Abstract
The gut microbiome is a community of commensal microbes in the gastrointestinal tract that are ecologically, physiologically, and symbiotically associated with the host from the early days of life. Gut microbiota is analogous to endocrine glands. Microbial colonies in the gut produce certain microbial metabolites from nutrient metabolism. These gut-derived metabolites regulate the host’s health and disease by influencing immunity and physiology. Gut microbiota protects the intestinal environment from invading non-native pathogens by immune modulation and direct competition with pathogens for nutrient access. The gut microbiome is essential in regulating the immune system through interaction with its microbial surface antigens and metabolites. Gut microbiota is coevolved with host development and varies among individuals. The proportion of gut microbiota is constant during health. This constancy is affected by factors such as diet, medications, environment, and mental status regulating the host’s health. The dysbiotic microbiome is a risk signature of immune dysfunction and disorders in host physiology. The gut microbiome modulates the immune system locally and systematically; thus, its composition balances an individual’s health and disease conditions. This chapter reviewed the link between microbiome composition and its outcome on host physiology, immune system development, metabolic syndromes, and cancer outcomes.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
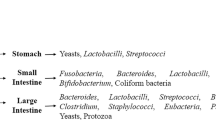
The human body harbors trillions of microbial communities in the gastrointestinal (GI) tract called gut microbiome. Joshua Lederberg explained gut microbiota as “The community of microorganisms presents in the gastrointestinal tract of the host” (Bäckhed et al. 2005; Neish 2009). The gut microbiota is considered a completely evolved and established organ in the human body analogous to hormone-secreting endocrine glands. Gut microbiota regulates multifarious physiological and metabolic pathways via its derived metabolites as substrates and maintains immunohomeostatic comprehensive cellular functions through cell signaling and biochemical cascades (Cox and Blaser 2013). Gut microbiota is recorded as an extension to the host genome by 150 times more than the human genome. It is estimated to contain 3.3 million microbial genes that code for certain essential enzymes not included in the set of native human proteomes. The enzymes coded by genes in the microbiome catalyze several biochemical processes in nutrient absorption and metabolism (Rodríguez et al. 2015; Bäckhed et al. 2005). Recent studies from researchers relevant to metagenomics, molecular biology, and microbiology delineated the human body as a mutualistic superorganism of eukaryotic and prokaryotic microbial communities (Szablewski 2018). Hosts provide nutrition and shelter to the microbes in the gut; in turn, gut microbiota establishes its mutualistic and symbiotic nature by providing the host with better immunity and physiometabolic health. Trillions of microbes from hundreds of species constitute healthy microflora in the host gut. Of all the microbial communities, members of Bacteroidetes, Firmicutes, Actinobacteria, and Proteobacteria classes are the major contributors to gut microbiome composition (Senghor et al. 2018).
Balance among the proportion of gut microbiota and these members directs the fate of host health. Microbial colonization in the GI tract began before birth. Reports from the placental microbiome characterization showed similarities with the oral microbiome of healthy adults (Aagaard et al. 2014). In neonates, lactating has a defensive effect, deliberated by an intricate combination of lysozymes, sIgA, α-lactalbumin, free oligosaccharides, complex lipids, and other glycoconjugates (Gordon et al. 2012). Oligosaccharides such as fructans are prebiotic factors that help the growth of beneficial bacteria such as Bifidobacterium and Lactobacillus. Understanding the gut microbiome unravels microbial-mediated immune and metabolic regulation mechanisms in the host body. Studying the entire microbial communities in the host GI tract was a challenge to researchers and scientists during the initial days when gut microbiota composition was analyzed based on culture methods. These methods are inadequate to examine the total profile of the gut microbiome; as a result, only 10–50% of the intestinal microbes were probably cultured. In recent years, understanding of gut microbiota increased with advanced sequencing technologies adapting next-generation sequencing approaches, metagenomics, and advancements in bioinformatics tools to handle and analyze the downstream data from sequencers ensured in estimating several classes of microbes and their phylogenetic relationships. The qualitative analysis of gut microbiota is mostly delineated using techniques like DNA fingerprinting, terminal RFLP, 16 s ribosomal RNA amplicon sequencing, microarray technique, and whole genome sequencing, which provided enormous data about the total microbial population. High-throughput sequencing technologies like Roche/454, GS20, Illumina’s Genome Analyzer IIx, Affymetrix microarray technique, and Qiagen’s Gene Read are tremendously eminent.
Moreover, advanced bioinformatics tools have assisted in understanding and illustrating the downstream analysis of sequence data. The gut microbiota is highly reactive and adaptive to dietary alterations, medication choice, genetic factors, and the host’s lifestyle. After weaning to solid foods, exorbitant modifications appear in the composition of their gut microbiota. Changes in the microbiota (Dysbiosis) could lead to numerous health disorders such as obesity, nonalcoholic fatty liver disease (NAFLD), diabetes, inflammatory bowel disease, ulcerative colitis, colorectal cancer, coronary heart disease, autoimmune diseases, and neurological disorders. The gut microbiome has become a major tool and a potential clinically important marker for diagnosing and treating many diseases in the body. Modulating or redirecting the gut microbiota to its native state (eubiosis) is an ideal and promising strategy for simulating host immunity. Reconstituting the gut microbial communities benefits the host with better health and immunity. Engineering gut environment with probiotic supplements, prebiotics, and functional foods effectively shapes host immunity. The importance of gut microbiota in immune system development and modulation, along with its fate in disease and health conditions, are discussed clearly in this chapter addressing the recent findings and outbreaks in gut microbiome research in correlation with host immunity and health.
2 Intestinal Microbiota and Host Immunity
The gut microbiota considerably regulates innate and adaptive immune system functions and development. The host’s immune system has two protective mechanisms: innate immunity, specified as an immediate and nonspecific response against the pathogen. And another one is adaptive immunity which ensures both memory and specificity. In the innate immune response, secretory IgA (sIgA) plays a significant role and is a protective mechanism against infectious agents. The production of sIgA over various mucosal surfaces is through the entry of antigens and their subsequent capture through Peyer’s patches, M cells, stimulation of T cells, dendritic cells (DCs), and changes in B cells to mesenteric lymph nodes (MLNs) recombination and lymphoid tissue connected to the gut. The group of cytokines such as IL-4, IL-5, IL-10 and including TGF-β increases the production of IgA. The sIgA binds to commensal bacteria and contributes to the gut barrier function and intestinal mucosal homeostasis (Chairatana and Nolan 2017).
The innate immune cells like DCs, natural killer (NK) cells, and macrophages express pattern recognition receptors (PRRs) that recognize specific molecular patterns on the bacterial surface, which are key mediators for communication between gut microbiota and the host (Pahari et al. 2018, 2019; Negi et al. 2019). These PRRs recognize pathogen- or microbe-associated molecular patterns (PAMPs or MAMPs) on the bacterial surface. PRRs majorly contain families of nucleotide-binding oligomerization domain (NOD)-like receptors (NLRs), toll-like receptors (TLRs), RIG-I-like receptors (RLRs), and C-type lectin receptors (CLRs) (Kumar et al. 2011). Identifying microbiota through PRRs promotes memory response on primary exposure (Mills 2011; Kleinnijenhuis et al. 2012). The TLRs exist on DCs, macrophages, intestinal epithelial cells (ECs), neutrophils, and other innate immune cells. The microbial products and metabolites alter the host immune system by stimulating different types of cells like intestinal epithelial cells (IECs), mononuclear phagocytes, innate lymphoid cells (ILCs), B cells, and T cells (Kabat et al. 2014).
The GI tract protects the host from habitat and interceding nutrient consumption. The IECs on the intestinal surface form a physical barrier that detaches the lumen from the lamina propria of commensal and intestinal microbes. Although IECs are not typical innate immune cells, these are essential in mucosal immunity. Despite this, IECs are armed with innate immune system receptors that could provide gut equilibrium by recognizing bacteria (Pott and Hornef 2012). ILCs are infrequent innate lymphocytes when correlated with adaptive lymphocytes, yet these are copious on the surface barrier of mucosal-connected tissues (Sonnenberg and Artis 2012). Several research studies demonstrated that specific microbiota metabolites could control ILCs (Lee et al. 2012) expressing IL-22 cytokine. The inadequacy of IL-22 is connected with various inflammations and metabolic diseases. IL-22 also elevates the antimicrobial peptides production (RegIIIγ and RegIIIβ) to reduce the SFB colonization, stimulate the surface proteins fucosylation to intensify the beneficial bacteria colonization, and increase the goblet cells proliferation for secretion of mucin (Goto et al. 2014). Based on T domain structures, the T cells can be further segregated into γδ T and αβ T cells. αβ TCR cells expressed by T cells are initially liable for antigen-specific cellular immunity, and γδ T cells are not MHC—restricted also engaged in initial immune responses (Pennington et al. 2005). Despite this, in the small intestine of murine, γδ TCR chains are expressed by a higher proportion of intraepithelial lymphocytes (IELs) (van Wijk and Cheroutre 2009). These γδ IELs specifically regulate IECs’ continuous turnover and increase the growth of epithelial cells by keratinocyte secretion, an in vitro growth factor (Boismenu and Havran 1994). The γδ IELs also maintain the functions of the epithelial barrier by inhibiting pathogen reincarnation (Dalton et al. 2006). The association of innate and adaptive immune systems is involved in eliminating invasive pathogens and regulating symbiotic bacteria at mucosal sites. The antigen-presenting cells like naïve CD4+ αβ T cells (CD4+ T cells) and DCs are further characterized into Th1, Th2, and Th17 or adaptive T-regulatory cells (Tregs). All these cells exist in intestinal lamina propria. Th17 is the group of CD4+T cells that secretes numerous cytokines (IL-22, IL-17F, and IL-17A) (Rossi and Bot 2013), including notable effects upon inflammation and immune homeostasis. These cells also retain various cytokine characteristic analyses and functions. Th1 and Th2 cells have a steady secretory analysis after differentiation. Tregs are essential mediators of immune tolerance, reducing an improper, immense inflammatory reaction, and their malfunctions lead to autoimmune disorders. Of interest, in the germfree mice administered with a lustrated dose of polysaccharide or by intestinal colonization with commensal bacteria, a non-toxigenic form of B. fragilis which expresses polysaccharide A (PSA), prevents the growth of experimental colitis by PSA-induced Foxp3+-regulatory cells expressed by IL-10, through TLR2-dependent action (Round and Mazmanian 2010). In commensal microbiota, a few microbes have a higher effect on the responses of mucosal T cells. For instance, in Th17 cells of the small intestine, segmented filamentous bacteria (SFB) are effective stimulators; in germfree mice, it was observed by the lack of Th17 cells and their revival when SFB colonized in germfree mice (Ivanov et al. 2009a). In the gut, the abundant presence of retinoic acid (RA) activates lymphocyte gut-homing compounds and restricts the growth of Th17 cells (Mucida et al. 2007); still, the mechanism of regulation of Th17 gut tropism is unknown (Maynard and Weaver 2009). Therefore, intestinal lamina propria is an elemental site for the evolution of Th17, probably by the colonization of SFB and the expression of innate IL-23 in the intestinal microhabitat.
3 Gut Microbiota Metabolism
Intestinal microbiota regulates various host physiological mechanisms such as nutrient uptake, energy expenditure, and immune responses through metabolism. Gut microbiome-derived metabolites act as substrates for various cell signaling processes and host metabolic pathways and can alter the immune responses post-maturation and differentiation. Gut microbiota-derived metabolites are crucial in health and disease conditions in the host. According to recent investigations and reports, over 50% of the metabolome in stool and urine are derivatives of modulated gut microbiota. The microbiota metabolites are bioactive and intensely affect physiology and host immunity (Donia and Fischbach 2015). The following sections further discuss the role of gut microbial metabolites and their metabolic actions.
3.1 Retinoic Acid (RA) Metabolism
Retinoic acid (RA), a lipid metabolite of vitamin A, can regulate the equity among pro-inflammatory and anti-inflammatory immune reactions. RA inadequacy can run down the orchestration of gut microbiota and immune system activities. In constant conditions, RA is pivotal in maintaining intestinal immune homeostasis since it facilitates the regulatory T-cell progression by TGF-β and the formation of IgA through B cells (Mucida et al. 2007). It is perplexing that RA is also entangled in drawing out pro-inflammatory CD4+ T-cell reactions to diseases during inflammation—other vitamins like vitamin D extremely influence T-cell activation. Multifarious research analyses have associated vitamin D inadequacy with inflammatory bowel disease. The hook-up between the intestinal microbiota and vitamins is conspicuous in vitamins of B and K groups (Martens et al. 2002). The inadequacy of vitamin B12 leads to a reduced count of lymphocytes and induces NK cell functioning.
3.2 Tryptophan Metabolism
Inadequacy of innate immunity pathways results in malfunction of gut microbe. For instance, complex proteins and carbohydrates which are unable to degrade by the host can be digested by microbial colonies. Gut microbiota influences tissue-level immune development through the catabolism of tryptophan. The Lactobacillus utilizes tryptophan as a vitality source to form ligands of the aryl hydrocarbon receptors (AhR) like the metabolite indole-3-aldehyde (Nicholson et al. 2012).
3.3 Short Chain Fatty Acids (SCFAs) Metabolism
The microbiome provides mammalian enzymes to degrade dietary nondigestible carbohydrates (NDCs) adherent starch by fermentation into short-chain fatty acids (SCFAs) in the GI tract (Holscher 2017). SCFAs are known as carboxylic acids, including 1–6 aliphatic carbon tails such as acetate, propionate, and butyrate produced in a molar ratio of approximately 60:20:20, respectively (den Besten et al. 2013), and other end products consist of ethanol, succinate, formate, valerate, isobutyrate, and 2-methyl butyrate. SCFAs potentiate colonocytes, and inhabitant bacteria, decrease GI luminal pH to reduce pathogen growth, regulate anti-inflammatory and immunostimulatory properties, and endorse bile acid secretion, which aids in the digestion of dietary fats and increases mineral absorption (Schuijt et al. 2016). The SCFAs are proposed to engage certain G-protein-coupled receptors (GPR41, GPR43). GPR109a are stimulated through ionized SCFA, increasing the excretion of peptide YY, glucagon-like peptide (GLP-1), enhanced glucose usage, and reduced fatty acid metabolism (Koh et al. 2016). SCFAs are recorded to defend from diet-induced obesity, regulate gene expression, and induce anti-inflammatory reaction and apoptosis. In addition, SCFAs stimulate lipid metabolism by increasing lipogenesis and preventing fatty acid oxidation, as formerly recorded. SCFAs are crucial in colonic health, notably in protecting and differentiating epithelial cells. Some of the known well-characterized transporters and receptors of SCFAs are given in Table 3.1. SCFAs also regulate the expression of inflammatory cytokines like IL-6, IL-7, IL-8, IL-12, IL-1β, and TNF-α by colonic epithelial cells (Asarat et al. 2015), regulating blood pressure, leading to gut-barrier dysfunction. Butyrate is an energy substrate that intensely affects the healthy colonic epithelial barrier and immunomodulatory effects. The gut microbiota synthesizes vitamins (like B vitamins, k, biotin, folates, riboflavin, and cobalamin) and amino acids and carries out bile transformation. The antimicrobial compounds produced from microbiota contend for nutrients and gut lining attachment, thereby inhibiting the growth of pathogens. As a result, it promotes to the reduction of the lipopolysaccharides and peptidoglycans synthesis that is pernicious to the host (Tlaskova-Hogenova et al. 2004).
3.4 Bile Acids Metabolism
Bile acids are steroid metabolites present in bile. They are produced in the liver from cholesterol. Bile acids ensure solubility and uptake of vitamins and fats. Bile acids directly synthesized from cholesterol in the liver are primary bile acids. Primary bile acids conjugate with glycine or taurine to form secondary bile acids. Gut resident microbes deconjugate secondary BAs to primary BAs and glycine or taurine again. BAs are signaling molecules to farnesoid X receptor (FXR) and GPCR TGR5 in controlling the uptake of fats and vitamins (Tolhurst et al. 2012; Velagapudi et al. 2010).
3.5 Choline Metabolism
Choline is a cell membrane component and also a cationic essential nutrient. Choline is found in meat and eggs. It is essential in lipid metabolism. Enzymatic degradation of choline in the liver yields TMA (trimethylamine). TMA further metabolizes into trimethylamine N-oxide (TMAO) (Spencer et al. 2011). TMA and TMA are toxic metabolites. Production of these metabolites is controlled and regulated by microbes in the gut microbiome. Disturbance in the gut ecosystem is associated with a rise in the levels of these metabolites, which further leads to immune dysfunction and cardiometabolic syndrome (Prentiss et al. 1961; Dumas et al. 2006). Hence, the gut microbiota is key in regulating host health and metabolism.
4 Gut Microbiota Dysbiosis and Disease
4.1 IBD
Inflammatory bowel disease (IBD) comprises Crohn’s disease (CD). Ulcerative colitis (UC) is an incurable condition characterized by GI tract inflammation evoked by the consolidation of genetic, environmental, and microbial components typified by abdominal ache, diarrhea, and bloody feces (Wilson et al. 2016; Cosnes et al. 2011). The IBD is an exorbitant host immune system and gut flora stimulation in inherently affected patients (Wong and Ng 2013). The IL-23/Th17 deregulation is connected with numerous genetic sensitivity of single-nucleotide polymorphisms (SNPs) in individuals affected with CD and UC due to deterioration of innate and adaptive immunity reactions (Yen et al. 2006). Remarkably, dysbiosis is linked with the exaggerated reproduction of the responsive oxygen category that consecutively results in alterations of intestinal microbiota composition, mucosal penetrability, and enhanced immune provocation. By way of illustration of how particular microbes produce intestinal inflammation and stimulate the pathogenesis of IBD exists in Bloom et al. (2011). In their examination, commensal Bacteroidetes strains have been secluded in IL-10r2 and Tgfbr2-insufficient mice (Bloom et al. 2011). There is a confirmation that the growth of IBD is a symbiotic impact of genetic and acquired components that results in the modulations in activities and arrangement of intestinal microbiota (Albenberg et al. 2012). Despite this, the metagenomic analysis explained that microbial ecosystem and intestinal flora were reduced in IBD-affected individuals compared with healthy adults (Hansen et al. 2010). Frequently, 25% lesser genes were discovered in the stool samples of IBD individuals than in healthy controls (Qin et al. 2010). In addition, humans with UC and CD have decreased the fewer microbes like Firmicutes (Sheehan et al. 2015; Frank et al. 2007; Walker et al. 2011) having anti-inflammatory and pro-inflammatory properties and enhanced the phyla of Bacteroidetes, Proteobacteria in mucosa-associated flora (Sokol et al. 2006). The CD-affected cases showed a lower abundance of Faecalibacterium prausnitzii, Clostridium lavalense, Roseburia inulinivorans, Ruminococcus torques, and Blautia faecis when correlated with healthy adults (Fujimoto et al. 2013; Takahashi et al. 2016).
Further, Sokol and co-workers demonstrated that mononuclear cells of human peripheral blood activated with F. praunizii to produce IL-10 and inhibit the formation of IL-12 and IFN-γ (Sokol et al. 2008). The other CD-associated E. coli AIEC (adherent invasive E. coli), which also contains pro-inflammatory features, a mucosa-associated E. coli with dynamic adhesive-invasive abilities, was initially isolated from CD-affected adults. Increased growth of AIEC has been observed in individuals of colonic CD, about 38% with effective ileal CD compared to healthy controls (Baumgart et al. 2007; Darfeuille-Michaud et al. 2004). As a result, the growth of pathogenic microorganisms that attach to gut epithelial cells influences intestinal penetrability, modulates the gut microbial configuration, and promotes inflammatory reactions by standardizing pro-inflammatory gene expression, eventually developing in colitis. In IBD patients, there is a reduction in the formation of SCFAs due to a decrease in the number of F. praunizii. Clostridium clusters IV, XIVa, and XVIII are butyrate-producing organisms in the gut, affecting the growth and differentiation of Tregs cells and an expansion of epithelial cells (Atarashi et al. 2013). Treg cells are CD4+ T cells that help to maintain gut homeostasis.
Furthermore, in IBD cases, there is a higher abundance of Desulfovibrio, which is sulfate-producing bacteria (Loubinoux et al. 2002; Zinkevich and Beech 2000). As a result, the formation of hydrogen sulfide harms the gut epithelial cells and stimulates mucosal inflammation (Loubinoux et al. 2002; Rowan et al. 2010). Accordingly, the above data indicate that gut microbial configuration changes are linked with IBD pathogenesis. The outcome of dysbiosis on IBD and the pathological changes are provided in Table 3.2.
4.2 Colorectal Cancer (CRC)
The World Cancer Research Foundation (WCRF), as well as the American Institute for Cancer Research (AICR), recognized that diet is one of the essential external components in CRC etiology (Dumas et al. 2016). The microbiota has been a prominent aspect of a few cancers such as breast, liver, biliary system, and CRC. Accommodating around 3 × 1013 microbes, the colorectum interplays with a huge population of microorganisms, and with that, the intestinal epithelium found a stable cross talk (Qin et al. 2010). The 16 s ribosomal RNA sequencing analyses were carried out to illustrate the CRC microbiota in stool and mucosal samples (Yu et al. 2017). Direct observation was that the microbiota of CRC individuals had undergone severe dysbiosis when correlated with the composition of healthy adults displaying numerous ecological microhabitats in individuals with CRC. In addition, certain microbes such as Bacteroides fragilis, E. coli, Enterococcus faecalis, and Streptococcus gallolyticus are independently associated with CRC in several combinations and systematic examinations. Metagenomic analysis revealed that gut microbiota associated with CRC, henceforth named CRC microbiota, consist of an abundance of species, a reduced plethora of Roseburia, and an enhanced myriad of procarcinogenic bacterial communities like Bacteroides, Escherichia, Fusobacteria, and Porphyromonas (Yu et al. 2017).
Recently, it was detected that intestinal bacteria could stimulate the development of CRC through chronic inflammation initiation, biosynthesis of genotoxin (meddle with the regulation of cell cycle), heterocyclic amine stimulation, or toxic metabolite synthesis of carcinogenic elements of pro-diet (Candela et al. 2014). Chronic inflammation is connected with the risk of evolving cancer and does through causing mutations, cell proliferation, and provoking angiogenesis or apoptosis inhibition (Medzhitov 2008; Grivennikov and Karin 2010). The microbiota dysbiosis benefits opportunistic pathogens that stimulate innate and adaptive immune system components, and bacterial shift, which results in chronic inflammation (Ivanov et al. 2009b). The commensal bacteria stimulate the innate immune system. As a result, dendritic cells, macrophages, and NK cells enhance the production of pro-inflammatory cytokines like TNF-α, IL-23, IL-12, and INFγ, with consequent stimulation of adaptive immune cells, including B cells, T cells, lymphocytes, and other mediators of inflammation (Keku et al. 2015). The inflammatory reaction to commensal bacteria is the stimulation of NF-κB transcription factor and (signal transducer and activator of transcription) STAT3 in epithelial cells (Greten et al. 2004; Guarner 2006; Hooper et al. 2014; Tian et al. 2003), the production of nitrogen and reactive oxygen species resulting in oxidative stress, damage of DNA, and the progression of CRC. In addition, colonic polyposis is linked with large microbial density compiled inside polyps that induce local inflammatory reactions. The development of polyps and the density of microorganisms may be inhibited through IL-10, a derivative of T cells and Tregs (Dennis et al. 2013). Therefore, it is concluded that the modulation of normal homeostasis among microbiota and host is important for inflammation and the subsequent alterations which cause colon carcinogenesis.
In the interaction between host and microbiota, metabolism is an essential factor. The microbial metagenome encrypts genes that digest more dietary components and host compounds like bile acids. The fecal bile acids increase through a high-fat diet, provoking their enterohepatic circulation and production. The 7α-dehydroxylating bacteria turn colonic initial bile acids into secondary bile acids that are cytotoxic to gut epithelial cells in animal models (Ridlon et al. 2006; Cheng and Raufman 2005). This conversion enhances these secondary bile acids’ hydrophilicity (de Giorgio and Blandizzi 2010). Consuming animal protein and a high-fat diet increases the number of secondary bile acids like lithocholic acid, cholic acid, and deoxycholic acid, which causes a higher CRC risk. The deoxycholic acid damages the tract of the mucosa intestine, causes DNA damage, creates genomic instability, and assists the development of tumors. This process might influence bile acids’ influence on the colon’s carcinogenesis (Rubin et al. 2012).
In contrast, people with a low-fat diet are also affected by CRC, and the risk is through various factors like host health, genetic predisposition, and luminal interplay. Studies determined that CRC cases contained reduced butyrate-producing bacteria F. prausnitzii, Eubacterium rectale, and increased Enterococcus faecalis. Therefore, it is concluded that the colonic bacterial community is a factor that causes CRC.
Furthermore, B. fragilis, an enterotoxigenic strain, colonizes the mucosa of adults in an asymptomatic process. However, in a few cases, these strains release B. fragilis toxin (BFT), which induces inflammatory diarrhea. The B. fragilis toxin stimulates NF-κB results in the expression of cytokines, which assist in mucosa inflammation (Sears 2009). Therefore, BFT is established as one of the major toxins in the progression of CRC; moreover, in CRC individuals, toxins are transcribed in tumors derived from Shigella flexneri, E. coli, and Salmonella enterica. The data indicate that enterobacterial toxins involve in tumorigenesis (Schwabe and Wang 2012).
The composition and activities of the intestinal microbiota are majorly affected by diet (Duncan et al. 2007). The colonic bacteria produce SCFAs like butyrate, which inhibits CRC progression, prevents histone deacetylases in colonocytes, and induces apoptosis in CRC cell lines (Leonel and Alvarez-Leite 2012; Zhang et al. 2010). Butyrate also stimulates the functions of the large intestine and prevents the growth of pathogens. In addition, butyrate and propionate were exhibited to alter colonic regulatory T cells and utilize an effective anti-inflammatory impact in animal models (Chen et al. 2013). Research studies demonstrated that a fiber-containing diet affects the production of SCFAs (Tomasello et al. 2014). It is concluded that a high-fiber diet increases SCFAs production, with a subsequent decrease in intestinal pH that benefits fermentation in the colon, inhibits pathogen colonization, and reduces the absorption of carcinogen (Macfarlane and Macfarlane 2012) therefore decreasing the risk of CRC (Keku et al. 2015). Different pathogenic mechanisms linked with colorectal cancer are listed in Table 3.3.
4.3 Obesity
Obesity is a global condition that is likely accelerating its prevalence worldwide. It affected approximately 107.7 million young children and 603.7 million adults worldwide, and over 60% of fatality is associated with excess body mass index (BMI) (Afshin et al. 2017). Obesity is strongly related to numerous antagonistic comorbidities, such as cardiovascular disease, cancer, and type 2 diabetes mellitus. Obesity is recognized as a complex and multifactorial disorder primarily derivable to peril components of genetic history, lifestyle, and habitat (Hruby and Hu 2015). Over the last decades, the connection and induced role enacted through gut microbiota and obesity have been an astounding discovery. The gut microbiota of mice and humans is dominated by numerous bacterial microbiota containing Bacteroidetes, Firmicutes, and Actinobacteria. The initial observation exhibited distinctive gut microbial configuration in genetically obese (ob/ob) mice correlated to lean (ob/+) and wild (+/+) offsprings in a context of similar polysaccharide-enriched diet (Ley et al. 2005) through epitomizing the decreased plethora of Bacteroidetes and enhanced Firmicutes in obese patients. To characterize the impacts of gut microbiota from genetic alterations, Turnbaugh and co-workers relocated lean and obese microbiota to germfree mice; consequently, more enhancements in total body fat in recipients colonized by microbiota of obese were observed when correlated to lean microbiota (Turnbaugh et al. 2006). The malfunction of a gut ecosystem that leads to reduced microbiota certainty was linked with IBD and obesity (Qin et al. 2010; Turnbaugh et al. 2009). The initial observations on the association between the gut microbiota and obesity have revealed enhanced Firmicutes number, though a decrease in the number of Bacteroidetes in both humans and mice affected obesity when correlated with lean individuals (Furet et al. 2010). Fascinatingly, these changes can be reversed through weight loss through dietary habits. In the selection of microbiota, the immune system is also considered pivotal. The mice models with unusual TLR signaling or express bactericidal reactive oxygen microbes have exalted antibody serum titers to counteract one’s commensal bacteria (Slack et al. 2009). The enriched serum titers are needed to retain the host’s and gut microbiota’s commensal association. The deficiency of TLRs in mutant mice showed a modified gut microbial composition. The deficiency of TLR-5 mice promotes obesity, metabolic disorders, and inflammation.
The gut microbiota of mice has an enhanced potential to harvest energy from the gut when correlated to their counterparts of germfree mice (Wostmann et al. 1983). Metagenomic gut microbiota studies in obese human and mouse models have identified enhanced carbohydrate fermentation ability (Turnbaugh et al. 2009). This transformation enhances the SCFAs production in the host to enhance the energy harvest. The SCFAs have been suggested to attach to certain GPC receptors such as GPR41, GPR43, FFAR2, and FFAR3, which could improve the nutrient consumption and/or progression of adipose tissue mass. The clinical analyses performed in mice with insufficient GPR41 proposed that the stimulation of GPR41 through SCFAs is responsible for the secretion of PYY gut hormone. Despite this, the mice with abundant expression of GPR43 are fed an obesogenic that enhances the propagation of adipocytes and prevents lipolysis in adipocytes. The mice with GPR43 deficiency are treated with enriched carbohydrates and an enriched fat diet containing a meager body mass and a myriad lean mass correlated with mice of wild type (Bjursell et al. 2011). In addition, the drastic modulations in the composition of gut microbiota, which appear aftermath of medication with antibiotics, can act defense against glucose sensitivity, obesity, and insulin resistance stimulated through enriched fat and a free carbohydrate diet (Cani et al. 2008). According to a recent hypothesis, the gut microbiota can retain the host’s metabolic homeostasis. Metabolic disorders like T2DM and obesity are connected with low-level inflammation and modified microbial composition; a microbial strain might enact as a provoking factor in the progression of DM, obesity, as well as inflammation stimulated by a fat-enriched diet.
Low-level metabolic inflammation is considered a pivotal component of metabolic disorders. Numerous analyses illustrated that the metabolic system is unified with an enhanced pro-inflammatory cytokine-like TNF-α, common obesity-associated inflammation, and insulin resistance. Lipopolysaccharides (LPS) endotoxin, an important factor in Gram-negative bacterial cell walls such as Bacteroidetes, enhances the progression of adipose tissues, affecting insulin resistance and inflammation. LPS also acts as a stimulating factor of fat and enriches diet-activated metabolic disorders. However, metabolic endotoxemia provokes the production of TNF-α, IL-1, and IL-6. The research studies determined that metabolic endotoxemia exists because of the alterations in intestinal microbiota due to antibiotic medication that drastically decreased the native intestinal microbiota and reestablished the common plasma LPS values in the fat-enriched diet fed in mice models. Antibiotic medication suggests that bacteria in the gut affected by antibiotic consumption regulate intestinal penetrability; metabolic endotoxemia occurs. The deficiency of TLR4 (considered as LPS) is defensive against obesity from visceral and subcutaneous adipose tissue development, glucose resistance stimulated by a fat-enriched diet, and the endoplasmic reticulum stress is the major organ for digestion of lipids and glucose.
4.4 Diabetes
Genetic background, diet, and environmental conditions influence the gut microbial community. Any significant deviation of these factors influences the apparent habitat alterations. It is significantly stable in middle-aged humans. However, there is a high number of notable gut microbiota alterations that have been in interindividuals. The surfeit of biological reactions regulates with the assistance of modulated gut microbiota.
4.4.1 Type 1 Diabetes Mellitus (T1DM)
T1DM is a perennial autoimmune disorder diagnosed usually at a young age and distinguished by the demolition of immune-mediated responses of insulin formation from the pancreatic β-cells (Lamichhane et al. 2018). The ubiquity of T1DM is increasing globally because of a deficiency of suitable therapeutic procedures. The environmental factors associated with a genetic predisposition are eminent for the progression of T1DM (Battaglia and Atkinson 2015). The initial pathogenesis of T1DM is identified by insulitis, abundance expression of autoantibodies over β-cell antigens observed by decreased insulin production, and demise of β-cells (Battaglia and Atkinson 2015). The definite factors responsible for inducing T1DM pathogenesis are still unknown; moreover, the usual aspect that triggers T1DM is genetic history and habitat (Battaglia and Atkinson 2015). The triggering factors like viral infections, usage of antibiotics, consumption of cow milk proteins at early ages, deficiency in breastfeeding and vitamin D supplement, and disclosure to endocrine disrupting synthesis. The function of gut microbiota can affect intestinal mucosa, such as autoimmunity over β-cells. Clinical studies showed that in T1DM models, reduced Firmicutes and enhanced Bacteroides numbers are identified, exhibiting an association between T1DM and microbiota.
In contrast, the reduced number of Bacteroides and Firmicutes is linked with individuals correlated to lean individuals (Schwiertz et al. 2010). Modifications in microbial composition might occur because of differences in the glucose levels of host results due to diet and intestinal habitat. However, the definite mechanisms are yet unknown, though these alterations might be connected with the progression of T1DM, as reduced Bifidobacterium can impact the gut penetrability and mucosal immune reactions affecting autoimmune responses. The interplay between intestinal microbiota and the host immune system enacts an important role in the growth of T1DM. The immune system cells can perceive the metabolites and analytes of gut microbiota which can alter the role of immune cells, stimulating the development of T1DM pathogenesis.
Similarly, the pancreas also consists of its microbiota, and the modification of pancreatic microbiota is linked with the assistance of intrapancreatic immune reactions and initiation of diabetes in addition to pancreatic cancer and T1DM (Pushalkar et al. 2018). The dysbiosis and functions of gut metabolites can stimulate the immune system’s GALT malfunctions, like unusual IgA excretion and reproduction of colonic regulatory T cells (Pabst and Mowat 2012). The microbiota-stimulated deterioration of the immune reactions in GALT can also affect systematic immune reactions.
As discussed above, the intestinal microbiota can be able to control the host immune reactions by certain mechanisms such as through stimulating the innate immune reactions by TLRs as well as through stimulating free fatty acid receptors 2/3 (FFAR) by gut metabolites like SCFAs (acetate, butyrate, and propionate) and lactic acid. Butyrate is recognized as linked with the distinction of endemic T cells into Tregs, although acetate and propionate are familiar to be fundamental for shifting Tregs to the intestine (Scott et al. 2018). Abundance stimulation of TLRs and usually less production of SCFAs, majorly butyrate, are noted to have reactive impacts on T1DM-related autoimmunity and might contribute essential therapeutic marks for the inhibition of T1DM. TLRs are imperative for identifying microbial compounds containing nucleic acids, proteins, and LPS. TLRs can also recognize the endogenous compounds produced from the injured tissues or cells by damage-associated molecular patterns (DAMPs) (Scott et al. 2018). In addition, a few analyses proposed that the TLRs (for instance, TLR 3, 7, and 9) are produced in the pancreas of individuals affected with T1DM. TLR mechanisms modify the transcription factor NF-kB and I kappa B kinase (IKK) complex (Xie et al. 2018). NF-kB also controls inflammatory intercessors like IL-Iβ, the usual stimulus of T1DM pathogenesis (Xie et al. 2018).
4.4.2 Type 2 Diabetes Mellitus
Globally, T2DM is a common chronic disease with an escalating predominance in several countries. However, the genetic history of individuals is pivotal, although the environmental aspects, lifestyle, and dietary habits are recognized as fundamental factors in T2DM individuals. An auspicious prospective path could use a symbiotic approach linking gut microbiota and diet to treat T2DM. T2DM is distinguished by the decrease in Firmicutes and an enrichment of Bacteroidetes and Firmicutes ratio due to variations in plasma glucose levels (Graessler et al. 2013; Larsen et al. 2010). In the patients affected with T2DM, obesity is proximately associated. Studies have shown that gut microbiota modifications are not similar between both category patients. The consumption of a high-fat diet enhances certain microbes in the gut, leading to increased levels of lipopolysaccharides and insulin tolerance. T2DM is a complex metabolic disorder characterized by insulin tolerance, hyperglycemia, and metabolic disruption of blood lipids. The gut microbiota is vital in preventing T2DM by modulating individuals’ biological activities and metabolism. T2DM associated with the aberrant intestinal microbial composition initiates moderate inflammation. In T2DM individuals, the gut microbiota contains a decrease in the number of butyrate-expressing bacteria, specifically Roseburia intestinalis and Faecalibacterium prausnitzii; low-grade dysbiosis and pro-inflammatory habitat with enrichment in production of microbial genes responsible for oxidative stress; decreased genes expression entangled in the synthesis of vitamins; and enhanced serum LPS levels and increase in intestinal penetrability.
Furthermore, the major changes in the gut microbiota linked with T2DM contain a reduction in the levels of Firmicutes and an increase of Bacteroidetes and Proteobacteria (Roager et al. 2017). In T2DM patients, the microbiota contains high-grade levels of pathogens like Clostridium clostridioformis, Bacteroides caccae, Clostridium ramosum, Clostridium hathewayi, E. coli, Clostridium symbiosum, and Eggerthella spp. (Karlsson et al. 2013). The Gram-negative bacteria produce LPS, which can induce innate immunity by stimulating the TLRs and expressing inflammatory cytokines.
Moreover, LPS induces the expression of NF-kB and c-Jun-terminal kinase mechanisms; these two ways are associated with the progression of insulin resistance and the lack of insulin signaling in adipocytes, liver, and hypothalamus (Newsholme et al. 2016). The metabolites of gut microbiota, such as SCFAs like acetate, butyrate, and propionate, are responsible for the fermentation of dietary carbohydrates. Acetate and propionate are formed from the Bacteroidetes sp. The Firmicutes produce butyrate. Dysbiosis is associated with modifying SCFAs production, whereas butyrate progresses insulin resistance and secretion by activating the expression of GLP-1 and decreasing the adipocyte’s inflammation (Ríos-Covián et al. 2016). More prominently, butyrate is pivotal for assisting T2DM symptoms.
4.5 Irritable Bowel Syndrome
Irritable bowel syndrome (IBS) is a functional gastrointestinal disorder associated with altered bowel discharges and severe abdomen pain. IBS is a downstream signature disease of gut microbiota dysbiosis. Existing evidence claims that gut dysbiosis is the main reason for IBS. The prevalence of IBS is up to 12% in the general population (Lovell and Ford 2012). Pathogenesis of IBS stems from a disturbance in the gut-brain axis due to psychological stress and visceral hypersensitivity. Microbial distribution in the GI tract of healthy individuals differs from IBS patients (Tap et al. 2017). Beneficial microbial communities reduce in the GI tract of IBS patients (Carroll et al. 2011). In 2017, Botschuijver et al. found a decline in the diversity of beneficial mycobiome (fungal communities) in IBS patients (Botschuijver et al. 2017). The overgrowth of pathogenic bacteria in the small intestine induces the pathogenesis of IBS. Small intestine bacteria overgrowth (SIBO) triggers clinical obligations such as visceral sensation and poor nutrition uptake (Coelho et al. 2000; Giannella et al. 1974). The correlation between SIBO and IBS is quite intuitive. The lack of diagnostic tools that could detect the markers of SIBO is a big problem in IBS clinical practice. But it is possible to screen and characterize the microbial communities during IBS pathogenesis with metagenomics and culture-independent tools. Understanding the gut microbiome dynamics of healthy and diseased individuals might be achieved by case-control studies with advanced genomic tools. Targeting gut microbes as markers enables the choice of therapy with pharmaceutical or non-pharmaceuticals and nutraceuticals.
4.6 Diarrhea
Diarrhea is one of the main clinical manifestations ranging from mild to severe gastrointestinal exacerbations. Diarrheal cases are reported in children under 5 years of age in poor and developing countries (MacGill 2017; Roman et al. 2017). Diarrhea is identified as a frequent discharge of loose bowels with high liquidity, nevertheless, poor hygienic practices, intake of contaminated consumables, and multiple factors (Liu et al. 2012). Pathogen invasion is the main reason for diarrheal infections. Certain pathogens, viz., Salmonella, Campylobacter, Shigella, and Rotavirus, are responsible for disturbing the gut ecosystem with their invasive mechanisms (Garthright et al. 1988). Non-typhoid Salmonella enterica serovar Typhimurium is associated with higher infectivity in dysentery cases. Next to Salmonella, Campylobacter is the pathogen that severely damages the balance in the gut ecosystem. Shigella is another food-borne pathogen that affects the small intestine and cause inflammatory diarrhea. Shigella can cause infection even at very low inoculums. Shigella invasion occurs through contaminated food and water intake, unhygienic sex practices, and poor sanitation. Besides, protozoans Giardia and Entamoeba histolytica (amoebic dysentery) and Rotavirus are responsible for diarrheal dysbiosis in the gut microbiome. Diarrheal infections can be inflammatory or non-inflammatory. Pathogens invade the GI epithelium and affect the intestine’s colon and ileum. In non-inflammatory dysentery, the pathogen directly invades the small intestine and mediates its toxicity (Taylor et al. 2013). Antibiotics and oral rehydration solutions are used as therapeutic practices to treat dysentery damage in the gut. With the beneficial effects and nontoxic microbiome reconstructive properties of probiotics, they are currently being prescribed by doctors to combat these types of GI diseases (Kota et al. 2018).
5 Redirecting Gut Microbiome to Modulate Host Immunity and Health
Reconstituting the gut microbiome to its native state is called gut eubiosis. Therapeutic strategies with non-pharmaceutical active ingredients that target the host’s gut microbiome to modulate the gut microbiome’s composition offered promising and reliable outcomes in recent preclinical and clinical studies. Similar studies focusing on gut health and host immunity regulation with pre- and probiotics suggested strong and reliable observations toward exploring the gut microbiome as an operational tool for immunometabolic therapy. Prebiotics, probiotics, and some other functional foods which could favor nonpathogenic beneficial microbes in the GI tract to grow are mainly investigated and deeply studied as non-pharmaceutical factors to shape the gut environment by modulating the composition of the intestinal microbiome. Both pre- and probiotics are the better choices for immune and metabolic therapy because of their availability and accuracy. Probiotics and prebiotics used in human consumables are enlisted in Table 3.4. Probiotics are certain nonpathogenic microbes that may be residents of the GI tract. Probiotics alter the proportion of gut microbiome toward beneficial microbes and confer host with several benefits such as resistance to invading pathogenic groups and immunometabolic modulation. Prebiotics are the nutritional factors that help probiotic bacteria to grow. Dietary interventions with non-pharmaceutical factors such as probiotics and prebiotics offer an effective way of therapy to combat various gastrointestinal and non-gastrointestinal metabolic disorders by redirecting the gut microbiome to a native or eubiotic state.
6 Conclusions and Future Perspectives
The human body harbors several microbial ecosystems called gut, oral, vaginal, skin, and respiratory microbiomes. Gut microbiota regulates the host immune system, and diversions from normal microbial development such as C-sections, formulated diet, antimicrobial usage, and sterile vaccine in neonates alter the progression of immune system outcomes and possibly predispose entities to several inflammatory disorders after that in life. According to immunological and clinical analysis, it is believed that intestinal microbiota dysbiosis might be a fundamental aspect of various inflammatory diseases. Intestinal dysbiosis decreases beneficial microbes resulting in the progression of several inflammatory responses and immune-interceded diseases. Hence targeting and engineering gut microbiota are an effective therapeutic strategy for immune and metabolic issues. Redirecting the gut microbiota from a dysbiotic to a eubiotic state is the main agenda and algorithm of gut engineering. Prebiotics and probiotics or their derived nutraceuticals alter the gut microbes toward the beneficial microbial communities and suppress the inflammatory responses and immune dysregulation, conferring host with boosted immunity and better health.
References
Aagaard K, Ma J, Antony KM, Ganu R, Petrosino J, Versalovic J (2014) The placenta harbors a unique microbiome. Sci Transl Med 6:237ra65. https://doi.org/10.1126/scitranslmed.3008599
Afshin A, Forouzanfar MH, Reitsma MB, Sur P, Estep K et al (2017) Health effects of overweight and obesity in 195 countries over 25 years. N Engl J Med 377:13e27. https://doi.org/10.1056/NEJMoa1614362
Agus A, Denizot J, Thévenot J, Martinez-Medina M, Massier S, Sauvanet P et al (2016) Western diet induces a shift in microbiota composition enhancing susceptibility to Adherent-Invasive E. coli infection and intestinal inflammation. Sci Rep 6:1–14. https://doi.org/10.1038/srep19032
Albenberg LG, Lewis JD, Wu GD (2012) Food and the gut microbiota in inflammatory bowel diseases: a critical connection. Curr Opin Gastroenterol 28:314–320. https://doi.org/10.1097/MOG.0b013e328354586f
Asarat M, Vasiljevic T, Apostolopoulos V, Donkor O (2015) Short-chain fatty acids regulate secretion of IL-8 from human intestinal epithelial cell lines in vitro. Immunol Investig 44:678–693. https://doi.org/10.3109/08820139.2015.1085389
Atarashi K, Tanoue T, Oshima K et al (2013) Treg induction by a rationally selected mixture of clostridia strains from the human microbiota. Nature 500(7461):232–236. https://doi.org/10.1038/nature12331
Bäckhed F, Ley RE, Sonnenburg JL, Peterson DA, Gordon JI (2005) Host-bacterial mutualism in the human intestine. Science 307(5717):1915–1920. https://doi.org/10.1126/science.1104816
Balamurugan R, Rajendiran E, George S et al (2008) Real-time polymerase chain reaction quantification of specific butyrate-producing bacteria, Desulfovibrio and Enterococcus faecalis in the feces of patients with colorectal cancer. J Gastroenterol Hepatol 23(8 Pt 1):1298–1303. https://doi.org/10.1111/j.1440-1746.2008.05490.x
Battaglia M, Atkinson MA (2015) The streetlight effect in type 1 diabetes. Diabetes 64:1081–1090. https://doi.org/10.2337/db14-1208
Baumgart M, Dogan B, Rishniw M, Weitzman G, Bosworth B, Yantiss R et al (2007) Culture independent analysis of ileal mucosa reveals a selective increase in invasive Escherichia coli of novel phylogeny relative to depletion of Clostridiales in Crohn’s disease involving the ileum. ISME J 1:403–418. https://doi.org/10.1038/ismej.2007.52
Bjursell M et al (2011) Improved glucose control and reduced body fat mass in free fatty acid receptor 2-deficient mice fed a high-fat diet. Am J Physiol Endocrinol Metab 300:E211–E220. https://doi.org/10.1152/ajpendo.00229.2010
Bloom SM, Bijanki VN, Nava GM, Sun L, Malvin NP, Donermeyer DL et al (2011) Commensal Bacteroides species induce colitis in host-genotype-specific fashion in a mouse model of inflammatory bowel disease. Cell Host Microbe 9:390–403. https://doi.org/10.1016/j.chom.2011.04.009
Boismenu R, Havran WL (1994) Modulation of epithelial cell growth by intraepithelial gamma delta T cells. Science 266:1253–1255. https://doi.org/10.1126/science.7973709
Bonnet M, Buc E, Sauvanet P et al (2014) Colonization of the human gut by E. coli and colorectal cancer risk. Clin Cancer Res 20:859–867. https://doi.org/10.1158/1078-0432.CCR-13-1343
Borthakur A, Anbazhagan AN, Kumar A, Raheja G, Singh V, Ramaswamy K et al (2010) The probiotic Lactobacillus plantarum counteracts TNF-induced downregulation of SMCT1 expression and function. AJP Gastrointest Liver Physiol 299:G928–G934. https://doi.org/10.1152/ajpgi.00279.2010
Botschuijver S, Roeselers G, Levin E, Jonkers DM, Welting O, Heinsbroek S, de Weerd HH, Boekhout T, Fornai M, Masclee AA, Schuren F, de Jonge WJ, Seppen J, van den Wijngaard RM (2017) Intestinal fungal dysbiosis is associated with visceral hypersensitivity in patients with irritable bowel syndrome and rats. Gastroenterology 153(4):1026–1039. https://doi.org/10.1053/j.gastro.2017.06.004
Candela M, Turroni S, Biagi E, Carbonero F, Rampelli S, Fiorentini C et al (2014) Inflammation and colorectal cancer, when microbiota-host mutualism breaks. World J Gastroenterol 20:908–922. https://doi.org/10.3748/wjg.v20.i4.908
Cani PD et al (2008) Changes in gut microbiota control metabolic endotoxemia-induced inflammation in high-fat diet-induced obesity and diabetes in mice. Diabetes 57:1470–1481. https://doi.org/10.2337/db07-1403
Carroll IM, Ringel-Kulka T, Keku TO, Chang YH, Packey CD, Sartor RB, Ringel Y (2011) Molecular analysis of the luminal- and mucosal-associated intestinal microbiota in diarrhea-predominant irritable bowel syndrome. Am J Physiol Gastrointest Liver Physiol 301(5):G799–G807. https://doi.org/10.1152/ajpgi.00154.2011
Chairatana P, Nolan EM (2017) Defensins, lectins, mucins, and secretory immunoglobulin a: microbe-binding biomolecules that contribute to mucosal immunity in the human gut. Crit Rev Biochem Mol Biol 52(1):45–56. https://doi.org/10.1080/10409238.2016.1243654
Chen L, Karboune S (2019) Prebiotics in food and health: properties, functionalities, production, and overcoming limitations with second-generation levan-type fructooligosaccharides. Encyclopedia of Food Chem 3:271–279. https://doi.org/10.1016/B978-0-08-100596-5.21746-0
Chen HM et al (2013) Decreased dietary fiber intake and structural alteration of gut microbiota in patients with advanced colorectal adenoma. Am J Clin Nutr 97:1044–1052. https://doi.org/10.3945/ajcn.112.046607
Cheng K, Raufman JP (2005) Bile acid–induced proliferation of a human colon cancer cell line is mediated by transactivation of epidermal growth factor receptors. Biochem Pharmacol 70(7):1035–1047. https://doi.org/10.1016/j.bcp.2005.07.023
Coelho AM, Fioramonti J, Buéno L (2000) Systemic lipopolysaccharide influences rectal sensitivity in rats: role of mast cells, cytokines, and vagus nerve. Am J Physiol Gastrointest Liver Physiol 279(4):G781–G790. https://doi.org/10.1152/ajpgi.2000.279.4.G781
Cosnes J, Gower-Rousseau C, Seksik P, Cortot A (2011) Epidemiology and natural history of inflammatory bowel diseases. Gastroenterology 140:1785–1794. https://doi.org/10.1053/j.gastro.2011.01.055
Costa GM, Paula MM, Barão CE, Klososki SJ, Bonafe EG, Visentainer JV, Pimentel TC (2019) Yoghurt added with Lactobacillus casei and sweetened with natural sweeteners and/or prebiotics: implications on quality parameters and probiotic survival. Int Dairy J 97:139–148. https://doi.org/10.1016/j.idairyj.2019.05.007
Cox LM, Blaser MJ (2013) Pathways in microbe-induced obesity. Cell Metab 17:883–894
Dalton JE et al (2006) Intraepithelial gammadelta+ lymphocytes maintain the integrity of intestinal epithelial tight junctions in response to infection. Gastroenterology 131:818–829
Darfeuille-Michaud A, Boudeau J, Bulois P, Neut C, Glasser AL, Barnich N et al (2004) High prevalence of adherent-invasive Escherichia coli associated with ileal mucosa in Crohn’s disease. Gastroenterology 127:412–421. https://doi.org/10.1053/j.gastro.2004.04.061
de Giorgio R, Blandizzi C (2010) Targeting enteric neuroplasticity: diet and bugs as new key factors. Gastroenterology 138:1663–1666. https://doi.org/10.1053/j.gastro.2010.03.022
de Simone C (2019) The unregulated probiotic market. Clin Gastroenterol Hepatol 17(5):809–817. https://doi.org/10.1016/j.cgh.2018.01.018
den Besten G, van Eunen K, Groen AK, Venema K, Reijngoud DJ, Bakker BM (2013) The roles of short-chain fatty acids in the interplay between diet, gut microbiota, and host energy metabolism. J Lipid Res 54:2325–2340. https://doi.org/10.1194/jlr.R036012
Dennis KL, Wang Y, Blatner NR, Wang S, Saadalla A, Trudeau E et al (2013) Adenomatous polyps are driven by microbe-instigated focal inflammation and are controlled by IL-10-producing T cells. Cancer Res 73:5905–5913. https://doi.org/10.1158/0008-5472.CAN-13-1511
Donia MS, Fischbach MA (2015) Small molecules from the human microbiota. Science 349(6246):1254766
dos Santos DX, Casazza AA, Aliakbarian B, Bedani R, Saad SMI, Perego P (2019) Improved probiotic survival to in vitro gastrointestinal stress in a mousse containing Lactobacillus acidophilus La-5 microencapsulated with inulin by spray drying. Lwt 99:404–410. https://doi.org/10.1016/j.lwt.2018.10.010
Dumas ME, Barton RH, Toye A, Cloarec O, Blancher C, Rothwell A, Mitchell SC (2006) Metabolic profiling reveals a contribution of gut microbiota to fatty liver phenotype in insulin-resistant mice. Proc Natl Acad Sci U S A 103(33):12511–12516. https://doi.org/10.1073/pnas.0601056103
Dumas JA, Bunn JY, Nickerson J, Crain KI, Ebenstein DB, Tarleton EK, Makarewicz J, Poynter ME, Kien CL (2016) Dietary saturated fat and monounsaturated fat have reversible effects on brain function and the secretion of pro-inflammatory cytokines in young women. Metabolism 65:1582–1588. https://doi.org/10.1016/j.metabol.2016.08.003
Duncan SH, Louis P, Microbiol FHJ (2007) Cultivable bacterial diversity from the human colon. Lett Appl 44:343–350. https://doi.org/10.1111/j.1472-765X.2007.02129.x
Fan J, Chen L, Mai G, Zhang H, Yang J, Deng D, Ma Y (2019) Dynamics of the gut microbiota in developmental stages of Litopenaeus vannamei reveal its association with body weight. Scientific Reports 9(1):734
Frank DN, St Amand AL, Feldman RA et al (2007) Molecular-phylogenetic characterization of microbial community imbalances in human inflammatory bowel diseases. Proc Natl Acad Sci U S A 104(34):13780–13785. https://doi.org/10.1073/pnas.0706625104
Fujimoto T, Imaeda H, Takahashi K et al (2013) Decreased abundance of Faecalibacterium prausnitzii in the gut microbiota of Crohn’s disease. J Gastroenterol Hepatol 28(4):613–619. https://doi.org/10.1111/jgh.12073
Furet JP et al (2010) Differential adaptation of human gut microbiota to bariatric surgery-induced weight loss: links with metabolic and low-grade inflammation markers. Diabetes 59:3049–3057. https://doi.org/10.2337/db10-0253
Garthright WE, Archer DL, Kvenberg JE (1988) Estimates of incidence and costs of intestinal infectious diseases in the United States. Public Health Rep 103(2):107–115
Giannella RA, Rout WR, Toskes PP (1974) Jejunal brush border injury and impaired sugar and amino acid uptake in the blind loop syndrome. Gastroenterology 67(5):965–974
Gill RK (2005) Expression and membrane localization of MCT isoforms along the length of the human intestine. AJP Cell Physiol 289:C846–C852. https://doi.org/10.1152/ajpcell.00112.2005
Gordon JI, Dewey KG, Mills DA, Medzhitov RM (2012) The human gut microbiota and under nutrition. Sci Transl Med 6(4):137. https://doi.org/10.1126/scitranslmed.3004347
Goto Y, Obata T, Kunisawa J, Sato S, Ivanov II, Lamichhane A, Takeyama N, Kamioka M, Sakamoto M, Matsuki T (2014) Innate lymphoid cells regulate intestinal epithelial cell glycosylation. Science 345:1254009. https://doi.org/10.1126/science.1254009
Graessler J, Qin Y, Zhong H et al (2013) Metagenomic sequencing of the human gut microbiome before and after bariatric surgery in obese patients with type 2 diabetes: correlation with inflammatory and metabolic parameters. Pharmacogenomics J 13(6):514–522. https://doi.org/10.1038/tpj.2012.43
Greten FR, Eckmann L, Greten TF, Park JM, Li ZW, Egan LJ et al (2004) IKKbeta links inflammation and tumorigenesis in a mouse model of colitis-associated cancer. Cell 118:285–296. https://doi.org/10.1016/j.cell.2004.07.013
Grivennikov SI, Karin M (2010) Dangerous liaisons: STAT3 and NF-kappa B collaboration and crosstalk in cancer. Cytokine Growth Factor Rev 21:11–19. https://doi.org/10.1016/j.cytogfr.2009.11.005
Guarner F (2006) Enteric flora in health and disease. Digestion 73(Suppl 1):5–12. https://doi.org/10.1159/000089775
Hansen R, Thomson JM, El-Omar EM, Hold GL (2010) The role of infection in the aetiology of inflammatory bowel disease. J Gastroenterol 45:266–276. https://doi.org/10.1007/s00535-009-0191-y
Ho AL, Kosik O, Lovegrove A, Charalampopoulos D, Rastall RA (2018) In vitro fermentability of xylo-oligosaccharide and xylo-polysaccharide fractions with different molecular weights by human faecal bacteria. Carbohydr Polym 179:50–58. https://doi.org/10.1016/j.carbpol.2017.08.077
Holscher HD (2017) Dietary fiber and prebiotics and the gastrointestinal microbiota. Gut Microbes 8:172–184. https://doi.org/10.1080/19490976.2017.1290756
Hooper C, Jackson SS, Coughlin EE, Coon JJ, Miyamoto S (2014) Covalent modification of the NF-kappaB essential modulator (NEMO) by a chemical compound can regulate its ubiquitin binding properties in vitro. J Biol Chem 289:33161–33174. https://doi.org/10.1074/jbc.M114.582478
Hruby A, Hu FB (2015) The epidemiology of obesity: a big picture. PharmacoEconomics 33:673e89. https://doi.org/10.1007/s40273-014-0243-x
Ivanov II et al (2009a) Induction of intestinal Th17 cells by segmented filamentous bacteria. Cell 139:485–498. https://doi.org/10.1016/j.cell.2009.09.033
Ivanov K, Kolev N, Tonev A, Nikolova G, Krasnaliev I, Softova E et al (2009b) Comparative analysis of prognostic significance of molecular markers of apoptosis with clinical stage and tumor differentiation in patients with colorectal cancer: a single institute experience. Hepato-Gastroenterology 56:94–98
Kabat AM, Srinivasan N, Maloy KJ (2014) Modulation of immune development and function by intestinal microbiota. Trends Immunol 35(11):507–517. https://doi.org/10.1016/j.it.2014.07.010
Karlsson FH, Tremaroli V, Nookaew I, Bergström G, Behre CJ, Fagerberg B, Nielsen J, Bäckhed F (2013) Gut metagenome in European women with normal, impaired and diabetic glucose control. Nature 498(7452):99–103. https://doi.org/10.1038/nature12198
Keku TO, Dulal S, Deveaux A, Jovov B, Han X (2015) The gastrointestinal microbiota and colorectal cancer. Am J Physiol Gastrointest Liver Physiol 308:G351–G363. https://doi.org/10.1152/ajpgi.00360.2012
Kirat D, Kondo K, Shimada R, Physiol KS (2009) Dietary pectin up-regulates monocarboxylate transporter 1 in the rat gastrointestinal tract. Exp 94:422–433. https://doi.org/10.1113/expphysiol.2009.046797
Kleinnijenhuis J, Quintin J, Preijers F, Joosten LA, Ifrim DC, Saeed S et al (2012) Bacille calmette-guerin induces NOD2-dependent nonspecific protection from reinfection via epigenetic reprogramming of monocytes. Proc Natl Acad Sci U S A 109:17537–17542. https://doi.org/10.1073/pnas.1202870109
Koh A, De Vadder F, Kovatcheva-Datchary P, Bäckhed F (2016) From dietary fiber to host physiology: short-chain fatty acids as key bacterial metabolites. Cell 165:1332–1345. https://doi.org/10.1016/j.cell.2016.05.041
Kota RK, Ambati RR, Aswani Kumar YVV, Srirama K, Reddy PN (2018) Recent advances in probiotics as live biotherapeutics against gastrointestinal diseases. Curr Pharm Des 24(27):3162–3171. https://doi.org/10.2174/1381612824666180717105128
Kumar H, Kawai T, Akira S (2011) Pathogen recognition by the innate immune system. Int Rev Immunol 30:16–34. https://doi.org/10.3109/08830185.2010.529976
Lamichhane S, Ahonen L, Dyrlund TS, Siljander H, Hyoty H, Ilonen J, Toppari J, Veijola R, Hyotylainen T, Knip M et al (2018) A longitudinal plasma lipidomics dataset from children who developed islet autoimmunity and type 1 diabetes. Sci Data 5:180250. https://doi.org/10.1038/sdata.2018.250
Larsen N, Vogensen F, van den Berg F et al (2010) Gut microbiota in human adults with type 2 diabetes differs from non-diabetic adults. PLoS One 5(2):e9085. https://doi.org/10.1371/journal.pone.0009085
Lee JS, Cella M, Mcdonald KG, Garlanda C, Kennedy GD, Nukaya M, Mantovani A, Kopan R, Bradfield CA, Newberry RD (2012) AHR drives the development of gut ILC22 cells and postnatal lymphoid tissues via pathways dependent on and independent of notch. Nat Immunol 13:144–151. https://doi.org/10.1038/ni.2187
Leonel AJ, Alvarez-Leite JI (2012) Butyrate: implications for intestinal function. Curr Opin Clin Nutr Metab Care 15:474–479. https://doi.org/10.1097/MCO.0b013e32835665fa
Ley RE et al (2005) Obesity alters gut microbial ecology. Proc Natl Acad Sci U S A 102:11070–11075. https://doi.org/10.1073/pnas.0504978102
Liu L, Johnson HL, Cousens S, Perin J, Scott S, Lawn JE, Rudan I, Campbell H, Cibulskis R, Li M, Mathers C, Black RE, Child Health Epidemiology Reference Group of WHO and UNICEF (2012) Global, regional, and national causes of child mortality: an updated systematic analysis for 2010 with time trends since 2000. Lancet 379(9832):2151–2161. https://doi.org/10.1016/S0140-6736(12)60560-1
Loubinoux J, Bronowicki JP, Pereira IA et al (2002) Sulfate-reducing bacteria in human feces and their association with inflammatory bowel diseases. FEMS Microbiol Ecol 40(2):107–112. https://doi.org/10.1111/j.1574-6941.2002.tb00942.x
Lovell RM, Ford AC (2012) Global prevalence of and risk factors for irritable bowel syndrome: a meta-analysis. Clin Gastroenterol Hepatol 10(7):712–721.e4. https://doi.org/10.1016/j.cgh.2012.02.029
Macfarlane GT, Macfarlane S (2012) Bacteria, colonic fermentation, and gastrointestinal health. J AOAC Int 95:50–60. https://doi.org/10.5740/jaoacint.sge_macfarlane
MacGill M (2017) What you should know about diarrhea. https://www.medicalnewstoday.com/articles/158634.php
Madhukumar MS, Muralikrishna G (2012) Fermentation of xylo-oligosaccharides obtained from wheat bran and Bengal gram husk by lactic acid bacteria and bifidobacteria. J Food Sci Technol 49(6):745–752. https://doi.org/10.1007/s13197-010-0226-7
Martens JH, Barg H, Warren MJ, Jahn D (2002) Microbial production of vitamin B12. Appl Microbiol Biotechnol 58:275–285. https://doi.org/10.1007/s00253-001-0902-7
Maynard CL, Weaver CT (2009) Intestinal effector T cells in health and disease. Immunity 31:389–400. https://doi.org/10.1016/j.immuni.2009.08.012
Medzhitov R (2008) Origin and physiological roles of inflammation. Nature 454:428–435. https://doi.org/10.1038/nature07201
Mills KH (2011) TLR-dependent T cell activation in autoimmunity. Nat Rev Immunol 11:807–822. https://doi.org/10.1038/nri3095
Mucida D, Park Y, Kim G, Turovskaya O, Scott I, Kronenberg M, Cheroutre H (2007) Reciprocal TH17 and regulatory T cell differentiation mediated by retinoic acid. Science 317:256–260. https://doi.org/10.1126/science.1145697
Murray CM, Hutchinson R, Bantick JR, Belfield GP, Benjamin AD, Brazma D et al (2005) Monocarboxylate transporter Mctl is a target for immunosuppression. Nat Chem Biol 1:371–376. https://doi.org/10.1038/nchembio744
Nastasi C, Candela M, Bonefeld CM, Geisler C, Hansen M, Krejsgaard T et al (2015) The effect of short-chain fatty acids on human monocyte-derived dendritic cells. Sci Rep 5:1–10. https://doi.org/10.1038/srep16148
Negi S, Pahari S, Das DK, Khan N, Agrewala JN (2019) Curdlan limits mycobacterium tuberculosis survival through STAT-1 regulated nitric oxide production. Front Microbiol 10:1173
Neish AS (2009) Microbes in gastrointestinal health and disease. Gastroenterology 136:65–80. https://doi.org/10.1053/j.gastro.2008.10.080
Newsholme P, Cruzat VF, Keane KN, Carlessi BPI (2016) Molecular mechanisms of ROS production and oxidative stress in diabetes. Biochem J 473:4527–4550. https://doi.org/10.1042/BCJ20160503C
Nicholson JK, Holmes E, Kinross J, Burcelin R, Gibson G, Jia W, Pettersson S (2012) Host-gut microbiota metabolic interactions. Science 336:1262–1267. https://doi.org/10.1126/science.1223813
Pabst O, Mowat AM (2012) Oral tolerance to food protein. Mucosal Immunol 5:232–239. https://doi.org/10.1038/mi.2012.4
Pahari S, Kaur G, Negi S, Aqdas M, Das DK, Bashir H et al (2018) Reinforcing the functionality of mononuclear phagocyte system to control tuberculosis. Front Immunol 9:193. https://doi.org/10.3389/fimmu.2018.00193
Pahari S, Negi S, Aqdas M, Arnett E, Schlesinger LS, Agrewala JN (2019) Induction of autophagy through CLEC4E in combination with TLR4: an innovative strategy to restrict the survival of mycobacterium tuberculosis. Autophagy 8:1–23. https://doi.org/10.1080/15548627.2019.1658436
Pennington DJ, Silva-Santos B, Hayday AC (2005) Gammadelta T cell development—having the strength to get there. Curr Opin Immunol 17:108–115. https://doi.org/10.1016/j.coi.2005.01.009
Pott J, Hornef M (2012) Innate immune signalling at the intestinal epithelium in homeostasis and disease. EMBO Rep 13:684–698. https://doi.org/10.1038/embor.2012.96
Prentiss PG, Rosen H, Brown N, Horowitz RE, Malm OJ, Levenson SM (1961) The metabolism of choline by the germfree rat. Arch Biochem Biophys 94(3):424–429. https://doi.org/10.1016/0003-9861(61)90069-8
Pushalkar S, Hundeyin M, Daley D, Zambirinis CP, Kurz E, Mishra A, Mohan N, Aykut B, Usyk M, Torres LE et al (2018) The pancreatic cancer microbiome promotes oncogenesis by induction of innate and adaptive immune suppression. Cancer Discov 8:403–416. https://doi.org/10.1158/2159-8290.CD-17-1134
Qin J et al (2010) A human gut microbial gene catalogue established by metagenomic sequencing. Nature 464:59–65. https://doi.org/10.1038/nature08821
Ridlon JM, Kang DJ, Hylemon PB (2006) Bile salt biotransformations by human intestinal bacteria. J Lipid Res 47(2):241–259. https://doi.org/10.1194/jlr.R500013-JLR200
Ríos-Covián D, Ruas-Madiedo P, Margolles A, Gueimonde M, De Los Reyes-Gavilán CG, Salazar N (2016) Intestinal short chain fatty acids and their link with diet and human health. Front Microbiol 7:185. https://doi.org/10.3389/fmicb.2016.00185
Roager HM, Vogt JK, Kristensen M, LBS H, Ibrugger S, Maerkedahl RB, Bahl MI, Lind MV, Nielsen RL, Frøkiaer H, Gøbel RJ, Landberg R, Ross AB, Brix S, Holck J, Meyer AS, Sparholt MH, Christensen AF, Carvalho V, Hartmann B, Holst JJ, Rumessen JJ, Linneberg A, Sicheritz-Pontén T, Dalgaard MD, Blennow A, Frandsen HL, Villas-Bôas S, Kristiansen K, Vestergaard H, Hansen T, Ekstrøm CT, Ritz C, Nielsen HB, Pedersen OB, Gupta R, Lauritzen L, Licht TR (2017) Whole grain-rich diet reduces body weight and systemic low-grade inflammation without inducing major changes of the gut microbiome: a randomised cross-over trial. Gut 68(1):83–93. https://doi.org/10.1136/gutjnl-2017-314786
Rodríguez JM, Murphy K, Stanton C et al (2015) The composition of the gut microbiota throughout life, with an emphasis on early life. Mi-crobEcol Health Dis 26(10):26050. https://doi.org/10.3402/mehd.v26.26050
Roman C, Solh T, Broadhurst M (2017) Infectious diarrhea. Physician Assist Clin 2(2):229–245
Rossi M, Bot A (2013) The Th17 cell population and the immune homeostasis of the gastrointestinal tract. Int Rev Immunol 32(5–6):471–474. https://doi.org/10.3109/08830185.2013.843983
Round JL, Mazmanian SK (2010) Inducible Foxp3+ regulatory T-cell development by a commensal bacterium of the intestinal microbiota. Proc Natl Acad Sci U S A 107:12204–12209. https://doi.org/10.1073/pnas.0909122107
Rowan F, Docherty NG, Murphy M et al (2010) Desulfovibrio bacterial species are increased in ulcerative colitis. Dis Colon Rectum 53(11):1530–1536. https://doi.org/10.1007/DCR.0b013e3181f1e620
Rubin DC, Shaker A, Levin MS (2012) Chronic intestinal inflammation: inflammatory bowel disease and colitis-associated colon cancer. Front Immunol 3:107. https://doi.org/10.3389/fimmu.2012.00107
Schuijt TJ, Lankelma JM, Scicluna BP et al (2016) The gut microbiota plays a protective role in the host defence against pneumococcal pneumonia. Gut 65(4):575–583. https://doi.org/10.1136/gutjnl-2015-309728
Schwabe RF, Wang TC (2012) Cancer-bacteria deliver a genotoxic hit. Science 338:52–53. https://doi.org/10.1126/science.1229905
Schwiertz A, Taras D, Schafer K, Beijer S, Bos NA, Donus C, Hardt PD (2010) Microbiota and SCFA in lean and overweight healthy subjects. Obesity (Silver Spring) 18:190–195. https://doi.org/10.1038/oby.2009.167
Scott NA, Andrusaite A, Andersen P, Lawson M, Alcon-Giner C, Leclaire C, Caim S, Le Gall G, Shaw T, Connolly JPR et al (2018) Antibiotics induce sustained dysregulation of intestinal T cell immunity by perturbing macrophage homeostasis. Sci Transl Med 10:eaao4755. https://doi.org/10.1126/scitranslmed.aao4755
Sears CL (2009) Enterotoxigenic Bacteroides fragilis: a rogue among symbiotes. Clin Microbiol Rev 22:349–369. https://doi.org/10.1128/CMR.00053-08
Senghor B, Sokhna C, Ruimy R, Lagier JC (2018) Gut microbiota diversity according to dietary habits and geographical provenance. Human Microbiome Journal 7:1–9. https://doi.org/10.1016/j.humic.2018.01.001
Sheehan D, Moran C, Shanahan F (2015) The microbiota in inflammatory bowel disease. J Gastroenterol 50(5):495–507. https://doi.org/10.1007/s00535-015-1064-1
Slack E et al (2009) Innate and adaptive immunity cooperate flexibly to maintain host-microbiota mutualism. Science 325:617–620. https://doi.org/10.1126/science.1172747
Smith PM, Howitt MR, Panikov N, Michaud M, Gallini CA, Bohlooly-Y M et al (2013) The microbial metabolites, short-chain fatty acids, regulate colonic Treg cell homeostasis. Science 341:569–573. https://doi.org/10.1126/science.1241165
Sokol H, Lepage P, Seksik P, Dore J, Marteau P (2006) Temperature gradient gel electrophoresis of fecal 16S rRNA reveals active Escherichia coli in the microbiota of patients with ulcerative colitis. J Clin Microbiol 44:3172–3177. https://doi.org/10.1128/JCM.02600-05
Sokol H, Pigneur B, Watterlot L et al (2008) Faecalibacterium prausnitzii is an anti-inflammatory commensal bacterium identified by gut microbiota analysis of Crohn’s disease patients. Proc Natl Acad Sci U S A 105(43):16731–16736. https://doi.org/10.1073/pnas.0804812105
Sonnenberg GF, Artis D (2012) Innate lymphoid cell interactions with microbiota: implications for intestinal health and disease. Immunity 37:601–610. https://doi.org/10.1016/j.immuni.2012.10.003
Spencer MD, Hamp TJ, Reid RW, Fischer LM, Zeisel SH, Fodor AA (2011) Association between composition of the human gastrointestinal microbiome and development of fatty liver with choline deficiency. Gastroenterology 140(3):976–986. https://doi.org/10.1053/j.gastro.2010.11.049
Szablewski L (2018) Human gut microbiota in health and Alzheimer’s disease. J Alzheimers Dis 62(2):549–560. https://doi.org/10.3233/JAD-170908
Takahashi K, Nishida A, Fujimoto T et al (2016) Reduced abundance of butyrate-producing bacteria species in the fecal microbial community in Crohn’s disease. Digestion 93(1):59–65. https://doi.org/10.1159/000441768
Tap J, Derrien M, Törnblom H, Brazeilles R, Cools-Portier S, Doré J, Störsrud S, Le Nevé B, Öhman L, Simrén M (2017) Identification of an intestinal microbiota signature associated with severity of irritable bowel syndrome. Gastroenterology 152(1):111–123.e8. https://doi.org/10.1053/j.gastro.2016.09.049
Taylor EV, Herman KM, Ailes EC, Fitzgerald C, Yoder JS, Mahon BE, Tauxe RV (2013) Common source outbreaks of campylobacter infection in the USA, 1997-2008. Epidemiol Infect 141(5):987–996. https://doi.org/10.1017/S0950268812001744
Thangaraju M, Cresci GA, Liu K, Ananth S, Gnanaprakasam JP, Browning DD et al (2009) GPR109A is a g-protein–coupled receptor for the bacterial fermentation product butyrate and functions as a tumor suppressor in colon. Cancer Res 69:2826–2832. https://doi.org/10.1158/0008-5472.CAN-08-4466
Tian J, Lin X, Zhou W, Xu J (2003) Hydroxyethyl starch inhibits NF-kappaB activation and prevents the expression of inflammatory mediators in endotoxic rats. Ann Clin Lab Sci 33:451–458
Tlaskova-Hogenova H, Stepankova R, Hudcovic T et al (2004) Commensal bacteria (normal microflora), mucosal immunity and chronic inflammatory and autoimmune diseases. Immunol Lett 93:97–108. https://doi.org/10.1016/j.imlet.2004.02.005
Tolhurst G, Heffron H, Lam YS, Parker HE, Habib AM, Diakogiannaki E, Cameron J, Grosse J, Reimann F, Gribble FM (2012) Short-chain fatty acids stimulate glucagon-like peptide-1 secretion via the G-protein-coupled receptor FFAR2. Diabetes 61(2):364–371. https://doi.org/10.2337/db11-1019
Tomasello G, Tralongo P, Damiani P, Sinagra E, Di Trapani B, Zeenny MN et al (2014) Dismicrobism in inflammatory bowel disease and colorectal cancer: changes in response of colocytes. World J Gastroenterol 20:18121–18130. https://doi.org/10.3748/wjg.v20.i48.18121
Toprak NU, Yagci A, Gulluoglu BM et al (2006) A possible role of Bacteroides fragilis enterotoxin in the aetiology of colorectal cancer. Clin Microbiol Infect 12:782–786. https://doi.org/10.1111/j.1469-0691.2006.01494.x
Tunaru S, Kero J, Schaub A, Wufka C, Blaukat A, Pfeffer K et al (2003) PUMAG and HM74 are receptors for nicotinic acid and mediate its anti-lipolytic effect. Nat Med 9:352–355. https://doi.org/10.1038/nm824
Turnbaugh PJ, Ley RE, Mahowald MA, Magrini V, Mardis ER, Gordon JI (2006) An obesity-associated gut microbiome with increased capacity for energy harvest. Nature 444:1027e31. https://doi.org/10.1038/nature05414
Turnbaugh PJ et al (2009) A core gut microbiome in obese and lean twins. Nature 457:480–484. https://doi.org/10.1038/nature07540
Uronis JM, Muhlbauer M, Herfarth HH et al (2009) Modulation of the intestinal microbiota alters colitis-associated colorectal cancer susceptibility. PLoS One 4:e6026. https://doi.org/10.1371/journal.pone.0006026
van Wijk F, Cheroutre H (2009) Intestinal T cells: facing the mucosal immune dilemma with synergy and diversity. Semin Immunol 21:130–138. https://doi.org/10.1016/j.smim.2009.03.003
Velagapudi VR, Hezaveh R, Reigstad CS, Gopalacharyulu P, Yetukuri L, Islam S, Felin J, Perkins R, Borén J, Oresic M, Bäckhed F (2010) The gut microbiota modulates host energy and lipid metabolism in mice. J Lipid Res 51(5):1101–1112. https://doi.org/10.1194/jlr.M002774
Velikonja A, Lipoglavšek L, Zorec M, Orel R, Avguštin G (2019) Alterations in gut microbiota composition and metabolic parameters after dietary intervention with barley beta glucans in patients with high risk for metabolic syndrome development. Anaerobe 55:67–77. https://doi.org/10.1016/j.anaerobe.2018.11.002
Walker AW, Sanderson JD, Churcher C et al (2011) High-throughput clone library analysis of the mucosa-associated microbiota reveals dysbiosis and differences between inflamed and noninflamed regions of the intestine in inflammatory bowel disease. BMC Microbiol 11:7. https://doi.org/10.1186/1471-2180-11-7
Wilson JC, Furlano RI, Jick SS, Meier CR (2016) Inflammatory bowel disease and the risk of autoimmune diseases. J Crohns Colitis 10:186–193. https://doi.org/10.1093/ecco-jcc/jjv193
Wong SH, Ng SC (2013) What can we learn from inflammatory bowel disease in developing countries? Curr Gastroenterol Rep 15:313. https://doi.org/10.1007/s11894-013-0313-9
Wostmann BS, Larkin C, Moriarty A, Bruckner-Kardoss E (1983) Dietary intake, energy metabolism, and excretory losses of adult male germfree Wistar rats. Lab Anim Sci 33:46–50. PMID: 6834773
Wu S, Rhee KJ, Albesiano E et al (2009) A human colonic commensal promotes colon tumorigenesis via activation of T helper type 17 T cell responses. Nat Med 15:1016–1022. https://doi.org/10.1038/nm.2015
Wu Y, Pan L, Shang QH, Ma XK, Long SF, Xu YT, Piao XS (2017) Effects of isomalto-oligosaccharides as potential prebiotics on performance, immune function and gut microbiota in weaned pigs. Anim Feed Sci Technol 230:126–135. https://doi.org/10.1016/j.anifeedsci.2017.05.013
Xie Z, Huang G, Wang Z, Luo S, Zheng P, Zhou Z (2018) Epigenetic regulation of toll-like receptors and its roles in type 1 diabetes. J Mol Med 96:741–751. https://doi.org/10.1007/s00109-018-1660-7
Yen D, Cheung J, Scheerens H, Poulet F, McClanahan T, McKenzie B et al (2006) IL-23 is essential for T cell-mediated colitis and promotes inflammation via IL-17 and IL-6. J Clin Invest 116:1310–1316. https://doi.org/10.1172/JCI21404
Yu J et al (2017) Metagenomic analysis of faecal microbiome as a tool towards targeted non-invasive biomarkers for colorectal cancer. Gut 66:70–78. https://doi.org/10.1136/gutjnl-2015-309800
Zeng J, Song M, Jia T, Gao H, Zhang R, Jiang J (2019) Immunomodulatory influences of sialylated lactuloses in mice. Biochem Biophys Res Commun 514(2):351–357. https://doi.org/10.1016/j.bbrc.2019.04.157
Zhang Y, Zhou L, Bao YL, Wu Y, Yu CL, Huang YX et al (2010) Butyrate induces cell apoptosis through activation of JNK MAP kinase pathway in human colon cancer RKO cells. Chem Biol Interact 185:174–181. https://doi.org/10.1016/j.cbi.2010.03.035
Zinkevich VV, Beech IB (2000) Screening of sulfate-reducing bacteria in colonoscopy samples from healthy and colitic human gut mucosa. FEMS Microbiol Ecol 34(2):147–155. https://doi.org/10.1111/j.1574-6941.2000.tb00764.x
Acknowledgments
Prakash Narayana Reddy thanks the INSPIRE division of the Department of Science and Technology, Government of India, for awarding the INSPIRE Faculty award and research grant (DST/INSPIRE/04/2017/000565). The authors thank the management and administration of Vignan’s University and Krishna University for providing the necessary facilities during the preparation of this article.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Ethics declarations
Authors declare no conflict of interests.
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Phani, P., Kolla, H.B., Bramhachari, P.V., Reddy, P.N. (2023). Role of Gut Microbiome Composition in Shaping Host Immune System Development and Health. In: Veera Bramhachari, P. (eds) Human Microbiome in Health, Disease, and Therapy. Springer, Singapore. https://doi.org/10.1007/978-981-99-5114-7_3
Download citation
DOI: https://doi.org/10.1007/978-981-99-5114-7_3
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-99-5113-0
Online ISBN: 978-981-99-5114-7
eBook Packages: MedicineMedicine (R0)