Abstract
Multi-slice CT and Cone Beam CT are actually both used to image the temporal bone. Two completely different MR protocols are used to respectively image the inner ear and middle ear.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
These keywords were added by machine and not by the authors. This process is experimental and the keywords may be updated as the learning algorithm improves.
1 CT Techniques for Temporal Bone Imaging
Multi-slice CT (MSCT) has been used for many years to image the temporal bone. However, the last couple of years Cone Beam CT (CBCT) is taking over that role.
1.1 CBCT of the Temporal Bone
CBCT uses a rotating gantry on which an X-ray tube and detector is attached. A cone-shaped X-ray beam is directed through the middle of the temporal bone onto a two-dimensional X-ray detector. Because CBCT uses the entire FOV of the two-dimensional X-ray detector, only a single 360° gantry rotation is necessary to acquire a 3D-volumetric data set. Of this data reconstructions can be made in any desired plane.
The advantages of CBCT over MSCT are the shorter examination time, high spatial resolution, and low radiation dose. It is also less sensitive for metallic and beam hardening artifacts because image acquisition is based on conventional radiographic images. The most important disadvantage of CBCT is its high sensitivity for motion artifacts because the patient has to hold the head perfectly still during the acquisition time of approximately 40 s.
Many manufacturers construct cone beam scanners, and their parameters will differ. In some scanners the patients are in a sitting position. We chose a scanner with supine patient position. Fixation of the patient’s head is done to prevent motion artifacts. We use the following parameters (only suggestive because scanner specific):
-
110 kV
-
±140 mAs
-
Field of view 15 × 5 cm High Resolution
-
Slice thickness 0.15 mm
-
Scan time 40 s
Reconstructions in the axial and coronal planes are made of the axial raw data images with a slice thickness of respectively 0.3 and 1 mm using special software.
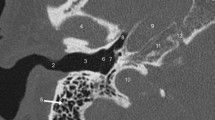
The technicians are instructed to make this reconstruction in a plane parallel to the lateral semicircular canal. This is the axial imaging set. The coronal imaging set is reconstructed exactly perpendicular to this axial set of images. On the most cranial axial image the superior semicircular canal is shown. The most anterior coronal image is made just anterior to the geniculate ganglion of the facial nerve. This procedure is repeated for both the right and left temporal bones separately, and images are viewed using a window width of 3050 HU and a window level of 525 HU. These parameters for windowing only have an indicative value, as each radiologist has to make his/her own choice. Systematic visualization of both stapes crura and of the suspensory ligaments in the middle ear cavity can be a helpful indicator when choosing the windowing parameters.
1.2 MSCT of the Temporal Bone
The images are acquired in a single imaging plane using a multi-slice detector scanner. The patient is lying on his/her back and the gantry of the scanner is not tilted. We use the following imaging parameters (only indicative because scanner and user-specific):
-
120 kV
-
250 mAs
-
Collimation 0.5 mm or 0.625 mm
-
Scan time 1.0 s
Postprocessing is done in a similar way as data acquired with CBCT. After acquiring the raw dataset images are reconstructed with a slice thickness of 1 mm and by using an ultra high resolution reconstruction mode. The technicians are instructed to make this reconstruction in a plane parallel to the lateral semicircular canal. This is the axial imaging set. The coronal imaging set is reconstructed exactly perpendicular to this axial set of images. On the most cranial axial image the superior semicircular canal is shown. The most anterior coronal image is made just anterior to the geniculate ganglion of the facial nerve. This procedure is repeated for both the right and left temporal bones separately, and the images are viewed using a window width of 4000 HU and a window level of 200 HU. These parameters for windowing only have an indicative value, as each radiologist has to make his/her own choice. Systematic visualization of both stapes crura and of the suspensory ligaments in the middle ear cavity can be a helpful indicator when choosing the windowing parameters.
2 MR Techniques for Temporal Bone Imaging
Since many years MR is used for inner ear imaging. During the last years, an increasing role is reserved for MR in the detection of cholesteatoma.
2.1 Imaging of the Cerebellopontine Angle and Inner Ear
A lot of discussion exists on which MR imaging protocol should be used for the temporal bone. Controversy exists on which sequences should be used, what the exact slice thickness of the images should be and even the eventual use of contrast agents. The following imaging protocol can be considered as an example of how a good protocol can look like, but each radiologist can tailor them according to personal experiences or according to different indications. The following sequences are standard in our department:
-
1.
5 mm thick axial TSE T2-weighted images of the brain, brain stem, and posterior fossa, performed to study the brain for cerebral anomalies causing hearing loss, tinnitus, vertigo, … (e.g., cerebral arteriovenous malformations, brain stem ischemia, …)
-
2.
1–3 mm thick axial SE T1-weighted images of the temporal bone
-
3.
0.4–0.7 mm thick axial high resolution T2-weighted images of the inner ear structures
-
4.
1–3 mm thick axial SE T1-weighted images of the temporal bone after intravenous injection of gadolinium
-
5.
1–3 mm thick coronal SE T1-weighted images of the temporal bone after intravenous injection of gadolinium
The following changes are currently made:
-
Performing T1-weighted images in 3D technique with the use of thin slices (e.g., 1 mm). This is especially interesting to study the relationship between small tumors and the cranial nerves in the internal auditory meatus
-
Performing reconstructions of the 3D TSE T2-weighted sequence in other planes than the axial one. This is most often done to study the relationship between different small structures in the cerebellopontine angel and internal auditory meatus, such as cranial nerves, vessels, and small tumors
-
Performing additional MR angiographic sequences, especially interesting if vascular lesions are detected
-
Performing specific sequences for detection of endolymphatic hydrops (see chapter on inner ear pathology)
2.2 Cholesteatoma Imaging
Since the introduction of MR for cholesteatoma imaging, two completely different techniques have been introduced, the one basically using diffusion-weighted images (DW), the other performing T1-weighted images before and after intravenous injection of gadolinium. Non-echoplanar (non-EP) DW proved to be better than echoplanar DW images.
Following scan protocol can be used for cholesteatoma imaging:
-
1.
2 mm thick coronal b0 and b800 or b1000 non-EP DW images with ADC map
-
2.
2 mm thick axial TSE T2-weighted images
-
3.
2 mm thick coronal T2-weighted images
If complications (such as middle cranial fossa invasion, facial nerve paralysis, or membranous labyrinth invasion) are suspected, following protocol is performed 45 min after intravenous injection of gadolinium:
-
1.
2 mm thick coronal b0 and b800 or b1000 non-EP DW images with ADC map
-
2.
0.4–0.7 mm thick axial high resolution T2-weighted images
-
3.
2 mm thick coronal TSE T2-weighted images
-
4.
2 mm thick coronal SE T1-weighted images
-
5.
2 mm thick axial SE T1-weighted images
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2014 Springer-Verlag Berlin Heidelberg
About this chapter
Cite this chapter
Lemmerling, M., De Foer, B., Smet, B. (2014). Temporal Bone Imaging Techniques. In: Lemmerling, M., De Foer, B. (eds) Temporal Bone Imaging. Medical Radiology(). Springer, Berlin, Heidelberg. https://doi.org/10.1007/174_2014_1026
Download citation
DOI: https://doi.org/10.1007/174_2014_1026
Published:
Publisher Name: Springer, Berlin, Heidelberg
Print ISBN: 978-3-642-17895-5
Online ISBN: 978-3-642-17896-2
eBook Packages: MedicineMedicine (R0)