Abstract
Autism spectrum disorders (ASDs) result from multifaceted deficits and manifest differently in every individual. The developmental abnormalities of ASDs could be a consequence of genetic aberrations, environmental stressors, or interactions between the two during critical periods of neurodevelopment. Increasing attention has been devoted to investigating lipid signalling molecules since lipids play pivotal roles in the development and function of the human brain and body by acting as regulatory molecules that modulate growth and maintenance. Growing evidence supports the idea that altered fatty acid metabolic pathways may be involved in the pathogenesis of autism and contribute to the variable expression of autism-related traits. This chapter provides an overview of the abnormalities associated with the synthesis of lipid signalling metabolites in individuals with ASDs due to genetic and environmental factors, including dietary lipid imbalances, oxidative stress, and immunological triggers. In particular, the deficits associated with the lipid metabolic pathway for prostaglandin biosynthesis are discussed in further detail. The existing literature provides compelling evidence for the contribution of altered lipid neurobiology to the pathology of ASDs and reveals potential molecular mechanisms that may be important for the development of novel treatments and interventions.
Access provided by Autonomous University of Puebla. Download reference work entry PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction to Lipids
Fatty acids are the simplest type of lipids that serve as building blocks for more complex lipids such as phospholipids, cholesterol, and vitamin E, which are integral to cell membranes (Fig. 1). Abnormal metabolism and imbalances of these three complex lipids have all been associated with autism spectrum disorders (ASDs) and will be outlined in following sections. Fatty acids can be saturated, monounsaturated, or polyunsaturated; the latter will be elaborated upon due to its link with ASDs. Essential fatty acids (EFAs), also called polyunsaturated fatty acids (PUFAs), play an important role in maintaining the structural and functional integrity of the central nervous system (CNS). They serve as major components of neural cell membrane phospholipids and are necessary for the modulation of ion channels, enzymes, and receptor activity (Boland et al. 2009; Guizy et al. 2008). PUFAs must be obtained through the diet since the ability to synthesize them is limited. The two major types of PUFAs are omega-6 linoleic acid (LA; 18:2n-6) and omega-3 α-linolenic acid (ALA; 18:3n-3), which are converted to arachidonic acid (AA, 20:4n-6) and to eicosapentaenoic acid (EPA, 20:5n-3) or docosahexaenoic acid (DHA, 22:6n-3), respectively (Haag 2003) (Figs. 1 and 2).
One of the most commonly derived PUFAs from cell membranes is AA. Through the action of phospholipase A2 (PLA2), an enzyme important for cell membrane maintenance, AA is cleaved from membrane phospholipids and further metabolized to potent bioactive messengers including prostaglandins, thromboxanes, leukotrienes, lipoxins, and cannabinoids. The metabolic products of AA are collectively known as eicosanoids.
The Importance of Lipids in the Brain
Compared to all organs other than adipose tissue, the human brain has the highest percentage of lipids by mass, with approximately 60 % of its dry mass being lipids – specifically phospholipids and PUFAs (Lawrence 2010). AA and DHA/EPA are the most abundant PUFAs in the brain (Sastry 1985), and a sufficient supply of and balance between omega-6 and omega-3 fatty acids are important for plasma membrane integrity, which is tightly integrated with healthy development, maintenance, and function of the nervous system (Lawrence 2010). An extensive body of research has been devoted to determining the role of fatty acids in the nervous system.
Rapid brain growth begins during prenatal fetal development and continues postnatally for 2 years following birth. The majority of brain growth occurs during the fetal stage, and at birth, a newborn’s brain is already 70 % the size of the adult brain (Clandinin et al. 1994). There is a high PUFA demand during the brain growth spurt (Lauritzen et al. 2001), and during this period, the omega-6 and omega-3 fatty acid content in grey and white matter increases significantly (Martinez 1992). The importance of PUFAs in fetal development is emphasized by the high lipid content found in breast milk, as well as the increasing proportions of PUFAs in the phospholipids when comparing levels found in the maternal blood to the placenta and to the fetal brain (Crawford et al. 1981). This process ensures that the high concentrations of long-chain PUFAs necessary for the developing brain can be acquired (Crawford et al. 1989).
Healthy development of the human brain relies greatly on the functions of lipids (Calderon and Kim 2004). For example, AA and DHA are important for retinal development and vision (Hoffman et al. 2009), neuroplasticity and signal transduction (Wu et al. 2008), inflammation (Ferrucci et al. 2006), learning and memory (Su 2010), and sleep (Ladesich et al. 2011). The final structure and breakdown of phospholipids (AA and DHA precursors) represent a unique interaction between genetic and environmental factors. Proper brain functioning relies on the supply of dietary PUFAs and the release of their metabolites from membrane phospholipids through the activity of enzymes such as PLA2 (Yehuda et al. 1999) (Fig. 3). Therefore, alterations in phospholipid metabolism may affect normal functions of the CNS. Anomalies in lipid concentrations due to insufficient dietary intake or aberrant lipid regulation may lead to irregular lipid profiles and signalling and could be highly detrimental to the developing brain. Recent literature provides sufficient evidence that dysregulation of the lipid metabolic pathway may be an underlying biological component involved in the pathophysiology of ASDs. Abnormalities at multiple sites of this pathway have been associated with ASDs and will be further discussed in proceeding sections.
Defects in lipid derivatives and prostanoids. Prostanoids(PGE2, PGF2α, PGD2, PGI2) and thromboxane A2 (TXA2) are bioactive lipid metabolites that elicit cellular events through the action of their respective receptors (EP, FP, DP, IP, and TP) (dashed arrows indicate an increase or decrease level in individuals with ASD; asterisks indicate a link to ASD)
Lipid Imbalances in ASDs
Essential Fatty Acid Profiles in ASDs
Current literature suggests that imbalances in the lipid profiles of omega-6 (i.e., AA) and omega-3 (i.e., DHA and EPA) fatty acids may be an underlying mechanism to the manifestation of autistic-like behaviors. Specifically, several studies have reported altered AA, DHA, and EPA levels in patients with autism. Investigation of blood samples revealed that children with autism have a higher AA: DHA ratio (Meguid et al. 2008) and a higher AA: EPA ratio (Bell et al. 2010) compared to healthy controls. Other studies have reported significantly lower-than-normal levels of AA and DHA in the blood plasma of individuals with autism (Wiest et al. 2009; Vancassel et al. 2001). Another study revealed an increase in plasma DHA levels in high-functioning males with autism (Sliwinski et al. 2006). Though the causes of atypical PUFA levels have yet to be fully understood at the molecular level, potential reasons include defects in the enzymes that convert dietary PUFAs into longer and highly unsaturated derivatives, inadequacy in the integration of PUFAs into membrane phospholipids, or deficient dietary intake of PUFA precursors (Vancassel et al. 2001). Moreover, aberrant activity of fatty acid desaturase-1 and fatty acid desaturase-2 (FADS1 and FADS2), the enzymes that catalyze the breakdown of LA and ALA into AA and DHA, can lead to irregular lipid profiles (Morales et al. 2011) and may be involved in lipid imbalances reported in autism (Figs. 1 and 3). Notably, the chromosomal locations of FADS1 and FADS2 are in close proximity to an autism-candidate linkage peak on chromosome 11q22 (Craddock and Lendon 1999; Ma et al. 2007). The presence of altered lipid composition and its potential contribution to the behavioral outcomes of ASDs have been conveyed in animal studies using rodent models, which revealed that altered brain phospholipid composition induced by environmental agents, including enteric bacteria and diet, can lead to the appearance of autism-like behavior (Shultz et al. 2009; Thomas et al. 2010). Altogether, these studies provide evidence that irregular lipid profiles are a common characteristic of ASDs.
Insufficient Dietary Fatty Acids and Autism
The availability of fatty acids for brain development can be heavily impacted by the maternal diet during the prenatal stage and by the infant’s diet (i.e., breast milk or formula) in the postnatal stage. Since abnormal lipid profiles have commonly been characterized in individuals with ASDs, the ability to alter lipid concentrations through dietary means is encouraging. Healthy infants fed with PUFA-supplemented milk formula showed improvements in infant cognitive scores compared to infants on a no-PUFA formula, suggesting that inadequate intake of dietary PUFAs during early development may be associated with altered cognition (Willatts et al. 1998). Considering that higher problem-solving scores in infancy have been associated with higher childhood IQ scores, PUFA supplementation may modify the development of childhood intelligence. There is also a significantly higher likelihood for infants to develop autism if they were not breastfed or not supplemented with PUFAs (Schultz et al. 2006), and administration of PUFA supplementation has been shown to restore normal fatty acid profiles and improve behavioral outcomes in children with autism. For example, when diet was supplemented with fish oils high in omega fatty acids for 6 months, children with autism or Asperger’s syndrome exhibited reduced omega-6:omega-3 and AA: EPA ratios compared to supplementation-naïve autistic controls (Bell et al. 2010). Another study found that supplementation of omega-6 and omega-3 fatty acids in children with autism led to elevated levels of fatty acids in the blood, decreased AA: DHA ratio, and improvements in several autism-affected behavioral domains such as eye contact, concentration, language development, and motor skills (Meguid et al. 2008). Another group revealed that stereotypy and hyperactivity associated with autism were mitigated with omega-3 fatty acid supplementation (Amminger et al. 2007). Such supplementation also led to improvements in basic language and learning skills in children with autism (Patrick and Salik 2005).
A case study on a child with autism and associated high levels of anxiety and agitation showed the elimination of irregular fatty acid levels and the complete resolution of anxiety and agitation after EPA supplementation was administered (Johnson and Hollander 2003). A better quality of life was also reported in the study. Additionally, these improvements in fatty acid levels and behavior were stable at the 8-month follow-up. In contrast, a study investigating young adults (18–40 years old) with autism revealed that omega-3 fatty acid supplementation did not lead to significant improvements in behavior (Politi et al. 2008), which suggests that there may be a specific time window for the potential beneficial effects of supplementation.
Furthermore, cholesterols are lipids that are important components of cell membranes (Fig. 1) involved in the induction of normal motor and mental capacity (Gilbert 2003). Cholesterol is needed for proper embryonic and fetal development as well. Specifically, it is necessary for the Sonic Hedgehog signal transduction pathways, which are crucial for the induction of brain formation, neural patterning, mood regulation, and cerebral development (Gilbert 2003). Cholesterol affects the availability of essential lipid molecules, and as such, its insufficient consumption by the mother could lead to unhealthy metabolic deficiencies that may contribute to the development of autism in the offspring (Tallberg et al. 2011). Imbalances in cholesterol levels have also been associated with ASDs (Tierney et al. 2006). Prevailing evidence for this stems from studies on Smith-Lemli-Opitz Syndrome (SLOS), which is a genetic condition of impaired cholesterol biosynthesis (Sikora et al. 2006; Bukelis et al. 2007). Cholesterol treatment in individuals with SLOS resulted in a decrease in autism-related behaviors, infections, and symptoms of irritability and hyperactivity, as well as improvements in physical growth, sleep, and social interactions (Aneja and Tierney 2008). It is interesting to note that cholesterol supplementation also improved other behaviors such as aggression, self-injury, temper outbursts, and trichotillomania (Aneja and Tierney 2008).
Taken together, the existing literature indicates that dietary imbalances in lipids and fatty acids may influence the development of autism-related behavioral outcomes. However, the molecular mechanisms of lipid dysregulation in ASDs still have to be determined. This would aid in establishing recommended dietary supplementation for individuals with ASDs.
Association of Prostaglandin Metabolic Pathway with ASDs
While PUFAs such as AA or DHA are crucial for membrane structure and function, their metabolites, such as bioactive prostanoids, are very important for the normal functioning of the brain (Tassoni et al. 2008). Upon the release of AA from membrane phospholipids via the action of PLA2, cyclooxygenase-1 (COX-1) or cyclooxygenase-2 (COX-2) converts AA into an unstable intermediate, PGG2, which is then metabolized to the prostanoid precursor, PGH2 (Fig. 3). Prostaglandin (PG) or thromboxane synthases convert PGH2 to active lipid signalling messengers including prostanoids, PGs (PGE2, PGF2α, PGD2, PGI2), and thromboxane A2 (TXA2) (Tamiji and Crawford 2010c). Prostanoids can elicit cellular effects by binding to their respective G-protein-coupled receptors called E-prostanoid (EP), FP, DP, IP, and TP receptors, respectively (Breyer et al. 2001) (Fig. 3).
Phospholipase A2
Phospholipases are enzymatic molecules that break down phospholipids, which are precursors of important lipid mediators such as PGs. Phospholipase A2 (PLA2) is of particular interest since it is an upstream regulator of a wide range of physiologic functions. PLA2 selectively hydrolyzes the sn-2 fatty acid ester bond of phospholipids to produce free fatty acids such as AA (Murakami and Kudo 2002). PLA2 activation and the subsequent release of AA and its metabolites can be stimulated by various neurotransmitters such as glutamate (Marin et al. 1997). Alternatively, the presence of other stimuli, such as cytokines activated during inflammation, can cause the release of AA and DHA from phospholipid membranes (Farooqui et al. 2007).
A member of the PLA2 protein family that is a human calcium-independent phospholipase called iPLA2 is located on the chromosome region 7q31, which has been associated with autism (Abrahams and Geschwind 2008). Moreover, clinical studies have reported significantly higher concentrations of PLA2 in the red blood cells of individuals with autism and Asperger’s syndrome compared to healthy controls (Bell et al. 2004) (Fig. 3). The increased activity of PLA2 in patients with ASDs could interfere with the proper maintenance of membrane phospholipids, and this may contribute to their abnormal PUFA profiles. Current literature provides support for a link between aberrant PLA2 enzyme activity or concentrations and ASDs, reinforcing the hypothesis that abnormal lipid metabolism may play a role in the pathophysiology of these disorders.
COX Enzymes
The enzymes cyclooxygenases-1 and -2 (COX-1, -2) catalyze the reaction of oxygen with PUFAs, producing bioactive lipid substances, such as prostaglandins (PGs), from AA (Sang and Chen 2006). Collectively, these lipid metabolites are known as eicosanoids, each of which is formed by a different sequence of enzyme-catalyzed reactions. Both COX enzymes assist in the production of autoregulatory and homeostatic prostanoids, which may be released during inflammation. The enzymatic activity of COX can be inhibited by nonsteroidal anti-inflammatory drugs, consequently inhibiting the biosynthesis of PGs (Vane 1971).
COX-1, the constitutive form, is expressed in nearly all human tissues including the brain, lung, kidney, and stomach (O’Neill and Ford-Hutchinson 1993). Although most commonly known as a mediator of housekeeping functions, new evidence shows that COX-1 may also be important in developmental and inflammatory functions (Loftin et al. 2002). For example, COX-1 activity may alter progenitor cell proliferation and hippocampal neurogenesis (Russo et al. 2011), neuroinflammation (Shukuri et al. 2011), as well as parturition (Gross et al. 1998). COX-2, the inducible form, is heavily involved with the inflammatory response. It is normally found in low levels, but various stimuli such as growth factors (Hinz and Brune 2002), inflammation due to injury or infection (Ricciotti and FitzGerald 2011), synaptic activity (Yamagata et al. 1993), and oxidative stress (Kwiecien et al. 2012) can trigger its upregulation.
Interestingly, COX-2 plays important roles in the CNS, gastrointestinal tract (GI), and pain perception (Hinz and Brune 2002) via the production of downstream signalling metabolites such as PGE2. Abnormalities in the CNS, GI, and nociception have been reported in cases of ASDs (Dubois et al. 2010; Gorrindo et al. 2012; Kohane et al. 2012) and increasing lines of evidence demonstrates that these abnormalities are associated with alterations in the COX-2/PGE2 pathway (Fig. 3). The activity and production of COX-2 are induced by cytokines and proinflammatory agents, and irregular immune responses have been characterized in patients with ASDs (Ashwood et al. 2006). Additionally, COX-2 is a key contributor to neurodevelopment. COX-2 is richly expressed in the dendrites of neurons (Yamagata et al. 1993). However, its distribution pattern is anomalous in the brain tissue of individuals with Rett syndrome, a form of ASD (Kaufmann et al. 1997). Furthermore, ASDs have been associated with a polymorphism in PTGS2, the gene encoding for the COX-2 protein (Yoo et al. 2008).
Prostaglandin E2 During Development
PUFAs are essential structural components of cell membranes, while eicosanoids are crucial metabolites required for the normal functioning of the brain (Tassoni et al. 2008). PGE2 is an eicosanoid that is generated from the metabolism of PGH2 by the enzymatic action of PG synthase. PGE2 diffuses rapidly through membranes, exerting its signalling effects by binding to E-prostanoid receptors (EP1-4). EP receptors are G-protein-coupled receptors and are expressed differentially across varying tissue types (Sugimoto and Narumiya 2007). PGE2 is an important lipid mediator that typically acts within the local microenvironment, providing autocrine and paracrine stimulation to a number of signalling pathways in the nervous system (Legler et al. 2010) and regulating the function of many immune cell types, thus mediating the inflammatory response in the brain (Zhang and Rivest 2001). Evidence shows that it is also involved in dendritic spine formation (Burks et al. 2007), synaptic plasticity (Koch et al. 2010), pain transmission (Harvey et al. 2004), and cell survival (Jiang et al. 2010) or death (Jonakait and Ni 2009). In early prenatal development, there is an increase in the number of COX-2 and PG synthases (Saint-Dizier et al. 2011), as well as elevated levels of EP receptor transcripts (Tamiji and Crawford 2010b), suggesting that PGE2 is involved in early development. The PGE2 pathway is summarized in Fig. 4.
Clinical studies have revealed a connection between misuse of the drug misoprostol during the first trimester of pregnancy and neurodevelopmental aberrations, including Mobius sequence and ASDs (Bandim et al. 2003) (Fig. 3). Misoprostol is an analogue of prostaglandin type E, which has been proven to bind and activate EP receptors activating the PGE2 pathway (Tamiji and Crawford 2010a) (Fig. 4). It was initially used to treat stomach ulcers and has since been used also to induce labor and to terminate pregnancy (Lin et al. 2011). During the early stages of pregnancy (5–6 weeks after fertilization), the embryo is the most vulnerable to misoprostol exposure (Genest et al. 1999). Exposure to this drug during early embryonic development may alter the PGE2 signalling pathway and have toxic effects on the developing nervous system. Misoprostol and PGE2 can increase the intracellular level and fluctuation amplitude of calcium in neuronal growth cones, as well as reduce the number and length of neurite extensions through the activation of EP receptors (Tamiji and Crawford 2010a, b). Dysfunctional calcium regulation has been previously suggested in the etiology of ASDs (Krey and Dolmetsch 2007). When considering these studies together, they demonstrate that abnormalities in the PGE2 pathway through misoprostol exposure could lead to neurotoxic effects on the development and communication of neurons.
The importance of the PGE2 signalling pathway during early development is further established through the significantly increased expression of four EP receptors transcripts – EP1, EP2, EP3β, and EP4 – during early neurogenesis (embryonic day 11–15) in the mouse (Tamiji and Crawford 2010b). It is intriguing that this embryonic period marks the development of many brain structures (Rice and Barone 2000) including the cerebellum, amygdala, hippocampus, and caudate nucleus of the basal ganglia, which have been reported to be abnormal in individuals with autism (Amaral et al. 2008). However, it is still unclear how COX-2/PGE2 signalling may directly affect the development of these brain areas.
There is growing evidence supporting an interaction between the PGE2 and the WNT (wingless) pathways (Evans 2009). PGE2-dependent signalling may converge with the WNT pathway at the level of β-catenin through EP1-4 receptors, including the association of the Gαs subunit with axin, the stimulation of the cAMP/PKA pathway, or the phosphorylation of GSK-3β by PI-3K (Buchanan and DuBois 2006) (Fig. 5). Such an interaction is of particular interest since WNTs are morphogens necessary for the formation of a healthy nervous system (Ciani and Salinas 2005). They are signalling molecules that act through Frizzled (FZD) transmembrane receptors and are vital to embryonic development, participating in the determination of cell fates through activating transcription of various target genes (Buechling and Boutros 2011). Cross talk and joint regulation between these pathways have been reported previously in various nonneuronal cells. For example, in osteocytes, PGE2 interacts with β-catenin to modulate bone mass and density (Genetos et al. 2011), as well as apoptosis following induced stress (Kitase et al. 2010). The COX-2/PGE2 signalling pathway is highly stimulated in gastric cancer cells, which results in significantly increased levels of PGE2 and subsequent activation of WNT (Oshima et al. 2009). In these cells, PGE2 and WNT signalling cooperated to cause dysplastic growth and development (Oshima and Oshima 2010), while a dose-dependent effect of PGE2 on WNT activation in bone and prostate cancer cells has been reported (Liu et al. 2010). Furthermore, in colon cancer cells, PGE2 induces a decrease in β-catenin phosphorylation, which increases the activation of TCF/LEF transcription factors and upregulates certain genes, resulting in increased proliferation (Castellone et al. 2005). WNT and PGE2 also collaborate to promote the survival and proliferation of zebra fish hematopoietic stem cells (Goessling et al. 2009). Through this model, it was also demonstrated that PGE2 and WNT are important in the regulation of vertebrate regeneration and recovery.
Although the interaction between these two pathways in the nervous system still remains elusive, our current studies have shown that PGE2 can modulate the expression of WNT-target genes and change the proliferation and migration behavior of neuroectodermal (NE-4C) stem cells (Wong et al. 2011, 2012). WNT signalling proteins are also essential for neuronal precursor proliferation (Zhou et al. 2006), radial migration of cortical neurons (Zhou et al. 2004), and synapse formation (Sahores and Salinas 2011), all of which are cellular events driven by calcium signalling. Therefore, calcium fluctuations induced by PGE2 or misoprostol as demonstrated by Tamiji and Crawford (2010c) may interfere with the WNT signalling pathway, influencing its various functions. For example, calcium signalling triggered by neuronal activity mediates the CREB-dependent transcription of Wnt-2 as well as the production and secretion of its corresponding protein. Wnt-2, one of many wingless genes, contributes to proper dendritic outgrowth and branching (Wayman et al. 2006). Notably, this gene is located in the chromosome region 7q31-33, which has been linked to autism, and its polymorphisms have been associated with speech delay inherent in ASDs (Lennon et al. 2007; Lin et al. 2012). Moreover, WNT signalling participates in the formation of the cerebellum (Hall et al. 2000), hippocampus (Galceran et al. 1999), and amygdala (Abu-Khalil et al. 2004). As mentioned earlier, structural deviations in these brain areas have been implicated in autism. Misguided neuronal migration resulting in misplaced neurons, especially Purkinje cells, has also been connected to autism (Wegiel et al. 2010). Given that WNTs are crucial regulators of cell fate specification, cell proliferation, and cell migration during development (Buechling and Boutros 2011), PGE2-dependent dysregulation of WNT signalling could result in brain abnormalities and contribute to autism. These lines of evidence validate the increasing interest in investigating the molecular mechanisms underlying the interaction between the COX-2/PGE2 and WNT signalling pathways and link to autism.
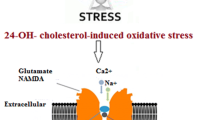
Oxidative Stress and Lipid Peroxidation in ASDs
Under normal conditions, there is a dynamic equilibrium between the production of reactive oxygen species (ROS) and the rate at which they are neutralized by antioxidants. Oxidative stress occurs when there is an imbalance in this equilibrium and the level of ROS produced by a cell exceeds its antioxidant capacity. ROS such as oxygen ions, free radicals, and peroxides are highly reactive molecules that can damage the cell by targeting lipids, a key building block of cells (Choe 2010). Elevated levels of free radicals and reduced antioxidant defense mechanisms are the prime initiators of oxidative stress (Sies 1997). The activity of ROS can lead to altered cell function due to abnormal lipid metabolism affecting proliferation and differentiation during neurodevelopment and can even cause cell death (Filomeni and Ciriolo 2006). The PUFAs from membrane phospholipids are the primary targets of ROS because they contain many double bonds, making them particularly vulnerable to lipid peroxidation, which is the oxidative breakdown of lipids (Adibhatla and Hatcher 2008). This results in increased metabolism of AA and activates the PGE2 signalling pathway (Pepicelli et al. 2005). A number of neurological disorders, such as autism, schizophrenia, and Alzheimer’s, have been associated with dysregulation of lipid metabolism and increased levels of oxidative stress. A combination of genetic and environmental factors influencing lipid peroxidation may contribute to the etiology of autism (Deth et al. 2008).
An imbalance between the oxidative and antioxidative stress systems due to increased oxidative damage and decreased antioxidant neutralization has been reported in individuals with autism (Ghanizadeh et al. 2012). The brain is particularly vulnerable to oxidative stress and consequent lipid peroxidation because lipids are the primary component of the human brain (Adibhatla and Hatcher 2008), and because the brain uses a great amount of oxygen, generating potentially elevated levels of harmful reactive by-products. The high oxygen requirement of the brain is exemplified by the fact that although the human brain is approximately 2 % of an individual’s total body mass, it uses around 20 % of the available body oxygen (Shulman et al. 2004). The brain also has limited antioxidant defense mechanisms because neurons cannot produce glutathione (GSH), one of the most important antioxidants for the free radical neutralization of environmental toxins (Shulman et al. 2004). As the majority of the energy consumed in the brain is used by neurons, they are the first cells to be affected by reduced antioxidant levels and thus in the most danger. Infants who are in a sensitive period of development are more vulnerable than adults to oxidative stress because they have naturally lower levels of GSH (Ono et al. 2001), which may suggest greater risk of oxidative stress. Children with autism have been reported to have lower levels of GSH and a deficiency in GSH precursors, methionine, and cysteine, which indicate their increased susceptibility to oxidative stress and the associated risk of developing brain disorders (James et al. 2004; Al-Gadani et al. 2009). The diminished antioxidant capacity could amplify oxidative damage to the cells. Several studies have also discovered genetic variances (allele deletions and polymorphisms) that directly impact methionine and GSH metabolism in individuals with autism (Buyske et al. 2006; Ming et al. 2010; Williams et al. 2007), hinting at the influence of genetics in the abnormalities of lipid peroxidation observed in ASDs. In addition to GSH, aberrations in a number of other antioxidants have been reported in several studies. Protein antioxidants, ceruloplasmin, and transferrin levels were significantly reduced, and lipid peroxidation was significantly elevated in the plasma samples of children with autism compared to controls (Chauhan et al. 2004).
Current literature also provides support for the connection between elevated oxidative damage and lipid/prostanoid metabolites in cases of autism. Two protein adducts, carboxyethyl pyrrole (CEP) and iso[4]levuglandin (iso[4]LG)E2 (Fig. 1), are uniquely formed through the peroxidation of DHA- and AA-containing lipids, respectively, and are markers of oxidative damage. Significantly increased fluorescent immunoreactivity of these compounds was detected in the cortical tissue of subjects with ASD compared to healthy controls (Evans et al. 2008). Moreover, a distinct expression pattern specific to the autistic brain was also visualized – significant staining was found in white and grey matter. Increased levels of lipid peroxidation markers 2, 3-dinor-thromboxane (TXB2) and 6-ketoprostaglandin PGF1α (6-keto-PGF1α), which are metabolites of TXA2 and PGI2, respectively (Fig. 3), were quantified in urine samples of children with autism (Yao et al. 2006). Likewise, elevated levels of 8-isoprostane-F2α(8-iso-PGF2α) and isoprostane F2α-VI (iPF2α-VI), by-products of PGF2α peroxidation via the oxidation of AA (Fig. 3), have been measured in the urine of children with autism compared to healthy controls (Yao et al. 2006). A significantly higher concentration of iPF2α was also reported in plasma samples of children with autism (Mostafa et al. 2010) and patients with Rett syndrome (De Felice et al. 2009). Under normal conditions, the accumulation of F2-isoprostanes induces platelet aggregation and vasoconstriction (Pratico et al. 2001). However, when the accumulation becomes abnormal, as evident in the blood and urine samples from individuals with autism, it may contribute to the altered platelet reactivity and vascular irregularities reported in these patients (Yao et al. 2006).
There has also been mounting evidence that links abnormalities in vitamin E and the pathology of ASDs. Vitamin E, a lipid and a powerful antioxidant capable of protecting cells and tissues from oxidative damage, is important in the regulation of lipid peroxidation. It is a key component of cell membranes (Fig. 1) that is also stored in fat and liver for future mobilization during elevated levels of oxidative stress (Lawrence 2010). Deficient levels of vitamin E have been reported in blood samples of children with autism (Al-Gadani et al. 2009). Supplementation of PUFAs and vitamin E led to dramatic improvements in a number of areas including speech, imitation, coordination, eye contact, behavior, sensory issues, and the development of pain sensation in 97 % of 187 ASD-affected children (Morris and Agin 2009). When the supplementation was halted, speech and coordination regressed in some children, suggesting that abnormal fatty acid metabolism may contribute to the manifestation of these autism-associated traits.
In summary, the reported findings provide additional evidence for irregular lipid biogenesis in ASDs. Current publications reveal altered antioxidant capacity and increased oxidative stress markers in individuals with autism. Lipids are the prime targets for oxidative stress, suggesting that abnormal lipid signalling may be associated with the development and/or expression of symptomatic deficits in affected individuals.
Immunological Factors Contributing to Lipid Dysregulation
Immunological events associated with infections in early fetal life through alterations in the vasculature and maternal-fetal immune responses may play a role in the initiation of neurological disorders such as autism, epilepsy, and schizophrenia (Atladottir et al. 2010; Brown and Derkits 2010; Stolp et al. 2012). Immune dysfunctions and insults during sensitive periods of brain development could predispose the developing nervous system to potential failures in subsequent cell migration, target selection, and synapse maturation (Harvey and Boksa 2012). During embryonic and fetal life, the immune system is still immature. This may be an adaptive measure to safeguard the fetus from premature maternal immune rejection, which could lead to fetal damage or even death (de la Cochetière et al. 2007). Paradoxically, this beneficial adaption also increases the risk for the fetus to acquire an infection.
Although autism is a disorder that primarily affects brain function, many cases have shown that other systems, such as the immune system, are also affected. Clinical studies and case reports have revealed the potential contribution that viral infections and aberrant immune responses have towards the pathology of ASDs (Libbey et al. 2005). Additionally, women who develop a fever while pregnant may be more than twice as likely to have a child with an ASD or some other form of developmental delay (Zerbo et al. 2012). Research by various scientists utilizing animal models has demonstrated that certain pre- and postnatal infections can induce gene alterations in the brain, morphological changes in cells and brain regions, immunological deviations in offspring, and irregular behaviors analogous to those characterized in ASDs (Fatemi et al. 2002, 2005, 2008; Ponzio et al. 2007; Shi et al. 2003, 2009).
Although the direct molecular mechanisms by which infections and inflammation may lead to the pathological outcomes of autism through the COX-2/PGE2 lipid signalling pathway remain to be fully elucidated, existing literature supplies indirect evidence of their possible roles. Eicosanoids derived from omega-6 and omega-3 PUFAs are central regulators of the immune and inflammatory responses (Wall et al. 2010). Specifically, AA (omega-6 metabolite) has proinflammatory and immunoactive properties, while EPA and DHA (omega-3 metabolites) have anti-inflammatory roles. Cyclooxygenase-derived mediators, such as the lipid signalling molecule PGE2, are significantly elevated during infections and the inflammatory response (Fitzgerald et al. 2012), especially if the viral or bacterial exposure occurs during pregnancy (Christiaens et al. 2008). PGE2, the most abundantly produced eicosanoid derived from AA, can modulate the sensitivity of sensory nerves and functions as a mediator to induce fever (Lawrence 2010). Heightened PGE2-related inflammatory responses during early development may produce developmental defects in the nervous system. The inflammatory response in the brain can be mediated by PGE2 since it regulates the function of many immune cell types (Zhang and Rivest 2001). It promotes the production of cytokines (Legler et al. 2010), which are compounds made and secreted by leukocytes at the site of inflammation. Cytokines, along with other products of immune activation, have widespread effects on neuronal pathways, which may contribute to common features of ASDs (Ashwood and Van de Water 2004). They also represent the primary mediators of communication between the brain and the immune system. Cytokines act locally as signalling molecules between immune cells, but they may also enter the bloodstream and target remote structures including the brain (Rothwell and Hopkins 1995). The activation of endothelial cells associated with the blood brain barrier is responsible for the subsequent release of second messengers such as prostaglandins that act on specific brain targets (de Vries et al. 1996). Cytokines are also involved in many aspects of CNS function and development as well. They are of particular importance during early neural development, including the induction of the neuroepithelium (Gaulden and Reiter 2008). They are also critical modulators of neuronal and glial migration (Zhu et al. 2002), differentiation (Soleymaninejadian et al. 2012), and selective pruning or programmed cell death to acquire proper neural connections (Sedel et al. 2004). Taken altogether, studies demonstrate that infections and the resultant inflammatory responses could disturb several processes involved in brain development and potentially be in part responsible for the abnormalities of autism. Additional studies are necessary to establish a direct link between the effects of immunological factors and the COX-2/PGE2 pathway, and how consequent alterations are manifested in the molecular and behavioral outcomes of ASDs.
Closing Remarks
There are several lines of research that provide evidence supporting the involvement of abnormal lipid metabolism in individuals with ASDs. Lipid signalling participates in the development of the nervous system, oxidative balance, immune function, as well as gastrointestinal repair and sleep behavior consistent with reported medical complications in some children with autism. The COX-2/PGE2 signalling pathway can become defective due to genetic aberrations or environmental conditions, such as exposure to drugs or infections. There is evidence linking the impairment of this pathway at various steps and the development of ASDs. Collectively, the available literature suggests that lipid signalling may have a crucial impact during pre- and postnatal periods. Anomalous changes along this pathway can be detrimental to the development of the nervous system and may contribute to the pathogenesis and symptomatic manifestations of autism. Considering that ASDs are complex neurodevelopment disorders characterized by a wide range of behaviors, dysregulation at different points of the lipid signalling pathways discussed herein might provide some explanation to the diverse behavioral outcomes of ASDs. Current research gives compelling evidence that lipid irregularities may be a potential underlying cause of autism. However, additional investigation into the various genetic and environmental factors involved with lipid signalling in individuals with autism is essential for understanding the molecular mechanisms of the disorder and may aid in the development of novel diagnostic and therapeutic tools as well as preventative strategies for ASDs.
Key Terms
-
Arachidonic acid. An omega-6 essential fatty acid containing 20 carbons and has 4 carbon-carbon dioxide double bonds. It is metabolized to numerous bioactive eicosanoids and related compounds.
-
Cyclooxygenase. This enzyme catalyzes reactions of polyunsaturated fatty acids with molecular oxygen to produce prostaglandins G2 and H2 from arachidonic acid; these are further metabolized to other prostaglandins and thromboxanes.
-
Cytokines. These include interferons, interleukins, tumor necrosis factor-alpha in addition to many other growth and cell adhesion factors. Cytokines, or protein messengers, provide signals for a wide range of responses related to the growth and development of the body and stimulate the immune system.
-
Eicosanoids. Derivatives of fatty acids; this family includes prostaglandins, thromboxanes, leukotrienes, lipoxins, and cannabinoids. Many eicosanoids are potent bioactive molecules.
-
Fatty acids. The most simple kinds of lipids and are components of several other classes of lipids including triglycerides, phospholipids, glycolipids, cholesteryl esters, and waxes.
-
Free radicals. These are highly reactive substances formed by removing or adding an atom or electron from or to the parent substance. Many of the free radicals are derived from oxygen in the atmosphere and are oxidizing substances. Antioxidants prevent the destructive effects of free radicals.
-
Inflammation. A series of interrelated events involving immune cells attacking foreign substances or damaged tissue resulting in swelling and increased temperature.
-
Lipids. This term refers to fats, oils, fatty acids, phospholipids, steroids, fat-soluble vitamins, and other oily substances that dissolve in nonpolar organic solvents – such as hexane or chloroform – but not in water.
-
Lipid peroxidation. This occurs when polyunsaturated fatty acids are exposed to free radicals and oxygen and react by forming oxidized products such as fatty acid hydroperoxides, aldehydes, conjugated dienes, and malondialdehyde. This process can destroy cell membranes.
-
Phospholipids. Polar lipids that form bilayer lipid membranes that are essential components of cell membranes.
-
Prostaglandins. A branch of the bioactive eicosanoids, formed from polyunsaturated fatty acids such as arachidonic acid and eicosapentaenoic acid found in cell membranes. Different prostaglandins will display similar physiological actions but with subtle differences in activity.
-
Prostaglandin E 2 . PGE2 is one of the primary COX products of arachidonic acid and one of the most widely investigated prostaglandins. Its activity influences inflammation, fertility and parturition, gastric membrane integrity, and immune modulation. The downstream effects of PGE2 are transduced by four distinct receptors designated EP1, EP2, EP3, and EP4. Affinity constants of PGE2 for these receptors range from 1 to 10 nM depending on the receptor subtype and tissue.
Key Points of Lipids
-
Lipids are composed of fatty acids and serve as major building blocks for cellular components.
-
“Fats” are often used synonymously with the term “lipids,” but fats are technically a subgroup of lipids called triglycerides.
-
Essential fatty acids must be included in the diet, similar to vitamins and minerals.
-
Essential fatty acids are necessary for brain development during fetal growth, toddlerhood, and childhood, and are required for proper brain functioning in adulthood.
-
Important biological functions of lipids include energy storage, membrane integrity, cellular signalling, metabolism, and transport.
-
Essential fatty acids can be broken down into powerful bioactive substances called eicosanoids.
-
Genetic and environmental factors could cause imbalances in eicosanoid profiles, and subsequent aberrant signalling could influence the course of several diseases.
-
Genetic mutations in enzymes involved in lipid biosynthetic pathways and inadequate dietary intake of essential lipids can impact lipid profiles and alter developmental functions.
-
Lipids can be affected by environmental factors such as exposure to oxidative stress and infections, which have been reported in people with ASDs.
-
PGE2 is a lipid derivative that acts as an important signalling molecule in the brain.
-
The cooperative regulation of the lipid signalling molecules, PGE2 and morphogen WNT, is crucial for early development.
Summary Points
-
This chapter summarizes the existing evidence for the involvement of lipid metabolism in the pathophysiology of ASDs.
-
Lipids are crucial building blocks of cell membranes but also act as important signalling molecules that can regulate cell function.
-
Omega-6 and omega-3 polyunsaturated fatty acids (PUFAs), vitamin E, and cholesterol are lipids essential to membrane integrity, and abnormalities in these lipids due to genetic and environmental factors have been associated with ASDs.
-
Development and proper functioning of the CNS are dependent on the concentrations of lipids and their metabolites, including prostaglandins (PGs).
-
The lipid concentrations of essential PUFAs, vitamin E, and cholesterol are irregular in individuals with ASDs and may contribute to autism-like behaviors.
-
Studies have reported abnormalities in the COX/PGE2 lipid metabolic pathway.
-
PGE2 is derived from lipids and contributes to pre- and postnatal development.
-
Emerging evidence on the functions and interaction of PGE2 and morphogen WNT is compelling and draws attention to their potential roles in ASDs.
-
Moreover, lipids are particularly susceptible to the damaging effects of oxidative stress.
-
Elevated levels of lipid peroxidation as well as decreased antioxidant capacity have been quantified in the autism population.
-
Immunological factors, such as inflammation and infections, contribute to dysregulation of lipid metabolism and have been linked to an increased risk of ASDs.
-
Lipid dysregulation due to various factors has been demonstrated in cases of ASDs, highlighting its significance and potential roles in the development of the disorders.
References
Abrahams BS, Geschwind DH. Advances in autism genetics: on the threshold of a new neurobiology. Nat Rev Genet. 2008;9(5):341–55.
Abu-Khalil A, Fu L, Grove EA, Zecevic N, Geschwind DH. Wnt genes define distinct boundaries in the developing human brain: implications for human forebrain patterning. J Comp Neurol. 2004;474(2):276–88.
Adibhatla RM, Hatcher JF. Altered lipid metabolism in brain injury and disorders. Subcell Biochem. 2008;49:241–68.
Al-Gadani Y, El-Ansary A, Attas O, Al-Ayadhi L. Metabolic biomarkers related to oxidative stress and antioxidant status in Saudi autistic children. Clin Biochem. 2009;42(10–11):1032–40.
Amaral DG, Schumann CM, Nordahl CW. Neuroanatomy of autism. Trends Neurosci. 2008;31(3):137–45.
Amminger GP, Berger GE, Schafer MR, Klier C, Friedrich MH, Feucht M. Omega-3 fatty acids supplementation in children with autism: a double-blind randomized, placebo-controlled pilot study. Biol Psychiatry. 2007;61(4):551–3.
Aneja A, Tierney E. Autism: the role of cholesterol in treatment. Int rev psychiatry (Abingdon, England). 2008;20(2):165–70.
Ashwood P, Van de Water J. A review of autism and the immune response. Clin Dev Immunol. 2004;11(2):165–74.
Ashwood P, Wills S, Van de Water J. The immune response in autism: a new frontier for autism research. J Leukoc Biol. 2006;80(1):1–15.
Atladottir HO, Thorsen P, Ostergaard L, et al. Maternal infection requiring hospitalization during pregnancy and autism spectrum disorders. J Autism Dev Disord. 2010;40(12):1423–30.
Bandim JM, Ventura LO, Miller MT, Almeida HC, Costa AE. Autism and mobius sequence: an exploratory study of children in northeastern Brazil. Arq Neuropsiquiatr. 2003;61(2A):181–5.
Bell JG, MacKinlay EE, Dick JR, MacDonald DJ, Boyle RM, Glen AC. Essential fatty acids and phospholipase A2 in autistic spectrum disorders. Prostaglandins Leukot Essent Fatty Acids. 2004;71(4):201–4.
Bell JG, Miller D, MacDonald DJ, et al. The fatty acid compositions of erythrocyte and plasma polar lipids in children with autism, developmental delay or typically developing controls and the effect of fish oil intake. Br J Nutr. 2010;103(8):1160–7.
Boland LM, Drzewiecki MM, Timoney G, Casey E. Inhibitory effects of polyunsaturated fatty acids on Kv4/KChIP potassium channels. Am J Physiol Cell Physiol. 2009;296(5):C1003–14.
Breyer RM, Bagdassarian CK, Myers SA, Breyer MD. Prostanoid receptors: subtypes and signaling. Annu Rev Pharmacol Toxicol. 2001;41:661–90.
Brown AS, Derkits EJ. Prenatal infection and schizophrenia: a review of epidemiologic and translational studies. Am J Psychiatry. 2010;167(3):261–80.
Buchanan FG, DuBois RN. Connecting COX-2 and Wnt in cancer. Cancer Cell. 2006;9(1):6–8.
Buechling T, Boutros M. Wnt signaling signaling at and above the receptor level. Curr Top Dev Biol. 2011;97:21–53.
Bukelis I, Porter FD, Zimmerman AW, Tierney E. Smith-Lemli-Opitz syndrome and autism spectrum disorder. Am J Psychiatry. 2007;164(11):1655–61.
Burks SR, Wright CL, McCarthy MM. Exploration of prostanoid receptor subtype regulating estradiol and prostaglandin E2 induction of spinophilin in developing preoptic area neurons. Neuroscience. 2007;146(3):1117–27.
Buyske S, Williams TA, Mars AE, et al. Analysis of case-parent trios at a locus with a deletion allele: association of GSTM1 with autism. BMC Genet. 2006;7:8.
Calderon F, Kim HY. Docosahexaenoic acid promotes neurite growth in hippocampal neurons. J Neurochem. 2004;90(4):979–88.
Castellone MD, Teramoto H, Williams BO, Druey KM, Gutkind JS. Prostaglandin E2 promotes colon cancer cell growth through a Gs-axin-beta-catenin signaling axis. Science. 2005;310(5753):1504–10.
Chauhan A, Chauhan V, Brown WT, Cohen I. Oxidative stress in autism: increased lipid peroxidation and reduced serum levels of ceruloplasmin and transferrin – the antioxidant proteins. Life Sci. 2004;75(21):2539–49.
Choe E. Chemistry and Reactions of Reactive Oxygen Species in Lipid Oxidation. In A. Kamal-Eldin & D. Min (Eds.), Lipid Oxidation Pathways. 2010;2:31–50. Urbana, IL: AOCS Publishing.
Christiaens I, Zaragoza DB, Guilbert L, Robertson SA, Mitchell BF, Olson DM. Inflammatory processes in preterm and term parturition. J Reprod Immunol. 2008;79(1):50–7.
Ciani L, Salinas PC. WNTs in the vertebrate nervous system: from patterning to neuronal connectivity. Nat Rev Neurosci. 2005;6(5):351–62.
Clandinin MT, Jumpsen J, Suh M. Relationship between fatty acid accretion, membrane composition, and biologic functions. J Pediatr. 1994;125(5 Pt 2):S25–32.
Craddock N, Lendon C. Chromosome workshop: chromosomes 11, 14, and 15. Am J Med Genet. 1999;88(3):244–54.
Crawford MA, Hassam AG, Stevens PA. Essential fatty acid requirements in pregnancy and lactation with special reference to brain development. Prog Lipid Res. 1981;20:31–40.
Crawford MA, Doyle W, Drury P, Lennon A, Costeloe K, Leighfield M. n-6 and n-3 fatty acids during early human development. J Intern Med Suppl. 1989;731:159–69.
De Felice C, Ciccoli L, Leoncini S, et al. Systemic oxidative stress in classic Rett syndrome. Free Radic Biol Med. 2009;47(4):440–8.
de la Cochetière MF, Rougé C, Darmaun D, Rozé JC, Potel G, Gras-Leguen C. Intestinal microbiota in neonates and preterm infants: a review. Curr Pediatr Rev. 2007;3:21–34.
de Vries HE, Blom-Roosemalen MC, van Oosten M, et al. The influence of cytokines on the integrity of the blood–brain barrier in vitro. J Neuroimmunol. 1996;64(1):37–43.
Deth R, Muratore C, Benzecry J, Power-Charnitsky VA, Waly M. How environmental and genetic factors combine to cause autism: a redox/methylation hypothesis. Neurotoxicology. 2008;29(1):190–201.
Dubois A, Rattaz C, Pry R, Baghdadli A. Autism and pain – a literature review. Pain Res Manag. 2010;15(4):245–53.
Evans T. Fishing for a WNT-PGE2 link: beta-catenin is caught in the stem cell net-work. Cell Stem Cell. 2009;4(4):280–2.
Evans TA, Siedlak SL, Lu L, et al. The autistic phenotype exhibits a remarkably localized modification of brain protein by products of free radical-induced lipid oxidation. Am J Biotechno Biochem. 2008;4(2):61–72.
Farooqui AA, Horrocks LA, Farooqui T. Modulation of inflammation in brain: a matter of fat. J Neurochem. 2007;101(3):577–99.
Fatemi SH, Halt AR, Realmuto G, et al. Purkinje cell size is reduced in cerebellum of patients with autism. Cell Mol Neurobiol. 2002;22(2):171–5.
Fatemi SH, Pearce DA, Brooks AI, Sidwell RW. Prenatal viral infection in mouse causes differential expression of genes in brains of mouse progeny: a potential animal model for schizophrenia and autism. Synapse. 2005;57(2):91–9.
Fatemi SH, Reutiman TJ, Folsom TD, et al. Maternal infection leads to abnormal gene regulation and brain atrophy in mouse offspring: implications for genesis of neurodevelopmental disorders. Schizophr Res. 2008;99(1–3):56–70.
Ferrucci L, Cherubini A, Bandinelli S, et al. Relationship of plasma polyunsaturated fatty acids to circulating inflammatory markers. J Clin Endocrinol Metab. 2006;91(2):439–46.
Filomeni G, Ciriolo MR. Redox control of apoptosis: an update. Antioxid Redox Signal. 2006;8(11–12):2187–92.
Fitzgerald DW, Bezak K, Ocheretina O, et al. The effect of HIV and HPV coinfection on cervical COX-2 expression and systemic prostaglandin E2 levels. Cancer Prev Res (Phila). 2012;5(1):34–40.
Galceran J, Farinas I, Depew MJ, Clevers H, Grosschedl R. Wnt3a-/-- like phenotype and limb deficiency in Lef1(-/-)Tcf1(-/-) mice. Genes Dev. 1999;13(6):709–17.
Gaulden J, Reiter JF. Neur-ons and neur-offs: regulators of neural induction in vertebrate embryos and embryonic stem cells. Hum Mol Genet. 2008;17(R1):R60–6.
Genest DR, Di Salvo D, Rosenblatt MJ, Holmes LB. Terminal transverse limb defects with tethering and omphalocele in a 17 week fetus following first trimester misoprostol exposure. Clin Dysmorphol. 1999;8(1):53–8.
Genetos DC, Yellowley CE, Loots GG. Prostaglandin E2 signals through PTGER2 to regulate sclerostin expression. PLoS One. 2011;6(3):e17772.
Ghanizadeh A, Akhondzadeh S, Hormozi, Makarem A, Abotorabi M, Firoozabadi A. Glutathione-related Factors and Oxidative Stress in Autism, a Review. Curr Med Chem. 2012;19(23):4000–5.
Gilbert SF. Developmental biology. 7th ed. Sunderland: Sinauer Associates; 2003.
Goessling W, North TE, Loewer S, et al. Genetic interaction of PGE2 and Wnt signaling regulates developmental specification of stem cells and regeneration. Cell. 2009;136(6):1136–47.
Gorrindo P, Williams KC, Lee EB, Walker LS, McGrew SG, Levitt P. Gastrointestinal dysfunction in autism: parental report, clinical evaluation, and associated factors. Autism Res. 2012;5(2):101–8.
Gross GA, Imamura T, Luedke C, et al. Opposing actions of prostaglandins and oxytocin determine the onset of murine labor. Proc Natl Acad Sci USA. 1998;95(20):11875–9.
Guizy M, David M, Arias C, et al. Modulation of the atrial specific Kv1.5 channel by the n-3 polyunsaturated fatty acid, alpha-linolenic acid. J Mol Cell Cardiol. 2008;44(2):323–35.
Haag M. Essential fatty acids and the brain. Can J Psychiatry. 2003;48(3):195–203.
Hall AC, Lucas FR, Salinas PC. Axonal remodeling and synaptic differentiation in the cerebellum is regulated by WNT-7a signaling. Cell. 2000;100(5):525–35.
Harvey L, Boksa P. Prenatal and postnatal animal models of immune activation: Relevance to a range of neurodevelopmental disorders. Dev Neurobiol. Oct 2012;72(10):1335–48.
Harvey RJ, Depner UB, Wassle H, et al. GlyR alpha3: an essential target for spinal PGE2-mediated inflammatory pain sensitization. Science. 2004;304(5672):884–7.
Hinz B, Brune K. Cyclooxygenase-2 – 10 years later. J Pharmacol Exp Ther. 2002;300(2):367–75.
Hoffman DR, Boettcher JA, Diersen-Schade DA. Toward optimizing vision and cognition in term infants by dietary docosahexaenoic and arachidonic acid supplementation: a review of randomized controlled trials. Prostaglandins Leukot Essent Fatty Acids. 2009;81(2–3):151–8.
James SJ, Cutler P, Melnyk S, et al. Metabolic biomarkers of increased oxidative stress and impaired methylation capacity in children with autism. Am J Clin Nutr. 2004;80(6):1611–7.
Jiang J, Ganesh T, Du Y, et al. Neuroprotection by selective allosteric potentiators of the EP2 prostaglandin receptor. Proc Natl Acad Sci USA. 2010;107(5):2307–12.
Johnson SM, Hollander E. Evidence that eicosapentaenoic acid is effective in treating autism. J Clin Psychiatry. 2003;64(7):848–9.
Jonakait GM, Ni L. Prostaglandins compromise basal forebrain cholinergic neuron differentiation and survival: action at EP1/3 receptors results in AIF-induced death. Brain Res. 2009;1285:30–41.
Kaufmann WE, Worley PF, Taylor CV, Bremer M, Isakson PC. Cyclooxygenase-2 expression during rat neocortical development and in Rett syndrome. Brain Dev. 1997;19(1):25–34.
Kitase Y, Barragan L, Qing H, et al. Mechanical induction of PGE2 in osteocytes blocks glucocorticoid-induced apoptosis through both the beta-catenin and PKA pathways. J Bone Miner Res. 2010;25(12):2657–68.
Koch H, Huh SE, Elsen FP, et al. Prostaglandin E2-induced synaptic plasticity in neocortical networks of organotypic slice cultures. J Neurosci. 2010;30(35):11678–87.
Kohane IS, McMurry A, Weber G, et al. The co-morbidity burden of children and young adults with autism spectrum disorders. PLoS One. 2012;7(4):e33224.
Krey JF, Dolmetsch RE. Molecular mechanisms of autism: a possible role for Ca2+ signaling. Curr Opin Neurobiol. 2007;17(1):112–9.
Kwiecien S, Konturek PC, Sliwowski Z, et al. Interaction between selective cyclooxygenase inhibitors and capsaicin-sensitive afferent sensory nerves in pathogenesis of stress-induced gastric lesions. Role of oxidative stress. J Physiol Pharmacol. 2012;63(2):143–51.
Ladesich JB, Pottala JV, Romaker A, Harris WS. Membrane level of omega-3 docosahexaenoic acid is associated with severity of obstructive sleep apnea. J Clin Sleep Med. 2011;7(4):391–6.
Lauritzen L, Hansen HS, Jorgensen MH, Michaelsen KF. The essentiality of long chain n-3 fatty acids in relation to development and function of the brain and retina. Prog Lipid Res. 2001;40(1–2):1–94.
Lawrence GD. The fats of life: essential fatty acids in health and disease. New Brunswick: Rutgers University Press; 2010.
Legler DF, Bruckner M, Uetz-von Allmen E, Krause P. Prostaglandin E2 at new glance: novel insights in functional diversity offer therapeutic chances. Int J Biochem Cell Biol. 2010;42(2):198–201.
Lennon PA, Cooper ML, Peiffer DA, et al. Deletion of 7q31.1 supports involvement of FOXP2 in language impairment: clinical report and review. Am J Med Genet A. 2007;143A(8):791–8.
Libbey JE, Sweeten TL, McMahon WM, Fujinami RS. Autistic disorder and viral infections. J Neurovirol. 2005;11(1):1–10.
Lin CJ, Chien SC, Chen CP. The use of misoprostol in termination of second-trimester pregnancy. Taiwan J Obstet Gynecol. 2011;50(3):275–82.
Lin PI, Chien YL, Wu YY, et al. The WNT2 gene polymorphism associated with speech delay inherent to autism. Res Dev Disabil. 2012;33(5):1533–40.
Liu XH, Kirschenbaum A, Weinstein BM, Zaidi M, Yao S, Levine AC. Prostaglandin E2 modulates components of the Wnt signaling system in bone and prostate cancer cells. Biochem Biophys Res Commun. 2010;394(3):715–20.
Loftin CD, Tiano HF, Langenbach R. Phenotypes of the COX-deficient mice indicate physiological and pathophysiological roles for COX-1 and COX-2. Prostaglandins Other Lipid Mediat. 2002;68–69:177–85.
Ma DQ, Cuccaro ML, Jaworski JM, et al. Dissecting the locus heterogeneity of autism: significant linkage to chromosome 12q14. Mol Psychiatry. 2007;12(4):376–84.
Marin P, Hamon B, Glowinski J, Premont J. Nicotine-induced inhibition of neuronal phospholipase A2. J Pharmacol Exp Ther. 1997;280(3):1277–83.
Martinez M. Tissue levels of polyunsaturated fatty acids during early human development. J Pediatr. 1992;120(4 Pt 2):S129–38.
Meguid NA, Atta HM, Gouda AS, Khalil RO. Role of polyunsaturated fatty acids in the management of Egyptian children with autism. Clin Biochem. 2008;41(13):1044–8.
Ming X, Johnson WG, Stenroos ES, Mars A, Lambert GH, Buyske S. Genetic variant of glutathione peroxidase 1 in autism. Brain Dev. 2010;32(2):105–9.
Morales E, Bustamante M, Gonzalez JR, et al. Genetic variants of the FADS gene cluster and ELOVL gene family, colostrums LC-PUFA levels, breastfeeding, and child cognition. PLoS One. 2011;6(2):e17181.
Morris CR, Agin MC. Syndrome of allergy, apraxia, and malabsorption: characterization of a neurodevelopmental phenotype that responds to omega 3 and vitamin E supplementation. Altern Ther Health Med. 2009;15(4):34–43.
Mostafa GA, El-Hadidi ES, Hewedi DH, Abdou MM. Oxidative stress in Egyptian children with autism: relation to autoimmunity. J Neuroimmunol. 2010;219(1–2):114–8.
Murakami M, Kudo I. Phospholipase A2. J Biochem. 2002;131(3):285–92.
O'Neill GP, Ford-Hutchinson AW. Expression of mRNA for cyclooxygenase-1 and cyclooxygenase-2 in human tissues. FEBS Lett. 1993;330(2):156–60.
Ono H, Sakamoto A, Sakura N. Plasma total glutathione concentrations in healthy pediatric and adult subjects. Clin Chim Acta. 2001;312(1–2):227–9.
Oshima H, Oshima M. Mouse models of gastric tumors: Wnt activation and PGE2 induction. Pathol Int. 2010;60(9):599–607.
Oshima H, Oguma K, Du YC, Oshima M. Prostaglandin E2, Wnt, and BMP in gastric tumor mouse models. Cancer Sci. 2009;100(10):1779–85.
Patrick L, Salik R. The effect of essential fatty acid supplementation on language development and learning skills in autism and Asperger’s syndrome. Autism Asperger’s Digest. 2005; Jan–Feb:36–7.
Pepicelli O, Fedele E, Berardi M, et al. Cyclo-oxygenase-1 and -2 differently contribute to prostaglandin E2 synthesis and lipid peroxidation after in vivo activation of N-methyl-D-aspartate receptors in rat hippocampus. J Neurochem. 2005;93(6):1561–7.
Politi P, Cena H, Comelli M, et al. Behavioral effects of omega-3 fatty acid supplementation in young adults with severe autism: an open label study. Arch Med Res. 2008;39(7):682–5.
Ponzio NM, Servatius R, Beck K, Marzouk A, Kreider T. Cytokine levels during pregnancy influence immunological profiles and neurobehavioral patterns of the offspring. Ann N Y Acad Sci. 2007;1107:118–28.
Pratico D, Lawson JA, Rokach J, FitzGerald GA. The isoprostanes in biology and medicine. Trends Endocrinol Metab. 2001;12(6):243–7.
Ricciotti E, FitzGerald GA. Prostaglandins and inflammation. Arterioscler Thromb Vasc Biol. 2011;31(5):986–1000.
Rice D, Barone Jr S. Critical periods of vulnerability for the developing nervous system: evidence from humans and animal models. Environ Health Perspect. 2000;108 Suppl 3:511–33.
Rothwell NJ, Hopkins SJ. Cytokines and the nervous system. I: expression and recognition. Trends Neurosci. 1995;18(2):83–8.
Russo I, Amornphimoltham P, Weigert R, Barlati S, Bosetti F. Cyclooxygenase-1 is involved in the inhibition of hippocampal neurogenesis after lipopolysaccharide-induced neuroinflammation. Cell Cycle. 2011;10(15):2568–73.
Sahores M, Salinas PC. Activity-mediated synapse formation a role for Wnt-Fz signaling. Curr Top Dev Biol. 2011;97:119–36.
Saint-Dizier M, Guyader-Joly C, Charpigny G, Grimard B, Humblot P, Ponter AA. Expression of enzymes involved in the synthesis of prostaglandin E2 in bovine in vitro-produced embryos. Zygote. 2011;19(3):277–83.
Sang N, Chen C. Lipid signaling and synaptic plasticity. Neuroscientist. 2006;12(5):425–34.
Sastry PS. Lipids of nervous tissue: composition and metabolism. Prog Lipid Res. 1985;24(2):69–176.
Schultz ST, Klonoff-Cohen HS, Wingard DL, et al. Breastfeeding, infant formula supplementation, and autistic disorder: the results of a parent survey. Int Breastfeed J. 2006;1:16.
Sedel F, Bechade C, Vyas S, Triller A. Macrophage-derived tumor necrosis factor alpha, an early developmental signal for motoneuron death. J Neurosci. 2004;24(9):2236–46.
Shi L, Fatemi SH, Sidwell RW, Patterson PH. Maternal influenza infection causes marked behavioral and pharmacological changes in the offspring. J Neurosci. 2003;23(1):297–302.
Shi L, Smith SE, Malkova N, Tse D, Su Y, Patterson PH. Activation of the maternal immune system alters cerebellar development in the offspring. Brain Behav Immun. 2009;23(1):116–23.
Shukuri M, Takashima-Hirano M, Tokuda K, et al. In vivo expression of cyclooxygenase-1 in activated microglia and macrophages during neuroinflammation visualized by PET with 11C-ketoprofen methyl ester. J Nucl Med. 2011;52(7):1094–101.
Shulman RG, Rothman DL, Behar KL, Hyder F. Energetic basis of brain activity: implications for neuroimaging. Trends Neurosci. 2004;27(8):489–95.
Shultz SR, Macfabe DF, Martin S, et al. Intracerebroventricular injections of the enteric bacterial metabolic product propionic acid impair cognition and sensorimotor ability in the Long-Evans rat: further development of a rodent model of autism. Behav Brain Res. 2009;200(1):33–41.
Sies H. Oxidative stress: oxidants and antioxidants. Exp Physiol. 1997;82(2):291–5.
Sikora DM, Pettit-Kekel K, Penfield J, Merkens LS, Steiner RD. The near universal presence of autism spectrum disorders in children with Smith-Lemli-Opitz syndrome. Am J Med Genet A. 2006;140(14):1511–8.
Sliwinski S, Croonenberghs J, Christophe A, Deboutte D, Maes M. Polyunsaturated fatty acids: do they have a role in the pathophysiology of autism? Neuro Endocrinol Lett. 2006;27(4):465–71.
Soleymaninejadian E, Pramanik K, Samadian E. Immunomodulatory properties of mesenchymal stem cells: cytokines and factors. Am J Reprod Immunol. 2012;67(1):1–8.
Stolp H, Neuhaus A, Sundramoorthi R, Molnar Z. The long and the short of it: gene and environment interactions during early cortical development and consequences for long-term neurological disease. Front Psychiatry. 2012;3:50.
Su HM. Mechanisms of n-3 fatty acid-mediated development and maintenance of learning memory performance. J Nutr Biochem. 2010;21(5):364–73.
Sugimoto Y, Narumiya S. Prostaglandin E receptors. J Biol Chem. 2007;282(16):11613–7.
Tallberg T, Dabek J, Hallamaa R, Atroshi F. Lipidomics: the function of vital lipids in embryogenesis preventing autism spectrum disorders, treating sterile inflammatory diatheses with a lymphopoietic central nervous system component. J lipids. 2011;2011:137175.
Tamiji J, Crawford DA. Misoprostol elevates intracellular calcium in neuro-2a cells via protein kinase a. Biochem Biophys Res Commun. 2010a;399(4):565–70.
Tamiji J, Crawford DA. Prostaglandin E(2) and misoprostol induce neurite retraction in neuro-2a cells. Biochem Biophys Res Commun. 2010b;398(3):450–6.
Tamiji J, Crawford DA. The neurobiology of lipid metabolism in autism spectrum disorders. Neurosignals. 2010c;18(2):98–112.
Tassoni D, Kaur G, Weisinger RS, Sinclair AJ. The role of eicosanoids in the brain. Asia Pac J Clin Nutr. 2008;17 Suppl 1:220–8.
Thomas RH, Foley KA, Mepham JR, Tichenoff LJ, Possmayer F, MacFabe DF. Altered brain phospholipid and acylcarnitine profiles in propionic acid infused rodents: further development of a potential model of autism spectrum disorders. J Neurochem. 2010;113(2):515–29.
Tierney E, Bukelis I, Thompson RE, et al. Abnormalities of cholesterol metabolism in autism spectrum disorders. Am J Med Genet B Neuropsychiatr Genet. 2006;141B(6):666–8.
Vancassel S, Durand G, Barthelemy C, et al. Plasma fatty acid levels in autistic children. Prostaglandins Leukot Essent Fatty Acids. 2001;65(1):1–7.
Vane JR. Inhibition of prostaglandin synthesis as a mechanism of action for aspirin-like drugs. Nat New Biol. 1971;231(25):232–5.
Wall R, Ross RP, Fitzgerald GF, Stanton C. Fatty acids from fish: the anti-inflammatory potential of long-chain omega-3 fatty acids. Nutr Rev. 2010;68(5):280–9.
Wayman GA, Impey S, Marks D, et al. Activity-dependent dendritic arborization mediated by CaM-kinase I activation and enhanced CREB-dependent transcription of Wnt-2. Neuron. 2006;50(6):897–909.
Wegiel J, Kuchna I, Nowicki K, et al. The neuropathology of autism: defects of neurogenesis and neuronal migration, and dysplastic changes. Acta Neuropathol. 2010;119(6):755–70.
Wiest MM, German JB, Harvey DJ, Watkins SM, Hertz-Picciotto I. Plasma fatty acid profiles in autism: a case–control study. Prostaglandins Leukot Essent Fatty Acids. 2009;80(4):221–7.
Willatts P, Forsyth JS, DiModugno MK, Varma S, Colvin M. Effect of long-chain polyunsaturated fatty acids in infant formula on problem solving at 10 months of age. Lancet. 1998;352(9129):688–91.
Williams TA, Mars AE, Buyske SG, et al. Risk of autistic disorder in affected offspring of mothers with a glutathione S-transferase P1 haplotype. Arch Pediatr Adolesc Med. 2007;161(4):356–61.
Wong C, Li H, Crawford DA. The role of prostaglandin E2 signaling pathway in neuroectodermal stem cell function. Poster# 151.08/V6. Society for Neuroscience – Annual Meeting; Sunday, 13 Nov 2011; 2011. Washington, DC.
Wong C, Li H, Crawford DA. The implications of prostaglandin E2-wnt signaling pathway interaction in autism. Poster# 108.128. International meeting for autism research; Thursday, 17 May 2012; 2012, Toronto, Ontario, Canada.
Wu A, Ying Z, Gomez-Pinilla F. Docosahexaenoic acid dietary supplementation enhances the effects of exercise on synaptic plasticity and cognition. Neuroscience. 2008;155(3):751–9.
Yamagata K, Andreasson KI, Kaufmann WE, Barnes CA, Worley PF. Expression of a mitogen-inducible cyclooxygenase in brain neurons: regulation by synaptic activity and glucocorticoids. Neuron. 1993;11(2):371–86.
Yao Y, Walsh WJ, McGinnis WR, Pratico D. Altered vascular phenotype in autism: correlation with oxidative stress. Arch Neurol. 2006;63(8):1161–4.
Yehuda S, Rabinovitz S, Mostofsky DI. Essential fatty acids are mediators of brain biochemistry and cognitive functions. J Neurosci Res. 1999;56(6):565–70.
Yoo HJ, Cho IH, Park M, et al. Association between PTGS2 polymorphism and autism spectrum disorders in Korean trios. Neurosci Res. 2008;62(1):66–9.
Zerbo O, Iosif AM, Walker C, Ozonoff S, Hansen RL, Hertz-Picciotto I. Is Maternal Influenza or Fever During Pregnancy Associated with Autism or Developmental Delays? Results from the CHARGE (CHildhood Autism Risks from Genetics and Environment) Study. J Autism Dev Disord. Jan 2013;43(1):25–33.
Zhang J, Rivest S. Anti-inflammatory effects of prostaglandin E2 in the central nervous system in response to brain injury and circulating lipopolysaccharide. J Neurochem. 2001;76(3):855–64.
Zhou CJ, Zhao C, Pleasure SJ. Wnt signaling mutants have decreased dentate granule cell production and radial glial scaffolding abnormalities. J Neurosci. 2004;24(1):121–6.
Zhou CJ, Borello U, Rubenstein JL, Pleasure SJ. Neuronal production and precursor proliferation defects in the neocortex of mice with loss of function in the canonical Wnt signaling pathway. Neuroscience. 2006;142(4):1119–31.
Zhu Y, Yu T, Zhang XC, Nagasawa T, Wu JY, Rao Y. Role of the chemokine SDF-1 as the meningeal attractant for embryonic cerebellar neurons. Nat Neurosci. 2002;5(8):719–20.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer Science+Business Media New York
About this entry
Cite this entry
Wong, C., Crawford, D.A. (2014). Lipid Signalling in the Pathology of Autism Spectrum Disorders. In: Patel, V., Preedy, V., Martin, C. (eds) Comprehensive Guide to Autism. Springer, New York, NY. https://doi.org/10.1007/978-1-4614-4788-7_68
Download citation
DOI: https://doi.org/10.1007/978-1-4614-4788-7_68
Publisher Name: Springer, New York, NY
Print ISBN: 978-1-4614-4787-0
Online ISBN: 978-1-4614-4788-7
eBook Packages: Behavioral ScienceReference Module Humanities and Social SciencesReference Module Business, Economics and Social Sciences