Abstract
Biomechanical weakening of the aorta leads to aneurysm formation and/or dissection and total biomechanical failure results in rupture, which is often fatal. The most common aneurysm is the abdominal aortic aneurysm (AAA) whereas thoracic aortic aneurysms (TAA) involve the ascending or descending segments of the aorta. Biomechanical strength of the aorta is maintained in part via balance between the integrity of the aortic medial and adventitial extracellular matrix and the health of the mural cells. From a biomechanical perspective, aneurysms rupture or dissect when wall stresses locally exceed the wall strength. Pathobiologic mechanisms, pre-disposing disorders and variability of patient demographic characteristics can weaken the aortic wall while increased blood pressure and dilatation increase the stress acting on it, leading to further aneurysm expansion. Thoracic and abdominal aortic aneurysms arise from very different pathophysiologies that ultimately result in a final common outcome of matrix degeneration and biomechanical failure. Therefore, the patient-specific knowledge of both wall stress and wall strength distributions for a given aneurysm will greatly improve the ability to identify those aortic aneurysms that are at highest risk of rupture. Towards this end, the biomechanics of AAA has been studied extensively by many groups whereas TAA biomechanics has not been fully considered. This chapter articulates the state-of-the-art of aortic biomechanics, including the modeling of tensile strength and wall stress distributions and the biological mechanisms which influence them. The potential clinical utility of these biomechanical estimates in predicting AAA rupture is also discussed.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Abdominal Aortic Aneurysm
- Aortic Dissection
- Connective Tissue Growth Factor
- Wall Stress
- Bicuspid Aortic Valve
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 Introduction
Aortic aneurysm is a consequence of biomechanical weakening of the vessel that leads to a local enlargement of the aorta over years but can rupture suddenly, often without warning. Thus, aortic rupture is a catastrophic failure of the vessel that is responsible for high mortality and morbidity. The most common aneurysm is the abdominal aortic aneurysm (AAA) whereas thoracic aortic aneurysms (TAA) involve the ascending or descending segments of the aorta. Dissection is another pathology in which the aortic wall dissects, thereby permitting the blood to enter the wall and causing enlargement. Biomechanical strength of the aorta is maintained in part via balance between the integrity of the aortic medial and adventitial extracellular matrix (ECM) and the health of the mural cells; namely, the medial smooth muscle cells and adventitial fibroblasts. This state of balance is known as tissue homeostasis and is essential for proper functioning of the aorta.
The diagnosis of an aortic aneurysm occurs principally via radiologic imaging of the aorta. Current clinical practice dictates that replacement of the aneurysmal aorta should be performed when the aneurysm size reaches 5.0–5.5 cm in maximum diameter for both TAAs [1] and AAAs [2–4]. However, rupture or dissection can occur at diameters <5.0 mm in 0–23% cases (Table 1) [5–9]. This wide discrepancy in rupture or dissection occurrence may be due to variability in the pathology of the aortic disease, which can be influenced by patient demographics, co-morbidities or pre-disposing conditions such as connective tissue disorders. Furthermore, studies reporting rates of rupture are limited by lack of information regarding the diagnosis criteria and post-mortem studies [7, 10] and are likely unreliable due to diameter measurement discrepancies [5]. Clearly, a patient-specific approach would be desirable for more reliable rupture or dissection risk predictions to improve clinical management, and tailoring a prognosis and treatment course unique to the patient.
From a biomechanical perspective, aneurysms rupture or dissect when wall stresses locally exceeds the wall strength. Pathobiologic mechanisms, pre-disposing disorders and variability of patient demographic characteristics tend to weaken the aneurysm wall [11–13] while increased blood pressure and aneurysmal enlargement increase the stress acting on it [14, 15], leading to further aneurysmal expansion. This cycle continues as the aneurysm enlarges eventually ruptures or dissects, unless repaired or the patient succumbs to other causes.
The earliest predictions of wall stress used the law of Laplace (Eq. 1) as the theoretical basis for using the “maximum diameter” as the criterion for predicting AAA rupture potential. This law states that wall tension (T) increases in proportion to an increase in the intraluminal pressure (P), an increase in diameter D(R) or a decrease in wall thickness (t).
The law of Laplace has two major fallacies for its application in biomechanics. First, the aorta is not a simple cylindrical or spherical shape of uniform radius of curvature for which the law of Laplace is valid. Rather, the geometry of the aortic wall is complex, containing a greater and lesser curvature, and these vary spatially [16, 17]. Therefore, the maximum diameter criterion to predict rupture risk ignores the important roles of vessel wall topography and geometry. This notion is supported by studies which demonstrated that stress on the wall is dependent on wall shape unique to each aneurysm [15, 16, 18]. Secondly, rupture predictions based on only the wall stress are not sufficient because a region of the aneurysmal wall that is under elevated wall stress may also have higher wall strength, thus equalizing its rupture potential. The wall strength will have spatial variance within a given aneurysm and also from patient-to-patient [19–21]. The rupture potential is highest in the location of peak ratio of wall stress to wall strength. However, risk analysis for rupture based upon the maximum diameter criterion is improved when a measurement of peak wall stress is also considered [22–24]. Ruptured AAAs demonstrated higher peak stress compared to diameter-matched electively repaired AAAs [12]. Clearly, the ability to noninvasively predict the locally acting wall stress and wall strength of an aortic aneurysm on a patient-specific basis will provide a more accurate diagnostic tool for evaluating the high risk of failure of an aortic aneurysm. Preliminary efforts toward this end have been reported [18, 25–28].
Although the in vivo wall strength distribution of an aneurysm can only be estimated [29], biomechanical experimental testing has been performed to assess ex vivo the biomechanical behavior of the aneurysmal and non-aneurysmal human aorta. Several studies have found that aneurysmal tissue is substantially weaker and stiffer than normal aorta [11, 12, 26, 29–31]. The aorta displays anisotropic biomechanical strength that is spatially dependent in both ascending [32–34] and abdominal [20, 31] segments. For both aneurysmal and non-aneurysmal aorta, the longitudinal segments were stiffer than segments measured in the circumferential orientation (Fig. 1) [32, 33]. Perhaps the most important piece of biomechanical data is the finding that tensile strength does not appear to be related to aneurysm diameter [33]. Hence, aortic diameter is not the only determinant of either wall strength or wall stress [15], and rupture risk prediction criteria that account solely for aortic diameters do not offer a complete picture of the true risk for aortic failure. Other criteria have been proposed for rupture prediction models such as rate of aneurysm growth [3, 35, 36], stiffness [37] intraluminal thrombus (ILT) thickness in AAA [38], wall tension [8] and peak AAA wall stress [22–24]. However, all these were empirical approaches and have their limitations and could potentially lead to sometimes fatal errors in the decision pertaining to clinical management of AAA and TAA. Using a concept of the Rupture Potential Index (RPI) proposed and preliminarily applied by Vorp et al. [26–28] demonstrated for AAA that this new index may hold promise for a patient-specific diagnostic assessment. The RPI, which is the ratio of acting wall stress to the wall strength at a particular point on the aneurysm wall, was found to be higher in AAA that ruptured compared to those that did not rupture. Currently, there is only one model to assess the RPI of AAAs that has been used recently [28, 39]. Indeed, significant differentiation of rupture risk by RPI was found for aneurysm diameter ranging between 55 and 75 mm of asymptomatic and symptomatic/ruptured AAAs where the maximum diameter criterion failed to adequately predict risk [28].
Tensile strength of human thoracic aortic aneurysms (black bars) in the longitudinal (LONG) and circumferential (CIRC) orientations and non-aneurysmal controls (white bars). Bars present mean ±SEM. (Adapted from Fig. 2 of Vorp et al. [33])
Thoracic and abdominal aortic aneurysms are thought to arise from different, very distinct pathophysiologies. However, both pathologies culminate to a final common pathway of matrix degeneration and biomechanical failure. Aneurysms of the thoracic aorta are generally non-inflammatory in nature and are related to connective tissue disorders such as Marfan, Ehlers-Danlos or Loeys-Dietz syndrome, the presence of a congenital defect such as the bicuspid aortic valve (BAV) or other familial aortic disease. TAAs and dissections can also arise from non-genetic pathologies including Takayasu’s arteritis [40], giant cell arteritis [41], or tuberculous mycotic infection [42] and these conditions involve an inflammatory component. Aneurysms arising from these causes are less common than those of a genetic basis.
Matrix metalloproteinases (MMPs) are over-expressed in aortic aneurysms [43–46] specifically in TAAs [47–50] MMPs control degradation of elastin and collagen [51] and rupture or dissection occurs when the physiologic forces exerted on the vessel wall exceed its strength. Although AAAs exhibit marked inflammatory changes and associated atherosclerosis [52–59] there is a lack of evidence of an inflammatory component in TAAs [60–62]. This non-inflammatory phenomena is uniformly consistent with aortopathies of the ascending aorta, of which, key effector proteins inciting the phenotype have been identified for the Marfan (fibrillin-1) [63], Loeys-Dietz (TGF-βR) [64], and Ehlers-Danlos-vascular type (Type III collagen) [65] syndromes and familial forms of TAAs, including mutations in genes that regulate SMC contractility (α-smooth muscle actin (SMA) (ACTA2) and smooth muscle myosin heavy chain (SM-MHC) [66, 67]). The presence of a BAV also predisposes the patient to development of TAA and/or dissection in addition to aortic stenosis or insufficiency. [44, 45, 68–72]. The incidence of BAV overlaps with α-SMA and TGF-βR mutations at a frequency of 2.5–3% [73] but no gene or pathway responsible for inciting TAAs in BAV patients has been identified.
Common histopathological evidence for many incidences of TAAs include non-inflammatory smooth muscle cell loss, fragmentation of the elastin fibers, mucoid degeneration, and accumulation of proteoglycans within areas of cell depletion. These phenomena are collectively termed “cystic medial degeneration” or CMD and are observed within the medial layer of the aortic wall [45, 48, 60–62, 74, 75]. Development of AAAs often includes a contribution from inflammatory cells as increased MMP production by macrophages and occurrence of ILT which are generally absent in TAAs. The differing pathobiologies involved in aneurysm formation in the thoracic and abdominal aortas likely results in variations in the mechanical stresses and wall weakening associated with each type of aneurysm with patient-to-patient nuances. Hence, the clinical recommendation for patient management will depend upon understanding, with patient specificity, the role of biomechanics in diagnosis, counseling, monitoring and treating patients at risk for and presenting with, aortic aneurysm and determining their relative risk for rupture.
This chapter will detail the relative biological mechanisms that contribute to aneurysm formation in both the thoracic aorta and abdominal aorta and their role in vessel wall biomechanics, which ultimately leads to aneurysm formation and potential rupture of the aorta through weakened strength and increased stress.
2 Biological Mechanisms that Impact Mechanical Properties of the Aneurysmal Thoracic Aorta
2.1 Marfan Syndrome
Marfan syndrome (MFS) is a hereditary connective tissue disorder that is autosomal dominant and manifests in several organs including those of the cardiovascular, ocular and skeletal systems. Patients with MFS display a definitive body habitus, namely a tall stature and wing span that exceeds the height, arachnodactyle, craniofacial defects, pectus excavatum or carinatum. Ectopia lentis may occur in up to 80% of patients, usually bilaterally. MFS has widespread clinical presentation but the most dangerous and often lethal manifestation of the disorder is acute aortic dissection.
Aortic dissection often occurs after a period of progressive aortic dilation and involves weakening of the vessel wall. In MFS, this weakening results at least in part due to degeneration of the minute architecture of the extracellular matrix (ECM). In 1991, mutations in the fibrillin-1 (fbn1) were identified as the cause of MFS [63]. Fibrillins are ECM proteins that comprise microfibrils, which are the key connectors between elastin and collagen to local cells in the microenvironment. These microfibrils are essential for not only the microarchitecture of the tissue, but also provide substantial biomechanical support. Similar to fibrillins, a related protein family, the latent TGF-β-binding proteins (LTBPs) participate in both structure of the matrix and also function as a signaling molecules to direct cell behavior. LTBPs directly interact with TGF-β to sequester the growth factor within the tissue microenvironment and thus regulate the bioavailability. When bound to LTBPS, TGF-β isoforms cannot interact with their receptors and therefore, signaling activity is attenuated. LTBPs retain TGFs within the matrix, keeping them at the ready to be released in their active state and capable of receptor binding. Fibrillins are similar in structure to LTBPs. Both are cysteine-rich with multiple epidermal growth factor (EGF)-like domains that bind calcium [76]. An 8-cysteine module, which is distinct only to fibrillins and LTBPs may be critical for microfibril assembly [77] and also be responsible for interactions with TGF-β [78–79].
Fibrillins interact with TGF-βs as the microfibrils of the ECM. These microfibrils self-assemble and interact with integrins on the cell surface and other matrix molecules within the microenvironment. Fibrillins can be viewed as a physical tether between local cells and their matrix and contain the known integrin-interacting sequence RGD to support cell adhesion [80–82]. The amino acid sequence RGD serves as code for cell adhesion to matrix molecules and provides a means for direct cell–matrix interactions. Such interactions are essential for integrity of the matrix and the biomechanical strength of the tissue. In the case of the aorta, the elastic laminae are connected to the endothelial cells on the intimal side and the SMCs of the medial layer. Fibrillin-based microfibrils provide this connectivity between matrix and cells which contributes to stability of the tissue. Mice lacking these connections displayed increased elastin degradation and alterations in SMC phenotype in an apparent attempted repair mechanism to sustain loss of matrix. These defenses also include an increase in the MMPs that are induced as part of the remodeling process, but unfortunately mediate further degeneration of the matrix and contribute to weakening of the vessel. When cells are no longer physically linked to their matrix, they cannot sense the ongoing needs of the matrix for homeostasis. Cell–matrix interactions are a constant dynamic dialogue and exchange of information. Loss of cell–matrix connections is itself a signal to rebuild because the cell senses a matrix deficit. However, loss of cell-ECM connections is also a trigger for apoptosis which is a self-initiated program of induced cell death. SMC apoptosis is a characteristic of aortic diseases and vessel weakening and in the case of MFS, may stem from improperly formed fibrillin-based microfibrils.
The fibrillin microfibrils elicit their structural contribution to matrix homeostasis by providing a template for tropoelastin deposition. The microfibril network provides elasticity in elastin-based and non-elastin tissues. Normal organization of the microfibrils involves self-assembly of the fibrillin in moderately tight bundles of fibers that are oriented parallel to each other. The strength of the microfibrils is spatially dictated and controlled not only by the cells within the tissue, but also the forces upon which the tissue is subjected to. For this reason, microfibrils are often found within tissues that need to withstand considerable mechanical stress such as bone, and blood vessel, serving as anchors for various connective tissues (Fig. 2) [83]. In the MFS patient, mutations in fibrillin result in reductions in synthesis and deposition of fibrillin within the ECM and improper assembly of the microfibril bundles. These defects in fibrillin expression and organization are likely to impact the dual function of fibrillin as a regulator of TGF-β signaling and a biomechanical support for the aorta.
Fibrillin microfibrils in (a) lobster aorta and mouse aorta (b, c). Mf=microfibrillar mantle; El=elastin; Co=collagen fibrils. Scale bar is 400 μm. (Reproduced from Fig. 1, Kielty et al. [83])
There are over 600 mutations of the Fbn1 gene. The majority of the mutations are point mutations, with some being nonsense or missense mutations. Substitutions of cysteine residues that alter the disulfide bonds within the EGF or 8-Cys modules are the most frequent mutations, while other common mutations involve the calcium binding region. These alterations affect the organization of the fibrillin into microfibril bundles and substantially impact their ability to bind TGF-β, interact with the cell surface and orient properly to guide elastin deposition in the matrix. These shortcomings will ultimately contribute to reduced and possible failure of vessel biomechanical strength and result in a lethal rupture of the ascending aorta in MFS patients. A mouse model of MFS, the Fbn1 knockout support the theory that fibrillin-rich microfibrils significantly contribute to the overall biomechanical strength of the aorta. Fbn1-/- mice die within one year of birth due to aortic dissection and rupture. Although elastin fibers appear normal at birth, aneurysm initiates within 2 weeks of birth and continues to enlarge with time [84]. There is elastin degradation and disorganization along with considerable loss of fibrillin-1 [85]. SMCs adopt a synthetic phenotype in attempt to repair the insufficient ECM. These phenomena progress to elastin breakdown initiating from the adventitia and moving inward to the media. Aortic dilatation, aneurysm, dissection and rupture then coalesce. Microfibrils work together with elastin to provide biomechanical support to the aorta [86]. Fibrillin deficiency is related to increased aortic stiffness and decreased compliance, possibly due to a compensatory role for collagen to endure the bulk of load bearing in the absence of adequate fibrillin and elastin. Fibrillin works together with elastin to regulate the pressure-diameter relationship of the aortic wall. The biomechanical function of fibrillin-1 microfibrils is dependent upon its proper expression, assembly and incorporation. Details of the molecular assembly of fibrillin 1 into complex microfibrils are not completely understood. However, recombinant approaches have allowed the investigation of various domains on fibrillin molecular assembly into the higher-order microfibrils. Inter-molecular cross-linking is known to be driven by tissue transglutaminase to form dimers with disulfide bonds and furin processing appears to accelerate but is not essential for this event. However, it remains to be seen if these biochemical manipulations occur in vivo to maintain aortic biomechanics. The vital role of fibrillin-1 in aortic homeostasis targets this protein as a focus of extensive research for eventual therapeutic intervention for the care of MFS patients.
Mutations in fibrillin that impair its TGF-β-binding role lead to increases in free TGF-β and excessive signaling of this pathway. This led investigators to hypothesize that TGF-β played a role in aortic dilation in MFS patients. TGF-β neutralizing antibodies prevent elastin breakdown in fbn-/- mice but such a therapy lacks clinical feasibility. Losartan, an angiotensin (Ang) II inhibitor also antagonizes TGF-β signaling. As a currently FDA-approved drug, losartan is widely successful medication used to treat hypertension. While blood pressure control is commonly sought in patients with MFS and aortic aneurysm, a means to attenuate or reverse matrix damage in the vessel wall and maintenance of biomechanical stability of the aorta to prevent rupture is necessary. Treatment of fbn-/- mice with losartan effectively prevented matrix degradation in the ascending aorta and mice were phenotypically and histologically indistinguishable from wild-type mice [85]. This treatment was also effective in preventing aortic root dilatation in children [87]. Losartan may prevent dilation through two mechanisms: (1) decrease in the absolute blood pressure or rate of change in blood pressure reduces the effect of hemodynamics on the already compromised aortic wall due to fibrillin mutations and/or (2) inhibition of TGF-β signaling through regulation of the Ang II type I receptor (AT1). How TGF-β signaling regulates matrix homeostasis remains unclear but may be due to altered SMC phenotype and synthesis of new matrix proteins in effort to remodel a matrix damaged by degradation. Furthermore, since TGF-βs are important for growth and development, it will be important to include tissue targeting strategies in any therapeutic drug design in order to limit the potential deleterious side effects of TGF-β on normal development and renal function [87, 88].
MFS patients present clinically with manifestations of this connective tissue disorder in several organ systems. A multitude of mutations in fibrillin have been identified that may contribute to the diseases. However, fundamentally, the microfibrils of the ECM are composed of fibrillin and when improperly synthesized, assembled or maintained, alterations in biomechanical stability and growth factor signaling through TGF-β are significantly altered. These mechanisms contribute to degradation of the ECM through elastolysis and SMC loss and culminate in reduced biomechanical strength, progressive weakening of the vessel wall, aortic aneurysm, dissection and the highly-fatal rupture. However, to our knowledge, no ex vivo mechanical testing has been conducted on the ascending aorta of the MFS patient population. There have been some reports that used noninvasive ultrasonography to demonstrate that MFS patients have increased stiffness of the infrarenal aorta and decreased strain, despite normal aortic diameters [89]. Ex vivo mechanical testing has been limited to mouse models of MFS. Increased stiffness was reported in carotid arteries and aortae of fbn1-/- mice and elastin and fibrillin were shown to provide the primary biomechanical strength of the tissue [86, 90]. Efforts to further understand the role of these biological mechanisms on the individual efforts of each matrix molecule on the overall biomechanical strength of the vessel itself should be pursued in depth in order to develop better treatments for patients with MFS.
2.2 Loeys-Dietz Syndrome
Loeys-Dietz syndrome (LDS) is an autosomal dominant disorder linked to mutations in the TGF-β receptors (TGFBR1 and TGFBR2) [64]. In addition to a pre-disposition for TAA, LDS patients exhibit other manifestations of this connective tissue disorder such as craniosynostosis, bifid uvula, cleft palate and transluscent skin [91]. The histopathologic observations of the aorta in LDS patients are consistent with those of other TAAs including CMD, increased collagen deposition, elastin fragmentation and lack of an inflammatory response [92]. Interestingly, the mutations in TGFBRs result in excessive TGF-β signaling rather than inhibited signaling. This leads to effects similar to those observed for MFS and underscores the importance of TGF-βs in regulating vascular tissue homeostasis. In LDS patients, contrary to expectation, increased collagen deposition was observed, accompanied by elevated connective tissue growth factor (CTGF) expression and nuclear Smad2 localization [64, 91] which are all clear indicators of enhanced TGF-β signaling. CTGF is directly regulated by TGF-β via the Smad2 pathway and promotes proliferation and ECM production by fibroblasts and SMCs. The up-regulation of CTGF could propagate excessive TGF-β signaling via attenuation of the inhibitory Smad7, a key component of the TGF-β feedback loop [93]. CTGF has also been shown to regulate TGF-β responses and inhibition of CTGF can reduce TGF-β-induced collagen synthesis, while elevated levels of CTGF directly contribute to ECM accumulation (Fig. 3) [94]. As tissue homeostasis relies on a balance between organized matrix deposition and matrix degradation, TGF-β also elicits control over the remodeling process by activating inhibitors of tissue proteases such as plasminogen activator inhibitor-1 (PAI-1) and tissue inhibitors of the MMPs (TIMPs). These observations are counter-intuitive since aneurysm development is well known to include over-production of the ECM degenerative MMPs and calls into question the relative role of MMPs as instigators of aneurysm formation. Perhaps the causal agents lie upstream in the signaling cascade and initiate a faulty remodeling process which results in an improperly formed ECM, lacking sufficient biomechanical integrity. MMPs are essential for normal remodeling, evidenced in other tissues such as the skeletal system where ECM fragments are stimulators of new, organized matrix deposition. These apparently synergistic effects of TGF-β and CTGF create a fibrosis-like state of the aortic ECM in LDS patients, where biomechanical integrity is compromised. It has been well-established that both TGF-β and CTGF are potent fibrotic agents in many tissues; however the challenge that remains is devising an intervention at the molecular level to prevent these signaling events that cause impaired collagen deposition. CTGF, as a down-stream modulator of TGF-β-mediated fibrosis is an attractive target for therapeutic intervention to prevent collagen accumulation and matrix disorganization.
Pathways of vascular fibrosis involving Ang II and TGF-β. (Figure 3 from Ruiz-Ortega et al. [94])
Fibrosis occurs as a result of tissue defense to an assault or injury and represents a poorly repaired tissue, lacking adequate biomechanical properties. Often there is excessive insoluble collagen with improperly formed cross-links or poorly organized into fibrils. More collagen does not translate to increased strength. However, unlike fibrosis, this accumulated collagen in TAA patients occurs in the absence of an inflammatory response. Contrary to MFS, there have been no studies measuring the biomechanical strength of the aorta in LDS patients. However, given the disruption of the TGF-β signaling cascade, it is reasonable to hypothesize, that dis-regulation of collagen synthesis and factors that regulate matrix remodeling such as MMPs and inhibitors of tissue proteases will significantly impact the biomechanical integrity of the matrix and the vessel wall as a whole. The direct contributions of each pathway or mechanism on the biomechanical strength will likely be determined through a combination of animal models and targeted interrogation of particular molecules in the signaling cascade, complemented by analysis of the biomechanical properties of the aneurysmal aorta. Within any given tissue niche, the cell senses the needs of the matrix and responds in kind to remodel, repair, or regenerate and disruptions upstream can have devastating effects that contribute to the pathogenesis of the connective tissues. To avoid surgical intervention, medical therapies should target correction of the upstream events (i.e., TGF-β signaling) to prevent the deleterious effects of an improperly organized and maintained ECM on aortic biomechanics.
In the LDS patient, medical intervention with Ang II receptor inhibitors to combat the effects of increased TGF-β signaling in LDS patients may show similar to promise as treated MFS patients, but to date, no conclusive efficacy studies have been performed.
2.3 Ehlers-Danlos Syndrome
In patients with Ehlers-Danlos syndrome (EDS), the predilection for vascular abnormalities is rupture or dissection of the first-order branch arteries but aortic dissection and rupture do also occur [70]. EDS patients show clinical manifestation of the disorder as hyperextensibility of the skin which is thin and translucent, hypermobility of joints, extensive bruising, rupture of the arteries, intestines and uterus. The leading cause of death for EDS patients is rupture or dissection of thoracic or abdominal medium-large vessels and this often occurs when the patient age is in the fifties. Clinical management is very difficult in these patients because the vascular tissue is extremely fragile and is not easily sutured. Therefore, surgical intervention often leads to further complications and increases the risk for aortic catastrophe [70]. Expert opinion promotes regular monitoring of EDS patients by CT or MR angiography of the vasculature but there are no well-established guidelines for elective intervention [70]. The EDS patient is extremely difficult to treat due to the high risk of operative treatment and the lack of understanding of the appropriate mechanism to target for medical intervention.
Of the at least 12 known types of EDS with various genetic bases, there are 6 types that are associated with thoracic aortic disease [95]. Over 70 mutations have been linked to EDS and patients displaying the vascular effects of EDS (type IV) are known to have a mutation in the gene encoding type III procollagen [65, 96]. Mutations in type V alpha 1 procollagen have also been reported for EDS patients with arterial rupture [97].
Type III collagen, along with Type I collagen is a predominant form of collagen in the aortic media and is synthesized by aortic SMCs [98, 99]. The effects of Col3a1 mutation has been difficult to analyze due to lack of a successful animal model. Mutations achieved through targeted ablation of Col3a1 showed aortic dissection and bruising of the skin, however only 5% of homozygous mice survived at weaning and most died within 48 h of birth. Recently, a new mouse model with spontaneous mutation of the Col3a1 gene was identified serendipitously whilst investigating the role of Mro in sexual development [100]. These mice died of aortic dissection of the descending thoracic and abdominal aorta with no evidence of inflammation. While there was no difference in overall collagen gene expression, histological analysis of collagen deposition showed an overall decrease in collagen content in the aortic adventitia. Transmission electron microscopy displayed disrupted collagen as well as elastin fibers (Fig. 4). The investigators also provided evidence of normal TGF-β signaling as well as lack of hypertension in col3a1-mutated mice. This model should prove useful in future investigations of the role of Type III collagen in the microarchitecture of the aorta. Since the adventitia has long been recognized as providing substantial biomechanical support for the aorta, disruption in Col31a may abrogate this role of the adventitia in EDS IV patients. Improperly formed collagen fibrils probably provide less strength against hemodynamic forces and lead to dissection, rather than aneurysm. The mouse model described by Smith et al. [100] also brings to light a putative role for Type III collagen in maintaining the layers of SMCs and the collagen/elastin matrix within the aorta. Evidence of shearing between layers was observed with infiltration of red blood cells. This is primary evidence for impending dissection. Therefore, the biomechanical contribution of Type III collagen may be to protect inter-layer strength and mutations in this key ECM protein may place the patient at risk for rupture by aortic dissection. While Type I collagen is thought to provide most of the tensile strength of the aorta and organize as thicker fibers, Type III collagen is found as thinner fibers in close association with elastin where it can participate in recoil capabilities [101]. A point mutation was identified in a patient with EDS IV, located in one of the Gly-X-Y backbone sequences of the alpha chain [102]. The mutation causes the Gly to become a Glu and given that Gly is required for the triple-helical structure of the collagen fiber, this mutation de-stabilizes the collagen within the aorta and likely compromises its biomechanical integrity.
Transmission electron microscopy of aortas from +/Col3a1 Δ mice display abnormalities in matrix architecture. a Normal +/+ mice show regular continuous elastin (*) while there is reduced density of elastin (*) in +/Col3a1 Δ mice (b). The elastin lamellae is discontinuous (black arrows) and dissection through the media layer is also noted in +/Col3a1 Δ mice (white arrows) (c). There is evidence of erythrocyte infiltration within the medial layer in (d) and (e) and the elastin lamellae (arrow). Collagen fiber abnormalities are evident as shown (f) and (g) (arrows). L=lumen; m=media; r=erythrocytes; sm=smooth muscle; Le=leukocyte. Scale bar=5 μm for a–e and 2 μm for f, g. (Figure 4 from Smith et al. [100])
Collagen fiber strength is dependent on its cross-links formed between adjacent helical domains. The mechanical properties can be altered when cross-linking is modified either chemically or physically. The enzyme lysyl oxidase (Lox) catalyzes formation of lysine or hydroxylysine cross-links. Lox expression parallels that of Type I and III collagens [103–105]. Enzymatic activity of Lox is dependent on copper for the transfer of electrons to and from oxygen for delamination of peptidyl lysyl groups on collagen and elastin [106]. Furthermore, variations in copper metabolism have long been linked to EDS type IX which has clinical manifestations including bladder diverticula, skin hyperelasticity and skeletal abnormalities [107]. In patients with impaired copper metabolism, a reduction in Lox expression and decreased collagen cross-linking in cultured skin fibroblasts was reported. Inactivation of Lox has also been linked to aortic aneurysm formation and death in a mouse model [108]. Mutations in Type III collagen that alter collagen fiber assembly may also negatively impact the cross-linking by Lox by directly altering the sites for cross-link formation which are critical to the biomechanical function of the collagen fibers.
There is also an established link between EDS patients and mutations in TGFBRs, accompanied by elevated TGF-β signaling, similar to LDS patients. It is also thought that reduced expression of Type III collagen may be compensated for by enhanced TGF-β in an ineffective attempt to rebuild a deficient matrix. It has also been proposed that cellular response to TGF-β within the aortic wall differ by cell type as reviewed recently by Jones et al. [109]. During the process of aneurysm formation or other forms of vascular injury, the relative proportion of SMCs, fibroblasts and myofibroblasts changes and the phenotype of SMCs is also altered toward the undifferentiated, synthetic state. It is important to understand the molecular nuances of TGF-β signaling in the normal and aneurysmal aorta in order to ascertain the role of these pathways on the overall tissue homeostasis. Balanced interplay between cells and matrix ultimately drives maintenance of adequate biomechanical strength to support the efforts of the heart to deliver blood throughout all body tissues. There are clues in the biochemical pathways, but the real knowledge of tissue homeostasis lies with biomechanical analysis of the tissue itself.
As with MFS and LDS patients, to date, the biomechanical strength of ascending aorta from EDS patients has not been investigated using ex vivo approaches. The work of Sun et al. [110] using optical tweezers offers another strategy to quantify the strength of individual collagen fibers from native tissue or those produced by culture cells in vitro (Fig. 5). These analyses could allow the interrogation of mutated forms of collagen produced recombinantly to determine the role of particular collagens and collagen structure on the biomechanical strength of the aorta and the causal role of mutations in EDS. Understanding the metabolism of collagen cross-linking and the impact of improper collagen assembly on the overall biomechanical strength of the aorta will improve the clinical management and treatment of patients with EDS who are at increased risk for complications during surgical intervention. Strategies to derive medicinal therapies for EDS patients might include focus on targeted repair of collagen cross-linking and/or assembly to improve the biomechanical strength of the aorta and prevent dissection or rupture in these patients.
Demonstrate of using optical tweezers to measure force of stretching a single collagen molecular. Such technology will be useful for characterizing the biomechanical properties of collagen fibrils. (Figure 1 from Sun et al. [110])
2.4 Bicuspid Aortic Valve
BAV is the most common cardiac malformation and occurs in 1–2% of the general population with a gender bias of 2:1, males versus females [72]. The presence of a BAV pre-disposes the patient to formation of TAA and aortic dissection and usually requires careful surveillance and often surgical intervention for the associated co-morbidities of aortic insufficiency or stenosis in addition to ascending aortic replacement due to TAA or dissection. These phenomena that transpire in the BAV patients arise from an unknown pathway that is thought to stem from effects of altered hemodynamics through the BAV and/or due to an inherent defect in the wall of the ascending aorta which contributes to loss of biomechanical strength and leads to dilatation and aneurysm formation. The causal pathway of aneurysm formation in BAV patients appears to be distinct from patients with a morphologically normal aortic valve, known as tricuspid aortic valve (TAV). Within our clinical database, we confirm a remarkable bimodal age distribution for TAAs with a mean age of 51 for patients with BAV compared to a mean age of 68 for patients with TAV. This same bimodal age distribution was noted among patients with Stanford type A aortic dissection [111]. Strikingly, over 40% of patients undergoing replacement of the ascending aorta for aneurysm or dissection at large thoracic aortic surgical centers have BAV. BAV patients have uniformly larger diameter aortic roots and ascending aortas compared to age- and sex-matched controls [112]. The aortic roots of BAV patients, even in the absence of aneurysmal disease or valvular stenosis, have abnormal elasticity [113, 114]. This inherent aortopathy present with the BAV syndrome and the consequent aortic aneurysm formation greatly increases the risk of aortic dissection and sudden death in these patients [69].
Although linkage analysis shows evidence of genetic basis for BAV [70, 115, 116] and mutations in Notch 1 have been associated with calcification of the aortic valve and development of aortic stenosis [117], no gene or pathway to date has clearly defined a cause of the aortic pathologies occurring in patients with BAV. TAAs of the BAV patients display similar histopathology as those of connective tissue disorders discussed above. These included CMD, non-inflammatory SMC apoptosis, accumulation of proteoglycans, increased MMP activity and extensive elastin fragmentation. As with other TAAs, those occurring in BAV patients involve matrix degradation which results in a weakened biomechanical response, incapable of withstanding hemodynamic forces and as a result, aneurysm occurs and places the patient at increased risk for dissection and rupture.
Unlike the other connective tissue disorders, no gene has been identified for BAV, so there is considerably less known on the potential mechanism of TAA formation in BAV patients. The incidence of BAV overlaps with α-SMA and TGF-βR mutations at a frequency of 2.5–3% [73] but no gene or pathway responsible for inciting TAAs in BAV patients has been identified. A role for reactive oxygen species (ROS) in the development of TAAs in BAV patients has been reported by Phillippi and Gleason [118, 119] ROS have been implicated in the development of TAAs in non-BAV patients as well [120, 121], but the mechanism inciting TAAs remains elusive. Recent work from Phillippi and Gleason has focused on the role of the ascending aortic SMCs in maintenance of the aortic ECM. It was shown by gene array that several isoforms of a family of stress response proteins called metallothioneins (MTs) were substantially down-regulated in the ascending aorta of aneurysmal patients with BAV relative to normal non-aneurysmal patients and aneurysmal patients with TAV [119]. MTs are a superfamily of intracellular cysteine-rich proteins of low (<7 kD) molecular weight, with high metal binding and redox capabilities. MTs appear to be primarily stress response proteins and are transcriptionally activated under conditions of reactive oxygen species, hypoxia, UV irradiation and heavy metal exposure. The mechanism of action for MT has not been delineated. Many studies suggest that MT plays a role in the homeostasis of essential metals such as zinc [122] and cadmium (Cd) [123], detoxification of metals, and protection against oxidative stress [124–127]. MT-/- mice are non-lethal and studies have demonstrated that MT is not required for proper growth or development, however the absence of MT-1 or -2 increased Cd-induced lethality and hepatotoxicity, and overexpression of MTs provided protection from Cd-induced death [128]. MT has been implicated in the pathogenesis of multiple diseases including oxidative stress-induced cardiac dysfunction [129]. MT was also shown to rescue hypoxia-inducible factor 1-alpha (HIF-1α) activity and increase vascular endothelial growth factor (Vegf) expression in a mouse model of diabetic cardiomyopathy [130]. HIF-1α has been extensively characterized as a key player in processes of ECM degradation during neoangiogenesis in cancer progression [131–133] and in normal cells [134, 135]. Induction of Vegf in the presence of ROS was also dramatically reduced in primary SMCs from BAV patients [118]. However, MT has not yet been shown to play a direct role in ECM homeostasis. As part of the overall oxidative stress response and an upstream regulator of HIF-1α and Vegf, MT could elicit down-stream effects that are proponents of ECM degradation.
In a mouse model of Marfan syndrome, Fbn1C1039G/+ mice developed TAAs [136] with reduced expression of superoxide dismutase (SOD) and increased expression of iNOS, NADPH oxidase (NOX) and Xanthine oxidase (XO) [137]. Elevated levels of homocysteine and protein carbonyl content, accompanied by a decrease in total antioxidant capacity, were found in the serum of Marfan patients [121]. Homocysteine is thought to affect MMP/TIMP ratios by modulating Nitric oxide (NO) availability [138, 139], causing increased deposition of collagen and degradation of elastin leading ultimately to altered vessel biomechanics evidenced by reduced aortic flow velocity [140]. Oxidative stress has also been implicated in the pathogenesis of AAAs [141]. Increased expression of the NOX subunit p22phox in TAAs co-localized with MMP activity in the aortic media [120]. These data support a causal role for NOX activity in sub-clinical pathogenesis of BAV aortas. Mice deficient in Nox1 or NOX subunit p47phox were protected from angiotensin II-induced aneurysm and dissection, potentially through modulation of MMP/TIMP ratios [142, 143]. ROS appear to be associated with impaired vasomotor function [137].
A theoretical cause of TAAs is that the BAV elicits undue biomechanical stress on the aortic wall. This is substantiated by reports that altered hemodynamics cause aortic wall weakening and spatially dependent expression of matrix proteins [144–146] Evidence against a hemodynamic cause for TAAs in BAV patients arises from the clinical observation that BAV patients who have undergone aortic valve replacement prior to TAA development remain at increased risk for ongoing aortic dilatation [147] which is discordant with the degree of aortic stenosis or insufficiency [112, 114]. Patients with aneurysm or dissection of the ascending aorta, including those with BAV, exhibit evidence of ECM degeneration, such as elastin fragmentation and increased collagen deposition [45, 48, 60–62, 74, 75, 118] as do NOX-1-deficient animals [148, 149]. The increase in collagen matrix deposition [45, 47, 118, 150, 151] in BAV-TAAs as a putative result of ROS [142] may serve as a compensatory mechanism to counter the MMP/TIMP imbalance [152, 153]. Endothelial nitric oxide synthase (eNOS)-deficient mice demonstrate a 32–41% incidence of BAV [154, 155]. Polymorphisms of eNOS are linked to AAAs [156–158] and intracranial aneurysms [159–163] and reduced eNOS is observed in the aortic endothelium of BAV patients [164] and linked to experimental (elastase perfusion) [165] and age-related AAAs [166] but has not been characterized for TAAs. There is mounting evidence for a role of ROS in disrupted ECM homeostasis but a defined molecular mechanism has yet to be established. ROS is known to impact the SMC phenotype [167, 168], shifting them towards a de-differentiated state which increases ECM matrix synthesis [169] and is associated with TAAs of various origins [66, 67, 73, 170–173] and thus could modulate tissue biomechanical strength.
The BAV aorta is pathologically similar to those of the other connective tissue disorders but the mechanisms inciting the final common pathway of ECM degeneration and biomechanical failure appear to be distinct. Like LDS, collagen expression is elevated in TAAs of BAV patients [118]. Collagen is radically affected by the presence of ROS and the lucid SMC phenotype takes preference toward de-differentiation in TAAs [173] and is strongly influenced by oxidative stress [167, 168]. The inability of SMCs of BAV patients to adequately sense and cope with oxidative stress appears to negatively impact matrix deposition and orientation. Collagen fibers appear more disorganized in TAAs of BAV patients [174]. In agreement with the observations of increased collagen deposition and disorganization, preliminary results the authors' laboratories of ex vivo biomechanical testing of freshly-harvested TAA specimens demonstrated increased tensile strength and decreased delamination strength of BAV specimens when compared to aortas of healthy individuals [175–178].
These observations support a pivotal role of the SMCs in maintaining the aortic ECM. The aortic SMCs, presence of excess ROS, and the cells’ ability to manage oxidative stress warrants further investigation pertaining to their role in overall ECM homeostasis and biomechanical integrity of the vessel wall. Improved treatment of BAV patients will likely come from drawing connections between SMC response to ROS in the form of cell viability and phenotypic modulations and the impact of these behaviors on ECM deposition, organization and biomechanical integrity.
2.5 Other Familial Thoracic Aortic Aneurysms
There are many instances of familial TAA where there is no connective tissue disorder present, nor incidence of BAV but there is heritability of aortic diseases within families. Linkage analysis has documented genetic loci that are implicated in familial aortic disease but no gene or pathway inciting ECM degeneration has been identified to date. In some patients, mutations in fibrillin-1 are similar to that of Marfan syndrome but lacking clinical manifestations in other organ systems [73, 179]. Expert surgical opinion suggests that these patients follow strict surveillance similar to that recommended for MFS patients [70]. The fundamental mechanism of failure is likely similar to that of other TAAs and include ECM degradation. As mutated genes and faulty pathways are identified in these patients, the impact of their dysfunction on ECM homeostasis and biomechanical integrity can be investigated.
3 Biological Mechanisms that Impact Mechanical Properties of the Aneurysmal Abdominal Aorta
During AAA formation and enlargement, the biomechanics of the aortic wall change dramatically [11, 26, 30, 31, 180–182] due to loss of ECM integrity which is spatially variable [21, 31, 183–185] (Fig. 6). Several studies demonstrated that the tensile strength decreases as the aneurysm expands [11, 26] and wall strength and stiffness are spatially variable [21, 29, 31]. The evidence supports the notion that local factors such as wall stress and/or hypoxia negatively influence the biomechanical strength of the vessel wall by promoting localized ECM degradation that is known to occur in AAAs [30, 186, 187]. Portions of AAAs were found to be stiffer, contain less elastin and collagen when compared to normal aorta. It is now well accepted that AAAs arise and progress up to failure when stress in the aneurysm wall exceeds the strength of vessel wall. However, little is known of the biological mechanisms driving ECM degeneration in AAAs but two areas under close scrutiny are stress-mediated and strain-mediated wall weakening and hypoxia-mediated disruption of ECM homeostasis.
Relationship between hemodynamics and growth and remodeling simulations of blood vessels. (Reproduced from Fig. 1, Sheidaei et al. [185])
3.1 Stress/Strain-Mediated Formation of AAAs
Mechanical forces or deformations are considered to be paramount to maintenance of microstructure in normal tissue under physiological conditions. Elastin concentration was found to decrease with the diameter in the non-aneurysmal and aneurysmal aorta [188]. Variations in aortic wall stress are supported by the law of Laplace which indicates that vascular wall stress is directly proportional to its diameter. Hence, areas of dilatation may occur in response to spatial changes in wall stress [183]. The observation of focal saccular outpouchings, also known as “blebs” within the walls of AAAs are speculated to be sites of higher risk for rupture since these represent areas of stress concentration [189]. The latter is very important in practice because rupture of the material is commonly expected to start at the location of stress concentration. These blebs were also characterized by decreased collagen and elastin when compared to neighboring sites within the AAA [190]. Mechanical forces are known to influence ECM production by SMCs [191, 192], endothelial cells [193] and other cells [194]. These combined data on spatial variability in ECM content and cell response to stress support the fact that stress concentration leads to disrupted ECM homeostasis, resulting in weakening of the aortic wall. In atherosclerosis, the occurrence of lesions at branch in artery is also correlated with the stress concentration. Similar mechanisms may contribute to formation and/or progression of TAA since ECM proteins were found to be differentially expressed on the greater and lesser curve of the ascending aorta [195].
Some of the major known contributors to ECM degradation are the MMPs. Elevated MMPs have been identified in both TAAs and AAAs and are influenced locally by stress [43, 153], aneurysm size [196] and growth rate [197]. MMPs, and other proteolytic enzymes such as tPA and urokinase plasminogen activator are enhanced by mechanical stress [153]. Macrophages also play a dominant role in increasing MMP production as part of the inflammatory response that occurs with AAA [21, 198]. Macrophages are centralized to areas of atherosclerotic plaques and elevated MMP production is observed in these zones of decreased mechanical strength [199, 200]. These studies suggest that macrophages may play a key role in reducing the strength of AAA via stress-mediated expression of proteolytic enzymes. The local SMCs and/or fibroblasts and especially the macrophages appear to “sense” the mechanical stimulation and respond by increasing production of proteolytic enzymes. Elevated levels of MMPs then work to degrade the ECM and thus weaken the biomechanical integrity of the aortic wall, leading to aneurysm formation and risk for rupture. The molecular signaling mechanisms by which mechanical stimulation promotes increased MMP expression remain elusive but likely involves a complex network of intracellular signaling pathways connected to cytoskeletal proteins that are indirectly tethered to the ECM. Some recent studies have targeted the Jnk and MAPK pathways as mediators of MMP regulation in AAA [201, 202].
Therefore, locally acting forces (and therefore wall stresses) play an important role in the pathophysiology of aneurysmal disease. Specifically, local ECM degeneration of the aneurysmal wall, which could result in a compromised structural integrity of the AAA wall, appears to coincide with areas of increased wall stress. These studies support the idea of spatial variation of wall strength that could result in increased risk for rupture in defined locations that vary patient-to-patient.
3.2 Hypoxia-Mediated Wall Weakening
Another powerful modulator of ECM deposition is hypoxia. As discussed in the TAA sections above, hypoxia and ROS disrupt the normal balance of ECM synthesis and degradation by directly influencing production of ECM protein and regulatory proteins. Hypoxia has been shown to both increase [203–205] and decrease [206, 207] production of collagen by SMCs. These observations suggest that local hypoxia contribute to aneurysm wall weakening through inhibition of ECM synthesis. Expression of MMPs as well as their release of elastase [208] and cytokines [209] is also greatly enhanced in macrophages under hypoxic conditions [210]. The hypoxic state may be caused by the presence of ILT [21, 211]. As a consequence, the mural cells within these zones likely respond to this environment. A greater number of macrophages were found within [212] and in the vicinity [198] of the ILT along with many other inflammatory cells when compared to adjacent locations within the AAA. These areas displayed reduced elastin and increased MMPs. These collective data point to a role for hypoxia in stimulating ECM degradation and thus, negatively influence the biomechanical integrity of the aorta wall, consequently leading to AAA formation in these patients.
3.3 Genetic Causes of Abdominal Aortic Aneurysm
There have been extensive efforts made to identify genetic causes of AAA and a genetic basis for aneurysm growth. A recent systematic review of the literature by Saratzis et al. summarized a majority of these studies as of the year 2011 [213]. Most of the genetic studies center on the matrix-regulating proteins (MMPs, TIMPs), factors related to the inflammatory (interleukins, C reactive protein) and wound healing responses (TGF-βs, platelet-activating factor, plasminogen activator inhibitor 1 (PAI-1), osteopontin and osteoprotegrin (OPG)). The majority of studies investigating the role of these proteins in AAA formation demonstrated alterations in gene or protein expression and identified gene polymorphisms causing these changes in expression. However, most analyses failed to demonstrate a direct association between gene polymorphisms and AAA formation or growth. A few polymorphisms were found to be associated with development (MMP-3, [214] MMP-9, [215] TIMP-1 and -2 [216–218] the β-chemokine receptors, CCR5 [219] and CCR2 [220] angiotensin converting enzyme [221] methylene tetra hydro folate reductase (MTHFR) [222–224] and potentially endothelial nitric oxide synthase (eNOS), although the sample size was relatively small [225]) or growth (PAI-1 [226], and an OPG-regulating factor called peroxisome proliferator-activated receptor gamma (PPARG) [227]).
Another recent review by Krishna et al. discussed the genetic and epigenetic causes of AAA [228] and was in agreement with Saratzis et al. for which there is a general lack of genetic polymorphisms strongly correlated with AAA. The “Aneurysm Consortium” has undertaken large Genome-Wide Association Studies (GWAS) to analyze variance in diseased patients and controls [229]. From this work, there was a strong correlation of chromosome 9p21.3 locus performed with respect to AAAs and was originally identified from seven different populations [230]. A more recent study demonstrated that this association remained despite removing other AAA risk factors such as smoking, coronary heart disease, family history and dyslipidemia [231]. This chromosomal region is thought to be non-coding DNA, consisting of repetitive DNA of retrotransposons which are transient genetic elements that move across the genome. Among these are a long interspersed nuclear elements 1 (LINE-1) which can invade a variety of genes and result in multiple phenotypic outcomes. A recent study evaluated several polymorphisms of 9p21.3 and their association with AAA. Only two polymorphisms were found to be significantly associated with two open reading frames (ORFs), providing evidence that LINE-1 elements may be involved in a genetic cause of AAA [232]. However, further larger studies are needed to confirm this association. The Aneurysm Consortium also identified a single nucleotide polymorphism (SNP) on 9p21 which was previously shown to be associated with heart disease and recently with AAA [230]. Neighboring genes to this particular SNP code for proteins related to cell proliferation, apoptosis and senescence [229] and could be related to SMC phenotype.
Gene products which have been shown to be altered in AAA and may or may not have had polymorphisms identified include MMP-2,3,7, 9, TIMP-3, inducible nitric oxide synthase (iNOS), eNOS, interferon-gamma (INF-γ), tumor necrosis factor (TBN)-α, intercellular adhesion molecule (ICAM)-1, IL-6, TGF-βRII, platelet-derived growth factor (PDGF)-A, estrogen receptor (ER)-α/β, c-fos, 5-lipoxygenase (5-LO), extracellular superoxide dismutase (EC-SOD), fatty acid desaturase (Fads)-2, MTHFR and p53 [228]. Several epigenetic changes such as histone modifications and DNA methylation can alter expression of these genes, and therefore cause the variation observed in AAA relative to normal patients. These epigenetic alterations can stem from known AAA-related risk factors such as smoking, ageing and inflammation. Among these, smoking is the most prevalent risk factor for AAA, and over 80% of patients developing AAA have a history of smoking [233].
4 Biomechanics of AAA and TAA
4.1 Methods for Measuring and Modeling Aortic Biomechanics
Aneurysm rupture can be seen as a mechanical failure of the degenerated aortic wall that occurs when the wall stress acting on the aneurysmal wall exceeds the wall strength. Therefore, the knowledge of both wall stress and wall strength distributions for a given aneurysm will greatly improve the ability to identify those aortic aneurysms that are at highest risk of rupture. Towards this end, the biomechanics of AAA has been studied extensively by many groups whereas TAA biomechanics has not been fully considered. This section provides the state-of-the-art of AAA biomechanics, including the modeling of tensile strength and wall stress distributions and factors which influence them. Then the potential clinical utility of these estimates in predicting AAA rupture will be also presented. A summary of recent advances in TAA biomechanics is also articulated.
4.2 Analysis of Biomechanical Strength and Wall Stress In vivo
4.2.1 AAA Wall Strength
Given the general recognition of the importance of wall mechanics in the natural history of AAAs (e.g., [183, 234–236]), there have been numerous studies of AAA biomechanical properties. Noninvasive diagnostic techniques such as ultrasound and computer tomography have long been used to understand AAAs wall mechanics. Indeed, early studies focused on gross measurement of structural stiffness [37, 237–239] or vessel compliance [240, 241], including the effect of ILT [242]. Although these investigations were useful for clinical correlations, the AAA wall strength was not evaluated by these approaches.
Vessel wall strength has not yet been measured in vivo due to the deficiency of current experimental techniques. However, researchers have easily assessed AAA wall strength performing ex vivo experimental testing on excised normal and pathological aortic tissue. Early ex vivo studies on the biomechanical properties of AAAs focused on understanding the effect of extracellular derangement observed in aneurysms [186, 187]. Reported uniaxial sub-failure tensile data for eight human AAAs and eight age-matched controls (all axially oriented specimens) revealed a stiffer AAA wall compared to that of the normal aorta [30]. Similar findings demonstrated that the aneurysmal aorta in the circumferential direction was stiffer than the axial direction, and that posterior portions were less stiff than anterior or lateral portions, suggesting a stiffness variation around the lesion [31]. These findings were corroborated by Vallabhaneni et al. [243] suggesting a correlation between strength and variation in MMP production, and Ragahvan et al. [244] reporting spatial variation of wall thickness and tensile strength in an excised AAA. Variation in AAA wall strength from point-to-point in a given aneurysm or from patient-to-patient support the fact that evaluation of AAA wall stress alone is insufficient to predict rupture and that AAA wall strength cannot be assumed to be constant on aneurysms. Vorp et al. widely investigated AAA wall mechanics, reporting measurements of AAA wall strength [26], and formulating both microstructure-based [11] and hyperelastic, continuum-mechanics-based models for the AAA wall mechanics [181]. In particular, the latter study reports uniaxial tensile tests on 69 freshly-excised human AAA specimens oriented along either the circumferential and longitudinal directions. They also quantified experimental data with a strain energy function of the form W= α(I B −3) + β(I B −3)2 where I B =tr B=tr( F • F T ) and F is the deformation gradient, and α and β are the model parameters indicative of the mechanical properties in longitudinal or circumferential directions (Fig. 7). This continuum-based constitutive model is appropriate for wall stress prediction [183] since it can be easily implemented in finite element analysis compared to microstructure-based models. To investigate the association of aortic wall weakening with AAA rupture, ex vivo tensile tests on freshly-excised wall tissue specimens from patient who suffered AAA rupture prior to surgery were compared to specimen tissues from elective repaired, asymptomatic AAA [12]. The tensile strength of the ruptured AAA tissue was found to be significantly lower than that for the elective AAA tissue (Fig. 8). This data suggests that AAA rupture is associated with significant aneurysm wall weakening, supporting the idea that wall strength needs to be carefully considered on a patient-specific basis in order to accurately predict rupture potential of individual aneurysms.
The experimentally determined relationship between the first derivative of strain energy function and the first invariant of the stretch tensor for a representative AAA specimen. Linear regression resulted in a highly correlated fit (R2=0.99), indicating a linear relationship between the two. (From Fig. 1, Raghavan and Vorp [14])
Difference in tensile strength of ruptured and electively repaired AAA wall specimens. (From Fig. 10, Vorp [183])
Uniaxial testing is not sufficient for highlighting the multi-axial biomechanical response of vessel in vivo; therefore, normal and pathological abdominal aorta tissue specimens have been tested in a biaxial testing device [245] to obtain more appropriate constitutive relation of aortic tissue and to investigate any apparent anisotropy of the aorta. The high non-linear responses found on 26 AAA tissue samples and 8 aged-matched abdominal aorta samples were described well by a two-dimensional phenomenological Tong-Fung (1976) strain energy function. These results confirmed the general observation that AAAs are indeed stiffer and more anisotropic (i.e., stiffer in circumferential direction) than the normal aorta. Comparison between strain energy functions derived from uniaxial testing [14] and biaxial testing [246] provided evidence for remarkable differences in mechanical response of the tissue between the two models, demonstrating the importance of correct model choice in biomechanical simulations (Fig. 9).
There has been less attention to the influence of biomechanical properties of ILT that often lines AAAs. Di Martino [180] first reported uniaxial testing on 21 samples of thrombus obtained from 6 patients generating support for the idea that thrombus may be “mechanically protective” by providing stress shielding or a cushioning effect for AAA wall. The most comprehensive study of the biomechanical properties of ILT from human AAAs [247] revealed that the behavior is mildly non-linear over large strain, nearly isotropic [29] and inhomogeneous since portions of tissue from the luminal region were found to be stiffer and stronger when compared to middle region (Fig. 10).
Typical set of stress-stretch curves for ILT samples taken from the luminal region (upper set of curves) and the medial region (lower set of curves). All data were obtained from the same ILT (same patient). (From Fig. 3, Vorp [183])
Although these mentioned studies established that AAA biomechanical properties changes with aneurysm formation and that these properties are spatially variable, little progress has been made to provide methodology to noninvasively predict the local wall strength distribution in a given AAA. A statistical-multifactorial mathematical model is currently the only model for assessing the AAA wall strength with a noninvasively approach. Specifically, multiple linear regression techniques were used to derive a statistical model for the prediction of AAA wall strength based on experimental measurements and measurable pertinent predictors, including local AAA diameter, local ILT thickness, patient age and gender, and patient family history of AAA disease [see the excellent work by Vande Geest [20] for more on this statistical model]. The predictability and example applications of such a model are shown in Figs. 11 and 12 [20]. In this study, the concept of RPI, which is defined as the locally acting wall stress divided by the local wall strength, was also introduced to define the propensity to rupture of a given AAA.
4.2.2 AAA Wall Stress
In recent years, there has been an increasing effort to develop appropriate finite element (FE) models to assess the wall stress in dictating the fate of aneurysm failure. Early stress analyses have assumed idealized geometries, and are based on law of Laplace [248–250], axisymmetric membrane theory [16] or linear elastic material behavior [251, 252]. Moreover, Inzoli et al. [251] were the first group to introduce an important, but controversial, concept: that ILT may act to reduce AAA wall stress by a shielding effect. However, these models are inappropriate to describe the inherent non-linearity of the aorta under large deformations and fail to demonstrate the likely importance of blebs which, in turn, cause stress concentration (Fig. 13). The best models available utilize patient-specific geometries and treat the aneurysmal wall as a non-linear elastic, isotropic, homogenous body [22, 23, 253] (Fig. 14). From these studies, the stress magnitude and distribution were found to be dependent on either the shape of the AAA bulge as well as aneurysm diameter. These findings strengthen the argument for which aneurysm with the same diameter may not necessarily have the same propensity to failure.
Comparison of stresses computed for a 3D asymmetric AAA model using the hyperelastic constitutive model [12] with those using a linearized elasticity model along anterior surface (a), along posterior surface (b), and around mid-section (c). Note the substantial error involved with using the theory of linearized elasticity. (From Fig. 7, Raghavan and Vorp [14])
The distribution of von Mises stress on the posterior and anterior abdominal aortic walls of the control subject and the patients with abdominal aortic aneurysms. Grey regions are those with artificially high stress concentrations because of edge effects. The individual color scales give the stress magnitude. In all cases, blue represents the lowest stress magnitude, and red represents the highest stress magnitude. Note the comparatively lower range of stress in the control aorta. (From Fig. 4, Raghavan et al. [181])
To accurately mimic the physiological mechanical behavior of the normal and pathological aorta, the proper utilization of the constitutive material models implemented in FE models needs to be evaluated. This was accomplished by Vorp et al. who investigated the influence of constitutive-model material parameters [13, 181] and tissue anisotropy [246] on wall stress prediction. They performed a parametrical analysis by changing the α and β material parameters of the constitutive material model described by Raghavan et al. [181], on several FE stress analyses of hypothetical 3D asymmetric AAAs. The maximum variation of material parameters led to less than 5% in the predicted wall stress, and this suggests that the differences in AAA wall stress from patient-to-patient are driven more by the differences in surface geometry than in material properties. In a similar way, FE analyses on two non-ruptured and one-ruptured AAAs modeled with both isotropic [14] and anisotropic [29] wall constitutive relation demonstrated that an anisotropic material model provides a better prediction of the stress distribution in AAAs compared to an isotropic model. The most advanced FE models also consider the presence of ILT contained in most AAAs. Indeed, the incorporation of thrombus into computational stress analysis models the profound influence on the magnitude and distribution of stress acting on the AAA wall, and this should be considered for accurate wall stress estimations (Fig. 15). Recently, the statistical model for predicting wall strength and rupture potential index proposed by Vande Geest et al. [182] were implemented in FE analysis [28] and compared with the maximum diameter criterion to evaluate their reliability in AAA rupture prediction. The strength model reported by Vande Geest was misused by the authors (the local normalized diameter that was used was not as specified by the original model), and it is unclear how this affected their results.
Comparison of 3D wall stress distribution between AAA models with and without ILT. Individual color scales (right) indicate von Mises stress for each AAA. Both posterior and anterior views are shown for each case. (From Fig. 4, Wang et al. [19])
There has been increasing interest in fluid–structure interaction (FSI) modeling of AAAs, yet most studies assume the non-aneurysmal and aneurysmal aorta, and ILT as linear elastic, homogeneous, isotropic, nearly incompressible body [254–256]. While these studies have been important to demonstrate that the pressure field in AAAs is relatively constant [257, 258], the effect of shear stress was neglected. Perhaps, the most important sophisticated FSI model to date is that by Rissland et al. [259], incorporating ILT, wall calcification, and anisotropic tissue properties. Experimental biaxial data of AAAs [29] were fitted with the Holzapfel orthotropic material formulations [260] which models vessel wall as fiber-reinforced composite material. Calcified plaques surrounding AAAs were assumed to behave as stiff isotropic materials whereas the ILT was modeled as linearly elastic. Later, Xenos et al. [39] validated this FSI methodology to assess rupture propensity on cases of ruptured AAA using the wall strength model and RPI proposed by Vande Geest et al. [182] (Fig. 16).
Wall strength mapping and the corresponding rupture potential index, for the ruptured AAA cases. Multiple distinct regions of high RPI are observed, with at least one that coincides with the actual location of rupture. The RPI for both cases is close to unity indicating a very high risk of rupture, with a higher RPI (0.95) for the smaller rAAA. (from Fig. 6, Xenos et al. [39])
These studies have demonstrated that computational models have potential to improve the predictions of rupture potential. It should be also noted that many investigators report the Von Mises stress to assess the maximum stress, inducing to AAA failure. However, Von Mises stress has its importance in the fracture mechanics of ductile materials, which yield due to excessive shear stresses. The aorta has a nonlinearly elastic behavior, not exhibiting yielding, where failure is governed by maximum normal stress [261–263]. Therefore, this issue of a most appropriate failure criterion must be addressed in future investigations.
4.2.3 TAA Wall Strength and Wall Stress
Despite the aforementioned importance of wall strength in the mechanics underling the aortic failure, there has been less attention to that of thoracic aortic aneurysm. This pathology is also particular lethal although the relatively rare incidence. Similar to AAA, aneurysm involving the ascending and descending aortic segments can rupture. However, a more common pathology is dissection where an intimal tear, often circumferential in origin, permits blood to enter the aortic wall splitting the media and progressively separating the medial plane along the axial direction of the aorta. From a biomechanical viewpoint, the dissection represents a separation of the elastic layers of the degenerated aortic wall that occurs when the hemodynamic loads exerted on the aneurysmal wall exceed bonding forces that normally hold the layers together. Clinical hemodynamic disturbances that render the aorta susceptible to the onset of dissection are principally elevated maximum systolic and mean aortic blood pressure [264].
Early studies reported experimental data for normal descending and mid-thoracic aorta from uniaxial tensile tests [261, 265] and inflation tests [261, 266]. These studies indicated that wall strength is dependent on the anatomic site of the vessel and that tensile failure behavior is perhaps anisotropic. Early wall strength measurements of ascending thoracic aortic aneurysm (ATAA) revealed biomechanical characteristics similar to those of the abdominal aorta. Ex vivo studies by our laboratory on thirty aneurysmal aortic tissue specimens oriented in both the longitudinal and circumferential direction demonstrated that tensile strength in ATAA is 30% lower than non-aneurysmal ascending aorta, suggesting higher risk of rupture in patients with ATAA [33]. Additionally, tissue stiffness of ATAA wall was found to be higher than normal aorta and particularly, the longitudinal direction was stiffer than the axial direction. Later, Iliopoulos et al. [32] reported lower longitudinal tensile strength with aneurysm enlargement. The low wall strength in longitudinal direction found in these investigations may be responsible for aortic dissection in ATAAs.
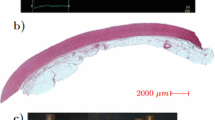
As found for AAAs, the ATAA wall strength and stiffness vary spatially. Ex vivo tensile testing data revealed uniform ATAA tissue strength and stiffness along the circumferential direction whereas, in the longitudinal direction the anterior region was the weakest and least stiff part of the aneurysm, and this can be associated with the clinical evidences of preferential ATAA bulging in the anterior region [267]. Tensile wall strength data associated with abnormal valve morphology revealed that ATAA tissues excised from patients with bicuspid aortic valve are stiffer than those from those patients with tricuspid aortic valve [34]. However, these findings are limited by a relatively small sample size (n = 6). Only one study reported media splitting testing measurements to understand the dissection properties of thoracic aorta [268]. By infusing liquid into media, a bleb was created and thus the propagation of the liquid was monitored to explore the mechanics of dissection.
Although FE methodology has been applied extensively in the prediction of wall stress for AAAs, it has not been given the same degree of importance in the investigation of wall stress in ATAAs. Therefore, computational modeling of ATAAs is very limited and recent. In the earliest study, the ATAA was modeled as an axisymmetric dilation in a cylindrical aorta as an isotropic, nonlinear, hyperelastic material behavior [269]. As the aneurysm grows, the longitudinal stress in the bulb of the aneurysm is the only stress that was found to increase significantly and thus is likely to cause rupture or dissection. The influence of the aortic root movement on the aortic wall stress as related to aortic dissection was also investigated in a single-layered, linear elastic, isotropic, homogeneous ATAA model [270]. The aortic root motion determined a direct impact on the longitudinal stress that was found to increase critically in the ascending aorta above the sino-tubular junction. This may explain why the intima tears circumferentially and aortic dissections occur more often in this orientation. FSI analyses of descending dissecting aneurysms were reported by several groups [271–273]. Recently, a FSI analysis of an idealized three-layered descending aorta under turbulent pulsatile flow revealed that the media layer exhibited a larger wall stress compared with the intimal and adventitial layers, and thus the high stress due to elastic properties mismatch in the aortic wall is a risk factor for tearing in aortic dissections [272]. The most sophisticated FE model of an ATAA has been presented recently by Nathan et al. [274]. For the purpose of understanding the pathogenesis of aortic dissection, the authors developed a patient-specific model of an ATAA, though their assumptions of homogeneous, incompressible, isotropic, linear elastic properties and uniform thickness are limitations of this work (Figs. 17 and 18). Their results suggested that peak systolic pressure induces localized high wall stress above the sino-tubular junction and at the ostia of the left subclavian artery that may account for the development of type A and type B aortic dissection, respectively.
Three-dimensional wall stress distribution for the normal ascending aorta. Stress in mega-pascals (MPa) is mapped, with the highest stress in red and lowest stress in blue. The black arrows indicate maxima of stress on the (a) convex and (b) concave side of the ascending aorta. (From Fig. 3, Nathan et al. [274])
Three-dimensional wall stress distribution for the normal thoracic aorta. Stress in mega-pascals (MPa) is mapped, with the highest stress in red and the lowest stress in blue. The black arrows indicate maxima of stress distal to left subclavian and innominate arteries. (From Fig. 4, Nathan et al. [274])
5 Using Aortic Biomechanical Data to Transform Clinical Care
All of the criteria that have been proposed to treat AAA and ATAA are based on empirical data with less emphasis on sound physical principles. The current gold standard for surgical intervention for a patient is based primarily on the maximum orthogonal diameter of the vessel, namely the “maximum diameter criterion”, which is 5.0–5.5 cm for both TAAs and AAAs. Nevertheless, this criterion can be improved as it has resulted in a rupture rate of 1% per year for patients under observation [2, 275]. Areas of peak wall stress were found to overlap with sites of rupture [39] and locations of deficient extracellular matrix [30, 186]. Efforts to refine surgical recommendations and predict relative risk for rupture in a patient-specific manner have included consideration of wall stiffness [37], ILT thickness [38], wall tension [8], peak wall stress [22–24] and growth rate [276]. Serum biomarkers of elastolysis also offer promising non-invasive methods and correlated with disease progression but are not of sufficient predicative value. However, all of these approaches have their own limitations, and may lead to errors in decisions pertaining to clinical management of aortic aneurysm.
In this section, we have emphasized the importance of both the wall stress and the wall strength and that these physical parameters derived from failure mechanics principles may be translated in a novel improved criterion to identify those aneurysms that are at highest risk of rupture or dissection. Toward this end, the RPI, which is defined as the locally acting wall stress divided by the local wall strength, appears to be currently the most promising approach. This model relies on the relatively well-established methods for estimating wall strength stress and the evolving field on noninvasive techniques for modeling wall stress.
Despite the great efforts over the past 20–30 years in identifying not only the pathology of aneurysm, but also the significant advances in discovering genetic causes for several forms of ATAAs and the risk factors for AAA, the current risk prediction models are unreliable. Current improvements on this model which incorporate wall stress and wall strength are not yet ready for clinical translation, and the potential future success of these ideas is dependent on the development of novel noninvasive imaging technologies to measure wall strength. One promising technique is 4-dimensional MR that has recently been demonstrated to evaluate systolic flow patterns in the ascending aorta of aneurysmal patients and healthy volunteers [144]. This study shows in dramatic fashion the disrupted flow in BAV patients in a nested helical pattern and could be used to not only estimate local wall shear stress but also model wall strength (Fig. 19).
Use of 4-dimensional flow magenetic resonance (MR) to characterize blood flow velocity in the human ascending aorta. a Smooth trajectory of normal systolic flow in a non-aneurysmal patient with tricuspid aortic valve. b Disrupted, turbulent and helical flow in a patient with an ascending aortic aneurysm and the abnormal bicuspid aortic valve. (Figure 1a and 2c, d from Hope et al. [144])
Our understanding of aortic diseases continues to advance as new partnerships between surgeons, biologists, engineers and mathematicians are established. The future of clinical care for aneurysmal patients lies at the intersection of these fields. In summary, the puzzle of how to care for patients with aneurysm will ideally incorporate knowledge of the biological pathways inciting matrix degradation, an understanding of the biomechanical contributions of the individual molecular entities comprising the matrix, the matrix as a whole and a thorough quantification of both wall strength and stress. The missing pieces lie in developing the enabling noninvasive technologies to measure wall stress and strain, refinement of the mathematical models and establishing links between the clinical manifestations and the biological mechanisms inciting them.
References
Ergin, M.A., Spielvogel, D., Apaydin, A., Lansman, S.L., McCullough, J.N., Galla, J.D., Griepp, R.B.: Surgical treatment of the dilated ascending aorta: when and how? Ann. Thorac. Surg. 67(6), 1834–1839 (1999). discussion 1853–1856 PMID:10391320
Ashton, H.A., Buxton, M.J., Day, N.E., Kim, L.G., Marteau, T.M., Scott, R.A., Thompson, S.G., Walker, N.M.: The Multicentre Aneurysm Screening Study (MASS) into the effect of abdominal aortic aneurysm screening on mortality in men: a randomised controlled trial. Lancet 360(9345), 1531–1539 (2002). PMID:12443589
Lederle, F.A., Johnson, G.R., Wilson, S.E., Ballard, D.J., Jordan W.D., Jr, Blebea, J., Littooy, F.N., Freischlag, J.A., Bandyk, D., Rapp, J.H., Salam, A.A.: Rupture rate of large abdominal aortic aneurysms in patients refusing or unfit for elective repair. JAMA 287(22), 2968–2972 (2002). PMID:12052126
Powell, J.T., Brady, A.R.: Detection, management, and prospects for the medical treatment of small abdominal aortic aneurysms. Arterioscler. Thromb. Vasc. Biol. 24(2), 241–245 (2004). PMID:14604835
Powell, J.T., Gotensparre, S.M., Sweeting, M.J., Brown, L.C., Fowkes, F.G., Thompson, S.G.: Rupture rates of small abdominal aortic aneurysms: a systematic review of the literature. Eur. J. Vasc. Endovasc. Surg. 41(1), 2–10 (2011). PMID:20952216
Pape, L.A., Tsai, T.T., Isselbacher, E.M., Oh, J.K., O’Gara, P.T., Evangelista, A., Fattori, R., Meinhardt, G., Trimarchi, S., Bossone, E., Suzuki, T., Cooper, J.V., Froehlich, J.B., Nienaber, C.A., Eagle, K.A.: Aortic diameter >or = 5.5 cm is not a good predictor of type A aortic dissection: observations from the International Registry of Acute Aortic Dissection (IRAD). Circulation 116(10), 1120–1127 (2007). PMID:17709637
Darling, R.C., Messina, C.R., Brewster, D.C., Ottinger, L.W.: Autopsy study of unoperated abdominal aortic aneurysms. The case for early resection. Circulation 56(Suppl 3), II161–II164 (1977). PMID:884821
Hall, A.J., Busse, E.F., McCarville, D.J., Burgess, J.J.: Aortic wall tension as a predictive factor for abdominal aortic aneurysm rupture: improving the selection of patients for abdominal aortic aneurysm repair. Ann. Vasc. Surg. 14(2), 152–157 (2000). PMID:10742430
Knipp, B.S., Deeb, G.M., Prager, R.L., Williams, C.Y., Upchurch, G.R., Patel, H.J.: A contemporary analysis of outcomes for operative repair of type A aortic dissection in the United States (vol 142, p 524, 2007). Surgery 143(2), 301 (2008) PMID:ISI:000253172300033
Simao da Silva, E., Rodrigues, A.J., Magalhaes Castro de Tolosa, E., Rodrigues, C.J., Villas Boas do Prado, G., Nakamoto, J.C.: Morphology and diameter of infrarenal aortic aneurysms: a prospective autopsy study. Cardiovasc. Surg. 8(7), 526–532 (2000). PMID:11068212
Raghavan, M.L., Webster, M.W., Vorp, D.A.: Ex vivo biomechanical behavior of abdominal aortic aneurysm: assessment using a new mathematical model. Ann. Biomed. Eng. 24(5), 573–582 (1996). PMID:8886238
Di Martino, E.S., Bohra, A., Vande Geest, J.P., Gupta, N., Makaroun, M.S., Vorp, D.A.: Biomechanical properties of ruptured versus electively repaired abdominal aortic aneurysm wall tissue. J. Vasc. Surg. 43(3), 570–576 (2006). PMID:ISI:000235848800027
Di Martino, E.S., Vorp, D.A.: Effect of variation in intraluminal thrombus constitutive properties on abdominal aortic aneurysm wall stress. Ann. Biomed. Eng. 31(7), 804–809 (2003). PMID:12971613
Raghavan, M.L., Vorp, D.A.: Toward a biomechanical tool to evaluate rupture potential of abdominal aortic aneurysm: identification of a finite strain constitutive model and evaluation of its applicability. J. Biomech. 33(4), 475–482 (2000). PMID:10768396
Vorp, D.A., Raghavan, M.L., Webster, M.W.: Mechanical wall stress in abdominal aortic aneurysm: influence of diameter and asymmetry. J. Vasc. Surg. 27(4), 632–639 (1998). PMID:9576075
Elger, D.F., Blackketter, D.M., Budwig, R.S., Johansen, K.H.: The influence of shape on the stresses in model abdominal aortic aneurysms. J. Biomech. Eng. 118(3), 326–332 (1996). PMID:8872254
Sacks, M.S., Vorp, D.A., Raghavan, M.L., Federle, M.P., Webster, M.W.: In vivo three-dimensional surface geometry of abdominal aortic aneurysms. Ann. Biomed. Eng. 27(4), 469–479 (1999). PMID:10468231
Doyle, B.J., Callanan, A., Burke, P.E., Grace, P.A., Walsh, M.T., Vorp, D.A., McGloughlin, T.M.: Vessel asymmetry as an additional diagnostic tool in the assessment of abdominal aortic aneurysms. J. Vasc. Surg. 49(2), 443–454 (2009). PMID:19028061
Wang, D.H., Makaroun, M.S., Webster, M.W., Vorp, D.A.: Effect of intraluminal thrombus on wall stress in patient-specific models of abdominal aortic aneurysm. J. Vasc. Surg. 36(3), 598–604 (2002). PMID:12218961
Vande Geest, J.P., Wang, D.H., Wisniewski, S.R., Makaroun, M.S., Vorp, D.A.: Towards a noninvasive method for determination of patient-specific wall strength distribution in abdominal aortic aneurysms. Ann. Biomed. Eng. 34(7), 1098–1106 (2006). PMID:16786395
Vorp, D.A., Lee, P.C., Wang, D.H., Makaroun, M.S., Nemoto, E.M., Ogawa, S., Webster, M.W.: Association of intraluminal thrombus in abdominal aortic aneurysm with local hypoxia and wall weakening. J. Vasc. Surg. 34(2), 291–299 (2001). PMID:11496282
Fillinger, M.F., Marra, S.P., Raghavan, M.L., Kennedy, F.E.: Prediction of rupture risk in abdominal aortic aneurysm during observation: wall stress versus diameter. J. Vasc. Surg. 37(4), 724–732 (2003). PMID:12663969
Fillinger, M.F., Raghavan, M.L., Marra, S.P., Cronenwett, J.L., Kennedy, F.E.: In vivo analysis of mechanical wall stress and abdominal aortic aneurysm rupture risk. J. Vasc. Surg. 36(3), 589–597 (2002). PMID:12218986
Venkatasubramaniam, A.K., Fagan, M.J., Mehta, T., Mylankal, K.J., Ray, B., Kuhan, G., Chetter, I.C., McCollum, P.T.: A comparative study of aortic wall stress using finite element analysis for ruptured and non-ruptured abdominal aortic aneurysms. Eur. J. Vasc. Endovasc. Surg. 28(2), 168–176 (2004). PMID:15234698
Doyle, B.J., Cloonan, A.J., Walsh, M.T., Vorp, D.A., McGloughlin, T.M.: Identification of rupture locations in patient-specific abdominal aortic aneurysms using experimental and computational techniques. J. Biomech. 43(7), 1408–1416 (2010). PMID:20152982
Vorp, D.A., Raghavan, M.L., Muluk, S.C., Makaroun, M.S., Steed, D.L., Shapiro, R., Webster, M.W.: Wall strength and stiffness of aneurysmal and nonaneurysmal abdominal aorta. Ann. N. Y. Acad. Sci. 800, 274–276 (1996). PMID:8959012
Wang, D., Makaroun, M., Vorp, D.: Noninvasive estimation of wall strength distribution in human abdominal aortic aneurysm. In: Proceedings of ASME-IMECE (2001)
Maier, A., Gee, M.W., Reeps, C., Pongratz, J., Eckstein, H.H., Wall, W.A.: A comparison of diameter, wall stress, and rupture potential index for abdominal aortic aneurysm rupture risk prediction. Ann. Biomed. Eng. 38(10), 3124–3134 (2010). PMID:ISI:000281895500008
Vande Geest, J.P., Sacks, M.S., Vorp, D.A.: The effects of aneurysm on the biaxial mechanical behavior of human abdominal aorta. J. Biomech. 39(7), 1324–1334 (2006). PMID:15885699
He, C.M., Roach, M.R.: The composition and mechanical properties of abdominal aortic aneurysms. J. Vasc. Surg. 20(1), 6–13 (1994). PMID:8028090
Thubrikar, M.J., Labrosse, M., Robicsek, F., Al-Soudi, J., Fowler, B.: Mechanical properties of abdominal aortic aneurysm wall. J. Med. Eng. Technol. 25(4), 133–142 (2001). PMID:11601439
Iliopoulos, D.C., Deveja, R.P., Kritharis, E.P., Perrea, D., Sionis, G.D., Toutouzas, K., Stefanadis, C., Sokolis, D.P.: Regional and directional variations in the mechanical properties of ascending thoracic aortic aneurysms. Med. Eng. Phys. 31(1), 1–9 (2009). PMID:18434231
Vorp, D.A., Schiro, B.J., Ehrlich, M.P., Juvonen, T.S., Ergin, M.A., Griffith, B.P.: Effect of aneurysm on the tensile strength and biomechanical behavior of the ascending thoracic aorta. Ann. Thorac. Surg. 75(4), 1210–1214 (2003). PMID:12683565
Duprey, A., Khanafer, K., Schlicht, M., Avril, S., Williams, D., Berguer, R.: In vitro characterisation of physiological and maximum elastic modulus of ascending thoracic aortic aneurysms using uniaxial tensile testing. Eur. J. Vasc. Endovasc. Surg. 39(6), 700–707 (2010). PMID:ISI:000279522700008
Brown, P.M., Zelt, D.T., Sobolev, B.: The risk of rupture in untreated aneurysms: the impact of size, gender, and expansion rate. J. Vasc. Surg. 37(2), 280–284 (2003). PMID:12563196
Hatakeyama, T., Shigematsu, H., Muto, T.: Risk factors for rupture of abdominal aortic aneurysm based on three-dimensional study. J. Vasc. Surg. 33(3), 453–461 (2001). PMID:11241112
Sonesson, B., Sandgren, T., Lanne, T.: Abdominal aortic aneurysm wall mechanics and their relation to risk of rupture. Eur. J. Vasc. Endovasc. Surg. 18(6), 487–493 (1999). PMID:10637144
Stenbaek, J., Kalin, B., Swedenborg, J.: Growth of thrombus may be a better predictor of rupture than diameter in patients with abdominal aortic aneurysms. Eur. J. Vasc. Endovasc. Surg. 20(5), 466–469 (2000). PMID:11112467
Xenos, M., Rambhia, S.H., Alemu, Y., Einav, S., Labropoulos, N., Tassiopoulos, A., Ricotta, J.J., Bluestein, D.: Patient-based abdominal aortic aneurysm rupture risk prediction with fluid structure interaction modeling. Ann. Biomed. Eng. 38(11), 3323–3337 (2010). PMID:ISI:000282506400006
Yadav, M.K.: Takayasu arteritis: clinical and CT-angiography profile of 25 patients and a brief review of literature. Indian Heart J. 59(6), 468–474 (2007). PMID:19151461
Cid, M.C., Garcia-Martinez, A., Lozano, E., Espigol-Frigole, G., Hernandez-Rodriguez, J.: Five clinical conundrums in the management of giant cell arteritis. Rheum. Dis. Clin. North Am. 33(4), 819–834 (2007). vii PMID:18037119
Long, R., Guzman, R., Greenberg, H., Safneck, J., Hershfield, E.: Tuberculous mycotic aneurysm of the aorta: review of published medical and surgical experience. Chest 115(2), 522–531 (1999). PMID:10027455
Boyum, J., Fellinger, E.K., Schmoker, J.D., Trombley, L., McPartland, K., Ittleman, F.P., Howard, A.B.: Matrix metalloproteinase activity in thoracic aortic aneurysms associated with bicuspid and tricuspid aortic valves. J. Thorac. Cardiovasc. Surg. 127(3), 686–691 (2004). PMID:15001896
Fedak, P.W., de Sa, M.P., Verma, S., Nili, N., Kazemian, P., Butany, J., Strauss, B.H., Weisel, R.D., David, T.E.: Vascular matrix remodeling in patients with bicuspid aortic valve malformations: implications for aortic dilatation. J. Thorac. Cardiovasc. Surg. 126(3), 797–806 (2003). PMID:14502156
Nataatmadja, M., West, M., West, J., Summers, K., Walker, P., Nagata, M., Watanabe, T.: Abnormal extracellular matrix protein transport associated with increased apoptosis of vascular smooth muscle cells in marfan syndrome and bicuspid aortic valve thoracic aortic aneurysm. Circulation 108(Suppl 1), II329–II334 (2003). PMID:12970255
Ikonomidis, J.S., Jones, J.A., Barbour, J.R., Stroud, R.E., Clark, L.L., Kaplan, B.S., Zeeshan, A., Bavaria, J.E., Gorman 3rd, J.H., Spinale, F.G., Gorman, R.C.: Expression of matrix metalloproteinases and endogenous inhibitors within ascending aortic aneurysms of patients with bicuspid or tricuspid aortic valves. J. Thorac. Cardiovasc. Surg. 133(4), 1028–1036 (2007). PMID:17382648
Lesauskaite, V., Tanganelli, P., Sassi, C., Neri, E., Diciolla, F., Ivanoviene, L., Epistolato, M.C., Lalinga, A.V., Alessandrini, C., Spina, D.: Smooth muscle cells of the media in the dilatative pathology of ascending thoracic aorta: morphology, immunoreactivity for osteopontin, matrix metalloproteinases, and their inhibitors. Hum. Pathol. 32(9), 1003–1011 (2001). PMID:11567232
Segura, A.M., Luna, R.E., Horiba, K., Stetler-Stevenson, W.G., McAllister Jr, H.A, Willerson, J.T., Ferrans, V.J.: Immunohistochemistry of matrix metalloproteinases and their inhibitors in thoracic aortic aneurysms and aortic valves of patients with Marfan’s syndrome. Circulation 98(19 Supp), II331–II337 (1998). discussion II337–II338 PMID:9852923
Tamarina, N.A., McMillan, W.D., Shively, V.P., Pearce, W.H.: Expression of matrix metalloproteinases and their inhibitors in aneurysms and normal aorta. Surgery 122(2), 264–271 (1997). discussion 271–272 PMID:9288131
LeMaire, S.A., Wang, X., Wilks, J.A., Carter, S.A., Wen, S., Won, T., Leonardelli, D., Anand, G., Conklin, L.D., Wang, X.L., Thompson, R.W., Coselli, J.S.: Matrix metalloproteinases in ascending aortic aneurysms: bicuspid versus trileaflet aortic valves. J. Surg. Res. 123(1), 40–48 (2005). PMID:15652949
Jacob, M.P.: Extracellular matrix remodeling and matrix metalloproteinases in the vascular wall during aging and in pathological conditions. Biomed. Pharmacother. 57(5–6), 195–202 (2003). PMID:12888254
Xiong, W., Zhao, Y., Prall, A., Greiner, T.C., Baxter, B.T.: Key roles of CD4+ T cells and IFN-gamma in the development of abdominal aortic aneurysms in a murine model. J. Immunol. 172(4), 2607–2612 (2004). PMID:14764734
Pan, J.H., Lindholt, J.S., Sukhova, G.K., Baugh, J.A., Henneberg, E.W., Bucala, R., Donnelly, S.C., Libby, P., Metz, C., Shi, G.P.: Macrophage migration inhibitory factor is associated with aneurysmal expansion. J. Vasc. Surg. 37(3), 628–635 (2003). PMID:12618703
Satta, J., Mennander, A., Soini, Y.: Increased medial TUNEL-positive staining associated with apoptotic bodies is linked to smooth muscle cell diminution during evolution of abdominal aortic aneurysms. Ann. Vasc. Surg. 16(4), 462–466 (2002). PMID:12132024
Treska, V., Kocova, J., Boudova, L., Neprasova, P., Topolcan, O., Pecen, L., Tonar, Z.: Inflammation in the wall of abdominal aortic aneurysm and its role in the symptomatology of aneurysm. Cytokines Cell Mol. Ther. 7(3), 91–97 (2002). PMID:12850808
Bobryshev, Y.V., Lord, R.S., Parsson, H.: Immunophenotypic analysis of the aortic aneurysm wall suggests that vascular dendritic cells are involved in immune responses. Cardiovasc. Surg. 6(3), 240–249 (1998). PMID:9705095
Curci, J.A., Liao, S., Huffman, M.D., Shapiro, S.D., Thompson, R.W.: Expression and localization of macrophage elastase (matrix metalloproteinase-12) in abdominal aortic aneurysms. J. Clin. Invest. 102(11), 1900–1910 (1998). PMID:9835614
Anidjar, S., Dobrin, P.B., Eichorst, M., Graham, G.P., Chejfec, G.: Correlation of inflammatory infiltrate with the enlargement of experimental aortic aneurysms. J. Vasc. Surg. 16(2), 139–147 (1992). PMID:1386635
Koch, A.E., Haines, G.K., Rizzo, R.J., Radosevich, J.A., Pope, R.M., Robinson, P.G., Pearce, W.H.: Human abdominal aortic aneurysms. Immunophenotypic analysis suggesting an immune-mediated response. Am. J. Pathol. 137(5), 1199–1213 (1990). PMID:1700620
Schlatmann, T.J., Becker, A.E.: Pathogenesis of dissecting aneurysm of aorta. Comparative histopathologic study of significance of medial changes. Am. J. Cardiol. 39(1), 21–26 (1977). PMID:831424
Marsalese, D.L., Moodie, D.S., Lytle, B.W., Cosgrove, D.M., Ratliff, N.B., Goormastic, M., Kovacs, A.: Cystic medial necrosis of the aorta in patients without Marfan’s syndrome: surgical outcome and long-term follow-up. J. Am. Coll. Cardiol. 16(1), 68–73 (1990). PMID:2358606
Coady, M.A., Rizzo, J.A., Goldstein, L.J., Elefteriades, J.A.: Natural history, pathogenesis, and etiology of thoracic aortic aneurysms and dissections. Cardiol. Clin. 17(4), 615–635 (1999). vii PMID:10589336
Dietz, H.C., Cutting, G.R., Pyeritz, R.E., Maslen, C.L., Sakai, L.Y., Corson, G.M., Puffenberger, E.G., Hamosh, A., Nanthakumar, E.J., Curristin, S.M., et al.: Marfan syndrome caused by a recurrent de novo missense mutation in the fibrillin gene. Nature 352(6333), 337–339 (1991). PMID:1852208
Loeys, B.L., Schwarze, U., Holm, T., Callewaert, B.L., Thomas, G.H., Pannu, H., De Backer, J.F., Oswald, G.L., Symoens, S., Manouvrier, S., Roberts, A.E., Faravelli, F., Greco, M.A., Pyeritz, R.E., Milewicz, D.M., Coucke, P.J., Cameron, D.E., Braverman, A.C., Byers, P.H., De Paepe, A.M., Dietz, H.C.: Aneurysm syndromes caused by mutations in the TGF-beta receptor. N. Engl. J. Med. 355(8), 788–798 (2006). PMID:16928994
Narcisi, P., Richards, A.J., Ferguson, S.D., Pope, F.M.: A family with Ehlers-Danlos syndrome type III/articular hypermobility syndrome has a glycine 637 to serine substitution in type III collagen. Hum. Mol. Genet. 3(9), 1617–1620 (1994). PMID:7833919
Zhu, L., Vranckx, R., Khau Van Kien, P., Lalande, A., Boisset, N., Mathieu, F., Wegman, M., Glancy, L., Gasc, J.M., Brunotte, F., Bruneval, P., Wolf, J.E., Michel, J.B., Jeunemaitre, X.: Mutations in myosin heavy chain 11 cause a syndrome associating thoracic aortic aneurysm/aortic dissection and patent ductus arteriosus. Nat. Genet. 38(3), 343–349 (2006). PMID:16444274
Pannu, H., Tran-Fadulu, V., Papke, C.L., Scherer, S., Liu, Y., Presley, C., Guo, D., Estrera, A.L., Safi, H.J., Brasier, A.R., Vick, G.W., Marian, A.J., Raman, C.S., Buja, L.M., Milewicz, D.M.: MYH11 mutations result in a distinct vascular pathology driven by insulin-like growth factor 1 and angiotensin II. Hum. Mol. Genet. 16(20), 2453–2462 (2007). PMID:17666408
Edwards, W.D., Leaf, D.S., Edwards, J.E.: Dissecting aortic aneurysm associated with congenital bicuspid aortic valve. Circulation 57(5), 1022–1025 (1978). PMID:639201
Fedak, P.W., Verma, S., David, T.E., Leask, R.L., Weisel, R.D., Butany, J.: Clinical and pathophysiological implications of a bicuspid aortic valve. Circulation 106(8), 900–904 (2002). PMID:12186790
Gleason, T.G.: Heritable disorders predisposing to aortic dissection. Semin. Thorac. Cardiovasc. Surg. 17(3), 274–281 (2005). PMID:16253833
Roberts, W.C.: The congenitally bicuspid aortic valve. A study of 85 autopsy cases. Am. J. Cardiol. 26(1), 72–83 (1970). PMID:5427836
Ward, C.: Clinical significance of the bicuspid aortic valve. Heart 83(1), 81–85 (2000). PMID:10618341
Milewicz, D.M., Guo, D.C., Tran-Fadulu, V., Lafont, A.L., Papke, C.L., Inamoto, S., Kwartler, C.S., Pannu, H.: Genetic basis of thoracic aortic aneurysms and dissections: focus on smooth muscle cell contractile dysfunction. Annu. Rev. Genomics Hum. Genet. 9, 283–302 (2008). PMID:18544034
Niitsuya, M., Kuwao, S., Sato, B., Kameya, T., Kikawada, R.: Histopathological study of aortic wall dissection. J. Cardiol. 21(2), 445–452 (1991). PMID:1841931
Niwa, K., Perloff, J.K., Bhuta, S.M., Laks, H., Drinkwater, D.C., Child, J.S., Miner, P.D.: Structural abnormalities of great arterial walls in congenital heart disease: light and electron microscopic analyses. Circulation 103(3), 393–400 (2001). PMID:11157691
Ramirez, F., Rifkin, D.B.: Cell signaling events: a view from the matrix. Matrix Biol. 22(2), 101–107 (2003). PMID:12782137
Reinhardt, D.P., Gambee, J.E., Ono, R.N., Bachinger, H.P., Sakai, L.Y.: Initial steps in assembly of microfibrils. Formation of disulfide-cross-linked multimers containing fibrillin-1. J. Biol. Chem. 275(3), 2205–2210 (2000). PMID:10636927
Gleizes, P.E., Beavis, R.C., Mazzieri, R., Shen, B., Rifkin, D.B.: Identification and characterization of an eight-cysteine repeat of the latent transforming growth factor-beta binding protein-1 that mediates bonding to the latent transforming growth factor-beta1. J. Biol. Chem. 271(47), 29891–29896 (1996). PMID:8939931
Saharinen, J., Taipale, J., Keski-Oja, J.: Association of the small latent transforming growth factor-beta with an eight cysteine repeat of its binding protein LTBP-1. EMBO J. 15(2), 245–253 (1996). PMID:8617200
D’Arrigo, C., Burl, S., Withers, A.P., Dobson, H., Black, C., Boxer, M.: TGF-beta1 binding protein-like modules of fibrillin-1 and -2 mediate integrin-dependent cell adhesion. Connect. Tissue Res. 37(1–2), 29–51 (1998). PMID:9643645
Pfaff, M., Reinhardt, D.P., Sakai, L.Y., Timpl, R.: Cell adhesion and integrin binding to recombinant human fibrillin-1. FEBS Lett. 384(3), 247–250 (1996). PMID:8617364
Sakamoto, H., Broekelmann, T., Cheresh, D.A., Ramirez, F., Rosenbloom, J., Mecham, R.P.: Cell-type specific recognition of RGD- and non-RGD-containing cell binding domains in fibrillin-1. J. Biol. Chem. 271(9), 4916–4922 (1996). PMID:8617764
Kielty, C.M., Baldock, C., Lee, D., Rock, M.J., Ashworth, J.L., Shuttleworth, C.A.: Fibrillin: from microfibril assembly to biomechanical function. Philos. Trans. R. Soc. Lond. B Biol. Sci. 357(1418), 207–217 (2002). PMID:11911778
Judge, D.P., Biery, N.J., Keene, D.R., Geubtner, J., Myers, L., Huso, D.L., Sakai, L.Y., Dietz, H.C.: Evidence for a critical contribution of haploinsufficiency in the complex pathogenesis of Marfan syndrome. J. Clin. Invest. 114(2), 172–181 (2004). PMID:15254584
Habashi, J.P., Judge, D.P., Holm, T.M., Cohn, R.D., Loeys, B.L., Cooper, T.K., Myers, L., Klein, E.C., Liu, G., Calvi, C., Podowski, M., Neptune, E.R., Halushka, M.K., Bedja, D., Gabrielson, K., Rifkin, D.B., Carta, L., Ramirez, F., Huso, D.L., Dietz, H.C.: Losartan, an AT1 antagonist, prevents aortic aneurysm in a mouse model of Marfan syndrome. Science 312(5770), 117–121 (2006). PMID:16601194
Carta, L., Wagenseil, J.E., Knutsen, R.H., Mariko, B., Faury, G., Davis, E.C., Starcher, B., Mecham, R.P., Ramirez, F.: Discrete contributions of elastic fiber components to arterial development and mechanical compliance. Arterioscler. Thromb. Vasc. Biol. 29(12), 2083–2089 (2009). PMID:19850904
Brooke, B.S., Habashi, J.P., Judge, D.P., Patel, N., Loeys, B., Dietz 3rd, H.C.: Angiotensin II blockade and aortic-root dilation in Marfan’s syndrome. N. Engl. J. Med. 358(26), 2787–2795 (2008). PMID:18579813
Kalluri, R., Han, Y.: Targeting TGF-beta and the extracellular matrix in Marfan’s syndrome. Dev. Cell 15(1), 1–2 (2008). PMID:18606132
Sonesson, B., Hansen, F., Lanne, T.: Abnormal mechanical properties of the aorta in Marfan’s syndrome. Eur J. Vasc. Surg. 8(5), 595–601 (1994). PMID:7813727
Eberth, J.F., Taucer, A.I., Wilson, E., Humphrey, J.D.: Mechanics of carotid arteries in a mouse model of Marfan syndrome. Ann. Biomed. Eng. 37(6), 1093–1104 (2009). PMID:19350391
Loeys, B.L., Chen, J., Neptune, E.R., Judge, D.P., Podowski, M., Holm, T., Meyers, J., Leitch, C.C., Katsanis, N., Sharifi, N., Xu, F.L., Myers, L.A., Spevak, P.J., Cameron, D.E., De Backer, J., Hellemans, J., Chen, Y., Davis, E.C., Webb, C.L., Kress, W., Coucke, P., Rifkin, D.B., De Paepe, A.M., Dietz, H.C.: A syndrome of altered cardiovascular, craniofacial, neurocognitive and skeletal development caused by mutations in TGFBR1 or TGFBR2. Nat. Genet. 37(3), 275–281 (2005). PMID:15731757
Maleszewski, J.J., Miller, D.V., Lu, J., Dietz, H.C., Halushka, M.K.: Histopathologic findings in ascending aortas from individuals with Loeys-Dietz syndrome (LDS). Am. J. Surg. Pathol. 33(2), 194–201 (2009). PMID:18852674
Wahab, N.A., Weston, B.S., Mason, R.M.: Modulation of the TGFbeta/Smad signaling pathway in mesangial cells by CTGF/CCN2. Exp. Cell Res. 307(2), 305–314 (2005). PMID:15950619
Ruiz-Ortega, M., Rodriguez-Vita, J., Sanchez-Lopez, E., Carvajal, G., Egido, J.: TGF-beta signaling in vascular fibrosis. Cardiovasc. Res. 74(2), 196–206 (2007). PMID:17376414
Beighton, P., De Paepe, A., Steinmann, B., Tsipouras, P., Wenstrup, R.J.: Ehlers-Danlos syndromes: revised nosology, Villefranche, 1997. Ehlers-Danlos National Foundation (USA) and Ehlers-Danlos Support Group (UK). Am. J. Med. Genet. 77(1):31–7 (1998) PMID:9557891
Pope, F.M., Narcisi, P., Nicholls, A.C., Germaine, D., Pals, G., Richards, A.J.: COL3A1 mutations cause variable clinical phenotypes including acrogeria and vascular rupture. Br. J. Dermatol. 135(2), 163–181 (1996). PMID:8881656
Borck, G., Beighton, P., Wilhelm, C., Kohlhase, J., Kubisch, C.: Arterial rupture in classic Ehlers-Danlos syndrome with COL5A1 mutation. Am. J. Med. Genet. A 152A(8), 2090–2093 (2010). PMID:20635400
Burke, J.M., Balian, G., Ross, R., Bornstein, P.: Synthesis of types I and III procollagen and collagen by monkey aortic smooth muscle cells in vitro. Biochemistry 16(14), 3243–3249 (1977). PMID:407926
McCullagh, K.A., Balian, G.: Collagen characterisation and cell transformation in human atherosclerosis. Nature 258(5530), 73–75 (1975). PMID:1186882
Smith, L.B., Hadoke, P.W., Dyer, E., Denvir, M.A., Brownstein, D., Miller, E., Nelson, N., Wells, S., Cheeseman, M., Greenfield, A.: Haploinsufficiency of the murine Col3a1 locus causes aortic dissection: a novel model of the vascular type of Ehlers Danlos Syndrome. Cardiovasc. Res. 90, 182–190 (2010) PMID:21071432
McCullagh, K.G., Duance, V.C., Bishop, K.A.: The distribution of collagen types I, III and V (AB) in normal and atherosclerotic human aorta. J. Pathol. 130(1), 45–55 (1980). PMID:6991657
Sadakata, R., Hatamochi, A., Kodama, K., Kaga, A., Yamaguchi, T., Soma, T., Usui, Y., Nagata, M., Ohtake, A., Hagiwara, K., Kanazawa, M.: Ehlers-Danlos syndrome type IV, vascular type, which demonstrated a novel point mutation in the COL3A1 gene. Intern. Med. 49(16), 1797–1800 (2010). PMID:20720362
Kim, Y., Peyrol, S., So, C.K., Boyd, C.D., Csiszar, K.: Coexpression of the lysyl oxidase-like gene (LOXL) and the gene encoding type III procollagen in induced liver fibrosis. J. Cell Biochem. 72(2), 181–188 (1999). PMID:10022501
Sharma, R., Kramer, J.A., Krawetz, S.A.: Lysyl oxidase, cellular senescence and tumor suppression. Biosci. Rep. 17(4), 409–414 (1997). PMID:9367056
Sommer, P., Gleyzal, C., Raccurt, M., Delbourg, M., Serrar, M., Joazeiro, P., Peyrol, S., Kagan, H., Trackman, P.C., Grimaud, J.A.: Transient expression of lysyl oxidase by liver myofibroblasts in murine schistosomiasis. Lab. Invest. 69(4), 460–470 (1993). PMID:7901452
Rucker, R.B., Kosonen, T., Clegg, M.S., Mitchell, A.E., Rucker, B.R., Uriu-Hare, J.Y., Keen, C.L.: Copper, lysyl oxidase, and extracellular matrix protein cross-linking. Am. J. Clin. Nutr. 67(5 Suppl), 996S–1002S (1998). PMID:9587142
Peltonen, L., Kuivaniemi, H., Palotie, A., Horn, N., Kaitila, I., Kivirikko, K.I.: Alterations in copper and collagen metabolism in the Menkes syndrome and a new subtype of the Ehlers-Danlos syndrome. Biochemistry 22(26), 6156–6163 (1983). PMID:6140952
Maki, J.M., Rasanen, J., Tikkanen, H., Sormunen, R., Makikallio, K., Kivirikko, K.I., Soininen, R.: Inactivation of the lysyl oxidase gene Lox leads to aortic aneurysms, cardiovascular dysfunction, and perinatal death in mice. Circulation 106(19), 2503–2509 (2002). PMID:12417550
Jones, J.A., Spinale, F.G., Ikonomidis, J.S.: Transforming growth factor-beta signaling in thoracic aortic aneurysm development: a paradox in pathogenesis. J. Vasc. Res. 46(2), 119–137 (2009). PMID:18765947
Sun, Y.L., Luo, Z.P., Fertala, A., An, K.N.: Direct quantification of the flexibility of type I collagen monomer. Biochem. Biophys. Res. Commun. 295(2), 382–386 (2002). PMID:12150960
Januzzi, J.L., Isselbacher, E.M., Fattori, R., Cooper, J.V., Smith, D.E., Fang, J., Eagle, K.A., Mehta, R.H., Nienaber, C.A., Pape, L.A.: Characterizing the young patient with aortic dissection: results from the International Registry of Aortic Dissection (IRAD). J. Am. Coll. Cardiol. 43(4), 665–669 (2004). PMID:14975480
Keane, M.G., Wiegers, S.E., Plappert, T., Pochettino, A., Bavaria, J.E., Sutton, M.G.: Bicuspid aortic valves are associated with aortic dilatation out of proportion to coexistent valvular lesions. Circulation 102(19 Suppl 3), III35–III39 (2000). PMID:11082359
Nistri, S., Grande-Allen, J., Noale, M., Basso, C., Siviero, P., Maggi, S., Crepaldi, G., Thiene, G.: Aortic elasticity and size in bicuspid aortic valve syndrome. Eur. Heart J. 29(4), 472–479 (2008). PMID:18096569
Nistri, S., Sorbo, M.D., Marin, M., Palisi, M., Scognamiglio, R., Thiene, G.: Aortic root dilatation in young men with normally functioning bicuspid aortic valves. Heart 82(1), 19–22 (1999). PMID:10377302
Cripe, L., Andelfinger, G., Martin, L.J., Shooner, K., Benson, D.W.: Bicuspid aortic valve is heritable. J. Am. Coll. Cardiol. 44(1), 138–143 (2004). PMID:15234422
Martin, L.J., Ramachandran, V., Cripe, L.H., Hinton, R.B., Andelfinger, G., Tabangin, M., Shooner, K., Keddache, M., Benson, D.W.: Evidence in favor of linkage to human chromosomal regions 18q, 5q and 13q for bicuspid aortic valve and associated cardiovascular malformations. Hum. Genet. 121(2), 275–284 (2007). PMID:17203300
Garg, V., Muth, A.N., Ransom, J.F., Schluterman, M.K., Barnes, R., King, I.N., Grossfeld, P.D., Srivastava, D.: Mutations in NOTCH1 cause aortic valve disease. Nature 437(7056), 270–274 (2005). PMID:16025100
Phillippi, J.A., Eskay, M.A., Kubala, A.A., Pitt, B.R., Gleason, T.G.: Altered oxidative stress responses and increased type I collagen expression in bicuspid aortic valve patients. Ann. Thorac. Surg. 90(6), 1893–1898 (2010). PMID:21095332
Phillippi, J.A., Klyachko, E.A., Kenny, J.P., Eskay, M.A., Gorman, R.C., Gleason, T.G.: Basal and oxidative stress-induced expression of metallothionein is decreased in ascending aortic aneurysms of bicuspid aortic valve patients. Circulation 119(18), 2498–2506 (2009). PMID:ISI:000266011500011
Ejiri, J., Inoue, N., Tsukube, T., Munezane, T., Hino, Y., Kobayashi, S., Hirata, K., Kawashima, S., Imajoh-Ohmi, S., Hayashi, Y., Yokozaki, H., Okita, Y., Yokoyama, M.: Oxidative stress in the pathogenesis of thoracic aortic aneurysm: protective role of statin and angiotensin II type 1 receptor blocker. Cardiovasc. Res. 59(4), 988–996 (2003). PMID:14553839
Fiorillo, C., Becatti, M., Attanasio, M., Lucarini, L., Nassi, N., Evangelisti, L., Porciani, M.C., Nassi, P., Gensini, G.F., Abbate, R., Pepe, G.: Evidence for oxidative stress in plasma of patients with Marfan syndrome. Int. J. Cardiol. 145, 544–546 (2010) PMID:20537738
Robbins, A.H., McRee, D.E., Williamson, M., Collett, S.A., Xuong, N.H., Furey, W.F., Wang, B.C., Stout, C.D.: Refined crystal structure of Cd, Zn metallothionein at 2.0 A resolution. J. Mol. Biol. 221(4), 1269–1293 (1991). PMID:1942051
Arseniev, A., Schultze, P., Worgotter, E., Braun, W., Wagner, G., Vasak, M., Kagi, J.H., Wuthrich, K.: Three-dimensional structure of rabbit liver [Cd7] metallothionein-2a in aqueous solution determined by nuclear magnetic resonance. J. Mol. Biol. 201(3), 637–657 (1988). PMID:3418714
Pitt, B.R., Schwarz, M., Woo, E.S., Yee, E., Wasserloos, K., Tran, S., Weng, W., Mannix, R.J., Watkins, S.A., Tyurina, Y.Y., Tyurin, V.A., Kagan, V.E., Lazo, J.S.: Overexpression of metallothionein decreases sensitivity of pulmonary endothelial cells to oxidant injury. Am. J. Physiol. 273(4 Pt 1), L856–L865 (1997). PMID:9357862
Abel, J., de Ruiter, N.: Inhibition of hydroxyl-radical-generated DNA degradation by metallothionein. Toxicol. Lett. 47(2), 191–196 (1989). PMID:2545017
Thornally, P., Vasak, M.: Possible role for metallothionein in protections against radiation-induced oxidative stress. Lineteics and mechanism of its reaction with superoxide hydroxyl radicals. Biochem. Biophys. Acta. 827, 36–44 (1985)
Oh, S.H., Deagen, J.T., Whanger, P.D., Weswig, P.H.: Biological function of metallothionein. V. Its induction in rats by various stresses. Am. J. Physiol. 234(3), E282–E285 (1978). PMID:629343
Klaassen, C.D., Liu, J.: Metallothionein transgenic and knock-out mouse models in the study of cadmium toxicity. J. Toxicol. Sci. 23(Suppl 2), 97–102 (1998). PMID:9760441
Fang, C.X., Doser, T.A., Yang, X., Sreejayan, N., Ren, J.: Metallothionein antagonizes aging-induced cardiac contractile dysfunction: role of PTP1B, insulin receptor tyrosine phosphorylation and Akt. Aging Cell 5(2), 177–185 (2006). PMID:16626396
Feng, W., Wang, Y., Cai, L., Kang, Y.J.: Metallothionein rescues hypoxia-inducible factor-1 transcriptional activity in cardiomyocytes under diabetic conditions. Biochem. Biophys. Res. Commun. 360(1), 286–289 (2007). PMID:17586470
Surazynski, A., Donald, S.P., Cooper, S.K., Whiteside, M.A., Salnikow, K., Liu, Y., Phang, J.M.: Extracellular matrix and HIF-1 signaling: the role of prolidase. Int. J. Cancer 122(6), 1435–1440 (2008). PMID:17999410
Kurban, G., Duplan, E., Ramlal, N., Hudon, V., Sado, Y., Ninomiya, Y., Pause, A.: Collagen matrix assembly is driven by the interaction of von Hippel-Lindau tumor suppressor protein with hydroxylated collagen IV alpha 2. Oncogene 27(7), 1004–1012 (2008). PMID:17700531
Elstner, A., Holtkamp, N., von Deimling, A.: Involvement of Hif-1 in desferrioxamine-induced invasion of glioblastoma cells. Clin. Exp. Metastasis 24(1), 57–66 (2007). PMID:17357815
Norman, J.T., Orphanides, C., Garcia, P., Fine, L.G.: Hypoxia-induced changes in extracellular matrix metabolism in renal cells. Exp. Nephrol. 7(5–6), 463–469 (1999). PMID:10559644
Kivela, R., Kyrolainen, H., Selanne, H., Komi, P.V., Kainulainen, H., Vihko, V.: A single bout of exercise with high mechanical loading induces the expression of Cyr61/CCN1 and CTGF/CCN2 in human skeletal muscle. J. Appl. Physiol. 103(4), 1395–1401 (2007). PMID:17673559
Pereira, L., Lee, S.Y., Gayraud, B., Andrikopoulos, K., Shapiro, S.D., Bunton, T., Biery, N.J., Dietz, H.C., Sakai, L.Y., Ramirez, F.: Pathogenetic sequence for aneurysm revealed in mice underexpressing fibrillin-1. Proc Natl Acad Sci USA 96(7), 3819–3823 (1999). PMID:10097121
Yang, H.H., van Breemen, C., Chung, A.W.: Vasomotor dysfunction in the thoracic aorta of Marfan syndrome is associated with accumulation of oxidative stress. Vascul. Pharmacol. 52(1–2), 37–45 (2010). PMID:19879959
Radomski, A., Sawicki, G., Olson, D.M., Radomski, M.W.: The role of nitric oxide and metalloproteinases in the pathogenesis of hyperoxia-induced lung injury in newborn rats. Br. J. Pharmacol. 125(7), 1455–1462 (1998). PMID:9884073
Tyagi, S.C., Matsubara, L., Weber, K.T.: Direct extraction and estimation of collagenase(s) activity by zymography in microquantities of rat myocardium and uterus. Clin. Biochem. 26(3), 191–198 (1993). PMID:8330388
Steed, M.M., Tyagi, N., Sen, U., Schuschke, D.A., Joshua, I.G., Tyagi, S.C.: Functional consequences of the collagen/elastin switch in vascular remodeling in hyperhomocysteinemic wild-type, eNOS-/-, and iNOS-/- mice. Am. J. Physiol. Lung Cell. Mol. Physiol. 299(3), L301–L311 (2010). PMID:20581102
McCormick, M.L., Gavrila, D., Weintraub, N.L.: Role of oxidative stress in the pathogenesis of abdominal aortic aneurysms. Arterioscler. Thromb. Vasc. Biol. 27(3), 461–469 (2007). PMID:17218601
Gavazzi, G., Deffert, C., Trocme, C., Schappi, M., Herrmann, F.R., Krause, K.H.: NOX1 deficiency protects from aortic dissection in response to angiotensin II. Hypertension 50(1), 189–196 (2007). PMID:17502491
Thomas, M., Gavrila, D., McCormick, M.L., Miller Jr, F.J., Daugherty, A., Cassis, L.A., Dellsperger, K.C., Weintraub, N.L.: Deletion of p47phox attenuates angiotensin II-induced abdominal aortic aneurysm formation in apolipoprotein E-deficient mice. Circulation 114(5), 404–413 (2006). PMID:16864727
Hope, M.D., Hope, T.A., Meadows, A.K., Ordovas, K.G., Urbania, T.H., Alley, M.T., Higgins, C.B.: Bicuspid aortic valve: four-dimensional MR evaluation of ascending aortic systolic flow patterns. Radiology 255(1), 53–61 (2010). PMID:20308444
Bauer, M., Siniawski, H., Pasic, M., Schaumann, B., Hetzer, R.: Different hemodynamic stress of the ascending aorta wall in patients with bicuspid and tricuspid aortic valve. J. Card. Surg. 21(3), 218–220 (2006). PMID:16684044
Nkomo, V.T., Enriquez-Sarano, M., Ammash, N.M., Melton 3rd, L.J., Bailey, K.R., Desjardins, V., Horn, R.A., Tajik, A.J.: Bicuspid aortic valve associated with aortic dilatation: a community-based study. Arterioscler. Thromb. Vasc. Biol. 23(2), 351–356 (2003). PMID:12588783
Yasuda, H., Nakatani, S., Stugaard, M., Tsujita-Kuroda, Y., Bando, K., Kobayashi, J., Yamagishi, M., Kitakaze, M., Kitamura, S., Miyatake, K.: Failure to prevent progressive dilation of ascending aorta by aortic valve replacement in patients with bicuspid aortic valve: comparison with tricuspid aortic valve. Circulation 108(Suppl 1), II291–II294 (2003). PMID:12970248
Wang, X., LeMaire, S.A., Chen, L., Shen, Y.H., Gan, Y., Bartsch, H., Carter, S.A., Utama, B., Ou, H., Coselli, J.S., Wang, X.L.: Increased collagen deposition and elevated expression of connective tissue growth factor in human thoracic aortic dissection. Circulation 114(1 Suppl), I200–I205 (2006). PMID:16820572
Whittle, M.A., Hasleton, P.S., Anderson, J.C., Gibbs, A.C.: Collagen in dissecting aneurysms of the human thoracic aorta. Increased collagen content and decreased collagen concentration may be predisposing factors in dissecting aneurysms. Am. J. Cardiovasc. Pathol. 3(4), 311–319 (1990). PMID:2129573
Choudhury, N., Bouchot, O., Rouleau, L., Tremblay, D., Cartier, R., Butany, J., Mongrain, R., Leask, R.L.: Local mechanical and structural properties of healthy and diseased human ascending aorta tissue. Cardiovasc. Pathol. 18(2), 83–91 (2009). PMID:18402840
Absi, T.S., Sundt 3rd, T.M., Tung, W.S., Moon, M., Lee, J.K., Damiano Jr, R.R., Thompson, R.W.: Altered patterns of gene expression distinguishing ascending aortic aneurysms from abdominal aortic aneurysms: complementary DNA expression profiling in the molecular characterization of aortic disease. J. Thorac. Cardiovasc. Surg. 126(2), 344–357 (2003). discission 357 PMID:12928630
Daugherty, A., Cassis, L.A.: Mouse models of abdominal aortic aneurysms. Arterioscler. Thromb. Vasc. Biol. 24(3), 429–434 (2004). PMID:14739119
Kadoglou, N.P., Liapis, C.D.: Matrix metalloproteinases: contribution to pathogenesis, diagnosis, surveillance and treatment of abdominal aortic aneurysms. Curr. Med. Res. Opin. 20(4), 419–432 (2004). PMID:15119978
Fernandez, B., Duran, A.C., Fernandez-Gallego, T., Fernandez, M.C., Such, M., Arque, J.M., Sans-Coma, V.: Bicuspid aortic valves with different spatial orientations of the leaflets are distinct etiological entities. J. Am. Coll. Cardiol. 54(24), 2312–2318 (2009). PMID:19958967
Lee, T.C., Zhao, Y.D., Courtman, D.W., Stewart, D.J.: Abnormal aortic valve development in mice lacking endothelial nitric oxide synthase. Circulation 101(20), 2345–2348 (2000). PMID:10821808
Atli, F.H., Manduz, S., Katrancioglu, N., Ozum, U., Disli, O.M., Atahan, E., Ozdemir, O., Dogan, K., Berkan, O.: eNOS G894T polymorphism and abdominal aortic aneurysms. Angiology 61, 125–130 (2010) PMID:19638352
Fatini, C., Sofi, F., Sticchi, E., Bolli, P., Sestini, I., Falciani, M., Azas, L., Pratesi, G.: eNOS G894T polymorphism as a mild predisposing factor for abdominal aortic aneurysm. J. Vasc. Surg. 42(3), 415–419 (2005). PMID:16171581
Sandrim, V.C.: Regarding “eNOS G894T polymorphism as a mild predisposing factor for abdominal aortic aneurysm”. J. Vasc. Surg. 43(5), 1079 (2006). PMID:16678714
Ko, N.U., Rajendran, P., Kim, H., Rutkowski, M., Pawlikowska, L., Kwok, P.Y., Higashida, R.T., Lawton, M.T., Smith, W.S., Zaroff, J.G., Young, W.L.: Endothelial nitric oxide synthase polymorphism (-786T->C) and increased risk of angiographic vasospasm after aneurysmal subarachnoid hemorrhage. Stroke 39(4), 1103–1108 (2008). PMID:18309169
Krischek, B., Kasuya, H., Akagawa, H., Tajima, A., Narita, A., Onda, H., Hori, T., Inoue, I.: Using endothelial nitric oxide synthase gene polymorphisms to identify intracranial aneurysms more prone to rupture in Japanese patients. J. Neurosurg. 105(5), 717–722 (2006). PMID:17121133
Ozum, U., Bolat, N., Gul, E., Ozdemir, O.: Endothelial nitric oxide synthase gene [G894T] polymorphism as a possible risk factor in aneurysmal subarachnoid haemorrhage. Acta Neurochir. (Wien) 150(1), 57–61 (2008). discussion 62 PMID:18046500
Starke, R.M., Kim, G.H., Komotar, R.J., Hickman, Z.L., Black, E.M., Rosales, M.B., Kellner, C.P., Hahn, D.K., Otten, M.L., Edwards, J., Wang, T., Russo, J.J., Mayer, S.A., Connolly Jr, E.S.: Endothelial nitric oxide synthase gene single-nucleotide polymorphism predicts cerebral vasospasm after aneurysmal subarachnoid hemorrhage. J. Cereb. Blood Flow Metab. 28(6), 1204–1211 (2008). PMID:18319732
Tamura, T., Jamous, M.A., Kitazato, K.T., Yagi, K., Tada, Y., Uno, M., Nagahiro, S.: Endothelial damage due to impaired nitric oxide bioavailability triggers cerebral aneurysm formation in female rats. J. Hypertens. 27(6), 1284–1292 (2009). PMID:19307983
Aicher, D., Urbich, C., Zeiher, A., Dimmeler, S., Schafers, H.J.: Endothelial nitric oxide synthase in bicuspid aortic valve disease. Ann. Thorac. Surg. 83(4), 1290–1294 (2007). PMID:17383329
Lee, J.K., Borhani, M., Ennis, T.L., Upchurch Jr, G.R., Thompson, R.W.: Experimental abdominal aortic aneurysms in mice lacking expression of inducible nitric oxide synthase. Arterioscler. Thromb. Vasc. Biol. 21(9), 1393–1401 (2001). PMID:11557662
Pimiento, J.M., Maloney, S.P., Tang, P.C., Muto, A., Westvik, T.S., Fitzgerald, T.N., Fancher, T.T., Tellides, G., Dardik, A.: Endothelial nitric oxide synthase stimulates aneurysm growth in aged mice. J. Vasc. Res. 45(3), 251–258 (2008). PMID:18182824
Hultgardh-Nilsson, A., Lovdahl, C., Blomgren, K., Kallin, B., Thyberg, J.: Expression of phenotype- and proliferation-related genes in rat aortic smooth muscle cells in rimary culture. Cardiovasc. Res. 34(2), 418–430 (1997). PMID:9205557
Thyberg, J.: Differentiated properties and proliferation of arterial smooth muscle cells in culture. Int. Rev. Cytol. 169, 183–265 (1996). PMID:8843655
Rensen, S.S., Doevendans, P.A., van Eys, G.J.: Regulation and characteristics of vascular smooth muscle cell phenotypic diversity. Neth. Heart J. 15(3), 100–108 (2007). PMID:17612668
Bunton, T.E., Biery, N.J., Myers, L., Gayraud, B., Ramirez, F., Dietz, H.C.: Phenotypic alteration of vascular smooth muscle cells precedes elastolysis in a mouse model of Marfan syndrome. Circ. Res. 88(1), 37–43 (2001). PMID:11139471
Guo, D.C., Pannu, H., Tran-Fadulu, V., Papke, C.L., Yu, R.K., Avidan, N., Bourgeois, S., Estrera, A.L., Safi, H.J., Sparks, E., Amor, D., Ades, L., McConnell, V., Willoughby, C.E., Abuelo, D., Willing, M., Lewis, R.A., Kim, D.H., Scherer, S., Tung, P.P., Ahn, C., Buja, L.M., Raman, C.S., Shete, S.S., Milewicz, D.M.: Mutations in smooth muscle alpha-actin (ACTA2) lead to thoracic aortic aneurysms and dissections. Nat. Genet. 39(12), 1488–1493 (2007). PMID:17994018
Morisaki, H., Akutsu, K., Ogino, H., Kondo, N., Yamanaka, I., Tsutsumi, Y., Yoshimuta, T., Okajima, T., Matsuda, H., Minatoya, K., Sasaki, H., Tanaka, H., Ishibashi-Ueda, H., Morisaki, T.: Mutation of ACTA2 gene as an important cause of familial and nonfamilial nonsyndromatic thoracic aortic aneurysm and/or dissection (TAAD). Hum. Mutat. 30(10), 1406–1411 (2009). PMID:19639654
Phillippi, J.A., Eskay, M.A., Kubala, A.A., Gleason, T.G.: Smooth Muscle Cell Phenotype Alterations in Patients With Bicuspid Aortic Valve. American Society for Cell Biology, Philadelphia (2010)
Phillippi, J.A., Kubala, A.A., Eskay, M.A., Chew, D.W., Gaitan, D., Hempel, J., Vorp, D.A., Watkins, S.C., Gleason, T.G.: Disrupted Collagen Homeostasis in Thoracic Aortic Aneurysms in Patients with Bicuspid Aortic Valve. International Society of Applied Cardiovascular Biology, Cambridge (2010)
Pasta, S., Phillippi, J.A., Gleason, T.G., Vorp, D.A.: Dissection properties of aneurysmal and nonaneurysmal human ascending thoracic aorta: preliminary results. In: ASME Summer Bioengineering Conference, Naples, FL (2010)
Pasta, S., Phillippi, J.A., Watkins, S.C., Gleason, T.G., Vorp, D.A.: The effect of aneurysm on the delamination strength in human ascending thoracic aorta. Biomedical Engineering Society Annual Meeting, Austin, TX (2010)
Pichamuthu, J.E., Phillippi, J.A., Gleason, T.G., Vorp, D.A.: Ascending aortic aneurysm biomechanical properties are variable depending on aortic valve morphology. Aortic Symposium, NY (2010)
Pichamuthu, J.E., Phillippi, J.A., Gleason, T.G., Vorp, D.A.: Association of wall strength of ascending thoracic aneurysms with different aortic valve morphologies. Biomedical Engineering Society, Austin, TX (2010)
Hayward, C., Brock, D.J.: Fibrillin-1 mutations in Marfan syndrome and other type-1 fibrillinopathies. Hum. Mutat. 10(6), 415–423 (1997). PMID:9401003
Di Martino, E., Mantero, S., Inzoli, F., Melissano, G., Astore, D., Chiesa, R., Fumero, R.: Biomechanics of abdominal aortic aneurysm in the presence of endoluminal thrombus: experimental characterisation and structural static computational analysis. Eur. J. Vasc. Endovasc. Surg. 15(4), 290–299 (1998). PMID:9610340
Raghavan, M.L., Vorp, D.A., Federle, M.P., Makaroun, M.S., Webster, M.W.: Wall stress distribution on three-dimensionally reconstructed models of human abdominal aortic aneurysm. J. Vasc. Surg. 31(4), 760–769 (2000). PMID:10753284
Van de Geest, J.P., Di Martino, E.S., Bohra, A., Makaroun, M.S., Vorp, D.A.: A biomechanics-based rupture potential index for abdominal aortic aneurysm risk assessment: demonstrative application. Ann. N. Y. Acad. Sci. 1085, 11–21 (2006). PMID:17182918
Vorp, D.A.: Biomechanics of abdominal aortic aneurysm. J. Biomech. 40(9), 1887–1902 (2007). PMID:17254589
Xenos, M., Alemu, Y., Zamfir, D., Einav, S., Ricotta, J.J., Labropoulos, N., Tassiopoulos, A., Bluestein, D.: The effect of angulation in abdominal aortic aneurysms: fluid-structure interaction simulations of idealized geometries. Med. Biol. Eng. Comput. 48, 1175–1190 (2010) PMID:21088917 DOI 10.1007/s11517-010-0714-y
Sheidaei, A., Hunley, S.C., Zeinali-Davarani, S., Raguin, L.G., Baek, S.: Simulation of abdominal aortic aneurysm growth with updating hemodynamic loads using a realistic geometry. Med. Eng. Phys. 33(1), 80–88 (2011) PMID:20961796
Dobrin, P.B.: Pathophysiology and pathogenesis of aortic aneurysms. Current concepts. Surg. Clin. North Am. 69(4), 687–703 (1989). PMID:2665139
Sumner, D.S., Hokanson, D.E., Strandness Jr, D.E.: Stress-strain characteristics and collagen-elastin content of abdominal aortic aneurysms. Surg. Gynecol. Obstet. 130(3), 459–466 (1970). PMID:5413429
Sakalihasan, N., Heyeres, A., Nusgens, B.V., Limet, R., Lapiere, C.M.: Modifications of the extracellular-matrix of aneurysmal abdominal aortas as a function of their size. Eur. J. Vasc. Surg. 7(6), 633–637 (1993). PMID:ISI:A1993MG43300007
Hunter, G.C., Leong, S.C., Yu, G.S., McIntyre, K.E., Bernhard, V.M.: Aortic blebs: possible site of aneurysm rupture. J. Vasc. Surg. 10(1), 93–99 (1989). PMID:2746804
Hunter, G.C., Smyth, S.H., Aguirre, M.L., Baxter, B.T., Bull, D.A., King, D.D., Wang, Y.P., Hall, K.A., Putnam, C.W.: Incidence and histologic characteristics of blebs in patients with abdominal aortic aneurysms. J. Vasc. Surg. 24(1), 93–101 (1996). PMID:8691533
Kapadia, S.R., Oral, H., Lee, J., Nakano, M., Taffet, G.E., Mann, D.L.: Hemodynamic regulation of tumor necrosis factor-alpha gene and protein expression in adult feline myocardium. Circ. Res. 81(2), 187–195 (1997). PMID:9242179
Leung, D.Y., Glagov, S., Mathews, M.B.: Cyclic stretching stimulates synthesis of matrix components by arterial smooth muscle cells in vitro. Science 191(4226), 475–477 (1976). PMID:128820
Sumpio, B.E., Banes, A.J., Link, G.W., Iba, T.: Modulation of endothelial cell phenotype by cyclic stretch: inhibition of collagen production. J. Surg. Res. 48(5), 415–420 (1990). PMID:2352417
Howard, P.S., Kucich, U., Taliwal, R., Korostoff, J.M.: Mechanical forces alter extracellular matrix synthesis by human periodontal ligament fibroblasts. J. Periodontal Res. 33(8), 500–508 (1998). PMID:9879524
Cotrufo, M., Della Corte, A., De Santo, L.S., Quarto, C., De Feo, M., Romano, G., Amarelli, C., Scardone, M., Di Meglio, F., Guerra, G., Scarano, M., Vitale, S., Castaldo, C., Montagnani, S.: Different patterns of extracellular matrix protein expression in the convexity and the concavity of the dilated aorta with bicuspid aortic valve: preliminary results. J. Thorac. Cardiovasc. Surg. 130(2), 504–511 (2005). PMID:16077420
McMillan, W.D., Tamarina, N.A., Cipollone, M., Johnson, D.A., Parker, M.A., Pearce, W.H.: Size matters: the relationship between MMP-9 expression and aortic diameter. Circulation 96(7), 2228–2232 (1997). PMID:ISI:A1997YA09800020
Speelman, L., Hellenthal, F.A., Pulinx, B., Bosboom, E.M.H., Breeuwer, M., van Sambeek, M.R., de Vosse, F.N.V., Jacobs, M.J., Wodzig, W.K.W.H., Schurink, G.W.H.: The influence of wall stress on AAA growth and biomarkers. Eur. J. Vasc. Endovasc. Surg. 39(4), 410–416 (2010). PMID:ISI:000277816300005
Kazi, M., Thyberg, J., Religa, P., Roy, J., Eriksson, P., Hedin, U., Swedenborg, J.: Influence of intraluminal thrombus on structural and cellular composition of abdominal aortic aneurysm wall. J. Vasc. Surg. 38(6), 1283–1292 (2003). PMID:14681629
Lee, R.T., Schoen, F.J., Loree, H.M., Lark, M.W., Libby, P.: Circumferential stress and matrix metalloproteinase 1 in human coronary atherosclerosis. Implications for plaque rupture. Arterioscler. Thromb. Vasc. Biol. 16(8), 1070–1073 (1996). PMID:8696948
Lendon, C.L., Davies, M.J., Born, G.V., Richardson, P.D.: Atherosclerotic plaque caps are locally weakened when macrophages density is increased. Atherosclerosis 87(1), 87–90 (1991). PMID:1872926
Yoshimura, K., Aoki, H., Ikeda, Y., Furutani, A., Hamano, K., Matsuzaki, M.: Identification of c-Jun N-terminal kinase as a therapeutic target for abdominal aortic aneurysm. Ann. N. Y. Acad. Sci. 1085, 403–406 (2006). PMID:17182964
Fernandez-Varo, G., Morales-Ruiz, M., Ros, J., Tugues, S., Munoz-Luque, J., Casals, G., Arroyo, V., Rodes, J., Jimenez, W.: Impaired extracellular matrix degradation in aortic vessels of cirrhotic rats. J. Hepatol. 46(3), 440–446 (2007). PMID:17156884
Gong, L.M., Du, J.B., Shi, L., Shi, Y., Tang, C.S.: Effects of endogenous carbon monoxide on collagen synthesis in pulmonary artery in rats under hypoxia. Life Sci. 74(10), 1225–1241 (2004). PMID:14697406
Horino, Y., Takahashi, S., Miura, T., Takahashi, Y.: Prolonged hypoxia accelerates the posttranscriptional process of collagen synthesis in cultured fibroblasts. Life Sci. 71(26), 3031–3045 (2002). PMID:12408871
Patel, R., Cardneau, J.D., Colles, S.M., Graham, L.M.: Synthetic smooth muscle cell phenotype is associated with increased nicotinamide adenine dinucleotide phosphate oxidase activity: effect on collagen secretion. J. Vasc. Surg. 43(2), 364–371 (2006). PMID:16476616
Levene, C.I., Kapoor, R., Heale, G.: The effect of hypoxia on the synthesis of collagen and glycosaminoglycans by cultured pig aortic endothelium. Atherosclerosis 44(3), 327–337 (1982). PMID:6816251
Pietila, K., Jaakkola, O.: Effect of hypoxia on the synthesis of glycosaminoglycans and collagen by rabbit aortic smooth muscle cells in culture. Atherosclerosis 50(2), 183–190 (1984). PMID:6712771
Campbell, E.J., Wald, M.S.: Hypoxic injury to human alveolar macrophages accelerates release of previously bound neutrophil elastase—implications for lung connective-tissue injury including pulmonary-emphysema. Am. Rev. Respir. Dis. 127(5), 631–635 (1983). PMID:ISI:A1983QP96200021
Scannell, G., Waxman, K., Kaml, G.J., Ioli, G., Gatanaga, T., Yamamoto, R., Granger, G.A.: Hypoxia induces a human macrophage cell-line to release tumor-necrosis-factor-alpha and its soluble receptors in vitro. J. Surg. Res. 54(4), 281–285 (1993). PMID:ISI:A1993LM66700003
Burke, B., Giannoudis, A., Corke, K.P., Gill, D., Wells, M., Ziegler-Heitbrock, L., Lewis, C.E.: Hypoxia-induced gene expression in human macrophages—implications for ischemic tissues and hypoxia-regulated gene therapy. Am. J. Pathol. 163(4), 1233–1243 (2003). PMID:ISI:000185517500003
Vorp, D.A., Wang, D.H., Webster, M.W.: Federspiel WJ effect of intraluminal thrombus thickness and bulge diameter on the oxygen diffusion in abdominal aortic aneurysm. J. Biomech. Eng. 120(5), 579–583 (1998). PMID:10412434
Adolph, R., Vorp, D.A., Steed, D.L., Webster, M.W., Kameneva, M.V., Watkins, S.C.: Cellular content and permeability of intraluminal thrombus in abdominal aortic aneurysm. J. Vasc. Surg. 25(5), 916–926 (1997). PMID:9152321
Saratzis, A., Abbas, A.A., Kiskinis, D., Melas, N., Saratzis, N., Kitas, G.D.: Abdominal aortic aneurysm: a review of the genetic basis. Angiology 62(1), 18–32 (2011). PMID:20566578
Yoon, S., Tromp, G., Vongpunsawad, S., Ronkainen, A., Juvonen, T., Kuivaniemi, H.: Genetic analysis of MMP3, MMP9, and PAI-1 in Finnish patients with abdominal aortic or intracranial aneurysms. Biochem. Biophys. Res. Commun. 265(2), 563–568 (1999). PMID:10558909
Jones, G.T., Phillips, V.L., Harris, E.L., Rossaak, J.I., van Rij, A.M.: Functional matrix metalloproteinase-9 polymorphism (C-1562T) associated with abdominal aortic aneurysm. J. Vasc. Surg. 38(6), 1363–1367 (2003). PMID:14681642
Hinterseher, I., Bergert, H., Kuhlisch, E., Bloomenthal, A., Pilarsky, C., Ockert, D., Schellong, S., Saeger, H.D., Krex, D.: Matrix metalloproteinase 2 polymorphisms in a caucasian population with abdominal aortic aneurysm. J. Surg. Res. 133(2), 121–128 (2006). PMID:16458924
Ogata, T., Shibamura, H., Tromp, G., Sinha, M., Goddard, K.A., Sakalihasan, N., Limet, R., MacKean, G.L., Arthur, C., Sueda, T., Land, S., Kuivaniemi, H.: Genetic analysis of polymorphisms in biologically relevant candidate genes in patients with abdominal aortic aneurysms. J. Vasc. Surg. 41(6), 1036–1042 (2005). PMID:15944607
Wang, X., Tromp, G., Cole, C.W., Verloes, A., Sakalihasan, N., Yoon, S., Kuivaniemi, H.: Analysis of coding sequences for tissue inhibitor of metalloproteinases 1 (TIMP1) and 2 (TIMP2) in patients with aneurysms. Matrix Biol. 18(2), 121–124 (1999). PMID:10372551
Ghilardi, G., Biondi, M.L., Battaglioli, L., Zambon, A., Guagnellini, E., Scorza, R.: Genetic risk factor characterizes abdominal aortic aneurysm from arterial occlusive disease in human beings: CCR5 Delta 32 deletion. J. Vasc. Surg. 40(5), 995–1000 (2004). PMID:15557916
Katrancioglu, N., Manduz, S., Karahan, O., Yilmaz, M.B., Sezgin, I., Bagci, G., Berkan, O.: The role of the CCR2 gene polymorphism in abdominal aortic aneurysms. Angiology 62(2), 140–143 (2011). PMID:21220372
Pola, R., Gaetani, E., Santoliquido, A., Gerardino, L., Cattani, P., Serricchio, M., Tondi, P., Flore, R., Grande, M., Carbonin, P., Fadda, G., Pola, P.: Abdominal aortic aneurysm in normotensive patients: association with angiotensin-converting enzyme gene polymorphism. Eur. J. Vasc. Endovasc. Surg. 21(5), 445–449 (2001). PMID:11352521
Brunelli, T., Prisco, D., Fedi, S., Rogolino, A., Farsi, A., Marcucci, R., Giusti, B., Pratesi, C., Pulli, R., Gensini, G.F., Abbate, R., Pepe, G.: High prevalence of mild hyperhomocysteinemia in patients with abdominal aortic aneurysm. J. Vasc. Surg. 32(3), 531–536 (2000). PMID:10957660
Ferrara, F., Novo, S., Grimaudo, S., Raimondi, F., Meli, F., Amato, C., Amodeo, G., Lo Presti, R., Caimi, G.: Methylenetetrahydrofolate reductase mutation in subjects with abdominal aortic aneurysm subdivided for age. Clin. Hemorheol. Microcirc. 34(3), 421–426 (2006). PMID:16614466
Sofi, F., Marcucci, R., Giusti, B., Pratesi, G., Lari, B., Sestini, I., Lo Sapio, P., Pulli, R., Pratesi, C., Abbate, R., Gensini, G.F.: High levels of homocysteine, lipoprotein (a) and plasminogen activator inhibitor-1 are present in patients with abdominal aortic aneurysm. Thromb. Haemost. 94(5), 1094–1098 (2005). PMID:16363254
Atli, F.H., Manduz, S., Katrancioglu, N., Ozum, U., Disli, O.M., Atahan, E., Ozdemir, O., Dogan, K., Berkan, O.: eNOS G894T polymorphism and abdominal aortic aneurysms. Angiology 61(2), 125–130 (2010). PMID:19638352
Jones, K., Powell, J., Brown, L., Greenhalgh, R., Jormsjo, S., Eriksson, P.: The influence of 4G/5G polymorphism in the plasminogen activator inhibitor-1 gene promoter on the incidence, growth and operative risk of abdominal aortic aneurysm. Eur. J. Vasc. Endovasc. Surg. 23(5), 421–425 (2002). PMID:12027469
Moran, C.S., Clancy, P., Biros, E., Blanco-Martin, B., McCaskie, P., Palmer, L.J., Coomans, D., Norman, P.E., Golledge, J.: Association of PPARgamma allelic variation, osteoprotegerin and abdominal aortic aneurysm. Clin. Endocrinol. (Oxf) 72(1), 128–132 (2010). PMID:19438902
Krishna, S.M., Dear, A.E., Norman, P.E., Golledge, J.: Genetic and epigenetic mechanisms and their possible role in abdominal aortic aneurysm. Atherosclerosis 212(1), 16–29 (2010). PMID:20347091
Genome Wide Association Studies: Identifying the genes that determine the risk of abdominal aortic aneurysm. Eur. J. Vasc. Endovasc. Surg. 36(4), 395–396 PMID:18621558 (2008)
Helgadottir, A., Thorleifsson, G., Magnusson, K.P., Gretarsdottir, S., Steinthorsdottir, V., Manolescu, A., Jones, G.T., Rinkel, G.J., Blankensteijn, J.D., Ronkainen, A., Jaaskelainen, J.E., Kyo, Y., Lenk, G.M., Sakalihasan, N., Kostulas, K., Gottsater, A., Flex, A., Stefansson, H., Hansen, T., Andersen, G., Weinsheimer, S., Borch-Johnsen, K., Jorgensen, T., Shah, S.H., Quyyumi, A.A., Granger, C.B., Reilly, M.P., Austin, H., Levey, A.I., Vaccarino, V., Palsdottir, E., Walters, G.B., onsdottir, T., Snorradottir, S., Magnusdottir, D., Gudmundsson, G., Ferrell, R.E., Sveinbjornsdottir, S., Hernesniemi, J., Niemela, M., Limet, R., Andersen, K., Sigurdsson, G., Benediktsson, R., Verhoeven, E.L., Teijink, J.A., Grobbee, D.E., Rader, D.J., Collier, D.A., Pedersen, O., Pola, R., Hillert, J., Lindblad, B., Valdimarsson, E.M., Magnadottir, H.B., Wijmenga, C., Tromp, G., Baas, A.F., Ruigrok, Y.M., van Rij, A.M., Kuivaniemi, H., Powell, J.T., Matthiasson, S.E., Gulcher, J.R., Thorgeirsson, G., Kong, A., Thorsteinsdottir, U., Stefansson, K.: The same sequence variant on 9p21 associates with myocardial infarction, abdominal aortic aneurysm and intracranial aneurysm. Nat. Genet. 40(2), 217–224 (2008). PMID:18176561
Bown, M.J., Braund, P.S., Thompson, J., London, N.J., Samani, N.J., Sayers, R.D.: Association between the coronary artery disease risk locus on chromosome 9p21.3 and abdominal aortic aneurysm. Circ. Cardiovasc. Genet. 1(1), 39–42 (2008). PMID:20031540
Biros, E., Cooper, M., Palmer, L.J., Walker, P.J., Norman, P.E., Golledge, J.: Association of an allele on chromosome 9 and abdominal aortic aneurysm. Atherosclerosis 212(2), 539–542 (2010). PMID:20605023
Annambhotla, S., Bourgeois, S., Wang, X., Lin, P.H., Yao, Q., Chen, C.: Recent advances in molecular mechanisms of abdominal aortic aneurysm formation. World J. Surg. 32(6), 976–986 (2008). PMID:18259804
Alexander, J.J.: The pathobiology of aortic aneurysms. J. Surg. Res. 117(1), 163–175 (2004). PMID:ISI:000220182100021
Fillinger, M.F., Racusin, J., Baker, R.K., Cronenwett, J.L., Teutelink, A., Schermerhorn, M.L., Zwolak, R.M., Powell, R.J., Walsh, D.B., Rzucidlo, E.M.: Anatomic characteristics of ruptured abdominal aortic aneurysm on conventional CT scans: implications for rupture risk. J. Vasc. Surg. 39(6), 1243–1252 (2004). PMID:ISI:000222018600016
Vorp, D.A., Vande Geest, J.P.: Biomechanical determinants of abdominal aortic aneurysm rupture. Arterioscler. Thromb. Vasc. Biol. 25(8), 1558–1566 (2005). PMID:16055757
Sonesson, B., Hansen, F., Lanne, T.: Abdominal aortic aneurysm: a general defect in the vasculature with focal manifestations in the abdominal aorta? J. Vasc. Surg. 26(2), 247–254 (1997). PMID:9279311
Wilson, K., Whyman, M., Hoskins, P., Lee, A.J., Bradbury, A.W., Fowkes, F.G., Ruckley, C.V.: The relationship between abdominal aortic aneurysm wall compliance, maximum diameter and growth rate. Cardiovasc. Surg. 7(2), 208–213 (1999). PMID:10353673
Wilson, K.A., Lindholt, J.S., Hoskins, P.R., Heickendorff, L., Vammen, S., Bradbury, A.W.: The relationship between abdominal aortic aneurysm distensibility and serum markers of elastin and collagen metabolism. Eur. J. Vasc. Endovasc. Surg. 21(2), 175–178 (2001). PMID:11237793
MacSweeney, S.T., Young, G., Greenhalgh, R.M., Powell, J.T.: Mechanical properties of the aneurysmal aorta. Br. J. Surg. 79(12), 1281–1284 (1992). PMID:1486417
Lanne, T., Sonesson, B., Bergqvist, D., Bengtsson, H., Gustafsson, D.: Diameter and compliance in the male human abdominal aorta: influence of age and aortic aneurysm. Eur. J. Vasc. Surg. 6(2), 178–184 (1992). PMID:1572458
Vorp, D.A., Mandarino, W.A., Webster, M.W., Gorcsan 3rd, J.: Potential influence of intraluminal thrombus on abdominal aortic aneurysm as assessed by a new non-invasive method. Cardiovasc. Surg. 4(6), 732–739 (1996). PMID:9013001
Vallabhaneni, S.R., Gilling-Smith, G.L., How, T.V., Carter, S.D., Brennan, J.A., Harris, P.L.: Heterogeneity of tensile strength and matrix metalloproteinase activity in the wall of abdominal aortic aneurysms. J. Endovasc. Ther. 11(4), 494–502 (2004). PMID:ISI:000223415300019
Raghavan, M.L., Kratzberg, J., DaSilva, E.S.: Heterogeneous, variable wall-thickness modeling of a ruptured abdominal aortic aneurysm. In: 2004 ASME International Mechanical Engineering Conference, Anaheim (CA) (2004)
Sacks, M.S.: Biaxial mechanical evaluation of planar biological materials. J. Elast. 61(1–3), 199–246 (2000). PMID:ISI:000169741700009
Van de Geest, J.P., Sacks, M.S., Vorp, D.A.: Age dependency of the biaxial biomechanical behavior of human abdominal aorta. J. Biomech. Eng. 126(6), 815–822 (2004). PMID:15796340
Wang, D.H., Makaroun, M., Webster, M.W., Vorp, D.A.: Mechanical properties and microstructure of intraluminal thrombus from abdominal aortic aneurysm. J. Biomech. Eng. 123(6), 536–539 (2001). PMID:11783723
Stringfellow, M.M., Lawrence, P.F., Stringfellow, R.G.: The influence of aorta aneurysm geometry upon stress in the aneurysm wall. J. Surg. Res. 42(4), 425–433 (1987). PMID:ISI:A1987H239900014
Marston, W.A., Criado, E., Baird, C.A., Keagy, B.A.: Reduction of aneurysm pressure and wall stress after endovascular repair of abdominal aortic aneurysm in a canine model. Ann. Vasc. Surg. 10(2), 166–173 (1996). PMID:ISI:A1996UK57200010
Mcgiffin, D.C., Mcgiffin, P.B., Galbraith, A.J., Cross, R.B.: Aortic-wall stress profile after repair of coarctation of the aorta—is it related to subsequent true aneurysm formation. J. Thorac. Cardiovasc. Surg. 104(4), 924–931 (1992). PMID:ISI:A1992JT19800011
Inzoli, F., Boschetti, F., Zappa, M., Longo, T., Fumero, R.: Biomechanical factors in abdominal aortic aneurysm rupture. Eur J. Vasc. Surg. 7(6), 667–674 (1993). PMID:8270069
Mower, W.R., Baraff, L.J., Sneyd, J.: Stress distributions in vascular aneurysms—factors affecting risk of aneurysm rupture. J. Surg. Res. 55(2), 155–161 (1993). PMID:ISI:A1993MC02400007
Raghavan, M.L., Fillinger, M.F., Marra, S.P., Naegelein, B.P., Kennedy, F.E.: Automated methodology for determination of stress distribution in human abdominal aortic aneurysm. J. Biomech. Eng.-Trans. ASME 127(5), 868–871 (2005). PMID:ISI:000232193200018
Di Martino, E.S., Guadagni, G., Fumero, A., Ballerini, G., Spirito, R., Biglioli, P., Redaelli, A.: Fluid-structure interaction within realistic three-dimensional models of the aneurysmatic aorta as a guidance to assess the risk of rupture of the aneurysm. Med. Eng. Phys. 23(9), 647–655 (2001). PMID:ISI:000173836400005
Scotti, C.M., Shkolnik, A.D., Muluk, S.C., Finol, E.A.: Fluid-structure interaction in abdominal aortic aneurysms: effects of asymmetry and wall thickness. Biomed. Eng. Online 4, 64 (2005). PMID:16271141
Finol, E.A., Amon, C.H.: Flow-induced wall shear stress in abdominal aortic aneurysms: part II–pulsatile flow hemodynamics. Comput. Methods Biomech. Biomed. Eng. 5(4), 319–328 (2002). PMID:12186711
Asbury, C.L., Ruberti, J.W., Bluth, E.I., Peattie, R.A.: Experimental investigation of steady flow in rigid models of abdominal aortic aneurysms. Ann. Biomed. Eng. 23(1), 29–39 (1995). PMID:7762880
Peattie, R.A., Riehle, T.J., Bluth, E.I.: Pulsatile flow in fusiform models of abdominal aortic aneurysms: flow fields, velocity patterns and flow-induced wall stresses. J. Biomech. Eng.-Trans. ASME 126(4), 438–446 (2004). PMID:ISI:000224668800006
Rissland, P., Alemu, Y., Einav, S., Ricotta, J., Bluestein, D.: Abdominal aortic aneurysm risk of rupture: patient-specific FSI simulations using anisotropic model. J. Biomech. Eng. 131(3), 031001 (2009). PMID:19154060
Holzapfel, G.A., Gasser, T.C., Stadler, M.: A structural model for the viscoelastic behavior of arterial walls: continuum formulation and finite element analysis. Eur. J. Mech. A-Solids 21(3), 441–463 (2002). PMID:ISI:000176078400007
Mohan, D., Melvin, J.W.: Failure properties of passive human aortic tissue.2. Biaxial tension tests. J. Biomech. 16(1), 31 (1983). PMID:ISI:A1983QE15900004
Lee, M.C., Haut, R.C.: Strain rate effects on tensile failure properties of the common carotid-artery and jugular veins of ferrets. J. Biomech. 25(8), 925–927 (1992). PMID:ISI:A1992JD39100011
Purslow, P.P.: Positional variations in fracture toughness, stiffness and strength of descending thoracic pig aorta. J. Biomech. 16(11), 947–953 (1983)
Rajagopal, K., Bridges, C., Rajagopal, K.R.: Towards an understanding of the mechanics underlying aortic dissection. Biomech. Model. Mechanobiol. 6(5), 345–359 (2007)
Adham, M., Gournier, J.P., Favre, J.P., De La Roche, E., Ducerf, C., Baulieux, J., Barral, X., Pouyet, M.: Mechanical characteristics of fresh and frozen human descending thoracic aorta. J. Surg. Res. 32(1), 32–34 (1996). PMID:8806470
Groenink, M., Langerak, S.E., Vanbavel, E., van der Wall, E.E., Mulder, B.J., van der Wal, A.C., Spaan, J.A.: The influence of aging and aortic stiffness on permanent dilation and breaking stress of the thoracic descending aorta. Cardiovasc. Res. 43(2), 471–480 (1999). PMID:10536677
Iliopoulos, D.C., Kritharis, E.P., Giagini, A.T., Papadodima, S.A., Sokolis, D.P.: Ascending thoracic aortic aneurysms are associated with compositional remodeling and vessel stiffening but not weakening in age-matched subjects. J. Thorac. Cardiovasc. Surg. 137(1), 101–109 (2009). PMID:19154911
Tiessen, I.M., Roach, M.R.: Factors in the initiation and propagation of aortic dissections in human autopsy aortas. J. Biomech. Eng.-Trans. ASME 115(1), 123–125 (1993). PMID:ISI:A1993KQ01400019
Thubrikar, M.J., Agali, P., Robicsek, F.: Wall stress as a possible mechanism for the development of transverse intimal tears in aortic dissections. J. Med. Eng. Technol. 23(4), 127–134 (1999). PMID:ISI:000082863900002
Beller, C.J., Labrosse, M.R., Thubrikar, M.J., Robicsek, F.: Role of aortic root motion in the pathogenesis of aortic dissection. Circulation 109(6), 763–769 (2004). PMID:ISI:000189005500013
Borghi, A., Wood, N.B., Mohiaddin, R.H., Xu, X.Y.: Fluid-solid interaction simulation of flow and stress pattern in thoracoabdominal aneurysms: a patient-specific study. J. Fluids Struct. 24(2), 270–280 (2008). PMID:ISI:000254747600007
Khanafer, K., Berguer, R.: Fluid-structure interaction analysis of turbulent pulsatile flow within a layered aortic wall as related to aortic dissection. J. Biomech. 42(16), 2642–2648 (2009). PMID:ISI:000273135200003
Tse, K.M., Chiu, P., Lee, H.P., Ho, P.: Investigation of hemodynamics in the development of dissecting aneurysm within patient-specific dissecting aneurismal aortas using computational fluid dynamics (CFD) simulations. J. Biomech. 44(5), 827–836 (2011). PMID:21256491
Nathan, D.P., Xu, C., Gorman III, J.H., Fairman, R.M., Bavaria, J.E., Gorman, R.C., Chandran, K.B., Jackson, B.M.: Pathogenesis of acute aortic dissection: a finite element stress analysis. Ann. Thorac. Surg. 91(2), 458–463 (2011)
Lederle, F.A., Wilson, S.E., Johnson, G.R., Reinke, D.B., Littooy, F.N., Acher, C.W., Ballard, D.J., Messina, L.M., Gordon, I.L., Chute, E.P., Krupski, W.C., Busuttil, S.J., Barone, G.W., Sparks, S., Graham, L.M., Rapp, J.H., Makaroun, M.S., Moneta, G.L., Cambria, R.A., Makhoul, R.G., Eton, D., Ansel, H.J., Freischlag, J.A., Bandyk, D.: Immediate repair compared with surveillance of small abdominal aortic aneurysms. N. Engl. J. Med. 346(19), 1437–1444 (2002). PMID:12000813
Li, Z.Y.: Computed wall stress may predict the growth of abdominal aortic aneurysm. Conf. Proc. IEEE Eng. Med. Biol. Soc. 1, 2626–2629 (2010). PMID:21096184
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2011 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Phillippi, J.A., Pasta, S., Vorp, D.A. (2011). Biomechanics and Pathobiology of Aortic Aneurysms. In: McGloughlin, T. (eds) Biomechanics and Mechanobiology of Aneurysms. Studies in Mechanobiology, Tissue Engineering and Biomaterials, vol 7. Springer, Berlin, Heidelberg. https://doi.org/10.1007/8415_2011_84
Download citation
DOI: https://doi.org/10.1007/8415_2011_84
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-18094-1
Online ISBN: 978-3-642-18095-8
eBook Packages: EngineeringEngineering (R0)