowledge of the biological underpinnings of many ailments. The pharmaceutical companies had to resort to random screening, trying tens of thousands of diverse natural or chemically derived compounds in test tube experiments and on laboratory animals in search for potential therapeutic effects. This process resulted in the compilation of enormous libraries of chemical compounds with known structure and studied properties. Random screening was generally inefficient—serendipity played a major role in finding a promising substance as the various action mechanisms (the biochemical and molecular pathways responsible for the therapeutic effects of drugs) were not well understood at the time.
Through the mid-1970s, significant advances in physiology, pharmacology, enzymology, and molecular biology, stemming mostly from publicly funded research, had propelled the understanding of the biochemical and molecular mechanisms of many diseases and the action pathways of existing drugs (Cockburn and Henderson 2001a). Yet, as most of the drugs at that time were derived from nature or through organic synthesis and fermentation, they were not suitable for the production of complex macromolecules such as proteins, which consist of genetically encoded long chains of amino acids. In the late 1970s to early 1980s, the advent of biotechnology and the technological breakthroughs made possible by the more versatile tools of genetic engineering marked a second watershed moment for the industry.Footnote 4
2.2.3 The Genesis of a Drug: From Inception to Market
2.2.3.1 Creating a Drug by Discovery or Design
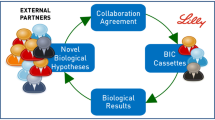
Human physiology is vastly complex, and there is a lot that is not known about the onset, the triggers, or the pathways of many diseases and disorders. For these reasons, interdisciplinary research spanning various scientific domains has become essential for modern drug discovery. Input from scientists competent in a broad range of disciplines is required in the process, e.g., skills and expertise in molecular biology, physiology, biochemistry, analytic and medicinal chemistry, crystallography, pharmacology, and even more distant areas such as information science and robotics. Advanced interpretative and integrative capabilities are critical for success. Collaboration transcending organizational, departmental, or therapeutic category boundaries has grown increasingly important for drug discovery (Henderson and Cockburn 1994). Thus, the combination of interdisciplinary competencies and openness to knowledge generated outside the firm can become the source of enduring competitive advantage for pharmaceutical firms.
Importantly, creating new drugs in the twenty-first century is no longer a series of accidental, serendipitous breakthroughs. Instead, a long and systematic process requiring steadfast commitment, diligence, and meticulous work has taken the place of the previous haphazard experimentation. The majority of modern new drugs have completed an involved and strictly regulated process to reach the market. We discuss the phases of this process next.
Prediscovery: understanding the disease and choosing a valid target molecule. In contrast to the old trial-and-error routines, nowadays the process starts with a clear understanding of the disease on a molecular level. Based on studies showing associations between biological mutations and disease states, pharmaceutical researchers formulate hypotheses about the action mechanisms involved—they study how genes have changed, how these changes affect the proteins encoded by the genes, how those proteins interact with each other in living cells, how the affected cells change the specific tissue they are in, and how all these processes combine to affect the patient.
Once scientists develop a good understanding of the underlying causes and pathways of a disease, a biological target for a potential new medicine is chosen. A biological target is most often a biomolecule (e.g., a gene or a protein), which is involved in that particular disease and can be modulated by a drug. For example, the focus in understanding autoimmune diseases such as cancer and HIV/AIDS is on discovering the proteins that affect the human immune system. The latest advances in genetics, genomics, and proteomics (studies of human genes and proteins) are employed in the process. Complicated experiments in living cells as well as tests on experimental animals are conducted to demonstrate that a particular target is relevant to the studied disease.
Drug discovery: finding promising leads for a drug candidate. Having developed a good understanding of the disease and its mechanism, scientists start looking for a drug. They search for a lead compound (an organic or other drug molecule) that may act on the target to alter the disease course, for example by inhibiting or stimulating the functions of the target biomolecule. If successful, the lead compound can ultimately become a new medicine.
Scientists turn to nature (plants, animals, or microorganisms) to find interesting compounds for fighting the disease. Microbes or bacteria, cells, tissues, and substances naturally produced by living organisms, or existing biological molecules can be used as a starting point, and then modified. An increasingly promising and flexible set of possibilities is furnished by the advancements in biotechnology, whereby scientists can genetically engineer living systems to produce disease-fighting biological molecules.Footnote 5 Rich drug source options are also provided by combinatorial chemistry, or the rapid actual or virtual synthesis of a large number of different but structurally related molecules. It enables the quick generation of new molecules to augment the chemical diversity of known molecule libraries. The method of high-throughput screening is the most common way for screening the already existing vast libraries to find those compounds that can modify the chosen target without affecting any off-target molecules. Advances in biorobotics, bioinformatics, and increased computational power allow researchers to test hundreds of thousands of compounds against the target to identify those that might have good potential.
Of late, thanks to advances in chemistry and pharmacology, scientists can abandon the generally inefficient method of systematic screening of existing molecules for a novel approach known as rational drug design. Applying analytical methods to figure out the genesis of the disease from its onset to chronicity, they come up with prototypes of a drug molecule designed from scratch. The structure of the target biomolecule can be identified with the assistance of X-ray crystallography or nuclear magnetic resonance. This information can then be used in computer modeling and simulation to predict the characteristics of potential drug candidates so that they can not only exhibit affinity and selectivity to the target biomolecule but also affect its biological and physical properties in the desired way. Designed drug molecules can be synthesized by researchers once they understand the molecular characteristics necessary for binding to the biological target. The designed drug molecules are then tested on the target biomolecule.
Next, scientists must learn how the generated compounds are absorbed into the bloodstream, if they are distributed to the proper site of action in the body, whether they can be metabolized efficiently and effectively, if they are being successfully excreted from the body, and whether they appear to be toxic in any way. Lead compounds that survive the initial testing can be optimized further or altered to make them safer and more effective. By changing the structure of a compound, scientists can change its properties to make it less likely to interact with other processes and mechanisms in the body, thus reducing the potential side effects. Hundreds of different variants of the initial leads are made and tested. Teams of biologists and chemists work closely together: the biologists test the effects of these variants on biological systems, while the chemists use that information to make additional alterations that are then retested by the biologists. After many iterations, the final compound becomes a drug candidate.
Even at this early stage, researchers attend to practical issues, considering the drug formulation (e.g., its right concentration as well as the inactive ingredients that will hold it together and make it dissolve at the desired rate), the administration route (e.g., oral application, injection, inhaler), even the details regarding the transition to large-scale manufacturing. Techniques for making the drug in the lab may not translate easily to large volume production. Still, before clinical trials can start, sufficient quantities of the drug will be needed.
Preclinical testing. With one or more optimized compounds in hand, researchers turn their attention to extensive preclinical testing. Before any human subjects can be involved in the trials, a safe starting dose must be established. Scientists carry out in vitro and in vivo tests to check the safety profile, the toxicology and the efficacy of the studied compounds.Footnote 6 Starting with approximately 5,000–10,000 lead compounds, scientists winnow them down to between 1 and 5 molecules (candidate drugs), which then enter a series of clinical trials.
2.2.3.2 Drug Development and Clinical Trials
Upon completion of drug discovery, pharmaceutical firms prepare for the next critical stage in the innovation process—drug development through clinical trials on humans. Before clinical trials can begin, the researchers must file an Investigational New Drug (IND) application with the FDA. As part of the submission, the drug sponsor must provide clinical evidence in support of claims about the primary drug indication (the targeted medical condition).Footnote 7
Drug development is structured as a linear sequence of several phases (Fig. 2.1). The transition to each next phase is conditional on a favorable outcome from the one preceding it. Each phase of the clinical trials could end up with a decision to proceed, suspend, or terminate the testing. The firm may decide to halt or withdraw its application on financial or commercial grounds, or choose to stop the trials in the light of adverse new information. The FDA can mandate that the trials be terminated at any time if problems arise. In addition, in some cases a study may be stopped because the candidate drug is performing so well that it would be unethical to withhold it from patients receiving a placebo or an inferior drug for comparison purposes.
Clinical trials Phase 1: initial human testing on healthy volunteers to establish safety. In Phase 1 trials the candidate drug is tested in people for the first time. These studies are usually conducted with about 20–100 healthy volunteers. The main goal of Phase 1 trials is to discover if the drug is safe in humans and to determine the range of safe dosage. Researchers look at the pharmacokinetics of a drug: how it is being absorbed, metabolized, and eliminated from the body. They also study the drug’s pharmacodynamics: whether it appears to produce the desired effects and if any prominent side effects may occur. These closely monitored trials are designed to help researchers determine if the drug is safe to use with actual patients.
Clinical trials Phase 2: testing in a small group of patients to demonstrate efficacy. In Phase 2 trials researchers evaluate the candidate drug’s effectiveness in about 100–500 patients who have the investigated disease or disorder. Possible short-term side effects and risks associated with the drug are noted. Researchers strive to understand if the drug is working by the expected action mechanism and whether it improves the condition in question. The optimal dose strength and the appropriate application regimen are being established. If the drug continues to show promise, it can proceed to the much larger Phase 3 trials.
Clinical trials Phase 3: testing in a large group of patients to establish safety and efficacy. In Phase 3 trials researchers study the drug candidate in a large number of patients (about 1,000–5,000) to generate statistically significant data about safety, efficacy, rare side effects, and determine the ultimate tradeoffs between benefits and risks. This phase of the research is crucial for determining whether the drug will be both effective and safe. For establishing drug efficacy, comparative testing against placebo options or against other standard treatments can be performed. Phase 3 trials are both the costliest and the longest trials (Fig. 2.1). Hundreds of sites around the USA and throughout the world participate in these trials to get a large and diverse group of patients. Coordination and monitoring of this activity can get rather challenging.
Upon the completion of clinical trials, if the analysis demonstrates that the experimental drug is both safe and effective, the company files a New Drug Application (NDA) or Biologic License Application (BLA) with the FDA, requesting approval to market the drug. The NDA/BLA includes all of the information from the previous years of work, as well as the proposals for manufacturing and labeling of the new medicine, and can run 100,000 pages or more. The FDA studies the data to determine whether the benefits outweigh the risks, what information must be included in the drug label, whether the proposed manufacturing process is adequate, and if there is any need for certain prescription criteria or special physician training.
Scaling-up for manufacturing. The transition from producing small drug quantities for testing purposes to large-scale manufacturing by the ton is not a trivial task: new manufacturing facilities may have to be built, equipment will need to be installed and processes must be calibrated. Meticulous planning and coordination are necessary to ensure smooth operations.
Post-market monitoring and Phase 4 trials. Research on a new medicine continues even after the FDA approval is obtained and the drug has been launched. As a much larger number of patients start taking the drug, companies must continue to monitor it carefully for newly found adverse effects. Periodic reports to the FDA are submitted on a quarterly basis for the first 3 years, and annually thereafter.
Sometimes, the FDA requires additional studies on the already approved drug in what is known as Phase 4 trials. These trials can be set up to evaluate the long-term safety of the new medicine. The company itself may also choose to conduct such studies to assess the drug’s potential benefits in other disease areas or for more specific patient populations (e.g., children, the elderly), leading to extended uses and indications.Footnote 8
The distinct phases of the drug innovation process with their characteristics are presented in Fig. 2.1.
2.2.4 Protecting Intellectual Property: Patents and Market Exclusivity
Pharmaceutical organizations can file for a patent on a new drug molecule they have synthesized. In addition, they can obtain market exclusivity for the drug. Although both patents and market exclusivity confer protection from competition for a specific molecule, they are conceptually and functionally distinct from one another. A patent protects the intellectual property of the firm from the time of its invention and is unrelated to the drug’s eligibility for commercialization. In contrast, market exclusivity adds more years past the FDA approval for market launch and is meant to hold off the entry of generic drugs. Patents and market exclusivity may or may not run concurrently and may or may not encompass the same claims. While some drugs have concurrent patent and exclusivity protection, others may have either type, or none whatsoever.
Patents are typically issued on novel pharmacological compounds quite early in the drug development process. They cover the active compound in a specific formulation and for specific indications. Firms can file several patents associated with a single drug, the first of which typically protects the key compound (the core of the drug as a specific new biomolecule or a new chemical entity [NCE]), while the subsequent ones can be related to different indications or new formulations. In the USA, patents can be granted by the Patent and Trademark Office (PTO) anytime along the development lifeline of a drug. Regardless of where the firm is in its clinical trials or with the FDA approval process, patents expire 20 years from the date of filing.
In contrast, market exclusivity pertains to the marketing rights granted by the FDA upon its approval of the drug, and is conferred on the actual product, inclusive of its quality, indications, and dosage. The rationale for having FDA-mandated exclusivity that is separate from the patent protection mechanism stems from the independence between the patent status and the timing of the FDA approval. As the development process leading to an FDA approval is long and uncertain, patents can expire before the drug approval, can be issued after the drug approval, or anywhere in between. Still, firms need assurance that their products will not be reproduced by competitors soon after the market launch, which can happen if the patents have expired by the time FDA approval is granted. Market exclusivity is the tool that provides such assurance. Hence, although market exclusivity does not directly extend patent life, it prevents competitors from entering the market with the exact same formulation, quality level, indications, and dosage.
Essentially, both patent protection and market exclusivity are designed to place the firm into what is a temporary monopoly situation so that it can recoup the hefty costs incurred in drug discovery and development. In the USA, firms that manage to get patent protection and exclusivity rights stacked up in the most favorable way can obtain a window of protection lasting more than 23 years. The duration of market exclusivity for new drugs can vary with the type of the drug. For an NCE, the exclusivity horizon is 5 years. If the drug is redesigned for children, additional 6–12 months of pediatric exclusivity can be obtained upon the submission of specific pediatric studies. Orphan drugs (drugs for rare disorders or for diseases that affect a small percentage of the population) get 7 years of exclusivity. For them, the extended exclusivity horizon is intended to compensate for the small market. Original biopharmaceuticals can obtain 12 years of exclusive market rights pursuant to the Patient Protection and Affordable Care Act of 2010.
If the original drug is reformulated for a different indication or for another dosage regimen, or if a modified version can demonstrate clinical superiority (e.g., greater safety, tolerability, or convenience of administration), an additional 3 years of exclusivity may be granted. However, this extension is contingent on the approval of a new application by the FDA, which requires reports on new clinical trials conducted to investigate the new formulation, indication, or dosage.
The clock on market exclusivity starts ticking at the time of obtaining FDA approval. In the USA, 74 % of all new drug sales tend to occur in the 5-year exclusivity window following drug approval, with additional 15 % of sales realized in the 3 years following the loss of exclusivity when cheaper generic versions enter the market (Higgins and Rodriguez 2006).
2.2.5 Late Entrants: Me-too and Follow-on Drugs
Despite patent protection and exclusivity, many pioneer, or first-in-class drugs do not remain the only “game in town” for too long. Even before generic alternatives enter the market, other branded drugs, also known as me-too and follow-on drugs, can make an incursion, essentially curtailing the uncontested reign of the pioneer drug over the market.
Me-too drugs. Typically, me-too drugs are minor variations of the original drug as they employ the same or similar action mechanisms, or have a related (although not identical) chemical structure. Compared to the pioneer drug, a me-too brand is a market follower, a late entrant offering a therapeutic solution that is very close to that of the pioneer drug. These drugs either replicate or provide a minor improvement over the breakthrough products in their class. Typically, they are priced at levels close to, or slightly lower than the price of the pioneer drug (reports place them in the range of 14 % below the price of the pioneer drug).
In reality, the vast majority of me-too drugs are not the product of brazen, deliberate imitation. Most of them have been in clinical development prior to the approval of the pioneer drug (DiMasi and Paquette 2004). By providing numerous viable leads, biomedical sciences create new opportunities for drug development. It stands to reason that different avenues can be simultaneously pursued by multiple firms.
The pharmaceutical industry is attractive to entrepreneurs because of its open access to fundamental knowledge, rapid information dissemination, opportunities for specialization, and connectedness to scientific networks. With the industry’s shift away from heuristics and random screening, and owing to the capabilities offered by targeted rational drug design, the discovery process has become more systematic. As a result, lots of new ventures, drawn by the alluring rewards and undaunted by the inherent risks, choose to enter. Inevitably, they engage in a race with a slew of competitors who are already working on compounds targeting an essentially finite set of publicly known diseases. As rivals get to work in parallel on similar targets, often applying the same fundamental knowledge sourced from open science, the solutions they come up with may not be all that different. Inevitably, when one of them is the first to obtain market approval, the successful rival products are going to fall in the me-too category as their market entry will be subsequent to that of the pioneer drug.
Vigorous efforts to win the innovation race are the norm as the first drug to reach the market will not only induce a significant reputation boost for the firm, but, in the absence of other alternatives, will be poised to dominate the market. For late entrants that are not well differentiated from the pioneer drug, this is no longer the case. While desperately needing to recoup their huge R&D costs, they can be left with a difficult choice: switch patients away from the pioneer drug, uncover new niches to tap into, or resort to an overall market expansion. To be lucrative, me-too brands need sufficient differentiation (actual or perceived) from existing alternatives in the market. If their market launch is at a price lower than that of the pioneer drug, price competition will ensue. Barring that, there is little reason why a patient happy with their treatment would want to switch to a me-too brand if it offers no extra therapeutic value. Moreover, prescription inertia may persist if physicians fail to perceive differential value in the me-too product, or are reluctant to interfere with an already successful therapy. Thus, marketing to physicians and direct to consumer advertising (DTC) tend to become the main battleground for share of mind and share of market for the me-too brands.
Me-too brands have been criticized primarily on the grounds of offering little or no additional advantages relative to the pioneer drug. However, clinical responses to different drugs in the same class can vary significantly by individual patient. Traditionally, physicians have adopted a trial-and-error process for finding the drug that works well for each patient. The availability of extra therapeutic options is not only clinically advantageous in case of adverse side effects induced by the pioneer drug, but is also economically and socially beneficial.
To the pioneer drug, the impending entry of me-too drugs is a threat that diminishes the incentives for costly breakthrough innovation. Despite the regulatory protection conferred upon FDA approval, the market dominance of the pioneer drug can be curtailed by the entry of closely positioned, yet differently formulated me-too alternatives. Due to relatively minor differences in formulation or action, me-too drugs can circumvent the mandated exclusivity that deters the generics, and can place the pioneer drug under intense competitive pressures much sooner, diluting its sales and eroding its market share.
Recent studies show that the effective period of marketing exclusivity enjoyed by the pioneer drug in a specific class has declined dramatically—from a median of 10.2 years in the 1970s to a mere 1.2 years in the late 1990s—due to the market entry of me-too alternatives (DiMasi and Paquette 2004). Insufficient value differentiation by the me-too brands is perhaps the worst case scenario: it can undermine the intent of patent protection and market exclusivity, and may effectively split the market without offering additional therapeutic benefits or lower price to patients. In this case, the vast resources firms have spent on R&D may never be recouped as the market proceeds are divided among multiple firms. Patients are not generally better off either except for those intolerant to the pioneer drug, as they will have extra options.Footnote 9
Follow-on drugs. In contrast to me-too drugs (the product of parallel development but belated launch, the timing of which can be beyond the firms’ control), the inception of follow-on drugs is rather deliberate and their launch is timed to occur after the pioneer drug. Even drugs that have gained FDA approval may have clinical shortcomings that are just not serious enough to terminate the project, but can nevertheless be improved upon by introducing minor alterations to the chemical structure of the breakthrough drug. Such incremental improvements are called follow-on drugs, and they constitute the majority of new drug introductions.
Developing breakthrough drugs that are safe and efficacious is very costly while the outcomes are unpredictable. In this case, another firm might see a modestly lucrative option in the incremental improvement of an existing drug. There is assurance that comes from exploiting an effective, tried-and-tested method of therapy. Besides, even the residual returns from a very large market can be rather substantial.
Overturning the conventional first-mover advantage, an improved follow-on drug may even surpass the pioneer drug through enhanced effectiveness, greater convenience, or weaker side effects, as done by Zocor®, Lipitor®, Symbicort®, and Xyzal® in their respective markets (Stremersch and van Dyck 2009). Still, the size of the market is essential as evidenced by the fact that late-market entry is less common for orphan drugs. The markets for orphan drugs are typically quite small and cannot support multiple treatments of a generally similar nature.
In some cases the opportunities for incremental changes (e.g., altered formulations, new combinations, different dosage, or novel administration routes) are well-known to the manufacturer of the breakthrough drug. If there are no compelling reasons to delay the launch, the firm can press on with the market release while simultaneously undertaking the development of improved follow-on versions to be launched soon thereafter.
It has been suggested that these two strategies—breakthrough invention with relatively short-lived first-mover advantages, and late entry with differentiated or incremental innovations—can be equally effective when examined over a 10-year horizon from their respective market introductions. Over time, breakthrough drug innovations are known to undergo drastic changes in market share—they tend to start with a systematic above-average growth, may even create a new market that they can effectively dominate for a while, but will experience a steep decline not too long after their release as other alternatives emerge. In contrast, the sales of their follow-on counterparts can be more stable overall and may quickly reach their long-term market position (Bottazzi et al. 2001). In Sect. 2.3.6.3, we outline additional findings from recent academic research on the benefits accruable to first and late market entrants.
If me-too drugs are sufficiently well-differentiated, and if follow-on drugs present incremental innovations, they can cumulatively raise the standard of patient care in the category, yield substantive treatment benefits, and enhance the value to patients.Footnote 10 The presence of multiple drugs in a category may not only address the increasing price sensitivity in the market, but can enable greater choice and thus, foster intense rivalry. The availability of alternatives can also provide leverage to health insurance companies to extract higher rebates from the drug manufacturers.
To branded drug manufacturers, though, a considerable downside of operating in a therapeutic category populated with me-too drugs is that collectively, they all become more vulnerable to each other’s fate: the loss of patent protection or market exclusivity by one member in the category can have a ripple effect on all competitors if their brands are close substitutes in terms of indications, applications, side effects, and dosage. These dynamics are discussed in more detail in Sect. 2.2.7.
2.2.6 Watch Out: Here Come the Generics!
Patent expiration or the end of the exclusivity period (whichever comes last) is the dreaded moment for every pioneer brand. Although in practice market exclusivity can extend past the loss of a patent, for brevity purposes hereafter we refer to the loss of all regulatory protection collectively as patent loss.
When the market opens up to generic entrants, aggressive price competition ensues and the original brand quickly loses market share. It is worth noting that by then, the brand might have been competing with me-too or follow-on drugs for some time. However, the competition with branded alternatives is likely to be more quality-based than price-centered. If marketing efforts emphasizing differentiation have been effective in expanding the market, the loss of market share for the pioneer brand might have been relatively limited. But when the drug patent expires, exact generic clones appear promptly at prices that can be as much as 50 % lower than those of the original brand (Griliches and Cockburn 1994).
Generally, the average price of the first generics to enter the market is about 25 % lower than that of the original brand. Over time and with increases in generic entry, generic drug prices stabilize at levels close to the long-term marginal cost of production and distribution, which is about 20 % of the original brand’s price. For example, in 2006 the average price of a brand name prescription in the USA was $111, whereas the average price for a generic prescription was $32 (Kanavos et al. 2008). Given that two-thirds of the global pharmaceutical market, currently valued at about $1 trillion, consists of molecules that are already subject to generic competition or whose patents have already expired (Kanavos et al. 2008), generic drugs offer an option for significant savings and cost-containment. Yet, generics represent a formidable threat to incumbent brands and their entry introduces a major turbulence in the markets they enter.
The selection of new markets for entry by generic drug manufacturers is driven primarily by economic factors and considerations. Empirical findings demonstrate that markets of large revenue potential, markets with a greater proportion of hospital sales relative to pharmacy sales, markets defined by chronic conditions, markets offering high profit margins to incumbents, and treatment forms or therapeutic areas with which the generic drug manufacturer has prior experience constitute the most attractive conditions for entry by generics (Morton 1999, 2000; Hudson 2000; Magazzini et al. 2004). Therefore, product/market characteristics conducive to greater price elasticity of demand, in conjunction with provisions associated with functional efficiency (scale and scope effects, experience, concentration of effort, business sustainability) have a preeminent role in the market entry strategies of generic drug manufacturers.
Brand-name manufacturers typically eschew price competition with the generic drugs. The price competition is left to the generics, which, due to insufficient differentiation, tend to experience a strong downward price pressure over time. By contrast, the price of the original brand remains higher and may even rise in nominal terms after the generic entry. This counterintuitive move is justified by the strategic decision to focus on its most loyal segment and harvest the market by maintaining premium pricing (Grabowski and Vernon 1992). However, the average market price for the molecule with the lost patent will decrease over time as the lower-priced generic alternatives achieve significant gains in market share.
Generic drugs are required to have the same active ingredients, strength, safety, quality, route of administration, and dosage form (e.g., capsule, tablet, liquid) as the brand name product, but may or may not contain the same inactive ingredients as the original brand (e.g., binders, coating, fillers), and must differ in appearance (most often, by shape or color). As the company that makes the original drug has already proved during extensive clinical trials that the drug formula is both safe and effective, the FDA approval process may not require the same rounds of clinical trials from the generic candidates, but will nevertheless demand evidence of sufficient bioequivalence.
The complex biomolecular and chemical processes involved with the action of a drug suggest that often, demonstrating identical active ingredients and concentrations may not be sufficient for a generic alternative to be approved by the FDA. With the more common small-molecule drugs, an exactly identical generic drug can be reliably produced and marketed, and minor differences in inactive ingredients may be largely inconsequential. But this is not the case with biopharmaceuticals (macromolecule drugs produced with the complex tools of biotechnology). Even a slightly different manufacturing process may result in large variations in the effects of biopharmaceuticals. The generic drug manufacturer may not have the same cell bank or compound library as the brand name manufacturer. Nearly undetectable differences in impurities and/or breakdown products have been known to incur serious health complications. This is why the generics must show that they are, within acceptable limits, bioequivalent to the original brand.
A bioequivalence test is a study to determine whether the administration of the same dosage of the generic brand will result in the same release pattern, i.e., whether, over time, it will produce the same levels of concentration in the bloodstream as the original brand. Although acceptable deviations are not disclosed by the FDA, many experts seem to believe that the generic drug must fall within an 80–125 % range of bioequivalence to the original brand.Footnote 11 Besides, all manufacturing, packaging, and testing sites for the generic drugs are held to the same quality standards as those of the original drug.
Often, generic drug manufacturers can reverse-engineer the original brand, or reproduce it by getting access to its patent documentation that discloses the active ingredients. If generic drug manufacturers choose to press on with filing for approval from the FDA before the expiry of the exclusivity period for the original drug, they would have to carry out all requisite clinical trials. For obvious economic, practical, and ethical reasons, generic entrants are often unlikely to attempt to reproduce the entire set of test data. The costs associated with replicating the rigorous clinical trials seem prohibitively dissipative and the wasted time would only extend the monopolistic reign of the original drug.
In 1984 new legislation enabled the extension of the original NDA process to all generic drugs, effectively allowing generic drug manufacturers to gain marketing approval by relying on the safety and efficacy data from the original drug’s NDA, but only after the expiration of the 5-year exclusivity period and any further extensions granted by the FDA. Thus, the mechanism of exclusive rights bestowed on the original drug prevents generic drug manufacturers from relying on its clinical data, or denies them the so-called right of reference for the duration of the exclusivity period, effectively deterring their entry.
If generic drug manufacturers can get access to the results of the original brand’s clinical trials, all they would need to do is demonstrate that the generic alternative is released in a similar way in the human body. In that case, the testing of the generic drug is performed on a sample of healthy volunteers, which is far less costly than conducting the full cycle of clinical trials. The results are then compared to those obtained in the original brand’s Phase 1 trials. For the generics, this approach represents a shortcut to market that is sanctioned by the FDA as it demonstrates the criteria for safety and efficacy are met. Formally, the generic drug manufacturer submits an Abbreviated New Drug Application (ANDA). When it is approved, the FDA adds the new alternative to its Approved Drug Products list (also known as the Orange Book), and annotates the list to show the equivalence between the original brand and the approved generic. The first generic drug that obtains FDA approval may be granted 6 months of market exclusivity.
2.2.7 Market Changes Following Generic Entry
The FDA reports that 70 % of all filled prescriptions are presently filled with generic drugs. However, the overall cost of dispensed generic drugs is only about 20 % of the total drug spending in the USA (Kanavos et al. 2008). The cumulative annual savings from generic drugs bought instead of their original branded counterparts are estimated to be in the range of $8–10 billion in the USA alone. These facts suggest that generic entry triggers dramatic shifts in the competitive landscape of a therapeutic class.
2.2.7.1 Changes in the Within-Molecule Competitive Dynamics
Upon patent expiration and in the presence of generic alternatives that replicate its formulation on a molecular level, the original brand starts losing market share relatively fast. Brand name recognition and the secured loyalty of patients or physicians remain its only sources of leverage. In the USA, drug formularies (lists of drugs that are covered by the health insurance companies) would only include the cheapest bioequivalent drug, which is typically a generic. The difference to the original brand’s price is not reimbursed by insurance companies and has to be paid out-of-pocket by patients who want to retain their original treatment. Although the vast price differential causes the original brand to lose much of its market share, it may still retain a decent stream of revenue from prescriptions to patients who perceive its quality as superior. On occasion, physicians can refuse to allow substitutions to generic drugs for fear that switching medication may interfere with their patients’ treatment, or apprehension that the cheaper alternatives may contain inactive ingredients that can cause allergies or other unwanted side effects.
It is precisely because of their bioequivalence to the original drug that, when finally given access to the market, generic drugs have a limited set of marketing tools to differentiate themselves. The lack of unique identity can prevent a generic brand from vertical differentiation based on quality, as the ANDA process has proven it equally effective and safe, but not superior to the original brand. This results in predominantly horizontal product differentiation. Parity in quality, however, seems to be questioned by some patients and physicians, and these qualms give rise to the segment that remains loyal to the original brand.
The most prominent characteristic of a generic brand is its low price relative to the original brand.
Offering a huge price advantage relative to the much more expensive branded drug is not problematic for the generics as they don’t need to recoup the significant R&D cost associated with the discovery and the development of the original molecule, and can get by on a fairly limited marketing budget. Besides, generic drugs can take a ride on the coattails of the existing market awareness for the pioneer drug they replicate, and often set out to exploit its brand recognition. Some generics openly reference the original brand on their product labels, trying to gain from favorable price comparisons and direct associations with an already familiar brand name.
Yet, overreliance on low price in a fairly competitive market can trigger a price war that can quickly annihilate the profits for the generic drug manufacturers. Occasionally, to remain viable, generic drug manufacturers turn to offering preferential arrangements and better terms to distributors (Kanavos et al. 2008). Branding their products in an effort to enhance recognition and build credibility can be an alternative strategy. Branded generics are prescription products that are either novel dosage forms of off-patent products, or a molecule copy of an off-patent product with a trade name. In either case, branded generics are produced by a manufacturer that is neither the originator nor is licensed by the originator of the molecule. By dispensing with the anonymity often associated with such products, generic drug manufacturers can create recognition and differentiation through a perception of better quality, which can also translate into higher prices.
In some countries, the original drug manufacturer may resort to a multi-branding strategy and introduce what is essentially a fighting brand by licensing its own subsidiary or an independent third party to sell a generic drug, sometimes known as a pseudo-generic or authorized generic, under the original patent. Sometimes the pseudo-generic drug is still manufactured by the originator firm, but is marketed under a different brand name. The introduction of pseudo-generics is usually a preemptive strategy originator firms may undertake pending the invasion of true generics (Hollis 2002, 2003). The intention is to ward off the significant loss of market share upon patent expiry and to retain greater market control by being the first firm to offer a generic option. However, the practice of introducing pseudo-generics is sanctioned differently across countries. As national regulators may find it objectionable enough to challenge it, it has not become routinely used yet.
As the differentiation value of generics is associated with their low price, the first generic entrant in a market seems poised to capture a considerable part of the price-sensitive segment and can essentially lock it in, ensuring long-lasting market domination. Late generic entrants would have to overcome pharmacy inertia and patient switching costs to displace the first generic entrant. Therefore, if a pseudo-generic is the first generic drug to enter a market previously dominated by the originator firm, the firm can retain more of its market power, although its sales revenue will inevitably plummet. Hollis (2002) points out that in Canada, where the practice of originator firms offering pseudo-generics is legal, it may cost about $1 million to introduce the first generic drug in the market. Still, the benefits are certainly worthwhile as the first generic can reach a sustainable market share advantage of 20–35 % relative to late generic entrants (Hollis 2002).
2.2.7.2 Changes in the Between-Molecule Competitive Dynamics
The incursion of generic drugs in the wake of a major patent loss will almost certainly affect the sales of the other branded, non-bioequivalent drugs in that class, even if they are still under patent protection. Price-sensitive physicians may increase the prescription incidences of generic drugs to the detriment of most branded drugs in a therapeutic class, regardless of their patent status. Moreover, the branded drug that has lost its patent will often scale back on its detailing efforts, enabling the drug representatives of rival non-bioequivalent brands to more easily switch detailing-sensitive physicians to their own brands. Gonzalez et al. (2008) find empirical evidence that with generic entry, the ensuing within-molecule price competition and the reduced marketing support of the firm losing its patent can also affect the between-molecule, non-bioequivalent competition in the same class. The overall effect on the sales of patent-protected non-bioequivalent drugs in that class will depend on: (a) their own marketing response in the wake of the patent loss; (b) the size of the price-sensitive and the size of the detailing-sensitive physician segments; and (c) the already established patient loyalties to the brand that is under attack because of patent loss.
In summary, the competitive landscape will get irreversibly altered when a major pioneer brand loses its patent protection, giving rise to interesting dynamics within the affected therapeutic class. In addition to the within-molecule rivalry instigated by the bevy of generic drugs, the between-molecule competition can also intensify, fostered by changes in the marketing efforts of rival non-bioequivalent brands. Over time, as incumbent firms or new entrants release novel and improved branded alternatives in the same class, physicians and patients will gradually move away from the older active molecules and the associated branded or generic drugs. Thus, the market share of an old molecule (regardless of its branding) will gradually decline over time at the expense of new active molecules launched in the same class.
2.3 Business Models in Drug Discovery and Development
2.3.1 Scale and Scope Effects in Innovation
The lengthy, costly, unpredictable, and research-intensive process of drug innovation calls for organizational settings that can help streamline operations, defray part of the costs, and enhance process efficiency. Two concepts from economics are often invoked to address such issues.
Economies of scale refer to reductions in unit cost as the size of the firm’s operations and the usage level of inputs increase. In contrast, economies of scope arise when, due to diversification in the product portfolio of the firm and in the presence of synergies across processes and activities, the same set of outcomes can be attained more efficiently, i.e., with less resources such as time, effort, or expenditure.
Economies of scale in drug discovery. Pharmaceutical companies typically organize their R&D efforts by therapeutic category based on the key systems in the body (e.g., respiratory, cardiovascular, digestive, central nervous system), then by research program (disease area), and ultimately, by specific project. Large research efforts tend to become less costly per program (and consequently, by project) in the presence of economies of scale from a large portfolio of research programs. In this case, the enormous R&D cost of drug discovery can be spread over a greater number of related research programs and projects.
Large pharmaceutical firms often invest in 10–15 distinct research programs run simultaneously. Several programs in the same therapeutic category can tap into the same pool of knowledge about the pathways related to particular biotargets or molecular processes. The new findings can be applicable across multiple programs. The more intensive use of the firm’s research talent and resources, the shared lab facilities and expertise, along with the enhanced rates of equipment utilization and reduced downtime can ensure reduction in the marginal cost of R&D. In turn, the declining marginal R&D cost of the firm makes the undertaking of risky new projects more affordable because of lower incremental costs.
Long-term market presence and cumulative experience in a therapeutic category can bring about strong learning and reputation effects. Researchers have found that firms focusing on drug discoveries in therapeutic categories in which they already have expertise (e.g., Merck with cardiovascular and cholesterol problems, Eli Lilly & Co. with psychiatric disorders, or GlaxoSmithKline with infectious diseases) are more effective than the relative novices in the category at converting R&D efforts into approved drugs (Chandy et al. 2006).
Scale effects can accumulate over time. Specifically, the firm’s cumulative technological experience in a therapeutic category has been associated with increases in the first year sales of a new drug from that category (Nerkar and Roberts 2004). It remains to be examined whether: (a) technological experience confers market advantages due to measurable improvements in drug quality, safety, or efficacy; (b) the effects are reputation-based and largely perceptual (and if so, if it is the physicians’-, the pharmacists’-, or the patients’ impressions that are of greater consequence); or (c) the positive impact stems from largely intangible firm assets, e.g., tacit knowledge about the category, special expertise with the core technologies, effective professional contacts and network leverage, or greater familiarity with the market gained during the firm’s previous launches in these categories. As this is an area of immense significance to drug manufacturers, more research disentangling the possible determinants of an experience-based sales boost for a new drug will be rather welcome.
Economies of scope in drug discovery. Competent deployment of integrative knowledge spanning different therapeutic categories may give rise to a richer set of novel ideas. It can also foster ingenious approaches and problem solutions. Internal spillovers of new know-how may galvanize the process of drug discovery by leveraging the inimitable asset of tacit knowledge that is proprietary to the firm.
Substantial economies of scope can ensue if the same amount of R&D in one therapeutic class produces valuable findings with favorable implications for another therapeutic class or category. Such positive crossover effects can emerge when knowledge acquired in the course of studying one disease can propel the research done in another program. Cross-fertilization between therapeutic categories can also occur—e.g., research programs focused on cardiovascular issues have brought about therapies related to the central nervous system (Henderson and Cockburn 1996). Internal spillovers of know-how will depend, however, on the presence of sufficient breadth of knowledge at the firm. Such proficiency will facilitate the recognition of diverse opportunities for asset redeployment stemming from the new discoveries.
Developing the foresight to identify therapeutic potential outside of the focal research area can be of immense value to the firm. First, drug candidates can be repositioned and projects can be redirected instead of terminated.Footnote 12 Second, even if a project fails or gets terminated, the accumulated specific knowledge will not simply vanish. Such knowledge remains within the firm and can be internalized or assimilated in subsequent work, potentially aiding other innovation projects. Competencies, experience, and insights developed during failed projects can be as important as those associated with successful drug outcomes. Besides, it is no small feat if the pursuit of unproductive research trajectories can be detected early and avoided in the future.
Mitigating the uncertainties associated with the success or failure of any specific investigational project is another advantage of research efforts that are broad in scope. With sufficient project diversification, the individual project risks get attenuated. As this may lower the overall credit risk associated with the firm, it can improve its access to capital.
Abundant and varied research experiences can contribute to effective learning, and may strengthen the capacity of the firm to adopt external know-how. For example, experience with diverse projects can foster more discerning capabilities for evaluating the applicability of emerging technologies, and may ease the process of integrating those technologies within the firm’s own technological stock.
A firm with a fairly diverse portfolio of research programs is also in a position to build an extensive compound library, which in itself becomes a valuable proprietary asset of a certain market value. Large libraries can assist in generating the leads in drug discovery and, thanks to high-throughput screening, have become much easier to work with. Meanwhile, smaller firms with no extensive libraries of their own may need access to the information accumulated in existing libraries. In fact, large pharmaceutical firms have started to trade access to their chemical libraries in exchange for access to new technologies, highlighting the growing significance of a more open market for information and technology in the pharmaceutical industry (Thomke and Kuemmerle 2002).
Yet, there can be a significant downside to excessive diversification in drug discovery. For example, research has shown that the simultaneous pursuit of too many project ideas can exert a negative impact on the probability of converting them into successfully launched drugs (Chandy et al. 2006). Also, with too many leads in discovery, the suggested economies of scope can be squandered due to heightened coordination and monitoring costs. Therefore, lest they spread their resources too thin, firms might be better off focusing on a moderate number of promising ideas.
Economies of scale in drug development. Economies of scale in drug development can arise from expertise that is easily transferable across different therapeutic categories because of its more fundamental nature (e.g., knowledge in biostatistics, experience with organizing large-scale clinical trials, or with obtaining regulatory approval in foreign countries). Increasingly efficient operations can result from the availability of such portable expertise. The project-related cost of having it in-house (as opposed to seeking it outside the firm on an as-needed basis) will decline if the company plans to engage in multiple development projects requiring the same areas of expertise.Footnote 13
Economies of scope in drug development. Economies of scope can be expected in drug development too as it relies on a wide range of diverse skills—from clinical pharmacology to biostatistics and metabolic chemistry. The participation of scientists and technicians whose focus is to determine the best way to manufacture and deliver the new compound (e.g., process chemists, operations engineers, or packaging experts) is also required at this stage (Cockburn and Henderson 2001b). Hence, enhanced productivity can be attained if the firm has developed diverse yet synergistic competencies, has installed the needed infrastructure (systems, technology, equipment, software), has invested in inimitable resources shared across the firm’s various programs (specialized centers and units, expert knowledge, physician networks, sales contacts), and has established the right coordination mechanisms to efficiently manage a multitude of research activities and processes.
Just as with drug discovery, a diversified research portfolio can reduce the variation in firm’s procedures and outcomes and, through learning and experience effects, increase the likelihood of successfully completing clinical trials. For example, a firm might learn to better recognize projects that, based on initial test results, signal low probability of conversion into successful drugs, and terminate or modify them early in the process to save time and costs. Experience gained through numerous NDA filings may prompt the firm to institute organizational changes to facilitate the navigation of the FDA approval process. In result, key routines can be optimized and streamlined, while the high standards and rigorous procedures required by the FDA can be carried out expertly and more efficiently.
The advantages of a solid track record of successful innovation outcomes can in turn translate into steady cash flows and help the firm attain better visibility and credibility, bolstering its position in the market. The acquired market power and enhanced professional clout can make the firm more attractive for strategic alliances and partnerships, which can essentially perpetuate its advantageous position.
The empirical evidence largely supports the presence of economies of scale and economies of scope in drug discovery (DiMasi et al. 1995; Henderson and Cockburn 1996). However, there is some ambiguity regarding measurable scale and scope effects in drug development. Economies of scale effects in drug development have remained elusive. One possible explanation is that firms have only recently started to enact coordinated project management practices to facilitate smooth transfers of tacit knowledge across dispersed research sites. With the greater deployment of such practices, data will become available to better test the premise of economies of scale through coordinated project management.
Performance advantages associated with economies of scope in drug development have been found in Cockburn and Henderson (2001b). The analysis of Sorescu et al. (2003) also supports these findings. Specifically, Sorescu et al. (2003) demonstrate that maintaining a greater scope of products (measured by the entropy in the product portfolio) enhances the value of radical innovations launched by a firm. In contrast, Danzon et al. (2005) find that more focused firms are more likely to reach successful completion of Phase 3 clinical trials. They explain their result with diseconomies of scope.
This divergence in the empirical findings can be indicative of differential patterns in scope effects depending on capacity-related organizational characteristics such as firm size. Smaller firms may need to focus on fewer therapeutic areas as their limited resources can stymie effective diversification. For them, specialization and narrow focus could be the most effective strategies. Large firms, however, can afford to develop expertise in multiple categories as their greater resources enable more successful diversification.
Still, even the largest and the best-funded pharmaceutical firms do not invest in all therapeutic categories (Henderson and Cockburn 1996). Instead, most seem to prefer to invest heavily in a few large programs, while also sustaining some involvement in various small programs. Finding the right balance in the research program portfolio and judiciously allocating the R&D budget across the right mix of diverse projects can be crucial for successful drug discoveries attained in the most efficient way.
In sum, discovery and development programs initiated within more diverse investigation portfolios can enhance the efficiency of the innovation process and increase the likelihood of getting FDA approval. The odds are stacked in favor of large pharmaceutical firms that can afford to maintain diverse portfolios and take advantage of the accrued benefits. Still, firm size is inherently scalable; organizational structures can be changed. Identifying possible regimes of size-related impact and detailing other boundary conditions that can modulate the process of drug innovation and enhance its efficiency would be a fertile ground for R&D portfolio optimization. Besides, firm reorganizations through mergers, acquisitions, spin-offs, and split-offs are frequent in this industry. They provide natural experimentation settings for examining various configurations of firm governance and size. Future research can elucidate their effects on innovation in finer detail.
2.3.2 The Changing Landscape in the Pharmaceutical Industry
2.3.2.1 Times of Transition for Big Pharma
The pharmaceutical industry is science-driven and technology-dependent in the extreme. For decades, the discovery of the next blockbuster drug (a drug likely to reach global sales of more than $1 billion) was seen as the golden grail at the end of the tortuous process of drug innovation. Creating novel drugs was deemed mostly the prerogative of large pharmaceutical firms as they were the ones best equipped to succeed.
The pressure to be first-to-market with a drug that offers unique value to millions of consumers has led to the so-called blockbuster mentality. It has propelled many a quest for drugs that can address widespread disorders and diseases, generate sky-high profits for the originating firm, cement its position as a market leader, and establish its reputation of a trailblazer and formidable rival. The appeal of creating a sustainable, lucrative, world-renowned franchise out of a single drug molecule has been too strong to resist.
To succeed in the ambitious pursuit of blockbuster hits, in their formative years most of today’s large pharmaceutical firms saw it fit to build an organization that could carry out functions encompassing all stages of the innovation process: from creating fundamental science to drug commercialization and post-market monitoring. For these Big Pharma firms—the powerhouses on the Fortune 500 list—this legacy business model has driven them to the top and kept them there for decades.
But the blockbuster mentality is essentially opportunistic. It is a costly gamble with high stakes, prone to generating many more “misses” than “hits.” Given the long time for drug development, the shorter exclusivity periods, the decrease in expected returns, and the constantly increasing costs of commercialization, the strategy of sourcing all the skills and knowledge necessary to create a new drug from within the firm, through a fully integrated business model, may have run its course.
Besides, the frequent breakthroughs in life sciences, combined with high-paced advances in technology and the ever-expanding toolsets for drug synthesis and design, suggest that fully integrated firms straddling all aspects of drug innovation might quickly fall behind in the race to invent fast and well. Highly specialized skills aligned with the constantly evolving technologies are becoming essential. The current proliferation of state-of-the-art technologies can steer the pharmaceutical industry toward more decentralized business models. This transition has already started, and its onset was marked by the emergence of a rather unprecedented new venture type—the biotech firm.
2.3.2.2 The Foray of Biotech Firms
The 1980s brought about a surge of entry into the pharmaceutical industry by small, research-focused, entrepreneurial firms that positioned themselves between the incumbents (the already large for-profit pharmaceutical companies) and the public sector research institutions (Cockburn 2007). The rise of these independent centers of vigorous R&D and invention, primarily in the area of biotechnology, was facilitated by a range of institutional and legal changes at the time. Widely known as biotech companies, these firms focus on the discovery and development of biopharmaceuticals (proteins, DNA, RNA, and other biomolecules created by means other than direct extraction from a native biological source).Footnote 14
Biotech firms are often credited as the engine of innovation in the pharmaceutical industry (Wuyts and Dutta 2008). They generate drug discoveries by maintaining a narrow focus on the latest knowledge in the life sciences and are dedicated to mastering leading-edge technology. However, the majority do not have easy access to large amounts of capital and could be severely underfunded or understaffed. Their limited resources may prevent them from attaining the critical mass or the diversity in R&D projects necessary for the realization of significant economies of scale or scope in drug innovation.
For example, recent research has found that although the out-of-pocket R&D costs for the development of an approved drug do not vary greatly between small biotech and large pharmaceutical companies, those originated by small biotech firms take about 7.5 months longer to reach FDA approval, which raises their capitalized cost (DiMasi and Grabowski 2007). Efficiencies in operations are hard to attain for these firms. Even if they manage to successfully take their innovative products through clinical trials, small biotech firms may not have the requisite commercialization capabilities to go to market. Therefore, the stages of the innovation process that need large-scale efforts combined with access to considerable capital, infrastructure, and proprietary assets (e.g., clinical trials, manufacturing, or marketing) might be the stages best delegated to other industry participants.
If the strategic preferences of biotech firms are more in line with building competencies in the life sciences and performing on the forefront of biotechnology, they may seek to outsource clinical trials to better equipped organizations (e.g., hospitals, university research centers), or form strategic alliances with firms that already have the necessary competencies, e.g., large pharmaceutical companies. Outsourcing the later stages of clinical trials to larger, better funded and well-staffed organizations can be not only the more effective but also the more efficient strategy to rapidly bring drug development to completion and, contingent on FDA approval, commercialization (Grewal et al. 2008). Partnerships and strategic alliances constitute a vehicle that can provide biotech firms with a shortcut to what they need the most—fast access to capital, infrastructure, or market knowledge. Delegating these concerns to those more adept to handle them enables biotech firms to remain focused on invention and discovery, and frees their resources to react swiftly to the latest scientific information needed for sustaining a technological edge. The attendant division of labor might be an efficient collaborative outcome stemming from existing competencies and the desired domains of expertise in the pharmaceutical industry.Footnote 15
If biotech companies need assistance with the organization of clinical trials, they have the option of outsourcing to independent Contract Research Organizations (CRO). Yet, many biotech firms may decide to license their products to large pharmaceutical firms despite the CRO option because of the greater marketing knowledge and experience large pharmaceutical firms can also bring in. For the originating biotech firms, the downsides of relinquishing market control can be more than offset by the infusion of vast amounts of capital and the massive advertising and sales effort large companies can deploy before and during the market launch.
2.3.2.3 Public Sector Research Institutions as Centers for the Creation of Open Science
The extraordinarily science-intensive process of innovation in the pharmaceutical industry is critically dependent on state-of-the-art technologies. The prediscovery phase of drug innovation starts with basic research, fundamental knowledge, and understanding of the mechanisms of pathology. By nature, such broadly applicable research is germane to the mission and the interests of research institutions operating in the public sector. The most active institutions in this regard are universities, hospitals, and government labs.
In the USA, public sector institutions, funded mostly by NIH, are an essential contributor to drug innovation. Their involvement comprises knowledge accumulation through fundamental research, participation in clinical studies, and training of future healthcare professionals. Public funding for fundamental science is predicated on its expected value: basic research creates fundamental knowledge, whose future applications and commercial potential might be presently unclear.
Unlike their counterparts in the for-profit sector, most public sector institutions are not inordinately governed by commercial considerations. For them, the scientific curiosity, the broader societal interests, the recognition by a community of peers, the wide range of implications, or the gratification of doing novel research can be among the most compelling drivers. Self-guided, replication-focused, regulated by publication measures and often sanctioned by a peer review system, the science created by public sector institutions generates the data, ideas, tools, and paradigms that push the scientific and technological frontiers in the pharmaceutical industry and chart its future trajectories. The expectation is that many of the advances in fundamental science are going to be utilized by applied researchers working on specific projects at for-profit firms. It is their job to eventually convert the fundamental knowledge generated by public institutions into specific, marketable drugs.
Because of the more general nature of fundamental science created in public research institutions (e.g., understanding metabolic processes and biological mechanisms), its ultimate benefits are contingent upon the open dissemination of results (e.g., through publications or presentations) to downstream firms and the industry at large. Fundamental scientific advances generated by public sector institutions are likely to be relevant to a broad range of fields. Open access to the latest basic discoveries, mandated by the public goods nature of this knowledge, makes them promptly available to all industry participants.
Scientific discoveries of great social value can transcend any private firm interests. This rationale dictates that they be kept in the public domain for maximum social returns.Footnote 16 Still, the widely accessible knowledge generated by the public sector creates a strong and positive externality for the private sector. This unconstrained availability of new fundamental knowledge is called open science (Cockburn 2007). The expected rapid diffusion of open science serves to stimulate distributed, decentralized research efforts and essentially prompts innovation. However, it can also make the returns on investment in fundamental science generally hard to attribute or appropriate (Cockburn and Henderson 1996).
However, the notion of the public sector as a designated entity for creating and disseminating fundamental knowledge is a simplification of its actual involvement and contribution. Many public sector institutions engage in building molecular libraries by screening compounds that can directly benefit private firms. The training of a vast pool of qualified personnel for the pharmaceutical industry is also in the hands of publicly funded organizations. They are often tasked with providing the necessary infrastructure for drug discovery and conduct clinical trials for commercially oriented, for-profit firms.
The distinctions between the roles assumed by the public and the private sectors can easily blur. Private firms sometimes straddle the boundaries between creating fundamental science and applied know-how. On occasion, pharmacologists working at for-profit firms may have to conduct basic research. Many academic institutions file for patents and retain exclusive rights on their innovations, underscoring the shifting roles the industry participants go through. Such practices notwithstanding, the current trend seems to be toward greater mutual dependence among autonomous organizations, which we discuss below.
2.3.3 Maps, Engines, Vehicles: The Trifecta Model for Navigating Drug Innovation
The traditional blockbuster model based on genuine breakthrough innovations has become increasingly hard to maintain. The majority of new drug launches are those of follow-on or next-in-class compounds that may not provide highly differentiated therapeutic value, but are released at short intervals. In fact, only about 20 % of firms’ R&D budget associated with clinical testing is for drugs categorized by the FDA as offering significant improvement over marketed products (Angell 2004). New innovation opportunities are associated mostly with segmentation strategies: niche markets, combination drugs addressing related or concurrent disorders, drugs tailored to specific genotypes, and ultimately, mass customization in the form of strictly personalized medications or therapy (Gassmann and Reepmeyer 2005). A new generation of blockbusters driven mainly by breakthrough innovation is still likely to emerge, but may need a more specialized business model (Gilbert et al. 2003).
What are the factors that have brought about greater specialization and decentralization pressures to the previously highly centralized, vertically integrated industry? The answer might be found in the specifics of the drug innovation process, its inherent modularity, and the “ticking clock” of patent protection and market exclusivity.
Commercial considerations still reign supreme in the pharmaceutical industry, as they do in any other high-tech industry. Yet, the considerable uncertainty related to a drug’s future may prevail. An important point of divergence from other industries is that in the pharmaceutical industry, decisions to terminate projects are rarely made on economic grounds. Although the direction of R&D efforts may be guided by stark commercial reasons (e.g., large markets associated with common diseases or chronic disorders are most attractive for investors in drug innovation), project outcomes are driven by modern science and technology and remain constrained by their limitations. Ultimately, the candidate drug’s safety and efficacy are the true deal-breakers on the route to market in this industry. Nevertheless, no firm can forecast or control them too well.
Furthermore, the drug innovation process can be disassembled into distinct stages with clear inputs, outputs, and objectives, which can be carried out by the same firm (provided it has the necessary resources), or distributed across different organizations. The act of invention, which is central to drug discovery, rests on fundamental knowledge that can be sourced from various organizations or disseminated as open science. Drug discovery produces a certain biomolecule, a tangible and finished product in its own right. Thus, it can be separated from the subsequent stages of clinical development, large-scale manufacturing, and commercialization, each one of which is also self-contained, with distinct and well-defined outcomes.
In line with this notion of modularity in the drug innovation process, a naturally occurring division of organizational focus and research effort has come to the forefront. Considerable efficiencies can be realized if tasks can be divided across different firm types based on their idiosyncratic competencies and strengths. As timing is critical under a limited window of patent protection and market exclusivity, arrangements that can streamline and expedite the innovation process, lower its costs, and diversify the inherent risks become increasingly attractive.
Hence, a multi-tier system of organizations supplementing each other’s competencies might be best equipped to handle the complexities of modern drug innovation both efficiently and effectively. In fact, it has already emerged. Three organizational tiers are involved in pharmaceutical innovation: public sector organizations provide the fundamental science that essentially maps out the landscape for subsequent innovations, small biotech firms serve as a veritable innovation engine, conducting cutting-edge research and supplying novel biomolecules, while large pharmaceutical firms, ambidextrous and multifunctional, are particularly adept to serve as a vehicle for advancing scores of drug candidates through clinical trials to FDA approval, and then to commercialization. These three organizational types complement each other’s strengths and can operate in symbiosis to advance biomedical research in a trifecta model of innovation (Fig. 2.2).
Note that these three types of organizations are not, by nature or by articles of incorporation, accustomed to be “chummy” with each other. They can be bona fide rivals, competing for market share, racing for patents, or vying for the position of a market leader in their field. And yet, they have come to coexist in a mutually agreeable way, gaining from synergies and benefiting from occasional acts of cooperation. The occurrence of drug-centered partnerships appears to be the new business model increasingly gaining prominence in the pharmaceutical industry.
Throughout the life cycle of a drug, the output of public institutions (i.e., universities, government labs, hospitals) benefits the private sector in at least two major ways. First, the created fundamental biological and chemical knowledge generated by the public sector is often used as groundwork for drug discovery as it maps out promising avenues for applied research. Second, the public sector can assist with clinical trials, e.g., by contributing practical knowledge for trial design, by carrying out the actual testing of new drugs, or by collecting and processing post-market information following the market launch.
Close connections between the private and the public sector can enhance the performance of private firms. Participation in the construction of publicly available research data and findings, as well as joint publications or presentations with leading researchers from the public sector are precursors to more effective drug discovery in private firms (Cockburn and Henderson 1998). Some evidence suggests a 30 % return on investment for research done in the public sector, when measured by its effects on the private sector (Cockburn and Henderson 2001a). This estimate is 2.6 times higher than the average return on innovation in this industry, assessed to be about 11.5 % (Grabowski et al. 2002). Positive externalities like open science and free information exchange help private firms overcome the boundaries of specialization, and make specialization itself more feasible and desirable. Immediate access to leading edge, publicly funded science bestows a competitive advantage on large pharmaceutical firms, but is particularly vital as a source of new knowledge, information, and intellectual stimulation for the emerging biotechnology sector with its small, research-focused private firms.
Notably, the open-science model underpinning interorganizational interactions and cooperation is sustained by a veritable bidirectional flow of information. The collaboration between the public and the private sector can be mutually beneficial: private firm researchers, too, can contribute practical experience and expertise, as well as knowledge (applied or experimental), to their counterparts in the public sector. The vibrant culture of applied science and the specific challenges encountered in drug innovation can stimulate the publication-driven public sector and reenergize its efforts by suggesting new research directions.
The ongoing shifts in the industry landscape and the increasing prominence of new types of organizations can be unsettling for large pharmaceutical firms which, because of their considerable resources, networks, and marketing prowess, are used to having an uncontested advantage in the complex and expensive process of drug innovation. After all, outspending, outlasting, or displacing poorly funded small rivals should come easy for them. Vast intangible assets like experience and reputation, tacit knowledge, contact networks, or proprietary know-how from years of intensive and diverse research should have been sufficient to sustain their dominance as the leaders in innovation productivity. Their capacity for economies of scale and scope should be indispensable as efficiency gains can be enormous in this highly research-intensive industry. And yet, the emergence of a specialized market for biotechnology, in conjunction with the multitudes of agile and inventive small firms drawn to it, has fostered vertical disintegration in the pharmaceutical industry.
The exigencies of rapidly changing modern technologies stemming from the life sciences may prompt large firms, too, to carve out specialized niches for themselves. Recent specialization tendencies, added to the constant pressures to perform on and beyond the ever-shifting frontiers of science, have increased the value of network externalities and the need for more open information exchanges. What remains to be seen is whether large pharmaceutical firms, accustomed to being ambidextrous in drug innovation, might shift gears and opt for efficiencies through tighter research focus, exploitation of existing assets, and aggressive pursuit of partnerships, so that they start scaling back on the range of scientific and technological areas they invest in.
Specialization by therapeutic area, disease pathway, target molecule, drug candidate molecule, method of drug synthesis, or even by patients’ pharmacogenomic profile seems to be the way of the future for pharmaceutical firms. Such streamlining and narrowing of their exploratory focus can free resources for obtaining greater scientific and technological proficiency and help develop unique experience and expertise in a few therapeutic areas. The acquired in-depth knowledge and know-how can still be shared with selected partners through various forms of collaboration and controlled information exchanges so that functional synergies and cross-pollination of ideas can occur.Footnote 17
Large pharmaceutical firms seem particularly well-equipped to serve as expedient platforms to market. Owing to their vast scale of operations, professional networks, and experience, they are adept at designing and overseeing extensive clinical trials, and can organize and conduct them faster. In addition, their sizable marketing prowess and already established sales forces can ensure more effective end-product commercialization. Researchers have already found empirical evidence in support of this premise. For example, products developed in interfirm partnerships turn out to have a greater probability of success, particularly if the licensee is a large firm (Danzon et al. 2005).
In summary, the pharmaceutical industry seems to have embarked on a gradual transformation away from the vertically integrated model with the strong blockbuster orientation. The emphasis is shifting to incremental innovations, greater specialization, and focused R&D in an effort to capitalize on established competencies, realize greater efficiencies, and benefit from synergies. In turn, these tendencies have brought about new business roles and practices that have supplanted the earlier vertically integrated model of self-sufficient firms with more distributed, collaboration-intensive models. Public sector research institutions, large pharmaceutical firms, and small biotech ventures seem to have found a way to flourish side by side and balance bouts of rivalry with forms of interdependency and collaboration. We examine these forms next.
2.3.4 Modes of Collaboration for Innovation in the Pharmaceutical Industry
The high stakes associated with exclusivity rights, unpredictable outcomes, fierce competition, and first-to-market races in the pharmaceutical industry have given rise to a multiplicity of business models and interfirm arrangements to choose from or gravitate between. The industry is evolving fast, mixing-and-matching from a smorgasbord of options based on fluctuating demands and environmental shifts. Large vertically integrated firms coexist and collaborate with organizations with a strictly narrow focus, alliances and partnerships are frequently formed and dissolved, new entry of small specialized firms is common, mergers and acquisitions are a familiar fixture, and the occasional spin-offs of divisions into autonomous ventures are no surprise either. Pharmaceutical innovation is no longer a stand-alone activity undertaken by individual firms in total isolation.
An increasing practice of technology transfers and know-how diffusion across firms builds upon the positive momentum created by the openness of fundamental science. In addition to staying alert to the intellectual output of public sector institutions, firms seek to lower the total costs of new drug creation and shorten the time to market through strategic alliances and licensing agreements. Calculated knowledge exchanges introduce system efficiencies by exploiting synergies between various assets and resources held or developed by the individual firms. Sharing know-how can facilitate and accelerate the innovation process and would explain the ever-increasing number of licensing deals, partnerships, and strategic alliances among pharmaceutical firms. Besides, the industry remains prone to occasional consolidations through mergers and acquisitions. The persistence of such tendencies indicates that economies of scale and scope may be too valuable to forgo despite the benefits of specialization.
There is evidence that drugs developed in a partnership are significantly more likely to succeed in Phase 2 and 3 of clinical trials. In a sample dominated by small- and medium-size firms, Danzon et al. (2005) find that interfirm cooperation in Phase 3 of clinical trials produces a 15 % greater probability of approval compared to independent efforts. These odds may actually be old news to the industry as indicated by current business practices, which show that compared to large pharmaceutical firms, biotech firms are less likely to take drug candidates to clinical trials on their own (Arora et al. 2007).
Large pharmaceutical firms are in a position to enjoy the vast awareness, credibility, and the brand equity that small firms find lacking. Owing to their sizable budgets and greater scale of operations, large firms are poised to have easier access to capital. They are also more likely to possess the necessary marketing resources small firms may find hard to acquire. Also, inimitable assets like a steadfast reputation for process rigor and product quality might turn out to be critical for sustaining a competitive edge in crowded therapy markets. Such intangible assets could be more easily accruable to large firms because of their vast drug portfolios and long track records of market presence and innovation.
Although they tend to operate on a smaller scale, the intellectual output of biotech firms has made them as significant to the US pharmaceutical industry as powerhouses like Merck, Pfizer, or Eli Lilly. However, biotech firms in general may not have the resources to maintain a diverse project portfolio and would often lack the downstream assets to take new drugs to market. Many seem inclined to specialize in advanced research, the outputs of which are licensed out to others. One implication of this practice is the lack of public visibility for their achievements, which may become a strategic deterrent in case of future plans for market entry.
Still, for all the entrepreneurial drive and agility of biotech firms, a narrow focus and concentration of efforts in a few therapeutic areas could be both more effective and more efficient given their limited resources. It is the combination of their in-depth knowledge and the willingness to tap into risky cutting-edge research that comprises biotech firms’ chief contribution to drug innovation. In fact, in some cases, licensing out newly developed technologies may be their only viable route to market, as the majority have no significant sales structure or marketing capacity in place. Thus, licensing fees may constitute their main source of revenue.
As biotech companies assume the role of renowned drivers and suppliers of innovation, those that succeed can enjoy a rather favorable business outlook. There is empirical evidence that firms investing more in research tend to obtain more licensing deals. In turn, having a wide portfolio of licensing deals translates into more new licensing deals (Wuyts and Dutta 2008). Thus, investment in focused R&D efforts can create a self-perpetuating momentum that bolsters firm viability and brings in sustainable revenue streams from licensing. Increased innovation output, learning effects, the accumulation of valuable R&D stock, or a growing reputation for creativity and novelty can explain these linkages.
Dedicated biotech firms investing in narrowly focused drug research can find themselves on a lucrative spiral of growth.Footnote 18 Developing specialty drugs for niche markets can be profitable as no large-scale marketing efforts are involved, and competitor entry is less likely due to the small market potential. There are indications that the stock market, too, regards small firms of a sharp research focus (i.e., those with small research portfolios) more favorably by boosting their stock prices, essentially acknowledging the greater likelihood that they can be successful if they sustain a narrow specialization (Grewal et al. 2008).
Still, too narrow a specialization in innovation can become risky as economies of scope might be hard to come by. Moreover, overreliance on partnerships and excessive dependence on collaboration, necessary to overcome the constraints of narrow specialization, can turn precarious. Disagreements between partners may occur, leading to delays. The incurred R&D costs can be difficult to allocate and recoup. A more detailed examination of licensing dynamics and their impact on performance is necessary to further elucidate the associated mechanisms, the drivers and the moderators, the boundary conditions and the most likely process outcomes under different conditions.
Generally, small firms would find large firms attractive to partner with because of their considerable resources and intangible assets. Yet, in a partnership, large firms will have to share the eventual market proceeds with another firm. If small firms can benefit from the immediate access to funding, downstream assets, and experience that alliances with large pharmaceutical firms make possible, what are the advantages from in-licensing agreements and other forms of cooperation for the large firms?
For them, in-licensing is a shortcut to quickly fill their product pipelines and extend their research portfolios. As continuous innovation is imperative in the pharmaceutical industry, replenishing drug pipelines on a regular basis is crucial for maintaining a strong competitive standing. Large pharmaceutical firms are under constant pressure to maintain full and promising project portfolios, which makes them appealing to shareholders and can affect these firms’ access to capital. As shown by Grewal et al. (2008), shareholders tend to support the large pharmaceutical firms that have broad research portfolios, and are particularly interested in firms with drugs in the later stages of development. In view of such considerations, publicly traded firms will look to sustain a reasonable number of ongoing investigative drug projects and will try to quickly replace those that have been concluded or terminated. Besides, maintaining large research portfolios can lead to economies of scale and scope, resulting in better resource utilization.
It is hardly a surprise that the largest pharmaceutical companies are the ones advancing most new chemical entities to market.Footnote 19 These firms can leverage superior integrative capabilities, tacit knowledge, and abundant experience to improve the chances of in-licensed drug candidates to get to market. For large firms, in-licensing is a rather desirable business strategy geared for the realization of synergies, reduction in effort duplication, and ultimately, more efficient use of firms’ resources. These arguments explain why taking products discovered by their smaller brethren—the biotechs—and bringing them to market seems like a reasonable and savvy move for many large pharmaceutical companies.Footnote 20
It is worth noting that although large firms are typically drawn to in-licensing, they may occasionally opt to out-license some of their own compounds. Even a large firm may have insufficient capacity to handle too many projects. If a large firm has a number of candidate drugs all approaching clinical trials, it may prefer to retain those with the greatest market potential, and license out the rest. The projects that get licensed out could be the riskiest ones or those with the lowest expected sales, although the firm will still keep a stake in their future performance. However, Danzon et al. (2005) find no evidence of such a “lemons” problem.
Of course, partnerships may occur between large pharmaceutical firms too. A compelling reason for such partnerships is the intention to diversify the risk and share the huge marketing costs for an impending market launch. In such cases, strategic alliances are created for the express purpose of marketing a specific drug jointly. Typically, the partner firms employ carefully coordinated pricing and communications strategies and, by pooling their sales forces together, can obtain broader access to markets.Footnote 21
Licensing has an immediate impact on the size of the firm’s project portfolio. It also affects the resource allocation of the firm. Simonet (2002) identifies three types of large pharmaceutical firms based on the prevalent sourcing of their project portfolios: (a) development-oriented firms choose to maintain a project portfolio dominated by in-licensed products, for which the focal firm conducts clinical development (e.g., Johnson & Johnson, Bristol-Myers Squibb); (b) firms with well-balanced portfolios strive to maintain a set of self-originated products that match or slightly exceed the number of in-licensed products in their pipeline (e.g., Eli Lilly, Pfizer, Roche, Novartis, GlaxoSmithKline); and (c) research-oriented firms operate with a relatively small number of in-licensed products in their portfolio, and place strong emphasis on self-originated products that they take into development (e.g., Merck & Co., Bayer, Boehringer Ingelheim, Novo Nordisk).
Regardless of their revenue, it is the firms experiencing a decline in new drug productivity (measured as depletion in their research pipeline) that are more likely to engage in R&D-focused alliances, in-licensing agreements, or consolidation through mergers and acquisitions (Higgins and Rodriguez 2006). The examples studied in Simonet (2002) seem congruent with this conclusion—two of the four development-oriented firms in that review were subsequently acquired.Footnote 22 Nonetheless, tempting as it is to make causal inferences about a precipitated downfall associated with too much dependence on in-licensed products, anecdotal and isolated cases like these are not sufficient for generalization. Besides, an acquisition can be a springboard to faster growth under a different identity instead of a death knell for the acquired company. Data including information on the retention of management and R&D teams and on the fate of projects initiated before the acquisition may shed more light on these issues.
The assimilation of external ideas, knowledge, technology, or know-how can determine the future market options for the firm, and can be an instrument to quickly balance a temporarily weakened pipeline. Given the uncertainty in gaining FDA approval with a single drug candidate, a richer portfolio will increase the firm’s chances to take at least one drug to market. The success of a business model with a stronger leaning toward external innovative input through in-licensing may be contingent on the current state of the firm’s R&D portfolio, as well as its capacity to attract, select, and carry out projects of greater potential for success.
Firms looking for licensing or acquisition targets may need to find the right balance between leveraging specific competencies and attaining pipeline diversity. Evaluating the knowledge-based assets of other firms can be rather challenging. Only firms actively engaged in certain therapeutic areas may have the confidence and the capabilities to accurately assess the potential of others’ R&D efforts, the expertise to manage the development process more efficiently, or the marketing experience and the sales contacts to execute the launch effectively. On the other hand, acquiring a firm with a rather different pipeline might be advantageous in its own right as it will contribute to the acquiring firm’s project diversification. Maintaining focused or diversified research portfolios may be differentially conducive to small vs. large firms or to upstream vs. downstream organizations. Therefore, large pharmaceutical and small biotech firms alike may need a clear recognition of the combination that could be optimal in their setting.
Collaboration assists firms by supplementing their own R&D activity. Licensing, strategic alliances, mergers, and acquisitions can invigorate firms’ internal research efforts and extend their research pipelines (Chan et al. 2007). Promising drug candidates can be brought forth for clinical investigation at a much higher rate, building a valuable momentum in the competitive race to market. Ding and Eliashberg (2002) find that firms underspend on drug development during clinical trials, suggesting that optimization of their pipelines could be necessary. The infusion of external know-how and the adoption of candidates from new therapeutic categories will lead to more diversified research programs, opening up options for more efficient utilization of resources. Besides, diversification through assimilation can create new strategic advantages and translate into greater gains for the firm.
Of course, there can be exceptions and variations from the business models and practices discussed heretofore. For example, not all biotech firms are small, nor are they solely confined to highly specialized research with a narrow focus. Some, like Amgen, are sufficiently vertically integrated to take promising drug candidates from prediscovery to market. Biotech firms can learn to successfully manage diverse R&D programs, too. The modes of collaboration in the pharmaceutical industry are abundant and multifaceted, and hold great potential for more in-depth analysis and continued empirical research.
Considerable differences in productivity across pharmaceutical firms might be associated with variability in their strategic decisions about the scope, the focus, or the coordinated timing of their innovation efforts. In the academic literature, two likely scenarios have been explored in more detail: overflowing project pipelines and shortages in the project pipeline. We sketch out some of the analytical inferences below.
Cassiman and Ueda (2006) analyze the conditions under which an established firm might be advised to spin off some of its newly conceived technologies to start-up ventures. Such spin-offs are typically headed by former employees (scientists) proven to be essential for the development of the said technologies at the incumbent firm. The authors conclude that firms will spawn off such ventures, and occasionally even partially subsidize them, if: (a) the firm undertakes a lot of successful R&D projects and has no free capacity for commercializing them all (that is, a capacity threshold has been reached); (b) the firm is already operating close to its commercialization capacity and thus, becomes increasingly selective about the market value of additional projects; (c) the spun-off technology is considered to be of low complementarity value to the firm (e.g., it is misaligned with the firm’s prevalent know-how, requires large investment in new co-specialized assets, or has a poor fit with the existing core markets); and (d) the new technology represents a low cannibalization threat for the incumbent firm’s other products. The assertion in (d) is based on the premise that potential cannibalization can be best controlled when the technology in question is kept in-house.
In case a firm has its R&D pipeline running low on projects of high expected value, the decision to “purchase” new projects may depend on the firm’s risk aversion. The potential trade-off between adjustment costs (the forgone returns from co-specialized investments if they become underutilized or must be downsized in the face of diminishing activity—e.g., the thinning out of a specialized sales force), and the candidate project’s transaction costs (the transfer and the assimilation costs for a licensed-in candidate) should be evaluated before a new project is brought in from outside the firm (Chan et al. 2007).
Analytically, it can be shown that even if entrant firms are more risk-seeking than incumbent firms, for sufficiently high adjustment costs relative to transaction costs, the entrants may choose to specialize in R&D and would rarely seek to commercialize projects (Chan et al. 2007). Knowing this, established firms may consider raising their own adjustment costs (by making a greater investment in co-specialized assets) as a preemptive strategic move aimed to lower the transfer cost (e.g., the license fee) of future projects offered by entrants. Although current practices in the pharmaceutical industry appear broadly consistent with the implications suggested by this analysis, targeted empirical research can help illuminate the related strategic interplay between entrants and incumbents in more detail.
2.3.5 Strategic Alliances as a Shortcut to Market in the Pharmaceutical Industry
The earlier and the later stages of the drug innovation process differ by nature. Accordingly, the tasks and the required skills, competencies, and resources would change along the innovation pathway of a drug. The specific objectives of each investigative phase enable tasks to be performed by different organizations so that the ones most adept in certain functions get to carry them out.
Strategic alliances represent a propitious ground for symbiotic collaboration between the small biotech and the large pharmaceutical firms. They provide for a closer interfirm relationship than licensing, yet are safer than outright acquisitions. Such alliances are intended for the commercialization of science and aim to exploit complementary competencies residing in different organizations.Footnote 23
Many of the earlier studies on strategic alliances in drug innovation have been largely case-based. The industry is fairly young and volatile, and there is a relative paucity of tractable measures on the partner selection process, the structure, governance, and evolution of alliance modes, or the way innovation value is created and appropriated in such partnerships. Due to space considerations, we briefly outline recent empirical findings from the academic literature that relate to alliance-related decisions. These studies have used large samples to enhance generalizability.
Rough estimates point to biotechnology as the industry with the highest rate of alliance formation and the one with the highest growth rate in new alliances (Hagedoorn 1993). This is hardly surprising given the advantages of strategic alliances as well as their considerable signaling value. For the generally less visible biotech firms, participating in alliances with large pharmaceutical firms can be seen as a tacit endorsement. Such partnerships can bestow special clout on small, relatively unknown ventures. A study by Stuart et al. (1999) demonstrates empirically that alliances can boost the stock market valuation and expedite the IPO of the biotech partner. In addition, as shown by Danzon et al. (2005), in the late stages of clinical trials a new drug developed in an alliance has a higher probability of success, especially if one of the partners is a large pharmaceutical firm. A strategic alliance between a biotech firm and a large pharmaceutical firm can also be a precursor to the pending acquisition of the biotech firm by its large partner. However, alliances in the pharmaceutical industry are not limited to biotech-pharmaceutical dyads and can also occur between peer biotech or peer pharmaceutical firms. Public institutions (e.g., universities) can also partner with biotech or pharmaceutical firms. Many organizations tend to engage in multiple alliances simultaneously. Tracking all alliances of a firm is difficult as firms are not expected to disclose their interfirm arrangements (but may choose to publicize them nevertheless). Also, some agreements could be rather informal (e.g., handshake deals).
The rationale for alliances in the pharmaceutical industry. The incumbent large pharmaceutical firms, vertically integrated and well-funded, already in command of considerable sales forces and embedded in vast networks of industry contacts and relations, have essentially become efficient vehicles for drug development and market access. They offer synergies to both public sector institutions and biotech firms, the majority of which may lack the requisite assets to carry drug discoveries to commercialization. In the absence of steady cash streams, the long horizon to market launch places biotech firms in a particularly vulnerable position to sustain operations and highlights the likely benefits of their partnerships with the incumbent large pharmaceutical firms.
The value of large pharmaceutical firms’ downstream assets (manufacturing, marketing, sales) can be crucial to biotech firms working in the same or similar therapeutic areas. Most of the dominant incumbents have developed valuable firm-specific competencies and market familiarity regarding certain types of disease. The competitive advantage conferred by such specific, in-depth knowledge could be strengthened with the ties between the firm’s drug representatives and the physicians specializing in certain therapeutic areas. The repeated visits of a pharmaceutical firm’s sales representatives with dedicated healthcare specialists may foster better rapport and increased credibility as the two sides get to capitalize on highly relevant pools of idiosyncratic, specialized knowledge. Good personal relationships with key decision makers in healthcare, reinforced with compelling sales presentations by the firm’s drug representatives, can become an inimitable co-specialized asset for the firm. For the dominant pharmaceutical firms, this can translate into considerable downstream leverage. It also provides an option for significant innovation rents to be extracted through target-specific alliances.
The leadership role of the established and profitable pharmaceutical firms in commercializing technological breakthroughs (pioneer drugs) and market breakthroughs (follow-on and me-too drugs) has been documented empirically in Sorescu et al. (2003). The findings show that such firms launch more new drugs, and that being backed up by such a firm boosts the value of newly released medications as measured by their net present value. The increase in market value is particularly pronounced in the case of pioneer drugs. Yet, as Sorescu’s et al. (2003) study had no controls for alliance activity, follow-up work could illuminate the share of drug innovations that large firms have sourced from partnerships. Such scrutiny can shed light on the contribution of strategic collaboration to both partners, essentially measuring the returns from alliance participation.
Alliance modes for large pharmaceutical firms. In a study of 889 strategic alliances between incumbent pharmaceutical firms and new biotech companies, Rothaermel (2001a) finds evidence that the large pharmaceutical firms prefer exploitation alliances (alliances that leverage their downstream assets, for example in the areas of clinical trials, FDA regulatory management, marketing, sales) to exploration alliances (alliances that build their upstream, technology-based competencies—e.g., discovery, R&D). The preference for exploitation alliances can be explained by efficiency considerations: exploitation alliances can leverage the already existing specialized downstream assets of large pharmaceutical firms, help them capture significant amounts of new revenue, as well as sustain their reputation as innovators, while limiting the amount of extra risk involved.
Alliance modes for biotech firms. Using a different nomenclature of alliance modes (upstream, horizontal, and downstream), Rothaermel and Deeds (2006) examine the new product output of 325 biotech firms participating in 2,226 alliances. Upstream alliances are defined as those with research universities or nonprofit institutions, when the goal is to tap into leading-edge scientific discoveries and develop them for commercial purposes; horizontal alliances are those with biotech peers or other technology ventures, whereby firms intend to combine complementary assets, realize economies of scale, and advance products to clinical trials or to the early stages of new drug commercialization; downstream alliances are those with established pharmaceutical firms, with the purpose of gaining access to manufacturing, regulatory, and marketing knowledge (Rothaermel and the Deeds 2006). Consequently, the three alliance modes differ by partner type, goals, and the nature of transferred knowledge.
The results of that study show that the biotech firms’ limited capability for alliance management is exhausted the fastest with upstream alliances, followed by horizontal, and then by downstream alliances, in this order. Upstream alliances, with their intrinsic transfer of tacit, complex, ambiguous knowledge of uncertain value, are the most taxing on a biotech firm. A firm’s potential to simultaneously engage in a number of upstream alliances is fairly low. In contrast, with downstream alliances, the drug formula has been discovered and the drug has been created, so the level of transferred knowledge ambiguity and complexity is at its lowest. Hence, downstream alliances are the least taxing on a firm’s alliance management capacity, and a firm can afford to handle a higher number of these. This suggests that a biotech firm can participate in a greater number of downstream alliances relative to upstream alliances. Horizontal alliances hold the middle ground—with them, the knowledge shared between the partners is more specific, application-oriented, and easier to assimilate compared to fundamental science, although it remains less structured than the knowledge necessary for commercialization. Hence, in this case the burden on a firm’s alliance management resources is lower compared to upstream alliances, but higher than that in downstream alliances.
Diminishing marginal returns in innovation output associated with high levels of alliance activity are found in all three alliance types, but the locations of the turning points differ. The tolerance threshold is the lowest when the firm has multiple upstream partners. It is higher with numerous horizontal partners, and is the highest in case of multiple downstream ones. Consequently, firms can afford to engage in more horizontal alliances compared to upstream ones and can manage an even greater number of downstream alliances (Rothaermel and Deeds 2006).
Selection of partners. In a study of 69 alliances between pharmaceutical and biotech companies, Lane and Lubatkin (1998) contend that the overall performance of an alliance is best explained not so much by the absolute absorptive capacity of the downstream partner (the pharmaceutical firm), but by the downstream partner’s relative absorptive capacity that is idiosyncratic to the partnership dyad and stems from similarities with the biotech partner’s: (a) basic knowledge—scientific, technical, and academic; (b) knowledge-processing systems; and (c) commercial objectives (the dominant logic in new product development). In other words, to be effective in interorganizational learning, the alliance partners must share similar theoretical and technical backgrounds, as well as have proximate organizational processes and common research communities. Such symbiotic partnerships would result in more successful innovation outcomes from the alliance (Lane and Lubatkin 1998).
Diminishing returns from excessive alliance activity. Simultaneous participation in multiple alliances can be conducive to prolific product development, but may incur significant transaction costs, manifested in increasing burden on the firm’s management. The heightened complexity and the specificity of information exchange with multiple partners, the need to monitor diverse relationships and to abide by multiple agreements can overextend the firm’s managerial capability. The scrutiny with which it selects new partners may wane, or the selection pool may shrink significantly once the most promising partners are already on board, rendering additional alliances less well-fitting or less productive. Diminishing marginal returns will eventually set in and may even transition to negative effects. The firm’s innovation performance may decline when the firm extends beyond a certain critical threshold of alliance connectivity.
Entering too many alliances opens up the venture to risks of coordination problems, mismanagement, opportunism, and expropriation. Yet, participation in too few can place the firm at a competitive disadvantage. The implied inverted-U effect of the number of alliances on a firm’s innovation performance has been supported in the empirical studies of Deeds and Hill (1996) and Rothaermel and Deeds (2006).
Network effects, experience effects and partner diversity. Exploring the alliance networks of a panel of 225 biotech firms in a dynamic setting, Powell et al. (1996) find that the majority of firms establish multiple alliances over time. The interfirm connectivity in the industry grows rapidly. Collaborative practices with diverse partners contribute to learning effects, which enhance firm growth. Hoang and Rothaermel (2005) propose that alliance experience obtained from a firm’s joint activities with a portfolio of diverse partners aids knowledge codification, brings about new intra- and interorganizational routines, and may even prompt the formation of new structures within the firm. The new routines or structures can be mutually beneficial: they may facilitate the functional cooperation between the partners, enhance the assimilation of new knowledge, and boost the information exchange between them. The locus of learning can be the development of alliance experience among dedicated alliance managers. Eventually, however, diminishing marginal effects from coordinating too many partnerships may set in.
The impact of experience obtained from the same set of a few long-term partners can be less effective. Having only a few partners leaves less room for organizational learning. The variation in new experiences will be limited. Complacency, process inertia, or functional rigidities between the partners may set in. The empirical results of Hoang and Rothaermel (2005), obtained from a study of 158 collaborative new product development projects, support these propositions. For the biotech firms in that study, the impact of diverse prior alliance experience has a positive but diminishing effect on the success probability of joint R&D projects, while the cumulative partner-specific alliance experience is rendered insignificant. The same pattern was subsequently demonstrated by Rothaermel and Deeds (2006) in another, larger sample.
Interestingly, these findings have failed to replicate with large pharmaceutical firms. Having a diverse alliance network does not exert a positive impact on their project success probabilities, suggesting some inherent deterrent in their harnessing of a rich experience from multiple alliances (Hoang and Rothaermel 2005). The authors’ explanation invokes an argument from organizational behavior: in the relatively small biotech firms, diverse alliance experiences can be easily concentrated in the hands of one key individual (often the founder or a top-level manager), who is also more motivated to learn from these experiences as alliances are particularly critical for the survival of small firms. In large firms, the management of multiple alliances is often distributed across the organization and is handled by different individuals. Such dispersion in the alliance experiences makes the cumulative benefits harder to materialize.Footnote 24
In general, the consensus in the academic literature is that for pharmaceutical and biotech firms alike, interfirm cooperation has a positive impact on innovation outcomes, particularly for a small number of alliance partners (Shan et al. 1994; Deeds and Hill 1996; Rothaermel 2001a). For biotech firms, access to public equity markets and a well-embedded network position exert additional positive effects on innovation outcomes (e.g., Shan et al. 1994).
The industry can benefit tremendously from a more fine-grained understanding of the rationale employed by different firms in their strategic choices regarding various forms of partnership activity. Insights about the evolution of alliances and assessment of the direct and indirect extra value they bestow on the partners can be rather informative for future strategic decisions. It will be illuminating to examine the interactions between different alliance types, to analyze the latent discrepancies in the partners’ interests, their reconciliation or resolution, and to study in detail the impact of relevant environmental, organizational, managerial, or structural factors. A better understanding of the potential synergies in the collaboration strategies of pharmaceutical and biotech firms, along with a clear recognition of the potential pitfalls, can guide firms toward systematic improvements in their partnering decisions for innovation—a win–win situation all around.
2.3.6 The Business of Drug Innovation from an Academic Perspective: Findings and Insights
Inventions are by default disruptive, which makes them relatively impenetrable to attempts to explain or predict. Yet, examining the process of drug innovation for pivot points that can introduce extra efficiencies, along with studying the various business models that arise in the industry are attractive areas for academic scrutiny. Detailed datasets present new opportunities for testing complex model frameworks; advanced estimation techniques enable the disentangling of interdependencies; the amassed conceptual understanding gives rise to reasonable data proxies and avenues for data augmentation; previously arcane mechanisms and procedures are made more transparent through case studies and open discourse.
Most of the academic papers cited in this chapter have focused on capturing the drivers behind successful innovation outcomes while accounting for factors germane to the pharmaceutical industry. Now that the readers are more familiar with the complex landscape in the industry, we will briefly discuss other academic findings illuminating additional aspects of the drug innovation process. Of course, we are limited by space considerations so this review will be somewhat sketchy, but we hope that even a brief exposition will incite the curiosity of more researchers to focus on this domain. Readers interested in a good summary of strategic marketing decision models in the pharmaceutical industry are referred to the detailed compilation by Shankar (2008).
2.3.6.1 Risk-Taking + Investment in R&D + Good Luck = Business Viability and Market Dominance
The sources of today’s strategic and performance heterogeneity in the pharmaceutical industry were examined by Lee (2003). In a historical study on the development trajectories of the US pharmaceutical firms from 1920 to 1960, he traces the current powerhouses back to their origins, and most importantly, to the decision to embrace large-scale manufacturing of antibiotics in the 1940s despite the uncertainties prevalent at the time. Considerable investments in R&D made this possible, although the risks were substantial. Also, those early innovators were able to charge premium prices. The most successful of them have managed to sustain their dominance in drug innovation by investing the market proceeds into hiring biologists and scientists at an increasing rate, which ultimately enabled them to branch away from antibiotics (Lee 2003).
Other pharmaceutical firms (imitators) chose not to commit considerable resources to R&D and survived for a while by selling existing, known products at low prices, thus remaining peripheral to drug innovation. The initial choice of product strategy, perhaps influenced by the risk adversity of the firms’ management teams at the time, has acquired irreversible momentum over the years, persistently widening the gap between these two groups (Lee 2003). A third group of less successful early innovators, constrained by modest market returns, could not sustain the high levels of R&D investment needed for risky innovation, and have either morphed into imitators or vanished altogether. This study demonstrates the stickiness in early strategic choices, as they get reinforced and perpetuated by their own consequences.
2.3.6.2 The Importance of Investing in Own R&D
Synergies between biotech firms and large pharmaceutical companies seem natural given their co-specialized assets. Indeed, the multiple licensing agreements and the numerous alliances in existence nowadays can certainly attest to the significant expected benefits from such partnerships. But if complementarity based on co-specialized assets prevails in the industry, the ensuing division of labor should have already eradicated the need of large pharmaceutical firms to invest in in-house R&D. After all, they could source numerous new projects from symbiotic relationships with research-focused firms (e.g., biotech ones). Yet, no such development has materialized. Private firms recognize the importance of investing in R&D bases of their own so that they can build and maintain the skills, the knowledge, and the organizational routines to identify and utilize the research output of others (Cockburn and Henderson 1998). Investing in leading edge research to stay current with the advancements of open science would also enhance the firms’ absorptive capacity (Cohen and Levintal 1989, 1990).
Firms that underestimate the importance of conducting internal R&D would not only curtail their own capability to originate novel drugs but may also relinquish their ability to benefit from the innovations of others. The theoretical and practical knowledge contained in open science can be adopted more quickly and more easily by firms which have the capacity to internalize it, while adjusting it to their own needs and goals. Virtually no firm in this high-paced industry can afford to sit on the sidelines regarding R&D activities—if it did, it would essentially disqualify itself from the race to market. Therefore, investment in own R&D keeps pharmaceutical firms at the forefront of technological advancements and facilitates the assimilation of know-how obtained through partnerships.
Even the largest pharmaceutical firms have limited financial, technological, organizational, managerial, production, and commercialization capacities. To partner up with other ventures, they need internally cultivated screening capabilities to assess the innovation potential of possible partners before they commit to joining them in collaboration. Conducting R&D in-house can strengthen the firm’s ability to recognize promising projects initiated by others. It can also be a strong and favorable signal to the stock market, reasserting the firm’s aptitude to generate innovation independently of others.
But there could be another, less apparent strategic reason behind incumbents’ reluctance to curtail investments in own R&D. Gans and Stern (2000) advance the argument that there are conditions under which incumbents may consider biotech firms’ R&D a strategic substitute for their own research, rather than a complementary asset they can easily acquire. In the presence of a market for ideas, incumbents obtain bargaining power if they develop and maintain cutting-edge R&D capabilities of their own. For the biotech firms, incumbents’ own R&D constitutes a credible threat of potential competition, particularly if information spillovers can preempt innovation outcomes. In case commercialization is costless and can be handled by biotech firms with no partner participation (i.e., in the absence of a need to engage external platforms to market), own R&D capacity assumes the role of leverage for the large pharmaceutical firms and can raise the share of the innovation rents they capture in strategic partnerships. Gans and Stern (2000) show analytically that in a dynamic bargaining game, incumbents’ ability to undertake imitative R&D acts as a negative market externality that can weaken the entrant’s position.
2.3.6.3 First or Late Movers’ Advantage?
In the neck-breaking race to market, late entrants are generally believed to be placed at a disadvantage. They miss out on a period of uncontested market monopoly and have to fight their way into an existing competitive market. Oftentimes, late entrants need to disrupt established loyalties and displace prescription regimens, which can be rather difficult.
Notably, being a late entrant can have its advantages, too. First, late entrants can gain by monitoring the marketing strategy of the pioneer brand as they learn from its deficiencies. Second, they can benefit from the extra time to improve or differentiate their formulation. Distinguishing between innovative and non-innovative late entrants, Shankar et al. (1998, 1999) set out to examine if innovative late movers may have a competitive advantage. For conceptual consistency and to align the terminology in these studies with the exposition in Sect. 2.2.5, hereafter we equate follow-on drugs and me-too drugs to innovative late movers and non-innovative late movers, respectively.
Being the first of its kind, the pioneer drug is faced with the task of creating awareness for the entire therapeutic class. In contrast, follow-on brands enter an established market. They face a different hurdle: to build brand awareness and differentiate themselves, which might not be too difficult if their superiority is apparent. Me-too drugs’ lack of a clear advantage though, places them in the least-favorable position regarding market potential and marketing effectiveness.
Using longitudinal data from 13 brands in two categories of ethical drugs for chronic conditions, Shankar et al. (1998) find that follow-on drugs, typically offering an improvement over the pioneer drug, enjoy an advantage over both the pioneer and the me-too brands. Presumably, follow-on drugs offer sufficient extra value—i.e., they are either superior in quality (e.g., offer greater regimen convenience, higher efficacy, or reduced side effects), or can sustain a lower price point. These distinctions let them expand the market further, while riding on the coattails of the pioneer brand’s awareness.
Due to their competitive strengths in positioning, follow-on brands are more effective than the pioneer at converting trials into repeat purchases—a transition that is particularly relevant for the analysis of chronic condition treatments, as in Shankar et al. (1998). More repeat purchases translate into higher sales growth for the follow-on brands. Consequently, they can eventually outsell and overtake the pioneer by slowing its diffusion, while remaining relatively unaffected by other competitors’ diffusion and marketing efforts. In contrast, me-too drugs, lacking a clear point of differentiation from the pioneer, are less effective with their marketing spending and attain lower repeat purchase rates compared to the pioneer and the follow-on brands.
Favorable market conditions for innovative follow-on brands will depend on the timing of their late entry relative to the stages of the product life cycle (PLC). If the follow-on brands enter in the growth stage of the PLC, they can benefit from a strong market response. In contrast, market entry in the maturity stage will face an established competitive market. Even superior late entrants may end up with limited growth prospects as market entry during maturity shortens the proverbial window of opportunity for these brands and pits them against scores of entrenched rivals.
Analyzing sales data and marketing expenditure from 29 brands in six prescription categories, Shankar et al. (1999) find that the market response to total marketing spending by brands in the same therapeutic class steadily declines over the PLC. It is the highest at the time of pioneer entry, then declines through the growth stage and reaches its lowest point in the maturity stage. Market expansion is confined to the early stages of the PLC, which is also when marketing efforts are most effective. The market’s reaction to brands’ quality, however, follows an inverted U-pattern—it is the highest during the growth stage (when perceived drug improvements can expand the market most effectively given the benchmark set by the pioneer), but is relatively lower in the maturity stage. Moreover, competitor diffusion affects rivals differently: it hurts the pioneer, has no effect on growth-stage entrants, and may even help maturity-stage entrants.
In a model that focuses on competitor reactions in the case of market entry, Shankar (1999) shows that an incumbent will tend to accommodate a new entrant if the entrant is: (a) more experienced (the entrant’s marketing is likely to be more effective); (b) entering with a strategy of high marketing spending (an aggressive response by the incumbent can trigger an advertising war), or (c) when the incumbent and the entrant face each other off in multiple markets (the incumbent is exposed to the hazard of retaliatory attacks in those other markets). In addition, small incumbents have limited ability to react, which is recognized by entrants as absence of competitive threats. An entrant would spend more on marketing (advertising and sales force effort) if it is a large firm and if the new drug is of a higher quality (Shankar 1999). Note that these results are also consistent with the arguments advanced in Sect. 2.3.5 to explain the expediency of downstream alliances for small biotech firms seeking the market leverage conferred by large partners.
2.3.6.4 Market Entry in the Presence of Pent-up Demand
If the new drug is indeed so revolutionary that no effective alternative has been available prior to its release, there might be a vast pent-up demand at the time of market launch. With such drugs, an atypical diffusion pattern can occur. Patients diagnosed with severe symptoms will know about the imminent launch and will be eagerly anticipating it. In this case, sales may soar sharply upon market entry, then embark on a steep decline as the wave of critical patients complete their treatment (Vakratsas and Kolsarici 2008). If the condition can be cleared relatively fast and there is no need for long-term treatment, repeat purchases will fail to materialize. However, a second market of less-intense demand can emerge, composed of the purchases made by newly diagnosed or mild case patients. The drug adoption in this second segment may evolve at a much lower rate, with sales growing gradually over time before a slow decline sets in.
Vakratsas and Kolsarici (2008) find evidence of such bimodality in the market adoption pattern for a lifestyle-related drug. The authors posit that such a pattern can stem from an underlying spectrum of treatment urgency. If need intensity can range from severe to mild, a dual-market diffusion model with a switching regime, which is a version of the Generalized Bass Model, is warranted. Differences in need intensity can essentially create two segments, distinguished by their market potential and by their ability to postpone treatment in anticipation of follow-on drugs of enhanced value.
Subsequent research can systematically examine the market dynamics upon entry of follow-on, me-too, and generic drugs in the presence of differential effects associated with idiosyncratic class characteristics. For example, the gravity and the prognosis of the disease, or the intensity and duration of its symptoms may moderate the repeat-purchase behavior of the market, its price elasticity, or the tolerance for potential side effects, systematically changing the diffusion patterns of pioneers and late entrants alike.
Diseases can range from acute to mild, from genetic to lifestyle-induced, and may run the gamut from life-threatening conditions to brief discomforts. Some are highly contagious, others are exceedingly rare. Some can be cleared once and for all, others occur intermittently, and still others become chronic. Related symptoms can also vary from debilitating to hardly detectable. Important distinctions in market behavior may be uncovered along these dimensions, and future research can elucidate specific diffusion patterns linked to disease type, severity, and trajectory.
2.3.6.5 Factors That Affect the Market Diffusion of a New Drug
Although this volume contains another dedicated chapter on the topic of market diffusion, a brief recount of some notable findings seems warranted here to wrap up our review of pharmaceutical innovation. Rao and Yamada (1988) and Hahn et al. (1994) have developed repeat purchase diffusion models in which drug prescriptions are a function of the firm’s marketing efforts (detailing to physicians) and word-of-mouth effects. As the informative role of detailing assumes higher significance with innovative drugs, as well as with drugs that address a broader spectrum of ailments, the effectiveness of detailing is shown to increase for these drug types (Rao and Yamada 1988). The effects of word-of-mouth vary by the type of prescribing physicians and are more pronounced when specialists are the source.
Empirically analyzing the market diffusion of 21 ethical drugs in seven therapeutic classes, Hahn et al. (1994) find that a brand’s promotion effectiveness and the corresponding trial rates are linked primarily to the brand’s efficacy and dosage, whereas the repeat purchase rate (indicator of the brand’s long-term market share) is affected by the drug’s side effects and dosage. Greater word-of-mouth effects are found with drugs for acute diseases.
Ding and Eliashberg (2008) examine the influences of physicians and patients on the market adoption of drugs by accounting for dyadic decision-making. Using prescription probability matrices for categories with multiple new brand offerings, the authors find that both patients and physicians can impact the prescription decisions for new drugs, but the effects would vary with symptom intensity. In case of serious symptoms, the patients’ influence is limited, and the effect of brands’ marketing activities is diminished.
2.4 Trends in Pharmaceutical Innovation
Fewer new drugs—symptom of declining innovation productivity? Despite the rapidly escalating R&D budgets in the pharmaceutical industry (Fig. 2.3), there seems to be a decline in the number of approved New Molecular Entities (NMEs), a trend visualized in Fig. 2.4a. The 2010 Pharmaceutical R&D Factbook, compiled by CMR International (Thomson Reuters), reports that in 2009, new drugs introduced within the last 5 years have accounted for less than 7 % of industry sales. Meanwhile, the number of experimental drug projects terminated in the final Phase 3 of clinical development has doubled in the period 2007–2009 compared to 2004–2006.
The decline in revenue from new medications seems particularly puzzling given the extraordinary biomedical and technological advances occurring in recent years: the decoding of the human genome, the transition to molecular biology and biotechnology, the development of advanced R&D techniques (e.g., high throughput screening, combinatorial chemistry, bioinformatics, rational drug design), all of which were supposed to galvanize the process of drug discovery and boost its rate of success.
Noting the dissonance between the ever-increasing R&D costs and the declining innovation outputs, analysts (e.g., Cockburn 2007) have raised the question of a possible productivity crisis in the pharmaceutical industry. The reasons for the presumed productivity crisis can be sought in the following factors noted by Cockburn (2007): (a) the vigorous drug research and successful market introductions over the last couple of decades have already created sufficiently good solutions to the “easy” medical problems, leaving the more challenging and complex diseases (e.g., cancer, HIV/AIDS, obesity, Alzheimer’s, Parkinson’s, diabetes) to become the focus of most firms’ current R&D efforts; (b) the industry appears to have failed to make the necessary investments in human and institutional capacity to quickly turn important biological discoveries into drugs and medical devices; (c) the existing regulatory review process and its standards are not well adapted to the new research technologies; (d) the drug companies are reluctant to bring forward products with low sales potential; (e) firms seem inclined to search for blockbuster drugs, and thus, prefer to seek out candidates with novel action mechanisms and large market potential, which can be more expensive to develop or more likely to fail; (f) the current extent of collaboration in innovation between drug companies could be insufficient. Changes in firms’ organizational objectives and strategies, supported by adequate modifications in the respective regulatory policies, can help overcome many of these roadblocks.
However, a more positive outlook challenges the notion of declining productivity in drug innovation by questioning the employed metrics. Properly adjusted cumulative measures (e.g., ones accounting for the increasing quality of follow-on drugs) can be a better yardstick for gauging innovative output than the simple counts of new branded drugs.
It is conceivable that in the absence of great potential for blockbuster drugs, the industry’s R&D spending is directed more toward enhancing drug efficacy and safety, or improving the delivery mechanisms of already existing treatments. Therefore, the relevant innovation output might be better assessed not solely by the total number of new drugs qualified as breakthrough innovations, but also by the cumulative value of incremental quality improvements—e.g., by accounting for the relatively minor but frequent drug modifications that create extra customer value (Cockburn 2007). The ultimate measure of productivity seems to require consideration of both drug quality and total impact. Generating fewer successful treatments that are highly efficacious and targeted toward large patient groups might be of greater social and economic value than launching a large number of undifferentiated treatments in already crowded therapeutic categories.
The question of whether the pharmaceutical industry is truly in a productivity crisis, or simply going through a slow growth phase (marked by dramatic shifts toward new knowledge and technologies), is further compounded by the significant delay between R&D spending and the actual drug commercialization. This delay makes the assessment of the relationship between R&D expenses and firm productivity rather difficult. Besides, while basic research performed in government-funded research labs may not result in patentable drugs, it can boost the applied research in the private sector, from which the majority of drug patents originate. The deferred but significant benefits of R&D spillovers from the public sector make the attribution of R&D outcomes in the private sector increasingly difficult. For all these reasons, any assessment of productivity based on simple counts of regulatory approvals is bound to remain a rather crude proxy for the true pharmaceutical output (Cockburn 2007).
Emphasis on more incremental innovations. The competitive dynamics following a major patent loss might be steering the pharmaceutical industry away from its one-of-a-kind, blockbuster orientation and more toward incremental, follow-on innovations. There is a sound economic rationale in the pharmaceutical firms’ endeavors to capitalize on their specialized technical knowledge and other existing assets. Most large pharmaceutical firms have invested in vast sales forces. As most of these firms are focused on certain therapeutic categories, their drug representatives would have good contacts and rapport with the physicians specializing in the treatment of a corresponding set of disease types. If the firm has new drugs forthcoming in the same category, the established contacts represent a co-specialized downstream asset that can be leveraged effectively even after the expiry of existing patents.
Besides, incremental drug innovations are easier to generate. Because of their structural proximity to approved drugs, there is a lower risk of failure. Incremental drugs are also more amenable to preplanning than blockbuster drugs. The associated cannibalization hazard or the threat of splintering the market might be more than offset by process efficiencies, reduced uncertainty, and desirable continuities in the product pipeline. By maintaining a stack of incrementally improved drugs in their product pipeline, and by releasing these follow-on drugs on a schedule timed around the patent expiration dates of older drugs, a firm can simply switch its manufacturing and marketing support to the next patent-protected successor drug, with little need for extra costs in production or distribution. A sustainable and smooth flow of new products, brought out by a robust strategy of sequential incremental innovations, can overcome the uncertainties associated with the pursuit of blockbuster drugs and generate steady streams of cash instead.
Influx of generic alternatives. Not only are fewer drugs introduced to market these days but there is also a decline in the sales of new drugs launched within the last 5 years at the expense of a gain in the sales of generics (Fig. 2.4b). The market share of generics has risen from 49 % in 2000 to 78 % in 2010. In fact, the IMS Institute estimates that 80 cents of every dollar spent on drugs in developed markets is spent on generics. Consumer spending on branded and unbranded generics has risen by 4.5 % and 21.7 %, respectively, while spending on branded drugs has declined by 0.7 % in 2010, indicating a shift to lower-cost alternatives.
The competitive landscape in the pharmaceutical industry faces ample changes due to unprecedented numbers of patents coming to the end of their duration. As more than 80 % of the brand prescription volume is replaced by generics within 6 months of patent expiration, the industry seems poised for a series of shocks triggered by a slew of upcoming patent expirations.Footnote 25
Customized drugs. The development of targeted drugs for niche markets, individually designed drugs, or combination drugs (e.g., drugs targeting symptoms or conditions that tend to appear in tandem), is another promising tendency addressing patient needs on a microlevel.Footnote 26 Advancements in the life sciences and particularly, the decoding of the human genome, along with the versatile tools of molecular design and biotechnology, offer substantial promise that custom-built therapies will be technically feasible in the not-too-distant future. Still, customized drugs may face considerable regulatory and economic hurdles.
There is potential in the smaller markets. A persistent and salient tendency is that large pharmaceutical markets continue to attract significantly more innovation (Acemoglu and Linn 2004). Economic as well as ethical reasons can explain why R&D spending in drug innovation is prioritized for conditions and ailments affecting large numbers of people (e.g., depression, high cholesterol, diabetes, hypertension, ulcers). Because attractive markets are also likely to be populated with multiple treatment alternatives, FDA scrutiny may tighten for new approvals. New drugs can face steeper hurdles to prove they are market-worthy. In this regard, experts have called for policy regulations that make small markets more appealing, e.g., by reducing the time and the cost of regulatory reviews, maximizing the access to fundamental science and its findings, or encouraging cooperation and collaboration within the industry as a way of supporting the efforts of firms venturing into small markets.
2.5 Conclusions and Directions for Future Research
Drug innovation is not only a multibillion dollar business but also a science- and technology-driven process with exceptionally high stakes that often transcend pure commercial interests. It is a topic that finds itself in the focus of increasing attention from researchers in economics, marketing, strategy, management, organizational theory, and social sciences alike. This thriving interest is fuelled by the unique and challenging issues the industry is facing, along with the ever-shifting opportunities and constraints associated with it. The fascination of the public with the inner workings of the pharmaceutical industry is also growing, and so is the media attention to it.
While new product development always carries a dose of risk, the exogenous locus of control in the approval of new drugs heightens the uncertainties associated with R&D spending in the pharmaceutical industry and introduces a major hurdle on a drug’s route to market. Academic researchers should be well aware of the contingencies in drug innovation and properly account for them in empirical work, lest they confound effects caused by process-related externalities with market-related factors that might be more pertinent in other industries. Recognition of the intricacies in the drug innovation process can assist with the interpretation of new empirical results or alert us to specific patterns and dependencies germane to this industry.
The objectives of this chapter were to synthesize some of the existing knowledge about organizational and strategic issues in drug innovation, and to elucidate the prevalent practices, organizational forms, modes of collaboration, and patterns of interdependence that are relevant for its success. Ideally, this summary will give impetus to further research efforts and pave the way toward a more systematic understanding of the determinants and the boundary conditions related to effective and efficient drug innovation.
It is only appropriate to conclude this overview with directions and suggestions for future research. A proposed stylized framework for future study and analysis is presented in Fig. 2.5. Still, while it summarizes the drivers and decisions involved in the process of drug innovation as discussed in this chapter, it is not meant to visualize all plausible interdependencies.
A sound starting point for future examination might be to come up with an appropriate metric for innovation outcomes. Variations in the relevant measures based on differences in total generated value might need to be addressed and resolved. For example, it might be argued that innovation measures can vary across therapeutic categories, or even across disease types (e.g., treatments might be differentially weighed based on indications for acute, chronic, or life-threatening prognosis, infectious disease profiles, symptom severity, and adjusted for side effects, regimen and administration route issues, or other nonmonetary costs).
Besides, there might be a gain in identifying appropriate outcome measures for different firm types based on their likely complementary roles in the drug innovation process—e.g., public vs. private firms, or vertically integrated (pharma) vs. discovery-oriented (biotech) firms. Perhaps researchers can try to develop a more detailed inventory of measures for drug innovation, enabling a more accurate value assessment and sharper attribution of market outputs, performance, and impact. Developing guidelines for the appropriate unit transformations might be needed before a universal scale for gauging innovation outcomes can be deployed.
The already complex and heavily regulated business of drug innovation is under considerable pressures that seem hard to reconcile. Strategic choices made under massive environmental strains or in brief windows of opportunity might steer firms toward greater diversification or specialization. Firms may strive to attain process efficiencies from greater economies of scale (e.g., large volumes of production) or from greater economies of scope (e.g., serving niche markets with custom treatments). Conflicting tensions are already afoot and firms often undertake organizational restructuring to modify the scale, the scope, or the focus of their operations. Deliberate or involuntary, such transitions may have considerable consequences for the firm, the duration of its innovation process, its likelihood for success, or its cost and revenue models.
Furthermore, the attendant organizational changes may affect firms’ sales and stock market performance, creating a dynamic, evolving ecosystem that would be especially worthy of detailed analysis and possibly, amenable to optimization. Examining the exceptions to the prevalent regularities, in conjunction with studying the environmental, technological, strategic, or structural factors that enable them to emerge and persist, can be illuminating. For example, if specialization can be more closely associated with economies of scale on the supply side while diversification is related to economies of scope on the demand side, then variations in the firms’ respective co-specialized assets (e.g., in drug discovery, in development and manufacturing, or in marketing and distribution) might differentially affect the attainable benefits from specialization and diversification, and consequently, the strategic orientation of firms.
Judicious selection of in-licensed products and technologies may increase firms’ innovation outputs, lead to greater market power, or create favorable experience and reputation effects. Such positive developments can make a firm more attractive as a potential partner. There is evidence that in-licensing begets more in-licensing. As it starts realizing increasing value from its investments, the firm itself may become more confident and proactive in seeking out additional collaboration arrangements. However, when inputs from multiple sources must be coordinated, potential downsides are overreliance on outside ideas and creative talent as well as the risk of overextending the firm’s integrative and managerial capacity. A closer scrutiny of licensing dynamics will make an interesting topic for empirical research.
Researchers can also examine the impact of excessive in-licensing on the future prospects of the firm. How likely is it that a firm may become an easy prey for a takeover bid if most of its products are being sourced from elsewhere? What are the precipitating factors for acquisition compared to other forms of collaboration in the pharmaceutical industry? What are the differential effects of acquisition on the fate of the acquired firm’s pipeline of drug candidates? Is there evidence that the rate of FDA approvals for two firms may undergo systematic changes when one gets acquired by the other, and what inferences can be made about the tacit knowledge and the quality of these firms’ proprietary R&D before the acquisition? All these questions seem worthy of examination.
The decision to engage in a specific mode of collaboration, the factors behind the choice of a partner, the ultimate impact of that partnership on the individual firms’ innovation and market outcomes, as well as the market performance of the drug(s) that are central to the partnership would constitute another fertile area for exploration. Also, it will be interesting to find out what makes a firm appealing as an alliance partner, how alliances evolve, and how they interact within more complex networks where unintended knowledge spillovers can occur. Estimating the costs of an alliance, teasing out its total added value, and understanding how this added value is created and appropriated will also be illuminating.
Future research could also look into the implications of using fundamental knowledge generated by nonprofit research institutions on the secrecy and proprietary rights demanded by private firms, if they are joined in an alliance. The signaling value on industry participants of organizational changes enacted through partnerships such as licensing, co-marketing agreements, alliances, mergers, or acquisitions could constitute another fecund area of study. Elucidating the most common pathway firms follow with the different modes of collaboration, as well as pinpointing directions amenable to optimization, can be worthwhile.
More research is needed to identify the environmental, structural, and strategic determinants that can affect drug innovation outcomes. What are the differential effects associated with firm size? How do the latest state-of-the-art technologies for drug design and discovery affect innovation productivity, FDA approval rates, sales performance, or the firms’ market valuation? Are there particular technology-related bottlenecks to be resolved or underutilized process synergies to be considered from an organizational or managerial perspective?
Another line of inquiry could examine if the open science generated by the public sector (i.e., free access to the latest advancements in fundamental biomedical knowledge) affects large and small firms similarly, or whether large firms may have an advantage because of inherently greater absorption capacity. Is it the firms with a more narrow functional focus or the vertically integrated firms, the more specialized ones or those with more diversified project portfolios that are poised to benefit more from open science?
Disentangling the impact of firm-level factors contributing to the sales performance of a new drug is another area that researchers could explore. For example, how does sales performance vary with prior experience in the therapeutic class or category, changes in the marketing budget, the size of the sales force, or embeddedness in vast networks of professional contacts? How does technological experience affect new drug sales for firms with established market presence in certain categories, and what are the underpinnings of these effects? Can the sales effects be attributed to measurable improvements in drug quality or efficacy, or are they largely perceptual, derived from other signals about organizational knowledge and expertise? If the effects are mostly perceptual, does the primary locus of the perceived effect lie with the physicians, the pharmacists, the health insurance companies, or with the patients?
The world is becoming an increasingly more compact place, presenting ample opportunities for dispersed innovation and expedient collaboration. This is particularly evident to global pharmaceutical companies whose subsidiaries and research centers are already spread around the world. The effectiveness and efficiencies of different models of international collaboration in innovation, the impact of policies and laws governing intellectual property across countries, as well as the influence of local cultures and entrepreneurial climate on innovation outcomes or on alliance proclivity can be interesting to explore, too.
In summary, we believe there is an abundance of issues and themes that merit considerable research attention in the field of pharmaceutical innovation. We hope this compilation will be a useful platform for many enthusiastic researchers to join in and contribute to the burgeoning stream of studies related to the discovery and development of efficacious novel drugs.
Notes
- 1.
The National Institutes of Health (NIH), part of the U.S. Department of Health and Human Services, is the nation’s leading medical research agency. It is also the largest source of funding for medical research in the world. More than 80 % of the NIH’s funding is awarded through about 50,000 competitive grants to more than 325,000 researchers at over 3,000 universities, medical schools, and other research institutions across the USA (Source: NIH website, www.nih.gov).
- 2.
It is hardly surprising that the innovation pipeline of the US pharmaceutical firms is primarily composed of drugs corresponding to the therapeutic categories with the largest sales in the USA: oncologics ($22.3 billion), respiratory agents ($19.3 billion), lipid regulators ($18.8 billion), antidiabetes ($16.9 billion), and antipsychotics ($16.1 billion). Sources: IMS Institute for Healthcare Informatics, Adis R&D Insight Database, PhRMA Pharmaceutical Industry Profile 2011.
- 3.
Some estimates indicate that 64 % of all research on new drugs approved in the last 10 years was done in the USA, making it the most relevant target of scrutiny.
- 4.
Two key events have come to be recognized as critical for the revolutionary union of genetics with biotechnology. One was the 1953 discovery of the structure of DNA by James D. Watson and Francis Crick, and the other was the 1973 discovery by Stanley N. Cohen and Herbert Boyer of a recombinant DNA (rDNA) technique by which a section of DNA from one organism (e.g., bacterium) could be transferred into the DNA of another, so that the latter could be induced to produce a specific protein. Popularly referred to as genetic engineering, this technique has come to define the foundations of modern biotechnology.
- 5.
If the medical drugs are created by biological processes, rather than being chemically synthesized, they are referred to as biopharmaceuticals or biologics. Recombinant DNA technology (rDNA), whereby scientists are bringing together genetic material from multiple sources to create sequences that may not otherwise be found in biological organisms (e.g., joining plant DNA with bacterial DNA), is often the technology used to derive them. Pioneered by Genentech, this is the main method for obtaining insulin nowadays, having replaced the animal sources previously used in the process. The technology has found many other applications—e.g., in HIV diagnosis, for the creation of growth hormones or blood-clotting proteins.
- 6.
In vitro tests are experiments conducted in the lab, usually carried out in test tubes and beakers. In vivo studies are those in living cell cultures and experimental animals, conducted to gauge the effects of the drug candidate on the metabolism and the systems of intact living organisms.
- 7.
The IND application outlines the results of the preclinical work, the candidate drug’s chemical structure and how it is thought to work in the body, a listing of the expected side effects, and information about the manufacturing process. The IND also contains a detailed test plan specifying how, where, and by whom the clinical studies will be performed.
- 8.
This was the case with Vioxx®, the anti-inflammatory drug developed by Merck, which was voluntarily taken off the market in 2004 because of findings about elevated risks for a heart attack or stroke. The unexpected risks were unveiled during a follow-up study designed to test the efficacy of its active ingredient for the prevention of colorectal cancer (Cockburn 2007).
- 9.
For at least one therapeutic category (antibiotics), there is definite value in the presence of more drug diversity per se. It is well known that bacteria mutate and can become resistant to the most common existing drugs, necessitating a wide variety of medication choices.
- 10.
There is an ongoing argument about raising the standards for late entrants so that a demonstration of performance superiority, or at least, non-inferiority compared to existing therapies is demanded before obtaining market approval (Angell 2004; Hollis 2004). However, such changes might considerably complicate and prolong the development process, and are likely to be fervently opposed by the industry. Essentially, adopting them will place the innovation race contenders in a position to chase after a moving target. The front-runner will be the only exception as it is competing against a placebo, or in some cases, against the conventional treatment.
- 11.
Although such a range of variation seems perfectly acceptable for many treatments and conditions, there are situations where severe adverse effects can occur if the drug concentrations exceed or fall below those ruled as safe and efficacious—for instance, when a precise calibration of a process is necessary (e.g., in the treatment of seizures, for regulating blood pressure, blood clotting and blood thinning, heart rhythm, thyroid activity). FDA will find it necessary to apply much stricter standards in these cases, which can explain its reluctance to publicly acknowledge the often-cited 80–125 % bioequivalence range.
- 12.
Pfizer discovered the key compound in what was to become the blockbuster hit Viagra® during Phase 1 of clinical trials for two totally different indications—high blood pressure and ischemic heart disease. When its efficacy for erectile dysfunction became apparent, Pfizer was quick to change research directions and made Viagra® one of the most successful drugs in history.
- 13.
For instance, Hoffmann-La Roche’s Pharma division has established a department called International Project Management. It is entrusted with the coordination of a resource pool of about 50 highly qualified project managers overseeing the firm’s dispersed R&D sites around the world, with the purpose of maintaining quality standards and ensuring consistency in procedures (Gassmann and von Zedtwitz 1998). Upon project completion, these project managers can be immediately reassigned to projects in other locations, thus enacting fast and seamless transfer of managerial experience, knowledge, and expertise within the firm.
- 14.
Nowadays, the US biotech firms account for 80 % of the world’s R&D investment in biotechnology. The US culture of encouraging entrepreneurship and innovation has been conducive to the creation of such firms. This tendency can be traced back to several noteworthy factors identified in Cockburn and Henderson (2001a): (a) strong intellectual property protection; (b) favorable financial climate with robust and vigorous venture capital industry (both of which are relatively uncertain in many European countries); (c) regulatory climate that is not restrictive of genetic experimentation; (d) strong scientific and medical establishment with developed infrastructure and access to the latest technologies to supplement the limited resources of fledging small firms; and (e) the existence of strong and facilitating academic and cultural norms that permit the rapid translation of academic results from the originating institutions (often in the public domain) to the private sector, with commercial purposes.
- 15.
In an exploratory study of biotech firms (Khulji et al. 2006), their managers—mostly scientists-turned-entrepreneurs—reveal the conflicting tensions they most frequently grapple with: the desire to retain leverage, control, and confidentiality by keeping the invention close to their chest for as long as they can, and the realization that to advance and be effective, they need to collaborate and attract partners who have greater access to capital, more business contacts, better organizational capabilities, and understanding of marketplace dynamics. Trust issues, insufficient alignment of interests, and coordination problems in asset deployment are some of the areas that introduce challenges in such arrangements.
- 16.
For example, the eradication of the smallpox virus was made possible, thanks to the efforts of the World Health Organization, which mounted a global vaccination program.
- 17.
For example, a firm that has serendipitously made a discovery in a non-focal area can partner up with a company whose research focus matches the discovery in question so that they can jointly take the new drug to market.
- 18.
Prior to its acquisition by Roche in 2009, Genentech, the company considered to be the first biotech firm, remained focused almost exclusively on large molecules, using partnerships to augment its core research and to increase its access to capital. Other companies have also chosen to restrict their R&D to few carefully selected areas, e.g., Biogen Idec Inc. is specializing in drugs for neurological disorders, autoimmune disorders, and cancer.
- 19.
In fact, by the late 1990s, the large pharmaceutical firms were marketing seven out of the ten top-selling biotech drugs, although none of the drugs had been developed by them. Those seven drugs accounted for two-thirds of the revenues from the top ten drugs at the time (Rothaermel 2001b). In 2000, more than half of the drugs in the pipelines of Schering-Plough, Bristol-Myers Squibb, and Johnson and Johnson were products of in-licensing agreements (Simonet 2002).
- 20.
The first firm to apply biotechnology in drug discovery was Genentech. Using recombinant DNA technology, it created synthetic human insulin, heralded as the first-ever approved genetically engineered therapeutic product. But Genentech didn’t take that revolutionary product to market. Instead, it licensed Eli Lilly to navigate the FDA approval process.
- 21.
A recent example for an international alliance of large pharmaceutical firms is that of Boehringer-Ingelheim and Pfizer for the joint manufacturing and marketing of Spiriva®, a treatment for chronic obstructive pulmonary disease.
- 22.
In 2009, Schering-Plough got acquired by Merck, while American Home Products was taken over by Pfizer.
- 23.
The onset of extensive interfirm cooperative arrangements in the pharmaceutical industry in the early 1980s coincides with the time of its sweeping transition from chemical to biological compounds, which had also triggered the emergence of biotech firms in the late 1970s. The confluence of several critical factors created favorable conditions that fostered such cooperation: the Supreme Court passed a decision that live forms could be patented, the Patent and Trademark Act allowed universities to patent discoveries funded with federal dollars, and the first biotech firm, Genentech, went through a very successful IPO, drawing the industry’s attention to the creative potential of such firms (Hoang and Rothaermel 2005). The trend toward strategic alliances got an extra boost in the 1990s in the wake of several biotech firms’ stock market failures that underscored the advantages of partnering with large pharmaceutical firms. Around the same time, drastic healthcare reforms curtailed the growth potential of large pharmaceutical firms and sent them scrambling for faster innovation. This precipitated the need for cooperation on their part.
- 24.
Eli Lilly has established a dedicated function called Office of Alliance Management to serve as an “integrator, intermediary, and catalyst for best practice performance” (Hoang and Rothaermel 2005). This move is consistent with the suggested need for intraorganizational streamlining of diverse alliance experiences.
- 25.
As reported by the IMS Institute for Healthcare Informatics, in 2009–2010 the combined worth of branded drugs set to face generic market competition due to patent loss was estimated as $32.1 billion (an all-time high). Major blockbusters such as Lipitor®, Plavix®, Zyprexa®, and Levaquin®—which have accounted for more than 93 million prescriptions in 2010 and generated a total of $17 billion in sales—may soon lose market exclusivity in the USA. This trend appears to hold worldwide as, over the next 5 years, branded drugs worth a total of $142 billion in sales are likely to see their patents expire in major developed markets. Two-thirds of that loss, or $98 billion, will be from forgone sales in the US market.
- 26.
For example, the FDA has recently approved Merck’s combination drug Juvisync, intended for the joint therapy of type 2 diabetes and high cholesterol. Enhanced patient compliance and better prevention are expected from the convenience of taking a single pill.
References
Acemoglu D, Linn J (2004) Market size in innovation: theory and evidence from the pharmaceutical industry. Quart J Econ 119(3):1049–1090
Angell M (2004) Excess in the pharmaceutical industry. Can Med Assoc J 171(12):1451–1453
Arora A, Gambardella A, Magazzini L, Pammolli F (2007) A breath of fresh air? Firm type, scale, scope and selection effects in drug development, working paper
Bottazzi G, Dosi G, Lippi M, Pammolli F, Riccaboni M (2001) Innovation and corporate growth in the evolution of the drug industry. Int J Ind Organ 19:1161–1187
Cassiman B, Ueda M (2006) Optimal project rejection and new firm start-ups. Manag Sci 52(2):262–275
Chan T, Nickerson JA, Owan H (2007) Strategic management of R&D pipelines with co-specialized investments and technology markets. Manag Sci 53(4):667–682
Chandy R, Hopstaken B, Narasimhan O, Prabhu J (2006) From invention to innovation: conversion ability in product development. J Market Res XLIII:494–508
Cockburn IM (2007) Is the pharmaceutical industry in a productivity crisis? In: Lerner J, Stern S (eds) Innovation policy and the economy, vol 7. NBER, MIT Press, Cambridge
Cockburn IM, Henderson RM (1996) Public-private interaction in pharmaceutical research. Proc Natl Acad Sci 93:12725–12730
Cockburn IM, Henderson RM (1998) Absorptive capacity, coauthoring behavior, and the organization of research in drug discovery. J Ind Econ 46(2):157–182
Cockburn IM, Henderson RM (2001a) Publicly funded science and the productivity of the pharmaceutical industry. In: Jaffe A, Lerner J, Stern S (eds) Innovation policy and the economy, vol 1. NBER, MIT Press, Cambridge
Cockburn IM, Henderson RM (2001b) Scale and scope in drug development: unpacking the advantages of size in pharmaceutical research. J Health Econ 20:1033–1057
Cohen WM, Levintal DA (1989) Innovation and learning: the two faces of R&D. Econ J 99:569–596
Cohen WM, Levintal DA (1990) Absorptive capacity: a new perspective on learning and innovation. Adm Sci Q 35(1):128–152
Danzon PM, Nicholson S, Pereira NS (2005) Productivity in pharmaceutical-biotechnology R&D: the role of experience and alliances. J Health Econ 24:317–339
Deeds DL, Hill CWL (1996) Strategic alliances and the rate of new product development: an empirical study of entrepreneurial biotechnology firms. J Bus Venturing 11:41–55
DiMasi JA, Grabowski HG (2007) The cost of biopharmaceutical R&D: is biotech different? Manag Decis Econ 28:469–479
DiMasi JA, Paquette C (2004) The economics of follow-on drug research and development: trends in entry rates and the timing of development. Pharmacoeconomics 22:1–14
DiMasi J, Grabowski HG, Vernon J (1995) R&D costs, innovative output and firm size in the pharmaceutical industry. Int J Econ Bus 2(2):201–219
DiMasi JA, Hansen RW, Grabowski HG (2003) The price of innovation: new estimates of drug development costs. J Health Econ 22:151–185
Ding M, Eliashberg J (2002) Structuring the new product development pipeline. Manag Sci 48(3):343–363
Ding M, Eliashberg J (2008) A dynamic competitive forecasting model incorporating dyadic decision making. Manag Sci 54(4):820–834
Gans JS, Stern S (2000) Incumbency and R&D incentives: licensing the gale of creative destruction. J Econ Manag Strat 9(4):485–511
Gassmann O, Reepmeyer G (2005) Organizing pharmaceutical innovation: from science-based knowledge creators to drug-oriented knowledge brokers. Creativity Innov Manag 14(3):233–245
Gassmann O, von Zedtwitz M (1998) Organization of industrial R&D on a global scale. R&D Manag 28(3):147–161
Gilbert J, Henske P, Singh A (2003), Rebuilding Big Pharma’s business model. In: In vivo: the business and medicine report, 21(10), www.elsevierbi.com
Gonzalez J, Sismeiro C, Dutta S, Stern P (2008) Can branded drugs benefit from generic entry? The role of detailing and price in switching to non-bioequivalent molecules. Int J Res Market 25:247–260
Grabowski H, Vernon J (1992) Brand loyalty, entry, and price competition in pharmaceuticals after the 1984 Drug Act. J Law Econ 35(2):331–350
Grabowski H, Vernon J, DiMasi J (2002) Returns on research and development for 1990s new drug introductions. Pharmacoeconomics 20(3):11–29
Grewal R, Chakravarty A, Ding M, Liechty J (2008) Counting chickens before the eggs hatch: associating new product development portfolios with shareholder expectations in the pharmaceutical sector. Int J Res Market 25:261–272
Griliches Z, Cockburn I (1994) Generics and new goods in pharmaceutical price indexes. Am Econ Rev 84(5):1213–1232
Hagedoorn J (1993) Understanding the rationale of strategic technology partnering: interorganizational modes of cooperation and sectoral differences. Strat Manag J 14:371–385
Hahn M, Park S, Krishnamurthi L, Zoltners AA (1994) Analysis of new product diffusion using a four-segment trial-repeat model. Market Sci 13(3):224–247
Henderson R, Cockburn I (1994) Measuring competence? Exploring firm effects in pharmaceutical research. Strat Manag J 15:63–84
Henderson R, Cockburn I (1996) Scale, scope and spillovers: the determinants of research productivity in drug discovery. Rand J Econ 27(1):32–59
Higgins MJ, Rodriguez D (2006) The outsourcing of R&D through acquisitions in the pharmaceutical industry. J Financ Econ 80:351–383
Hoang H, Rothaermel FT (2005) The effect of general and partner-specific alliance experience on joint R&D project performance. Acad Manag J 48(2):332–345
Hollis A (2002) The importance of being first: evidence from Canadian generic pharmaceuticals. Health Econ 11:723–734
Hollis A (2003) The anti-competitive effects of brand-controlled “Pseudo-generics in the Canadian pharmaceutical market”. Can Public Pol 29(1):21–32
Hollis A (2004) Me-too drugs: is there a problem? Mimeo, Department of Economics, University of Calgary, Calgary
Hudson J (2000) Generic take-up in the pharmaceutical market following patent expiry: a multi-country study. Int Rev Law Econ 20:205–221
Kanavos P, Costa-Font J, Seeley E (2008) Competition in off-patent drug markets: issues, regulation and evidence. Econ Policy 23:499–544
Khulji SE, Mroczkowski T, Bernstein B (2006) From invention to innovation: toward developing an integrated innovation model for biotech firms. J Prod Innov Manag 23:528–540
Lane PJ, Lubatkin M (1998) Relative absorptive capacity and interorganizational learning. Strat Manag J 19:461–477
Lee J (2003) Innovation and strategic divergence: an empirical study of the U.S. pharmaceutical industry from 1920 to 1960. Manag Sci 49(2):143–159
Magazzini L, Pammolli F, Riccaboni M (2004) Dynamic competition in pharmaceuticals. Eur J Health Econ 5:175–182
Morton FMS (1999) Entry decisions in the generic pharmaceutical industry. Rand J Econ 30(3):421–440
Morton FMS (2000) Barriers to entry, brand advertising, and generic entry in the US pharmaceutical industry. Int J Ind Organ 18:1085–1104
Nerkar A, Roberts PW (2004) Technological and product-market experience and the success of new product introductions in the pharmaceutical industry. Strat Manag J 25:779–799
PhRMA (2011) Pharmaceutical Industry Profile 2011. PhRMA, Washington, DC
Powell WW, Koput KW, Smith-Doerr L (1996) Interorganizational collaboration and the locus of innovation: networks of learning in biotechnology. Adm Sci Q 41(1):116–145
Rao AG, Yamada M (1988) Forecasting with a repeat purchase model. Manag Sci 34(6):734–752
Rothaermel FT (2001a) Complementary assets, strategic alliances, and the incumbent’s advantage: an empirical study of industry and firm effects in the biopharmaceutical industry. Res Policy 30:1235–1251
Rothaermel FT (2001b) Incumbent’s advantage through exploiting complementary assets via interfirm cooperation. Strat Manag J 22(6/7):687–699
Rothaermel FT, Deeds DL (2006) Alliance type, alliance experience and alliance management capability in high-technology ventures. J Bus Venturing 21:419–460
Shan WJ, Walker G, Kogut B (1994) Interfirm cooperation and startup innovation in the biotechnology industry. Strat Manag J 15:387–394
Shankar V (1999) New product introduction and incumbent response strategies: their interrelationship and the role of multimarket contract. J Market Res 36:327–344
Shankar V (2008) Strategic marketing decision models for the pharmaceutical industry. In: Wierenga B (ed) Handbook of marketing decision models. Springer, New York
Shankar V, Carpenter G, Krishnamurthi L (1998) Late mover advantage: how innovative late entrants outsell pioneers. J Market Res 35:54–70
Shankar V, Carpenter G, Krishnamurthi L (1999) The advantages of entry in the growth stage of the product life cycle: an empirical analysis. J Market Res 36:269–276
Simonet D (2002) Licensing agreements in the pharmaceutical industry. Int J Med Market 2(4):329–341
Sorescu AB, Chandy RK, Prabhu JC (2003) Sources and financial consequences of radical innovation. J Market 67:82–102
Stremersch S, van Dyck W (2009) Marketing of the life sciences: a new framework and research agenda for a nascent field. J Market 73(July):4–30
Stuart TE, Hoang H, Hybels RC (1999) Interorganizational endorsements and the performance of entrepreneurial ventures. Adm Sci Q 44:315–349
Thomke S, Kuemmerle W (2002) Asset accumulation, interdependence and technological change: evidence from pharmaceutical drug discovery. Strat Manag J 23(7):619–635
Vakratsas D, Kolsarici C (2008) A dual-market diffusion model for a new prescription pharmaceutical. Int J Res Market 25:282–293
Wuyts S, Dutta S (2008) Licensing exchange—insights from the pharmaceutical industry. Int J Res Market 25:273–281
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this chapter
Cite this chapter
Petrova, E. (2014). Innovation in the Pharmaceutical Industry: The Process of Drug Discovery and Development. In: Ding, M., Eliashberg, J., Stremersch, S. (eds) Innovation and Marketing in the Pharmaceutical Industry. International Series in Quantitative Marketing, vol 20. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-7801-0_2
Download citation
DOI: https://doi.org/10.1007/978-1-4614-7801-0_2
Published:
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-7800-3
Online ISBN: 978-1-4614-7801-0
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)