Abstract
Increasing knowledge about the role of calcitonin gene-related peptide (CGRP) in migraine pathophysiology has led to the development of antibodies against this peptide or its receptor. However, CGRP is widely expressed throughout the body, participating not only in pathophysiological conditions but also in several physiological processes and homeostatic responses during pathophysiological events. Therefore, in this chapter, the risks of long-term blockade of the CGRP pathway will be discussed, with focus on the cardiovascular system, as this peptide has been described to have a protective role during ischemic events, and migraine patients present a higher risk of stroke and myocardial infarction.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Migraine is a highly disabling neurovascular disorder (Stovner et al. 2018). As mentioned in the previous chapters, calcitonin gene-related peptide (CGRP) has been described to play an important role in migraine pathophysiology (Edvinsson 2017; Goadsby et al. 2002). As a result, the CGRP pathway has become a promising target.
Initially, CGRP receptor antagonists (gepants) were developed for the acute treatment of migraine and proved to be effective (Doods et al. 2000; Edvinsson and Linde 2010). Unfortunately, pharmacokinetic limitations and hepatotoxicity cases did not allow the initial gepants to reach the market (Negro et al. 2012). New gepants are currently in Phase II trials for the acute and prophylactic treatment of migraine, with no hepatotoxicity reported (Holland and Goadsby 2018; Tepper 2018); nevertheless, the concerns about the hepatotoxicity reports led to the development of CGRP (receptor) antibodies for the prophylactic treatment of migraine (Deen et al. 2017; Schuster et al. 2015; Wrobel Goldberg and Silberstein 2015). Preliminary results of the clinical trials are promising and have not reported serious side effects (Mitsikostas and Reuter 2017); however, it is important to consider the physiological role of this peptide and the possible side effects after long-term blockade of the CGRP pathway.
In this chapter, the role of CGRP in physiological processes will be described, with focus on the cardiovascular system, as migraine patients present a higher risk of stroke and myocardial infarction (Etminan et al. 2005; Kurth et al. 2009; Sacco et al. 2013; Scher et al. 2005).
2 CGRP and the Cardiovascular System
CGRP and its fibers are widely distributed in peripheral and central structures. In the cardiovascular system, sensory CGRPergic fibers have been described to innervate the blood vessels and the heart (Opgaard et al. 1995; Uddman et al. 1986; Wimalawansa and MacIntyre 1988). Several studies have shown that CGRP plays an important role in the regulation of blood pressure and in the homeostatic responses during ischemic events and hypertension (HT) (Edvinsson et al. 1998; Keith et al. 2000; Lindstedt et al. 2006; MaassenVanDenBrink et al. 2016; McCulloch et al. 1986; Russell et al. 2014).
2.1 CGRP and Hypertension
As mentioned above, CGRP has been demonstrated to be involved in the regulation of blood pressure. Although its role under physiological conditions may be limited (Smillie and Brain 2011), it seems to act as a protective/compensatory mechanism during HT (Smillie et al. 2014). In accordance with this hypothesis, in the deoxycorticosterone-salt HT model, CGRP knockout mice had a significant increase in 24-h mean arterial pressure (MAP) and renal damage when compared to wild types (Jianping et al. 2013), while in non-treated animals, only the 7-day average of the daytime MAP was significantly increased (Mai et al. 2014). Moreover, in a model of angiotensin II-induced HT, CGRP knockout mice exhibited an enhanced increase in MAP and aortic hypertrophy. This was accompanied by an upregulation of the CGRP receptor components expression, reinforcing the role of CGRP release as a safeguard mechanism against the onset and maintenance of HT (Smillie et al. 2014). This increase in blood pressure has been associated to an elevated sympathetic activation, as CGRP knockout mice show an increase in urine and plasma markers of catecholamine release (Mai et al. 2014). Indeed, bolus injections of the CGRP antagonist olcegepant enhance the vasopressor sympathetic outflow in pithed rats (Avilés-Rosas et al. 2017). Moreover, CGRP is not only involved in peripheral mechanisms, but it also participates in the maintenance of cerebrovascular reactivity during chronic HT (Wang et al. 2015).
The abovementioned studies support the role of CGRP in blood pressure regulation during HT. As a result, a novel CGRP analogue was recently developed to improve and reverse cardiovascular disease. Results from in vivo preclinical models of hypertension and cardiac failure showed positive antihypertensive effects, an attenuation of cardiac remodeling, and an increase in angiogenesis and cell survival after administration of the CGRP analogue (Aubdool et al. 2017).
2.2 CGRP and Ischemia
During severe HT and focal cerebral ischemia, CGRP has been demonstrated to act as a neuroprotector, by increasing cerebral blood flow (Moskowitz et al. 1989; Sakas et al. 1989; Zhang et al. 2011). In rats, if CGRP is administrated at the beginning of reperfusion after experimental cerebral artery occlusion, a reduction in brain edema is observed, probably due to a decrease in the blood-brain barrier disruption (Liu et al. 2011). In patients with subarachnoid hemorrhage (SAH), higher levels of plasma CGRP have been associated with delayed vasospasm (Juul et al. 1990) and infusion of CGRP further reduced vasospasm (Juul et al. 1994). Similarly, in another cohort of patients with SAH, CGRP levels in cerebrospinal fluid of patients without vasospasm were significantly higher than the levels of patients with vasospasm, with the former group not developing cerebral ischemia (Schebesch et al. 2013). In an experimental rat model of SAH, CGRP expression was decreased; however, an enhanced CGRP-dependent vasodilation was observed (Edvinsson et al. 1990). Finally, vasospasm after induction of SAH by placing a clot around the internal carotid artery bifurcation was significantly ameliorated in monkeys that were treated with slow-release CGRP tablets, consisting of compressed microspheres containing CGRP, and that were placed in the cerebrospinal fluid (Inoue et al. 1996). Due to their composition, these compressed microsphere tablets released CGRP for a period of several weeks, providing proof-of-concept data suggesting CGRP agonism as a possible therapeutic target for SAH patients.
In myocardial ischemia, CGRP is also considered to be released as a protective mechanism. Preclinical studies in rats and mice show protective hemodynamic and metabolic changes mediated by CGRP in response to ischemic events (Chai et al. 2006; Gao et al. 2015; Homma et al. 2014; Lei et al. 2016). Moreover, in clinical studies, intravenous administration of CGRP resulted in a decrease of both systolic and diastolic arterial pressure and an increase of heart rate (Gennari and Fischer 1985). Furthermore, when infused in patients with congestive heart failure, myocardial contractility is improved (Gennari et al. 1990). Interestingly, lower plasma levels of CGRP have been reported in patients with diabetes mellitus and coronary artery disease, when compared to controls, suggesting an alteration in the CGRP (cardioprotective) pathway (Wang et al. 2012). Obviously, these observations need to be confirmed in future, and it should be elucidated whether potential changes in patients with cardiovascular disease reflect a cause or consequence of this disease.
2.3 CGRP and Preeclampsia
CGRP also seems to be involved in the vascular adaptations during pregnancy, as plasma levels increase through the gestation period, reaching their maximum during the last trimester and normalizing after delivery. However, in preeclampsia, a pregnancy disorder characterized by high blood pressure and proteinuria, CGRP levels are lower (Yadav et al. 2014). The mechanisms behind this are not yet known but indicate an alteration in the CGRP signaling, similar as observed in patients with cardiovascular disease.
3 Cardiovascular Risk and Migraine
Numerous studies have shown that migraine patients present an increased risk of hemorrhagic and ischemic stroke, with the risk being higher for women (Chang et al. 1999; Etminan et al. 2005; Sacco et al. 2013; Schurks et al. 2009; Spector et al. 2010; Tzourio et al. 1995). Moreover, a higher risk of myocardial infarction, coronary artery disease, and altered arterial function has also been described (Scher et al. 2005; Vanmolkot et al. 2007). Unfortunately, the mechanisms behind these increases are not clear, but it is thought to involve genetic aspects and vascular dysfunction, among other factors. This poses a concern, as currently the main novel therapeutic target for migraine treatment is blocking CGRP or its receptor, which could increase cardiovascular risk (Deen et al. 2017; MaassenVanDenBrink et al. 2016).
3.1 Cardiovascular Risk, Migraine, and Women
Migraine is almost three times more prevalent in women than in men (Buse et al. 2013). Frequency, intensity of headaches, disability, and chronification have also been reported to be higher in female patients (Buse et al. 2013; Labastida-Ramirez et al. 2017). In addition, women with migraine present a higher risk of stroke when compared to men with migraine, and, as before menopause the prevalence of cardiovascular events is rather low, after menopause the occurrence rises sharply (Bushnell et al. 2014; Mieres et al. 2014).
In myocardial infarction, sex-related differences have also been observed. Women usually present angina-like chest pain and a positive response to stress testing but no visible obstructions during angiography as it is caused by vasospasms of the small intramyocardial portions of the coronary arteries (Humphries et al. 2008; Kaski et al. 1995). On the contrary, men usually present with occlusions of the proximal conducting portion, which are evident during an angiography (Fig. 1). This disparity may represent a downside for female migraine patients undergoing treatment with CGRP (receptor) blockade, as CGRP-dependent vasodilation (and cardioprotection) in coronary arteries is more pronounced in the distal portions than in the proximal portions (Chan et al. 2010; Gulbenkian et al. 1993; MaassenVanDenBrink et al. 2016). Moreover, CGRP signaling seems to be modulated by ovarian steroid hormones, as women have higher plasma levels than men, and the levels increase when patients are under contraceptives (Valdemarsson et al. 1990). Furthermore, the decrease in blood pressure and the positive inotropic effect induced by CGRP administration have been described to be enhanced when 17β-estradiol or progesterone is co-administered (Al-Rubaiee et al. 2013; Gangula et al. 2002). This evidence, taken together, strongly suggests a (protective) synergistic interaction between ovarian steroid hormones and CGRP and reiterates the concerns about CGRP (receptor) blockade in women, as this could increase their risk of suffering an ischemic event even more, especially after menopause.
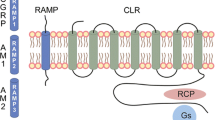
Theoretical concerns after long-term blockade of CGRP (receptor). Migraine patients present an increased risk of cardiovascular disease, and CGRP participates as a safeguard during ischemic events which suggest that after CGRP blockade, the (cardio)vascular risk could increase further. In myocardial ischemia, CGRP seems to have a more prominent role in the distal portion than in the proximal portion of the coronary arteries, which may represent a downside for women, as ischemic events in the distal portion are more common in female patients, while proximal obstructions are more prevalent in male patients
4 Safety Assessment of CGRP Blockade
Considering the increased cardiovascular risk of migraine patients discussed in the previous section, it is important to perform studies that correctly assess the safety of CGRP (receptor) blockade. For such a purpose, cardiovascularly compromised subjects should be included that properly represent the population of migraine patients potentially using these drugs.
Unfortunately, even though the grand majority of the CGRP (receptor) antibodies have been approved, currently only one group has evaluated their cardiovascular safety profile in cardiovascularly compromised patients (Depre et al. 2018). In this study, a randomized, double-blind, placebo-controlled trial was performed to evaluate the effect of erenumab, a fully human monoclonal antibody directed against the CGRP receptor, on exercise time during a treadmill test in patients with stable angina pectoris. The authors reported no alterations in performance between patients receiving erenumab and placebo. Apart from serious pharmacological concerns about the validity of this specific study, because no evidence was presented on whether effective CGRP receptor blockade was achieved at the time of the treadmill test (Maassen van den Brink et al. 2018), the study population needs further attention.
In the study from Depre et al., the patients included suffered from stable angina pectoris, most likely due to stenosis of the epicardial conducting portions of the coronary artery. As discussed previously, the role of CGRP is limited in the proximal coronary artery (Chan et al. 2010). Whereas most patients using the antibodies will be female, this study included 78% males, as stable angina related to epicardial stenosis is mainly present in male patients. Thus, women, who pose a major concern and may suffer from microvascular disease, where CGRP may be a relevant mediator, were underrepresented in this study.
While in some cases performing appropriate studies in relevant patient groups may be ethically and practically challenging, preclinical studies are excellent to shed more light on the role of CGRP in cardiovascular regulation. In this light, it is important also to take into account potential differences between short-term and long-term blockade of CGRP or its receptor in models of cardiovascular disease in both male and female animals.
5 Conclusion
CGRP plays an important role in (cardio)vascular protection. However, it is also involved in migraine pathophysiology, and the current novel treatments involve CGRP (receptor) blockade. As migraine patients present higher cardiovascular risk, with women at higher risk, chronic blockade of the CGRP pathway poses a concern. While the initial clinical trials don’t indicate frequent adverse events, it is of crucial importance to correctly evaluate the safety profile of these novel drugs, in order to prevent serious adverse effects when these drugs will be used on a large scale.
References
Al-Rubaiee M, Gangula PR, Millis RM, Walker RK, Umoh NA, Cousins VM, Jeffress MA, Haddad GE (2013) Inotropic and lusitropic effects of calcitonin gene-related peptide in the heart. Am J Physiol Heart Circ Physiol 304:H1525–H1537
Aubdool AA, Thakore P, Argunhan F, Smillie SJ, Schnelle M, Srivastava S, Alawi KM, Wilde E, Mitchell J, Farrell-Dillon K, Richards DA, Maltese G, Siow RC, Nandi M, Clark JE, Shah AM, Sams A, Brain SD (2017) A novel alphacalcitonin gene-related peptide analogue protects against end-organ damage in experimental hypertension, cardiac hypertrophy, and heart failure. Circulation 136:367–383
Avilés-Rosas VH, Rivera-Mancilla E, Marichal-Cancino BA, Manrique-Maldonado G, Altamirano-Espinoza AH, Maassen Van Den Brink A, Villalón CM (2017) Olcegepant blocks neurogenic and non-neurogenic CGRPergic vasodepressor responses and facilitates noradrenergic vasopressor responses in pithed rats. Br J Pharmacol 174:2001–2014
Buse DC, Loder EW, Gorman JA, Stewart WF, Reed ML, Fanning KM, Serrano D, Lipton RB (2013) Sex differences in the prevalence, symptoms, and associated features of migraine, probable migraine and other severe headache: results of the American Migraine Prevalence and Prevention (AMPP) Study. Headache 53:1278–1299
Bushnell C, McCullough LD, Awad IA, Chireau MV, Fedder WN, Furie KL, Howard VJ, Lichtman JH, Lisabeth LD, Piña IL, Reeves MJ, Rexrode KM, Saposnik G, Singh V, Towfighi A, Vaccarino V, Walters MR (2014) Guidelines for the prevention of stroke in women. Stroke 45:1545–1588
Chai W, Mehrotra S, Jan Danser AH, Schoemaker RG (2006) The role of calcitonin gene-related peptide (CGRP) in ischemic preconditioning in isolated rat hearts. Eur J Pharmacol 531:246–253
Chan KY, Edvinsson L, Eftekhari S, Kimblad PO, Kane SA, Lynch J, Hargreaves RJ, de Vries R, Garrelds IM, van den Bogaerdt AJ, Danser AH, Maassenvandenbrink A (2010) Characterization of the calcitonin gene-related peptide receptor antagonist telcagepant (MK-0974) in human isolated coronary arteries. J Pharmacol Exp Ther 334:746–752
Chang CL, Donaghy M, Poulter N (1999) Migraine and stroke in young women: case-control study. Br Med J 318:13–18
Deen M, Correnti E, Kamm K, Kelderman T, Papetti L, Rubio-Beltran E, Vigneri S, Edvinsson L, Maassen Van Den Brink A, European Headache Federation School of Advanced Studies (2017) Blocking CGRP in migraine patients – a review of pros and cons. J Headache Pain 18:96
Depre C, Antalik L, Starling A, Koren M, Eisele O, Lenz RA, Mikol DD (2018) A randomized, double-blind, placebo-controlled study to evaluate the effect of erenumab on exercise time during a treadmill test in patients with stable angina. Headache 58:715–723
Doods H, Hallermayer G, Wu D, Entzeroth M, Rudolf K, Engel W, Eberlein W (2000) Pharmacological profile of BIBN4096BS, the first selective small molecule CGRP antagonist. Br J Pharmacol 129:420–423
Edvinsson L (2017) The trigeminovascular pathway: role of CGRP and CGRP receptors in migraine. Headache 57(Suppl 2):47–55
Edvinsson L, Linde M (2010) New drugs in migraine treatment and prophylaxis: telcagepant and topiramate. Lancet 376:645–655
Edvinsson L, Delgado-Zygmunt T, Ekman R, Jansen I, Svendgaard NA, Uddman R (1990) Involvement of perivascular sensory fibers in the pathophysiology of cerebral vasospasm following subarachnoid hemorrhage. J Cereb Blood Flow Metab 10:602–607
Edvinsson L, Mulder H, Goadsby PJ, Uddman R (1998) Calcitonin gene-related peptide and nitric oxide in the trigeminal ganglion: cerebral vasodilatation from trigeminal nerve stimulation involves mainly calcitonin gene-related peptide. J Auton Nerv Syst 70:15–22
Etminan M, Takkouche B, Isorna FC, Samii A (2005) Risk of ischaemic stroke in people with migraine: systematic review and meta-analysis of observational studies. Br Med J 330:63
Gangula PRR, Wimalawansa SJ, Yallampalli C (2002) Sex steroid hormones enhance hypotensive effects of calcitonin gene-related peptide in aged female rats. Biol Reprod 67:1881–1887
Gao Y, Song J, Chen H, Cao C, Lee C (2015) TRPV1 activation is involved in the cardioprotection of remote limb ischemic postconditioning in ischemia-reperfusion injury rats. Biochem Biophys Res Commun 463:1034–1039
Gennari C, Fischer JA (1985) Cardiovascular action of calcitonin gene-related peptide in humans. Calcif Tissue Int 37:581–584
Gennari C, Nami R, Agnusdei D, Fischer JA (1990) Improved cardiac performance with human calcitonin gene related peptide in patients with congestive heart failure. Cardiovasc Res 24:239–241
Goadsby PJ, Lipton RB, Ferrari MD (2002) Migraine – current understanding and treatment. N Engl J Med 346:257–270
Gulbenkian S, Opgaard OS, Ekman R, Andrade NC, Wharton J, Polak JM, Queiroz e Melo J, Edvinsson L (1993) Peptidergic innervation of human epicardial coronary arteries. Circ Res 73:579–588
Holland PR, Goadsby PJ (2018) Targeted CGRP small molecule antagonists for acute migraine therapy. Neurotherapeutics 15:304–312
Homma S, Kimura T, Sakai S, Yanagi K-I, Miyauchi Y, Aonuma K, Miyauchi T (2014) Calcitonin gene-related peptide protects the myocardium from ischemia induced by endothelin-1: intravital microscopic observation and 31P-MR spectroscopic studies. Life Sci 118:248–254
Humphries KH, Pu A, Gao M, Carere RG, Pilote L (2008) Angina with “normal” coronary arteries: sex differences in outcomes. Am Heart J 155:375–381
Inoue T, Shimizu H, Kaminuma T, Tajima M, Watabe K, Yoshimoto T (1996) Prevention of cerebral vasospasm by calcitonin gene-related peptide slow-release tablet after subarachnoid hemorrhage in monkeys. Neurosurgery 39:984–990
Jianping L, Kevin AC, Donald JD, Scott CS (2013) Renal protective effects of α-calcitonin gene-related peptide in deoxycorticosterone-salt hypertension. Am J Physiol Renal Physiol 304:F1000–F1008
Juul R, Edvinsson L, Gisvold SE, Ekman R, Brubakk AO, Fredriksen TA (1990) Calcitonin gene-related peptide-LI in subarachnoid haemorrhage in man. Signs of activation of the trigemino-cerebrovascular system? Br J Neurosurg 4:171–179
Juul R, Aakhus S, Björnstad K, Gisvold SE, Brubakk AO, Edvinsson L (1994) Calcitonin gene-related peptide (human α-CGRP) counteracts vasoconstriction in human subarachnoid haemorrhage. Neurosci Lett 170:67–70
Kaski JC, Collins P, Nihoyannopoulos P, Maseri A, Poole-Wilson PA, Rosano GMC (1995) Cardiac syndrome X: clinical characteristics and left ventricular function: long-term follow-up study. J Am Coll Cardiol 25:807–814
Keith IM, Tjen-A-Looi S, Kraiczi H, Ekman R (2000) Three-week neonatal hypoxia reduces blood CGRP and causes persistent pulmonary hypertension in rats. Am J Physiol Heart Circ Physiol 279:H1571–H1578
Kurth T, Schürks M, Logroscino G, Buring JE (2009) Migraine frequency and risk of cardiovascular disease in women. Neurology 73:581–588
Labastida-Ramirez A, Rubio-Beltran E, Villalon CM, MaassenVanDenBrink A (2017) Gender aspects of CGRP in migraine. Cephalalgia 333102417739584
Lei J, Zhu F, Zhang Y, Duan L, Lei H, Huang W (2016) Transient receptor potential vanilloid subtype 1 inhibits inflammation and apoptosis via the release of calcitonin gene-related peptide in the heart after myocardial infarction. Cardiology 134:436–443
Lindstedt IH, Edvinsson ML, Evinsson L (2006) Reduced responsiveness of cutaneous microcirculation in essential hypertension – a pilot study. Blood Press 15:275–280
Liu Z, Liu Q, Cai H, Xu C, Liu G, Li Z (2011) Calcitonin gene-related peptide prevents blood–brain barrier injury and brain edema induced by focal cerebral ischemia reperfusion. Regul Pept 171:19–25
Maassen van den Brink A, Rubio-Beltrán E, Duncker D, Villalón CM (2018) Is CGRP receptor blockade cardiovascularly safe? Appropriate studies are needed. Headache 58:1257–1258
MaassenVanDenBrink A, Meijer J, Villalón CM, Ferrari MD (2016) Wiping out CGRP: potential cardiovascular risks. Trends Pharmacol Sci 37:779–788
Mai TH, Wu J, Diedrich A, Garland EM, Robertson D (2014) Calcitonin gene-related peptide (CGRP) in autonomic cardiovascular regulation and vascular structure. J Am Soc Hypertens 8:286–296
McCulloch J, Uddman R, Kingman TA, Edvinsson L (1986) Calcitonin gene-related peptide: functional role in cerebrovascular regulation. Proc Natl Acad Sci 83:5731–5735
Mieres JH, Gulati M, Merz NB, Berman DS, Gerber TC, Hayes SN, Kramer CM, Min JK, Newby LK, Nixon JV, Srichai MB, Pellikka PA, Redberg RF, Wenger NK, Shaw LJ (2014) Role of noninvasive testing in the clinical evaluation of women with suspected ischemic heart disease. Circulation 130:350–379
Mitsikostas DD, Reuter U (2017) Calcitonin gene-related peptide monoclonal antibodies for migraine prevention: comparisons across randomized controlled studies. Curr Opin Neurol 30:272–280
Moskowitz MA, Sakas DE, Wei EP, Kano M, Buzzi MG, Ogilvy C, Kontos HA (1989) Postocclusive cerebral hyperemia is markedly attenuated by chronic trigeminal ganglionectomy. Am J Physiol 257:H1736–H1739
Negro A, Lionetto L, Simmaco M, Martelletti P (2012) CGRP receptor antagonists: an expanding drug class for acute migraine? Expert Opin Investig Drugs 21:807–818
Opgaard OS, Gulbenkian S, Bergdahl A, Barroso CP, Andrade NC, Polak JM, Queiroz e Melo JQ, Edvinsson L (1995) Innervation of human epicardial coronary veins: immunohistochemistry and vasomotility. Cardiovasc Res 29:463–468
Russell FA, King R, Smillie SJ, Kodji X, Brain SD (2014) Calcitonin gene-related peptide: physiology and pathophysiology. Physiol Rev 94:1099
Sacco S, Ornello R, Ripa P, Pistoia F, Carolei A (2013) Migraine and hemorrhagic stroke: a meta-analysis. Stroke 44:3032–3038
Sakas DE, Moskowitz MA, Wei EP, Kontos HA, Kano M, Ogilvy CS (1989) Trigeminovascular fibers increase blood flow in cortical gray matter by axon reflex-like mechanisms during acute severe hypertension or seizures. Proc Natl Acad Sci 86:1401–1405
Schebesch K-M, Herbst A, Bele S, Schödel P, Brawanski A, Stoerr E-M, Lohmeier A, Kagerbauer SM, Martin J, Proescholdt M (2013) Calcitonin-gene related peptide and cerebral vasospasm. J Clin Neurosci 20:584–586
Scher AI, Terwindt GM, Picavet HSJ, Verschuren WMM, Ferrari MD, Launer LJ (2005) Cardiovascular risk factors and migraine: the GEM population-based study. Neurology 64:614–620
Schurks M, Rist PM, Bigal ME, Buring JE, Lipton RB, Kurth T (2009) Migraine and cardiovascular disease: systematic review and meta-analysis. Br Med J 339:b3914
Schuster NM, Vollbracht S, Rapoport AM (2015) Emerging treatments for the primary headache disorders. Neurol Sci 36(Suppl 1):109–113
Smillie S-J, Brain SD (2011) Calcitonin gene-related peptide (CGRP) and its role in hypertension. Neuropeptides 45:93–104
Smillie S-J, King R, Kodji X, Outzen E, Pozsgai G, Fernandes E, Marshall N, de Winter P, Heads Richard J, Dessapt-Baradez C, Gnudi L, Sams A, Shah Ajay M, Siow Richard C, Brain Susan D (2014) An ongoing role of α-calcitonin gene-related peptide as part of a protective network against hypertension, vascular hypertrophy, and oxidative stress. Hypertension 63:1056–1062
Spector JT, Kahn SR, Jones MR, Jayakumar M, Dalal D, Nazarian S (2010) Migraine headache and ischemic stroke risk: an updated meta-analysis. Am J Med 123:612–624
Stovner LJ, Nichols E, Steiner TJ, Abd-Allah F, Abdelalim A, Al-Raddadi RM, Ansha MG, Barac A, Bensenor IM, Doan LP, Edessa D, Endres M, Foreman KJ, Gankpe FG, Gopalkrishna G, Goulart AC, Gupta R, Hankey GJ, Hay SI, Hegazy MI, Hilawe EH, Kasaeian A, Kassa DH, Khalil I, Khang Y-H, Khubchandan J, Kim YJ, Kokubo Y, Mohammed MA, Moradi-Lakeh M, Nguyen HLT, Nirayo YL, Qorbani M, Ranta A, Roba KT, Safiri S, Santos IS, Satpathy M, Sawhney M, Shiferaw MS, Shiue I, Smith M, Szoeke CEI, Truong NT, Venketasubramanian N, Weldegwergs KG, Westerman R, Wijeratne T, Tran BX, Yonemoto N, Feigin VL, Vos T, Murray CJL (2018) Global, regional, and national burden of migraine and tension-type headache, 1990–2016: a systematic analysis for the Global Burden of Disease Study 2016. Lancet Neurol 17:954–976
Tepper SJ (2018) History and review of anti-calcitonin gene-related peptide (CGRP) therapies: from translational research to treatment. Headache 58(Suppl 3):238–275
Tzourio C, Tehindrazanarivelo A, Iglesias S, Alperovitch A, Chedru F, d’Anglejan-Chatillon J, Bousser M-G (1995) Case-control study of migraine and risk of ischaemic stroke in young women. Br Med J 310:830–833
Uddman R, Edvinsson L, Ekblad E, Håkanson R, Sundler F (1986) Calcitonin gene-related peptide (CGRP): perivascular distribution and vasodilatory effects. Regul Pept 15:1–23
Valdemarsson S, Edvinsson L, Hedner P, Ekman R (1990) Hormonal influence on calcitonin gene-related peptide in man: effects of sex difference and contraceptive pills. Scand J Clin Lab Invest 50:385–388
Vanmolkot FH, Van Bortel LM, de Hoon JN (2007) Altered arterial function in migraine of recent onset. Neurology 68:1563–1570
Wang LH, Zhou SX, Li RC, Zheng LR, Zhu JH, Hu SJ, Sun YL (2012) Serum levels of calcitonin gene-related peptide and substance P are decreased in patients with diabetes mellitus and coronary artery disease. J Int Med Res 40:134–140
Wang Z, Martorell BC, Wälchli T, Vogel O, Fischer J, Born W, Vogel J (2015) Calcitonin gene-related peptide (CGRP) receptors are important to maintain cerebrovascular reactivity in chronic hypertension. PLoS One 10:e0123697
Wimalawansa SJ, MacIntyre I (1988) Calcitonin gene-related peptide and its specific binding sites in the cardiovascular system of rat. Int J Cardiol 20:29–37
Wrobel Goldberg S, Silberstein SD (2015) Targeting CGRP: a new era for migraine treatment. CNS Drugs 29:443–452
Yadav S, Yadav YS, Goel MM, Singh U, Natu SM, Negi MPS (2014) Calcitonin gene- and parathyroid hormone-related peptides in normotensive and preeclamptic pregnancies: a nested case-control study. Arch Gynecol Obstet 290:897–903
Zhang J-Y, Yan G-T, Liao J, Deng Z-H, Xue H, Wang L-H, Zhang K (2011) Leptin attenuates cerebral ischemia/reperfusion injury partially by CGRP expression. Eur J Pharmacol 671:61–69
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2019 Springer Nature Switzerland AG
About this chapter
Cite this chapter
Rubio-Beltrán, E., van den Brink, A.M. (2019). Understanding CGRP and Cardiovascular Risk. In: Brain, S., Geppetti, P. (eds) Calcitonin Gene-Related Peptide (CGRP) Mechanisms. Handbook of Experimental Pharmacology, vol 255. Springer, Cham. https://doi.org/10.1007/164_2019_204
Download citation
DOI: https://doi.org/10.1007/164_2019_204
Published:
Publisher Name: Springer, Cham
Print ISBN: 978-3-030-21453-1
Online ISBN: 978-3-030-21454-8
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)