Abstract
Campylobacter acts using complex strategies to establish and promote intestinal infections. After ingestion via contaminated foods, this bacterium invades and can survive within the intestinal cells, also inducing epithelial translocation of non-invasive intestinal bacteria. In this investigation, the ability of human and avian C. jejuni and C. coli isolates to survive within two different intestinal epithelial cells lines, Caco-2 and INT 407, as well as the intestinal translocation phenomenon, was assessed. Our data demonstrated that both C. jejuni and C. coli strains survived in Caco-2 (81.8% and 100% respectively) and INT 407 monolayers (72.7% and 100% respectively) within the first 24 h post-infection period, with a progressive reduction in the prolonged period of 48 h and 72 h post-infection. The translocation of the non-invasive E. coli 60/06 FB was remarkably increased in C. jejuni treated Caco-2 monolayers (2.36 ± 0.42 log cfu/mL) (P < 0.01) and less in those treated with C. coli (1.2 ± 0.34 log cfu/mL), compared to E. coli 60/06 FB alone (0.37 ± 0.14 log cfu/mL). Our results evidenced the ability of both human and avian strains of C. jejuni and C. coli to efficiently survive within intestinal cells and induce the translocation of a non-invasive pathogen. Overall, these findings stress how this pathogen can interact with host cells and support the hypothesis that defects in the intestinal barrier function induced by Campylobacter spp. could have potentially negative implications for human health.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Campylobacter is considered the most common and important cause of bacterial gastroenteritis in humans in the developed world (Kaakoush et al. 2015; Cody et al. 2019). In the European Union (EU) the number of confirmed cases has continued to escalate over the years (214,000 in 2013 to 246,000 in 2016 and 2017) (European Food Safety Authority 2018), and in the United States, more than 800,000 cases are annually estimated (Scallan et al. 2011). Poultry is considered to be one of the most important reservoirs of human infections (Wilson et al. 2008; Friesema et al. 2012) and consumption, as well as handling of poultry meat, have been identified as important risk factors (Humphrey et al. 2007; Krutkiewicz and Klimuszko 2010; Wysok and Wojtacka 2018).
The molecular genetics of Campylobacter pathogenesis has been extensively studied (Krutkiewicz and Klimuszko 2010) and it is well acknowledged that important virulence factors are involved in the pathogenesis of Campylobacter infections, such as the flagella-mediated motility, adherence to intestinal epithelial cells, invasion and survival in the host cells, as well as the ability to produce toxins (Bang et al. 2003; Fouts et al. 2005). During the infection process, Campylobacter spp. can pass through the mucous layer of the epithelial cells, attach and then penetrate them (Bolton 2015; Igwaran and Okoh 2019). This interaction is possible to the motility of the bacteria, reached by flagellin, a protein of flagella encoded by flaA and flaB genes (Lertsethtakarn et al. 2011). Among these, flaA is the gene expressed at a higher level, thus considered crucial for bacterial motility. The other genes, cadF and racR, control Campylobacter spp. colonization (de Oliveira et al. 2019), while invasion ability is supported by the products of virB11 and pldA genes (Talukder et al. 2008; Wysok and Wojtacka 2018). Other important virulence genes and proteins synthesized by Campylobacter species including the invasion antigen C protein, involved in the full invasion of INT 407 cells, and the invasion associated protein gene (iamA) (Bolton 2015). Once inside the host cell, Campylobacter is able to survive intracellularly for a relatively long period of time, both in phagocytes and intestinal epithelial cells (Naikare et al. 2006; Šikić Pogačar et al. 2009; Buelow et al. 2011). Indeed, it is assumed that the invasion factors activate host cell plasma membrane invaginations (Cróinín and Backert 2012), forming an endosomal compartment that is transported from the apical to the basolateral surface, enabling Campylobacter translocation across the intestinal epithelial barrier (Konkel et al. 1992; Hu et al. 2008; Louwen et al. 2012; Backert and Hofreuter 2013). The Campylobacter translocation phenomenon may also translocate across the intestinal epithelium other commensal pathogens (Kalischuk et al. 2009), leading to important implications in human mucosal inflammatory responses towards intestinal bacteria.
In this research, the intracellular survival ability of different human and avian C. jejuni and C. coli strains, as well as the Campylobacter induced translocation phenomenon of a non-invasive pathogen was investigated.
2 Materials and Methods
2.1 Bacterial Strains and Growth Conditions
A total of 20 Campylobacter spp. belonging to our laboratory collection of strains isolated in Central Italy from human and animal were considered in this study. Samples included 11 C. jejuni strains, isolated from patients with gastroenteritis (n = 6) and from avian collected from slaughterhouse environment (n = 5), and 9 C. coli from human patients with gastrointestinal diseases (n = 5) and from avian collected from slaughterhouse environment (n = 4). All isolates were previously characterized for adhesion and invasion properties, as well as for the presence of several virulence genes (cad F, flaA, dnaJ, ciaB, pldA, cdtA, cdtB and cdtC) (unpublished data). The strains were grown on Columbia agar base (VWR, Milan, Italy) plates supplemented with 5% of Laked Horse Blood (Oxoid, Milan, Italy) and Preston Campylobacter Selective Supplement (VWR) h at 37 °C for 48 h under microaerophilic conditions (5% O2; 10% CO2; 85% N2).
2.2 Epithelial Cells
Caco-2 (human colon adenocarcinoma) cells were propagated as monolayers in Dulbecco’s Modified Eagle’s Medium (D-MEM) (Sigma, Milan, Italy) supplemented with 10% foetal bovine serum (FBS) (Sigma), 1% non-essential amino acids (Sigma) and 1% antibiotics solution (5000 U of streptomycin-penicillin; Sigma). Intestine 407 (INT 407) cells were cultured in Minimal Essential Media (MEM) (Sigma) supplemented with 10% foetal bovine serum (FBS) (Sigma) and 1 mM sodium pyruvate (Sigma). All the cells were maintained at 37 °C in a 5% CO2 humidified atmosphere. For internalization and survival assays, Caco-2 and INT 407 cells were seeded at 2 × 104 cells per well in 6-well plastic plates (VWR) and incubated for 7 days at 37 ° C in a 5% CO2 humidified atmosphere. Before the assays, the cell monolayers were washed twice with phosphate-buffered saline (PBS) pH 7.2.
2.3 Intracellular Survival of C. jejuni and C. coli Strains in Caco-2 and INT 407 Cells
C. jejuni and C. coli strains were cultured for 48 h in Mueller Hinton broth (VWR) with 5% of FCS at 37 °C in a shaking incubator under the above-mentioned microaerophilic conditions. Each bacterial suspension was centrifuged at 1.500 × g for 15 min, the pellet was resuspended in D-MEM containing 1% FBS and adjusted spectrophotometrically to approximately 1 × 108 cell/mL (OD660). One mL of this suspension was inoculated in 6-wells plates containing semi-confluent Caco-2 and INT 407 cells monolayers. Infected cells were then incubated at 37 °C for 3 h in an atmosphere of 5% CO2. After incubation, the infected Caco-2 and INT 407 cells were washed twice in PBS after 250 μg/mL gentamicin killing and further cultivated in D-MEM containing a sub-lethal dose of gentamicin (10 μg/mL) to suppress eventual growth of viable bacteria from cells. Quantification of intracellular bacteria after until 72 h was performed by twice washings in PBS and subsequent lysing with 1% Triton X-100. The number of surviving bacteria was determined by plating serial dilution of the lysates in sterile physiological solution on Columbia Agar base (VWR); the plates were incubated for 48 h at 37 °C under the described microaerophilic conditions for the quantification of the colonies forming units (cfu). Data were expressed as mean ± sd (cfu/mL) of three independent experiments performed in duplicate.
2.4 Selection of Non-invasive E. coli Strain
Four human strains of E. coli (E. coli 21/01, E. coli 126/18 FB, E. coli 85/27 AP, and E. coli 60/06 FB), kindly furnished by Gamma Laboratory (Fano, Pesaro, Italy), were used in this study. The identification, as well as the antibiotic susceptibility, was performed using VITEK 2 Compact (bioMérieux, Vercieux, France). All the strains were maintained in Tryptic Soya Agar (TSA) (VWR) at 37 °C, while stock cultures were kept at −80 °C in Nutrient Broth n°2 (Oxoid) with 15% glycerol.
To select one non-invasive E. coli, invasion assay on Caco-2 cell monolayers was carried out. Briefly, E. coli strains were grown in 20 mL of Tryptic Soya Broth (TSB) (VWR) at 37 °C for 18 h. At the end of the incubation period, the suspensions were centrifuged at 3500 rpm for 15 min and bacteria were harvested and re-suspended in 10 mL of DMEM at 1% FBS; for each strain, the optical density was spectrophotometrically adjusted to approximately 1 × 108 cell/mL (OD 610 nm) and 1 mL was added to 24 wells plate containing Caco-2 cells prepared as described above. After 6 h of incubation at 37 °C in an atmosphere of 5% CO2, infected cells were washed twice in PBS and incubated for another 2 h in DMEM containing 250 μg/mL of gentamicin to kill remaining viable extracellular bacteria. At this point, monolayers were lysed with 1% Triton X-100 (Sigma), serially diluted in physiological saline solution and plated onto TSA (VWR) for the enumeration of invasive E. coli (cfu/mL) as described above. Data are expressed as the mean values obtained in three independent experiments performed in duplicate (mean ± sd of cfu/mL). The invasion index, in percentage, was then calculated as a mean of cfu invasive bacteria/cfu inoculated bacteria. The E. coli strain with the lowest invasion index was identified as non-invasive and then used for the following experiments.
2.5 Caco-2 M-Like Cell Model
Caco-2 cells were grown in DMEM supplemented with 10% (v/v) fetal bovine serum, 200 mM L-glutamine, 100 U/mL penicillin, 100 μg/mL streptomycin, and incubated at 37 °C and 5% CO2. For E. coli translocation assay, cells were seeded onto Transwell filters (3 μm pore size, 1.13 cm2; Costar Corning Inc., Corning, NY) at 1.5 × 105 cells per filter and grown for 21 days, with a change of medium every 2 days.
2.6 E. coli Translocation Assays
Briefly, transwell-grown monolayers were washed with PBS and antibiotic-free DMEM was added to the apical and basal compartments. E. coli inoculum was added to the apical compartment of all monolayers to achieve a multiplicity of infection (MOI) of 100 cfu per enterocyte. Monolayers were then divided into two groups and half were inoculated with the selected strains of C. jejuni or C. coli at MOI of 100, whereas the other half received an equivalent volume of sterile broth (control treatment). Following incubation, E. coli recovered in the basal compartment (indicating translocation) were enumerated by spreading serial dilutions onto McConkey agar (VWR), incubating the cultures aerobically at 37 °C for 24 h, and enumerating at the dilution yielding 30–300 colony forming units (cfu) per culture. Preliminary experiments were performed to verify that 6 h was the optimal incubation time for E. coli internalization and/or translocation (data not shown).
2.7 Statistical Analysis
Statistical analysis was performed using Prism 5.0 (GraphPad Software, Inc., La Jolla, USA). All the data are expressed as the mean values obtained in three independent experiments performed in duplicate. The conditions necessary to perform the parametric tests (one-way Anova, Student t-test) were checked before conducting the analysis, otherwise, non-parametric tests (such as Kruskall-Wallis or Mann-Whitney U test) were utilized. The level of significance was always considered α = 0.05.
3 Results
3.1 Survival Ability of Campylobacter Spp.
A total of 20 Campylobacter spp. were examined for their ability to intracellularly survive in Caco-2 and INT 407 cells up to 72 h post-infection. As shown, most of the strains were able to survive within Caco-2 (90.0%) (Fig. 1a) and INT 407 (85.0%) (Fig. 1b) 24 h post-infection period. A progressive reduction in the survival ability of Campylobacter spp. was observed in the following 48 h post-infection period (55% and 40% within Caco-2 and INT 407 respectively). Finally, in the last 72 h post-infection period, only 15% of the strains survived within Caco-2 cells and 20.0% within INT 407 (Fig. 1a, b).
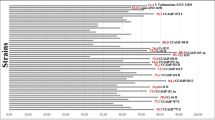
3.1.1 Campylobacter Spp. Survival Within Caco-2
The survival of C. jejuni and C. coli strains within cultured Caco-2 cells was analysed over a 72 h period of incubation (Fig. 2). Quite similar survival characteristics were observed for C. jejuni and C. coli human isolates, though with different cfu/mL values, with a progressive decrease in the number of intracellular bacteria after 24 and 72 h post-infection. In detail, in the case of CJHS05, 1.3 × 104 cfu/mL were recovered 24 h post-infection period higher than the values observed for the other strains (ranging from 6.67 × 101 to 9.33 × 103 cfu/mL); the only strain CJHS01 resulted unable to survive for 24 h within Caco-2 cell. In the following 48 h post-infection, the bacterial survival within Caco-2 cells was remarkably reduced, as showed by the low cfu/mL values recovered for only two C. jejuni strains (2 × 102 and 3.3 × 101 cfu/mL for CJHS241 and CJHS05 respectively); moreover, most of the strains did not survive 72 h post-infection (Fig. 2a). Considering C. coli human strains, the obtained cfu/mL values after 24 h of incubation were slightly higher compared to C. jejuni human isolates, reaching 2.37 × 105 cfu/mL in the case of CCHS010 and ranging from 1.33 × 102 to 2.33 × 104 cfu/mL for the other strains. After 48 h of incubation, CCHS010, CCHS015 and CCHS063 still survived within Caco-2 cells, showing 2 × 104, 2.33 × 103 and 1.33 × 103 cfu/mL respectively. Furthermore, in this case, no strain was able to survive up to 72 h (Fig. 2b).
As regards the survival of C. jejuni avian isolates within Caco-2 monolayers, 9 × 103 and 3.3 × 103 cfu/mL were recovered for CJAS07 and CJAS069 respectively 24 h post-infection, while for the other strains about 102 cfu/mL were determined; the only strain CJAS014 did not survive. After 48 h of incubation, most of the strains showed low survival ability (about 101 cfu/mL) with the only exception of CJAS069 and CJAS1085 that resulted still present within Caco-2 cells (4 × 102 and 3.2 × 102 cfu/mL respectively). No strain survived up to 72 h (Fig. 2c). In the case of C. coli avian strains, a higher survival ability compared to C. jejuni human isolates was evidenced after 24 h of incubation, with values ranging from 4.3 × 102 to 1.37 × 105 cfu/mL; in the prolonged 48 h post-infection period, only CCAS02 and CCAS091 still survived within Caco-2 cells, showing 5.3 × 103 and 3 × 104 cfu/mL respectively, while no strain was able to survive up to 72 h (Fig. 2d).
3.1.2 Campylobacter Spp. Survival Within INT 407
As regards the survival ability of C. jejuni and C. coli strains within INT 407 cells, data are presented in Fig. 3. Specifically, 24 h post-infection period, most of the human C. jejuni strains showed very low survival ability with values ranging from 6.7 × 101 to 3.0 × 102 cfu/mL and, in some cases, no survival was observed (CJHS01, CHJS088 and CJHS24). In the following 48 h post-infection, only the strain CJHS07 still survived with 2.3 × 102 cfu/mL and, as expected, no survival was evidenced 72 h post-infection period (Fig. 3a). Considering the human C. coli strains, after 24 h of incubation the survival ability resulted higher compared to C. jejuni human isolates, with values ranging from to 2 × 103 cfu/mL (CCHS015) to 6.3 × 104 cfu/mL (CCHS063). Most of the strains (CCHS010, CCHS015, CCHS063) were also able to survive 48 h post-infection (values ranging from 1.0 × 101 to 3.3 × 103 cfu/mL) but not up to the prolonged 72 h post-infection period (Fig. 3b).
In the case of the avian C. jejuni isolates, all the strains survived only after 24 h post-infection with values ranging from 3.3 × 101 to 1.6 × 102 cfu/mL, while no strains resulted able to survive up to 48 or 72 h post-infection (Fig. 3c). As already noted, all the C. coli avian strains showed higher ability to survive after 24 h post-infection in comparison to C. jejuni avian isolates, with values ranging from 7.0 × 102 cfu/mL (CCAS091) to 1.1 × 103 cfu/mL (CCAS02). In the following 48 h post-infection period, all the strains resulted still alive within INT 407 (from 3.93 × 101 cfu/mL to 4.33 × 102 cfu/mL), while in the prolonged 72 h post-infection period, only two strains (CCAS02 and CCAS091) still survived within INT 407 cells with low values (about 101 cfu/mL) (Fig. 3d).
3.2 Comparison of C. jejuni and C. coli Survival Ability
In Table 1 are summarized the different survival ability of C. jejuni and C. coli strains (human and avian source) in both the used cell lines. As shown, in the first 24 h post-infection period, most of C. jejuni strains (81.1%) were able to survive within Caco-2 cells regardless of the source (human and avian), as evident by the similar obtained percentages of survival (83.3 and 80% respectively), whilst in the case of C. coli 100% of the strains (both for human and avian) resulted surviving. In the second 48 h post-infection period, among the C. jejuni isolates, survived only 33.3% of the human strains in comparison to 80% of the avian ones. Similarly, 60% of human and 50% of avian C. coli strains were survived within Caco-2 cells. In the last 72 h post-infection period, only a survival percentage of 9.09% was determined for the C. jejuni strains, remarkable lower compared to 22.2% of the C. coli isolates (20% human strains and 25% avian strains).
As regards the survival ability within INT 407 cells, as already observed for Caco-2 cells, in the first 24 h post-infection period, 72.7% of C. jejuni strains were able to survive (50% human and 100% avian), as well as all the C. coli strains (100% human source and 100% avian source). In the second 48 h post-infection period, only 18.2% of C. jejuni isolates survived (16.7% human strains and 20% avian strains), in comparison to 66.7% of C. coli (80% human strains and 50% avian strains). In the last 72 h post-infection period, only 9.09% of the C. jejuni strains survived in opposition to 33.3% of the C. coli isolates (20% human strains and 50% avian strains).
3.3 E. coli Translocation Induced by Campylobacter Spp.
In the last part of this investigation, the E. coli translocation induced by Campylobacter spp. was examined. As first, we have selected two strains of Campylobacter, specifically C. jejuni CJHS05 and C. coli CCHS06, possessing broad invasive abilities (ID 38.2% and 25.7% respectively, unpublished data), as well as the non-invasive E. coli 60/06 FB resulted to possess the lowest invasive index (ID 0.67%) among the four examined strains (Table 2). In the following experiments, the translocation of E. coli 60/06 FB was remarkably increased in CJHS05 treated Caco-2 monolayers (2.36 ± 0.42 log cfu/mL) (P < 0.01) and less in CCHS06 treated Caco-2 monolayers (1.2 ± 0.34 log cfu/mL), compared to related control (0.37 ± 0.14 log cfu/mL) (Fig. 4).
E. coli translocation in Caco-2 monolayers inoculated with E. coli 60/06 FB and C. jejuni CCHS05 or C. coli CCHS06 versus monolayers treated with E. coli 60/06 FB alone (control). Data represent mean values of three independent experiments performed in duplicate and asterisks denote values statistically significant compared to the related control (∗∗P < 0.01; Student t-test)
4 Discussion
Campylobacteriosis is a significant public health concern worldwide with most human infections caused by C. jejuni and C. coli (Thakur et al. 2010) through the ingestion of poultry and retail meat products (Igwaran and Okoh 2019). Indeed, these microorganisms can colonise the intestine caecum in extremely high numbers causing severe watery or bloody diarrhoea depending on the individual itself (Scallan et al. 2011). In vitro culture assays and molecular methods (Friis et al. 2005; Zheng et al. 2006; Casabonne et al. 2016) have stressed the importance in determining the pathogenicity of Campylobacter spp. In addition, the survival of these microorganisms inside various cells has been proposed as a fundamental key in their pathogenesis and infections persistence (Klančnik et al. 2006; Buelow et al. 2011).
In this context, we have examined the survival ability of 20 human and avian Campylobacter strains (11 C. jejuni and 9 C. coli) within two different cell lines, specifically Caco-2 and INT 407, widely used to study Campylobacter virulence (Naikare et al. 2006; Buelow et al. 2011; Negretti et al. 2019). The in vitro cellular model herein applied was utilized to understand the pathogenic behavior of C. jejuni and C. coli in a different type of epithelial cell. Indeed, INT 407 cells are considered HeLa derivative because were originally derived from the jejunum and ileum of a 2-month-old Caucasian embryo, later contaminated with HeLa cells, while Caco-2 cells were originally derived from human colon carcinoma. In term of performance, INT 407 cells have the advantage to grow rapidly, we’re easy to maintain and manipulate, while Caco-2 cells have a slower grown and are less applicable for some experimental design. Our results showed that both Campylobacter spp. were efficiently internalized in Caco-2 and INT 407 monolayers within the first 24 h post-infection period (90% and 85% respectively). Interestingly, 48 h post-infection period, the number of survived bacteria was reduced almost twice within Caco-2 cells (55.5%) and INT 407 (40%), while after 72 h post-infection period, no substantial difference in the survival ability were visible in both the used cell lines (15% and 20% respectively). As regards the relation between Campylobacter isolation source (human and avian) and the observed survival ability, was evident that, after 24 and 48 h post-infection periods within Caco-2, the avian strains showed survival percentages higher (from 50% to 100%) compared to those of the human isolates (from 33.3% to 100%). On the contrary, in the case of INT 407 monolayers, in the same post-infection periods, the avian strains showed survival percentages ranging from 20% to 100%, quite similar to those of the human Campylobacter isolates (from 16.7% to 100%). All these observations are in line with data of similar researches that reported the ability of Campylobacter to survive within various types of non-phagocytic cells for at least 24 h (Backert and Hofreuter 2013) or more prolonged time (Naikare et al. 2006). Nevertheless, while the entry process of C. jejuni or C. coli into eukaryotic cells has been focused by many studies (Corcionivoschi et al. 2015; Rawat et al. 2018), only a few reports have examined the intracellular fate of these pathogens within eukaryotic cells (Naikare et al. 2006; Watson and Galán 2008; Buelow et al. 2011). Moreover, in the case of C. coli, to our knowledge, no reports are available on its ability to survive within intestinal cells, making difficult a comparison of the presented data. In this direction, our data give novel and additional information on the survival ability of Campylobacter species, with particular attention to C. coli strains that resulted able to highly survive in both the used cell lines.
The functionality of the intact gut barrier is fundamental to gut health, and any impairment of this barrier, including pathogens, toxins or drugs, can increase host susceptibility to various infectious and inflammatory diseases. As a result, certain bacteria could utilize this “active passage” to translocate across the gut epithelium, leading to a different typology of gut-associated diseases (Nagpal and Yadav 2017). This mechanism, defined as bacterial translocation, has been recognized for Campylobacter as a phenomenon that may facilitate the translocation of different non-invasive commensal bacteria. In literature Lamb-Rosteski and collaborators (2008) have hypothesized that C. jejuni can induce tight junctional disruption, allowing basolateral receptors to migrate to the apical cell surface and promote the following translocation of E. coli. In the last part of our research, a Caco-2 M-like cell model, as described by Kalischuk et al. (2010), was developed on transwell filters to study the induced translocation by C. jejuni or C. coli of a selected non-invasive E. coli. In the literature is well documented the translocation of E. coli induced by C. jejuni 81–176 strain (Kalischuk et al. 2009; Kalischuk et al. 2010) and, to reinforce this observation, here we presented evidence that not only C. jejuni but also C. coli can cross the intestinal epithelial barrier allowing the translocation of E. coli. Therefore, our data support the hypothesis that defects in the intestinal function and/or the disruption of intestinal barrier induced by pathogens, such as C. jejuni and C. coli, can increase the translocation of other bacteria across the intestinal barrier, with possible negative effects on gut and human health. Indeed, this phenomenon can lead to the loss of immunological tolerance (Shen and Turner 2006) and, the failure to downregulate these inflammatory responses in particularly susceptible individuals, can promote the insurgence of chronic inflammations (Resta-Lenert et al. 2005; Kalischuk and Buret 2010).
In conclusion, our investigation showed that both human and avian strains of C. jejuni and C. coli were efficiently internalized and survived within Caco-2 and INT 407 monolayers for 24–48 h after infection, but not for the prolonged period of 72 h. In addition, we showed that Campylobacter spp. can cross the intestinal epithelium thus promoting the translocation of other microorganisms, such as non-invasive E. coli, to extra-intestinal organs. In view of this, further investigations can be addressed to verify whether Campylobacter species may favor the translocation of other non-invasive intestinal bacteria, as well as to delineate the consequences of host responses in order to obtain more information on the gut ecosystem equilibrium in human health and diseases.
Abbreviations
- CJHS:
-
Campylobacter jejuni human sample
- CJAS:
-
Campylobacter jejuni avian sample
- CCHS:
-
Campylobacter coli human sample
- CCAS:
-
Campylobacter coli avian sample
References
Backert S, Hofreuter D (2013) Molecular methods to investigate adhesion, transmigration, invasion and intracellular survival of the foodborne pathogen Campylobacter jejuni. J Microbiol Methods 95:8–23
Bang DD, Nielsen EM, Scheutz F, Pedersen K, Handberg K, Madsen M (2003) PCR detection of seven virulence and toxin genes of Campylobacter jejuni and Campylobacter coli isolates from Danish pigs and cattle and cytolethal distending toxin production of the isolates. J Appl Microbiol 94:1003–1014
Bolton DJ (2015) Campylobacter virulence and survival factors. Food Microbiol 48:99–108
Buelow DR, Christensen JE, Neal-McKinney JM, Konkel ME (2011) Campylobacter jejuni survival within human epithelial cells is enhanced by the secreted protein CiaI. Mol Microbiol 80(5):1296–1312
Casabonne C, Gonzalez A, Aquili V, Subils T, Balague C (2016) Prevalence of seven virulence genes of Campylobacter jejuni isolated from patients with diarrhea in Rosario, Argentina. Int J Inf Secur 3(4):1–6
Cody AJ, Maiden MCJ, Strachan NJC, McCarthy ND (2019) Systematic review of source attribution of human campylobacteriosis using multilocus sequence typing. Euro Surveill 24(43)
Corcionivoschi N, Gundogdu O, Moran L, Kelly C, Scates P, Stef L et al (2015) Virulence characteristics of hcp+ Campylobacter jejuni and Campylobacter coli isolates from retail chicken. Gut Pathog 7:20
Cróinín TO, Backert S (2012) Host epithelial cell invasion by Campylobacter jejuni: trigger or zipper mechanism? Front Cell Infect Microbiol 2:25
de Oliveira MG, Rizzi C, Galli V, Lopes GV, Haubert L, Dellagostin OA, da Silva WP (2019) Presence of genes associated with adhesion, invasion, and toxin production in Campylobacter jejuni isolates and effect of temperature on their expression. Can J Microbiol 65(4):253–260
European Food Safety Authority (EFSA) (2018) The European Union summary report on trends and sources of zoonoses, zoonotic agents and food-borne outbreaks in 2017. EFSA J 16(12):5500
Fouts DE, Mongodin EF, Mandrell RE et al (2005) Major structural differences and novel potential virulence mechanisms from the genomes of multiple Campylobacter species. PLoS Biol 3:72–85
Friesema IH, Havelaar AH, Westra PP, Wagenaar JA, van Pelt W (2012) Poultry culling and Campylobacteriosis reduction among humans, the Netherlands. Emerg Infect Dis 18(3):466–468
Friis LM, Pin C, Pearson BM, Wells JM (2005) In vitro cell culture methods for investigating Campylobacter invasion mechanisms. J Microbiol Methods 61:145–160
Hu L, Tall BD, Curtis SK, Kopecko DJ (2008) Enhanced microscopic definition of Campylobacter jejuni 81176 adherence to, invasion of, translocation across, and exocytosis from polarized human intestinal Caco-2 cells. Infect Immun 76:5294–5304
Humphrey T, O’Brien S, Madsen M (2007) Campylobacters as zoonotic pathogen: a food production perspective. Int J Food Microbiol 117:237–257
Igwaran A, Okoh AI (2019) Human campylobacteriosis: a public health concern of global importance. Heliyon 5:e02814
Kaakoush NO, Castañ-Rodríguez N, Mitchell HM, Man SM (2015) Global epidemiology of Campylobacter infection. Clin Microbiol Rev 28:687–720
Kalischuk LD, Buret AG (2010) A role for Campylobacter jejuni-induced enteritis in inflammatory bowel disease? Am J Physiol Gastrointest Liver Physiol 298:G1–G9
Kalischuk LD, Inglis GD, Buret AG (2009) Campylobacter jejuni induces transcellular translocation of commensal bacteria via lipid rafts. Gut Pathog 1:2
Kalischuk LD, Leggett F, Inglis GD (2010) Campylobacter jejuni induces transcytosis of commensal bacteria across the intestinal epithelium through M-like cells. Gut Pathog 2:14
Klančnik A, Botteldoorn N, Herman L, Smole Možina S (2006) Survival and stress induced expression of groEL and rpoD of Campylobacter jejuni from different growth phases. Int J Food Microbiol 112:200–207
Konkel ME, Mead DJ, Hayes SF, Cieplak W Jr (1992) Translocation of Campylobacter jejuni across human polarized epithelial cell monolayer cultures. J Infect Dis 166:308–315
Krutkiewicz A, Klimuszko D (2010) Genotyping and PCR detection of potential virulence genes in Campylobacter jejuni and Campylobacter coli isolated from different sources in Poland. Folia Microbiol 55:167–175
Lamb-Rosteski JM, Kalischuk LD, Inglis DG, Buret AG (2008) Epidermal growth factor inhibits Campylobacter jejuni-induced claudin-4 disruption, loss of epithelial barrier function, and Escherichia coli translocation. Infect Immun 76:3390–3398
Lertsethtakarn P, Ottemann KM, Hendrixson DR (2011) Motility and chemotaxis in Campylobacter and Helicobacter. Ann Rev Microbiol 65:389–410
Louwen R, Nieuwenhuis EES, van Marrewijk L et al (2012) Campylobacter jejuni translocation across intestinal epithelial cells is facilitated by ganglioside-like lipooligosaccharide structures. Infect Immun 80(9):3307
Nagpal R, Yadav H (2017) Bacterial translocation from the gut to the distant organs: an overview. Ann Nutr Metab 71(Suppl 1):11–16
Naikare H, Palyada K, Panciera R, Marlow D, Stintzi A (2006) Major role for FeoB in Campylobacter jejuni ferrous iron acquisition, gut colonisation, and intracellular survival. Infect Immun 74:5433–5444
Negretti NM, Clair G, Talukdar PK et al (2019) Campylobacter jejuni demonstrates conserved proteomic and transcriptomic responses when co-cultured with human INT 407 and Caco-2 epithelial cells. Front Microbiol 10:755
Rawat N, Maansi KD, Upadhyay AK (2018) Virulence typing and antibiotic susceptibility profiling of thermophilic Campylobacters isolated from poultry, animal, and human species. Veterinary World 11(12):1698–1705
Resta-Lenert S, Smitham J, Barrett KE (2005) Epithelial dysfunction associated with the development of colitis in conventionally housed mdr1a−/−mice. Am J Physiol Gastrointest Liver Physiol 289:G153–G162
Scallan E, Hoekstra RM, Angulo FJ et al (2011) Foodborne illness acquired in the United States--major pathogens. Emerg Infect Dis 17(1):7–15
Shen L, Turner JR (2006) Role of epithelial cells in initiation and propagation of intestinal inflammation. Eliminating the static: tight junction dynamics exposed. Am J Physiol Gastrointest Liver Physiol 290:G577–G582
Šikić Pogačar M, Rubeša Mihaljević R, Klančnik A, Brumini G, Abram M, Smole MS (2009) Survival of stress exposed Campylobacter jejuni in the murine macrophage J774 cell line. Int J Food Microbiol 129:68–73
Talukder KA, Aslam M, Islam Z et al (2008) Prevalence of virulence genes and cytolethal distending toxin production in Campylobacter jejuni isolates from diarrheal patients in Bangladesh. J Clin Microbiol 46(4):1485–1488
Thakur S, Zhao S, McDermott PF et al (2010) Antimicrobial resistance, virulence, and genotypic profile comparison of Campylobacter jejuni and Campylobacter coli isolated from humans and retail meats. Foodborne Pathog Dis 7(7):835–844
Watson RO, Galán JE (2008) Campylobacter jejuni survives within epithelial cells by avoiding delivery to lysosomes. PLoS Pathog 4(1):e14
Wilson DJ, Gabriel E, Leatherbarrow AJ et al (2008) Tracing the source of campylobacteriosis. PLoS Genet 4:e1000203
Wysok B, Wojtacka J (2018) Detection of virulence genes determining the ability to adhere and invade in Campylobacter spp. from cattle and swine in Poland. Microb Pathog 115:257–263
Zheng J, Meng JH, Zhao SH, Singh R, Song WX (2006) Adherence to and invasion of human intestinal epithelial cells by Campylobacter jejuni and Campylobacter coli isolates from retail meat products. J Food Prot 69:768–774
Conflict of Interest
The authors declare that they have no competing interests.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Campana, R., Baffone, W. (2020). Intracellular Survival and Translocation Ability of Human and Avian Campylobacter jejuni and Campylobacter coli Strains. In: Donelli, G. (eds) Advances in Microbiology, Infectious Diseases and Public Health. Advances in Experimental Medicine and Biology(), vol 1282. Springer, Cham. https://doi.org/10.1007/5584_2020_531
Download citation
DOI: https://doi.org/10.1007/5584_2020_531
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-53646-6
Online ISBN: 978-3-030-53647-3
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)