Abstract
Obstructive sleep apnea syndrome (OSAS) is characterized by complete cessation of inspiratory flow (apnea) or upper airway airflow limitation (hypopnea) with increased respiratory muscle activity, which is repeatedly observed during sleep. Hypothyroidism has been described as a rare cause of OSAS, but it is considered to be the main cause of breathing disorders during sleep in patients in whom an improvement of OSAS is observed after thyroid hormone replacement therapy. Nevertheless, euthyreosis due to thyroxine replacement in patients with OSAS often does not improve the breathing disorder and treatment with continuous positive airway pressure is usually applied. The aim of this study was to assess thyroid function in patients with OSAS. We studied 813 patients in whom severe OSAS was diagnosed; the mean apnea-hypopnea index was 44.0. Most of the patients were obese (mean BMI 33.1 ± 6.6 kg/m2) and had excessive daytime sleepiness (ESS 12.8 ± 6.6). With the thyroid stimulating hormone (TSH) concentration as the major criterion, hypothyroidism was diagnosed in 38 (4.7 %) and hyperthyroidism was diagnosed in 31 (3.8 %) patients. Analysis of basic anthropometric data, selected polysomnography results, and TSH, fT3, and fT4 values did not reveal any significant correlations. In conclusion, the incidence of thyroid function disorders seems to be no different in OSAS than that in the general population. We did not find correlations between TSH activity and the severity of breathing disorders during sleep.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Obstructive sleep apnea syndrome (OSAS) is characterized by complete cessation of inspiratory flow (apnea) or upper airway airflow limitation (hypopnea) with increased respiratory muscle activity, which is repeatedly observed during sleep. OSAS is the most frequent disease among breathing disorders during sleep. Prevalence of OSAS ranges from 4 to 10 % of middle-aged men and from 2 to 4 % of middle-aged women (Young et al. 1993; Plywaczewski et al. 2008). The most important risk factors for OSAS are obesity, craniofacial structural abnormalities (curvature of the nasal septum, hyperglossia, structural abnormalities and position of the mandible, overgrown tonsils, and structural abnormalities of the soft palate and the uvula), and a decreased upper airway muscle activity.
Hypothyroidism has been described as a rare cause of OSAS. In 1964, Massumi and Winnacker (1964) reported a case of myxoedema and apneas. Hypothyroidism is considered to be the main cause of breathing disorders during sleep in patients in whom an improvement of OSAS is observed after thyroid hormone replacement therapy (Orr et al. 1981; Skatrud et al. 1981; Millman et al. 1983). However, euthyreosis due to thyroxine replacement in patients with OSAS often does not improve the breathing disorder and in these patients CPAP treatment is usually applied. According to Grunstein and Sullivan (1988), only does combined treatment significantly reduce the risk of myocardial infarction in these patients.
The incidence of OSAS in patients with hypothyroidism has been reported as high as 80 % (Grunstein and Sullivan 1988; Rajagopal et al. 1984). However, some of the later publications do not demonstrate a significant correlation between low thyroid hormone activity and the incidence or severity of OSAS (Resta et al. 2005). Lin et al. (1992) and Pelttari et al. (1994) have found a lower incidence hypothyroidism and OSAS. Winkelman et al. (1996) have found low thyroid hormone activity only in 3 of 103 patients with OSAS and concluded that in the absence of clinical symptoms consistent with hypothyroidism, OSAS patients do not require routine assessment of serum TSH and thyroxine levels. Similar results were obtained by Kapur et al. (1998) who noted hypothyroidism in 4 out of 284 patients with breathing disorders during sleep. Taking into account these equivocal reports, we decided to assess the thyroid hormonal status in a large unselected group of OSAS patients in order to establish a rationale for the routine thyroid function testing in this population.
2 Methods
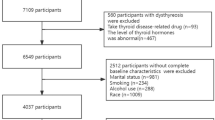
The study was approved by the institutional Review Board for Human Research. This retrospective study included 813 patients (F/M – 146/667). The diagnosis of OSAS was established in accordance with the American Academy of Sleep Medicine recommendations (AASM 2014). All patients underwent a 7-h polysomnography (Embla System – S4000; Reyjkjavik, Iceland) during which airflow, chest and abdominal motion, and the oxygen arterial blood saturation were monitored. Airflow was measured with the use of a pressure cannula or a three-channel thermistor placed in the front nostrils and the mouth area. Chest and abdominal motion were recorded with the use of two piezoelectric belts placed around the abdomen and chest; an integral part of the polysomnography system. Oxygen arterial blood saturation was recorded with pulse oximetry. The electroencephalogram (EEG), electrooculogram (EOG) and electromyogram (EMG) were recorded to determine sleep structure and number of awakenings. During sleep cardiac function was monitored by a one-lead ECG. The Epworth Sleepiness Scale (ESS) was used to assess the daytime sleepiness (Johns 1991). The diagnosis of OSAS was made when the apnea-hypopnea index (AHI) value exceeded 5.0.
Fasting serum concentrations of thyroid stimulating hormone (TSH), free triiodothyronine (fT3) and free thyroxine (fT4) were assessed by electrochemiluminescence (Roche Diagnostics; Basel, Switzerland). The normal value for our laboratory ranges from 0.27 to 4.2 μIU/ml for TSH, 3.1–6.8 pmol/l for fT3, and 12.0–22.0 pmol/l for fT4.
Data are reported as means ± SD. To assess the influence of TSH, fT3, and fT4 on the polysomnography results the non-parametric Mann-Whitney U test was applied. Statistical analysis was performed with Statistica 9 Software (StatSoft; Tulsa, OK).
3 Results
We studied 813 patients in whom severe OSAS was diagnosed; the mean AHI was 44.0. Most of the patients were obese (mean BMI 33.1 ± 6.6 kg/m2) and had excessive daytime sleepiness (ESS, 12.8 ± 6.6). Table 1 presents the characteristics of the group and the polysomnography (PSG) results.
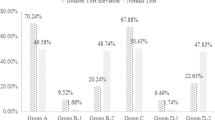
Lowered thyroid function was noted in 38 patients. Three patients from this group had been previously diagnosed and received replacement treatment with thyroxine. Thirty one patients had laboratory features of hyperthyroidism. Table 2 presents the characteristics of those groups.
With the TSH concentration as the major criterion, hypothyroidism was diagnosed in 38 (4.7 %) and hyperthyroidism was diagnosed in 31 (3.8 %) patients, respectively. Analysis of the basic anthropometric data, selected PSG results, and TSH, fT3 and fT4 values did not reveal significant correlations.
4 Discussion
Hypofunction of the thyroid gland in patients with OSAS has been reported in the literature. Some authors report the incidence of hypothyroidism in patients with OSAS to be as high as 40 % (Hira and Sibal 1999). Hypothyroidism is often accompanied by obesity, a major risk factor for OSAS. On the other hand, replacement therapy with thyroxine results in a decrease in the number of apneas even without a reduction in body weight, indicating a more complex mechanism of breathing disorders in these patients (Rajagopal et al. 1984). Some authors hypothesize that OSAS may also be a result of hypothyroid myopathy leading to upper airway muscle collapse and narrowing during sleep (Kendall-Taylor and Turnbull 1983). Thyroid hormone replacement therapy does not always result in a reduction of breathing disorders. In the series of patients studied by Misiolek et al. (2007), patients receiving replacement therapy showed a lower snoring intensity, but the respiratory disturbance index (RDI) did not change significantly; neither did the minimal oxygen saturation during sleep.
The accumulation of mucopolysaccharides in the upper airways, particularly in the throat and the palate, may be yet another pathogenic factor (Orr et al. 1981). In the study by Jha et al. (2006), hyperglossia was diagnosed in 33 % of the patients with hypothyroidism, and edema of the face or throat was noted in 83 %.
The prevalence of hypothyroidism in the patients with OSAS of the present study was 4.7 % and this is comparable with the incidence of hypothyroidism in adult population of Poland, estimated to be 2–5 % (Zgliczynska 1998). One study has reported a much lower prevalence of hypothyroidism in OSAS at 1.5 %; however, it included a smaller group consisting of 103 OSAS patients (Winkelman et al. 1996).
The present results showed no significant correlation between the TSH activity and the severity of OSAS; the correlation between TSH and age is well known and has also been confirmed in this study. TSH abnormalities alone are not necessarily associated with higher AHI/RDI values, as it has been shown that mainly the fT3 and fT4 concentrations influence breathing in a hypothyroid patient. These observations have been confirmed by Winkelman et al. (1996) who demonstrate that a higher TSH value indicates a higher risk of OSAS only in women over 60 years of age. One may assume that fT3 and fT4 concentrations are better markers in predicting apnea risk. Lower daytime sleepiness and higher oxygen saturation may be ameliorated by these two hormones, and we may hypothesize that they can relieve apnea symptoms.
The present study demonstrates that there is no rationale for a routine assessment of thyroid activity in patients suspected of breathing disorders during sleep. We agree with Winkelman et al. (1996) that thyroid hormone testing should be limited to patients with clinical symptoms suggestive of hypothyroidism such as characteristic skin color, psychomotor retardation, excessive sleepiness and asthenia, or a large increase in body weight. It should be remembered, however, that Deegan et al. (1997) have described a patient with biochemical features of hypothyroidism, without clinical symptoms, in whom significant breathing disorders during sleep were found. Therefore, assessment of thyroid hormones should be individually considered. In conclusion, the incidence of thyroid function disorders in sleep apnea patients seems to be no different than that in the general population. We failed to find correlations between TSH activity and the severity of breathing disorders during sleep.
References
AASM (2014) American Academy of Sleep Medicine. http://www.aasmnet.org/practiceguidelines.aspx. Accessed on 27 Mar 2015
Deegan PC, McNamara VM, Morgan WE (1997) Goitre: a cause of obstructive sleep apnoea in euthyroid patients. Eur Respir J 10:500–502
Grunstein RR, Sullivan CE (1988) Sleep apnea and hypothyroidism: mechanisms and management. Am J Med 85:775–779
Hira HS, Sibal L (1999) Sleep apnea syndrome among patients with hypothyroidism. J Assoc Physicians India 47(6):615–618
Jha A, Sharma SK, Tandon N, Lakshmy R, Kadhiravan T, Handa KK, Gupta R, Pandey RM, Chaturvedi PK (2006) Thyroxine replacement therapy reverses sleep-disordered breathing in patients with primary hypothyroidism. Sleep Med 7(1):55–61
Johns MW (1991) A new method for measuring daytime sleepiness: the Epworth sleepiness scale. Sleep 14:540–545
Kapur VK, Koepsell TD, deMaine J, Hert R, Sandblom RE, Psaty BM (1998) Association of hypothyroidism and obstructive sleep apnea. Am J Respir Crit Care Med 158:1379–1383
Kendall-Taylor P, Turnbull DM (1983) Endocrine myopathies. Br Med J 287:705–709
Lin CC, Tsan KW, Chen PJ (1992) The relationship between sleep apnea syndrome and hypothyroidism. Chest 102:1663–1667
Massumi RA, Winnacker JL (1964) Severe depression of the respiratory center in myxedema. Am J Med 36:876–882
Millman RP, Bevilacqua J, Peterson DD, Pack AI (1983) Central sleep apnea in hypothyroidism. Am Rev Respir Dis 127:504–507
Misiolek M, Marek B, Namyslowski G, Scierski W, Zwirska-Korczala K, Kazmierczak-Zagorska Z, Kajdaniuk D, Misiolek H (2007) Sleep apnea syndrome and snoring in patients with hypothyroidism with relation to overweight. J Physiol Pharmacol 58(Suppl 1):77–85
Orr WC, Males JR, Imes NK (1981) Myxedema and obstructive sleep apnea. Am J Med 70:1061–1066
Pelttari L, Rauhala E, Polo O, Hyyppä MT, Kronholm E, Viikari J, Kantola I (1994) Upper airway obstruction in hypothyroidism. J Intern Med 236:177–181
Pływaczewski R, Bednarek M, Jonczak L, Zieliński J (2008) Sleep disordered breathing in middle-aped and older Polish urban population. J Sleep Res 17:73–81
Rajagopal KR, Abbrecht PH, Derderian SS (1984) Obstructive sleep apnea in hypothyroidism. Ann Intern Med 101:491–494
Resta O, Carratu P, Carpagnano GE, Maniscalco M, Di Gioia G, Lacedonia D, Giorgino R, De Pergola G (2005) Influence of subclinical hypothyroidism and T4 treatment on the prevalence and severity of obstructive sleep apnoea syndrome (OSAS). J Endocrinol Invest 28(10):893–898
Skatrud J, Iber C, Ewart R, Thomas G, Rasmussen H, Schultze B (1981) Disordered breathing during sleep in hypothyroidism. Am Rev Respir Dis 124:325–329
Winkelman JW, Goldman H, Piscatelli N, Lukas SE, Dorsey CM, Cunningham S (1996) Are thyroid function tests necessary in patients with suspected sleep apnea? Sleep 19(10):790–793
Young T, Palta M, Dempsey J, Skatrud J, Weber S, Badr S (1993) The occurrence of sleep-disordered breathing among middle-aged adults. N Engl J Med 328:1230–1235
Zgliczynska-Widlak J (1998) Chapter 8: Hypothyroidism. In: Zgliczynski S (ed) Thyroid diseases. Elsevier Urban and Partner, Warsaw, pp 126–136 (Textbook in Polish)
Conflicts of Interest
The authors declare no conflicts of interest in relation to this article.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2015 Springer International Publishing Switzerland
About this chapter
Cite this chapter
Bielicki, P., Przybyłowski, T., Kumor, M., Barnaś, M., Wiercioch, M., Chazan, R. (2015). Thyroid Hormone Levels and TSH Activity in Patients with Obstructive Sleep Apnea Syndrome. In: Pokorski, M. (eds) Advances in Clinical Science. Advances in Experimental Medicine and Biology(), vol 878. Springer, Cham. https://doi.org/10.1007/5584_2015_180
Download citation
DOI: https://doi.org/10.1007/5584_2015_180
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-319-21496-2
Online ISBN: 978-3-319-21497-9
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)