Abstract
It is estimated that 80–90% of individuals with autism spectrum disorders (ASD) demonstrate sensory-related problem behaviors such as self-stimulating behaviors (finger flicking or excessive rocking), avoiding behaviors (such as placing hands over ears in response to typical levels of auditory input), sensory seeking behaviors (twirling, chewing, etc.), “tuning out” behaviors such as not responding to their name or other environmental cues, and difficulty enacting purposeful plans of action (Baranek et al. 2006; Huebner 2001; Kientz and Dunn 1997; O’Neill and Jones 1997; Ornitz 1974, 1989; Rogers et al. 2003; Tomchek and Dunn 2007). These behaviors, which may have a sensory basis, are termed sensory dysfunction (SD) and findings show that they limit participation in play, social, self-care and learning activities (Adrien et al. 1987; Baranek 1999, 2002; Edelson et al. 1999; Grandin 1995; Leekam et al. 2007; McClure and Holtz-Yotz 1991; Leekam et al. 2007, 1997; O’Riordan and Passetti 2006; Ornitz 1974, 1989; Rapin and Katzman 1998; Rogers and Ozonoff 2005; Schaaf et al. 2010; Williams 1992, 1994). Although interventions for SD are among the most requested services for children with ASD (Mandell et al. 2005; Green et al. 2006), there is limited evidence about their efficacy (Baranek et al. 2006; Dawson and Watling 2000; Rogers and Ozonoff 2005). The National Research Council (2001, p. 131) reports that there is a “pressing need for more basic and applied research to address the sensory aspects of behavior problems (in children with ASD).” Baranek (2002) also stressed that “best practice” for children with ASD should include interventions to address SD, but that more research is needed to guide parents, teachers, and other professionals to make informed decisions about intervention. Most studies to date fail to link basic science findings to behavioral or functional changes, and thus, it is not possible to determine the specific processes underlying behavioral gains reported in intervention studies. The purpose of this chapter is to define and describe SD in ASD, evaluate the evidence for current interventions that address SD in ASD, and discuss practice recommendations in light of these data.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Autism Spectrum Disorder
- Autism Spectrum Disorder
- Galvanic Skin Response
- Sensory Integration
- Social Validity
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
Introduction
It is estimated that 80–90% of individuals with autism spectrum disorders (ASD) demonstrate sensory-related problem behaviors such as self-stimulating behaviors (finger flicking or excessive rocking), avoiding behaviors (such as placing hands over ears in response to typical levels of auditory input), sensory seeking behaviors (twirling, chewing, etc.), “tuning out” behaviors such as not responding to their name or other environmental cues, and difficulty enacting purposeful plans of action (Baranek et al. 2006; Huebner 2001; Kientz and Dunn 1997; O’Neill and Jones 1997; Ornitz 1974, 1989; Rogers et al. 2003; Tomchek and Dunn 2007). These behaviors, which may have a sensory basis, are termed sensory dysfunction (SD) and findings show that they limit participation in play, social, self-care and learning activities (Adrien et al. 1987; Baranek 1999, 2002; Edelson et al. 1999; Grandin 1995; Leekam et al. 2007; McClure and Holtz-Yotz 1991; Leekam et al. 2007, 1997; O’Riordan and Passetti 2006; Ornitz 1974, 1989; Rapin and Katzman 1998; Rogers and Ozonoff 2005; Schaaf et al. 2010; Williams 1992, 1994). Although interventions for SD are among the most requested services for children with ASD (Mandell et al. 2005; Green et al. 2006), there is limited evidence about their efficacy (Baranek et al. 2006; Dawson and Watling 2000; Rogers and Ozonoff 2005). The National Research Council (2001, p. 131) reports that there is a “pressing need for more basic and applied research to address the sensory aspects of behavior problems (in children with ASD).” Baranek (2002) also stressed that “best practice” for children with ASD should include interventions to address SD, but that more research is needed to guide parents, teachers, and other professionals to make informed decisions about intervention. Most studies to date fail to link basic science findings to behavioral or functional changes, and thus, it is not possible to determine the specific processes underlying behavioral gains reported in intervention studies. The purpose of this chapter is to define and describe SD in ASD, evaluate the evidence for current interventions that address SD in ASD, and discuss practice recommendations in light of these data.
What Is Sensory Dysfunction in ASD?
Courtney is a six-year-old child diagnosed with ASD who attends a public school in a semi-inclusive classroom for children with special needs. Today, like most other days, Courtney is having difficulty participating in the class activities. The teacher already reprimanded Courtney several times this morning for “fidgeting” in her seat during circle time, disrupting the other children by making silly noises with her mouth and constantly getting up to wander about the room. During snack time, at 10 am, Courtney has an outburst and refuses to eat the graham crackers and milk provided by the school. The ticklish sensation of the milk on her lips is bothersome and the graham crackers are “too rough” for her liking. Instead of participating in snack time, Courtney sits by herself. During morning recess at 11 am, Courtney keeps to herself and is afraid to play on the slide with the other children. Finally, she runs to the swings and uses them to spin in circles. At 11:30 am, when the lunch bell rings, Courtney places her hands over her ears and runs into the closet, bothered by the noise. A classmate tries to comfort her but Courtney shoves the girl away and hurts her. In the cafeteria, Courtney becomes increasingly agitated. She sits alone with her hands over her ears until she feels able to negotiate the lunch line. After the crowd subsides, with the help of the classroom aide, Courtney manages to select a few items from the menu and place them on her tray. On the way back to her seat, Courtney trips over a backpack lying in the aisle and spills her tray. The other children begin to laugh. Courtney runs from the cafeteria with her hands covering her ears. The teacher finds her in the gym wedged under several gym mats that she has piled on top of herself. Her hands are over her ears and she is rocking.
Courtney is a child with ASD and a SD that contributes to her disability. Families indicate that SD is one of the most significant factors limiting their ability to participate in home and community activities (Mandell et al. 2005). For example, one parent of a child with ASD and SD stated, “(After) our last commercial flying experience, we both swore off of it. Never again. His sensory sensitivity made it unbearable. He was just inconsolable.” (Benevides et al. 2010). Others indicate that they must orchestrate their family routines and outings to accommodate the child’s SD. They are unable to participate as a family in mealtimes (they must feed the child with ASD earlier than the others due to food sensitivities), family outings such as going to the movies are impossible (the child is unable to tolerate typical levels of noise and stimulation of crowds), or socialization with friends (“our child’s self-stimulating behaviors make it impossible to be comfortable visiting with friends or meeting other children for a play date”) (Larson 2006; Schaaf et al. (in press); Schaaf and Nightlinger 2007). Self-reports from individuals with ASD confirm these findings and are particularly potent in their descriptions of the impact of SD on participation in daily life activities (Grandin 1995; O’Neill and Jones 1997; Williams 1992, 1994). These self-reported data portray how SD limits the ability of individuals with ASD to participate fully in society. For example, Temple Grandin, a high functioning woman with ASD, articulates how her unusual processing of auditory, visual, and tactile information impedes social conversation because she is over-stimulated and distracted by the non-essential stimuli (Grandin 1995). As a result, she does not enjoy or participate in many of the daily activities of her peers.
Interventions to Address Sensory Dysfunction
It is widely accepted that a comprehensive educational program for children with ASD is the most effective in achieving optimal outcomes (National Research Council 2001). In addition to educational, speech and language, and behavioral services, a comprehensive program for individuals with ASD often includes occupational therapy services to address SD and other sensory-motor delays. In fact, Mandell et al. (2005) and Green et al. (2006) found that occupational therapy to address SD is among the top three services requested by families of children with ASD. Schwenk and Schaaf (2003) found that 99% of the therapists surveyed who work in public school settings with children with ASD used strategies to address SD as part of their therapeutic approach.
Occupational therapists follow a professional clinical reasoning framework to evaluate and design interventions for children with SD. Treatment follows a well-documented theoretical framework (Ayres 1979, 1989; Schaaf et al. 2010) directed by a set of principles that guide the therapists’ clinical reasoning and interactions with the child (Schaaf and Miller 2005). The therapist chooses individually tailored sensory-motor activities for the child based on areas of need identified by systematic assessment. For example, for a child who is constantly rocking in his seat, systematic assessment might suggest a greater need for vestibular input. To address this issue the therapist generally takes a three-pronged approach:
-
Work directly with the child using specialized equipment in a clinic that allows the child to experience vestibular input such as swings, bolsters, or scooter boards
-
Provide environmental adaptations such as a small inflated cushion for the child to sit on in the classroom (thereby providing needed vestibular input and decreasing disruptive rocking behaviors)
-
Provide consultation to the parent or teacher, for example, to suggest that the school team provide greater opportunities for the child to access playground equipment, such as swings, to provide regular intervals of the needed input and thus decrease the rocking behaviors (environmental adaptation)
It is worth noting that the prescribed activities are meaningful to the child (i.e., developmentally appropriate and contextualized in play) and embedded within the daily routine when possible. The therapist maintains data on whether these strategies are effective in reducing the disruptive behaviors and improving the child’s attention and participation in class or home and community activities. Thus, by engaging the child in individually tailored sensory-motor activities, it is hypothesized that the child’s nervous system is better able to modulate, organize, integrate and utilize information from the environment, and thus, is not driven to seek or avoid sensation in maladaptive ways. Adequate processing of sensory information, in turn, provides a foundation for further adaptive responses and participation in activities through adaptive neuroplastic mechanisms (Baranek 2002). Parent education and environmental adaptations are provided in tandem with direct intervention to support the child’s sensory-motor needs.
This approach is child-centered and provides a just-right challenge (scaffolding) to facilitate progressively more sophisticated adaptive sensory-motor responses while engaging the child in affectively meaningful and developmentally appropriate play interactions. The child’s focus is intended to be placed on play (intrinsically motivated) and not on cognitive-behavioral strategies or repetitive drills; thus, gains made during treatment are expected to be generalized to everyday life situations. Treatment goals focus on improving the ability to process and utilize sensory information, so that the child can develop better sensory modulation for attention and behavioral control, or the ability to form perceptual schemas and practical abilities as a foundation for greater participation in school, social, and daily living activities (Baranek 2002; Mailloux 2006). Thus, the sensory-integrative approach is utilized within a professional domain of practice, such as occupational therapy, and is focused on improving the child’s participation in activities through the use of individually prescribed sensory motor activities.
Although this approach is based on solid theoretical principles that are contextualized within the professional framework of occupational therapy (Baranek 2002;), there is no manualized protocol and, thus, its utility and efficacy has not been systematically tested. Therefore, the evidence to support this approach is sparse and the studies that do exist have methodological flaws including that they do not explicitly describe the intervention and do not have a measure of fidelity, making it difficult to determine if the intervention provided was in keeping with the theoretical principles of the sensory-integrative approach. Evaluation of the evidence that does exist is further complicated by the fact that there are several techniques that utilize sensory stimulation but are not in keeping with the sensory-integrative approach and which are confused with it (Cox et al. 2009). These techniques usually provide passive stimulation to one sensory system rather than the holistic, child-directed, playful approach to intervention that is contextualized within a professional framework that is the hallmark of the sensory-integrative approach. The sensory-integrative approach is guided by the set of principles outlined in Table 9.1 (Parham et al. in press). The reader is referred to the work of Schaaf et al. (2010) for a full description of the sensory-integrative approach and the principles that guide the intervention.
Evidence for the Sensory-Integrative Approach
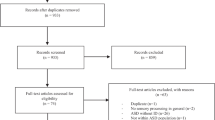
Like many other therapeutic interventions utilized with children with ASD, solid evidence for interventions to address SD in ASD is just beginning to surface and data are mainly from case reports, studies using single subject experimental designs (SSED), or small group design studies. To access available studies, we utilized Ovid Medline, PsychInfo, and OTSearch from 1995 forward using the search terms of “sensory integration,” “sensory therapy,” “sensory occupational therapy,” “occupational therapy sensory integration,” “auditory integration training,” “vestibular therapy,” “brushing,” “visual therapy,” “tactile therapy,” “tactile treatment,” “deep pressure,” “and pressure vest.” We have included one classic study of the sensory-integrative approach that dates back to 1980 because it was completed by the author of the sensory integration theory and thus we felt that it was important to include (Ayres and Tickle 1980). Our search yielded studies using both the sensory-integrative approach and sensory stimulation techniques. In the following sections, we report first on studies of intervention using a sensory-integrative approach and then on those that used a sensory stimulation technique.
Table 9.2 lists the studies that utilized the sensory-integrative frame of reference within occupational therapy, specifically investigated interventions for SD, and show emerging evidence. Collectively, they report that individuals with ASD and SD who receive occupational therapy using a sensory-integrative approach demonstrated gains in play, individualized goals, and social interaction (Ayres and Tickle 1980; Case-Smith and Bryan 1999; Linderman and Stewart 1999; Schaaf and Nightlinger 2007; Watling and Dietz 2007) and a decrease in sensory symptoms (Smith et al. 2005; Fazlioglu and Baran 2008).
Schaaf and Nightlinger (2007) case study reports on a child who received occupational therapy using a sensory-integrative approach and showed improvements in the hypothesized direction in several behaviors. The child in this study demonstrated improved motor skills, social skills, and adaptive behaviors (e.g., improved ability to tolerate foods and thus improved participation in mealtime with the family, as measured by individual Goal Attainment scales, and decreased SD, as measured by the sensory profile scores and individual Goal Attainment scales). The results obtained were consistent with anecdotal reports from parents and other sources describing how quality of life for the family improved because the child’s sensory over-responsive behaviors decreased and his ability to tolerate and participate in family activities improved (e.g., he was able to maintain self-regulation during grooming activities and to interact with other children during community playgroup activities). This study is promising in terms of its evidence for a sensory-integrative approach for ASD as it details the intervention in a replicable way and demonstrates how the intervention follows the theoretical principles of the sensory-integrative approach. In addition, the outcomes have social validity in that the child made gains that had an impact on his everyday life and the mother was extremely satisfied with the results. However, the study is limited in that it is a case study report, there is no measure of fidelity, and the rater was not blind to intervention.
Fazlioglu and Baran (2008) using a randomized two-group design, this study found statistically significant (p < 0.05) improvements between the groups in sensory-related behaviors pre- and post-intervention as measured by the Sensory Evaluation Form for Children with Autism. The study used a combination of sensory integration strategies (individually designed vestibular, somatosensory, and other sensory activities where the child was an active participant) and a “sensory diet” (systematically applied sensory stimuli) with 30 children diagnosed with low-functioning autism according to the criteria of the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV-TR; APA 2000). This study is promising in terms of its evidence for a sensory-integrative approach for ASD as the subject randomization is valid, the protocol for intervention is described in a manner that can be replicated (the principles and philosophy are described), the data analysis is linked to the research questions, and there is good social validity. However, there is no fidelity measure or mention of whether the raters were blind to the group assignment.
Smith et al. (2005) study considered seven subjects with ASD, aged 8–19 years. The study utilized a single subject withdrawal design (A–B–A–B) where weeks 1 and 3 represented the control sessions (30 min/day of table-top activities) and weeks 2 and 4 were the treatment sessions consisting of 30 min per day for 5 days per week. They video recorded the participants and performed frequency counts for presence and number of self-stimulating behaviors. They found that the overall frequency of self-stimulating behaviors decreased over the 4 weeks. Teachers also reported fewer self-stimulating and self-injurious behaviors during the treatment. This study was promising in that it describes the intervention and it is clear that it was in keeping with the principles of sensory integration (Smith et al. 2005, p. 421):
Subjects engaged in sensory based treatment that included a variety of tactile, proprioceptive and vestibular input, based on their unique sensory needs. This is distinguished from sensory stimulation programs in that treatment was individualized based on assessment results, and the type or types of sensation and specific activities used.… Vestibular, tactile and proprioceptive based activities were primarily used, which is consistent with the accepted characteristics of intervention.
However, the study was limited by the small, homogenous sample and lack of a fidelity measure. In addition, there was no mention as to whether the raters were blinded to the treatment versus control weeks.
Linderman and Stewart (1999) study used a single subject A–B design to explore the effects of occupational therapy using a sensory-integrative approach on the functional behaviors of two young children (aged 3 years 3 months and 3 years 9 months) with pervasive developmental disabilities (PDD). They used the revised Functional Behavioral Assessment for Children with Sensory Integrative Dysfunction (Cook 1991) to evaluate the duration, quality and frequency of targeted sensory behaviors. Participant 1 demonstrated major improvements in social interactions, approach to new activities and responses to hugging and holding. Participant 2 displayed improvements in social interaction and response to movement. Although the authors state that treatment was in keeping with the sensory-integrative principles (i.e., child-directed treatment and active participation of the child) there is no specific information about the treatment, no consideration was given to the effect of other interventions (e.g., one subject enrolled in a preschool and another started a vitamin regimen), and the sample size was small and homogenous.
Case-Smith and Bryan (1999) conducted a study with a single subject A–B design of five subjects with autism, at 4 and 5 years of age. Baseline measures of play, non-engaged behaviors, child–adult interactions, and peer interactions were obtained via video-coding for a 3-week period. Data were analyzed by plotting behaviors on line graphs, computing means for each phase, and then calculating regressions for each phase. Data from each phase were compared using the Wilcoxon signed rank test to assess differences in the means for each phase. Results were mixed as there were improvements in some areas but not in others. For example, following intervention, three of the five children showed significant improvements in mastery play, four of the children demonstrated significantly decreased non-engaged behaviors, and only one participant demonstrated a significant increase in adult interactions. None of the participants demonstrated significant increases in peer interactions. Despite the mixed findings, this study is promising in that it clearly describes the participants and the outcome measures and the intervention is described in detail. The data analysis is linked to the research questions and use of visual inspection is relevant and appropriate.
Watling and Dietz (2007) study used a withdrawal SSED (A–B–A–B) with four boys between the ages of 3 and 4.4 years of age who were diagnosed with ASD (criteria for diagnosis not known) to examine the immediate effects of occupational therapy using a sensory-integrative approach (Ayres Sensory IntegrationFootnote 1) on undesirable behaviors and engagement. Target behaviors were operationalized and coded. The target behaviors included: changes in individually defined undesirable behaviors that interfere with task engagement and participation in daily activities; and engagement defined as intentional, persistent, active, and focused interaction with the environment, people and objects. The study consisted of familiarization, baseline phase 1 and treatment phase 1, followed by baseline phase 2 and treatment phase 2. Baseline consisted of developmentally appropriate toys selected individually for each child. Intervention consisted of three, 40-min sessions of Ayres Sensory Integration per week followed by a 10-min table-top activity segment during which outcome data was collected. Data for each subject were plotted on a line graph and interpreted through visual inspection. In addition, data in a study log from researchers and weekly reports of the participant’s behavior in the home environment were reviewed. Visual inspection of the data for undesirable behaviors and engagement indicates considerable overlap in the number of intervals in which the behavior was observed in all phases; thus, Ayres Sensory Integration did not have a significantly different effect from the play scenarios on target behaviors. Data from study logs suggested that the intervention had a positive effect on transitions, socialization, compliance, and general behavior regulation, however, given the anecdotal nature of this data, the findings from this study cannot be interpreted to provide evidence for Ayres Sensory Integration. This study was promising in that participant characteristics were described in detail and dependent and independent variables were identified, however specific diagnostic information was missing and there was limited use of standardized test scores other than the Sensory Profile score that was used as an inclusion criterion. The information on the intervention was not provided except to mention that it followed the Ayres Sensory Integration approach. There was reliable measurement of fidelity. The comparable condition (a play scenario) was well described, the activity choices were individualized and presented in a random order, and the dependent variables were described in detail and also individually determined. There was good procedural reliability (above 99% for all phases). The social validity of this study was good in that dependent variable behaviors were identified based on parent interview and the data from study logs indicates an impact on daily life, however, the generality of the findings are limited by the design (single subject).
Ayres and Tickle (1980) study investigated whether the type of sensory processing disturbance predicted the response to sensory-integrative therapy. The subjects were ten children with autism aged between 3.5 and 13 years (mean age was 7.4). Subjects’ responses to sensory input were evaluated through the use of a test constructed by the researchers solely for this purpose. The test consisted of 14 specific sensory stimuli (e.g., response to light touch, response to pain, and response to sound of white noise) and rating was on a scale of 1–5 (no reaction to definite over-reaction). The test was administered by the investigator at least twice to enhance accuracy. Intervention was 1 year of occupational therapy using a sensory-integration approach “that focused on carefully providing somatosensory and vestibular sensory experiences and on eliciting an adaptive response to these stimuli” (Ayres and Tickle 1980, p. 378). Results were reported by individual subject changes on the test of responses to specific sensory stimuli and, in some cases, post-test scores on motor performance and vocabulary tests. A stepwise discriminant analysis was conducted to determine the parameters that best discriminated between subjects who were good responders to therapy versus those who were not. The good versus the poor responders had statistically significant (p < 0.05) differences on the presence of tactile defensiveness. There were no significant differences in the proposed direction for reactions to touch pressure, vibration, and movement. The best discriminators between the good and the poor responders were tactile defensiveness, reaction to movement, gravitational insecurity, and reaction to an air puff. Subjects who had normal or over-reactions to stimuli were better responders to therapy than non-responders. This study is interesting in that it is one of the first studies conducted to evaluate the effects of the sensory-integrative approach for children with autism and provides some preliminary data suggesting that children who are over responsive to stimuli will respond better than those who are under responsive. However, the study was weak in that it failed to adequately describe the participants’ characteristics and the independent variable (treatment) was not described. The dependent variables (measures) did not have reliability or validity, there was no comparison condition, and there was no calculation of power. The study has high social validity in that it is an area of high interest for clinicians and serves to provide preliminary guidelines for future studies in this area.
Conclusion
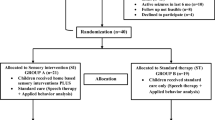
Although these studies provide promising evidence, it is not possible to draw strong practice implications because of small sample sizes, failure to adequately characterize the sample, lack of a detailed, replicable intervention protocol with a fidelity measure, and other methodological and design flaws. Future studies must address these issues and, fortunately, several efforts are underway to do so. For example, a Fidelity to Treatment Measure has been developed to evaluate whether intervention follows the sensory-integrative principles established in the literature (Parham et al. 2007). This fidelity scale evaluates constructs related to sensory-integration interventions, details the training of the people administering the intervention, and specifies the environment in which the treatment is conducted. It will ensure that future studies evaluating the sensory-integrative approach attain rigorous standards that include fidelity. A pilot version of this fidelity scale was used in the Watling and Dietz (2007) study. A manualized protocol has also been developed and is being tested for its utility and effectiveness for SD in ASD (Schaaf et al. in preparation). This manual is in keeping with the recommendations in the literature for intervention with the ASD population as outlined by Lord et al. (2005): it outlines key theoretical principles; it describes the objectives for each principle; it describes the clinical reasoning for each principle; and it is flexible in its application to allow for individualization of the treatment – an important aspect of interventions for ASD. An earlier version of the manual was used in a randomized pilot study for a non-ASD group (Miller et al. 2007; Miller et al. 2007). The findings show that, following a 10-week, 30-session intervention, children in the treatment group (n = 7) made gains that were significantly greater than the children in the other two groups (no treatment (n = 10) and active control (n = 7)) on Goal Attainment scales (p < 0.01). They also increased more than the other groups on attention, measured by Leiter-R (Roid and Miller 1997), with p = 0.03 compared to p = 0.07 for no treatment. Data showed trends in the predicted direction for the treatment group on sensory behaviors and the cognitive/social composite score on the Leiter-R. The treatment group showed a trend toward greater reduction in electrodermal activity (a measure of sensory responsivity) than the other groups.
Finally, to address the need for sensitive, meaningful outcome measures that are function-oriented and in keeping with the principles of the sensory-integrative approach, Goal Attainment Scaling (Kiresuk et al. 1994) has been adapted and applied for use with the sensory-integrative approach (Mailloux et al. 2007). Goal Attainment Scaling provides a means to monitor intervention goals that are specifically relevant to individuals and their families and thus holds promise as an effective, replicable outcome measure to evaluate the efficacy of the sensory-integrative approach for individuals with autism. The Goal Attainment scale provides a mechanism for assuring that outcomes have high social validity.
Evidence for Specific Sensory Techniques
A number of studies examine the effects of specific sensory strategies on reducing self-stimulating behaviors, improving attention and engagement in tasks, and decreasing sensory aversions for individuals with ASD. To reiterate, these interventions should be distinguished from the sensory-integrative approach in that they utilize stimulation of one specific sensory system rather than the holistic, integrated approach that is consistent with sensory integration. Broadly, these studies can be grouped into four categories: interventions that utilize touch (i.e., massage or touch therapy); interventions that utilize weighted vests; auditory interventions; and other interventions (the Wilbarger Protocol, therapy balls, and sensory diet). Again, the majority of the studies utilized case study, SSED, or group design protocols and are limited by small sample sizes and other methodological flaws. Thus, it is difficult to draw practice implications.
Touch-Based Treatments
The four studies summarized in Table 9.3 utilize massage, touch therapy, or deep pressure stimulation.
Escalona et al. (2001) examined whether nightly massage improved the sleeping habits and behaviors of children with autism. Twenty subjects with autism between the ages of 3 and 6 years of age were randomly assigned to either a control group or a massage therapy group. Parents were trained in the massage therapy and provided it every night for 15 min prior to bedtime for 1 month. Control subjects were read a story for 15 min by parents. Outcome measures were the Revised Conners Scales (Conners 1997) and observation of classroom behaviors (pre- and post-intervention). Parents also kept sleep diaries. The treatment group showed improvements on the Conners Scale (p < 0.05) and in observation measures of play behaviors including a greater decrease in stereotypical behaviors (t = 2.01, p < 0.05) and a greater increase in on-task behavior (t = 2.13, p < 0.05), and better sleeping patterns as evidenced by more time spent in deep sleep and less night wakening. The latter results do not report statistical significance.
Field et al. (1997) examined the effects of touch therapy on inattention, touch aversion, and withdrawal in 22 children with autism who had an average age of 4.5 years. Subjects were randomly assigned to either touch therapy or control. Touch therapy consisted of 15 min of touch in the form of moderate pressure and smooth strokes along the entire body. Children were assessed on the first and last day of intervention using the Autism Behavior Checklist (Krug et al. 1993) and the Early Social Communication Scales (Seibert et al. 1982). Touch aversion, off-task behavior, and orientating to irrelevant stimuli decreased in both groups although significantly ( p < 0.05) more in the treatment group. Only children in the touch-therapy group showed decreased scores on the sensory scale and the Autism Behavior Checklist. Children in the treatment group also showed significant (p < 0.05) changes on the Early Social Communication Scales in the area of joint attention (p < 0.05), behavioral regulation (p < 0.01), social behavior (p < 0.05), and initiating behavior (p < 0.01).
Silva et al. (2009) completed a multi-site, randomized control trial of massage, using a specific type of massage, Qigong Massage. They conducted a randomized controlled study of 46 children diagnosed with ASD and measured the effects of the treatment (Qigong massage) on adaptive behavior, sensory symptoms, digestion and sleep (all evaluated by parent and teacher report). Teacher report (blinded) showed that treated children had significant improvements in the language and social skills domains of the Vineland (p < 0.01) and reduction in autistic behaviors (p < 0.03) compared to controls. Parent data confirmed the findings and showed stability of results at 10 months. This study is strong methodologically as subjects were randomly assigned, interventionists were trained, and data were collected pre-treatment, post-treatment, and at 5 months following intervention; it thus provides emerging evidence for the use of Qigong Massage on the stated outcomes.
Edelson et al. (1999) reported a study of the effects of deep pressure on arousal and anxiety. The study used the Grandin hug machine (Grandin 1992), a device that allows for self-administration of lateral body pressure. Twelve subjects (nine males and three females ranging from 4 to 13 years of age) with a physician diagnosis of autism participated but there was no detail of the methods used for diagnosis. Five subjects were in the experimental condition and subjects were matched on age and gender. Prior to administration of treatment, both groups showed statistically similar levels of arousal and anxiety. Outcome measures were galvanic skin response (GSR) measured before and immediately after each session, the Conners’ parent rating scale (Goyette et al. 1978), and a side effects questionnaire to measure any side effects of the deep pressure. Data from the Conners’ scale was assessed using a 2 × 3 (group × time) MANOVA (pre-, mid-, and post-session time points) and showed that the tension and anxiety decreased in the experimental group (p < 0.05 and p < 0.10 respectively). Results of GSR are difficult to evaluate as they rely on demonstrating that physiological and behavioral measures converged prior to treatment and remain highly correlated with each other throughout the study. Further, in evaluating changes in GSR between the groups, there were non-significant differences but the authors did note that variability in GSR increased in the treatment group and decreased in the control group. They felt that this observation suggested that individuals within the treatment group responded differently to the intervention and thus, divided them into responders or non-responders based on their initial levels of anxiety or arousal. They found a marginally significant difference between those who benefited and those who did not – those who benefited were more likely to have higher GSR – but the sample sizes for this analysis are very small. They suggest that greater arousal may predict greater efficacy of deep pressure. This study is weak in that many of the study characteristics were not described (participant characteristics, inter-rater reliability) and random assignment was not detailed. The study did identify the independent and dependent variables, describe the comparison condition, and statistical tests, but findings were weak and liberties were taken in the interpretation of the findings.
Collectively, the studies using touch as the intervention show encouraging evidence in that improvements in target behaviors are noted. In general, the studies describe an intervention that can be replicated, describe the subject characteristics in detail, and utilize accepted statistical procedures in the data analysis and interpretation. Drawing strong conclusions from this data is limited, however, by the variability in intervention (touch pressure vs. massage) and the lack of an active control group or fidelity measure.
Interventions That Utilize Weighted Vests
Six studies, shown in Table 9.4, examined the effect of using weighted vests in children with ASD on attention, self-stimulatory behaviors, or on-task behaviors. One confounding factor in interpretation of these studies is that the weighted vest, although it provides mainly proprioception (the weight of the vest requires that increased muscle activity be utilized and thus increases the proprioceptive signals from the muscles, joints and tendons) may also provide some amount of pressure touch (due to the vest being placed on the torso) and thus, it is difficult to determine the nature of the stimuli that is being studied.
Fertel-Daly et al. (2001) examined the effects of weighted vests on five subjects with PDD (aged 2–4 years old) using an A–B–A withdrawal single subject study. Observations of focused attention to task, number of distractions, and duration and type of self-stimulatory behaviors during a 5-min fine motor activity were collected and plotted for visual analysis. Data for the intervention began in the third week of the study. The intervention consisted of wearing the weighted vest (four quarter-pound weights) three times per week for 2 weeks. Vests were worn for 2 h as soon as the child arrived at school and data were collected after 1.5 h of wearing the vest. Intervention was discontinued in the fifth week of the study and data were collected for two additional weeks. Results compared mean duration of focused attention, number of distractions, and duration of self-stimulatory behavior during each phase of the study. The authors concluded through visual analysis that all subjects’ data “supports the clinical observation that a weighted vest had a positive effect on at least two measures of attention for all five participants” (Fertel-Daly et al. 2001, page 638). An additional finding was that the increase in focused attention that occurred during the intervention was not sustained when the vest was removed and four participants had an abrupt drop in the duration of focused attention to task. The article concluded that a weighted vest “appeared to be beneficial... for five children with PDD who had difficulty attending to tasks and who exhibited self-stimulatory behaviors.”
Kane et al. (2004–05) conducted a single subject study with an A–B–C (no vest, vest with no weight, weighted vest) counterbalanced design with three subjects with autism and one participant with PDD using a vest specifically made for the study that was 5% of the child’s weight. The findings indicated no significant improvements in attention or decreases in stereotypic behaviors with the use of a weighted vest and the authors conclude that their study does not support the use of a weighted vest to decrease stereotypic behaviors or improve attention. The study design was single subject and thus the generality of these findings is limited. In addition, the study is flawed in that inter-observer agreement was not assessed. It is difficult to assess if findings are specifically related to the weight of the vest or to other qualities of the study (the vest was noted to be distracting to some subjects, activities provided to evaluate attention were not counterbalanced), nonetheless, this study is methodologically strong in its adherence and use of the single subject A–B–C design.
Reichow et al. (in press) completed a study of three subjects (aged 2–6 years), with an educational or medical diagnosis of autism or developmental delay, to determine if wearing a weighted vest increased engagement during a table-top activity. The vest was 5% of the child’s weight. This study was methodologically strong in that it utilized an alternating treatments design with three conditions (vest with weight, vest with no weight, and no vest), controlled for the vest-with-no-weight condition to ensure that there were no visually perceived differences between this and the weighted-vest conditions and thus the observers were blind to the study condition, and the conditions were randomly assigned based on a 5-day schedule (for example, one child might have 2 days with no vest, then 2 days with a vest and 1 day without the vest whereas another subject might have a different schedule). Videotape recordings of behavior during table-top activities were utilized and raters coded for engagement, non-engagement, stereotypic behaviors, and problem behaviors. Each behavior was defined. Interobserver agreement was excellent (0.93–0.96). Findings are reported by subject. For one subject there was an increase in problematic behaviors when wearing the vest and a decrease in stereotypic behaviors. There were no differences for the other two subjects in any of the observed behaviors among the three conditions. Findings do not provide any evidence of positive gain from the vest and suggested the possibility of negative outcomes (i.e., decreased engagement). This study provides emerging evidence that weighted vests are not effective for improving engagement during table-top activities. The quality of the study is high given the attention to methodological issues stated above, however, the ability to generalize is limited by the SSED methodology and would be strengthened by including a greater number of sessions. The observers were graduate students and it is not clear if they were blind to the opinions of the other members of the research team. The social validity of the study is high in that it is an area of high interest for teacher, clinicians, and families.
Cox et al. (2009) examined the effects of a weighted vest, a vest with no weights and no vest on in-seat behavior during a group activity on three elementary-age students with autism, intellectual disabilities, and sensory processing difficulties. This study was methodologically strong as it used an alternating treatments design to compare the effects of the three conditions – the three conditions are randomly and rapidly alternated and counterbalanced across participants to control for sequence effects – and then utilized a generalization condition to determine if effects would generalize to a different group activity. In-seat behavior was defined and evaluated by viewing videotapes of observed behaviors in 10-s intervals. Interobserver agreement on occurrence (94.7% average agreement) and nonoccurrence ratings of behaviors (88.2% average agreement) was good. The percentage of intervals for appropriate in-seat behavior was visually displayed for baseline and each condition and the percentage overlap between conditions was calculated by counting the number of data points in the second condition that fall within the range of the first condition and then multiplying by 100. High percentages of overlap were found and, thus, the authors concluded that the weighted vest did not have an effect on appropriate in-seat behavior for the participants. A second experiment was conducted to evaluate whether a behaviorally based intervention (noncontingent reinforcement, where subjects were given the choice of two highly preferred objects that they were allowed to access during the group activity) had an effect on in-seat behavior. Findings indicated that this strategy did improve in-seat behavior in the subjects. The authors concluded that, for these participants, the behavioral intervention had a stronger effect on in-seat behavior than the sensory intervention even though participants were identified as having sensory processing abnormalities.
This study is limited by the use of single subject methodology and thus the findings cannot be generalized. Another limitation is that the subjects were diagnosed with autism using different assessments and at different institutions. In addition, in-seat behavior was scored based on the subjects remaining in their seat for a full 10 s, which may limit the ability to detect changes that occur in smaller time increments. Finally, the study suggests that they were evaluating the effects of “sensory integration” whereas they are studying the effects of one sensory modality; they suggest that the study evaluates “deep pressure” on in-seat behavior, although it is difficult to determine if deep pressure (from the tightness of the vest) was provided at all or if the major sensory system stimulated was proprioception (as is generally the case with a weighted vest). This is important because it points to confusion about the use of sensory integration as opposed to sensory-based (single sensory system) strategies and the need to tailor treatment strategies to the individual needs of the child. For example, based on the information provided, it is impossible to evaluate whether the choice of the weighted vest was made based on the subjects scoring deficient in proprioceptive processing or some other criteria. Of note, only one subject scored in the “definite difference” range on tactile sensitivity and there is no information about proprioceptive processing. This issue speaks to the importance of individually tailoring sensory-based interventions to the child’s specific needs rather than utilizing a strategy for all subjects universally. Further, this issue speaks to the importance of a comprehensive assessment of the child’s ability to process and integrate sensory information that includes not only a measure of sensory modulation (as in the Short Sensory Profile) but a more comprehensive assessment of processing and integration of sensation and its effects on praxis and behavior.
Of the remaining two reports on weighted vests used with an ASD population, one article was a review of existing studies (Stephenson and Carter 2009) and another was a survey of therapists (members of the School-Based Special Interest Section or the Sensory Integration Special Interest Section of the American Occupational Therapy Association, AOTA) to determine their protocols and clinical reasoning for using weighted vests (Olson and Moulton 2004). These two reviews are shown in Table 9.4 but not elaborated on here.
Overall, the use of weighted vests to improve attention and self-stimulating behaviors is difficult to evaluate as few studies were found for children with ASD and they were conducted using SSED.
Auditory Interventions
Four studies, shown in Table 9.5, report on auditory interventions with children with ASD. Conclusions from this group of studies are difficult because they utilize different types of auditory intervention with varying levels of rigor, however, there is a trend that auditory interventions do not demonstrate any notable improvements in behaviors over either no treatment or a control condition of auditory input.
Mudford et al. (2000) reported a crossover experimental design study of 16 children with autism using an auditory integration training developed by Berard (1993). The intervention program involved playing modified music through headphones for 30-min sessions twice a day for 10 days whereas the control condition played music in the room but not through the training device or headphones. The study is promising in that participants were adequately described (ages 5.7–13.9 years with an average age of 9.42); the diagnosis of autism was confirmed based on the International Classification of Diseases and Related Health Problems, 10th edition (ICD-10; World Health Organization 1992) and DSM-IV (APA 1994) classifications; and measures of cognitive abilities and adaptive behavior were used. Dependent variables were the Aberrant Behavior Checklist (Aman et al. 1996) and direct observational recordings of behavior for an average of 3.82 h across the 14 months of the study. They reported seven statistically significant effects from 32 dependent variables, but none of the effects favored the auditory intervention. For example, they found that parent-rated behaviors on the Aberrant behavior checklist decreased more following the control condition compared to the auditory training intervention (Wilcoxon z = 1.91, p = 0.06, two-tailed) and that ear occlusion increased after the auditory intervention (p = 0.03). Overall IQ scores on the Leiter did not increase significantly (decreased from 68 to 66) and Vineland Adaptive Behavior Composite scores decreased but not significantly. The authors concluded that the control condition was more beneficial than the auditory integration training.
Corbett et al. (2008) reported a study designed to test the effects of the Tomatis Method on language skills. Eleven subjects with autism (based on DSM-IV criteria (APA 1994)), which was corroborated by the Autism Diagnostic Observation Schedule (ADOS; Lord et al. 2002) and clinical judgment. Subjects were aged 3.5–7.2 years; nine subjects were male and two were female. Outcomes were measured using the ADOS, the Stanford-Binet intelligence scale (Thorndike et al. 1986), the Peabody Picture Vocabulary Test (PPVT; Dunn and Dunn 1997), and the expressive one-word picture vocabulary test (Brownell 2000). They use a randomized, double-blind, placebo-controlled crossover design. Tomatis training was administered by trained assistants and researchers and parents were blind to condition. In keeping with the Tomatis Method, the combination of filtered music listened to through an “electronic ear” headphones and auditory feedback should result in enhanced auditory perception. However, no significant difference was found between treatment and control groups on the PPVT or the Expressive one-word picture vocabulary test and, thus, the authors concluded that their results do not provide evidence for the treatment.
Bettison (1996) reported a study of the long-term effects of auditory training on 80 children (66 males and 14 female), aged 3.9–17.1 years. All children had a primary diagnosis of autism, significant autism symptoms, or Asperger syndrome from an independent agency (no further information on autism diagnosis was provided). There were no differences between the groups on age, sex, or educational program attended. Auditory training followed the Berard (1993) method, which involved listening to filtered music on 16 CDs (up to 14 frequencies). The control group received structured listening to unmodified music under the same conditions as the treatment group (two half-hour sessions at least 4 h apart each day for 10 consecutive days). Measures included the Autism Behavior Checklist (ABC) (Krug et al. 1993), the Developmental behavior checklist (DBC), parent and teacher (Brereton et al. 2002), subtests from the PPVT (Dunn and Dunn 1981), and the Leiter international performance scale (Roid and Miller 1997). Sensory behaviors were assessed using the sensory problems checklist and the sound sensitivity questionnaire (SSQ; Rimland and Edelson 1994). Scores on each child’s audiogram were also assessed pre- and post-intervention. Inter-rater reliability was established for each measure and ranged from 0.90 to 0.99. T-tests to compare pre- and post-test scores were conducted at 1, 3, 6, and 12 months after intervention. Overall, there were marked improvements in the behavioral measures for both groups at 1 month, but there was a general lack of statistically significant differences between the groups. The authors suggested that the lack of difference between the groups suggests that, “some aspect of both conditions was operating to cause these changes” (Bettison 1996, p. 370). Of interest, the IQ scores as measured by the Leiter improved in both groups, however, the magnitude of improvement was greater for the intervention group. The authors felt that this may suggest an intervention effect on IQ score although they also noted that practice obtained during intervention cannot be ruled out as a factor influencing this finding. For example, for the ABC, statistically significant improvements were found at 1 month and these were maintained through 6 months but reverted to levels at 1 month when tested at 12 months. The main finding from this study is that both the auditory training and the structured listening may lead to reductions in auditory sensitivities but that further research is needed to confirm this finding. This study is strong in that it contains several primary quality indicators: participant characteristics are described, independent variable, intervention and comparison condition, and dependent variable are described, and the link between research question and data analysis is clear. The use of statistical tests is appropriate and several secondary quality indicators are present including random assignment and inter-rater agreement. The social validity is high in that the research addresses a question that is of high interest in the field.
Other Sensory Techniques
In this section, we consider three studies that each examined one specific other intervention (the Wilbarger Protocol, therapy balls, and sensory diet). They are summarized in Table 9.6.
Kimball et al. (2007) conducted a study to evaluate the Wilbarger protocol, which provides “very deep pressure input to the skin with a specially manufactured non-scratching brush followed by compression of the major joints” (Wilbarger and Wilbarger 2001, p. 406). They evaluated changes in salivary cortisol after 4 weeks of treatment. The protocol is designed to be administered every 1.5–2 h but it was administered only once per week in the morning so as to keep with the routine of the subjects. The study used a single subject A–B design with a convenience sample of four boys (aged 3–5 years) showing signs of sensory defensiveness as indicated by their primary occupational therapist. Sensory defensiveness was confirmed using the short sensory profile but no cut-off scores were mentioned. They also administered the Conners’ Rating Scale (Conners 1997) to examine correlates of behavioral issues pre- and post-intervention. Although all children’s salivary cortisol levels moved in the direction expected after application of the Wilbarger-based protocol, no statistical significance is reported. This study is very weak in that it lacked adequate subject descriptions, failed to report statistical significance, the protocol was not carried out in the way intended, the link between research question and data analysis was not clear and there was no mention of inter-rater agreement. The social validity is high in that the research addresses a question that is of high interest in the field.
Schilling and Schwartz (2004) conducted a study to evaluate the use of therapy balls used as a seating alternative for young children with ASD on engagement and in-seat behavior. Four male subjects (aged from 3 years 11 months to 4 years 2 months) participated in a withdrawal SSED. Each subject had a physician diagnosis of ASD but no further detail about the diagnostic criteria was mentioned. Each participant’s characteristics were described in detail and participants were selected for the study based on teacher reports of difficulty with engagement and in-seat behavior and the intervention was individualized based on each participant’s situation (e.g., participant 1 received intervention during art activities in his extended day program and, since the length of time for each art activity varied, the data collection varied from 5 to 10 min). Data on dependent variables (sitting and engagement) were collected via real time sampling and interobserver agreement ranged from 82% to 100%. Intervention (use of therapy ball for classroom sitting during an individually chosen activity) was implemented for a minimum of 2 weeks. Three of the four participants showed immediate and substantial improvements for in-seat behavior with the implementation of therapy balls. These three individuals also showed a marked return to baseline levels upon withdrawal. This study is strong in that primary quality indicators such as independent variable, dependent variable, description of participants, and adherence to study design are evident as is the link between research question and data analysis. Social validity is directly addressed in the design of the study and data on social validity is collected via staff questionnaire.
Ingersoll et al. (2003) studied the effects of sensory feedback on immediate object imitation for children with ASD. Sensory feedback was achieved through the use of toys with flashing lights and sound. The subjects were 15 children (nine boys and six girls) with ASD and 14 typically developing children (five boys and nine girls). Subjects with ASD were previously diagnosed and confirmed by the study author. Participants ranged in age from 23 to 53 months and there were no differences between the groups on mental age. The experiment compared imitation using toys that had sensory feedback versus the same toy with no sensory feedback using the motor imitation scale (Stone et al. 1997). Analysis used mixed-model repeated measures ANOVA and although overall imitation performance did not differ significantly between the two groups, the imitation performance of the participants with autism was significantly higher with sensory toys than with non-sensory toys (p < 0.02). The imitation performance of typically developing participants did not differ between the two sets of toys and both groups played significantly more with the sensory toys during free play, indicating that the sensory toys were more reinforcing for both groups. Additional results demonstrated that typical children used significantly more social behaviors during imitation than children with autism, but they did not differ in object-oriented behaviors, replicating previous findings. It is argued that children with autism may be less motivated to imitate by social interaction, but may be motivated to imitate to receive a nonsocial reward (sensory feedback). Although inter-rater reliability was calculated (it ranged from 0.71 to 0.95) and the experimental conditions were clearly described, the diagnosis of autism was not confirmed, and the study did not report on a number of other primary and secondary quality indicators.
Conclusion
Overall, the data supporting the sensory-integrative approach is promising, whereas the data related to isolated sensory strategies is problematic. Several factors have limited the conduct of rigorously controlled studies of the sensory integration approach, including lack of a specific intervention protocol, the absence of a fidelity measure, and the paucity of meaningful outcome measures that are in keeping with the theoretical principles of the intervention and that describe changes at the levels of activity and participation as recommended by the World Health Organization (2001). These issues were discussed in the introductory section of this chapter, as were the efforts that are underway to fill these voids and lay the foundation for rigorous controlled studies. However, from the findings of the majority of studies that investigated the sensory-integrative approach, it is felt that there is emerging evidence to support the use of the sensory-integrative approach for individuals with ASD, in particular to impact sensory and motor outcomes and individual client-centered goals.
Overall, the studies of other sensory techniques, with the exception of Qigong Massage, do not establish the techniques as evidence-based and they should be regarded as still in the experimental stages. The strongest support comes from the group of studies using touch-based intervention; however, given that each study used different interventions, it is not possible to draw strong conclusions. Thus, touch-based interventions should also be used cautiously. In general, interventions that use isolated sensory techniques should be recommended cautiously and, when used, systematic data should be collected and analyzed frequently to assess utility. Given that many children with ASD are receiving treatment for their SD to help deal with behavioral issues and sensory sensitivities and parents and funding agencies are spending a great deal of money and time on these, the need for solid research has reached a critical level.
Notes
- 1.
Ayres Sensory Integration was trademarked in an effort to clarify the concepts that reflect Ayres’s sensory integration framework and to distinguish it from other sensory approaches that do not use Ayres work in the way it was intended (Smith Roley and Mailloux 2007)
Abbreviations
- ADOS:
-
Autism Diagnostic Observation Schedule
- ANOVA:
-
Analysis of variance
- ASDs:
-
Autism spectrum disorders
- DBC:
-
Developmental behavior checklist
- DSM-IV-TR:
-
Diagnostic and Statistical Manual of Mental Disorders, 4th edition
- GSR:
-
Galvanic skin response
- ICD-10:
-
International Classification of Diseases and Related Health Problems, 10th edition
- MANOVA:
-
Multivariate analysis of variance
- PDD:
-
Pervasive developmental disorder
- PPVT:
-
Peabody picture vocabulary test
- SD:
-
Sensory dysfunction
- SSED:
-
Single subject experimental design
- SSQ:
-
Sound sensitivity questionnaire
References
Adrien, J. L., Ornitz, E., Barthelemy, C., Sauvage, D., & Lelord, G. (1987). The presence or absence of certain behaviors associated with infantile autism in severely retarded autistic and nonautistic retarded children and very young normal children. Journal of Autism and Developmental Disorders, 17(3), 407–416.
Aman, M. G., Tasse, M. J., Rojahn, J., & Hammer, D. (1996). The Nisonger CBRF: A child behavior rating form for children with developmental disabilities. Research in Developmental Disabilities, 17(1), 41–57.
APA. (1994). Diagnostic and statistical manual of mental disorders (4th ed. – text revision). Washington, DC: American Psychiatric Association.
APA. (2000). Diagnostic and statistical manual of mental disorders (4th ed. – text revision). Washington, DC: American Psychiatric Association.
Ayres, A. J. (1979). Sensory integration and the child. Los Angeles, CA: Western Psychological Services.
Ayres, A. J. (1989). The sensory integration and praxis tests. Los Angeles, CA: Western Psychological Services.
Ayres, A. J., & Tickle, L. S. (1980). Hyper-responsivity to touch and vestibular stimuli as a predictor of positive response to sensory integration procedures by autistic children. The American Journal of Occupational Therapy, 34(6), 375–381.
Baranek, G. T. (1999). Autism during infancy: A retrospective video analysis of sensory-motor and social behaviors at 9–12 months of age. Journal of Autism and Developmental Disorders, 29(3), 213–224.
Baranek, G. T. (2002). Efficacy of sensory and motor interventions for children with autism. Journal of Autism and Developmental Disorders, 32(5), 397–422.
Baranek, G. T., David, F. J., Poe, M. D., Stone, W. L., & Watson, L. R. (2006). Sensory experiences questionnaire: Discriminating sensory features in young children with autism, developmental delays, and typical development. Journal of Child Psychology and Psychiatry and Allied Disciplines, 47(6), 591–601.
Benevides, T., Schaaf, R., Toth-Cohen, S., Johnson, S. L., & Madrid, G. (2010) The everyday routines of families of children with autism: Examining the impact of sensory processing difficulties in children with autism on the family. Presented at 9th International Meeting for Autism Research, Philadelphia, PA, May 2010.
Berard, G. (1993). Hearing equals behaviour. New Canaan, CT: Keats Publishing.
Bettison, S. (1996). The long-term effects of auditory training on children with autism. Journal of Autism and Developmental Disorders, 26(3), 361–374.
Brereton, A. V., Tonge, B. J., Mackinnon, A. J., & Einfeld, S. L. (2002). Screening young people for autism with the developmental behavior checklist. Journal of the American Academy of Child and Adolescence Psychiatry, 41(11), 1369–1375.
Brownell, R. (2000). Expressive one-word picture vocabulary test. Novato, CA: Academic Therapy Publications.
Case-Smith, J., & Bryan, T. (1999). The effects of occupational therapy with sensory integration emphasis on preschool-age children with autism. The American Journal of Occupational Therapy: Official Publication of the American Occupational Therapy Association, 53(5), 489–497.
Conners, K. (1997). Conners’ rating scales – revised. North Tonawanda, NY: Multi-Health Systems.
Cook, D. G. (1991). The assessment process. In W. Dunn (Ed.), Pediatric occupational therapy: Facilitating effective service provision (pp. 35–72). Thorofare, NJ: Slack.
Corbett, B. A., Shickman, K., & Ferrer, E. (2008). Brief report: The effects of Tomatis sound therapy on language in children with autism. Journal of Autism and Developmental Disorders, 38(3), 562–566.
Cox, A. L., Gast, D. L., Luscre, D., & Ayres, K. M. (2009). The effects of weighted vests on appropriate in-seat behaviors of elementary-age students with autism and severe to profound intellectual disabilities. Focus on Autism and Other Developmental Disabilities, 24(1), 17–26.
Dawson, G., & Watling, R. (2000). Interventions to facilitate auditory, visual, and motor integration in autism: A review of the evidence. Journal of Autism and Developmental Disorders, 30(5), 415–421.
Dunn, L. M., & Dunn, L. M. (1981). The peabody picture vocabulary test (2nd ed.). Bloomington, MN: Pearson Assessments.
Dunn, L. M., & Dunn, L. M. (1997). The peabody picture vocabulary test (3rd ed.). Bloomington, MN: Pearson Assessments.
Edelson, S. M., Edelson, M. G., Kerr, D. C., & Grandin, T. (1999). Behavioral and physiological effects of deep pressure on children with autism: A pilot study evaluating the efficacy of Grandin’s hug machine. The American Journal of Occupational Therapy, 53(2), 145–152.
Escalona, A., Field, T., Singer-Strunck, R., Cullen, C., & Hartshorn, K. (2001). Brief report: Improvements in the behavior of children with autism following massage therapy. Journal of Autism and Developmental Disorders, 31(5), 513–516.
Fazlioglu, Y., & Baran, G. (2008). A sensory integration therapy program on sensory problems for children with autism. Perceptual and Motor Skills, 106(2), 415–422.
Fertel-Daly, D., Bedell, G., & Hinojosa, J. (2001). Effects of a weighted vest on attention to task and self-stimulatory behaviors in preschoolers with pervasive developmental disorders. The American Journal of Occupational Therapy, 55(6), 629–640.
Field, T., Lasko, D., Mundy, P., Henteleff, T., Kabat, S., et al. (1997). Brief report: Autistic children’s attentiveness and responsivity improve after touch therapy. Journal of Autism and Developmental Disorders, 27(3), 333–338.
Goyette, C. H., Conners, C. K., & Ulrich, R. F. (1978). Normative data on revised Conners parent and teacher rating scales. Journal of Abnormal Child Psychology, 6(2), 221–236.
Grandin, T. (1992). Calming effects of deep touch pressure in patients with autistic disorder, college students, and animals. Journal of Child and Adolescent Psychopharmacology, 2(1), 63–72.
Grandin, T. (1995). Thinking in pictures: And other reports from my life with autism. New York: Random House.
Green, V. A., Pituch, K. A., Itchon, J., Choi, A., O’Reilly, M., & Sigafoos, J. (2006). Internet survey of treatments used by parents of children with autism. Research in Developmental Disabilities, 27(1), 70–84.
Huebner, R. (2001). Autism: A sensorimotor approach to management. Gaithersburg, MD: Aspen.
Ingersoll, B., Schreibman, L., & Tran, Q. H. (2003). Effect of sensory feedback on immediate object imitation in children with autism. Journal of Autism and Developmental Disorders, 33(6), 673–683.
Kane, A., Luiselli, J. K., Dearborn, S., & Young, N. (2004–05). Wearing a weighted vest as intervention for children with autism/pervasive developmental disorder: Behavioral assessment of stereotypy and attention to task. The Scientific Review of Mental Health Practice, 3(2), 19–24.
Kientz, M. A., & Dunn, W. (1997). A comparison of the performance of children with and without autism on the sensory profile. The American Journal of Occupational Therapy, 51(7), 530–537.
Kimball, J. G., Lynch, K. M., Stewart, K. C., Williams, N. E., Thomas, M. A., & Atwood, K. D. (2007). Using salivary cortisol to measure the effects of a Wilbarger protocol-based procedure on sympathetic arousal: A pilot study. The American Journal of Occupational Therapy, 61(4), 406–413.
Kiresuk, T. J., Smith, A., & Cardillo, J. E. (1994). Goal attainment scaling: Applications, theory and measurement. Hillsdale, NJ: Lawrence Erlbaum.
Krug, D., Arick, J., & Almond, P. (1993). Autism screening instrument for educational planning. Austin, TX: Pro-ed.
Larson, E. (2006). Caregiving and autism: How does children’s propensity for routinization influence participation in family activities? Occupational Therapy Journal of Research: Occupation, Participation and Health, 26(2), 69–79.
Leekam, S. R., Nieto, C., Libby, S. J., Wing, L., & Gould, J. (2007). Describing the sensory abnormalities of children and adults with autism. Journal of Autism and Developmental Disorders, 37(5), 894–910.
Linderman, T. M., & Stewart, K. B. (1999). Sensory integrative-based occupational therapy and functional outcomes in young children with pervasive developmental disorders: A single subject study. The American Journal of Occupational Therapy, 53(2), 207–213.
Lord, C., Rutter, M., DilLavore, P. C., & Risi, S. (2002). Autism diagnostic observation schedule. Los Angeles, CA: Western Psychological Services.
Lord, C., Wagner, A., Rogers, S., Szatmari, P., Aman, M., et al. (2005). Challenges in evaluating psychosocial interventions for autistic spectrum disorders. Journal of Autism and Developmental Disorders, 35(6), 695–711.
Mailloux, Z. (2006). Setting goals and objectives around sensory integration concerns. In R. C. Schaaf & S. Smith Roley (Eds.), Sensory integration: Applying clinical reasoning to practice with diverse populations (pp. 63–70). Austin, TX: PsychCorp.
Mailloux, Z., May-Benson, T. A., Summers, C. A., Miller, L. J., Brett-Green, B., et al. (2007). Goal attainment scaling as a measure of meaningful outcomes for children with sensory integration disorders. The American Journal of Occupational Therapy, 61(2), 254–259.
Mandell, D. S., Novak, M. M., & Levey, S. (2005). Frequency and correlates of treatment use among a community sample of children with autism. Paper presented at the International Meeting for Autism Research, Boston, MA.
McClure, M. K., & Holtz-Yotz, M. (1991). The effects of sensory stimulatory treatment on an autistic child. The American Journal of Occupational Therapy, 45(12), 1138–1142.
Miller, L. J., Coll, J. R., & Schoen, S. A. (2007). A randomized controlled pilot study of the effectiveness of occupational therapy for children with sensory modulation disorder. The American Journal of Occupational Therapy, 61, 228–238.
Miller, L. J., Schoen, S. A., James, K., & Schaaf, R. C. (2007). Lessons learned: A pilot study on occupational therapy effectiveness for children with sensory modulation disorder. The American Journal of Occupational Therapy, 61(2), 161–169.
Mudford, O. C., Cross, B. A., Breen, S., Cullen, C., Reeves, D., et al. (2000). Auditory integration training for children with autism: No behavioral benefits detected. American Journal of Mental Retardation, 105(2), 118–129.
National Research Council. (2001). Educating young children with autism. Washington, DC: National Academy Press.
O’Neill, M., & Jones, R. S. (1997). Sensory-perceptual abnormalities in autism: A case for more research? Journal of Autism and Developmental Disorders, 27(3), 283–293.
O’Riordan, M., & Passetti, F. (2006). Discrimination in autism within different sensory modalities. Journal of Autism and Developmental Disorders, 36(5), 665–675.
Olson, L. J., & Moulton, H. J. (2004). Use of weighted vests in pediatric occupational therapy practice. Physical & Occupational Therapy in Pediatrics, 24(3), 45–60.
Ornitz, E. M. (1974). The modulation of sensory input and motor output in autistic children. Journal of Autism and Childhood Schizophrenia, 4(3), 197–215.
Ornitz, E. M. (1989). Autism: Nature, diagnosis, and treatment. New York: Guilford.
Parham, D., & Mailloux, Z. (1995). Sensory integrative principles in intervention with children with autistic disorder. In J. Case-Smith, A. S. Allen, & P. N. Pratt (Eds.), Occupational therapy for children (3rd ed., pp. 329–382). St. Louis, MO: Mosby.
Parham, L. D., Cohn, E. S., Spitzer, S., Koomar, J. A., Miller, L. J., et al. (2007). Fidelity in sensory integration intervention research. The American Journal of Occupational Therapy, 61(2), 216–227.
Parham, L. D., Smith Roley, S., May Benson, T., Koomar, J., et al. (in press) Development of a fidelity measure for research on effectiveness of Ayres Sensory Integration intervention. The American Journal of Occupational Therapy.
Rapin, I., & Katzman, R. (1998). Neurobiology of autism. Annals of Neurology, 43(1), 7–14.
Reichow, B., Barton, E. E., Neeley, J., Good, L., & Wolery, M. (in press). Effects of wearing a weighted vest on engagement in young children with developmental disabilities. Focus on Autism and Other Developmental Disabilities.
Reichow, B., Barton, E. E., Neeley, J., Good, L., & Wolery, M. (2010). Effects of wearing a weighted vest on engagement in young children with developmental disabilities. Focus on Autism and Other Developmental Disabilities, XX(X) 1–9. http://www.sagepub.com/journalsPermissions.navDOI: 10.1177/1088357609353751
Rimland, B., & Edelson, S. M. (1994). The effects of auditory integration training on autism. American Journal of Speech-Language Pathology, 3, 16–24.
Rogers, S. J., & Ozonoff, S. (2005). Annotation: What do we know about sensory dysfunction in autism? A critical review of the empirical evidence. Journal of Child Psychology and Psychiatry and Allied Disciplines, 46(12), 1255–1268.
Rogers, S. J., Hepburn, S., & Wehner, E. (2003). Parent reports of sensory symptoms in toddlers with autism and those with other developmental disorders. Journal of Autism and Developmental Disorders, 33(6), 631–642.
Roid, G. H., & Miller, L. J. (1997). Leiter international performance scale-revised. Wood Dale, IL: Stoelting.
Schaaf, R. C., & Miller, L. J. (2005). Occupational therapy using a sensory integrative approach for children with developmental disabilities. Mental Retardation and Developmental Disabilities Research Reviews, 11(2), 143–148.
Schaaf, R. C., & Nightlinger, K. M. (2007). Occupational therapy using a sensory integrative approach: A case study of effectiveness. The American Journal of Occupational Therapy, 61(2), 239–246.
Schaaf, R.C, Benevides, T., Johnson S., Madrid, G., Toth-Cohen, S. (2010). The everyday routines of families of children with autism: Examining the impact of sensory processing difficulties on the family. Presented at 9th International Meeting for Autism Research, Philadelphia, PA, May 2010.
Schaaf, R.C, Benevides, T., Johnson S., Madrid, G.; Toth-Cohen, S. (in press – accepted for publication). The everyday routines of families of children with autism: examining the impact of sensory processing difficulties on the family. Autism Research
Schaaf, R. C., Schoen, S. A., Smith Roley, S., Lane, S. J., Koomar, J. A., & May-Benson, T. A. (2010). A frame of reference for sensory integration. In P. Kramer & J. Hinojosa (Eds.), Frames of reference for pediatric occupational therapy (3rd ed.). Philadelphia, PA: Lippincott Williams & Wilkins.
Schaaf, R. C., Blanche, E. I., Mailloux, Z., Benevides, T., Burke, J. P., et al. (in preparation). The sensory integration intervention manual.
Schilling, D. L., & Schwartz, I. S. (2004). Alternative seating for young children with autism spectrum disorder: Effects on classroom behavior. Journal of Autism and Developmental Disorders, 34(4), 423–432.
Schwenk, H.A. & Schaaf, R.C. (2003). Assessments used by occupational therapists working with children with autism. Pennsylvania Occupational Therapy Association Annual Conference, Pittsburg, PA.
Seibert, A., Hogan, E., & Mundy, P. C. (1982). Assessing interactional competencies: The early social-communication scales. Infant Mental Health Journal, 3(4), 244–258.
Silva, L. M., Ayres, R., & Schalock, M. (2009). Outcomes of a pilot training program in a qigong massage intervention for young children with autism. The American Journal of Occupational Therapy, 62(5), 538–546.
Sinha, Y., Silove, N., Wheeler, D., & Williams, K. (2006). Auditory integration training and other sound therapies for autism spectrum disorders: A systematic review. Archives of Disease in Childhood, 91(12), 1018–1022.
Smith Roley, S., & Mailloux, Z. (2007). Understanding Ayres sensory integration. Occupational Therapy Practice, 12(17), CE1–CE7.
Smith, S. A., Press, B., Koenig, K. P., & Kinnealey, M. (2005). Effects of sensory integration intervention on self-stimulating and self-injurious behaviors. The American Journal of Occupational Therapy, 59(4), 418–425.
Stephenson, J., & Carter, M. (2009). The use of weighted vests with children with autism spectrum disorders and other disabilities. Journal of Autism and Developmental Disorders, 39(1), 105–114.
Stone, W. L., Ousley, O. Y., & Littleford, C. D. (1997). Motor imitation in young children with autism: What’s the object? Journal of Abnormal Child Psychology, 25(6), 475–485.
Thorndike, R. L., Hagen, E. P., & Sattler, J. M. (1986). Stanford-Binet intelligence scale (4th ed.). Itasca, IL: Riverside Publishing.
Tomchek, S. D., & Dunn, W. (2007). Sensory processing in children with and without autism: A comparative study using the short sensory profile. The American Journal of Occupational Therapy, 61(2), 190–200.
Watling, R. L., & Dietz, J. (2007). Immediate effect of Ayres’s sensory integration-based occupational therapy intervention on children with autism spectrum disorders. The American Journal of Occupational Therapy, 61(5), 574–583.
Wilbarger, P. L., & Wilbarger, J. L. (2001). Sensory defensiveness: A comprehensive treatment approach. Panorama City, CA: Avanti Educational Programs.
Williams, D. (1992). Nobody nowhere: The extraordinary autobiography of an autistic. New York: Crown.
Williams, D. (1994). Somebody somewhere: Breaking free from the world of autism. New York: Crown.
World Health Organization. (1992). International classification of diseases and related health problems (10th ed.). Geneva, Switzerland: WHO.
World Health Organization. (2001). International classification of functioning, disability and health. Geneva, Switzerland: WHO.
Acknowledgements
The author wishes to thank Amanda Pallotta for her assistance with the preparation of the manuscript.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2011 Springer Science+Business Media, LLC
About this chapter
Cite this chapter
Schaaf, R.C. (2011). Interventions That Address Sensory Dysfunction for Individuals with Autism Spectrum Disorders: Preliminary Evidence for the Superiority of Sensory Integration Compared to Other Sensory Approaches. In: Reichow, B., Doehring, P., Cicchetti, D., Volkmar, F. (eds) Evidence-Based Practices and Treatments for Children with Autism. Springer, Boston, MA. https://doi.org/10.1007/978-1-4419-6975-0_9
Download citation
DOI: https://doi.org/10.1007/978-1-4419-6975-0_9
Published:
Publisher Name: Springer, Boston, MA
Print ISBN: 978-1-4419-6973-6
Online ISBN: 978-1-4419-6975-0
eBook Packages: Behavioral ScienceBehavioral Science and Psychology (R0)