Abstract
Chemotherapy-induced neutropenia and its complications are major dose-limiting toxicities of cancer chemotherapy. The myeloid growth factors have been shown to reduce the risk of neutropenic events across malignancies, regimens, and associated risk categories often enabling the delivery of greater chemotherapy dose intensity. Three different practice guidelines for the myeloid growth factors have recently been published by major professional organizations. A comprehensive review and comparison of the guidelines using a priori structured content criteria and a previously validated quality appraisal tool are reported. Consistency in the final recommendations from these guidelines is observed for primary prophylaxis with the colony-stimulating factors (CSFs) when the risk of febrile neutropenia is in the range of 20% or greater. There is also consistency in the recommendation that patients receiving regimens associated with lower risk should have CSF use guided by individual risk assessment. Critical quality appraisal indicates that the scope and purpose, stakeholder involvement, and applicability of the guidelines differ little. There is more emphasis on comprehensive literature reviews in the ASCO and EORTC guidelines while the NCCN guidelines are more current based on systematic annual updates. The clarity of presentation also favors the NCCN guidelines with recommendations generally presented as both text and algorithmic diagram. All three new or updated guidelines recommend prophylactic use of the myeloid growth factors in patients at greater than a 20% risk of febrile neutropenia and in those with important factors increasing individual risk of neutropenic complications.
This chapter is reproduced from J Natl Compr Canc Netw. 2007 Feb;5(2):217–28. With kind permission of Cold Spring Publishing.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Chemotherapy-induced neutropenia, including febrile neutropenia (FN), is a major dose-limiting toxicity of many common systemic chemotherapy regimens. Although the reported risk of hematologic toxicity including FN has been consistently underreported in randomized controlled trials (RCTs), it clearly varies across treatment regimens and patient populations [1]. The risk of the initial FN event for many regimens appears to be greatest during the early cycles of chemotherapy [2]. However, when a prophylactic colony-stimulating factor (CSF) is not employed and dose intensity of the same regimen is maintained, the rates of severe or FN are nearly constant across cycles with approximately one-third experiencing two or more events [3]. Most patients with FN require hospitalization for prompt clinical evaluation and the administration of empiric, broad-spectrum antibiotics to reduce the mortality associated with delayed treatment of serious infections in the neutropenic patient. Whatever the risk of occurrence, FN and its consequences are associated with substantial morbidity, mortality, and cost [4].
Neutropenic complications are frequently associated with dose reductions and treatment delays resulting in reduced delivered chemotherapy dose intensity potentially compromising disease control and long-term survival in patients treated with curative intent [5, 6]. Both retrospective studies and prospective RCTs of adjuvant chemotherapy in early-stage breast cancer (ESBC) with patients randomized to different dose intensities have demonstrated a significant relationship between the chemotherapy dose intensity and both disease-free and overall survival [7–10]. In addition, dose-dense regimens based on shortened treatment intervals with CSF support permitting upward of 50% increase in relative dose intensity (RDI) have been shown to improve survival over standard regimens in ESBC and non-Hodgkin lymphoma (NHL) [11, 12]. Nevertheless, a large proportion of patients receiving chemotherapy for potentially curable malignancies are undertreated in the United States [5, 6]. In a study of nearly 20,000 women with ESBC treated in 1,200 oncology practices, more than half received less than 85% of standard dose intensity for their regimen often following an episode of severe or FN [5]. Undertreatment was more prevalent among elderly patients, those receiving certain regimens and overweight or obese patients [13]. Many authors have concluded that such reductions in dose intensity represent a major reason for subsequent treatment failure in patients with responsive malignancies [14].
The myeloid growth factors have been shown to reduce the incidence, duration, and severity of neutropenic events across a broad range of malignancies and regimens often enabling the delivery of full chemotherapy dose intensity [15, 16]. A number of additional RCTs confirming the impact of the myeloid growth factors on reducing the risk of FN have been published over the past few years [17–20]. An updated meta-analysis of RCTs of primary prophylactic G-CSF administered within 3 days of completing myelosuppressive chemotherapy in adult cancer patients has recently been presented [21]. Significant reductions in the risk of FN were observed in both NHL and solid tumor studies, in studies limited to elderly patients as well as all adult age groups and with all forms of G-CSF. In addition to confirming a reduction in the relative risk of FN, this analysis has demonstrated a significant reduction in infection-related mortality.
The decision to use primary CSF prophylaxis in support of patients receiving cancer chemotherapy is generally based on clinical judgment including (1) the estimated risk of neutropenic complications expected based on the treatment regimen; (2) patient-specific characteristics, including age, functional status, and comorbidities; and (3) the treatment intention, balancing the anticipated benefit of chemotherapy with the risk of serious and life-threatening complications [22]. Treatment intention determines the relevance or potential harm associated with alternative options to the addition of CSF support, such as dose reduction, treatment delay, use of an alternative chemotherapy regimen, or withholding treatment altogether. When there are no compelling clinical indications for the use of myeloid growth factors based on reducing the risk of FN or infection-related mortality, the decision to use these agents may be based on economic considerations [23–25].
Older age is consistently identified as a predictor of neutropenic complications, including dose reductions and delays. Other predictors include poor performance status, the presence of comorbid conditions, and baseline laboratory abnormalities. A risk model for time to initial FN in aggressive non-Hodgkin’s lymphoma patients receiving CHOP was derived from a retrospective series of 577 patients and included 6 independent risk factors: age, baseline hemoglobin, heart disease, renal disease, planned dose intensity, and no CSF prophylaxis [2]. A risk model for first-cycle severe or FN based on a prospective registry of nearly 4,500 patients treated with a new chemotherapy regimen at 117 randomly selected practices in the United States is under development [26]. Independent risk factors in multivariate analysis included the type of cancer, treatment regimen, age, certain comorbidities (liver disease, renal disease, diabetes) and concomitant medications, baseline blood counts, the intention to provide full-dose chemotherapy, and no prophylactic CSF support. Once fully validated, such a risk model may guide clinicians and patients on the most efficacious and cost-effective use of myeloid growth factors.
Clinical practice guidelines statements are generally based on a systematic review of a topic in order to guide practitioners and patients in making informed decisions about appropriate health care. This chapter summarizes and contrasts recently developed or updated guidelines for the use of the myeloid growth factors. The results of recently conducted RCTs and meta-analyses of these trials were reviewed by the respective guidelines panels. The similarities and differences between the guidelines content and process are summarized and contrasted.
Methods
Three sets of clinical practice guidelines for the use of the myeloid growth factors have recently been developed or updated by major professional oncology organizations. These include guidelines updates by The American Society of Clinical Oncology (ASCO) and the National Comprehensive Cancer Network (NCCN) along with newly developed guidelines by the European Organization for Research and Treatment of Cancer (EORTC). ASCO published their initial clinical practice guideline for the use of the hematopoietic CSFs in 1994 [27]. These guidelines were subsequently updated in 1996, 1997, and 2000, only recently completing the most recent update in 2006 with the most extensive revision provided since the original report [28, 29]. In 2005, the NCCN presented and published their initial guidelines on the use of the myeloid growth factors which were updated in 2006 as a part of a systematic annual update [30, 31]. In 2006, the EORTC published guidelines for the use of the CSFs in adults with lymphoma and solid tumors [32]. The EORTC guidelines were intended to complement previously published guidelines on the use of the CSFs in the elderly [33].
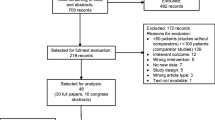
The authors undertook a comprehensive review and comparison of the three guidelines using a priori structured content criteria and previously validated quality appraisal tools. Content areas extracted for each guideline included recommendations related to: primary prophylaxis; secondary prophylaxis; therapeutic use; afebrile neutropenia; sustaining dose intensity; progenitor cell transplant; acute leukemia and myelodysplasia; older patients; pediatric patients; schedule and dose; G-CSF versus GM-CSF; and radiation injury. In addition, risk factors associated with disease, treatment, and patient-specific factors such as age, gender, ethnicity, performance status, the presence of comorbidities, and laboratory abnormalities. Guideline content was also contrasted for the major chemotherapy regimens and assumed rates of FN associated with each regimen.
The quality of the recently updated or developed guidelines was then critically appraised using the Appraisal of Guidelines Research and Evaluation (AGREE) Instrument which provides a framework for assessing the quality of clinical practice guidelines based on the potential for bias in guideline development as well as the internal and external validity and feasibility for practice [34]. The AGREE instrument was developed using a sequential process including item generation, selection, scaling, field evaluation, and finalization. An initial list of 82 items was extracted from existing tools and relevant literature addressing these domains [35]. A draft was field tested on the 100 guidelines by 194 appraisers and after further refinement, a final instrument underwent further validation The internal consistency of the final instrument was acceptable with Cronbach’s alpha ranging from 0.64 to 0.88 and intraclass correlation coefficients ranging from 0.57 to 0.91 with different appraisers [36]. The use of the AGREE instrument involves taking into account the benefits, harms, and costs of the recommendations, as well as their practical use. Therefore, the assessment includes judgments about the methods used for developing the guidelines, the content of the final recommendations, and the factors linked to their application. The AGREE Instrument assesses both the quality of the recommendations as well as reporting. The tool consists of 23 key items organized in 6 domains, each intended to capture a separate dimension of quality. Items 1–3 assess the scope and purpose of guideline, the clinical questions being asked, and the target population. Items 4–7 reflect the stakeholder involvement or the extent to which the guideline represents the views of its users. Items 8–14 assess the rigor of guideline development or the process used to gather and synthesize the evidence, the methods of developing the recommendations as well as to update them. Items 15–18 evaluate the clarity and presentation of the guidelines in terms of language and format. Items 19–21 assess the applicability of the guidelines including the impact on behavior and costs. Items 22–23 evaluate the editorial independence of the recommendations and any conflicts of interest. As recommended by the developers, the guidelines were assessed by two independent appraisers (GHL, JMK). Each scale item was rated from 4 “Strongly Agree” to 1 “Strongly Disagree”, with 3 “Agree” and 2 “Disagree.” Domain scores were calculated by summing up all the scores of the individual scale items in a domain. The total score was standardized by presenting the score as a percentage of the maximum possible score for each domain. The developers recommend that the domain scores not be aggregated into a single score and that they be presented and compared independently.
Results
Myeloid growth factor guidelines from the NCCN were initially put forward in 2005 and then updated in 2006. As summarized in Fig. 9.1, these guidelines recommend a stepwise process of starting with an initial evaluation based on the type of cancer, chemotherapy regimen, patient-specific risk factors, and treatment intention. This is to be followed by a formal risk assessment, then a recommendation on the use of the myeloid growth factors based on the level of risk. Unlike the ASCO guidelines in effect at the time, the NCCN guidelines recommended use of G-CSF prophylaxis when patients are thought to be at 20% or greater risk. Patients at intermediate risk, 10–20%, may be considered for prophylactic G-CSF if there are additional considerations that either may place the patient at greater risk for FN or for serious consequences of FN such as prolonged hospitalization or death. Routine prophylaxis with G-CSF should not be employed in patients thought to have a low risk of FN (under 10%). The 2006 ASCO White Blood Cell Growth Factor Guidelines Update Committee agreed unanimously that reduction in FN was an important clinical outcome that justified use of the CSFs when the risk of FN was about 20% and no other equally effective regimen that did not require CSF was available. This was a distinct change from the threshold recommended in previous ASCO guidelines for some 12 years. An additional change with the 2006 guidelines was the introduction of several derivative products including executive and patient summaries, a PowerPoint slide set, and a work sheet or flow sheet to assist practitioners in the application of the guidelines as well as monitoring for guidelines compliance when appropriate. As shown in Fig. 9.2, along with other information, this flow sheet assessed the justification for use of the CSFs and the treatment plan including dose, schedule, route, and duration of use of the white blood cell growth factors. The EORTC also issued guidelines for the use of G-CSF in 2006. As shown in Fig. 9.3, the overall recommendation for prophylactic use of G-CSF is remarkably similar to that of the NCCN and revised ASCO guidelines with routine use in those receiving a regimen with a 20% or greater risk, none when the risk is less than 10%, and then an individual risk assessment in those receiving a regimen associated with a risk of 10–20%. If the individual patient risk for FN after such assessment is deemed to be 20% or greater, primary prophylaxis with G-CSF is recommended.
Schematic diagram of the decision process for the use of the myeloid growth factors based on the NCCN Guidelines [3]. After an initial evaluation based on disease, regimen, patient risk factors, and the intention of treatment, the risk of febrile neutropenia should be formally assessed with each patient classified as high (>20%), intermediate (10–20%), or low (<10%) risk. The use of prophylactic CSFs can then be based on the individual patient’s assessed risk
Flow sheet developed by ASCO to accompany the updated 2006 White Blood Cell Growth Factor Guidelines [29]. The flow sheet assesses the justification for use of a white blood cell growth factor for primary or secondary prevention, therapeutic use, or other reasons and then provides a framework for documenting the dose, schedule, and actual administration of such support. The flow sheet is available on the website of the Journal of Oncology Practice. http://www.jopasco.org/jopasco/Main/
Schematic of the clinical decision pathway for the use of prophylactic G-CSF from the recently published EORTC CSF Guidelines [32]. Primary prophylaxis is recommended routinely for a risk of FN ≥ 20% and not for patients at a <10% risk. Patients with a risk of FN of 10–20% should be further assessed for their individual risk based on age and other disease-specific, treatment-specific, and patient-specific risk factors. Patients should be considered for primary G-CSF prophylaxis if their individual risk is thought to be ≥20%
Table 9.1 summarizes and compares recommendations of the three myeloid growth factor guidelines for the major topics considered as discussed in the methods section. Clearly, not every topic was discussed or equally considered across all guidelines. However, remarkable similarity in the final recommendations is observed for the three guidelines for primary prophylaxis, secondary prophylaxis, sustaining dose intensity, and management of the elderly. There is consistency across the guidelines in the recommendation to consider prophylactic use of the CSFs when the risk of FN is in the range of 20% or greater (Table 9.2). Likewise, there is consistency in the recommendations that patients at lower levels of risk should have their individual risk assessed by the clinician and CSF use considered if there are sufficient risk factors such as advanced age to indicate a greater level of individual patient risk than the RCTs for a given regimen might otherwise indicate.
Table 9.3 summarizes and contrasts the disease-related, treatment-related, and patient-related factors considered to increase the risk of FN and its complications in each of the guidelines. While some differences in emphasis exist, there is consistency across guidelines in recognizing the importance of assessing patient-specific risk factors such as advanced disease, previous episodes of FN, prior extensive chemotherapy, age ≥ 65, poor performance or nutritional status, serious comorbidities, and low baseline blood counts or bone marrow involvement. The issues related to the use of the CSFs for treating FN, afebrile neutropenia, progenitor cell transplantation, acute leukemia and myelodysplastic syndrome (MDS), pediatric patients, and the recommended dose and schedule are not addressed by all of the guidelines (Table 9.1).
Each of the guidelines lists common regimens associated with varying levels of risk for FN. Table 9.4 summarizes and compares the regimens that were considered representative of those used in the treatment of common cancers and the assumed level of risk for FN associated with these regimens. Given the differences in process and the inherent variation in oncology practice between Europe and the United States, differences in the regimens mentioned are not a surprise. The EORTC guidelines present considerably more regimens including many that are not mentioned in the ASCO and NCCN guidelines probably reflecting differences in oncology practice in Europe. Although the presumed risk of FN associated with regimens presented across guidelines is relatively comparable, there are some differences evident in the interpretation of clinical trial data on the risk of FN with common regimens presented in these guidelines including doxorubicin and cyclophosphamide (AC) and AC–Docetaxel in breast cancer and cisplatin and paclitaxel (DP) in lung cancer.
Finally, each guideline was critically appraised by the authors independently using the previously validated AGREE measurement tool and discrepancies resolved as discussed in the methods section. Table 9.5 summarizes and contrasts the results of this critical appraisal by domain of focus of the scale. For issues related to the scope and purpose, stakeholder involvement, and applicability of the guidelines, little or no differences in appraisal were found. The NCCN guideline was appraised as less rigorous in its development largely related to the recognized consensus process employed compared to a more rigorous evidence-based approach used by ASCO and EORTC. While a literature review was undertaken by each of the Panels, the review process was found to be more systematic and comprehensive in the ASCO and EORTC guidelines than in the NCCN guidelines in which no criteria for the search and selection of relevant literature are presented. Differences are also noted in the review process with an explicit process for independent and external review of the ASCO and EORTC guidelines. Similarly, there appears to be no indication of individual conflicts of interest for Panel members of the NCCN Panel as there are for the ASCO and EORTC guidelines. In contrast, the NCCN guidelines are updated on an annual basis while no explicit process for update of the ASCO and EORTC guidelines are stated. In addition, the clarity of presentation favors the NCCN guidelines with the recommendations generally presented in both text and algorithmic diagrams for ease of access and use. While no meaningful overall summary measure can be derived from the critical appraisal, the differences observed are largely accountable by the differences in process employed by the different professional groups involved. All guidelines in the end recommend further clinical investigation of a number of areas that remain unclear.
Discussion
Chemotherapy-induced neutropenia and its complications are major dose-limiting toxicities of cancer chemotherapy. The myeloid growth factors have been shown to reduce the risk of FN and its related complications. Three different practice guidelines for the myeloid growth factors have recently been published by major professional organizations. A comprehensive review and comparison of the guidelines demonstrates remarkable consistency in the final recommendations from these guidelines for the use of CSF primary prophylaxis in patients at approximately a 20% risk of FN or greater. All guidelines also recommend CSF use be considered when individual risk assessment by the clinician concludes a patient is at increased risk.
The quality of clinical practice guidelines has recently been brought into question [37]. Overall, the quality of the myeloid growth factor guidelines was rated as good with little or no difference between guidelines in the stated scope and purpose, stakeholder involvement, and applicability of the guidelines. There is clearly more emphasis on systematic and comprehensive literature reviews in the ASCO and EORTC guidelines, while the NCCN guidelines are updated on an annual basis and appear to offer better clarity of presentation.
References
Dale DC, McCarter GC, Crawford J, et al. Myelotoxicity and dose intensity of chemotherapy: reporting practices from randomized clinical trials. J Natl Compr Canc Netw. 2003;1:440–54.
Lyman GH, Morrison VA, Dale DC, Crawford J, et al. Risk of febrile neutropenia among patients with intermediate-grade non-Hodgkin’s lymphoma receiving CHOP chemotherapy. Leuk Lymphoma. 2003;44:2069–76.
Lyman GH. Guidelines of the National Comprehensive Cancer Network on the use of the myeloid growth factors with cancer chemotherapy: a review of the evidence. J Natl Compr Canc Netw. 2005;3:557–71.
Kuderer NM, Dale D, Crawford J, Cosler L, Lyman GH. The morbidity, mortality and cost of febrile neutropenia in cancer patients. Cancer. 2006;106:2258–66.
Lyman GH, Dale D, Crawford J. Incidence, practice patterns and predictors of low dose intensity in adjuvant breast cancer chemotherapy: results of a nationwide study of community practices. J Clin Oncol. 2003;21:4524–31.
Lyman GH, Dale D, Friedberg J, Crawford J, Fisher RI. Incidence and predictors of low chemotherapy dose intensity in aggressive non-Hodgkin’s lymphoma: a nationwide study. J Clin Oncol. 2004;22:4302–11.
Bonadonna G, Valagussa P, Moliterni A, et al. Adjuvant cyclophosphamide, methotrexate, and fluorouracil in node-positive breast cancer: the results of 20 years of follow-up. N Engl J Med. 1995;332:901–6.
Early Breast Cancer Trialists’ Collaborative Group. Effects of chemotherapy and hormonal therapy for early breast cancer on recurrence and 15-year survival: an overview of the randomized trials. Lancet 2005;365:1687–1717.
Budman DR, Berry DA, Cirrincione CT, et al. Dose and dose intensity as determinants of outcome in the adjuvant treatment of breast cancer. The Cancer and Leukemia Group B. J Natl Cancer Inst. 1998;90:1205–11.
Bonneterre J, Roche H, Kerbrat P, et al. Epirubicin increases long-term survival in adjuvant chemotherapy of patients with poor-prognosis, node-positive, early breast cancer: 10-year follow-up results of the French Adjuvant Study Group 05 randomized trial. J Clin Oncol. 2005;23:2686–93.
Citron ML, Berry DA, Cirrincione C, et al. Randomized trial of dose-dense versus conventionally scheduled and sequential versus concurrent combination chemotherapy as postoperative adjuvant treatment of node-positive primary breast cancer: first report of Intergroup Trial C9741/Cancer and Leukemia Group B Trial 9741. J Clin Oncol. 2003;21:1431–9.
Pfreundschuh M, Trümper L, Kloess M, et al. 2-weekly or 3-weekly CHOP chemotherapy with or without etoposide for the treatment of elderly patients with aggressive lymphomas: results of the NHL-B2 trial of the DSHNHL. Blood. 2004;104:634–41.
Griggs JJ, Sorbero MES, Lyman GH. Undertreatment of obese women receiving breast cancer chemotherapy. Int Arch Med. 2005;165:1267–73.
Chu E, DeVita V. Principles of medical oncology. In: DeVita VT, Rosenberg SA, editors. Cancer: principles and practice of oncology. 7th ed. Philadelphia, PA: Lippincott; 2006. pp. 295–306.
Crawford J, Ozer H, Stoller R, et al. Reduction by granulocyte colony-stimulating factor of fever and neutropenia induced by chemotherapy in patients with small-cell lung cancer. N Engl J Med. 1991;325:164–70.
Lyman GH, Kuderer NM, Djulbegovic B. Prophylactic granulocyte colony-stimulating factor in patients receiving dose-intensive cancer chemotherapy: a meta-analysis. Am J Med. 2002;112:406–11.
Osby E, Hagberg H, Kvaloy S, et al. CHOP is superior to CNOP in elderly patients with aggressive lymphoma while outcome is unaffected by filgrastim treatment: results of a Nordic Lymphoma Group randomized trial. Blood. 2003;101:3840–8.
Doorduijn JK, van der HB, van Imhoff GW, et al. CHOP compared with CHOP plus granulocyte colony-stimulating factor in elderly patients with aggressive non-Hodgkin’s lymphoma. J Clin Oncol. 2003;21:3041–50.
Timmer-Bonte JN, de Boo TM, Smit HJ, et al. Prevention of chemotherapy-induced febrile neutropenia by prophylactic antibiotics plus or minus granulocyte colony-stimulating factor in small-cell lung cancer: a Dutch randomized phase III study. J Clin Oncol. 2005;23:7974–84.
Vogel C, Wojtukiewicz MZ, Caroll RR, et al. First and subsequent cycle use of pegfilgrastim prevents febrile neutropenia in patients with breast cancer: a multicenter, double-blind, placebo-controlled phase III study. J Clin Oncol. 2005;23:1178–84.
Kuderer NM, Crawford J, Dale DC, Lyman GH. Meta-analysis of prophylactic granulocyte colony-stimulating factor (G-CSF) in cancer patients receiving chemotherapy. J Clin Oncol. 2005;23:758 s. Abstract 8117.
Lyman GH, Lyman CH, Agboola O. Risk models for predicting chemotherapy-induced neutropenia. Oncologist. 2005;10:427–37.
Lyman GH, Lyman CG, Sanderson RA, Balducci L. Decision analysis of hematopoietic growth factor use in patients receiving cancer chemotherapy. J Natl Cancer Inst. 1993;85:488–93.
Lyman GH, Kuderer N, Greene J, Balducci L. The economics of febrile neutropenia: implications for the use of colony-stimulating factors. Eur J Cancer. 1998;34:1857–64.
Lyman GH, Kuderer NM. Economics of hematopoietic growth factors. In: Morstyn G, Foote M, Lieschke GJ, editors. Cancer drug discovery and development. Hematopoietic growth factors in oncology: basic science and clinical therapeutics. Totowa, NJ: Humana Press Inc; 2004. pp. 409–443.
Lyman GH, Kuderer NM, Crawford J, et al. Prospective validation of a risk model for first cycle neutropenic complications in patients receiving cancer chemotherapy. J Clin Oncol. 2006;24:483 s. Abstract 8561.
American Society of Clinical Oncology. Recommendations for the use of hematopoietic colony-stimulating factors: evidence-based, clinical practice guidelines. J Clin Oncol. 1994;12(11):2471–508.
Ozer H, Armitage JO, Bennett CL, et al. Update of recommendations for the use of hematopoietic colony-stimulating factors: evidence-based, clinical practice guidelines. American Society of Clinical Oncology Growth Factors Expert Panel. J Clin Oncol. 2000;2000(18):3558–85.
Smith TJ, Khatcheressian J, Lyman GH, et al. Update of recommendations for the use of white blood cell growth factors: an evidence-based clinical practice guideline. J. Clin Oncol. 2006;24:3187–205.
Crawford J, Althaus B, Armitage J, et al. Myeloid growth factors. J Natl Compr Canc Netw. 2005;3:540–55.
Crawford J, Althaus B, Armitage J, Blayney DW, Cataland S, Dale DC, Demetri GD, Foran J, Heaney ML, Htoy S, Kloth DD, Lyman GH, Michaud L, Motl S, Vadham-Raj S, Wong MK. Myeloid growth factors. 2006. http://www.nccn.org/professionals/physician_gls/PDF/myeloid_growth.pdf.
Aapro MS, Cameron DA, Pettengell R, et al. European Organisation for Research and Treatment of Cancer (EORTC) Granulocyte Colony-Stimulating Factor (G-CSF) Guidelines Taskforce. EORTC guidelines for the use of granulocyte colony-stimulating factor in adult patients with chemotherapy-induced febrile neutropenia. Eur J Cancer 2006;42: 2433–53.
Repetto L, Biganzoli L, Koehne CH, et al. EORTC cancer in the elderly task force guidelines for the use of colony-stimulating factors in elderly patients with cancer. Eur J Cancer. 2003;39(16):2264–72.
The AGREE Collaboration. Appraisal of the Guidelines for Research and Evaluation (AGREE) Instrument. http://www.agreecollaboraiton.org.
AGREE Collaboration. Development and validation of an international appraisal instrument for assessing the quality of clinical practice guidelines: the AGREE project. Qula Saf Health Care. 2003;12:18–23.
Burgers JS, Fervers B, Haugh M, et al. International assessment of the quality of clinical practice guidelines in oncology using the appraisal of guidelines and research and evaluation instrument. J Clin Oncol. 2004;22:2000–7.
Shanaeyfelt TM, Mayo-Snith MF, Rothwangl J. Are guidelines following guidelines? The methodological quality of clinical practice guidelines in the peer-reviewed medical literature. JAMA. 2006;281:1900–5.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2010 Springer Science+Business Media, LLC
About this chapter
Cite this chapter
Lyman, G.H., Kleiner, J.M. (2010). Summary and Comparison of Myeloid Growth Factor Guidelines in Patients Receiving Cancer Chemotherapy. In: Lyman, G., Dale, D. (eds) Hematopoietic Growth Factors in Oncology. Cancer Treatment and Research, vol 157. Springer, Boston, MA. https://doi.org/10.1007/978-1-4419-7073-2_9
Download citation
DOI: https://doi.org/10.1007/978-1-4419-7073-2_9
Published:
Publisher Name: Springer, Boston, MA
Print ISBN: 978-1-4419-7072-5
Online ISBN: 978-1-4419-7073-2
eBook Packages: MedicineMedicine (R0)