Abstract
Growth hormone and insulin-like growth factor-1 (IGF-1) play a crucial role in the regulation of bone turnover. Adequate vitamin D status supports proper bone remodeling, leading to normal longitudinal bone growth and normal peak bone mass. The aim of this study was to evaluate the association between serum 25-hydroxyvitamin D [25(OH)D] and carboxy-terminal cross-linked telopeptide of type I collagen (ICTP) in children and adolescents with growth hormone deficiency at baseline and during recombinant human growth hormone (rhGH) replacement therapy. The study was prospective and included 30 children and adolescents aged 5 to 17 years. Concentrations of 25(OH)D, ICTP, and IGF-1 were measured at baseline and during the first year of rhGH therapy. Baseline serum 25(OH)D concentration correlated with ICTP concentrations during the first trimester of rhGH therapy (r = 0.38, p < 0.050); the correlation was stronger in the second trimester of therapy (r = 0.6, p = 0.002). We conclude that proper vitamin D status is important in reaching the adequate dynamics of bone remodeling during growth, which is essential to achieve a catch-up growth during rhGH therapy.
Access provided by CONRICYT-eBooks. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Bone turnover is regulated by a variety of factors that act systemically or locally. Some of them are nutritional factors, including 25-hydroxyvitamin D [25(OH)D] (Schwetz et al. 2017; Bonjour et al. 2014). Hypovitaminosis D is common among children and adolescents, especially those who do not receive supplementation during autumn and winter seasons. The relationship between bone turnover markers and 25(OH)D status is not quite clear, but in recent years it has been studied extensively in children, adolescents, and adults (Larijani et al. 2016; Thiering et al. 2015; Napoli et al. 2014; Fares et al. 2003). Bone turnover markers are widely used in medicine. They are a useful tool in evaluating bone health, diagnosing, and in treatment monitoring in primary and secondary bone diseases in oncology, rheumatology, nephrology, cardiology, and endocrinology (Shetty et al. 2016; Fardellone et al. 2014; Wheater et al. 2013; Lijnen et al. 2012; Coleman et al. 2011). In pediatric endocrinology, bone turnover markers are used in the evaluation of skeletal metabolism and growth (Bowden et al. 2016; Szulc et al. 2000). These markers could be particularly helpful in metabolic disorders related to diabetes, obesity, and in those patients who are treated with corticosteroids (Matusik et al. 2015; Zhukouskaya et al. 2014). In children with growth hormone deficiency, selected bone turnover markers could be used to monitor the efficacy of recombinant human growth hormone (rhGH) therapy (Andersson et al. 2015; Kandemir et al. 2002). The interpretation of bone turnover marker values could be difficult due to their variability depending on age, pubertal stage, current growth velocity, mineral accrual, nutritional status, and the influence of hormones, especially growth hormone/insulin-like growth factors (GH/IGFs) axis and sex steroids (Locatelli and Bianchi 2014; Federico et al. 2003; Szulc et al. 2000).
Classical biochemical markers of bone turnover are divided into two groups: bone formation markers and bone resorption markers. Bone formation markers are products of osteoblasts’ activity during different phases of their development. These markers are measured in serum or plasma and they are categorized as by-products of collagen synthesis [carboxy- (PICP) and amino-terminal (PINP) propeptides of procollagen type I], osteoblast enzymes [total alkaline phosphatase (ALP) and bone-specific alkaline phosphatase (BALP)], and matrix proteins [osteocalcin (OC)]. Bone resorption markers, on the other side, arise during the resorption phase of bone remodeling. They can be measured in serum or urine. They are mainly products of collagen degradation by osteoclasts, such as telopeptides of type I collagen (carboxy-terminal: CTX-1 and ICTP, also referred to as CTX-matrix metalloproteinases - MMP; and amino-terminal: NTX-1), hydroxyproline and pyridinium crosslinks [pyridinoline (PYD), deoxypyridinoline (DPD)]. Bone resorption markers are also non-collagenous proteins (bone sialoprotein) and osteoclastic enzymes [tartrate-resistant acid phosphatase – isoform 5b (TRAP5b), cathepsin K] (Chapurlat and Confavreux 2016; Wheater et al. 2013; Szulc et al. 2000). According to Shetty et al. (2016), the group of bone resorption markers also includes osteocyte activity markers such as a receptor activator of nuclear factor kappa-B ligand (RANKL), osteoprotegerin (OPG), Dickkopf-related protein-1 (DKK-1), and sclerostin. Recently, some authors have described potential new bone markers such as markers of bone metabolism (periostin and sphingosine-1-phosphate), hormones (fibroblast growth factor-23, klotho, osteocalcin), and micro-RNAs (miR-148a, miR125b) (Chapurlat and Confavreux 2016; Garnero 2014).
The aim of the present study was to evaluate the association between serum 25(OH)D and carboxy-terminal cross-linked telopeptide of type I collagen (ICTP) levels in children with growth hormone deficiency at baseline and during the first year of rhGH therapy. We also sought to determine if ICTP could help predict the growth response to rhGH therapy in children and adolescents with growth hormone deficiency.
2 Methods
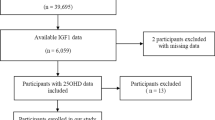
The study was approved by the Bioethics Committee of Medical University of Warsaw, Poland. All patients or their parents gave written informed consent for participation in the study. The study was conducted at the Department of Paediatrics and Endocrinology of the Medical University of Warsaw in Poland in the years 2013–2016 and it included 30 children and adolescents (9 girls and 21 boys) aged 4.8–16.6 years (mean 11.4 ± 3.2 years) with growth hormone deficiency. The study was prospective in nature as it evaluated the first year of rhGH treatment. Growth hormone deficiency was diagnosed as growth hormone concentrations below 10 ng/ml in the following three tests: one test evaluating spontaneous growth hormone secretion at night during sleep and two stimulation tests with different stimuli such as clonidine, insulin, glucagon, or arginine. The maximum growth hormone secretion in a particular patient was defined as the highest concentration of growth hormone in any of the three tests. Growth rate at baseline was calculated based on the measurement of height taken twice at six-month intervals. Anthropometric measurements were taken at baseline and after 3, 6, and 12 months of rhGH treatment. Based on those measurements, growth rate in the first year of rhGH treatment was calculated. Bone age was evaluated in each patient using the Greulich and Pyle method at baseline and after 12 months of rhGH treatment (Greulich and Pyle 1959). 25(OH)D concentration was measured at baseline and after 6 and 12 months of rhGH treatment. ICTP and insulin-like growth factor-1 (IGF-1) were measured at baseline and after 3, 6, and 12 months of rhGH treatment. The mean dose of rhGH in the first 12 months of therapy was 0.187 mg/kg/week. Apart from rhGH treatment, all patients received cholecalciferol in doses of 1,000 IU/day within the first 12 months of rhGH therapy.
2.1 Biochemical Evaluation
GH and IGF-1 concentrations were measured by immunoassay using Immulite Analyzer from Siemens (Erlangen, Germany); 25(OH)D concentration was measured by immunoassay using Architect Analyzer (Abbott Diagnostics; Abbott Park, IL); and ICTP concentration was measured by Human ICTP ELISA kit using Asys UVM 340 Microplate Reader from Biochrom (Cambridge, England).
2.2 Statistical Elaboration
Data are reported as means ±SD, median and interquartile ranges, or as percentages. Data normality was checked by the Shapiro-Wilk normality test. Comparisons between baseline and treatment values were conducted using the Wilcoxon signed-rank test for non-parametric parameters and a t-test for parametric parameters. In addition, Spearman and Pearson’s correlation analyses were performed. A p-value <0.05 was used to indicate statistically significant differences. Statistical elaboration was conducted with a commercial Statistica v13.1 package (StatSoft; Tulsa, OK).
3 Results
The maximum growth hormone secretion in the study group was 7.4 ± 1.7 ng/ml. In the first year of rhGH therapy, the mean growth rate increased significantly from 4.6 ± 1.3 cm/year at baseline to 9.3 ± 1.8 cm/year (p < 0.00001). Height deficit declined during that time from 2.5 ± 0.4 cm at baseline to −1.9 ± 0.5 cm (p < 0.00001). A reduction in height deficit was significant as early as after the first trimester of rhGH therapy (p < 0.00002). The mean bone age increased significantly after the start of rhGH therapy from 8.9 ± 3.1 years at baseline to 10.6 ± 3.0 years (p < 0.000001). The characteristics of the study group at baseline and during the first 12 months rhGH therapy are shown in Table 1. The mean 25(OH)D concentration was 24.2 ± 7.8 ng/ml at baseline and increased significantly during the first 6 months of rhGH therapy to 28.5 ± 5.3 ng/ml (p = 0.014). 25(OH)D concentration after six and 12 months of rhGH therapy was not appreciably different. The mean ICTP value at baseline was 0.72 ± 0.42 ng/ml and decreased after the first 3 months of rhGH therapy to 0.68 ± 0.27 ng/ml; the difference was insignificant. After 6 months of rhGH therapy, ICTP concentration increased to 0.79 ± 0.49 ng/ml, which was higher than the baseline value (p = 0.02). After 12 months of rhGH therapy, ICTP concentration slightly decreased to 0.74 ± 0.11 ng/ml; the figure was still significantly greater than the baseline level (p < 0.001), but not so compared with the level present 6 months after rhGH therapy. As expected, IGF-1 concentrations increased significantly in the first 12 months of rhGH treatment (p < 0.000001), and the difference was significant as early as after 3 months of therapy (p = 0.000002). Table 2 details the biochemical indices evaluated at baseline and during rhGH treatment.
The serum 25(OH)D concentration did not correlate with that of ICTP at baseline, but it did correlate with ICTP changes during the first 3 months of rhGH therapy (r = 0.38, p < 0.05, Fig. 1). Likewise, there was no correlation between the serum 25(OH)D and ICTP after 6 months of rhGH therapy, but 25(OH)D did correlate with ICTP changes between the three and 6 months of rhGH therapy (r = 0.6, p = 0.002) (Fig. 2). The latter correlation was no longer present after 12 months of therapy. In addition, we found that ICTP changes between baseline and first 6 months of fhGH therapy correlated positively with growth rate (cm/year) (r = 0.43, p = 0.042).
4 Discussion
Growth hormone, insulin-like growth factors, and IGF-binding proteins are essential proteins, among many other factors regulating bone turnover, for achieving a normal longitudinal bone growth and peak bone mass (Schwetz et al. 2017; Bonjour et al. 2014). During puberty GH/IGF axis’s effects on bone are supported by sex steroids action (Locatelli and Bianchi 2014; Mrak et al. 2007). Bone development is also affected by genetic and environmental factors such as nutrition and lifestyle, including calcium intake and 25(OH)D level. Adequate 25(OH)D status is needed to achieve peak bone mass and 25(OH)D contributes to normal bone formation and resorption (Rizzoli et al. 2010). 25(OH)D is especially important in adolescents because of rapid growth during puberty and development of peak bone mass (Fares et al. 2003). There is no clear explanation of the relationship between bone turnover markers and 25(OH)D, although this relationship has been extensively studied in recent years (Schwetz et al. 2017, Larijani et al. 2016, Thiering et al. 2015, Napoli et al. 2014). Bone turnover correlates closely with growth rate and pubertal status, and it is at its dynamic most during the first 2 years of life and during the adolescence growth spurt. A faster bone turnover in these two periods is accompanied by a large increase in the concentration of bone remodeling markers (Fares et al. 2003; Federico et al. 2003). A study by van Coeverden et al. (2002) shows that markers of bone formation (BALP, OC, and PICP) and markers of bone resorption (ICTP) in children and adolescents reach the maximum values at pubertal stage G4 in boys and Th 3 in girls. The markers content parallels the increases in sex steroids and IGF-1 concentrations.
In children with growth hormone deficiency, content of bone turnover markers declines as a consequence of decreased bone metabolism, which leads to decreased bone mineral density (Szulc et al. 2000; Vihervuori et al. 1997; Kubo et al. 1995). GH therapy stimulates the secretion of insulin-like growth factors-1 and IGF-binding protein-3, which activates bone turnover. After onset of growth hormone therapy, markers of both bone formation and resorption increase with a peak between the three and 6 months of treatment and then remain elevated over the following months of therapy (Andersson et al. 2015; Mrak et al. 2007; Kandemir et al. 2002; Baroncelli et al. 2000).
In the present study, ICTP values increased significantly after onset of rhGH therapy, with a peak at 6 months of therapy and remained still higher than the baseline value at 12 months of therapy. This is in line with the studies of other authors above mentioned. Changes in ICTP content within the first 6 months of therapy correlated positively with the growth rate achieved in the first year of rhGH therapy. That supports the hypothesis that biochemical markers of bone turnover can help predict the gain in height during rhGH therapy. According to the literature, PICP, and BALP among bone formation markers, and ICTP, PYD, and DPD among bone resorption markers have the greatest predictive strength (Szulc et al. 2000; Kubo et al. 1995).
In the present study, the mean baseline 25(OH)D level was 24.2 ± 7.8 ng/ml. Vitamin D3 supplementation had been recommended to most patients in a dose of 1000 IU/d before onset of rhGH therapy, while diagnosing short stature. After regular supplementation, 25(OH)D level increased to 28.5 ± 5.3 ng/ml at 6 months, reaching a plateau for the next months. The baseline 25(OH)D values were not associated with the baseline ICTP values. We failed to find a direct correlation between the 25(OH)D and ICTP levels in any of the measurements at any evaluated time point, but we found a correlation between the 25(OH)D levels and changes in ICTP concentrations during rhGH therapy. Baseline 25(OH)D correlated positively with an increase in ICTP concentrations during the first 3 months of rhGH therapy, while 25(OH)D level after 6 months of therapy correlated with changes in ICTP concentrations between the three and 6 months of therapy. Those results are in line with some recent studies that have shown a positive correlation between the serum 25(OH)D level and bone turnover. Such a correlation has been found in healthy children and adolescents during rapid growth during puberty, and in children with GHD during catch-up growth after onset of rhGH therapy (Larijani et al. 2016; Thiering et al. 2015; Fares et al. 2003). These results confirm that proper 25(OH)D status is important in the bone remodeling during growth and helps improve the growth rate. Vitamin D3 supplementation is important during rapid growth in healthy children and adolescents and in children treated with rhGH.
5 Conclusions
Bone resorption increases significantly after onset of rhGH therapy. Early increases in the concentration of carboxy-terminal cross-linked telopeptide of type I collagen correlate with the growth rate during rhGH therapy. Correct vitamin D3 status contributes to an increase in bone turnover after onset of rhGH therapy, which is necessary to achieve catch-up growth. Vitamin D3 supplementation should be recommended to patients with growth hormone deficiency treated with rhGH.
References
Andersson B, Swolin-Eide D, Magnusson P, Albertsson-Wikland K (2015) Short-term changes in bone formation markers following growth hormone (GH) treatment in short prepubertal children with a broad range of GH secretion. Clin Endocrinol 82(1):91–99
Baroncelli GI, Bertelloni S, Ceccarelli C, Cupelli D, Saggese G (2000) Dynamics of bone turnover in children with growth hormone (GH) deficiency treated with GH until final height. Eur J Endocrinol 142:549–556
Bonjour JP, Kohrt W, Levasseur R, Warren M, Whiting S, Kraenzlin M (2014) Biochemical markers for assessment of calcium economy and bone metabolism: application in clinical trials from pharmaceutical agents to nutritional products. Nutr Res Rev 27:252–267
Bowden SA, Akusoba CI, Hayes JR, Mahan JD (2016) Biochemical markers of bone turnover in children with clinical bone fragility. J Pediatr Endocrinol Metab 29(6):715–722
Chapurlat RD, Confavreux CB (2016) Novel biological markers of bone: from bone metabolism to bone physiology. Rheumatology 55:1714–1725
Coleman R, Costa L, Saad F, Cook R, Hadji P, Terpos E, Garnero P, Brown J, Body JJ, Smith M, Lee KA, Major P, Dimopoulos M, Lipton A (2011) Consensus on the utility of bone markers in the malignant bone disease setting. Crit Rev Oncol Hematol 80:411–432
Fardellone P, Séjourné A, Paccou J, Goëb V (2014) Bone remodeling markers in rheumatoid arthritis. Mediat Inflamm 2014:484280. https://doi.org/10.1155/2014/484280
Fares JE, Choucair M, Nabulsi M, Salamoun M, Shahine CH, Fuleihan GEH (2003) Effect of gender, puberty, and vit. D status on biochemical markers of bone remodeling. Bone 33:242–247
Federico G, Baroncelli GI, Vanacore T, Fiore L, Saggese G (2003) Pubertal changes in biochemical markers of growth. Horm Res 60(Suppl 1):46–51
Garnero P (2014) New developments in biological markers of bone metabolism in osteoporosis. Bone 66:46–55
Greulich WW, Pyle SI (1959) Radiographic atlas of skeletal development of the hand and wrist, 2nd edn. Stanford University Press, Stanford
Kandemir N, Gonc EN, Yordam N (2002) Responses of bone turnover markers and bone mineral density to growth hormone therapy in children with isolated growth hormone deficiency and multiple pituitary hormone deficiencies. J Pediatr Endocrinol Metab 15(6):809–816
Kubo T, Tanaka H, Inoue M, Kanzaki S, Seino Y (1995) Serum levels of carboxyterminal propeptide of type I procollagen and pyridinoline crosslinked telopeptide of type I collagen in normal children and children with growth hormone (GH) deficiency during GH therapy. Bone 17:397–401
Larijani B, Hossein-Nezhad A, Feizabad E, Maghbooli Z, Adibi H, Ramezani M, Taheri E (2016) Vitamin D deficiency, bone turnover markers and causative factors among adolescents: a cross-sectional study. J Diabetes Metab Disord 15:46. https://doi.org/10.1186/s40200-016-0266-2
Lijnen PJ, Maharani T, Finahari N, Prihadi JS (2012) Serum collagen markers and heart failure. Cardiovasc Hematol Disord Drug Targets 12(1):51–55
Locatelli V, Bianchi VE (2014) Effect of GH/IGF-1 on bone metabolism and osteoporosis. Int J Endocrinol 2014:235060. https://doi.org/10.1155/2014/235060
Matusik P, Olszanecka-Glinianowicz M, Chudek J, Małecka-Tendera E (2015) Bone turnover markers in the obese children – relations to gender, body composition and leptin level. Pediatr Endocrinol Diabetes Metab 21(4):154–161
Mrak E, Villa I, Lanzi R, Losa M, Guidobono F, Rubinacci A (2007) Growth hormone stimulates osteoprotegerin expression and secretion in human osteoblast-like cells. J Endocrinol 192:639–645
Napoli N, Strollo R, Sprini D, Maddaloni E, Rini GB, Carmina E (2014) Serum 25-OH vit. D in relations to bone mineral density and bone turnover. Int J Endocrinol 2014:487463. https://doi.org/10.1155/2014/487463
Rizzoli R, Bianchi ML, Garabédian M, McKay HA, Moreno LA (2010) Maximizing bone mineral mass gain during growth for the prevention of fractures in the adolescents and the elderly. Bone 46:294–305
Schwetz V, Trummer C, Pandis M, Grübler MR, Verheyen N, Gaksch M, Zittermann A, März W, Aberer F, Lang A, Treiber G, Friedl C, Obermayer-Pietsch B, Pieber TR, Tomaschitz A, Pilz S (2017) Effects of vit. D supplementation on bone turnover markers: a randomized controlled trial. Forum Nutr 9(5). https://doi.org/10.3390/nu9050432
Shetty S, Kapoor N, Bondu JD, Thomas N, Paul TV (2016) Bone turnover markers: emerging tool in the management of osteoporosis. Indian J Endocrinol Metab 20(6):846–852
Szulc P, Seeman E, Delmas PD (2000) Biochemical measurements of bone turnover in children and adolescents. Osteoporosis Int 11(4):281–294
Thiering E, Brüske I, Kratzsch J, Hofbauer LC, Berdel D, von Berg A, Lehmann I, Hoffmann B, Bauer CP, Koletzko S, Heinrich J (2015) Associations between serum 25-hydroxyvit. D and bone turnover markers in a population based sample of German children. Sci Rep 5:18138. https://doi.org/10.1038/srep18138
van Coeverden SC, Netelenbos JC, de Ridder CM, Roos JC, Popp-Snijders C, Delemarre-van de Waal HA (2002) Bone metabolism markers and bone mass in healthy pubertal boys and girls. Clin Endocrinol 57:107–116
Vihervuori E, Turpeinen M, Siimes MA, Koistinen H, Sorva R (1997) Collagen formation and degradation increase during growth hormone therapy in children. Bone 20:133–138
Wheater G, Elshahaly M, Tuck SP, Datta HK, van Laar JM (2013) The clinical utility of bone marker measurements in osteoporosis. J Transl Med 11:201. https://doi.org/10.1186/1479-5876-11-201
Zhukouskaya VV, Eller-Vainicher C, Shepelkevich AP, Dydyshko Y, Cairoli E, Chiodini I (2014) Bone health in type 1 diabetes: focus on evaluation and treatment in clinical practice. Adv Endocrinol Invest 38(9):941–950
Conflicts of Interest
The authors declare no conflicts of interest in relation to this article.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2017 Springer International Publishing AG
About this chapter
Cite this chapter
Witkowska-Sędek, E., Stelmaszczyk-Emmel, A., Kucharska, A., Demkow, U., Pyrżak, B. (2017). Association Between Vitamin D and Carboxy-Terminal Cross-Linked Telopeptide of Type I Collagen in Children During Growth Hormone Replacement Therapy. In: Pokorski, M. (eds) Clinical Investigation. Advances in Experimental Medicine and Biology(), vol 1047. Springer, Cham. https://doi.org/10.1007/5584_2017_109
Download citation
DOI: https://doi.org/10.1007/5584_2017_109
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-74079-9
Online ISBN: 978-3-319-74080-5
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)