Abstract
As shown by clinical genetic studies, affective and anxiety disorders are complex genetic disorders with genetic and environmental factors interactively determining their respective pathomechanism. Advances in molecular genetic techniques including linkage studies, association studies, and genome-wide association studies allow for the detailed dissection of the genetic influence on the development of these disorders. Besides the molecular genetic investigation of categorical entities according to standardized diagnostic criteria, intermediate phenotypes comprising neurobiological or neuropsychological traits (e.g., neuronal correlates of emotional processing) that are linked to the disease of interest and that are heritable, have been proposed to be closer to the underlying genotype than the overall disease phenotype. These intermediate phenotypes are dimensional and more precisely defined than the categorical disease phenotype, and therefore have attracted much interest in the genetic investigation of affective and anxiety disorders. Given the complex genetic nature of affective and anxiety disorders with an interaction of multiple risk genes and environmental influences, the interplay of genetic factors with environmental factors is investigated by means of gene-environment interaction (GxE) studies. Pharmacogenetic studies aid in the dissection of the genetically influenced heterogeneity of psychotropic drug response and may contribute to the development of a more individualized treatment of affective and anxiety disorders. Finally, there is some evidence for genetic factors potentially shared between affective and anxiety disorders pointing to a possible overlapping phenotype between anxiety disorders and depression.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Affective Disorders
The group of affective disorders comprises both major depressive disorder (MDD; unipolar depression) with various subtypes as well as bipolar disorder (BPD). The latter displays by changes between (hypo-)manic and depressive phases, with intermittent euthymic phases, while the course of MDD is characterized by depression and euthymia. As patients not rarely develop their first manic phase only years after their first depression, they might well be initially mischaracterized as MDD patients (so-called “hidden bipolars”), which is a challenge for genetic studies on affective disorders. To overcome this problem, several indicators for the presence of BPD in depression have been suggested, e.g. subthreshold hypomanic symptoms (Angst et al. 2010; Fiedorowicz et al. 2011). This however has not been incorporated in current genetic studies and thus one should always consider that MDD studies might well include a substantial amount of “hidden bipolar” patients, obfuscating MDD-specific findings. Furthermore, in the following section more recent approaches such as genome-wide association studies (GWAS) and copy-number variant (CNV) analyses are reviewed, as there are already plenty of scholarly review articles on linkage and association studies. These issues will therefore be touched upon more briefly; with respect to intermediate phenotype and gene x environment (GxE) studies in affective disorders, the reader is referred to more specialized reviews for the sake of space, as this extensive topic is beyond the scope of this article.
1.1 Clinical Genetics (Family, Twin, Adoption Studies)
There is ample evidence that BPD is a highly genetic condition featuring an estimated heritability of 0.75 as evidenced by numerous clinical genetic studies. The risk for a bipolar patient to have a bipolar first-degree relative is increased about tenfold, and the risk to have an MDD relative is even higher (10- to 15-fold). The largest study to date, that investigated more than two million Swedish nuclear families (Lichtenstein et al. 2009), demonstrated a heritability of bipolar disorder of 59%. Furthermore, relatives of bipolar patients also had a two to fourfold increased risk to suffer from schizophrenia. Environmental influences were mainly due to non-shared environment. In line with these data, twin studies also argue for a heritability ranging from 59 to 87% (for an overview see Shih et al. 2004). As little as two adoption studies on bipolar disorder have been carried out to date (Mendlewicz and Rainer 1977; Wender et al. 1986), also argued for a genetic cause of the disorder. An excellent overview on clinical genetic studies in bipolar disorder can be obtained from Smoller and Finn (2003).
On the other hand, the heritability of MDD is comparatively lower (estimated to be around 0.37 in the most comprehensive review and meta-analysis available to date; Sullivan et al. 2000) and environmental influences (unique, but not shared environment) are considered to play a more important role as compared to BPD. This is also reflected in twin and adoption studies. However, especially older studies do not discriminate between bipolar and unipolar depression and hence explicit data on unipolar depression is in fact quite limited; only five family and six twin studies, but no adoption study meet the stringent inclusion criteria in a comprehensive analysis (Sullivan et al. 2000). Across the five family studies, the summary odds ratio for MDD in first relatives of MDD patients was 2.84 and significant. Interestingly, the odds ratio increased when only considering controls which have been screened for absence of psychiatric disorders. Two of the three reported twin studies argued for a substantial genetic component of MDD, and finally, the twin studies including more than 21,000 individuals yielded a heritability of 37% and an influence of individual-specific environmental effects of 63%. No large differences in heritability indices were found between community and clinical studies, and the influence of shared environment was negligible. Hence, taken together, there is a clear genetic liability towards MDD although it is much smaller as compared to BPD—which has also been taken into account when reviewing studies where both conditions were not carefully treated separately. Furthermore, it is evident for both MDD as well as BPD that these disorders do not follow a strict Mendelian pattern of inheritance, but rather are complex genetic in nature featuring polygenic and oligogenic models (“common variant, common disease” model), but probably also—for a part of the patients—highly penetrant risk genes (“multiple rare variant, common disease” model, see below).
1.2 Molecular Genetics (Linkage, Association, GWAS, CNV Analysis)
1.2.1 Linkage Studies
More than 40 linkage scans for BPD have been published to date which generated plenty of disparate findings. However, quite a number of loci meeting significance criteria were described by two or more groups: 3p12-14, 4p16, 4q31-35, 5q31-33, 6q16/21-25, 8q21-24, 10q25-26, 11p15.5, 12q23-24, 13q14-32, 18p11, 18q21-22 20q13, 21q21-22, 22q11-12, and Xq24-28. Confirmed positional candidate genes however are yet to emerge from these studies. An initially highly promising linkage peak on chromosome 11p15 is considered meanwhile to be due to type I error (Egeland et al. 1987; Berrettini 2001). Also, other loci which have been initially promising could subsequently not be confirmed. A paradigmatic case in this respect is for e.g. the 12q23-24 locus (Dawson et al. 1995; Ewald et al. 1998, 2002; Green et al. 2005), which is noteworthy due to the co-segregation of Darier’s disease with BPD (Maziade et al. 2001). It has been shown that, in some families suffering from both disorders, the BPD locus lies outside of the Darier’s disease causing ATP2A2 gene, yet is in linkage disequilibrium with this variant (Jones et al. 2002). Hence, there might indeed be intermediately penetrant variants in this region which are exclusive to only a few families and which are lost in noise when combining many families, or cases, respectively. Similarly, a functional mutation in the gene encoding the brain-specific tryptophan hydroxylase 2 (TPH2) has been described which segregates with BPD in three families (Cichon et al. 2008; Grigoroiu-Serbanescu et al. 2008). Findings like these argue for a “common disease, multiple rare variant” model (McCarthy et al. 2008) and underscore the clinical and genetic heterogeneity of BPD. This however does not argue against the concurrent existence of a “common disease, common variant model”. As both models most likely are present in clinical samples, this additional level of complexity further hampers the identification of BPD risk genes.
Different meta-analyses found the strongest evidence for BPD susceptibility loci on 13q and 22q (Badner and Gershon 2002; 1228 patients from 353 families), or 9p22.3-21.1, 10q11.21-22.1 and 14q24.1-32.12 (948 to 2437 patients; Segurado et al. 2003). The latter study used the rank-based genome scan (GSAM) method which, together with sample heterogeneity, might account for the different findings as compared to the first study. Finally, in a combined analysis, 6q21-q25 and 8q24 showed genome-wide significance (5179 patients from 1067 families; McQueen et al. 2005). Again, the underlying genes have not yet been identified. Further scholarly reviews on this topic have been provided by Schulze and McMahon (2003), Serretti and Mandelli (2008), Barnett and Smoller (2009), and Craddock und Sklar (2009).
Also in MDD, numerous linkage scans were carried out (reviewed e.g. by Lohoff (2010) yet did not point to clear regions of susceptibility, as expected from the lower heritability rate of MDD as compared to BPD. No meta-analysis has been performed to date, which is surprising given the recent efforts to uncover the genetic basis of MDD and hence there is a clear need for further research. There is no meaningful overlap of linkage peaks between studies, although it is noteworthy that two linkage signals have previously been implicated in BPD: one on chromosome 18q (Camp et al. 2005) and the locus mentioned above on 12q23-24 (McGuffin et al. 2005; Abkevich et al. 2003). Therefore, this region appears to be a promising region for affective disorders, yet most likely carries more than just one risk gene.
1.2.2 Association Studies
With regard to candidate gene studies, many genes were shown to be associated with BPD, but none of them has been established as a specific BPD susceptibility gene. Among the best replicated genes are DAOA/G72 (which was associated in a case–control study, but not in a meta-analyses; Muller et al. 2011; Shi et al. 2008), BDNF (again, meta-analyses provided differing data: Kanazawa et al. 2007; Fan and Sklar 2008), DISC1, NRG1, ARNTL/CLOCK, FAT, and GSK3B (Barnett and Smoller 2009; Serretti and Mandelli 2008; Luykx et al. 2010). Not surprisingly, many genes encoding for components of neurotransmitter pathways have been tested for an association with BPD (such as SLC6A3, HTR2A, TPH2, MAOA, COMT, DRD1, and SLC6A4). Coming from GWAS on schizophrenia, the risk gene ZNF804A was demonstrated not to be specific for this disorder, but rather was also associated with BPD (O’Donovan et al. 2008; Williams et al. 2011; Steinberg et al. 2011). The same was true for the GWAS schizophrenia risk loci around the MHC region and NRGN (Williams et al. 2011) and other genes which initially have been described as schizophrenia risk genes: the above-mentioned DISC1 and DAOA/G72 genes, but also NRG1, DTNB1, and NPAS3 (Huang et al. 2010; Pickard et al. 2009).
Most of the association studies published to date suffer from the drawback of small sample sizes and lack of replication, and hence, the combination of large, well described international samples (as done in the Psychiatric GWAS consortium [PGC]) is paramount especially in the search for risk variants assuming a “common variant, common disease” model. Furthermore, meta-analytic treatment of existing data might shed some light on the contribution of suggested BPD risk genes. Such have been performed on considerably sized samples on only a few genes. The gene encoding for methylenetetrahydrofolate reductase (MTHFR) has been tested for an analysis with mood disorders several times. While the first study on 1222 MDD patients yielded negative results (Gaysina et al. 2008), the latest analysis comprising 9648 cases (MDD, BPD and schizophrenia combined) yielded again a significant yet unspecific association of MTHFR with mood disorders (best OR = 1.26; Peerbooms et al. 2011). This is in line with a positive meta-analysis on BPD by Gilbody et al. (2007), but in discrepancy to three further meta-analyses on MTHFR in BPD (Zintzaras 2006, 1415 cases; Chen et al. 2009, 1260 cases; Cohen-Woods et al. 2010, 2584 cases). Given that the original genotyping data which was presented in the Cohen-Woods study (n = 897 BPD patients) was negative, but not included in the Peerbooms study, which demonstrated a significant effect only when all mood disorders were combined, the role of MTHFR in affective disorders seems to be rather unspecific and small.
A meta-analysis on all mood disorders found borderline evidence for an association of the dopamine receptor 2 (DRD2) Taq1 polymorphism (which in fact localizes to the neighboring gene ANKK1) with affective disorders, yet two more SNPs in DRD2 proved to be negative in much larger data sets so that there is only weak evidence for this gene being associated with BPD or MDD (Zou et al. 2010). The gene for catechol-O-methyltransferase (COMT) that degrades dopamine, features a well described functional polymorphism resulting in a Val to Met transition and which has been shown to be linked to BPD in a meta-analysis on 2944 cases (Zhang et al. 2009b), although this seemed to be more pronounced in Asian populations. Obviously, also genes coding for components of the serotonin system were subjected to meta-analyses, which often were combined with genuine genotyping efforts. A functional SNP in the promoter region of the serotonin receptor gene HTR1A (rs6295) was demonstrated to be significantly associated with BPD (1148 cases, Kishi et al. 2011). In the MAOA gene, three polymorphisms (sample sizes mostly >1000 cases) were meta-analyzed and the main finding was an association of an intronic CA repeat with BPD in Caucasians (Fan et al. 2010). The SLC6A4 promoter polymorphism (5-HTTLPR), which has mainly been studied in MDD GxE (see below) was also included in several meta-analyses that conclusively demonstrated a small yet significant association of the short variant with BPD (Lasky-Su et al. 2005; Cho et al. 2005, 1712 cases). Two meta-analyses focused on the TPH1 gene (Chen et al. 2008, 2011) and in unison came to the conclusion that TPH1 is not associated with MDD (2340 and 1812 patients, respectively), but with BPD (1951 and 2083 cases). Given that in the brain only the TPH2 isoform of tryptophan hydroxylase is expressed, this finding is rather surprising; however, as the foetal brain depends on maternal 5-HT production which is accomplished by placental TPH1 the observed association might in fact be true but rather due to maternal and not case genotype as has been described for rare TPH1 mutations in ADHD (Halmoy et al. 2010).
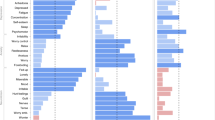
The lower heritability of MDD as compared to BPD notwithstanding, plenty of case–control association studies have been published thereon as well. A scholarly overview on candidate gene studies is provided by Lohoff (2010). In order to separate the wheat from the chaff, replication is key and meta-analytic aggregation of data is a possible route to success. Accordingly, a thorough meta-analysis on the data available until June 2007 examined 183 papers on 393 polymorphisms (Lopez-Leon et al. 2008). Twenty-two of these polymorphisms have been tested in at least three studies and were thus subjected to further meta-analysis. Here, significant association was demonstrated for the genes APOE2 (827 cases), GNB3 (375 cases), MTHFR (875 cases), SLC6A4 (3752 cases), and SLC6A3 (as little as 151 cases). Negative results were obtained for ACE, BDNF, COMT, DRD3, GABRA3, HTR1A, HTR1B, HTR2A, HTR2C, MAOA, SLC6A2, and TPH1. Further meta-analyses which have been published before this study were performed on ACE, DRD4, HTR2A, MTHFR, SLC6A4, and TH; positive findings were obtained for DRD4 (Lopez Leon et al. 2005; 917 cases). In the years following the meta-analysis by Lopez Leon, only few other meta-analytic studies have been published including those on MTHFR and TPH1 cited above. Furthermore, Franke and associates recently conducted a meta-analysis on the functional BDNF Val66Met polymorphism. As BDNF has been implicated both in the pathogenesis of depression as well as the mechanism of action of anti-depressant treatment (Duman and Monteggia 2006), it is an obvious candidate gene and accordingly was shown to be associated with depression in this meta-analysis of 2812 cases, although the association is sex-specific and only detectable in males (Verhagen et al. 2010).
The largest body of evidence, and by far the largest sample sizes, exists for the gene encoding the serotonin transporter (SLC6A4). Following the seminal finding by Caspi et al. (2003) that environmental influences interact with SLC6A4 genotype to increase the risk toward depression, emphasis has been put on studies aimed to test such GxE interactions adding a further level of complexity. Following positive meta-analyses confirming a main gene effect of SLC6A4 in depression (Furlong et al. 1998; Lopez-Leon et al. 2008; Clarke et al. 2010), also meta-analyses on GxE interaction studies yielded support for the notion that SLC6A4 has a role in the etiology of depression (Karg et al. 2011). As Karg and Sen elaborate in depth on this topic in this book, the reader is referred to their contribution as well as the review articles by Uher and McGuffin (2008, 2010).
Also, genes encoding components of the cortisol pathway have proven to be interesting candidates for GxE in MDD. The glucocorticoid receptor-regulating co-chaperone FKBP5 has first been associated with recurrence of depression and response to antidepressant treatment in 2004 (Binder et al. 2004). This has later been replicated (Lekman et al. 2008) and FKBP5 was shown to interact with HTR2A and GRIK4 in moderating the response to antidepressant treatment (Horstmann et al. 2010). Most interestingly, FKBP5 has been shown to interact with severity of childhood abuse on later-life PTSD symptoms (Binder et al. 2008) which however might be confined to African Americans (Xie et al. 2010). One of the involved SNPs (rs1360780) was later replicated to interact with childhood maltreatment to affect depression measures (BDI-II) in adult life (Appel et al. 2011). This SNP also displayed a main gene effect on suicidal events in depressive adolescents (Brent et al. 2010), a categorical diagnosis of depression (Lekman et al. 2008) and general depressive symptoms (Lavebratt et al. 2010; Zobel et al. 2010; Velders et al. 2011) and interestingly is associated with decreased cortisol levels (Velders et al. 2011) providing a possible pathophysiological mechanism for the association data. Also, rs1360780 went along with smaller right hippocampal volume in patients with depression (Zobel et al. 2010). Taken together, there is good evidence (Binder 2009) that risk genotypes in FKBP5 (especially rs1360780) interact with early life adversity on later life depression, possibly by long-term adaptive changes of the HPA axis and subsequent morphological changes of the hippocampus increasing vulnerability to disease. In line with these findings, it was also shown that rs110402 in the corticotropin-releasing hormone receptor (CRHR1) interacted with child abuse to increase the risk toward later life depression (Bradley et al. 2008), most interestingly in interaction with the serotonin transporter risk genotype mentioned above (Ressler et al. 2010).
It seems to be a common phenomenon that candidate genes rarely replicate when tested for in GWAS (see below) data sets. A thorough study on MDD candidate genes (Bosker et al. 2011) tested 57 genes in the Genetic Association Information Network (GAIN) MDD sample (n = 1862 cases). From 93 selected candidate SNPs, only 18 were present on the array, and a further 47 were imputed. Of those, only five (including an SNP in NPY) were associated in the GAIN sample, all with p>0.03. When candidates were tested on a gene-based level, analyzing 4870 SNPs, the TNF and NET genes yielded suggestive evidence. In general, heavy use of imputation might have introduced a further source of noise in this particular study. Likewise, when candidate genes were targeted in other individual GWAS, rarely more than expected by chance replicated.
Taken together, numerous association studies on MDD and BPD—actually too many to mention in this overview—hitherto only presented few convincing findings. Amongst them, associations of affective disorders with MTHFR, BDNF, and SLC6A4 seem to be robust. A length variant in the latter gene shows solid evidence for GxE effect; FKBP5 is another promising candidate for the moderating effects of early life stress regarding depression in adult life. Lessons that can be learned from the plethora of false-positive findings to date are that large and well-characterized samples have to be accrued, with careful evaluation of life events and the assessment of biological measures such as neuroimaging endophenotypes or therapy response.
1.2.3 Genome-Wide Association Studies
Along with autism, attention-deficit hyperactivity disorder (ADHD) and schizophrenia affective disorder comprise the core disorders of the Psychiatric GWAS Consortium (Sullivan 2010; Psychiatric GWAS Consortium [PGC] 2009), and at the time of writing, more than 12,000 cases of BPD and 14,000 cases of MDD are available within the PGC, with 20,000 more cases each expected to be included over the next 2 to 3 years. While these numbers may at first sound impressive, one has to consider that GWAS are the method of choice to pick common risk alleles conveying only small individual risk. Other complex-genetic traits might provide some clues for appropriate sample sizes: it took almost a quarter million people to detect and respectively confirm 32 risk variants for body mass index, explaining as little as 2–4% of genetic variance, and it was estimated that another 284 variants would carry comparable effect sizes and together would explain 6–11% of the genetic variation. The authors assumed that further 730,000 individuals would have to be genotyped to uncover 95% of these variants (Speliotes et al. 2010). Likewise, a recent study on body height (Lango Allen et al. 2010) examined 180,000 subjects and found 180 loci explaining 16% of phenotypic variants. As body weight and height are for sure somewhat easier to determine than depression, which is a heterogeneous condition from the start, one can easily see the obstacles one has to face when dealing with these kinds of studies. Having said this, and thereby also lowering the bar of expectations somehow, the above-mentioned studies are also encouraging and can be seen as proof-of-principle: GWAS can detect novel pathways and provide meaningful results, and thus larger scale studies should be encouraged in order to identify the molecular determinants of affective disorders, as previous linkage and association studies fell short in conclusively delineating these. Concluding these introductory remarks, the recent debate on the missing—or, rather, hidden—heritability has to be mentioned. The discussion whether the major endogenous psychoses are due to the sum of multiple common alleles with small individual effects (e.g. Purcell et al. 2009) or due to many rare variants, also including copy number variants (CNV), and causing “synthetic associations” (Dickson et al. 2010) and resulting in phenocopies (Gershon et al. 2011) is held lively and far from being resolved. These authors’ personal view is that both models might exist—which however complicates matters even more.
BPD
GWA studies on BPD, which has a higher heritability and presumably less GxE effects as compared to depression, have (probably due to these facts) provided stronger findings than MDD GWAS. The following section elaborates on the most interesting findings from BPD GWAS at the time of writing (04/2011) with focus on replicated risk genes and pathways, while issues like population admixture, microarray technology, and statistical comments are not further commented upon.
In one of the first published GWAS on BPD, Baum et al. (2008a) reported genome-wide significance of rs10120253 in intron 1 of diacylglycerol kinase eta (DGKH) in a German and US American population using a pooling approach. The gene product of DGKH metabolizes diacylglycerol (DAG), which is produced upon cleavage of PIP2 into IP3 and DAG by phospholipase C. DAG, in turn, activates protein kinase C which phosphorylates a variety of proteins including Dishevelled, an inhibitor of GSK3β (which itself has been considered an outstanding candidate gene for BPD due to several lines of molecular genetic evidence; Luykx et al. 2010). Furthermore, DGKH knockdown in HeLa cells impaired the MEK/ERK pathway, while overexpression activated the pathway (Yasuda et al. 2009). DGKH might therefore be involved in crucial pathways for psychiatric disorders and especially the mechanism of action of lithium. However, replication of DGKH failed in three studies on BPD and/or lithium response, respectively (Manchia et al. 2009; Tesli et al. 2009; Takata et al. 2011) while four other studies were ambiguous or positive (Baum et al. 2008b; Ollila et al. 2009; Squassina et al. 2009; Zeng et al. 2011). A recent study provided evidence for an association of a DGKH risk haplotype with MDD, BPD, and adult ADHD (Weber et al. 2011). Meta-analyses on Caucasian (Weber et al. 2011) as well as Asian (Takata et al. 2011) samples however demonstrated that DGKH is significantly associated with BPD. Furthermore, increased expression of DGKH in BPD (Moya et al. 2010) was demonstrated in human post-mortem tissue, so that DGKH represents one of the most promising candidate genes for BPD to date. Other candidates from the Baum et al. GWAS include NXN, VGCNL1, DFNB31, and SORCS2, the latter two of which were replicated in a later study (Ollila et al. 2009).
The UK Wellcome Trust Case Control Consortium (WTCCC 2007) aims at the investigation of several complex genetic disorders with high prevalence. As evident from the first glance on the Manhattan plots in this paper, there are no “skyscraping” BPD risk SNPs as compared to very clear signals in cardiovascular or metabolic disorders. The WTCCC BPD GWAS provided genome-wide evidence for a non-gene marker next to PALB2, NDUFAB1, and DCTN5; other signals were observed for KCNC2, GABRB1, GRM7, and SYN3, all of which are in pathways previously implicated in BPD. Shortly after the WTCCC report, Sklar et al. reported on the STEP-UCL study and provided significant findings for MYO5B, TSPAN8, CDH7, and EGFR (Sklar et al. 2008). Some of those genes were attempted to replicate using a targeted approach; both TSPAN8 (Scholz et al. 2010) and CDH7 (Soronen et al. 2010) were confirmed in doing so. When the significant signals from the WTCCC and Baum data sets were tested in Sklar’s STEP-BD/UCL sample, negative findings were observed for DGKH and PALB2, however, this analysis provided further support for CACNA1C and DFNB31 arguing for the rationale to combine large data sets. Accordingly, the fourth GWAS study, ED-DUB-STEP2 (Ferreira et al. 2008), investigated another 1000 patients and included meta-analytic treatment of the WTCCC and STEP-UCL data sets (total n = 4387 cases). In doing so, the holy grail of genome-wide significance was reached for markers in two genes: CACNA1C (alpha-1 subunit of a voltage dependent calcium channel) and ANK3 (ankyrin 3). Other interesting candidate genes from this study include SYNE1, SPRED1, CMTM8 (which interacts with EGFR), NPAS3 (which has previously been suggested to be associated with schizophrenia and bipolar disorder; Pickard et al. 2009), and ARNT2. In a subsequent meta-analysis including two samples from Nordic countries, the breast cancer risk genes PALB2 and BRCA2 were followed up in these as well as the WTCCC and STEP-UCL/ED-DUB-STEP2 samples (total case n = 5547). In doing so, variants in both genes were shown to be associated with BPD (Tesli et al. 2010). Not surprisingly nevertheless, CACNA1C and ANK3 drew most attention in follow-up studies.
For both ANK3 and CACNA1C, it is noteworthy that replication attempts not only provided evidence that these genes are associated with BPD; rather, they were demonstrated to be associated with a broad range of disorders across diagnostic boundaries arguing for a more unspecific role of these genes in psychiatric disorders. For example, ANK3 was not only replicated in BPD (Lee et al. 2010; Schulze et al. 2009; Scott et al. 2009; Smith et al. 2009), but also associated with schizophrenia (Athanasiu et al. 2010). Likewise, CACNA1C was again found to be associated with BPD (Keers et al. 2009), but also with schizophrenia (Green et al. 2009; Moskvina et al. 2009; Nyegaard et al. 2010), MDD (Green et al. 2009), and psychopathological features (e.g., agitation) therein (Casamassima et al. 2010). Neuroimaging studies demonstrated an effect of the CACNA1C risk variant rs1006737 on brain structure (Franke et al. 2010; Kempton et al. 2009) as well as function (Erk et al. 2010; Krug et al. 2010; Wessa et al. 2010).
In the last 2 years, several other GWAS and meta-analyses on BPD have been published. A small study from Japan (Hattori et al. 2009), which applied a two-stage design, provided nominal although not corrected significance for markers within AUTS2 (previously implicated in autism), SNAP25 (which is a schizophrenia and ADHD candidate gene), PLXNA2 (which has been found in schizophrenia and anxiety GWAS) and CSMD1, which was already one of the candidates from the Baum et al. study (Baum et al. 2008a). No other top hits from previous BPD GWAS however were replicated. In Han Chinese patients suffering from BPD type I, Lee et al. (2010) likewise did not provide findings on the genome-wide level, yet interestingly also found suggestive association of BPD with SNPs in another voltage-dependent calcium channel subunit, CACNB2 (other highly significant SNPs were located in KCTD12, SP8, and ST8SIA2) pointing again to calcium signalling having a role in BPD. Targeted investigation of previously identified GWAS candidate genes yielded a p = 10−5 for an SNP near ANK3, yet no other gene has been replicated.
Scott and colleagues combined two GWAS studies from the US, Canada, and UK (the NIMH/Pritzker and GSK GWAS) and analyzed them separately as well as in conjunction with the WTCCC study (Scott et al. 2009). In doing so, no genome-wide significant finding was observed; yet three regions with a p around 10−7 were reported encompassing the genes MCTP1 (which encodes a high-affinity calcium binding protein which is highly expressed in the brain), ITIH1 and GLN3. Furthermore, CTNNA2 was amongst the top hits which also gained support from other hypothesis-free approaches in psychiatric disorders such as ADHD (Lesch et al. 2008). Neither DGKH, ANK3 nor CACNA1C were confirmed in this GWAS, however the latter yielded convincing support upon a fixed-effects meta-analysis including the Ferreira and Schulze studies. In 2009, Kelsoe and associates reported on two GWAS examining US Americans of European and African ancestry (Smith et al. 2009), respectively, with a combined n = 1346 BPD cases. Again, no genome-wide significant findings emerged and interestingly, significant findings were discrepant for each subsample. One of the promising top hits in this study is NTRK2, as this gene which encodes a neurotrophin receptor has been implicated in mood disorders previously. When previous GWAS risk genes were tested for, ANK3 yielded further support, while CACNA1C was negative. It should be noted that this sample overlaps with the one tested by Baum et al.; generally, the sample overlap between different studies will become the rule rather than the exception due to the need for international cooperation and large sample sizes. Furthermore, a small GWAS from Norway (n = 194), which however was followed up in a larger Icelandic sample (Djurovic et al. 2010), provided suggestive evidence for several interesting candidate genes (e.g. GUCY1B2, SHANK, and CNTNAP5), none of which however was amongst the top hits in previous studies. The largest study to date has employed a two-stage design using a discovery cohort of 682 BPD patients and carried over the top 48 SNPs to replication samples; SNPs surviving this procedure were subjected to a meta-analysis with previous BPD GWAS data sets (Cichon et al. 2011). The total case number investigated in this study was thus n = 8441 BPD patients. In doing so, the neurocan (NCAN) gene was identified as a susceptibility factor for BPD with the best SNP yielding a p = 2.1 × 10−9, i.e. genome-wide significance.
In conclusion, GWAS on BPD and subsequent meta-analysis provided evidence that BPD shares risk variants with schizophrenia, MDD, and ADHD; furthermore, calcium and GABA signalling pathways were repeatedly found to be associated with disease, along with genes modifying neuronal plasticity. At the time of writing, CACNA1C, ANK3, and DGKH can be considered the risk genes with the most compelling body of evidence. Accordingly, those are scrutinized more thoroughly and first functional studies already provided evidence for changes in brain function in risk allele carriers.
MDD
While the prevalence of MDD is five to tenfold higher as compared to BPD, its heritability is lower and presumably heterogeneity is even higher. These issues complicate GWAS on this phenotype, probably explaining the lack of genome-wide findings despite the fact that studies on MDD and schizophrenia feature the largest of all disorders analyzed in the PGC.
The NIH sponsored Genetic Association Information Network (GAIN) studies also featured major depression and these studies were amongst the first published GWAS on MDD (Sullivan et al. 2009). Discovery sample patients came from two Dutch longitudinal studies (NESDA and NTR, combined n >1700). The top 25 SNPs featured four SNPs in the PCLO gene, which encodes for a subunit of the presynaptic vesicle fusion complex, although none of them met the criteria for genome-wide significance. Considerable overlap was noted for the mood disorder candidate genes CACNA1C, ANK3, GRM7, and DGKH. While PCLO did not clearly replicate in the Sullivan et al. study, a later reanalysis questioned this initial notion and argued for an association of a non-synonymous coding SNP with MDD in the very same replication cohorts (Bochdanovits et al. 2009). Furthermore, a later population-based study demonstrated an association of PCLO rs2522833 with depressive disorders (Hek et al. 2010), which also held true when a meta-analysis of all published data was conducted especially when only population-based studies were considered (p = 1.9 × 10−9). Most interestingly, in a hypothesis-free approach, PCLO was demonstrated to be differentially expressed and associated with BPD again questioning the diagnostic specificity of GWAS candidate genes (Choi et al. 2011). However, meta-analysis of an MDD and a BPD GWAS did not support a role of PCLO in BPD (Liu et al. 2011).
In a medium-sized GWAS from Germany (Rietschel et al. 2010), there was a suggestive finding for HOMER1 which replicated in an independent sample. In this study, the authors also conducted a genomic imaging study and demonstrated decreased dorsolateral prefrontal cortex activation in the n-back task as well as decreased anterior cingulate cortex activation upon anticipation of a monetary reward in risk allele carriers. Especially the latter might be related to anhedonic behavior, one of the key features of depression. Most interestingly, also CACNA1B was amongst the highest ranked genes, again implicating calcium signalling in affective disorders. A larger (n = 1636 cases) UK-based GWAS argued for the BICC1 gene in MDD (almost needless to say, genome-wide significance was missed); however, it was not replicated in samples from Munich and Lausanne. When all three studies were treated by meta-analysis, the schizophrenia/autism candidate gene NLGN1 was amongst the most promising findings with a p combined = 8.5 × 10−6 (Lewis et al. 2010). When the STAR*D study was analyzed for the phenotype MDD (n = 1,221; Shyn et al. 2011), no genome-wide significant findings also emerged. Promising or previously implicated candidate genes—however, all at a p >10−5—included ANKRD46, CTNND2, and CSMD3. Another recent GWAS focused on recurrent early onset MDD, as defined by an onset before the age of 31 (GenRED, n = 1020; Shi et al. 2011). Nested candidate gene analysis yielded the lowest p value in CACNA1C; as is common for all mood disorder GWAS, there were no findings meeting the genome-wide significance threshold, but several highly suggestive findings with the top hit in a brain-expressed transcript of unknown function. Other interesting candidates include GDNF, SP4, STIM1, KCNQ1, VAMP4, and CSMD1. Most noteworthy, the SP4 signal (which almost entirely came from female subjects) became stronger when the GenRED sample was treated meta-analytically with the STAR*D and GAIN studies (total n cases = 3,957; Shyn et al. 2011). This meta-analysis yielded better, although still only suggestive significance levels and also argued for an association of the GRM7 gene. While SP4 encodes a transcription factor orchestrating gene networks implicated in affective disorders (and most notably, as mentioned above, the SP8 transcription factor has been found in a BPD GWAS), GRM7 which encodes a glutamate receptor was not only of suggestive significance in the WTCCC BPD GWAS, but also amongst the top hits of another MDD GWAS (Muglia et al. 2010). This study was performed in two European samples from Southern Bavaria and Lausanne (total n> 1,500), yet also did not result in genome-wide significant findings or meaningful overlap of top SNPs between both samples. The authors computed a meta-analysis of both samples as well, along with the implementation of gene-wide tests. This interesting method yielded several genes which also survived a correction procedure, the genes with the lowest p-values being SMG7 and NFKB1. Candidate genes from previous studies however did not replicate in this analysis, apart from the glutamate receptor gene GRM7. A similar approach (i.e., discovery GWAS followed by meta-analysis and gene-based tests) was taken by the largest MDD GWAS to date, the MDD2000 + study (Wray et al. 2012). Here, a total of >2400 cases were examined and a meta-analysis was conducted by including the GAIN sample and the UK-based study reported by Lewis et al. (total n> 5700 cases). Suggestive findings (p<10−5) include NOS1AP, ADCY3, and the schizophrenia/autism risk gene CNTNAP2 (the latter in males only). The adenylate cyclase ADCY3 gene was ranked second in the gene-based test, and also the gene encoding galanin (which was previously shown to be associated with antidepressant treatment response and disease severity in MDD and anxiety disorders; Unschuld et al. 2010) was amongst the top ten hits in this analysis. From the pre-selected candidate genes, IL10, OPRM1 (being a candidate stemming from the GAIN MDD GWAS), HTT, HTR1B, GRIN1, and the apparently pleiotropic risk gene CACNA1C were associated with disease. Meta-analysis did not yield significant findings and in particular did not support PCLO as a risk gene for MDD.
Trait depression, as assessed with the NEO-PI personality questionnaire (where “depression” is a subscale of the Neuroticism domain) was assessed in two GWAS in the general population from Sardinia and the US (combined n = 4811; Terracciano et al. 2010). The top hit, at a p = 6 × 10−7, was an intronic SNP in the RORA gene. Two other noteworthy high-ranking candidates include the glutamate receptor gene GRM8, which hitherto has mainly been associated with cognitive phenotypes, and CDH13, which has been identified in an ADHD linkage scan meta-analysis (Zhou et al. 2008) as well as GWAS on ADHD (Lesch et al. 2008) and substance use disorders.
Cross-Disorder Analyses
In order to yield larger samples, several meta-analyses have been conducted. The largest meta-analysis combined the WTCCC, STEP-BD, NIMH-BD, and the German BPD sample, as well as the GAIN-MDD GWAS on MDD. The total number of cases exceeded 6600, compared against >9000 controls (McMahon et al. 2010). An inherent problem with this kind of study is the use of different genotyping platforms, diagnostic heterogeneity, as well as ethnic heterogeneity; to minimize these limitations, only subjects of European descent have been analyzed. In doing so, six SNPs which were located in the PBRM1 gene met the criteria for genome-wide significance. The best SNP was also significant in the replication sample, yielding a final p = 1.7 × 10−9. When the ED-DUB-STEP2 GWAS was analyzed together with an MDD GWAS (Liu et al. 2011), CACNA1C SNPs passed the hurdle of genome-wide significance while ANK3 was not supported in the meta-analysis, probably suggesting that this gene is more specific to BPD. SYNE1 was one of the candidates where the significance level actually increased upon meta-analysis, and which interestingly also turned up in the primary PGC BPD GWAS meta-analysis. Not surprisingly, also schizophrenia and BPD were treated meta-analytically (Wang et al. 2010). In this study, meta-analysis provided evidence for the genes ASTN2 and CNTNAP2, both of which have been implicated in ADHD, as well as the GABA receptors GABRR1 and GABRR2. When the three large US American GWAS on psychiatric disorders and treatment efficacy—namely, STEP-BD (BPD), CATIE (schizophrenia), and STAR*D (MDD) were analyzed jointly (yielding a total n cases >3000; (Huang et al. 2010), one locus met the criteria for being genome-wide significant (near the ADM gene, and apparently being specific for bipolar II disorder). A total of 24 more SNPs reached the defined Omnibus GWAS Test Threshold; however, more than half of them were imputed. Promising candidates are again CTNND2, SP8, ODZ4, and NPAS3.
An alternative rationale is to search for risk variants influencing phenotypic features of mood disorders. Suitable phenotypes include, for example, therapy response (see below) or suicidal ideation. Accordingly, the STEP-BP, WTCCC, UCL, and STAR*D studies were evaluated with respect to the latter (Perlis et al. 2010). None of the 11 loci which were identified in the discovery cohorts however replicated. Also, candidate genes which were selected according to previous data (such as HTR1A or TPH2) did not yield convincing evidence. Meta-analysis of all samples argued for an involvement of SORBS1 and PRKCE, a gene with some a priori biological evidence. Analysis of STAR*D alone, where 90 out of 1953 patients developed treatment-emergent suicidal ideation (Laje et al. 2009), revealed a highly significant association of an SNP in PAPLN and suggestive association of an IL28RA SNP. Additive effects with previous risk alleles for treatment-associated suicidal ideation in the GRIK2 and GRIA3 genes were observed. However, paucity of psychometric data on the suicidal patients along with the very limited sample size bears the high chance of a type-I error. Similar analyses in GENDEP (total n = 706, thereof n = 244 with treatment-associated suicidal ideation under treatment with either escitalopram or nortriptyline; Perroud et al. 2010) provided some evidence for the genes GDA, KCNIP4, and ELP3 to be associated with escitalopram-associated suicidal ideation. Nested candidate-driven approaches did not yield significant results. A major concern regarding these studies is whether or not treatment-associated suicidal ideation is genetic at all and whether these studies are homogeneous—the striking differences in the percentage of suicidal ideation casts some doubts on this assumption.
Analysis of the complete PGC data set, comprising 12,000 BPD cases and 52,000 controls, yielded 21 SNPs with a corrected p <0.05, the best candidate genes being CACNA1C, ODZ4, and two regions of chromosome 11 and 12. As also suggested from earlier cross-disorder analyses demonstrating a significant overlap of common risk variants for BPD and schizophrenia (including also CACNA1C, as well as another voltage-dependent calcium channel and a member of the diacylglycerol kinase family [DGKI]; Moskvina et al. 2009), the latest cross-disorder analysis of the PGC yielded strong evidence for an association of CACNA1C with endogenous psychoses as evidenced by p = 8.45 × 10−9 when BPD and schizophrenia samples were combined. In these analyses, it became also evident that BPD risk genes were highly predictive for schizophrenia, and vice versa. On the other hand, BPD neither predicted MDD nor did MDD predict BPD or schizophrenia. When all three disorders were pooled together (total n cases >25,000), six genes met the criteria for genome-wide significance: ITIH3, the HLA/HIST cluster on chromosome 6p21-p22, CACNA1C, TCF4, NT5C2/CNNM2, and IFI44/ELTD1. In MDD alone, the situation is much more frustrating: when combining more than 11,000 cases from the GAIN, GenRED, GSK, mdd2000, MPIP, RADIANT, STAR*D, and NGFN Germany studies, only two SNPs (in the genes NVL and GPHN, which is a highly interesting candidate) came near the level of genome-wide significance. Lower heritability in conjunction with increased heterogeneity might explain the scarcity of solid findings in MDD as compared to BPD.
1.2.4 Copy Number Variations
Currently, there is increasing interest about the role of deletions/duplications of large chunks of the genome (copy number variations, CNVs) in psychiatric disorders. Especially large (>100 kb) and rare CNV harboring many different genes seem to occur more often in schizophrenia, mental retardation, and autism—although there is no diagnostic specificity and some CNVs might underlie any of these three conditions. In any case, these CNVs are rare and can only account for a small percentage of cases, again arguing for a “common disease, multiple rare variant” model. In bipolar disorder, there are only two studies to date which yielded conflicting findings. While the first study (Zhang et al. 2009a; 1001 patients) demonstrated an excess of large (>100 kb) and rare CNVs in BPD, Grozeva et al. (2010) did not find an increased rate of large and rare CNVs in almost 1700 patients suffering from BPD. Hence, even larger samples are needed to unequivocally evaluate the contribution of CNVs in BPD, although from the present data it seems to be clear that at least large and rare CNVs can only account for a very small fraction of BPD cases, if at all.
1.3 Pharmacogenetics
In the treatment of depression, antidepressive pharmacotherapeutic agents have proven to be highly effective for a large proportion of patients. However, two major problems have to be faced: (1) treatment resistance: 30–40% of all patients fail to respond sufficiently to the initial treatment (Fava and Davidson 1996) and (2) treatment intolerance: There is a considerable rate of “treatment emergent adverse effects” associated with antidepressive pharmacotherapy such as hypotension, weight gain, anticholinergic effects, antidepressant-induced mania, or sleep disturbance, which leads to discontinuation of treatment in about 10% of the cases (MacGillivray et al. 2003).
Among multiple reasons underlying non-response to antidepressive pharmacotherapy or differential development of treatment emergent adverse effects under antidepressants, it has been suggested that psychotropic drug response may be heritable with first-degree relative pairs being significantly concordant for antidepressant treatment response (Pare et al. 1971; O’Reilly et al. 1994; Franchini et al. 1998). Pharmacogenetic studies allowing for the detailed dissection of the genetically influenced heterogeneity of psychotropic drug response have revealed several risk genes on a pharmacokinetic as well as on a pharmacodynamic level to drive antidepressant treatment response. On a pharmacokinetic level, variation in the CYP2D6 gene resulting either in poor metabolizers (PM; 7% of the Caucasian population) or in rapid (RM) or even ultrarapid metabolizers (UM; 3% of the Caucasian population) has been reported to be associated with response to tricyclic antidepressants and SSRIs, particularly paroxetine (cf. Kirchheiner et al. 2004). On a pharmacodynamic level, association of response to antidepressants has been observed with variation in candidate genes of depression, especially those involved in the serotonergic system (e.g. SLC6A4, HTR1A, HTR2A, MAOA, TPH1 (for a review see Kato and Serretti 2010; Serretti et al. 2005). Additionally, there is first evidence for differential genetic effects on treatment response specifically in melancholic depression (Baune et al. 2008), depression with comorbid anxiety (Domschke et al. 2008a, 2010) or in gender subgroups (Domschke et al. 2008c). The identification of genetic risk factors for antidepressant treatment response as known to date tremendously helps in better understanding the mechanism of action of antidepressants. These rapidly growing molecular genetic findings might nourish further biochemical, physiological, or pharmacological studies and eventually lead to a personalized medicine with an individually tailored antidepressive pharmacotherapy according to genotype reducing the patients’ suffering and lowering healthcare costs at the same time.
Most of the MDD GWAS were embedded in efficacy studies; thus not surprisingly, treatment response GWAS were reported frequently. It should be noted that treatment response of course encompasses a plethora of diverse factors ranging from adherence to medication to exogenous pharmacokinetic influences, adding further noise to already noisy genetic data. The first report was on the German MARS trial and also included an independent German sample as well as the STAR*D study (Ising et al. 2009). Obviously, not only diagnostic but also treatment heterogeneity has to be taken into account in the interpretation. The best signal, which however was not significant on the genome-wide level, came from an SNP in the 5′ region of CDH17; when the 338 best SNPs from the German samples were tested in the STAR*D sample, 46 were associated at the nominal level of significance. Amongst them, interestingly, was HOMER1 (see above). When the level 1 participants of STAR*D, which received citalopram, were analyzed separately (743 remitters versus 608 non-remitters; Garriock and Hamilton 2009a, b), as little as three SNPs were associated with response on the p< 1 × 10−5 level. The most interesting finding from this study probably is ARNTL, which is also a member of the PAS superfamily and related to NPAS3. In 2010, the GWAS data of the multicentre European GENDEP study was published (n = 811 cases, treated with either nortriptyline or escitalopram; Uher et al. 2010). Analysis of the complete sample did not provide meaningful signals, while analysis of either compound alone pointed to the IL11, UST, and RGL1 genes. Genotype by drug interaction analyses interestingly implicated a region 11 kb downstream of NOL4, which was also one of the four top regions in the STAR*D study. As both studies were published in parallel, this was not mentioned in either paper, yet can be considered a true independent replication.
As compared to MDD, pharmacogenomics studies in BPD are sparser. As treatment response to lithium, the gold standard drug treatment in BPD, is familial, lithium treatment response studies seem to be most worthwhile; as only ca. 40% of all BPD patients can be considered clear lithium responders, and as treatment might go along with considerable side effects in the case of non-response, data on genetic prediction of lithium response would directly translate into the clinical routine. Several case–control association studies comparing responders to non-responders have suggested a variety of risk genes such as the SLC6A4 (seven studies, mixed findings) and other hypothesis-driven targets mainly of neurotransmitter pathways, intracellular signal transduction pathways involved in the mechanism of action of lithium, and circadian clock genes. GSK3B and CREB1 are amongst the candidates with the best empirical support and also good face validity and hence should be further tested, as evidence is far from being solid. Samples were often rather small and again, most genes lack replication. Scholarly overviews on published association studies can be obtained from McCarthy et al. (2010) and Smith et al. (2010). Although not specifically designed for this question, the STEP-BD trial tested for lithium response as well by means of a GWA study, which was replicated in a second, independent sample (n = 458, and n = 359 bipolar I or II patients, respectively). Not surprisingly, there were no genome-wide significant findings, however five SNPs associated in the STEP-BD cohort replicated in the second sample including a polymorphism within the GRIA2 gene (Perlis et al. 2009). To specifically search for lithium response genes, the ConLiGen consortium (Schulze et al. 2010) has gathered more than 1200 lithium treated BPD patients whose treatment response has been evaluated using the Alda scale. Genome-wide genotyping has been accomplished and initial data are expected for the second half of 2011.
2 Anxiety Disorders
2.1 Clinical Genetics
Panic disorder has been found to be highly familial with an up to three to fivefold increased prevalence of the disorder in first-degree relatives of patients with panic disorder (Horwath et al. 1995; Maier et al. 1993; Hettema et al. 2001). In relatives of the subgroup of patients with panic disorder and suffocation anxiety, an even higher familiarity has been discerned (Horwath et al. 1997). Furthermore, familiarity of panic disorder seems to depend on the age of onset in the index patient with an onset before the age of 20 years predicting a 17-fold increased risk of panic disorder in first-degree relatives (Goldstein et al. 1997). Also for generalized anxiety disorder and specific phobias a significant familial aggregation was reported (Hettema et al. 2001; Marks and Herst 1970).
Twin studies have identified up to 2–3 times higher concordance rates for panic disorder in monozygotic as compared to dizygotic twins (Skre et al. 1993), with an even higher concordance rate for the subgroup of patients with carbon dioxide-sensitive panic disorder (Bellodi et al. 1998). According to a comprehensive meta-analysis, the contribution of genetic factors has been calculated to be as high as up to 48%, with the remaining 52% being attributable to individual environmental factors. Generalized anxiety disorder has been estimated to have a heritability of about 32%, while the common heritability of phobias was reported to be about 30%, with highest estimates for agoraphobia (67%), blood-injection-phobia (59%), and social phobia (51%). The heritability of posttraumatic stress disorder was reported to be about 20–30% (Kendler et al. 1999; Hettema et al. 2001; Segman and Shalev 2003). Finally, several studies point towards overlapping genetic risk factors for panic disorder and agoraphobia or other phobias, respectively (Kendler et al. 1995; Mosing et al. 2009; Tsuang et al. 2004). In panic disorder and other anxiety disorders, segregation analyses failed to identify a mode of inheritance according to Mendelian patterns, which points to a complex genetic inheritance with an interaction of multiple “vulnerability” or “risk genes”, each with only a minor individual influence (“oligo- or polygenic model”), and environmental influences (Vieland et al. 1996).
2.2 Molecular Genetics
2.2.1 Linkage Studies
In panic disorder, linkage studies have yielded a variety of potential risk loci on chromosomes 1p, 4q, 7p, 9q, 11p, 15q, und 20p (Crowe et al. 1987, 2001; Knowles et al. 1998; Gelernter et al. 2001; Hamilton et al. 2003; Thorgeirsson et al. 2003; Fyer et al. 2006; Kaabi et al. 2006). In subgroups of patients with panic disorder with comorbid bipolar disorder or kidney/bladder dysfunction, respectively, risk loci on chromosomes 2, 12, 13, and 18 or 13 and 22, respectively, have been described (MacKinnon et al. 1998; Logue et al. 2009; Weissman et al. 2000; Hamilton et al. 2003). In social or specific phobia, linkage studies have excluded a major influence of HTR2A and SLC6A4 loci, with however, some evidence for potential risk loci on chromosomes 16q and 14p (Stein et al. 1998; Gelernter et al. 2003, 2004).
2.2.2 Association Studies
In panic disorder, a variety of association studies has been published so far. Most studies have investigated variation in classical candidate genes for panic disorder as suggested by animal models (e.g. knock-out mice), challenge experiments (e.g. cholecystokinin [CCK] challenge, caffeine challenge), or pharmacological observations (e.g. clinical efficacy of selective serotonin reuptake inhibitors (SSRIs), monoamine oxidase (MAO) inhibitors). Most significant evidence has been yielded for association of variants in the CCKBR (Kennedy et al. 1999; Hösing et al. 2004), MAOA, particularly in female patients (Deckert et al. 1999; Samochowiec et al. 2004; Maron et al. 2005b), COMT (again restricted to female patients, Hamilton et al. 2002; Domschke et al. 2004; Woo et al. 2002; Woo et al. 2004; Domschke et al. 2007; Zintzaras and Sakelaridis 2007), HTR1A (Rothe et al. 2004; Huang et al. 2004) and ADORA2A (Deckert et al. 1998; Hamilton et al. 2004a; Hohoff et al. 2010). Furthermore, there is some evidence for several other potential risk variants to be involved in the pathogenesis of panic disorder such as polymorphisms in HTR2A (Inada et al. 2003; Rothe et al. 2004; Maron et al. 2005a; Unschuld et al. 2007; Yoon et al. 2008), SLC6A4 (Ohara et al. 1998; Maron et al. 2005a, b; Strug et al. 2010; but: Deckert et al. 1997; Hamilton et al. 1999; Blaya et al. 2007), TPH2 (Maron et al. 2007; Kim et al. 2009; but: Mössner et al. 2006), NET (Lee et al. 2005; but: Sand et al. 2002a), CCK (Wang et al. 1998; Hattori et al. 2001), ACE (Olsson et al. 2004; Erhardt et al. 2008; Bandelow et al. 2010; but: Shimizu et al. 2004), the transcription factor CREM (Domschke et al. 2003; Hamilton et al. 2004b), ‚regulator of G-protein signaling’ (RGS2, RGS7) (Leygraf et al. 2006, Smoller et al. 2008b; Hohoff et al. 2009b) and several hormone receptors (Sand et al. 2002b; Ho et al. 2004; Keck et al. 2008; Hodges et al. 2009). However, since most of these studies either did not withstand replication in independent samples or still warrant replication, these results have to be considered preliminary. The role of the GABA-ergic system in panic disorder remains to be further elucidated on a molecular genetic level with only little evidence so far for the glutamate decarboxylase (GAD) or GABA receptors and transporters, respectively (Crowe et al. 1997; Sand et al. 2000; Hettema et al. 2006; Nakamura et al. 2006; Kobayashi et al. 2007; Thoeringer et al. 2007, 2009; Unschuld et al. 2009). Recently, besides the classic neurotransmitter systems much attention has been paid to the role of neuropeptides in the mediation of anxiety. Significant association of anxiety or panic disorder in particular have been reported for variants in genes for galanin (Unschuld et al. 2008), the neuropeptide Y (NPY) system (Domschke et al. 2008b) and the neuropeptide S receptor (NPSR) (Domschke et al. 2011). Finally, there is preliminary support for possible interactive effects of several genetics variants in the mediation of the genetic risk for panic disorder, e.g. for HTR1A and COMT (Freitag et al. 2006). For social phobia and generalized anxiety disorder, association has been reported with variation in the dopamine transporter (SLC6A3) gene (Rowe et al. 1998), while DRD2 variants seem to play a role in the pathogenesis of posttraumatic stress disorder (Segman and Shalev 2003). Further associations were observed for COMT in specific phobias (McGrath et al. 2004), for HTR2A in social phobia (Lochner et al. 2007) and MAOA in generalized anxiety disorder (Tadic et al. 2003).
In summary, consistent with findings from clinical genetic and linkage studies, molecular genetic association studies point to a complex genetic etiology of anxiety disorders with an additive or rather interactive effect of multiple risk variants.
2.2.3 Genome-Wide Association Studies
The first genome-wide association study in panic disorder in a Japanese sample yielded evidence for several markers in genes, which have not been implicated in the pathogenesis of anxiety before (PKP1, PLEKHG1, TMEM16B, CALCOCO1, SDK2, and CLU) (Otowa et al. 2009). However, these findings could not be replicated in a follow-up GWAS by the same group (Otowa et al. 2010). Another genome-wide association study in three German samples points to a potential role of the TMEM132D gene in the pathogenesis of panic disorder (Erhardt et al. 2011). Currently, another large GWAS on a homogenous sample from Germany is under analysis (Reif et al., in preparation).
2.3 Genetics of Intermediate Phenotypes of Anxiety Disorders
Dimensional markers such as neuroticism, anxiety sensitivity, state or trait anxiety or behavioral inhibition have been proposed as valid intermediate phenotypes of anxiety disorders with aggregation in families and elevated concordance rates in monozygotic twins pointing to a significant heritability (e.g. Rosenbaum et al. 1991; Maier et al. 1992; Stein et al. 1999). Linkage studies have discerned risk loci on chromosomes 8, 18, 20, and 21 for harm avoidance (e.g. Cloninger et al. 1998), and association studies have reported a potential role of genetic variation of e.g. SLC6A4 for harm avoidance and neuroticism (Lesch et al. 1996) and the corticotropin releasing hormone (CRH) for behavioral inhibition (Smoller et al. 2003, 2005), respectively.
Besides neuropsychological markers, more recently, neurobiological traits have been investigated as intermediate phenotypes of anxiety disorders. Here, significant association was observed, for e.g. increased sympathetic activity and ADORA2A as well as COMT gene variation (Hohoff et al. 2009a; Kang et al. 2010), blushing propensity in social phobia with SLC6A4 variation (Domschke et al. 2009), an increased startle response with COMT and SLC6A4 variants (e.g. Montag et al. 2008; Brocke et al. 2006), as well as CO2-sensitivity to panic attacks with again SLC6A4 variation (Schmidt et al. 2000; Schruers et al. 2011).
Another very promising intermediate phenotype of mental disorders in general and affective and anxiety disorders in particular are neuronal activation correlates of emotional processing as captured by functional imaging techniques such as magnetic resonance imaging (fMRI). In panic disorder, first imaging genetics findings may indicate a distorted corticolimbic interaction depending on variants of the COMT and HTR1A (Domschke et al. 2006, 2008d). In patients with social phobia, polymorphisms in SLC6A4 and TPH were found to be associated with increased amygdala excitability (Furmark et al. 2004, 2008, 2009). Finally, markers spanning RGS2 were reported to be associated with childhood behavioral inhibition and with increased limbic activation during emotion processing (Smoller et al. 2008b). In summary, these first imaging genetics findings in panic disorder, social phobia, and anxiety-related traits may indicate that—depending on variants of COMT, SLC6A4, HTR1A, and RGS2—patients with anxiety disorders are prone to impaired cerebral processing of anxiety-related stimuli in cortical regions known to play a crucial role in the evaluation of emotional stimuli and determination of salient events (for a review see Domschke and Dannlowski 2010).
2.4 Gene-Environment Interaction
In contrast to a multitude of gene-environment studies (GxE) available in depression (see 1.2.2., e.g. SLC6A4 and FKBP5), with respect to anxiety disorders as a categorical nosological entity or anxiety-related traits, to the best of our knowledge only few GxE studies have been performed yet (for a review see Klauke et al. 2010). No associations were found between 5-HTTLPR, childhood emotional abuse, and neuroticism (Antypa and Van der Does 2010). An exemplary GxE study with respect to anxiety-related traits has been published by Stein et al. (2008), who observed a significant interaction between levels of childhood maltreatment and the less active 5-HTTLPR S allele on anxiety sensitivity as measured by the anxiety sensitivity index (ASI). 5-HTTLPR S and LG haplotypes were furthermore reported to be associated with increased anxiety in interaction with daily stressors (Gunthert et al. 2007). Conversely, assessing 5-HTTLPR genotype and environmental adversity at birth (family adversity) and at 19 years of age (stressful life events), Laucht et al. (2009) found an interactive effect of more active 5-HTTLPR LL genotype and high family adversity on anxiety disorders. Other studies have identified association of the ADORA2A with increased anxiety after caffeine administration in healthy volunteers, demonstrating that a panic disorder risk gene might drive the sensitivity to an environmental stimulus and, therefore, the vulnerability to anxiety (Alsene et al. 2003; Childs et al. 2008).
2.5 Pharmacogenetics
In anxiety disorders, so far only three exemplary studies have investigated the impact of genetic variants on response to a pharmacological treatment regime. Two groups reported significant association of 5-HTTLPR with response to SSRI treatment in panic disorder as well as in generalized anxiety disorder (Perna et al. 2005; Stein et al. 2006). Furthermore, SSRI treatment in panic disorder might in part be driven by variation in HTR1A (Yevtushenko et al. 2010).
3 Overlapping Phenotypes
Depression and anxiety are highly comorbid with up to 60% of patients with depression also displaying anxiety (Leckman et al. 1983) and about 58% of those patients actually meeting DSM criteria for anxiety disorders (see review by Lydiard 1991; e.g. de Graaf et al. 2002; Kessler et al. 1996; Zimmerman et al. 2002). Comorbidity of affective and anxiety disorders has a significant impact on the course and treatment of the respective leading disease with a more chronic course and a significantly detrimental effect on treatment response (e.g. Clayton et al. 1991; Liebowitz 1993; Lydiard 1991). Patterns of occurrence allow for both affective and anxiety disorders preceding the respective other disease.
Besides either simultaneous or sequential true comorbidity of anxiety disorders and major depression there is a continuous debate about a possible overlapping phenotype between anxiety disorders and depression. The clinical phenotype of “anxious depression” (Overall et al. 1966; Overall and Zisook 1980) capturing major depression with subthreshold anxious features has been suggested to constitute a diagnostic entity of its own requiring specific diagnostic and therapeutic attention (see Levine et al. 2001; Lydiard and Brawman-Mintzer 1998; Silverstone and von Studnitz 2003). Dual action drugs acting as reuptake inhibitors on both transporters (serotonin and norepinephrine reuptake inhibitors, SNRI) have been suggested to be superior to SSRI only or tricyclic antidepressants TCA in the treatment of anxious depression (Rudolph et al. 1998; Silverstone and Ravindran 1999). While three large meta-analyses discerned similar response rates to antidepressant treatment in highly anxious and less anxious patients with major depression (Levine et al. 2001; Nelson et al. 2009; Papakostas et al. 2008; see Nelson 2008), there is accumulating evidence for anxious features of depression potentially complicating the course of antidepressant treatment (e.g. Altamura et al. 2004; Domschke et al. 2010; Fava et al. 2008; Joffe et al. 1993; see review by Bagby et al. 2002).
Apart from the individual genetic risk for affective and anxiety disorders, both disease entities also exhibit a common familial risk (as reviewed by Middeldorp et al. 2005). There is evidence from twin studies that depression and general anxiety disorder, panic disorder, and post-traumatic stress disorder share a considerable proportion of their genetic risk (Kendler et al. 1992, 2007; Kendler 1996; Roy et al. 1995). Consistently, molecular genetic studies have yielded evidence for specific genetic loci that may generally influence susceptibility across the anxiety-depression spectrum, e.g. on chromosome 18q (cf. Camp et al. 2005; Hettema 2008). In particular, the combined clinical phenotype of anxious depression has been suggested to constitute a specific subtype with an increased familial risk of depression (Clayton et al. 1990, 1991), which points to a possibly increased heritability of anxious depression with a specific set of genetic risk factors mediating the vulnerability for the development of anxious depression. First imaging and pharmacogenetic studies in anxious depression have implied CNR1, NPY, and SLC6A4 to confer parts of antidepressant treatment response particularly in the clinical phenotype of anxious depression, potentially via a dysfunctional corticolimbic interaction underlying distorted emotional processing (e.g. Baffa et al. 2010; Domschke et al. 2008a; 2010).
These molecular and imaging genetic findings of overlapping genetic variants as well as common brain networks of emotional processing partly driving both clinical phenotypes of anxiety and affective disorders point to similar neurobiological mechanisms underlying these disorders and therefore possibly a common clinical sub-phenotype shared by anxiety and affective disorders. Particularly, the clinical phenotype of “anxious depression” might thus possibly constitute a diagnostic entity of its own requiring specific diagnostic and therapeutic attention (cf. Lydiard and Brawman-Mintzer 1998; Silverstone and von Studnitz 2003). So, back from bench to bedside, genetic and imaging studies might inspire a re-evaluation and refinement of DSM-IV categorized nosological concepts of depression and anxiety. Alternatively, the current and still emerging body of knowledge in the field of neurobiological research in anxiety and depression might have even more far-reaching consequences in the future by challenging the DSM concept in itself in favor of a more neurobiologically oriented taxonomy of mental disorders. As suggested by Smoller et al. (2008a), genetic and imaging research revealing etiological mechanisms of mental disorders might infer a novel nosological concept based on pathogenesis more than phenomenology. To date, however, despite first essential steps having been made, neurobiological knowledge about the pathomechanism of depression and anxiety has still not progressed far enough to provide a reliable and valid fundament for diagnostic decisions in daily clinical practice. So, in summary the presently known vulnerability genes and patterns of affective and anxiety disorders are slowly beginning to challenge the DSM-defined nosological boundaries and might have the potential to evolve into a valuable tool to more precisely delineate the diagnostic system of mental disorders in the future.
4 Outlook
Future research with respect to the genetic dissection of affective and anxiety disorders will have to comprise technical as well as clinical aspects. On a molecular genetic level, more comprehensive analyses such as tagging SNP approaches, haplotype analyses, as well as the investigation of epistasis of several genes constituting relevant biochemical pathways or cascades are warranted. Here, novel genomic techniques such as duplication/deletion analysis using genotyping arrays and next-generation sequencing of the whole exome or genome for point mutation identification might have a large impact on risk gene identification. Furthermore, it will be of utmost importance to analyze the functional consequences of the associated genetic variants and thereby gain more knowledge about the pathomechanism of the disease of interest. Additionally, there is a need for more detailed gene-environment interaction studies potentially also in a genome-wide fashion (cf. Poulton et al. 2008; Thomas 2010) in order to disentangle the interactive effect of genetic and environmental factors conferring risk or resilience, respectively, to affective and anxiety disorders. In this respect, epigenetic studies investigating e.g. DNA methylation or histone modifications regulating gene activity will tremendously contribute to the elucidation of the interplay between environmental and genetic factors in the pathogenesis of affective and anxiety disorders (cf. for bipolar disorder and schizophrenia: Abdolmaleky et al. 2006, 2008).
Besides the more technical aspects as detailed above, future research in the genetics of affective and anxiety disorders will greatly benefit from clinical considerations. Given that—apart from very few results—most linkage and association findings either did not withstand replication in independent samples or still warrant replication and given that genome-wide association studies in affective as well as in anxiety disorders so far fell short of expectations regarding replicating previous candidate genes or generating novel hypotheses, one possible reason might be the great neuropsychological and neurobiological heterogeneity of the investigated phenotypes of categorical nosological entities as defined by DSM- or ICD-criteria. Thus, besides the recruitment of even larger sample sizes, a more precise definition of the clinical phenotype will be key. In the latter respect, the approach of investigating intermediate phenotypes of affective and anxiety disorders will have to be intensified with the search for novel depression- and/or anxiety-related neurophysiological, biochemical, endocrinological, neuroanatomical, cognitive, or neuropsychological endophenotypes (cf. for major depression: Hasler et al. 2004) and their analysis with respect to their genetic basis.
In summary, to date there is some support for several risk genes contributing to the development of affective and anxiety disorders or their intermediate phenotypes and some light has been shed on gene-environment interactions contributing to the disease risk. However, so far the identified genetic risk factors are of no diagnostic or predictive value, which will only change if the entirety of all genetic risk factors interdependent with environmental factors is identified, which is not foreseeable in the near future. Nevertheless, the increasing elucidation of genetic risk factors tremendously helps in better understanding the pathophysiology of affective and anxiety disorders and might nourish the development of innovative pharmacotherapeutic substances in the treatment of these diseases (e.g. Domschke and Zwanzger 2008), preferably in an individually tailored manner according to genotype.
References
Abdolmaleky HM, Cheng KH, Faraone SV et al (2006) Hypomethylation of MB-COMT promoter is a major risk factor for schizophrenia and bipolar disorder. Hum Mol Genet 15:3132–3145
Abdolmaleky HM, Zhou JR, Thiagalingam S et al (2008) Epigenetic and pharmacoepigenomic studies of major psychoses and potentials for therapeutics. Pharmacogenomics 9:1809–1823
Abkevich V, Camp NJ, Hensel CH et al (2003) Predisposition locus for major depression at chromosome 12q22–12q23.2. Am J Hum Genet 73:1271–1281
Alsene K, Deckert J, Sand P et al (2003) Association between A2a receptor gene polymorphisms and caffeine-induced anxiety. Neuropsychopharmacology 28:1694–1702
Altamura AC, Montresor C, Salvadori D et al (2004) Does comorbid subthreshold anxiety affect clinical presentation and treatment response in depression? A preliminary 12-month naturalistic study. Int J Neuropsychopharmacol 7:481–487
Angst J, Cui L, Swendsen J et al (2010) Major depressive disorder with subthreshold bipolarity in the National Comorbidity Survey Replication. Am J Psychiatry 167:1194–1201
Antypa N, Van der Does J (2010) Serotonin transporter gene, childhood emotional abuse and cognitive vulnerability to depression. Genes Brain Behav 9:615–620
Appel K, Schwahn C, Mahler J, Schulz A, Spitzer C, Fenske K, Stender J, Barnow S, John U, Teumer A, Biffar R, Nauck M, Völzke H, Freyberger HJ, Grabe HJ (2011) Moderation of adult depression by a polymorphism in the FKBP5 gene and childhood physical abuse in the general population. Neuropsychopharmacology 36(10):1982–1991
Athanasiu L, Mattingsdal M, Kahler AK et al (2010) Gene variants associated with schizophrenia in a Norwegian genome-wide study are replicated in a large European cohort. J Psychiatr Res 44:748–753
Badner JA, Gershon ES (2002) Meta-analysis of whole-genome linkage scans of bipolar disorder and schizophrenia. Mol Psychiatry 7:405–411
Baffa A, Hohoff C, Baune BT et al (2010) Norepinephrine and serotonin transporter genes: impact on treatment response in depression. Neuropsychobiology 62:121–131
Bagby RM, Ryder AG, Cristi C (2002) Psychosocial and clinical predictors of response to pharmacotherapy for depression. Rev Psychiatr Neurosci 27:250–257
Bandelow B, Saleh K, Pauls J et al (2010) Insertion/deletion polymorphism in the gene for angiotensin converting enzyme (ACE) in panic disorder: A gender-specific effect? World J Biol Psychiatry 11:66–70
Barnett JH, Smoller JW (2009) The genetics of bipolar disorder. Neuroscience 164:331–343
Baum AE, Akula N, Cabanero M et al (2008a) A genome-wide association study implicates diacylglycerol kinase eta (DGKH) and several other genes in the etiology of bipolar disorder. Mol Psychiatry 13:197–207
Baum AE, Hamshere M, Green E et al (2008b) Meta-analysis of two genome-wide association studies of bipolar disorder reveals important points of agreement. Mol Psychiatry 13:466–467
Baune BT, Hohoff C, Roehrs T et al (2008) Serotonin receptor 1A–1019C/G variant: Impact on antidepressant pharmacoresponse in melancholic depression? Neurosci Lett 436:111–115
Bellodi L, Perna G, Caldirola D et al (1998) CO2-induced panic attacks: a twin study. Am J Psychiatry 155:1184–1188
Berrettini WH (2001) Molecular linkage studies of bipolar disorders. Bipolar Disord 3:276–283
Binder EB (2009) The role of FKBP5, a co-chaperone of the glucocorticoid receptor in the pathogenesis and therapy of affective and anxiety disorders. Psychoneuroendocrinology 34(Suppl 1):186–195
Binder EB, Bradley RG, Liu W et al (2008) Association of FKBP5 polymorphisms and childhood abuse with risk of posttraumatic stress disorder symptoms in adults. JAMA 299:1291–1305
Binder EB, Salyakina D, Lichtner P et al (2004) Polymorphisms in FKBP5 are associated with increased recurrence of depressive episodes and rapid response to antidepressant treatment. Nat Genet 36:1319–1325
Blaya C, Salum GA, Lima MS et al (2007) Lack of association between the Serotonin Transporter Promoter Polymorphism (5-HTTLPR) and panic disorder: a systematic review and meta-analysis. Behav Brain Funct 3:41
Bochdanovits Z, Verhage M, Smit AB et al (2009) Joint reanalysis of 29 correlated SNPs supports the role of PCLO/Piccolo as a causal risk factor for major depressive disorder. Mol Psychiatry 14:650–652
Bosker FJ, Hartman CA, Nolte IM et al (2011) Poor replication of candidate genes for major depressive disorder using genome-wide association data. Mol Psychiatry 16:516–532
Bradley RG, Binder EB, Epstein MP et al (2008) Influence of child abuse on adult depression: moderation by the corticotropin-releasing hormone receptor gene. Arch Gen Psychiatry 65:190–200
Brent D, Melhem N, Ferrell R et al (2010) Association of FKBP5 polymorphisms with suicidal events in the treatment of resistant depression in adolescents (TORDIA) study. Am J Psychiatry 167:190–197
Brocke B, Armbruster D, Muller J et al (2006) Serotonin transporter gene variation impacts innate fear processing: acoustic startle response and emotional startle. Mol Psychiatry 11:1106–1112
Camp NJ, Lowry MR, Richards RL et al (2005) Genome-wide linkage analyses of extended Utah pedigrees identifies loci that influence recurrent, early-onset major depression and anxiety disorders. Am J Med Genet B Neuropsychiatr Genet 135:85–93
Casamassima F, Huang J, Fava M et al (2010) Phenotypic effects of a bipolar liability gene among individuals with major depressive disorder. Am J Med Genet B Neuropsychiatr Genet 153:303–309
Caspi A, Sugden K, Moffitt TE et al (2003) Influence of life stress on depression: moderation by a polymorphism in the 5-HTT gene. Science 301:386–389
Chen C, Glatt SJ, Tsuang MT (2008) The tryptophan hydroxylase gene influences risk for bipolar disorder but not major depressive disorder: results of meta-analyses. Bipolar Disord 10:816–821
Chen D, Liu F, Yang C, Liang X, Shang Q, He W, Wang Z (2011) Association between the TPH1A218C polymorphism and risk of mood disorders and alcohol dependence: evidence from the current studies. J Affect Disord (in press)
Chen Z, Liu Y, Zhang D (2009) C677T methylenetetrahydrofolate reductase gene polymorphisms in bipolar disorder: an association study in the Chinese population and a meta-analysis of genetic association studies. Neurosci Lett 449:48–51
Childs E, Hohoff C, Deckert J et al (2008) Association between ADORA2A and DRD2 polymorphisms and caffeine-induced anxiety. Neuropsychopharmacology 33:2791–2800
Cho HJ, Meira-Lima I, Cordeiro Q et al (2005) Population-based and family-based studies on the serotonin transporter gene polymorphisms and bipolar disorder: a systematic review and meta-analysis. Mol Psychiatry 10:771–781
Choi KH, Higgs BW, Wendland JR et al (2011) Gene expression and genetic variation data implicate PCLO in bipolar disorder. Biol Psychiatry 69:353–359
Cichon S, Muhleisen TW, Degenhardt FA et al (2011) Genome-wide association study identifies genetic variation in neurocan as a susceptibility factor for bipolar disorder. Am J Hum Genet 88:372–381
Cichon S, Winge I, Mattheisen M et al (2008) Brain-specific tryptophan hydroxylase 2 (TPH2): a functional Pro206Ser substitution and variation in the 5′-region are associated with bipolar affective disorder. Hum Mol Genet 17:87–97
Clarke H, Flint J, Attwood AS et al (2010) Association of the 5- HTTLPR genotype and unipolar depression: a meta-analysis. Psychol Med 40:1767–1778
Clayton PJ (1990) The comorbidity factor: establishing the primary diagnosis in patients with mixed symptoms of anxiety and depression. J Clin Psychiatry 51:35–39
Clayton PJ, Grove WM, Coryell W et al (1991) Follow-up and family study of anxious depression. Am J Psychiatry 148:1512–1517
Cloninger CR, Van-Erdewegh P, Goate A et al (1998) Anxiety proneness linked to epistatic loci in genome scan of human personality traits. Am J Med Genet 81:313–317
Cohen-Woods S, Craig I, Gaysina D et al (2010) The bipolar association case-control study (BACCS) and meta-analysis: no association with the 5, 10-Methylenetetrahydrofolate reductase gene and bipolar disorder. Am J Med Genet B Neuropsychiatr Genet 153:1298–1304
Craddock N, Sklar P (2009) Genetics of bipolar disorder: successful start to a long journey. Trends Genet 25:99–105
Crowe RR, Goedken R, Samuelson S (2001) Genome wide survey of panic disorder. Am J Med Genet 105:105–109
Crowe RR, Noyes R Jr, Wilson AF (1987) A linkage study of panic disorder. Arch Gen Psychiatry 44:933–937
Crowe RR, Wang Z, Noyes R Jr (1997) Candidate gene study of eight GABAA receptor subunits in panic disorder. Am J Psychiatry 154:1096–1100
Dawson E, Parfitt E, Roberts Q et al (1995) Linkage studies of bipolar disorder in the region of the Darier’s disease gene on chromosome 12q23–24.1. Am J Med Genet 60:94–102
de Graaf R, Bijl RV, Smit F et al (2002) Risk factors for 12-month comorbidity of mood, anxiety, and substance use disorders: findings from the Netherlands mental health survey and incidence study. Am J Psychiatry 159:620–629
Deckert J, Catalano M, Heils A et al (1997) Functional promoter polymorphism of the human serotonin transporter: lack of association with panic disorder. Psychiatr Genet 7:45–47
Deckert J, Catalano M, Syagailo YV (1999) Excess of high activity monoamine oxidase A gene promoter alleles in female patients with panic disorder. Hum Mol Genet 8:621–624
Deckert J, Nothen MM, Franke P (1998) Systematic mutation screening and association study of the A1 and A2a adenosine receptor genes in panic disorder suggest a contribution of the A2a gene to the development of disease. Mol Psychiatry 3:81–85
Dickson SP, Wang K, Krantz I (2010) Rare variants create synthetic genome-wide associations. PLoS Biol 8:e1000294
Djurovic S, Gustafsson O, Mattingsdal M (2010) A genome-wide association study of bipolar disorder in Norwegian individuals, followed by replication in Icelandic sample. J Affect Disord 126:312–316
Domschke K, Braun M, Ohrmann P et al (2006) Association of the functional -1019C/G 5-HT1A polymorphism with prefrontal and amygdala activation measured with 3T fMRI in panic disorder. Int J Neuropsychopharmacol 9:349–355
Domschke K, Dannlowski U (2010) Imaging genetics of anxiety disorders. Neuroimage 53(3):822–831
Domschke K, Zwanzger P (2008) GABAergic and endocannabinoid dysfunction in anxiety—future therapeutic targets? Curr Pharm Des 14:3508–3517
Domschke K, Dannlowski U, Hohoff C (2010) Neuropeptide Y (NPY) gene: impact on emotional processing and treatment response in anxious depression. Eur Neuropsychopharmacol 20:301–309
Domschke K, Dannlowski U, Ohrmann P (2008a) Cannabinoid receptor 1 (CNR1) gene: impact on antidepressant treatment response and emotion processing in major depression. Eur Neuropsychopharmacol 18:751–759
Domschke K, Deckert J, O’Donovan MC (2007) Meta-analysis of COMT val158met in panic disorder: ethnic heterogeneity and gender specificity. Am J Med Genet B Neuropsychiatr Genet 144:667–673
Domschke K, Freitag CM, Kuhlenbäumer G (2004) Association of the functional V158M catechol-O-methyl-transferase polymorphism with panic disorder in women. Int J Neuropsychopharmacol 7:183–188
Domschke K, Hohoff C, Jacob C (2008b) Chromosome 4q31–34 panic disorder risk locus: Association of neuropeptide Y Y5 receptor variants. Am J Med Genet B Neuropsychiatr Genet 147B:510–516
Domschke K, Hohoff C, Mortensen LS (2008c) Monoamine oxidase A variant influences antidepressant treatment response in female patients with major depression. Prog Neuropsychopharmacol Biol Psychiatry 32:224–228
Domschke K, Kuhlenbaumer G, Schirmacher A (2003) Human nuclear transcription factor gene CREM: genomic organization, mutation screening, and association analysis in panic disorder. Am J Med Genet B Neuropsychiatr Genet 117:70–78
Domschke K, Ohrmann P, Braun M et al (2008d) Influence of the catechol-O-methyltransferase val158met genotype on amygdala and prefrontal cortex emotional processing in panic disorder. Psychiatry Res 163:13–20
Domschke K, Reif A, Weber H, Richter J, Hohoff C, Ohrmann P, Pedersen A, Bauer J, Suslow T, Kugel H, Heindel W, Baumann C, Klauke B, Jacob C, Maier W, Fritze J, Bandelow B, Krakowitzky P, Rothermundt M, Erhardt A, Binder EB, Holsboer F, Gerlach AL, Kircher T, Lang T, Alpers GW, Ströhle A, Fehm L, Gloster AT, Wittchen HU, Arolt V, Pauli P, Hamm A, Deckert J (2011) Neuropeptide S receptor gene—converging evidence for a role in panic disorder. Mol Psychiatry 16(9):938–948
Domschke K, Stevens S, Beck B (2009) Blushing propensity in social anxiety disorder: influence of serotonin transporter gene variation. J Neural Transm 116:663–666
Duman RS, Monteggia LM (2006) A neurotrophic model for stress-related mood disorders. Biol Psychiatry 59:1116–1127
Egeland JA, Gerhard DS, Pauls DL (1987) Bipolar affective disorders linked to DNA markers on chromosome 11. Nature 325:783–787
Erhardt A, Czibere L, Roeske D, Lucae S, Unschuld PG, Ripke S, Specht M, Kohli MA, Kloiber S, Ising M, Heck A, Pfister H, Zimmermann P, Lieb R, Pütz B, Uhr M, Weber P, Deussing JM, Gonik M, Bunck M, Kebler MS, Frank E, Hohoff C, Domschke K, Krakowitzky P, Maier W, Bandelow B, Jacob C, Deckert J, Schreiber S, Strohmaier J, Nöthen M, Cichon S, Rietschel M, Bettecken T, Keck ME, Landgraf R, Müller-Myhsok B, Holsboer F, Binder EB (2011) TMEM132D, a new candidate for anxiety phenotypes: evidence from human and mouse studies. Mol Psychiatry 16(6):647–663
Erhardt A, Lucae S, Kern N et al (2008) Association of polymorphisms in the angiotensin-converting enzyme gene with syndromal panic attacks. Mol Psychiatry 13:242–243
Erk S, Meyer-Lindenberg A, Schnell K et al (2010) Brain function in carriers of a genome-wide supported bipolar disorder variant. Arch Gen Psychiatry 67:803–811
Ewald H, Degn B, Mors O et al (1998) Significant linkage between bipolar affective disorder and chromosome 12q24. Psychiatr Genet 8:131–140
Ewald H, Flint T, Kruse TA et al (2002) A genome-wide scan shows significant linkage between bipolar disorder and chromosome 12q24.3 and suggestive linkage to chromosomes 1p22–21, 4p16, 6q14–22, 10q26 and 16p13.3. Mol Psychiatry 7:734–744
Fan J, Sklar P (2008) Genetics of bipolar disorder: focus on BDNF Val66Met polymorphism. Novartis Found Symp 289:60-72; discussion 72-63, 87-93
Fan M, Liu B, Jiang T et al (2010) Meta-analysis of the association between the monoamine oxidase-A gene and mood disorders. Psychiatr Genet 20:1–7
Fava M, Davidson KG (1996) Definition and epidemiology of treatment-resistant depression. Psychiatr Clin North Am 19:179–200
Fava M, Rush AJ, Alpert JE (2008) Difference in treatment outcome in outpatients with anxious versus nonanxious depression: a STAR*D report. Am J Psychiatry 165:342–351
Ferreira MA, O’Donovan MC, Meng YA et al (2008) Collaborative genome-wide association analysis supports a role for ANK3 and CACNA1C in bipolar disorder. Nat Genet 40:1056–1058
Fiedorowicz JG, Endicott J, Leon AC (2011) Subthreshold hypomanic symptoms in progression from unipolar major depression to bipolar disorder. Am J Psychiatry 168:40–48
Franchini L, Serretti A, Gasperini M et al (1998) Familial concordance of fluvoxamine response as a tool for differentiating mood disorder pedigrees. J Psychiatr Res 32:255–259
Franke B, Vasquez AA, Veltman JA, Brunner HG, Rijpkema M, Fernández G (2010) Genetic variation in CACNA1C, a gene associated with bipolar disorder, influences brainstem rather than gray matter volume in healthy individuals. Biol Psychiatry 68(6):586–588
Freitag CM, Domschke K, Rothe C et al (2006) Interaction of serotonergic and noradrenergic gene variants in panic disorder. Psychiatr Genet 16:59–65
Furlong RA, Ho L, Walsh C et al (1998) Analysis and meta-analysis of two serotonin transporter gene polymorphisms in bipolar and unipolar affective disorders. Am J Med Genet 81:58–63
Furmark T, Appel L, Henningsson S et al (2008) A link between serotonin-related gene polymorphisms, amygdala activity, and placebo-induced relief from social anxiety. J Neurosci 28:13066–13074
Furmark T, Henningsson S, Appel L (2009) Genotype over-diagnosis in amygdala responsiveness: affective processing in social anxiety disorder. J Psychiatry Neurosci 34:30–40
Furmark T, Tillfors M, Garpenstrand H et al (2004) Serotonin transporter polymorphism related to amygdala excitability and symptom severity in patients with social phobia. Neurosci Lett 362:189–192
Fyer AJ, Hamilton SP, Durner M (2006) A third-pass genome scan in panic disorder: evidence for multiple susceptibility loci. Biol Psychiatry 60:388–401
Garriock HA, Hamilton SP (2009a) Genetic studies of drug response and side effects in the STAR*D study, part 1. J Clin Psychiatry 70:1186–1187
Garriock HA, Hamilton SP (2009b) Genetic studies of drug response and side effects in the STAR*D study, part 2. J Clin Psychiatry 70:1323–1325
Gaysina D, Cohen S, Craddock N et al (2008) No association with the 5, 10-methylenetetrahydrofolate reductase gene and major depressive disorder: results of the depression case control (DeCC) study and a meta-analysis. Am J Med Genet B Neuropsychiatr Genet 147B:699–706
Gelernter J, Bonvicini K, Page G et al (2001) Linkage genome scan for loci predisposing to panic disorder or agoraphobia. Am J Med Genet 105:548–557
Gelernter J, Page GP, Bonvicini K et al (2003) A chromosome 14 risk locus for simple phobia: results from a genomewide linkage scan. Mol Psychiatry 8:71–82
Gelernter J, Page GP, Stein MB et al (2004) Genome-wide linkage scan for loci predisposing to social phobia: evidence for a chromosome 16 risk locus. Am J Psychiatry 161:59–66
Gershon ES, Alliey-Rodriguez N, Liu C (2011) After GWAS: searching for genetic risk for schizophrenia and bipolar disorder. Am J Psychiatry 168:253–256
Gilbody S, Lewis S, Lightfoot T (2007) Methylenetetrahydrofolate reductase (MTHFR) genetic polymorphisms and psychiatric disorders: a HuGE review. Am J Epidemiol 165:1–13
Goldstein RB, Wickramaratne PJ, Horwath E (1997) Familial aggregation and phenomenology of ‘early’-onset (at or before age 20 years) panic disorder. Arch Gen Psychiatry 54:271–278
Green E, Elvidge G, Jacobsen N et al (2005) Localization of bipolar susceptibility locus by molecular genetic analysis of the chromosome 12q23–q24 region in two pedigrees with bipolar disorder and Darier’s disease. Am J Psychiatry 162:35–42
Green EK, Grozeva D, Jones I et al (2009) The bipolar disorder risk allele at CACNA1C also confers risk of recurrent major depression and of schizophrenia. Mol Psychiatry 15:1016–1022
Grigoroiu-Serbanescu M, Diaconu CC, Herms S et al (2008) Investigation of the tryptophan hydroxylase 2 gene in bipolar I disorder in the Romanian population. Psychiatr Genet 18:240–247
Grozeva D, Kirov G, Ivanov D et al (2010) Rare copy number variants: a point of rarity in genetic risk for bipolar disorder and schizophrenia. Arch Gen Psychiatry 67:318–327
Gunthert KC, Conner TS, Armeli S et al (2007) Serotonin transporter gene polymorphism (5-HTTLPR) and anxiety reactivity in daily life: a daily process approach to gene-environment interaction. Psychosom Med 69:762–768
Halmoy A, Johansson S, Winge I et al (2010) Attention-deficit/hyperactivity disorder symptoms in offspring of mothers with impaired serotonin production. Arch Gen Psychiatry 67:1033–1043
Hamilton SP, Fyer AJ, Durner M et al (2003) Further genetic evidence for a panic disorder syndrome mapping to chromosome 13q. Proc Natl Acad Sci USA 100:2550–2555
Hamilton SP, Heiman GA, Haghighi F et al (1999) Lack of genetic linkage or association between a functional serotonin transporter polymorphism and panic disorder. Psychiatr Genet 9:1–6
Hamilton SP, Slager SL, de Baisre LA et al (2004a) Evidence for genetic linkage between a polymorphism in the adenosine 2A receptor and panic disorder. Neuropsychopharmacology 29:558–565
Hamilton SP, Slager SL, Heiman GA et al (2002) Evidence for a susceptibility locus for panic disorder near the catechol-O-methyltransferase gene on chromosome 22. Biol Psychiatry 51:591–601
Hamilton SP, Slager SL, Mayo D (2004b) Investigation of polymorphisms in the CREM gene in panic disorder. Am J Med Genet B Neuropsychiatr Genet 126:111–115
Hasler G, Drevets WC, Manji HK et al (2004) Discovering endophenotypes for major depression. Neuropsychopharmacology 29:1765–1781
Hattori E, Ebihara M, Yamada K et al (2001) Identification of a compound short tandem repeat stretch in the 5′-upstream region of the cholecystokinin gene, and its association with panic disorder but not with schizophrenia. Mol Psychiatry 6:465–470
Hattori E, Toyota T, Ishitsuka Y et al (2009) Preliminary genome-wide association study of bipolar disorder in the Japanese population. Am J Med Genet B Neuropsychiatr Genet 150B:1110–1117
Hek K, Mulder CL, Luijendijk HJ et al (2010) The PCLO gene and depressive disorders: replication in a population-based study. Hum Mol Genet 19:731–734
Hettema JM (2008) What is the genetic relationship between anxiety and depression? Am J Med Genet C Semin Med Genet 148C:140–146
Hettema JM, An SS, Neale MC et al (2006) Association between glutamic acid decarboxylase genes and anxiety disorders, major depression, and neuroticism. Mol Psychiatry 11:752–762
Hettema JM, Neale MC, Kendler KS (2001) A review and meta-analysis of the genetic epidemiology of anxiety disorders. Am J Psychiatry 158:1568–1578
Ho HP, Westberg L, Annerbrink K (2004) Association between a functional polymorphism in the progesterone receptor gene and panic disorder in women. Psychoneuroendocrinology 2:1138–1141
Hodges LM, Weissman MM, Haghighi F (2009) Association and linkage analysis of candidate genes GRP, GRPR, CRHR1, and TACR1 in panic disorder. Am J Med Genet B Neuropsychiatr Genet 150:65–73
Hohoff C, Domschke K, Schwarte K et al (2009a) Sympathetic activity relates to adenosine A(2A) receptor gene variation in blood-injury phobia. J Neural Transm 116:659–662
Hohoff C, Mullings EL, Heatherley SV, Freitag CM, Neumann LC, Domschke K, Krakowitzky P, Rothermundt M, Keck ME, Erhardt A, Unschuld PG, Jacob C, Fritze J, Bandelow B, Maier W, Holsboer F, Rogers PJ, Deckert J (2010) Adenosine A(2A) receptor gene: evidence for association of risk variants with panic disorder and anxious personality. J Psychiatr Res 44(14):930–937
Hohoff C, Neumann A, Domschke K et al (2009b) Association analysis of Rgs7 variants with panic disorder. J Neural Transm 116:1523–1528
Horstmann S, Lucae S, Menke A et al (2010) Polymorphisms in GRIK4, HTR2A, and FKBP5 show interactive effects in predicting remission to antidepressant treatment. Neuropsychopharmacology 35:727–740
Horwath E, Adams P, Wickramaratne P et al (1997) Panic disorder with smothering symptoms: evidence for increased risk in first-degree relatives. Depress Anxiety 6:147–153
Horwath E, Wolk SI, Goldstein RB et al (1995) Is the comorbidity between social phobia and panic disorder due to familial cotransmission or other factors? Arch Gen Psychiatry 52:574–582
Hösing VG, Schirmacher A, Kuhlenbäumer G, Freitag C, Sand P, Schlesiger C, Jacob C, Fritze J, Franke P, Rietschel M, Garritsen H, Nöthen MM, Fimmers R, Stögbauer F, Deckert J (2004) Cholecystokinin- and cholecystokinin-B-receptor gene polymorphisms in panic disorder. J Neural Transm Suppl 68:147–156
Huang J, Perlis RH, Lee PH, Rush AJ, Fava M, Sachs GS, Lieberman J, Hamilton SP, Sullivan P, Sklar P, Purcell S, Smoller JW (2010) Cross-disorder genomewide analysis of schizophrenia, bipolar disorder, and depression. Am J Psychiatry 167(10):1254–1263
Huang YY, Battistuzzi C, Oquendo MA et al (2004) Human 5-HT1A receptor C(-1019)G polymorphism and psychopathology. Int J Neuropsychopharmacol 7:441–451
Inada Y, Yoneda H, Koh J et al (2003) Positive association between panic disorder and polymorphism of the serotonin 2A receptor gene. Psychiatry Res 118:25–31
Ising M, Lucae S, Binder EB et al (2009) A genomewide association study points to multiple loci that predict antidepressant drug treatment outcome in depression. Arch Gen Psychiatry 66:966–975
Joffe RT, Bagby RM, Levitt A (1993) Anxious and nonanxious depression. Am J Psychiatry 150:1257–1258
Jones I, Jacobsen N, Green EK et al (2002) Evidence for familial cosegregation of major affective disorder and genetic markers flanking the gene for Darier’s disease. Mol Psychiatry 7:424–427
Kaabi B, Gelernter J, Woods SW et al (2006) Genome scan for loci predisposing to anxiety disorders using a novel multivariate approach: strong evidence for a chromosome 4 risk locus. Am J Hum Genet 78:543–553
Kanazawa T, Glatt SJ, Kia-Keating B et al (2007) Meta-analysis reveals no association of the Val66Met polymorphism of brain-derived neurotrophic factor with either schizophrenia or bipolar disorder. Psychiatr Genet 17:165–170
Kang EH, Song YJ, Kim KJ et al (2010) Sympathetic nervous function and the effect of the catechol-O-methyltransferase Val(158)Met polymorphism in patients with panic disorder. J Affect Disord 123:337–340
Karg K, Burmeister M, Shedden K et al (2011) The serotonin transporter promoter variant (5-HTTLPR), stress, and depression meta-analysis revisited: evidence of genetic moderation. Arch Gen Psychiatry 68:444–454
Keers R, Farmer AE, Aitchison KJ (2009) Extracting a needle from a haystack: reanalysis of whole genome data reveals a readily translatable finding. Psychol Med 39:1231–1235
Kato M, Serretti A (2010) Review and meta-analysis of antidepressant pharmacogenetic findings in major depressive disorder. Mol Psychiatry 15:473–500
Keck ME, Kern N, Erhardt A et al (2008) Combined effects of exonic polymorphisms in CRHR1 and AVPR1B genes in a case/control study for panic disorder. Am J Med Genet B Neuropsychiatr Genet 147B:1196–1204
Kempton MJ, Ruberto G, Vassos E et al (2009) Effects of the CACNA1C risk allele for bipolar disorder on cerebral gray matter volume in healthy individuals. Am J Psychiatry 166:1413–1414
Kendler KS (1996) Major depression and generalised anxiety disorder. Same genes, (partly) different environments—revisited. Br J Psychiatry 30:68–75
Kendler KS, Gardner CO, Gatz M et al (2007) The sources of co-morbidity between major depression and generalized anxiety disorder in a Swedish national twin sample. Psychol Med 37:453–462
Kendler KS, Karkowski LM, Prescott CA (1999) Fears and phobias: reliability and heritability. Psychol Med 29:539–553
Kendler KS, Neale MC, Kessler RC et al (1992) Major depression and generalized anxiety disorder. Same genes, (partly) different environments? Arch Gen Psychiatry 49:716–722
Kendler KS, Walters EE, Neale MC et al (1995) The structure of the genetic and environmental risk factors for six major psychiatric disorders in women. Arch Gen Psychiatry 52:374–383
Kennedy JL, Bradwejn J, Koszycki D et al (1999) Investigation of cholecystokinin system genes in panic disorder. Mol Psychiatry 4:284–285
Kessler RC, Nelson CB, McGonagle KA (1996) Comorbidity of DSM-III-R major depressive disorder in the general population: results from the US National Comorbidity Survey. Br J Psychiatry Suppl 30:17–30
Kim YK, Lee HJ, Yang JC et al (2009) A tryptophan hydroxylase 2 gene polymorphism is associated with panic disorder. Behav Genet 39:170–175
Kirchheiner J, Nickchen K, Bauer M et al (2004) Pharmacogenetics of antidepressants and antipsychotics: the contribution of allelic variations to the phenotype of drug response. Mol Psychiatry 9:442–473
Kishi T, Okochi T, Tsunoka T et al (2011) Serotonin 1A receptor gene, schizophrenia and bipolar disorder: an association study and meta-analysis. Psychiatry Res 185:20–26
Klauke B, Deckert J, Reif A et al (2010) Life events in panic disorder—An update on “candidate stressors”. Depress Anxiety 27:716–730
Knowles JA, Fyer AJ, Vieland VJ et al (1998) Results of a genome-wide genetic screen for panic disorder. Am J Med Genet 81:139–147
Kobayashi Y, Akiyoshi J, Kanehisa M et al (2007) Lack of polymorphism in genes encoding mGluR 7, mGluR 8, GABA(A) receptor alfa-6 subunit and nociceptin/orphanin FQ receptor and panic disorder. Psychiatr Genet 17:9
Krug A, Nieratschker V, Markov V et al (2010) Effect of CACNA1C rs1006737 on neural correlates of verbal fluency in healthy individuals. Neuroimage 49:1831–1836
Laje G, Allen AS, Akula N et al (2009) Genome-wide association study of suicidal ideation emerging during citalopram treatment of depressed outpatients. Pharmacogenet Genomics 19:666–674
Lango Allen H, Estrada K, Lettre G et al (2010) Hundreds of variants clustered in genomic loci and biological pathways affect human height. Nature 467:832–838
Lasky-Su JA, Faraone SV, Glatt SJ et al (2005) Meta-analysis of the association between two polymorphisms in the serotonin transporter gene and affective disorders. Am J Med Genet B Neuropsychiatr Genet 133B:110–115
Laucht M, Treutlein J, Blomeyer D et al (2009) Interaction between the 5-HTTLPR serotonin transporter polymorphism and environmental adversity for mood and anxiety psychopathology: evidence from a high-risk community sample of young adults. Int J Neuropsychopharmacol 12:737–747
Lavebratt C, Aberg E, Sjoholm LK et al (2010) Variations in FKBP5 and BDNF genes are suggestively associated with depression in a Swedish population-based cohort. J Affect Disord 125:249–255
Leckman JF, Weissman MM, Merikangas KR et al (1983) Panic disorder and major depression. Increased risk of depression, alcoholism, panic, and phobic disorders in families of depressed probands with panic disorder. Arch Gen Psychiatry 40:1055–1060
Lee MT, Chen CH, Lee C et al (2010) Genome-wide association study of bipolar I disorder in the Han Chinese population. Mol Psychiatry 16:548–556
Lee YJ, Hohoff C, Domschke K et al (2005) Norepinephrine transporter (NET) promoter and 5′-UTR polymorphisms: association analysis in panic disorder. Neurosci Lett 377:40–43
Lekman M, Laje G, Charney D et al (2008) The FKBP5-gene in depression and treatment response–an association study in the sequenced treatment alternatives to relieve depression (STAR*D) cohort. Biol Psychiatry 63:1103–1110
Lesch K, Bengel D, Heils A et al (1996) Association of anxiety-related traits with a polymorphism in the serotonin transporter gene regulatory region. Science 274:1527–1531
Lesch KP, Timmesfeld N, Renner TJ et al (2008) Molecular genetics of adult ADHD: converging evidence from genome-wide association and extended pedigree linkage studies. J Neural Transm 115:1573–1585
Levine J, Cole DP, Chengappa KN et al (2001) Anxiety disorders and major depression, together or apart. Depress Anxiety 14:94–104
Lewis CM, Ng MY, Butler AW et al (2010) Genome-wide association study of major recurrent depression in the U.K. population. Am J Psychiatry 167:949–957
Leygraf A, Hohoff C, Freitag C et al (2006) Rgs 2 gene polymorphisms as modulators of anxiety in humans? J Neural Transm 113:1921–1925
Lichtenstein P, Yip BH, Bjork C et al (2009) Common genetic determinants of schizophrenia and bipolar disorder in Swedish families: a population-based study. Lancet 373:234–239
Liebowitz MR (1993) Depression with anxiety and a typical depression. J Clin Psychiatry 54:10–14
Liu Y, Blackwood DH, Caesar S et al (2011) Meta-analysis of genome-wide association data of bipolar disorder and major depressive disorder. Mol Psychiatry 16:2–4
Lochner C, Hemmings S, Seedat S et al (2007) Genetics and personality traits in patients with social anxiety disorder: a case-control study in South Africa. Eur Neuropsychopharmacol 17:321–327
Logue MW, Durner M, Heiman GA et al (2009) A linkage search for joint panic disorder/bipolar genes. Am J Med Genet B Neuropsychiatr Genet 150:1139–1146
Lohoff FW (2010) Overview of the genetics of major depressive disorder. Curr Psychiatry Rep 12:539–546
Lopez-Leon S, Janssens AC, Gonzalez-Zuloeta Ladd AM et al (2008) Meta-analyses of genetic studies on major depressive disorder. Mol Psychiatry 13:772–785
Lopez Leon S, Croes EA, Sayed-Tabatabaei FA et al (2005) The dopamine D4 receptor gene 48-base-pair-repeat polymorphism and mood disorders: a meta-analysis. Biol Psychiatry 57:999–1003
Luykx JJ, Boks MP, Terwindt AP et al (2010) The involvement of GSK3beta in bipolar disorder: integrating evidence from multiple types of genetic studies. Eur Neuropsychopharmacol 20:357–368
Lydiard RB (1991) Coexisting depression and anxiety: special diagnostic and treatment issues. J Clin Psychiatry 52:48–54
Lydiard RB, Brawman-Mintzer O (1998) Anxious depression. J Clin Psychiatry 59:10–17
MacGillivray S, Arroll B, Hatcher S et al (2003) Efficacy and tolerability of selective serotonin reuptake inhibitors compared with tricyclic antidepressants in depression treated in primary care: systematic review and meta-analysis. BMJ 326:1014
MacKinnon DF, Xu J, McMahon FJ et al (1998) Bipolar disorder and panic disorder in families: an analysis of chromosome 18 data. Am J Psychiatry 155:829–831
Maier W, Lichtermann D, Minges J et al (1992) Personality traits in subjects at risk for unipolar major depression: a family study perspective. J Affect Disord 24:153–163
Maier W, Lichtermann D, Minges J (1993) A controlled family study in panic disorder. J Psychiatr Res 27:79–87
Manchia M, Squassina A, Congiu D et al (2009) Interacting genes in lithium prophylaxis: preliminary results of an exploratory analysis on the role of DGKH and NR1D1 gene polymorphisms in 199 Sardinian bipolar patients. Neurosci Lett 467:67–71
Marks IM, Herst ER (1970) A survey of 1200 agoraphobics in Britain. Soc Psychiatry 5:16–24
Maron E, Lang A, Tasa G et al (2005a) Associations between serotonin-related gene polymorphisms and panic disorder. Int J Neuropsychopharmacol 8:261–266
Maron E, Nikopensius T, Koks S et al (2005b) Association study of 90 candidate gene polymorphisms in panic disorder. Psychiatr Genet 15:17–24
Maron E, Toru I, Must A et al (2007) Association study of tryptophan hydroxylase 2 gene polymorphisms in panic disorder. Neurosci Lett 411:180–184
Maziade M, Roy MA, Rouillard E et al (2001) A search for specific and common susceptibility loci for schizophrenia and bipolar disorder: a linkage study in 13 target chromosomes. Mol Psychiatry 6:684–693
McCarthy MI, Abecasis GR, Cardon LR et al (2008) Genome-wide association studies for complex traits: consensus, uncertainty and challenges. Nat Rev Genet 9:356–369
McCarthy MJ, Leckband SG, Kelsoe JR (2010) Pharmacogenetics of lithium response in bipolar disorder. Pharmacogenomics 11:1439–1465
McGrath M, Kawachi I, Ascherio A et al (2004) Association between catechol-O-methyltransferase and phobic anxiety. Am J Psychiatry 161:1703–1705
McGuffin P, Knight J, Breen G et al (2005) Whole genome linkage scan of recurrent depressive disorder from the depression network study. Hum Mol Genet 14:3337–3345
McMahon FJ, Akula N, Schulze TG et al (2010) Meta-analysis of genome-wide association data identifies a risk locus for major mood disorders on 3p21.1. Nat Genet 42:128–131
McQueen MB, Devlin B, Faraone SV et al (2005) Combined analysis from eleven linkage studies of bipolar disorder provides strong evidence of susceptibility loci on chromosomes 6q and 8q. Am J Hum Genet 77:582–595
Mendlewicz J, Rainer JD (1977) Adoption study supporting genetic transmission in manic–depressive illness. Nature 268:327–329
Middeldorp CM, Cath DC, Van Dyck R et al (2005) The co-morbidity of anxiety and depression in the perspective of genetic epidemiology. A review of twin and family studies. Psychol Med 35:611–624
Montag C, Buckholtz JW, Hartmann P et al (2008) COMT genetic variation affects fear processing: psychophysiological evidence. Behav Neurosci 122:901–909
Mosing MA, Gordon SD, Medland SE et al (2009) Genetic and environmental influences on the co-morbidity between depression, panic disorder, agoraphobia, and social phobia: a twin study. Depress Anxiety 26:1004–1011
Moskvina V, Craddock N, Holmans P et al (2009) Gene-wide analyses of genome-wide association data sets: evidence for multiple common risk alleles for schizophrenia and bipolar disorder and for overlap in genetic risk. Mol Psychiatry 14:252–260
Mössner R, Freitag CM, Gutknecht L et al (2006) The novel brain-specific tryptophan hydroxylase-2 gene in panic disorder. J Psychopharmacol 20:547–552
Moya PR, Murphy DL, McMahon FJ, Wendland JR (2010) Increased gene expression of diacylglycerol kinase η in bipolar disorder. Int J Neuropsychopharmacol 13(8):1127–1128
Muglia P, Tozzi F, Galwey NW et al (2010) Genome-wide association study of recurrent major depressive disorder in two European case-control cohorts. Mol Psychiatry 15:589–601
Muller DJ, Zai CC, Shinkai T et al (2011) Association between the DAOA/G72 gene and bipolar disorder and meta-analyses in bipolar disorder and schizophrenia. Bipolar Disord 13:198–207
Nakamura K, Yamada K, Iwayama Y et al (2006) Evidence that variation in the peripheral benzodiazepine receptor (PBR) gene influences susceptibility to panic disorder. Am J Med Genet B Neuropsychiatr Genet 141B:222–226
Nelson JC (2008) Anxious depression and response to treatment. Am J Psychiatry 165:297–299
Nelson JC, Delucchi K, Schneider LS (2009) Anxiety does not predict response to antidepressant treatment in late life depression: results of a meta-analysis. Int J Geriatr Psychiatry 24:539–544
Nyegaard M, Demontis D, Foldager L et al (2010) CACNA1C (rs1006737) is associated with schizophrenia. Mol Psychiatry 15:119–121
O’Donovan MC, Craddock N, Norton N et al (2008) Identification of loci associated with schizophrenia by genome-wide association and follow-up. Nat Genet 40:1053–1055
Ohara K, Nagai M, Suzuki Y et al (1998) Association between anxiety disorders and a functional polymorphism in the serotonin transporter gene. Psychiatry Res 81:277–279
Ollila HM, Soronen P, Silander K et al (2009) Findings from bipolar disorder genome-wide association studies replicate in a Finnish bipolar family-cohort. Mol Psychiatry 14:351–353
Olsson M, Annerbrink K, Westberg L et al (2004) Angiotensin-related genes in patients with panic disorder. Am J Med Genet B Neuropsychiatr Genet 127:81–84
O’Reilly RL, Bogue L, Singh SM (1994) Pharmacogenetic response to antidepressants in a multicase family with affective disorder. Biol Psychiatry 36:467–471
Otowa T, Tanii H, Sugaya N et al (2010) Replication of a genome-wide association study of panic disorder in a Japanese population. J Hum Genet 55:91–96
Otowa T, Yoshida E, Sugaya N et al (2009) Genome-wide association study of panic disorder in the Japanese population. J Hum Genet 54:122–126
Overall JE, Hollister LE, Johnson M et al (1966) Nosology of depression and differential response to drugs. JAMA 195:946–948
Overall JE, Zisook S (1980) Diagnosis and the phenomenology of depressive disorders. J Consult Clin Psychol 48:626–634
Papakostas GI, Stahl SM, Krishen A et al (2008) Efficacy of bupropion and the selective serotonin reuptake inhibitors in the treatment of major depressive disorder with high levels of anxiety (anxious depression): a pooled analysis of 10 studies. J Clin Psychiatry 69:1287–1292
Pare CM, Mack JW (1971) Differentiation of two genetically specific types of depression by the response to antidepressant drugs. J Med Genet 8:306–309
Peerbooms OL, van Os J, Drukker M, Kenis G, Hoogveld L, MTHFR in Psychiatry Group, de Hert M, Delespaul P, van Winkel R, Rutten BP (2011) Meta-analysis of MTHFR gene variants in schizophrenia, bipolar disorder and unipolar depressive disorder: evidence for a common genetic vulnerability? Brain Behav Immun 25(8):1530–1543
Perlis RH, Huang J, Purcell S et al (2010) Genome-wide association study of suicide attempts in mood disorder patients. Am J Psychiatry 167:1499–1507
Perlis RH, Smoller JW, Ferreira MA et al (2009) A genomewide association study of response to lithium for prevention of recurrence in bipolar disorder. Am J Psychiatry 166:718–725
Perna G, Favaron E, DiBella D et al (2005) Antipanic efficacy of paroxetine and polymorphism within the promoter of the serotonin transporter gene. Neuropsychopharmacol 30:2230–2235
Perroud N, Uher R, Ng MY, Guipponi M, Hauser J, Henigsberg N, Maier W, Mors O, Gennarelli M, Rietschel M, Souery D, Dernovsek MZ, Stamp AS, Lathrop M, Farmer A, Breen G, Aitchison KJ, Lewis CM, Craig IW, McGuffin P (2010) Genome-wide association study of increasing suicidal ideation during antidepressant treatment in the GENDEP project. Pharmacogenomics J (in press)
Pickard BS, Christoforou A, Thomson PA et al (2009) Interacting haplotypes at the NPAS3 locus alter risk of schizophrenia and bipolar disorder. Mol Psychiatry 14:874–884
Poulton R, Andrews G, Millichamp J (2008) Gene-environment interaction and the anxiety disorders. Eur Arch Psychiatry Clin Neurosci 258:65–68
Purcell SM, Wray NR, Stone JL et al (2009) Common polygenic variation contributes to risk of schizophrenia and bipolar disorder. Nature 460:748–752
Ressler KJ, Bradley B, Mercer KB et al (2010) Polymorphisms in CRHR1 and the serotonin transporter loci: gene x gene x environment interactions on depressive symptoms. Am J Med Genet B Neuropsychiatr Genet 153B:812–824
Rietschel M, Mattheisen M, Frank J et al (2010) Genome-wide association-, replication-, and neuroimaging study implicates HOMER1 in the etiology of major depression. Biol Psychiatry 68:578–585
Psychiatric GWAS Consortium (2009) A framework for interpreting genome-wide association studies of psychiatric disorders. Mol Psychiatry 14:10–17
Rosenbaum JF, Biederman J, Hirshfield DR et al (1991) Further evidence of an association between behavioral inhibition and anxiety disorders: results from a family study of children from a non-clinical sample. J Psychiatr Res 25:49–65
Rothe C, Gutknecht L, Freitag C et al (2004) Association of a functional 1019C>G 5-HT1A receptor gene polymorphism with panic disorder with agoraphobia. Int J Neuropsychopharmacol 7:189–192
Rowe DC, Stever C, Gard JM et al (1998) The relation of the dopamine transporter gene (DAT1) to symptoms of internalizing disorders in children. Behav Genet 28:215–225
Roy MA, Neale MC, Pedersen NL et al (1995) A twin study of generalized anxiety disorder and major depression. Psychol Med 25:1037–1049
Rudolph RL, Entsuah R, Chitra R (1998) A meta-analysis of the effects of venlafaxine on anxiety associated with depression. J Clin Psychopharmacol 18:136–144
Samochowiec J, Hajduk A, Samochowiec A et al (2004) Association studies of MAO-A, COMT, and 5-HTT genes polymorphisms in patients with anxiety disorders of the phobic spectrum. Psychiatry Res 128:21–26
Sand P, Lesch KP, Catalano M et al (2000) Polymorphic MAO-A and 5-HT-transporter genes: analysis of interactions in panic disorder. World J Biol Psychiatry 1:147–150
Sand PG, Mori T, Godau C et al (2002a) Norepinephrine transporter gene (NET) variants in patients with panic disorder. Neurosci Lett 333:41–44
Sand PG, Schlurmann K, Luckhaus C et al (2002b) Estrogen receptor 1 gene (ESR1) variants in panic disorder. Am J Med Genet 114:426–428
Schmidt NB, Storey J, Greenberg BD et al (2000) Evaluating gene x psychological risk factor effects in the pathogenesis of anxiety: a new model approach. J Abnorm Psychol 109:308–320
Scholz CJ, Jacob CP, Buttenschon HN et al (2010) Functional variants of TSPAN8 are associated with bipolar disorder and schizophrenia. Am J Med Genet B Neuropsychiatr Genet 153B(4):967–972
Schruers K, Esquivel G, van Duinen M, Wichers M, Kenis G, Colasanti A, Knuts I, Goossens L, Jacobs N, van Rozendaal J, Smeets H, van Os J, Griez E (2011) Genetic moderation of CO2-induced fear by 5-HTTLPR genotype. J Psychopharmacol 25(1):37–42
Schulze TG, Alda M, Adli M et al (2010) The International Consortium on Lithium Genetics (ConLiGen): an initiative by the NIMH and IGSLI to study the genetic basis of response to lithium treatment. Neuropsychobiology 62:72–78
Schulze TG, Detera-Wadleigh SD, Akula N et al (2009) Two variants in Ankyrin 3 (ANK3) are independent genetic risk factors for bipolar disorder. Mol Psychiatry 14:487–491
Schulze TG, McMahon FJ (2003) Genetic linkage and association studies in bipolar affective disorder: a time for optimism. Am J Med Genet C Semin Med Genet 123C:36–47
Scott LJ, Muglia P, Kong XQ et al (2009) Genome-wide association and meta-analysis of bipolar disorder in individuals of European ancestry. Proc Natl Acad Sci USA 106:7501–7506
Segman RH, Shalev AY (2003) Genetics of posttraumatic stress disorder. CNS Spectr 8:693–698
Segurado R, Detera-Wadleigh SD, Levinson DF et al (2003) Genome scan meta-analysis of schizophrenia and bipolar disorder, part III: Bipolar disorder. Am J Hum Genet 73:49–62
Serretti A, Artioli P, Quartesan R (2005) Pharmacogenetics in the treatment of depression: pharmacodynamic studies. Pharmacogenet Genom 15:61–67
Serretti A, Mandelli L (2008) The genetics of bipolar disorder: genome ‘hot regions’, genes, new potential candidates and future directions. Mol Psychiatry 13:742–771
Shi J, Badner JA, Gershon ES et al (2008) Allelic association of G72/G30 with schizophrenia and bipolar disorder: a comprehensive meta-analysis. Schizophr Res 98:89–97
Shi J, Potash JB, Knowles JA et al (2011) Genome-wide association study of recurrent early-onset major depressive disorder. Mol Psychiatry 16:193–201
Shih RA, Belmonte PL, Zandi PP (2004) A review of the evidence from family, twin and adoption studies for a genetic contribution to adult psychiatric disorders. Int Rev Psychiatry 16:260–283
Shimizu E, Hashimoto K, Kobayashi K et al (2004) Lack of association between angiotensin I-converting enzyme insertion/deletion gene functional polymorphism and panic disorder in humans. Neurosci Lett 363:81–83
Shyn SI, Shi J, Kraft JB et al (2011) Novel loci for major depression identified by genome-wide association study of sequenced treatment alternatives to relieve depression and meta-analysis of three studies. Mol Psychiatry 16:202–215
Silverstone PH, Ravindran A (1999) Once-daily venlafaxine extended release (XR) compared with fluoxetine in outpatients with depression and anxiety. Venlafaxine XR 360 Study Group. J Clin Psychiatry 60:22–28
Silverstone PH, von Studnitz E (2003) Defining anxious depression: going beyond comorbidity. Can J Psychiatry 48:675–680
Sklar P, Smoller JW, Fan J et al (2008) Whole-genome association study of bipolar disorder. Mol Psychiatry 13:558–569
Skre I, Onstad S, Torgersen S (1993) A twin study of DSM-III-R anxiety disorders. Acta Psychiatr Scand 88:85–92
Smith DJ, Evans R, Craddock N (2010) Predicting response to lithium in bipolar disorder: a critical review of pharmacogenetic studies. J Ment Health 19:142–156
Smith EN, Bloss CS, Badner JA et al (2009) Genome-wide association study of bipolar disorder in European American and African American individuals. Mol Psychiatry 14:755–763
Smoller JW, Finn CT (2003) Family, twin, and adoption studies of bipolar disorder. Am J Med Genet C Semin Med Genet 123C:48–58
Smoller JW, Gardner-Schuster E et al (2008a) Genetics of anxiety: would the genome recognize the DSM. Depress Anxiety 25:368–377
Smoller JW, Paulus MP, Fagerness JA et al (2008b) Influence of RGS2 on anxiety-related temperament, personality, and brain function. Arch Gen Psychiatry 65:298–308
Smoller JW, Rosenbaum JF, Biederman J et al (2003) Association of a genetic marker at the corticotropin releasing hormone locus with behavioral inhibition. Biol Psychiatry 54:1376–1381
Smoller JW, Yamaki LH, Fagerness JA et al (2005) The corticotropin releasing hormone gene and behavioral inhibition in children at risk for panic disorder. Biol Psychiatry 57:1485–1492
Soronen P, Ollila HM, Antila M et al (2010) Replication of GWAS of bipolar disorder: association of SNPs near CDH7 with bipolar disorder and visual processing. Mol Psychiatry 15:4–6
Speliotes EK, Willer CJ, Berndt SI et al (2010) Association analyses of 249, 796 individuals reveal 18 new loci associated with body mass index. Nat Genet 42:937–948
Squassina A, Manchia M, Congiu D et al (2009) The diacylglycerol kinase eta gene and bipolar disorder: a replication study in a Sardinian sample. Mol Psychiatry 14:350–351
Stein MB, Chartier MJ, Kozak MV et al (1998) Genetic linkage to the serotonin transporter protein and 5HT2A receptor genes excluded in generalized social phobia. Psychiatry Res 81:283–291
Stein MB, Jang KL, Livesley WJ (1999) Heritability of anxiety sensitivity. Am J Psychiatry 156:246–251
Stein MB, Schork NJ, Gelernter J (2008) Gene-by-environment (serotonin transporter and childhood maltreatment) interaction for anxiety sensitivity, an intermediate phenotype for anxiety disorders. Neuropsychopharmacology 33:312–319
Stein MB, Seedat S, Gelernter J (2006) Serotonin transporter gene promoter polymorphism predicts SSRI response in generalized social anxiety disorder. Psychopharmacology (Berl) 187:68–72
Steinberg S, Mors O, Borglum AD et al (2011) Expanding the range of ZNF804A variants conferring risk of psychosis. Mol Psychiatry 16:59–66
Strug LJ, Suresh R, Fyer AJ et al (2010) Panic disorder is associated with the serotonin transporter gene (SLC6A4) but not the promoter region (5-HTTLPR). Mol Psychiatry 15:166–176
Sullivan PF (2010) The psychiatric GWAS consortium: big science comes to psychiatry. Neuron 68:182–186
Sullivan PF, de Geus EJ, Willemsen G et al (2009) Genome-wide association for major depressive disorder: a possible role for the presynaptic protein piccolo. Mol Psychiatry 14:359–375
Sullivan PF, Neale MC, Kendler KS (2000) Genetic epidemiology of major depression: review and meta-analysis. Am J Psychiatry 157:1552–1562
Tadic A, Rujescu D, Szegedi A et al (2003) Association of a MAOA gene variant with generalized anxiety disorder, but not with panic disorder or major depression. Am J Med Genet B Neuropsychiatr Genet 117:1–6
Takata A, Kawasaki H, Iwayama Y et al (2011) Nominal association between a polymorphism in DGKH and bipolar disorder detected in a meta-analysis of East Asian case-control samples. Psychiatry Clin Neurosci 65:280–285
Terracciano A, Tanaka T, Sutin AR et al (2010) Genome-wide association scan of trait depression. Biol Psychiatry 68:811–817
Tesli M, Athanasiu L, Mattingsdal M et al (2010) Association analysis of PALB2 and BRCA2 in bipolar disorder and schizophrenia in a scandinavian case-control sample. Am J Med Genet B Neuropsychiatr Genet 153B:1276–1282
Tesli M, Kahler AK, Andreassen BK et al (2009) No association between DGKH and bipolar disorder in a Scandinavian case-control sample. Psychiatr Genet 19:269–272
Thoeringer CK, Binder EB, Salyakina D et al (2007) Association of a Met88Val diazepam binding inhibitor (DBI) gene polymorphism and anxiety disorders with panic attacks. J Psychiatr Res 41:579–584
Thoeringer CK, Ripke S, Unschuld PG et al (2009) The GABA transporter 1 (SLC6A1): a novel candidate gene for anxiety disorders. J Neural Transm 116:649–657
Thomas D (2010) Gene-environment-wide association studies: emerging approaches. Nat Rev Genet 11:259–272
Thorgeirsson TE, Oskarsson H, Desnica N et al (2003) Anxiety with panic disorder linked to chromosome 9q in Iceland. Am J Hum Genet 72:1221–1230
Tsuang M, Domschke K, Jerskey BA et al (2004) Agoraphobic behavior and panic attack: a study of male twins. J Anxiety Disord 18:799–807
Uher R, McGuffin P (2008) The moderation by the serotonin transporter gene of environmental adversity in the aetiology of mental illness: review and methodological analysis. Mol Psychiatry 13:131–146
Uher R, McGuffin P (2010) The moderation by the serotonin transporter gene of environmental adversity in the etiology of depression: 2009 update. Mol Psychiatry 15:18–22
Uher R, Perroud N, Ng MY et al (2010) Genome-wide pharmacogenetics of antidepressant response in the GENDEP project. Am J Psychiatry 16:555–564
Unschuld PG, Ising M, Erhardt A et al (2007) Polymorphisms in the serotonin receptor gene HTR2A are associated with quantitative traits in panic disorder. Am J Med Genet B Neuropsychiatr Genet 144:424–429
Unschuld PG, Ising M, Erhardt A et al (2008) Polymorphisms in the galanin gene are associated with symptom-severity in female patients suffering from panic disorder. J Affect Disord 105:177–184
Unschuld PG, Ising M, Roeske D et al (2010) Gender-specific association of galanin polymorphisms with HPA-axis dysregulation, symptom severity, and antidepressant treatment response. Neuropsychopharmacology 35:1583–1592
Unschuld PG, Ising M, Specht M et al (2009) Polymorphisms in the GAD2 gene-region are associated with susceptibility for unipolar depression and with a risk factor for anxiety disorders. Am J Med Genet B Neuropsychiatr Genet 150:1100–1109
Velders FP, Kuningas M, Kumari M, Dekker MJ, Uitterlinden AG, Kirschbaum C, Hek K, Hofman A, Verhulst FC, Kivimaki M, Van Duijn CM, Walker BR, Tiemeier H (2011) Genetics of cortisol secretion and depressive symptoms: a candidate gene and genome wide association approach. Psychoneuroendocrinology 36(7):1053–1061
Verhagen M, van der Meij A, van Deurzen PA et al (2010) Meta-analysis of the BDNF Val66Met polymorphism in major depressive disorder: effects of gender and ethnicity. Mol Psychiatry 15:260–271
Vieland VJ, Goodman DW, Chapman T et al (1996) New segregation analysis of panic disorder. Am J Med Genet 67:147–153
Wang KS, Liu XF, Aragam N (2010) A genome-wide meta-analysis identifies novel loci associated with schizophrenia and bipolar disorder. Schizophr Res 124:192–199
Wang Z, Valdes J, Noyes R et al (1998) Possible association of a cholecystokinin promotor polymorphism (CCK-36CT) with panic disorder. Am J Med Genet 81:228–234
Weber H, Kittel-Schneider S, Gessner A, Domschke K, Neuner M, Jacob CP, Buttenschon HN, Boreatti-Hümmer A, Volkert J, Herterich S, Baune BT, Gross-Lesch S, Kopf J, Kreiker S, Nguyen TT, Weissflog L, Arolt V, Mors O, Deckert J, Lesch KP, Reif A (2011) Cross-disorder analysis of bipolar risk genes: further evidence of DGKH as a risk gene for bipolar disorder, but also unipolar depression and adult ADHD. Neuropsychopharmacology 36(10):2076–2085
Weissman MM, Fyer AJ, Haghighi F et al (2000) Potential panic disorder syndrome: clinical and genetic linkage evidence. Am J Med Genet 96:24–35
Wender PH, Kety SS, Rosenthal D et al (1986) Psychiatric disorders in the biological and adoptive families of adopted individuals with affective disorders. Arch Gen Psychiatry 43:923–929
Wessa M, Linke J, Witt SH, Nieratschker V, Esslinger C, Kirsch P, Grimm O, Hennerici MG, Gass A, King AV, Rietschel M (2010) The CACNA1C risk variant for bipolar disorder influences limbic activity. Mol Psychiatry 15(12):1126–1127
Williams HJ, Craddock N, Russo G et al (2011) Most genome-wide significant susceptibility loci for schizophrenia and bipolar disorder reported to date cross-traditional diagnostic boundaries. Hum Mol Genet 20:387–391
Woo JM, Yoon KS, Choi YH et al (2004) The association between panic disorder and the L/L genotype of catechol-O-methyltransferase. J Psychiatr Res 38:365–370
Woo JM, Yoon KS, Yu BH (2002) Catechol O-methyltransferase genetic polymorphism in panic disorder. Am J Psychiatry 159:1785–1787
Wray NR, Pergadia ML, Blackwood DH, Penninx BW, Gordon SD, Nyholt DR, Ripke S, Macintyre DJ, McGhee KA, Maclean AW, Smit JH, Hottenga JJ, Willemsen G, Middeldorp CM, de Geus EJ, Lewis CM, McGuffin P, Hickie IB, van den Oord EJ, Liu JZ, Macgregor S, McEvoy BP, Byrne EM, Medland SE, Statham DJ, Henders AK, Heath AC, Montgomery GW, Martin NG, Boomsma DI, Madden PA, Sullivan PF (2012) Genome-wide association study of major depressive disorder: new results, meta-analysis, and lessons learned. Mol Psychiatry 17(1):36–48
WTCCC (2007) Genome-wide association study of 14,000 cases of seven common diseases and 3,000 shared controls. Nature 447:661–678
Xie P, Kranzler HR, Poling J et al (2010) Interaction of FKBP5 with childhood adversity on risk for post-traumatic stress disorder. Neuropsychopharmacology 35:1684–1692
Yasuda S, Kai M, Imai S et al (2009) Diacylglycerol kinase eta augments C-Raf activity and B-Raf/C-Raf heterodimerization. J Biol Chem 284:29559–29570
Yevtushenko OO, Oros MM, Reynolds GP (2010) Early response to selective serotonin reuptake inhibitors in panic disorder is associated with a functional 5-HT1A receptor gene polymorphism. J Affect Disord 123:308–311
Yoon HK, Yang JC, Lee HJ et al (2008) The association between serotonin-related gene polymorphisms and panic disorder. J Anxiety Disord 22:1529–1534
Zeng Z, Wang T, Li T et al (2011) Common SNPs and haplotypes in DGKH are associated with bipolar disorder and schizophrenia in the Chinese Han population. Mol Psychiatry 16:473–475
Zhang D, Cheng L, Qian Y et al (2009a) Singleton deletions throughout the genome increase risk of bipolar disorder. Mol Psychiatry 14:376–380
Zhang Z, Lindpaintner K, Che R et al (2009b) The Val/Met functional polymorphism in COMT confers susceptibility to bipolar disorder: evidence from an association study and a meta-analysis. J Neural Transm 116:1193–1200
Zhou K, Dempfle A, Arcos-Burgos M et al (2008) Meta-analysis of genome-wide linkage scans of attention deficit hyperactivity disorder. Am J Med Genet B Neuropsychiatr Genet 147B:1392–1398
Zimmerman M, Chelminski I, McDermut W (2002) Major depressive disorder and axis I diagnostic comorbidity. J Clin Psychiatry 63:187–193
Zintzaras E (2006) C677T and A1298C methylenetetrahydrofolate reductase gene polymorphisms in schizophrenia, bipolar disorder and depression: a meta-analysis of genetic association studies. Psychiatr Genet 16:105–115
Zintzaras E, Sakelaridis N (2007) Is 472G/A catechol-O-methyl-transferase gene polymorphism related to panic disorder? Psychiatr Genet 17:267–273
Zobel A, Schuhmacher A, Jessen F et al (2010) DNA sequence variants of the FKBP5 gene are associated with unipolar depression. Int J Neuropsychopharmacol 13:649–660
Zou YF, Wang F, Feng XL, Li WF, Tian YH, Tao JH, Pan FM, Huang F (2010) Association of DRD2 gene polymorphisms with mood disorders: a meta-analysis. J Affect Disord (in press)
Acknowledgments
This paper was supported by the DFG (Grant RE1632/1-1,/1-3 and/5 to AR, KFO 125 TP4 to AR, DE357/4-1 to AR, SFB TRR 58 C2 and Z2 to AR and KD, respectively; RTG 1252, to AR) and the BMBF (Panik-Net Subproject 6, to AR). We thank A. Alttoa for valuable discussions and her kind help in the preparation of the manuscript.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2011 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Domschke, K., Reif, A. (2011). Behavioral Genetics of Affective and Anxiety Disorders. In: Cryan, J., Reif, A. (eds) Behavioral Neurogenetics. Current Topics in Behavioral Neurosciences, vol 12. Springer, Berlin, Heidelberg. https://doi.org/10.1007/7854_2011_185
Download citation
DOI: https://doi.org/10.1007/7854_2011_185
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-27858-7
Online ISBN: 978-3-642-27859-4
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)