Abstract
Ascorbic acid (vitamin C) occurs physiologically as the ascorbate anion. Ascorbate is a water-soluble antioxidant found throughout the body, but occurs in especially high concentrations (10 mM) in neurons. In the central nervous system (CNS), ascorbate is part of the antioxidant network, and as such is normally neuroprotective. Recent studies suggest that ascorbate may play a unique role in the CNS by permitting signaling by a novel diffusible messenger, hydrogen peroxide (H2O2), yet providing protection from damage from the reactive hydroxyl radical, which can be formed from H2O2 oxidation. In order to learn about the function of ascorbate in the CNS, it is necessary to understand how it is compartmentalized. Ascorbate enters the CNS primarily by active transport at the choroid plexus, but also by uptake of oxidized ascorbate, dehydroascorbate, via glucose transporters. After entry into the cerebrospinal fluid (CSF), it diffuses into brain extracellular fluid (ECF), where its concentration is regulated homeostatically, as well as dynamically. From ECF, ascorbate is taken up into brain cells, where it is further concentrated up to 20-fold. Thus, brain ascorbate is located predominantly in the intracellular compartment of brain tissue, with complementary distribution between neurons and glia that may contribute importantly to its role as a neuroprotective agent that also permits redox signaling.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Ascorbate Biosynthesis and Chemistry
Ascorbic acid is a water-soluble sugar acid, with a molecular weight of 176.13. It has two dissociable protons with pKa values of 4.2 and 11.8 (Davies et al. 1991), so that it occurs as the monovalent anion, ascorbate, at physiological pH. The enediol structure of ascorbate enables it to be an electron donor: loss of two electrons leads to formation of dehydroascorbate (DHA), the final oxidation product. Most free radicals (molecules with one unpaired electron) generated by biological systems can cause a one-electron oxidation of ascorbate to form semi-dehydroascorbate, also known as the ascorbyl radical. Detection of ascorbyl radicals using electron-spin resonance has been used as an index of oxidative stress (Buettner and Jurkiewicz 1993). This radical intermediate is also formed in enzymatic reactions that involve ascorbate as an electron-donating co-factor (Diliberto et al. 1987).
The roles of ascorbate as an antioxidant and free radical scavenger are derived from its properties as an electron donor. Ascorbate has a relatively low redox potential and is therefore a broad-spectrum radical scavenger that is effective against peroxyl and hydroxyl radicals, superoxide, singlet oxygen, and peroxynitrite (Nishikimi 1975; Bodannes and Chan 1979; Machlin and Bendich 1987; Cohen 1994; Vatassery 1996). As part of the predominantly intracellular antioxidant network, ascorbate acts in concert with other low-molecular-weight substances, including glutathione (GSH) and vitamin E, as well as antioxidant enzymes, including superoxide dismutase and GSH peroxidase (Cohen 1994). Although redox reactions with ascorbate occur in the aqueous phase, this can prevent oxidation of lipid-soluble vitamin E (α-tocopherol), which can in turn stop peroxidation of cell membranes (Seregi et al. 1978; Niki 1991; Buettner 1993; Sato et al. 1993). Oxidized ascorbate, semi-dehydroascorbate and DHA, can be recycled by intracellular thiols, including GSH (Meister 1994; Winkler et al. 1994), and in some cells by a GSH-dependent DHA reductase (Rose 1993; Fornai et al. 1999). In the brain, immunocytochemical studies show regionally distinct patterns of localization for DHA reductase, with staining primarily in neurons (Fornai et al. 2001). Additionally, glutaredoxins, which are GSH-dependent reducing enzymes, also have DHA reductase activity (Washburn and Wells 1999; Ehrhart and Zeevalk 2003), as do thioredoxin reductase (May et al. 1997) and omega class GSH transferases (Board et al. 2000). Oxidized GSH, in turn, is recycled by GSH reductase (Meister 1994).
Another key function of ascorbate is to serve as an electron-donating enzyme co-factor. The most well-known ascorbate-dependent enzyme processes include collagen biosynthesis via hydroxylation reactions (Barnes 1975), noradrenaline/adrenaline synthesis by dopamine-β-hydroxylase (Diliberto et al. 1987), and myelin formation by enabling Schwann cells to lay down the basal lamina (Carey and Todd 1987; Eldridge et al. 1987). Promoting myelin formation may be the mechanism by which therapeutically administered ascorbate enhances myelination and reverses motor deficits in a mouse model of Charcot-Marie-Tooth disease, which is the most common hereditary peripheral neuropathy (Passage et al. 2004). More recently, it has been recognized that ascorbate is an essential factor for the prolyl 4-hydroxylases that control hypoxia inducible factor (HIF), a ubiquitous transcription factor that plays a key role in the cellular response to low oxygen conditions (Vissers et al. 2007; Pagé et al. 2008). Given the role of HIF in the transcriptional regulation of genes that can provide compensation for hypoxia, metabolic disruption, or oxidative stress (Siddiq et al. 2007), understanding the role of ascorbate, as well as ascorbate depletion, in HIF stabilization is an important emerging area in ascorbate research.
In most animals, ascorbic acid is synthesized from glucose in the following simplified pathway:
d-glucose → d-glucuronic acid → l-gulonic acid → l-gulono-γ-lactone → l-ascorbic acid
Humans, nonhuman primates, and guinea pigs cannot synthesize ascorbate because they carry a nonfunctional gene for the enzyme, l-gulono-γ-lactone oxidase, which catalyzes the last step of ascorbate biosynthesis (Nishikimi et al. 1994). Importantly, mutations in this gene were not fatal to the species that carry it for several reasons. First, ascorbate is available from dietary sources and is readily absorbed from the gut (Kallner et al. 1977). In addition, in animals that can synthesize ascorbate, synthesis occurs only in liver (mammals) or kidney (reptiles) (Chatterjee et al. 1975), with subsequent distribution to all other tissues via plasma. Consequently, all tissues have mechanisms for uptake and storage of ascorbate at cell-specific levels. In humans, the effects of vitamin C deficiency, which can lead to scurvy, were noticed first during long sea voyages, away from fresh fruits and vegetables, with primary symptoms caused by loss of collagen synthesis, although depression is also an early consequence of ascorbate deficiency (Carpenter 1986).
2 Ascorbate Transport and Transporters
For many years, understanding of ascorbate regulation in the CNS was impeded by the lack of molecular information about the transporters responsible for ascorbate uptake into the brain and into brain cells. This changed profoundly when Tsukaguchi et al. (1999) described the first members of a new family of Na+-dependent vitamin C [ascorbate] transporters (SVCT1 and SVCT2), isolated from rat cDNA libraries. These isoforms share 65% amino acid homology and facilitate electrogenic, Na+-dependent uptake of ascorbate with similar affinities (Tsukaguchi et al. 1999). The major difference between the transporter isoforms appears to be their complementary localization, with SVCT1 in kidney, liver and lung, for example, and SVCT2 in neural, neuroendocrine, exocrine and endothelial tissues. Only SVCT2 is found in the brain (Tsukaguchi et al. 1999). Shortly after this initial report, two human isoforms were cloned from human cDNA libraries (Rajan et al. 1999; Daruwala et al. 1999). Human SVCT2 shares a 95% sequence homology with rat SVCT2 and is also found in the brain (Rajan et al. 1999). SVCT1 and SVCT2 were subsequently classified as members of the SLC23 human gene family, which also contains two orphan members, SVCT3 and SVCT4 (for reviews, see Takanaga et al. 2004; Savini et al. 2008).
Consistent with the key role of the choroid plexus in transporting ascorbate into the CNS (Spector and Lorenzo 1973) (Fig. 37.1), in situ hybridization in rat brain indicates that this organ, which produces cerebrospinal fluid (CSF) from plasma, expresses high levels of SCVT2 (Tsukaguchi et al. 1999). Importantly, SVCT2 is also found in high levels in neurons, but not in glial cells (Tsukaguchi et al. 1999; Berger and Hediger 2000; Astuya et al. 2005), which is reflected in a ten-fold higher concentration of ascorbate in neurons than in glia, as discussed in Sect. 3. Transporter expression occurs in both excitatory and inhibitory neurons, including glutamatergic pyramidal cells of the hippocampus, glutamatergic granule cells of the cerebellum, and GABAergic cerebellar Purkinje cells (Tsukaguchi et al. 1999). Intriguingly, expression levels of SCVT2 are plastic, although the regulatory mechanisms are incompletely understood. For example, although apparently absent in glial cells in situ, SVCT2 can be expressed in astrocytes in culture (Berger and Hediger 2000); moreover, the transporters expressed are functional, as a number of studies have examined characteristics of ascorbate uptake in cultured astrocytes (e.g., Wilson 1989). This plasticity is physiologically relevant: SVCT2 is upregulated in both neurons and glia in the area surrounding a cerebral infarct during reperfusion in an experimental stroke model involving occlusion of the middle cerebral artery (Berger et al. 2003).
Ascorbate transport, compartmentalization, and concentrations in the CNS. Whether ascorbate is synthesized in liver or kidney or acquired from the diet, it is distributed to all organs via plasma; plasma ascorbate concentration is typically 50 μM (see Sect. 3 for references). Active transport at the choroid plexus, via the SVCT2 isoform of the ascorbate transporter is the first step of brain entry of ascorbate. Transport via the choroid plexus, which is found in the cerebral ventricles, accumulates ascorbate in ventricular cerebrospinal fluid (CSF) to a concentration of 500 μM. This pool of ascorbate is contiguous with the extracellular fluid (ECF) compartment of the brain, so that ascorbate originating in the CSF is distributed throughout the CNS via ECF (gray arrow). Ascorbate can also enter brain ECF at the blood-brain barrier at the level of brain capillaries; however, this presumably occurs via GLUT1-facilitated transport of oxidized ascorbate, DHA, as brain capillaries do not express SVCT2. Existing evidence, discussed in Sect. 2, indicates that this is a minor route for ascorbate entry into the CNS. The extracellular concentration of ascorbate ([Asc]o) is homeostatically regulated in a range of 200–400 μM, with dynamic modulation that is glutamate dependent, as discussed in Sect. 4. Ascorbate is taken up from ECF into neurons and glia. In neurons, ascorbate is transported via SVCT2; however, glia do not normally express SVCT2, leading to the suggestion that uptake of DHA via GLUT1 may be a primary route of entry for glial ascorbate
An additional mechanism for ascorbate entry across the blood-brain barrier (BBB) can occur through facilitated transport of oxidized ascorbate, DHA by a glucose transporter, GLUT1, with subsequent reduction of DHA back to ascorbate by thiols and DHA reductase activity (Agus et al. 1997) (Fig. 37.1). The fact that ascorbate is found almost exclusively in the reduced form in plasma (Dhariwal et al. 1991), however, suggests that transport of DHA into the CNS via GLUT1 is a minor route of entry for ascorbate (Tsukaguchi et al. 1999). The predominant role of SVCT2 in normal maintenance of brain ascorbate content was confirmed by studies in transgenic mice in which the mouse analogue of SVCT2 (Slc23a1) was knocked out (Sotiriou et al. 2002). Mice with this mutation died within a few minutes of birth from respiratory failure and widespread brain hemorrhage. Significantly, brain tissue from these animals was virtually devoid of ascorbate, demonstrating that active transport via SVCT2 is how ascorbate enters the CNS (Sotiriou et al. 2002).
3 Ascorbate Concentrations in Plasma, Cerebrospinal Fluid, Extracellular Fluid, and Brain Cells
As discussed in Sect. 2, the first step in providing ascorbate to the CNS is via stereospecific, Na+-dependent transport at the choroid plexus via SVCT2 (Spector and Lorenzo 1973; Tsukaguchi et al. 1999). This uptake process transfers ascorbate from the blood into CSF (Fig. 37.1). In rat brain, this process accumulates ascorbate in CSF to a concentration of about 500 μM (Stamford et al. 1984), which is tenfold higher than the typically 50 μM concentration found in plasma in a variety of mammalian species (Hornig 1975; Chatterjee et al. 1975; Spector 1977; Drew et al. 1999) (Fig. 37.1). Although ascorbate can also enter the CNS by carrier-mediated uptake at the level of brain capillaries via GLUT1 (Agus et al. 1997) and by simple diffusion across brain capillaries (Lam and Daniel 1986) (Fig. 37.1), these capillaries do not express SVCT2 (Tsukaguchi et al. 1999; Qiao and May 2008), offering further evidence that the choroid plexus is the primary site of ascorbate entry.
Brain and spinal cord CSF is contiguous with the extracellular fluid (ECF) that surrounds brain cells, permitting equilibrium of CSF ascorbate concentration with that in ECF as seen with other extracellular molecules (e.g., Ichimura et al. 1991). Basal ascorbate concentration in ECF (or extracellular ascorbate concentration, [Asc]o), is 200–400 μM (Fig. 37.1), with the lower limit determined in brain slices (McIlwain et al. 1956; Schenk et al. 1982) and the upper limit determined in vivo (Stamford et al. 1984; Miele and Fillenz 1996). From ECF, ascorbate is transported into brain cells (Spector and Lorenzo 1973; Kalir and Mytilenou 1992; Rice et al. 1994; Brahma et al. 2000; Rice and Russo-Menna 1998). The average concentration in neurons is estimated to be 10 mM, whereas the concentration in glia is only 1 mM (Rice and Russo-Menna 1998), consistent with expression of SVCT2 in neurons but not glia under normal conditions in situ (Tsukaguchi et al. 1999; Berger and Hediger 2000; Astuya et al. 2005) (Fig. 37.1). How do glia accumulate ascorbate? One hypothesis is that GLUT1 expressed by glia transport DHA, thereby providing an important mechanism for the recycling of ascorbate, should it become oxidized in the ECF through its role as an antioxidant (Astuya et al. 2005). Although ECF levels of DHA would be expected to be low, this process could contribute to maintenance of physiological levels of re-reduced ascorbate in glia. The mechanisms by which ascorbate concentrations are maintained at cell specific levels in either neurons or glia, however, are unknown.
Brain levels of ascorbate are region dependent, with higher tissue content in anterior structures like cortex and hippocampus, but progressively lower levels in more posterior regions like brainstem and spinal cord (Milby et al. 1982; Rice et al. 1995). This pattern largely reflects the increasing white matter content of posterior regions of the CNS, because the ascorbate content of glia-rich white matter is low compared to neuron-rich gray matter (Rice et al. 1995). Regional and sub-regional variation in neuron-to-glia ratio also contributes to tissue-specific levels. Difference in neuron density may also underlie gender differences in ascorbate content of several regions of rat brain, including hippocampus, with lower, estrogen-regulated levels in females than males (Kume-Kick and Rice 1998).
4 Homeostatic and Dynamic Regulation of Brain Extracellular Ascorbate
The brain, spinal cord, and adrenal glands have the highest ascorbate concentration in the body, as well as the greatest retention capacity (Hornig 1975). Under normal conditions, turnover of ascorbate in brain is about 2% per hour (Spector 1977). Under conditions of ascorbate deficiency, however, brain ascorbate content is retained tenaciously, with a loss of less than 2% per day in guinea pigs fed an ascorbate-free diet (Hughes et al. 1971). Thus, brain ascorbate levels are under strong homeostatic regulation (Spector 1977; Spector and Lorenzo 1973), which is largely due to the characteristics and location of SVCT2 in the CNS.
The Michaelis-Menten constant, K m, for ascorbate uptake by SVCT2 expressed in most native cells or heterologous cell systems is generally 20–40 μM (Savini et al. 2008), which is similar to the K m of 30–50 μM reported previously for ascorbate uptake by choroid plexus and brain slices (Spector and Lorenzo 1973; Spector 1977). However, cultured neurons have apparent K m values outside this range, with both higher affinity uptake indicated by a K m of ∼10 μM (Castro et al. 2001) and lower affinity uptake indicated by a K m of ∼100 μM (Castro et al. 2001; Qiu et al. 2007). Assuming that typical K m values of 20–40 μM reflect the state of SVCT2 in vivo rather than plastic changes from the in vitro environment required for analysis, these data indicate that the rate of SVCT2-mediated transport at the choroid plexus would be roughly half-maximal at normal plasma ascorbate concentrations (50 μM) and approach maximal rate at normal brain [Asc]o (200–400 μM). These conditions, coupled with the two-step uptake process involving transport from plasma to CSF then from CSF into neurons, contribute to the strong homeostasis of CNS ascorbate levels (Spector 1977).
Like overall brain ascorbate content, [Asc]o is also maintained homeostatically (Schenk et al. 1982). This was first shown in isolated mammalian brain slices, which rapidly lose ascorbate when incubated in ascorbate free-media. Up to 80% of tissue ascorbate content is lost from brain slices after only brief incubation (McIlwain et al. 1956; Schenk et al. 1982; Rice et al. 1994), possibly via reversal of the ascorbate transporter (Diliberto et al. 1987). In early studies of rat brain slices, McIlwain and colleagues found that the tissue lost ascorbate when incubated in media with ascorbate concentrations of less than 200 μM, but concentrated it in the presence of levels that were higher than this concentration (McIlwain et al. 1956). Subsequently, Schenk and colleagues used voltammetric microelectrodes to monitor ascorbate in the ECF of rat striatal slices during incubation in ascorbate-free medium and found that [Asc]o remained constant over an initial 30 min period while tissue content fell by 75% (Schenk et al. 1982). This suggested that [Asc]o was maintained homeostatically at the expense of intracellular stores. The mechanisms that determine the “set point” for [Asc]o are not yet understood.
Importantly, Meile and Fillenz discovered that [Asc]o is also regulated homeostatically in vivo, in awake, behaving animals (Miele and Fillenz 1996). In these studies, 100–1,000 μM ascorbate was perfused through a microdialysis probe, with voltammetric detection of [Asc]o in the tissue adjacent to the probe. Perfusion of ascorbate concentrations lower than 400 μM caused [Asc]o to fall, whereas higher concentrations caused [Asc]o to increase. After each perturbation, [Asc]o recovered within a few minutes, demonstrating efficient homeostasis. The concentration at which there was no net change in [Asc]o was 400 μM (Miele and Fillenz 1996), consistent with previous estimates for [Asc]o in vivo (Stamford et al. 1984). Homeostatic regulation of [Asc]o implies that the extracellular compartment of brain tissue is an important site of action for ascorbate.
Although brain [Asc]o is regulated homeostatically, dynamic, activity-dependent changes in [Asc]o also occur. Notably, [Asc]o in rat brain shows marked circadian variation (O’Neill et al. 1983); in these nocturnal animals, average [Asc]o is 20–60% higher throughout the brain during the dark cycle than in the light. Moreover, variation in [Asc]o is closely linked with motor behavior, with up to two-fold higher levels in motor striatum when an animal is active versus inactive (O’Neill et al. 1983). Consistent with these findings, the stimulant amphetamine causes an increase in striatal [Asc]o, which is attenuated, albeit not abolished, in anesthetized compared to awake rats (Gonon et al. 1981). This amphetamine-induced increase in [Asc]o is not a generalized phenomenon, but is specific to motor striatum (for reviews, see Grünewald 1993; Rebec and Pierce 1994). The explanation is that activity-dependent increases in striatal [Asc]o, including amphetamine-enhanced motor behavior, is a consequence of activation of glutamatergic input to the striatum, and involves glutamate release and uptake. The primary mechanism thought to underlie increases in [Asc]o is glutamate/ascorbate heteroexchange, in which ascorbate is released from cells as glutamate is taken up by a stereospecific transporter (O’Neill 1984; Grünewald and Fillenz 1984; Miele et al. 1994). Glutamate-dependent increases in [Asc]o in vivo can be prevented by glutamate uptake inhibitors, but not by glutamate-receptor blockers, further implicating glutamate transporters in the process (Cammack et al. 1991). Consistent with this mechanism, both circadian (O’Neill et al. 1983) and amphetamine-induced (Basse-Tomusk and Rebec 1990) increases in striatal [Asc]o are attenuated after cortical lesions that remove the cortical glutamatergic input to striatum. The amphetamine-induced response appears to require dopamine release, which then activates a loop that includes substantia nigra, thalamus, cortex and striatum (Rebec and Pierce 1994). Existing evidence implicates neurons (Grünewald and Fillenz 1984), rather than astrocytes (Wilson et al. 2000), as the cellular site of glutamate/ascorbate heteroexchange, but the specific glutamate transporters involved remain unresolved (for review, see Rice 2000).
5 Compartmentalization of Ascorbate Between Neurons and Glia
As discussed in Sect. 4, ascorbate is homeostatically regulated between the intra- and extracellular compartments of the brain, with additional compartmentalization between neurons and glia. How was the difference between neurons and glia determined? The most obvious approach would be to examine isolated populations of neurons and glia in culture. However, as already discussed, ascorbate is readily lost from mammalian cells in vitro. In fact, ascorbate loss from isolated cells is even greater than in brain slices, with ascorbate levels that are below detection limits in cells cultured in ascorbate-free media (Kalir and Mytilenou 1992; Makar et al. 1994; Siushansian and Wilson 1995).
Several lines of evidence from whole-tissue studies, however, pointed to preferential localization of ascorbate in neurons, rather than in glia. Histochemical studies identified ascorbate in the cytosol of neurons in the locus coeruleus, with lower levels in surrounding glia (Shimizu et al. 1960). This was of particular interest, because ascorbate is a co-factor for noradrenaline synthesis; however, later studies showed that there is little correlation between tissue levels of ascorbate and noradrenergic innervation (Milby et al. 1982). On the other hand, studies using HPLC to quantify tissue ascorbate content found that ascorbate levels in neuron-rich cerebral cortex from adult rats was roughly four-fold higher than in the essentially neuron-free optic nerve, consistent with predominant localization of ascorbate in neurons rather than glia (Rice et al. 1995).
Quantitative determination of intracellular ascorbate concentrations in neurons and glia was subsequently made through comparisons of the ascorbate contents of brain samples with known differences in neuron density or neuron-to-glial ratio. The first comparison examined the ascorbate content of samples of cerebral cortex from several mammalian species, based on the previous observation that neuron density varies across species with an inverse dependence on brain size (Tower and Elliott 1952). Consistent with primary neuronal localization, ascorbate content was found to increase linearly with increasing neuron density: human < rabbit < guinea pig < rat < mouse (Rice and Russo-Menna 1998). The y-axis intercept of the resulting plot of ascorbate content versus neuron density was used to estimate ascorbate levels in tissue with zero neuron density, i.e., a pure glial population. With appropriate values for the volume fractions of the intra- and extracellular compartments, an intracellular glial ascorbate concentration was calculated to be about 1 mM (Rice and Russo-Menna 1998). The second comparison examined ascorbate content in developing rat brain, in which regionally distinct patterns of changes in neuron-to-glia ratio occur over the first three postnatal weeks (Altman 1972; Parnavelas et al. 1983). In cerebral cortex, tissue ascorbate content is highest on postnatal day 3 (P3), when cortical tissue is nearly entirely composed of neurons with only few immature glial cells (Rice and Russo-Menna 1998). Over the next 3 weeks, ascorbate levels fall, consistent with the time course of cortical gliogenesis. In the cerebellum, by contrast, ascorbate levels are relatively constant until P9, when they begin to increase markedly, coincident with the onset of cerebellar granule-cell proliferation (Altman 1972); a maximum ascorbate content in developing cerebellum is reached by P15. The tissue ascorbate contents of rat cortex at P3 and cerebellum at P15 represent levels in relatively pure neuronal populations. Again using the appropriate intra- and extracellular volume fractions, intracellular ascorbate concentration in neurons was calculated to be 10 mM (Rice and Russo-Menna 1998). Because this concentration was obtained from two regionally and developmentally distinct neuron populations, high intracellular ascorbate levels appear to be a general characteristic of neurons.
6 Ascorbate and GSH
Ascorbate and GSH are the two most abundant low molecular weight antioxidants in the brain. Total tissue contents for each are 2–3 mM (Lyrer et al. 1991; Uemura et al. 1991; Rice et al. 1995), which are 10–20 times higher than that of cysteine and 500–1,000 times higher than that of uric acid (Lyrer et al. 1991; Uemura et al. 1991). Ascorbate and GSH have similarities and differences in their properties, which suggest that they have complementary, but distinct roles in the CNS (Orlowski and Karkowsky 1976; Makar et al. 1994; Rice 2000). GSH is an anionic tripeptide, γ-glutamyl-cysteinyl-glycine, synthesized in all cells in the CNS (Orlowski and Karkowsky 1976; Makar et al. 1994). In contrast to ascorbate, which is more highly concentrated in neurons than glia, as discussed in Sect. 5, GSH is more highly concentrated in glia, with average intracellular GSH levels that are 60% higher in glia (4 mM) than in neurons (2.5 mM) (Rice and Russo-Menna 1998). This distribution is consistent with higher levels of GSH synthesizing enzymes and GSH peroxidase in glia (Slivka et al. 1987; Raps et al. 1989; Makar et al. 1994; Desagher et al. 1996; Trépanier et al. 1996; Peuchen et al. 1997).
An apparently key function of both ascorbate and GSH is their ability to neutralize reactive hydroxyl radicals (•OH), because there are no enzymes analogous to superoxide dismutase or GSH peroxidase to scavenge •OH (Cohen 1994). In addition, ascorbate and GSH can interact as a redox couple (Meister 1994; Winkler et al. 1994); depletion of either ascorbate or GSH can be compensated for by the continued presence of the other. For example, ascorbate administration can prevent tissue damage after inhibition of GSH synthesis (Meister 1994; Avshalumov et al. 2004, 2007), as discussed further below, whereas administration of GSH ester can prevent the onset of scurvy in ascorbate-deficient guinea pigs (Meister 1994). On a cellular level, the distinct ascorbate:GSH ratio in neurons (4:1) and glia (1:4) (Rice and Russo-Menna 1998) might alter the dynamics of ascorbate/GSH interactions, with greater reliance on ascorbate in neurons and GSH in glia.
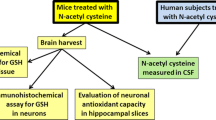
Brain slice studies again provided novel insight into dynamic consequences of an imbalance between oxidant production and antioxidant protection, i.e., oxidative stress, and how ascorbate and GSH prevent consequent oxidative damage. For example, in vitro studies using hippocampal slices from either rat or guinea pig showed a reversible inhibition of the population spike (PS) evoked by Schaffer collateral stimulation during brief exposure to exogenous H2O2 (1.0–3.0 mM) (Pellmar 1986, 1987, 1995; Avshalumov et al. 2000; Avshalumov and Rice 2002). In rat hippocampal slices, recovery of the primary PS following H2O2 washout is accompanied by mild epileptiform activity, indicated by an additional PS after the primary spike (Avshalumov and Rice 2002). When guinea pig hippocampal slices are exposed to H2O2 under identical conditions, the evoked PS is also reversibly depressed during H2O2 exposure. However, unlike rat slices, only a single PS is seen in guinea-pig hippocampal slices after H2O2 washout, indicating the absence of lasting pathophysiology (Avshalumov et al. 2004).
The higher tolerance of guinea-pig brain than rat brain tissue to H2O2 exposure, implies that the higher glia:neuron ratio in this species provides additional antioxidant protection, particularly from glia. The possible importance of GSH-based antioxidant protection in glia, was tested by examining the effect of GSH synthesis or GSH peroxidase inhibition on H2O2-induced pathophysiology in guinea-pig brain slices. Both GSH and ascorbate are readily lost from rat and guinea-pig brain slices in vitro, with slice contents that are at least 60% lower than those in intact tissue (McIlwain et al. 1956; Rice et al. 1994; Avshalumov et al. 2004). Nonetheless, in slices of guinea-pig hippocampus, an additional small, but significant, decrease in GSH (and ascorbate) content after inhibition of GSH synthesis by buthionine sulfoximine is accompanied by epileptiform activity in guinea-pig slices following H2O2 exposure (Avshalumov et al. 2004). The loss of H2O2 tolerance in guinea-pig hippocampal slices after GSH synthesis inhibition, despite a relatively small absolute decrease in GSH content, suggests that the protective effect of endogenous GSH is mediated through its role as a co-factor for GSH peroxidase, glutaredoxins, and GSH transferases, as well as by direct recycling of oxidized ascorbate (Meister 1994; Washburn and Wells 1999; Board et al. 2000; Rice 2000; Ehrhart and Zeevalk 2003; Avshalumov et al. 2004).
Consistent with this hypothesis, enhanced H2O2-induced pathophysiology in guinea-pig hippocampal slices also occurs when GSH peroxidase is inhibited by mercaptosuccinate (Avshalumov et al. 2004). Although GSH peroxidase inhibition alone has no effect on hippocampal PS amplitude, exposure to H2O2 during GSH peroxidase inhibition causes a larger suppression of the evoked PS than in ACSF alone. The recovery of PS amplitude during H2O2 washout under these conditions is not only accompanied by secondary H2O2-induced pathology, but is also delayed compared to that in ACSF alone. Importantly, inclusion of ascorbate at its normal extracellular concentration in vivo (400 μM) in the washout solution prevented these pathophysiological consequences of H2O2 exposure after GSH peroxidase inhibition.
Prolonged H2O2 exposure as a model of oxidative stress can also cause other pathophysiological effects in brain tissue, including edema (Brahma et al. 2000; Avshalumov et al. 2004). This consequence is also species dependent, however: significant water gain is seen in coronal slices of rat forebrain after 3 h exposure to H2O2 (Brahma et al. 2000), however no increase in edema is seen in guinea-pig slices incubated under identical conditions (Avshalumov et al. 2004). Once again, guinea-pig brain tissue behaves like rat tissue when GSH synthesis or GSH peroxidase is inhibited; importantly, H2O2-induced edema under these conditions was again prevented when ascorbate is present (Avshalumov et al. 2004). Studies in neuron-glia co-cultures have shown that the glial antioxidant network can protect neurons from H2O2 toxicity (Desagher et al. 1996; Drukarch et al. 1997, 1998; Tanaka et al. 1999; Dringen et al. 1999). The results from brain slices show that this is also true in tissue in which neuronal and glial integrity is maintained. Even more significantly, these data demonstrate that ascorbate can compensate for GSH depletion and GSH peroxidase inhibition to prevent pathophysiological consequences of peroxide-induced oxidative stress (Avshalumov et al. 2004).
7 Brain Ascorbate: Protective, Yet Permissive
7.1 Neuroprotection by Ascorbate
High levels of ascorbate and of SVCT2 in a variety of neuronal types imply a function for neuronal ascorbate beyond its actions as a cell-specific enzyme co-factor. Importantly, the tenfold difference in ascorbate levels between neurons and glia (Rice and Russo-Menna 1998) is consistent with the estimated tenfold higher rate of oxidative metabolism in neurons compared with glial cells (Siesjö 1980). Although ascorbate has been shown to be a pro-oxidant in some studies, albeit mostly in vitro, the occurrence of naturally high levels of ascorbate in neuronal cytosol together with other data discussed below argue strongly against normally pro-oxidant actions in vivo (Halliwell 1996; Rice 2000). For example, the importance of ascorbate as an intracellular antioxidant is supported by the finding that brain ascorbate (but not GSH) levels in pond turtles are two to three times higher than in mammals (Rice et al. 1995). These diving animals have a remarkable tolerance of hypoxia through a variety of mechanisms (Lutz 1992; Milton and Prentice 2007). Selective elevation of brain ascorbate levels, but not GSH or other antioxidant enzymes (Rice et al. 1995; Milton and Prentice 2007) could represent a specific adaptation to prevent oxidative damage during reoxygenation after a hypoxic dive (Rice et al. 1995; 2002). Interestingly, turtle brain tissue also maintains its ascorbate content in vitro (Rice and Cammack 1991), unlike isolated mammalian tissue, suggesting another neuroprotective adaptation. In hypoxia-tolerant turtles, whether normoxic or hypoxic, and in mammals under normal aerobic conditions, ascorbate is recycled as it is used (see Sect. 1), which provides on-going antioxidant protection in vivo.
When cerebral blood is compromised in mammals, for example, under conditions of ischemic or hemorrhagic stroke, energy failure and anoxic depolarization lead to efflux of ascorbate from cells to the ECF (Hillered et al. 1988). With continued ischemia, tissue levels of ascorbate and other low-molecular-weight antioxidants fall (Lyrer et al. 1991). Consequently, when aerobic metabolism resumes, intracellular stores of these agents are no longer adequate to quench reactive oxygen species (ROS), leaving cells vulnerable to oxidative damage. Increased detection of •OH during post-ischemic reperfusion (Cao et al. 1988) is one consequence of antioxidant depletion. Can elevated ascorbate protect brain tissue from ischemic injury? The answer appears to be yes. Enhanced brain ascorbate content from dietary supplementation protects cortical mitochondria from in vivo ischemia/reperfusion injury in rats (Sciamanna and Lee 1993) and decreases focal ischemia-induced damage in primates (Ranjan et al. 1993; Henry and Chandry 1998). This may be due, at least in part to upregulation of SVCT2 in the region surrounding the infarct core, which should facilitate ascorbate uptake (Berger et al. 2003). Mechanisms of ascorbate protection suggested by in vitro studies include prevention of mitochondrial hyperoxidation and tissue edema formation during post-ischemic reoxygenation in brain slices (Pérez-Pinzón et al. 1997; MacGregor et al. 2003), as well as amelioration of excitoxicity from excessive glutamate receptors activation in cultured cells (for review, see Rice 2000). Notably, although transport of oxidized ascorbate, DHA, via GLUT1 is normally a minor route of ascorbate entry into the CNS, this pathway provides a much more efficient means of elevating brain ascorbate than transport via SVCT2 at the choroid plexus, which is already saturated at normal plasma ascorbate concentrations (Sect. 3). Indeed, administration of DHA provides potent neuroprotection in vivo in rodent stroke models, including decreased lipid peroxidation and a significant decrease in infarct volume (Huang et al. 2001; Mack et al. 2006).
Additional evidence for ascorbate neuroprotection via its properties as an antioxidant and •OH scavenger comes from brain slice studies in which exogenous H2O2 is used to induce oxidative stress. Strikingly, H2O2 exposure, which normally leads to suppression of the evoked PS in hippocampal slices (Sect. 6) has no effect on the PS when applied in the presence of 400 μM ascorbate (Avshalumov et al. 2000). Similar prevention of PS suppression is provided by deferoxamine, a metal ion chelator that prevents iron or copper-catalyzed •OH formation from H2O2, indicating that the effect of H2O2 on the PS is mediated by •OH and that protection by ascorbate under these conditions is by •OH scavenging (Avshalumov et al. 2000). H2O2-dependent PS suppression is also prevented by isoascorbate (d-ascorbate) (Avshalumov et al. 2000), the non-biologically active stereoisomer of l-ascorbate that is not transported by stereoselective SVCT2 (Tsukaguchi et al. 1999), indicating an extracellular site of antioxidant action. As discussed in Sect. 6, ascorbate can also prevent long-lasting pathophysiological consequences of H2O2 exposure, indicated by the absence of epileptiform activity when ascorbate is present only during H2O2 washout in rat hippocampal slices (Avshalumov and Rice 2002) or in guinea-pig hippocampal slices in which the antioxidant network is compromised (Avshalumov et al. 2004). This secondary protection by ascorbate must occur intracellularly in neurons, however, because non-transported isoascorbate is not protective under these conditions (Avshalumov and Rice 2002). Taken together, these findings strongly support a neuroprotective role for both intra- and extracellular ascorbate.
A number of other actions of ascorbate, from alterations in neurotransmitter binding affinity to inhibition of Na+/K+-ATPase activity, have been reported in the literature. Because most of these studies were conducted in vitro, often in isolated cells or cell membranes that lack an intact antioxidant network, the potential for pro-oxidant effects of ascorbate is high, which casts doubt on the physiological relevance of some of the findings. This does not mean that ascorbate never acts as a pro-oxidant in vivo. Indeed, under pathological conditions such as ischemia, when ascorbate compartmentalization is disrupted, these actions could occur and contribute to CNS injury, as discussed above. Under normal conditions, however, ascorbate is neuroprotective.
7.2 Reactive Oxygen Species (ROS) as Signaling Molecules in the Brain
Demonstration of neuroprotection by ascorbate and other antioxidants is consistent with the traditional view that ROS are harmful agents and must be tightly controlled. This view is further supported by evidence of oxidative damage as a contributing factor to cell death following acute brain injury, including cerebral ischemia-reperfusion (Cao et al. 1988; Hyslop et al. 1995; Chan 2004; Starkov et al. 2004), as well as in slowly progressing neurodegenerative disorders like Parkinson disease (Cohen 1994; Ebadi et al. 1996; Olanow and Tatton 1999; Zhang et al. 2000; Greenamyre et al. 2001; Xu et al. 2002; Orth and Schapira 2002; Wood-Kaczmar et al. 2006; Fukae et al. 2007; Dodson and Guo 2007). This traditional perspective is evolving rapidly, however, in light of increasing evidence that ROS also act as cellular messengers that modulate processes from short-term ion-channel activation (Seutin et al. 1995; Krippeit-Drews et al. 1999; Avshalumov and Rice 2003; Tang et al. 2004; Avshalumov et al. 2005; Bao et al. 2005; Hidalgo et al. 2005) to gene transcription and cell proliferation (Suzuki et al. 1997; Sauer et al. 2001; Haddad 2002; Esposito et al. 2004; Rhee et al. 2005; Rhee 2006; Infanger et al. 2006; Bedard and Krause 2007).
Of the ROS generated by various cellular processes, H2O2 is a particularly strong candidate as a signaling agent because it is membrane permeable, possibly facilitated by aquaporins (Bienert et al. 2006, 2007). H2O2 is also relatively inert; in contrast to other ROS that are reactive free radicals, including superoxide and •OH, H2O2 is a mild oxidant (Cohen 1994; Rhee 2006). As discussed in Sects. 1 and 6, ascorbate works in concert with other components of the antioxidant network. The emerging role for H2O2 and other ROS as signaling agents, however, requires that oxidant regulation must be more subtle than previously thought.
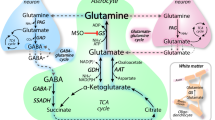
The first evidence suggesting that H2O2 might regulate neurotransmission was the finding that exogenous H2O2 could suppress the evoked PS in hippocampal slices, possibly by inhibiting transmitter release (Pellmar 1986, 1987). The hypothesis that transmitter release can be inhibited by exogenous H2O2 was confirmed by the demonstration that evoked dopamine (DA) release in striatal slices is reversibly suppressed during brief H2O2 exposure (Chen et al. 2001). More significantly, subsequent studies showed that endogenously generated H2O2 inhibits axonal DA release in the striatum (Chen et al. 2001, 2002; Avshalumov et al. 2003; Avshalumov and Rice 2003) and suppresses the activity of dopaminergic neurons in the substantia nigra pars compacta (SNc) (Avshalumov et al. 2005). These studies were the first to show that endogenous H2O2 is an activity-dependent neuromodulator. Regulation of the nigrostriatal DA system is important because of the central role this pathway plays in the control of movement by the basal ganglia, with loss of dopaminergic neurons in the SNc leading to the motor deficits of Parkinson disease (Albin et al. 1989). In dopaminergic neurons, intracellular H2O2 modulates cell excitability via ATP-sensitive K+ (KATP) channels (Avshalumov et al. 2005). By contrast, modulatory H2O2 in the striatum is generated downstream from the activation of glutamatergic AMPA receptors (Avshalumov et al. 2003), which are not found on dopaminergic axons (Chen et al. 1998; Bernard and Bolam 1998). This implies that modulatory H2O2 is not generated within dopaminergic axons, but rather must be produced postsynaptically in striatal neurons, then diffuse from these sites to modulate presynaptic DA release. Recent studies have confirmed this mode of intercellular communication by demonstrating AMPA-receptor dependent H2O2 generation in medium spiny neurons (MSNs) (Avshalumov et al. 2008), the principal output neurons of the striatum (Kemp and Powell 1971), but not dopaminergic axons.
Thus, H2O2 serves different functions in the striatum than in SNc. In striatum, diffusible H2O2 mediates regulation of axonal DA release by glutamate and GABA. When glutamatergic striatal afferents are activated, this has no direct effect on DA release, as there are no presynaptic glutamate receptors on dopaminergic axons, as already noted. However, this excitatory input leads to postsynaptic H2O2 generation in MSNs, which leads to inhibition of DA release. Thus, diffusible H2O2 mediates the effect of glutamate on DA release in the striatum. Local release of GABA in the striatum apparently opposes this process by suppressing the excitability of MSNs, resulting in less H2O2 generation and thus enhancing DA release. Overall, therefore, in striatum, H2O2-dependent inhibition via KATP channel activation on dopaminergic axons reverses the conventional effects of glutamate and GABA, with inhibition of DA release following AMPA receptor activation and enhancement of DA release following GABAA receptor activation (Avshalumov et al. 2003). By contrast, spontaneous pacemaker activity in dopaminergic neurons of the SNc produces H2O2 that serves as an autoregulatory signal that leads to a decrease in cell firing rate, again via KATP channel activation (Avshalumov et al. 2005). Although the mechanism by which H2O2 activates KATP channels is not yet clear, this process circumvents the need for a catastrophic fall in cell ATP levels to activate KATP channels, thereby providing a subtle, but effective way to link metabolism to excitability.
Importantly, neuromodulation by H2O2 is not limited to the nigrostriatal system. Other studies have shown that H2O2 influences characteristics of LTP in the hippocampus (Auerbach and Segal 1997; Kamsler and Segal 2003, 2004), which has implications for memory formation. Diffusible H2O2 also plays a role in neuron-glia signaling in the hippocampus, in which neuronal activation leads to H2O2-dependent phosphorylation of myelin basic protein in oligodendrocytes (Atkins and Sweatt 1999). Overall, these findings indicate that H2O2 can act both as an intracellular signaling agent and as a diffusible messenger in the brain.
7.3 Ascorbate Is a Unique Neuronal Antioxidant
For H2O2 to act at both intracellular and potentially distant targets requires that the brain antioxidant network allows functional levels of H2O2 and other ROS, while still preventing oxidative stress, which adds a previously unrecognized dimension to oxidant management. Key features of such a permissive environment are the predominance of ascorbate in neurons and the predominance of cytosolic GSH and GSH peroxidase activity in glia (Cohen 1994; Rice and Russo-Menna 1998; Rice 2000; Avshalumov et al. 2004).
In striking contrast to the efficacy of ascorbate in preventing pathophysiological consequences of exogenous H2O2 exposure (Avshalumov et al. 2000, 2004; Avshalumov and Rice 2002), this antioxidant and •OH scavenger has no effect on dynamic modulation of axonal DA release by endogenous H2O2 generated downstream from AMPA receptor activation in the striatum (Avshalumov et al. 2003). This finding indicates that inhibition of DA release is a direct action of H2O2, rather than •OH. Equally important, however, it shows that ascorbate does not interfere with H2O2-dependent signaling in striatum. The lack of interference is consistent with in vitro studies showing little redox reactivity between ascorbate and H2O2: ascorbate, at 400 μM, is surprisingly stable in the presence of mM levels of H2O2, as is H2O2 in the presence of ascorbate, when precautions are taken to minimize the presence of trace metal ions (Avshalumov et al. 2000). By contrast, GSH is rapidly oxidized under similar conditions in the presence of H2O2 (Avshalumov et al. 2000). Thus, ascorbate is ideally suited as a key neuronal antioxidant because of its unique redox potential, which gives it the dual ability to permit H2O2 signaling, yet prevent pathological consequences that could occur from dysregulated H2O2 generation and ·OH production.
8 Conclusions and Future Directions
The high intracellular concentration of ascorbate in neurons suggests that it has a significant role in normal neuronal physiology. Given the well-established characteristics of ascorbate as an electron donor and free radical scavenger, it is likely that its primary role comes from neuroprotective actions as a component of the neuronal antioxidant network. In addition, ascorbate is one of the few antioxidants found in significant concentration in ECF. The fact that [Asc]o is regulated homeostatically, but modulated by glutamatergic activity suggests that the extracellular compartment is also an important site for ascorbate neuroprotection. Ongoing research on ascorbate and glutamate transporters should lay the groundwork for future understanding of ascorbate regulation in the brain. As new tools to manipulate ascorbate levels become available, new insights into its specific functions in the brain should also emerge.
It is also relevant to note that regulation of striatal DA release by endogenous H2O2 is similar in guinea-pig and rat, as well as in non-human primate (Rice et al. 2002). This not only demonstrates that H2O2 signaling is not impaired by the presence of the stronger antioxidant network afforded by the higher glia:neuron ratio of guinea-pig or primate versus rat brain, but also supports the hypothesis that precise neuron-glial antioxidant compartmentalization, regardless of species, is required for neuronal signaling, as well as neuronal protection. A key feature of this compartmentalization is the predominance of ascorbate in neurons, which is permissive for H2O2 signaling because it does not alter either intra- or extracellular concentrations of H2O2 or hinder the escape of diffusible H2O2 from the cells in which it is generated. On the other hand, homeostatically regulated levels of ascorbate in neurons, glia, and in ECF provides protection against •OH, as needed, in both the intra- and extracellular compartments of the CNS.
References
Agus DB, Gambhir SS, Pardridge WM, Spielholz C, Baselga J, Vera JC, Golde DW (1997) Vitamin C crosses the blood-brain barrier in the oxidized form through the glucose transporters. J Clin Invest 100:2842–2848
Albin RL, Young AB, Penney JB (1989) The functional anatomy of basal ganglia disorders. Trends Neurosci 12:366–375
Altman J (1972) Postnatal development of the cerebellar cortex of the rat: III. Maturation of the components of the granular layer. J Comp Neurol 145:465–514
Astuya A, Caprile T, Castro M, Salazar K, García Mde L, Reinicke K, Rodríguez F, Vera JC, Millán C, Ulloa V, Low M, Martínez F, Nualart F (2005) Vitamin C uptake and recycling among normal and tumor cells from the central nervous system. J Neurosci Res 79:146–156
Atkins CM, Sweatt JD (1999) Reactive oxygen species mediate activity-dependent neuron-glia signaling in output fibers of the hippocampus. J Neurosci 19:7241–7248
Auerbach JM, Segal M (1997) Peroxide modulation of slow onset potentiation in rat hippocampus. J Neurosci 17:8695–8701
Avshalumov MV, Rice ME (2002) NMDA-receptor activation mediates hydrogen peroxide-induced pathophysiology in rat hippocampal slices. J Neurophysiol 87:2896–2903
Avshalumov MV, Rice ME (2003) Activation of ATP-sensitive K+ (KATP) channels by H2O2 underlies glutamate-dependent inhibition of striatal dopamine release. Proc Natl Acad Sci USA 100:11729–11734
Avshalumov MV, Chen BT, Rice ME (2000) Mechanisms underlying H2O2-mediated inhibition of synaptic transmission in rat hippocampal slices. Brain Res 882:86–94
Avshalumov MV, Chen BT, Marshall SP, Peña DM, Rice ME (2003) Glutamate-dependent inhibition of dopamine release in striatum is mediated by a new diffusible messenger, H2O2. J Neurosci 23:2744–2750
Avshalumov MV, MacGregor DG, Sehgal LM, Rice ME (2004) The glial antioxidant network and neuronal ascorbate: permissive yet protective for H2O2 signaling? Neuron Glia Biol 1:365–376
Avshalumov MV, Chen BT, Kóos T, Tepper JM, Rice ME (2005) Endogenous hydrogen peroxide regulates the excitability of midbrain dopamine neurons via ATP-sensitive potassium channels. J Neurosci 25:4222–4231
Avshalumov MV, Bao L, Patel JC, Rice ME (2007) H2O2 signaling in the nigrostriatal dopamine pathway via ATP-sensitive potassium channels: issues and answers. Antioxid Redox Signal 9:219–231
Avshalumov MV, Patel JC, Rice ME (2008) AMPA receptor-dependent H2O2 generation in striatal spiny neurons, but not dopamine axons: one source of a retrograde signal that can inhibit dopamine release. J Neurophysiol 100:1590–1601
Bao L, Avshalumov MV, Rice ME (2005) Mitochondrial inhibition causes functional dopamine denervation and striatal medium spiny neurons depolarization via increased H2O2, not decreased ATP. J Neurosci 25:10029–10040
Barnes MJ (1975) Function of ascorbic acid in collagen metabolism. Ann N Y Acad Sci 258:264–277
Basse-Tomusk A, Rebec GV (1990) Corticostriatal and thalamic regulation of amphetamine-induced ascorbate release in the neostriatum. Pharmacol Biochem Behav 35:55–60
Bedard K, Krause KH (2007) The NOX family of ROS-generating NADPH oxidases: physiology and pathophysiology. Physiol Rev 87:245–313
Berger UV, Hediger MA (2000) The vitamin C transporter SVCT2 is expressed by astrocytes in culture but not in situ. NeuroReport 11:1395–1399
Berger UV, Lu XC, Liu W, Tang Z, Slusher BS, Hediger MA (2003) Effect of middle cerebral artery occlusion on mRNA expression for the sodium-coupled vitamin C transporter SVCT2 in rat brain. J Neurochem 86:896–906
Bernard V, Bolam JP (1998) Subcellular and subsynaptic distribution of the NR1 subunit of the NMDA receptor in the neostriatum and globus pallidus of the rat: colocalization at synapses with the GluR2/3 subunit of the AMPA receptor. Eur J Neurosci 10:3721–3738
Bienert GP, Schjoerring JK, Jahn TP (2006) Membrane transport of hydrogen peroxide. Biochim Biophys Acta 1758:994–1003
Bienert GP, Møller AL, Kristiansen KA, Schulz A, Møller IM, Schjoerring JK, Jahn TP (2007) Specific aquaporins facilitate the diffusion of hydrogen peroxide across membranes. J Biol Chem 282:1183–1192
Board PG, Coggan M, Chelvanayagam G, Easteal S, Jermiin LS, Schulte GK, Danley DE, Hoth LR, Griffor MC, Kamath AV, Rosner MH, Chrunyk BA, Perregaux DE, Gabel CA, Geoghegan KF, Pandit J (2000) Identification, characterization, and crystal structure of the Omega class glutathione transferases. J Biol Chem 275:24798–24806
Bodannes RS, Chan PC (1979) Ascorbic acid as a scavenger of singlet oxygen. FEBS Lett 105:195–196
Brahma B, Forman RE, Stewart EE, Nicholson C, Rice ME (2000) Ascorbate inhibits edema in brain slices. J Neurochem 74:1263–1270
Buettner GR (1993) The pecking order of free radicals and antioxidants: lipid peroxidation, α-tocopherol, and ascorbate. Arch Biochem Biophys 300:535–543
Buettner GR, Jurkiewicz BA (1993) Ascorbate free radical as a marker of oxidative stress: an EPR study. Free Rad Biol Med 14:49–55
Cammack J, Ghasemzadeh B, Adams RN (1991) The pharmacological profile of glutamate-evoked ascorbic acid efflux measured by in vivo voltammetry. Brain Res 565:17–22
Cao W, Carney JM, Duchon A, Floyd RA, Chevion M (1988) Oxygen free radical involvement in ischemia and reperfusion injury to brain. Neurosci Lett 88:233–238
Carey DJ, Todd MS (1987) Schwann cell myelination in a chemically defined medium: demonstration of a requirement for additives that promote Schwann cell extracellular matrix formation. Brain Res 429:95–102
Carpenter KJ (1986) The history of scurvy and vitamin C. Cambridge University Press, New York
Castro M, Caprile T, Astuya A, Millán C, Reinicke K, Vera JC, Vásquez O, Aguayo LG, Nualart F (2001) High-affinity sodium-vitamin C co-transporters (SVCT) expression in embryonic mouse neurons. J Neurochem 78:815–823
Chan PH (2004) Mitochondria and neuronal death/survival signaling pathways in cerebral ischemia. Neurochem Res 29:1943–1949
Chatterjee IB, Majumbar AK, Nandi BK, Subramanian N (1975) Synthesis and some major functions of vitamin C in animals. Ann N Y Acad Sci 258:24–47
Chen Q, Veenman L, Knopp K, Yan Z, Medina L, Song WJ, Surmeier DJ, Reiner A (1998) Evidence for the preferential localization of glutamate receptor-1 subunits of AMPA receptors to the dendritic spines of medium spiny neurons in rat striatum. Neuroscience 83:749–761
Chen BT, Avshalumov MV, Rice ME (2001) H2O2 is a novel, endogenous modulator of synaptic dopamine release. J Neurophysiol 85:2468–2476
Chen BT, Avshalumov MV, Rice ME (2002) Modulation of somatodendritic dopamine release by endogenous H2O2: susceptibility in substantia nigra but resistance in the ventral tegmental area. J Neurophysiol 87:1155–1158
Cohen G (1994) Enzymatic/nonenzymatic sources of oxyradicals and regulation of antioxidant defenses. Ann N Y Acad Sci 738:8–14
Daruwala R, Song J, Koh WS, Rumsey SC, Levine M (1999) Cloning and functional characterization of the human sodium-dependent vitamin C transporters hSVCT1 and hSVCT2. FEBS Lett 460:480–484
Davies MB, Austin J, Partridge DA (1991) Vitamin C: its chemistry and biochemistry. Royal Society of Chemistry, Cambridge, UK
Desagher S, Glowinski J, Premont J (1996) Astrocytes protect neurons from hydrogen peroxide toxicity. J Neurosci 16:2553–2562
Dhariwal KR, Hartzell WO, Levine M (1991) Ascorbic acid and dehydroascorbic acid measurements in human plasma and serum. Am J Clin Nutr 54:712–716
Diliberto EJ Jr, Menniti FS, Knoth J, Daniels AJ, Kizer JS, Viveros OH (1987) Adrenomedullary chromaffin cells as a model to study the neurobiology of ascorbic acid: from monooxygenation to neuromodulation. Ann N Y Acad Sci 498:28–53
Dodson MW, Guo M (2007) Pink1, Parkin, DJ-1 and mitochondrial dysfunction in Parkinson’s disease. Curr Opin Neurobiol 17:331–337
Drew KL, Osborne PG, Frerichs KU, Hu Y, Koren R, Hallenbeck JM, Rice ME (1999) Ascorbate and glutathione regulation in hibernating ground squirrels. Brain Res 851:1–8
Dringen R, Kussmaul L, Gutterer JM, Hirrlinger J, Hamprecht B (1999) The glutathione system of peroxide detoxification is less efficient in neurons than in astroglial cells. J Neurochem 72:2523–2530
Drukarch B, Schepens E, Jongenelen CA, Stoof JC, Langeveld CH (1997) Astrocyte-mediated enhancement of neuronal survival is abolished by glutathione deficiency. Brain Res 770:123–130
Drukarch B, Schepens E, Stoof JC, Langeveld CH, Van Muiswinkel FL (1998) Astrocyte-enhanced neuronal survival is mediated by scavenging of extracellular reactive oxygen species. Free Rad Biol Med 25:217–220
Ebadi M, Srinivasan SK, Baxi MD (1996) Oxidative stress and antioxidant therapy in Parkinson’s disease. Prog Neurobiol 48:1–19
Ehrhart J, Zeevalk GD (2003) Cooperative interaction between ascorbate and glutathione during mitochondrial impairment in mesencephalic cultures. J Neurochem 86:1487–1497
Eldridge CF, Bunge MB, Bunge RP, Wood PM (1987) Differentiation of axon-related Schwann cells in vitro. I. Ascorbic acid regulates basal lamina assembly and myelin formation. J Cell Biol 105:1023–1034
Esposito F, Ammendola R, Faraonio R, Russo T, Cimino F (2004) Redox control of signal transduction, gene expression and cellular senescence. Neurochem Res 29:617–628
Fornai F, Saviozzi M, Piaggi S, Gesi M, Corsini GU, Malvaldi G, Casini AF (1999) Localization of a glutathione-dependent dehydroascorbate reductase within the central nervous system of the rat. Neuroscience 94:937–948
Fornai F, Piaggi S, Gesi M, Saviozzi M, Lenzi P, Paparelli A, Casini AF (2001) Subcellular localization of a glutathione-dependent dehydroascorbate reductase within specific rat brain regions. Neuroscience 104:15–31
Fukae J, Mizuno Y, Hattori N (2007) Mitochondrial dysfunction in Parkinson’s disease. Mitochondrion 7:58–62
Gonon F, Buda M, Cespuglio R, Jouvet M, Pujol JF (1981) Voltammetry in the striatum of chronic freely moving rats: detection of catechols and ascorbic acid. Brain Res 223:69–80
Greenamyre JT, Sherer TB, Betarbet R, Panov AV (2001) Complex I and Parkinson’s disease. IUBMB Life 52:135–141
Grünewald RA (1993) Ascorbic acid in the brain. Brain Res Rev 18:123–133
Grünewald RA, Fillenz M (1984) Release of ascorbate from a synaptosomal fraction of rat brain. Neurochem Int 6:491–500
Haddad JJ (2002) Antioxidant and prooxidant mechanisms in the regulation of redox(y)-sensitive transcription factors. Cellular Signal 14:879–897
Halliwell B (1996) Vitamin C: antioxidant or pro-oxidant in vivo? Free Rad Res 25:439–454
Henry PT, Chandry MJ (1998) Effect of ascorbic acid on infarct size in experimental focal cerebral ischemia and reperfusion in a primate model. Acta Neurochir (Wien) 140:977–980
Hidalgo C, Donoso P, Carrasco MA (2005) The ryanodine receptors Ca2+ release channels: cellular redox sensors? IUBMB Life 57:315–322
Hillered L, Persson L, Bolander HG, Hallstrom A, Ungerstedt U (1988) Increased extracellular levels of ascorbate in striatum after middle cerebral artery occlusion in the rat monitored by intracerebral microdialysis. Neurosci Lett 95:286–290
Hornig D (1975) Distribution of ascorbic acid, metabolites and analogues in man and animals. Ann N Y Acad Sci 258:103–117
Huang J, Agus DB, Winfree CJ, Kiss S, Mack WJ, McTaggart RA, Choudhri TF, Kim LJ, Mocco J, Pinsky DJ, Fox WD, Israel RJ, Boyd TA, Golde DW, Connolly ES Jr (2001) Dehydroascorbic acid, a blood-brain barrier transportable form of vitamin C, mediates potent cerebroprotection in experimental stroke. Proc Natl Acad Sci USA 98:11720–11724
Hughes RE, Hurley RJ, Jones PR (1971) The retention of ascorbic acid by guinea-pig tissues. Brit J Nutr 26:433–438
Hyslop PA, Zhang Z, Pearson DV, Phebus LA (1995) Measurement of striatal H2O2 by microdialysis following global forebrain ischemia and reperfusion in the rat: correlation with the cytotoxic potential of H2O2 in vitro. Brain Res 671:181–186
Ichimura T, Fraser PA, Cserr HF (1991) Distribution of extracellular tracers in perivascular spaces of the rat brain. Brain Res 545:103–113
Infanger DW, Sharma RV, Davisson RL (2006) NADPH oxidases of the brain: distribution, regulation, and function. Antioxid Redox Signal 8:1583–1596
Kalir HH, Mytilenou C (1992) Ascorbic acid in mesencephalic cultures: effects on dopaminergic neuron development. J Neurochem 57:458–464
Kallner A, Hartmann D, Hornig D (1977) On the absorption of ascorbic acid in man. Int J Vitam Nutr Res 47:383–388
Kamsler A, Segal M (2003) Hydrogen peroxide modulation of synaptic plasticity. J Neurosci 23:269–276
Kamsler A, Segal M (2004) Hydrogen peroxide as a diffusible signal molecule in synaptic plasticity. Mol Neurobiol 29:167–178
Kemp JM, Powell TP (1971) The structure of the caudate nucleus of the cat: light and electron microscopy. Philos Trans R Soc Lond B Biol Sci 262:383–401
Krippeit-Drews P, Kramer C, Welker S, Lang F, Ammon HP, Drews G (1999) Interference of H2O2 with stimulus-secretion coupling in mouse pancreatic beta-cells. J Physiol (Lond) 514:471–481
Kume-Kick J, Rice ME (1998) Estrogen-dependent modulation of rat brain ascorbate levels and ischemia-induced ascorbate loss. Brain Res 803:105–113
Lam DKC, Daniel PM (1986) The influx of ascorbic acid into the rat’s brain. Quart J Exp Physiol 71:483–489
Lutz PL (1992) Mechanisms for anoxic survival in the vertebrate brain. Ann Rev Physiol 54: 601–618
Lyrer P, Landolt H, Kabiersch A, Langemann H, Kaeser H (1991) Levels of low molecular weight scavengers in the rat brain during focal ischemia. Brain Res 567:317–320
MacGregor DG, Avshalumov MV, Rice ME (2003) Brain edema induced by in vitro ischemia: causal factors and neuroprotection. J Neurochem 85:1402–1411
Machlin LJ, Bendich A (1987) Free radical tissue damage: protective role of antioxidant nutrients. FASEB J 1:441–445
Mack WJ, Mocco J, Ducruet AF, Laufer I, King RG, Zhang Y, Guo W, Pinsky DJ, Connolly ES Jr (2006) A cerebroprotective dose of intravenous citrate/sorbitol-stabilized dehydroascorbic acid is correlated with increased cerebral ascorbic acid and inhibited lipid peroxidation after murine reperfused stroke. Neurosurgery 59:383–388
Makar TK, Nedergaard M, Preuss A, Gebard AS, Perumal AS, Cooper AJL (1994) Vitamin E, ascorbate, glutathione, glutathione disulfide, and enzymes of oxidative metabolism in cultures of chick astrocytes and neurons: evidence that astrocytes play an important role in oxidative processes in the brain. J Neurochem 62:45–53
May JM, Mendiratta S, Hill KE, Burk RF (1997) Reduction of dehydroascorbate to ascorbate by the selenoenzyme thioredoxin reductase. J Biol Chem 272:22607–22610
McIlwain H, Thomas J, Bell JL (1956) The composition of isolated cerebral tissues: ascorbic acid and cozymase. Biochem J 64:332–335
Meister A (1994) Glutathione-ascorbic acid antioxidant system in animals. J Biol Chem 269: 9397–9400
Miele M, Fillenz M (1996) In vivo determination of extracellular brain ascorbate. J Neurosci Methods 70:15–19
Miele M, Boutelle MG, Fillenz M (1994) The physiologically induced release of ascorbate in rat brain is dependent on impulse traffic, calcium influx and glutamate uptake. Neuroscience 62:87–91
Milby K, Oke A, Adams RN (1982) Detailed mapping of ascorbate distribution in rat brain. Neurosci Lett 28:15–20
Milton SL, Prentice HM (2007) Beyond anoxia: the physiology of metabolic downregulation and recovery in the anoxia-tolerant turtle. Comp Biochem Physiol A Mol Integr Physiol 147:277–290
Niki E (1991) Action of ascorbic acid as a scavenger of active and stable oxygen radicals. Am J Clin Nutr 54:1119S–11124S
Nishikimi M (1975) Oxidation of ascorbic acid with superoxide anion generated by the xanthine-xanthine oxidase system. BBRC 63:463–468
Nishikimi M, Fukuyama R, Minoshima S, Shimizu N, Yagi K (1994) Cloning and chromosomal mapping of the human nonfunctional gene for l-gulono-γ-lactone oxidase, the enzyme for l-ascorbic acid biosynthesis missing in man. J Biol Chem 269:13685–13688
O’Neill RD (1984) Voltammetrically monitored brain ascorbate as an index of excitatory amino acid releases in the unrestrained rat. Neurosci Lett 52:227–233
O’Neill RD, Grunewald RA, Fillenz M, Albery WJ (1983) The effect of unilateral cortical lesions on the circadian changes in rat striatal ascorbate and homovanillic acid levels measured in vivo using voltammetry. Neurosci Lett 42:105–110
Olanow CW, Tatton WG (1999) Etiology and pathogenesis of Parkinson’s disease. Annu Rev Neurosci 22:123–144
Orlowski M, Karkowsky A (1976) Glutathione metabolism and some possible functions of glutathione in the nervous system. Int Rev Neurobiol 19:75–121
Orth M, Schapira AH (2002) Mitochondrial involvement in Parkinson’s disease. Neurochem Int 40:533–541
Pagé EL, Chan DA, Giaccia AJ, Levine M, Richard DE (2008) Hypoxia-inducible factor-1alpha stabilization in nonhypoxic conditions: role of oxidation and intracellular ascorbate depletion. Mol Biol Cell 19:86–94
Parnavelas JG, Luder R, Pollard SG, Sullivan K, Lieberman AR (1983) A quantitative and qualitative ultrastructural study of glial cells in the developing visual cortex of the rat. Phil Trans R Soc (Lond) 301:55–84
Passage E, Norreel JC, Noack-Fraissignes P, Sanguedolce V, Pizant J, Thirion X, Robaglia-Schlupp A, Pellissier JF, Fontés M (2004) Ascorbic acid treatment corrects the phenotype of a mouse model of Charcot-Marie-Tooth disease. Nat Med 10:396–401
Pellmar T (1986) Electrophysiological correlates of peroxide damage in guinea pig hippocampus in vitro. Brain Res 364:377–381
Pellmar TC (1987) Peroxide alters neuronal excitability in the CA1 region of guinea-pig hippocampus in vitro. Neuroscience 23:447–456
Pellmar TC (1995) Use of brain slices in the study of free-radical actions. J Neurosci Methods 59:93–98
Pérez-Pinzón MA, Mumford PL, Rosenthal M, Sick TJ (1997) Antioxidants, mitochondrial hyperoxidation and electrical recovery after anoxia in hippocampal slices. Brain Res 754:163–170
Peuchen S, Bolanos JP, Heales SJ, Almeida A, Duchen MR, Clark JB (1997) Interrelationships between astrocyte function, oxidative stress and antioxidant status within the central nervous system. Prog Neurobiol 52:261–281
Qiao H, May JM (2008) Development of ascorbate transporters in brain cortical capillary endothelial cells in culture. Brain Res 1208:79–86
Qiu S, Li L, Weeber EJ, May JM (2007) Ascorbate transport by primary cultured neurons and its role in neuronal function and protection against excitotoxicity. J Neurosci Res 85:1046–1056
Rajan DP, Huang W, Dutta B, Devoe LD, Leibach FH, Ganapathy V, Prasad PD (1999) Human placental sodium-dependent vitamin C transporter (SVCT2): molecular cloning and transport function. Biochem Biophys Res Comm 262:762–768
Ranjan A, Theodore D, Haran RP, Chandy MJ (1993) Ascorbic acid and focal ischaemia in a primate model. Acta Neurochir 123:87–91
Raps SP, Lai JCK, Hertz L, Cooper AJL (1989) Glutathione is present in high concentrations in cultured astrocytes but not in cultured neurons. Brain Res 493:398–401
Rebec GV, Pierce RC (1994) A vitamin as neuromodulator: Ascorbate release into the extracellular fluid of the brain regulates dopaminergic and glutamatergic transmission. Prog Neurobiol 43:537–565
Rhee SG (2006) H2O2, a necessary evil for cell signaling. Science 312:1882–1883
Rhee SG, Kang SW, Jeong W, Chang TS, Yang KS, Woo HA (2005) Intracellular messenger function of hydrogen peroxide and its regulation by peroxiredoxins. Curr Opin Cell Biol 17: 183–189
Rice ME (2000) Ascorbate regulation and its neuroprotective role in the brain. Trends Neurosci 23:209–216
Rice ME, Cammack J (1991) Anoxia-resistant turtle brain maintains ascorbic acid content in vitro. Neurosci Lett 132:141–145
Rice ME, Russo-Menna I (1998) Differential compartmentalization of brain ascorbate and glutathione between neurons and glia. Neuroscience 82:1213–1223
Rice ME, Pérez-Pinzón MA, Lee EJK (1994) Ascorbic acid, but not glutathione, is taken up by brain slices and preserves cell morphology. J Neurophysiol 71:1591–1596
Rice ME, Lee EJK, Choy Y (1995) High levels of ascorbic acid, not glutathione, in the CNS of anoxia-tolerant reptiles contrasted with levels in anoxia-intolerant species. J Neurochem 64:1790–1799
Rice ME, Forman RE, Chen BT, Avshalumov MV, Cragg SJ, Drew KL (2002) Brain antioxidant regulation in mammals and anoxia-tolerant reptiles: balanced for neuroprotection and neuromodulation. Comp Biochem Physiol (Part C) 133:515–525
Rose RC (1993) Cerebral metabolism of oxidized ascorbate. Brain Res 628:49–55
Sato K, Saito H, Katsuki H (1993) Synergism of tocopherol and ascorbate on the survival of cultured neurons. NeuroReport 4:1179–1182
Sauer H, Wartenberg M, Hescheler J (2001) Reactive oxygen species as intracellular messengers during cell growth and differentiation. Cell Physiol Biochem 11:173–186
Savini I, Rossi A, Pierro C, Avigliano L, Catani MV (2008) SVCT1 and SVCT2: key proteins for vitamin C uptake. Amino Acids 34:347–355
Schenk JO, Miller E, Gaddis R, Adams RN (1982) Homeostatic control of ascorbate concentration in CNS extracellular fluid. Brain Res 253:353–356
Sciamanna MA, Lee CP (1993) Ischemia/reperfusion-induced injury of forebrain mitochondria and protection by ascorbate. Arch Biochem Biophys 305:215–224
Seregi A, Schafer A, Komlos M (1978) Protective role of ascorbic acid content against lipid peroxidation. Experientia 34:1056–1057
Seutin V, Scuvee-Moreau J, Masotte L, Dresse A (1995) Hydrogen peroxide hyperpolarizes rat CA1 pyramidal neurons by inducing an increase in potassium conductance. Brain Res 683:275–278
Shimizu N, Matunami T, Onishi S (1960) Histochemical demonstration of ascorbic acid in the locus coeruleus of the mammalian brain. Nature 186:479–480
Siddiq A, Aminova LR, Ratan RR (2007) Hypoxia inducible factor prolyl 4-hydroxylase enzymes: center stage in the battle against hypoxia, metabolic compromise and oxidative stress. Neurochem Res 32:931–946
Siesjö BK (1980) Brain energy metabolism. Wiley, New York, pp 131–150
Siushansian R, Wilson JX (1995) Ascorbate transport and intracellular concentrations in cerebral astrocytes. J Neurochem 65:41–49
Slivka A, Mytilineou C, Cohen G (1987) Histochemical evaluation of glutathione in brain. Brain Res 409:275–284
Sotiriou S, Gispert S, Cheng J, Wang Y, Chen A, Hoogstraten-Miller S, Miller GF, Kwon O, Levine M, Guttentag SH, Nussbaum RL (2002) Ascorbic-acid transporter Slc23a1 is essential for vitamin C transport into the brain and for perinatal survival. Nat Med 8:514–517
Spector R (1977) Vitamin homeostasis in the central nervous system. N Engl J Med 296:1293–1398
Spector R, Lorenzo AV (1973) Ascorbic acid homeostasis in the central nervous system. Am J Physiol 225:757–763
Stamford JA, Kruk ZL, Millar J (1984) Regional differences in extracellular ascorbic acid levels in the rat brain determined by high speed cyclic voltammetry. Brain Res 299:289–295
Starkov AA, Chinopoulos C, Fiskum G (2004) Mitochondrial calcium and oxidative stress as mediators of ischemic brain injury. Cell Calcium 36:257–264
Suzuki YJ, Forman HJ, Sevanian A (1997) Oxidants as stimulators of signal transduction. Free Rad Biol Med 22:269–285
Takanaga H, Mackenzie B, Hediger MA (2004) Sodium-dependent ascorbic acid transporter family SLC23. Pflugers Arch 447:677–682
Tanaka J, Toku K, Zhang B, Ishihara K, Sakanaka M, Maeda N (1999) Astrocytes prevent neuronal death induced by reactive oxygen and nitrogen species. Glia 28:85–96
Tang XD, Santarelli LC, Heinemann SH, Hoshi T (2004) Metabolic regulation of potassium channels. Annu Rev Physiol 66:131–159
Tower DB, Elliott KAC (1952) Activity of the acetylcholine system in cerebral cortex of various unanesthetized animals. Am J Physiol 168:747–759
Trépanier G, Furling D, Puymirat J, Mirault ME (1996) Immunocytochemical localization of seleno-glutathione peroxidase in the adult mouse brain. Neuroscience 75:231–243
Tsukaguchi H, Tokui T, Mackenzie B, Berger UV, Chen X-Z, Wang Y, Brubaker RF, Hediger MA (1999) A family of mammalian Na+-dependent l-ascorbic acid transporters. Nature 399:70–75
Uemura Y, Miller JM, Matson WR, Beal MF (1991) Neurochemical analysis of focal ischemia in rats. Stroke 22:1548–1553
Vatassery GT (1996) Oxidation of vitamin E, vitamin C, and thiols in rat brain synaptosomes by peroxynitrite. Biochem Pharmacol 52:579–586
Vissers MC, Gunningham SP, Morrison MJ, Dachs GU, Currie MJ (2007) Modulation of hypoxia-inducible factor-1 alpha in cultured primary cells by intracellular ascorbate. Free Radic Biol Med 42:765–772
Washburn MP, Wells WW (1999) The catalytic mechanism of the glutathione-dependent dehydroascorbate reductase activity of thioltransferase (glutaredoxin). Biochemistry 38:268–274
Wilson JX (1989) Ascorbic acid uptake by a high-affinity sodium-dependent mechanism in cultured rat astrocytes. J Neurochem 53:1064–1071
Wilson JX, Peters CE, Sitar SM, Daoust P, Gelb AW (2000) Glutamate stimulates ascorbate transport by astrocytes. Brain Res 858:61–66
Winkler BS, Orselli SM, Rex TS (1994) The redox couple between glutathione and ascorbic acid: a chemical and physiological perspective. Free Rad Biol Med 17:333–349
Wood-Kaczmar A, Gandhi S, Wood NW (2006) Understanding the molecular causes of Parkinson’s disease. Trends Mol Med 12:521–528
Xu J, Kao SY, Lee FJ, Song W, Jin LW, Yankner BA (2002) Dopamine-dependent neurotoxicity of α-synuclein: A mechanism for selective neurodegeneration in Parkinson disease. Nat Med 8:600–606
Zhang Y, Dawson VL, Dawson TM (2000) Oxidative stress and genetics in the pathogenesis of Parkinson’s disease. Neurobiol Dis 7:240–250
Acknowledgments
The author gratefully acknowledges support from NIH/NINDS grant NS036362, the National Parkinson Foundation, and the NYU Ricciardi Research Fund, as well as constructive comments on this chapter from Dr. Jyoti C. Patel.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2012 Springer Science+Business Media, LLC
About this chapter
Cite this chapter
Rice, M.E. (2012). Brain Ascorbate: Protective, Yet Permissive for Redox Signaling. In: Choi, IY., Gruetter, R. (eds) Neural Metabolism In Vivo. Advances in Neurobiology, vol 4. Springer, Boston, MA. https://doi.org/10.1007/978-1-4614-1788-0_37
Download citation
DOI: https://doi.org/10.1007/978-1-4614-1788-0_37
Published:
Publisher Name: Springer, Boston, MA
Print ISBN: 978-1-4614-1787-3
Online ISBN: 978-1-4614-1788-0
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)