Abstract
The notion of having a psychiatric disorder in at least 90% of suicides cannot be supported by available evidence in Bangladesh. Although the rate is lower, the health system is not adequate and even not prepared to deal with suicide and self-harm behavior in the country. Due to being categorized as a criminal offense, persons with suicidal behavior are being avoided by private hospitals while public hospitals literally neglect the psychological care demand in the country. There is inadequacy and inequitable distribution of psychiatrists, psychologists, and psychiatric social workers. Additionally, there is no notable formal training on suicide prevention for any category of service providers. There are only two suicide prevention clinics in Bangladesh that are yet to get momentum due to poor awareness, high stigma, and low suicide literacy. There is no alternative to extending psychiatric services, raising awareness about suicide prevention, urgent attention of policymakers, and responsible authorities to address the service care of patients and their family members with suicide and self-harm behavior. This chapter discusses the psychiatric morbidity among suicides and the current status of psychiatric services provided to the incumbents in Bangladesh.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Suicide is a global public health issue that is not an exception for Bangladesh (World Health Organization, 2021). In 2019, about 703,000 people died by suicide in the world; 77% of the suicides happened in low- and middle-income countries (LMICs) (World Health Organization, 2021). It is still mysterious to know the suicide pathway in a definitive fashion. Suicide is an outcome of a complex interaction between several factors like gene-environment interaction, proximal–distal factor interaction, and biopsychosocial interaction (Zalsman et al., 2016; World Health Organization, 2014). Among several factors, the psychiatric disorder has been considered as an important risk factor for suicide across the world with some variations in rate (Zalsman et al., 2016; Cho et al., 2016). Current evidence supports that about 90% of suicides have at least one psychiatric illness in Western countries (Zalsman et al., 2016). However, recent repeated autopsy studies from eastern countries like China, India, and Bangladesh revealed a lower rate of mental illness among suicides (Zalsman et al., 2016; Cho et al., 2016; Milner et al., 2013; Arafat, Menon, et al., 2022). One systematic review concluded that the prevalence of mental illness is possibly lower in LMICs (Knipe et al., 2019). Another recent meta-analysis replicates the lower prevalence of the depressive disorder in suicides and suicidal behavior in South Asian regional countries (Arafat, Saleem, et al., 2022). It revealed the pooled prevalence of depression was 37.3% in suicide and 32.7% in non-fatal attempts (Arafat, Saleem, et al., 2022).
Bangladesh is an LMIC located in South Asia with potential economic growth in recent decades. It has an area of 147,570 square kilometers and about 171 million populations substantiating it as one of the highest densely populated states in the world (World Population Review, 2022). Among the population, more than 90% are Muslims. Suicide is prohibited in Islam and it is considered as a criminal offense in the country (Arafat, Martheonis et al., 2022). Bangladesh is enjoying a demographic dividend from its huge young population that makes its prolific economic growth despite huge corruption and money laundering to Western countries. The country is lifted from low-income to lower-middle-income groups in recent years. At the same time, it is facing a double burden of diseases with a gradual inclination to non-communicable diseases. Currently, more than 60% of the disease burden is incurred by non-communicable diseases (Ahmed, 2018). Mental disorders are one of the major burdens after cardiovascular diseases, diabetes mellitus, chronic respiratory diseases, and malignancy (Ahmed, 2018). The latest nation-wide mental health survey of Bangladesh conducted by the national institute of mental health (NIMH), the Ministry of Health, and World Health Organization (WHO) in 2018–2019 revealed that the prevalence of psychiatric disorders was 16.8% (95% CI 15.5–18.2) which was 16.1% in 2003–2005 (World Health Organization, 2019b). Among the disorders, the highest prevalence was noted for depression (6.7%), followed by anxiety disorders (4.5%), somatic symptoms and related disorders (2.1%), and psychotic disorders (1%) (World Health Organization, 2019b). The study identified a treatment gap of 92.3% among the adult populations of Bangladesh (World Health Organization, 2019b). A significant portion of the patients visits traditional healers (Samans, Kabiraz, etc.) and non-medical health professionals before reaching the mental health professionals (Giasuddin et al., 2012; Nuri et al., 2018). Studies identified that less than 30% of the patients visit mental health professionals at their first contact (Giasuddin et al., 2012; Nuri et al., 2018). Another important aspect of health services should be mentioned regarding the high out-of-pocket expense for the treatment of mental illness in Bangladesh. I couldn’t find any specific study on the out-of-pocket expense of psychiatric disorders in the country. However, available studies identified the out-of-pocket expense on overall health revealed more than 70% of the expenses are incurred as out-of-pocket expenses in Bangladesh (The World Bank, 2022). Being a densely populated country with a low health budget, double disease burden, low mental health literacy, high stigma, and attribution of mental illness to super-natural power like jinn, overall mental health care is grossly under-prioritized especially for the community people of Bangladesh. As a result, the association between suicide and psychiatric disorders is yet to be discovered adequately.
2 Epidemiology of Suicide in Bangladesh
We discuss the details of the epidemiology of suicide in Chap. 1 of this book (Kabir et al., 2023). We mention here some details to maintain the context. At the same time, I was careful to reduce the repetitions. Suicidal behavior is an under-researched problem in Bangladesh. The country still lacks a suicide surveillance system and any national suicide prevention initiative (Arafat, 2017). The rate of suicide rate varies among the empirical studies and WHO reports (Arafat, 2019a). The latest WHO report revealed the suicide rate was 3.9 per 100,000 population in 2019 which was 6.1 in 2016, 7.8 in 2012, and 7.8 per 100,000 in 2000. The total number of suicides was 5998, 9544, and 10,167 in 2019, 2016, and 2012, respectively (WHO, 2014, 2019c, 2021). The statistics indicate a decline in suicide rates and numbers in the last decade. However, the empirical studies revealed different rates in regard to the WHO estimates and even vary among the studies (Arafat, 2019a). Nation-wide studies are warranted to determine the prevalence rates. Additionally, there is an extreme dearth of research estimating the prevalence rate of self-harm in the country.
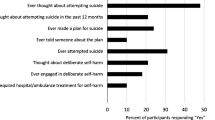
The first nation-wide epidemiological study among adolescents and youths on suicidal behavior was completed in 2021 by NIMH (Dhaka), WHO (Bangladesh), and Non-communicable diseases control, Ministry of Health, Bangladesh (NIMH, 2021). The study utilized the adapted Bangla WHO multisite intervention study on suicidal behaviors SUPRE-MISS among 1744 participants aged between 10 and 24 years. It found the rate of suicidal ideation, planning, and attempt was 4.7%, 1.5%, and 1.5%, respectively. The rate was significantly higher among females and urban populations. Several aspects should be considered while considering the rates such as sources of data, concerns of under-reporting and misclassification, and methods of data recording in the context of countries like Bangladesh.
Hanging is the commonest method of suicide followed by poisoning (Arafat, Ali et al., 2021). Females die more than males and the majority of the suicides occur among persons under the age of 30 years (Arafat, 2019b). Familial discord, marital disharmony, psychiatric disorders, immediate life events, past suicide attempts, sexual violence, unemployment, and social isolation were identified as the major risk factors for suicide in Bangladesh (Arafat, 2017, 2019a; Arafat, Mohit, Mullick, Khan et al., 2021; Feroz et al., 2012, Reza et al., 2013; Salam et al., 2017; Shahnaz et al., 2017). However, social factors have a dominant role over clinical factors in Bangladesh (Arafat, Khan, et al., 2021). One analysis identified that if the life events could be prevented about 86% of suicides would be prevented which was about 50% for psychiatric disorders (Arafat, Khan, et al., 2021).
3 Psychiatric Disorders in Suicide and Self-Harm in Bangladesh
3.1 Psychiatric Disorder in Suicide in Bangladesh
The assessment of the prevalence and role of psychiatric disorders in suicide and suicidal behavior is grossly under-studied in Bangladesh. Only one case–control psychological autopsy study was conducted in an urban setting, i.e. Dhaka city, the capital of the country which was published in 2020 (Arafat, Mohit, Mullick, Kabir, et al., 2021). The study identified that 61% of the suicides had at least one mental illness. Among them, the major depressive disorder was the most prevalent diagnosis (44%), followed by personality disorder (14%), amphetamine (yaba) use disorder (9%), acute stress disorder (4%), adjustment disorder (3%), and schizophrenia (1%) (Arafat, Mohit, Mullick, Kabir, et al., 2021). The study also identified co-morbidities of psychiatric disorders, personality disorders, and substance use disorders among suicide deceased. Among the suicides, only 13% were previously diagnosed and being treated and only one suicide with depression was regular and compliant with the psychiatrist. Among the 13 previously identified cases, five had depressive disorder, seven had substance use disorder, and the rest one was psychotic (Arafat, Mohit, Mullick, Kabir, et al., 2021). The study identified the service gap was 87%. It also revealed that only 14% had past suicidal attempts (Arafat, Mohit, Mullick, Kabir, et al., 2021). This is perhaps the only systematized attempt assessing the psychiatric disorders among suicides where the psychiatric diagnoses were assessed by Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I) (First et al., 1996) and Structured Clinical Interview for DSM-IV Personality Disorders (SCID-II) (First et al., 1994). A different analysis of the same data by comparing suicides with and without mental disorders revealed some additional interesting findings (Arafat, Mohit, Mullick, Khan, et al., 2021). Mental illness was significantly higher among the suicides that happened in adulthoods than adolescents, males than females, and socially isolated persons than whom were living with family (Arafat, Mohit, Mullick, Khan, et al., 2021). The analysis indicates that 70% of the depressive disorder cases were males, 70% of the adults had psychiatric disorders while it was 36% among suicides by adolescents. Significantly higher age was noted among the suicides with mental disorders than suicides without mental illness. All the suicides with acute stress disorder were developed among females in response to sexual harassment (Arafat, Mohit, Mullick, Khan, et al., 2021). Interestingly, psychiatric disorders were significantly higher in the middle and upper socio-economic class and persons living in a parental house or had house ownership (Arafat, Mohit, Mullick, Khan, et al., 2021). In a summary, psychiatric disorders were more common among suicides of adult age, males, living alone, and having a middle- and upper-class environment. The findings clearly indicate a lower rate of mental illness among the suicides in Bangladesh in comparison to the Western countries. Additionally, it drags our attention toward the social factors and life events like marital discord, familial disharmony, sexual harassment, and premarital and extramarital relationships in attributing and preventing suicides. However, poor mental health and suicide literacy could be important reasons for this low attribution.
3.2 Psychiatric Disorder in Self-Harm/Non-Fatal Attempt in Bangladesh
Assessment of psychiatric morbidity in suicidal behaviors has been poorly prioritized in Bangladesh. Available studies indicate the rate is 45–65% (Uddin et al., 2019; Islam et al., 2019; Roy et al., 2016; Reza et al., 2013; Qusar et al., 2009). A study of 51 patients with NSSI in Chattagram (Chittagong) revealed that 45% of the patients had psychiatric disorder which was assigned by clinical interviews conducted by a psychiatrist (Uddin et al., 2019). Among the disorders, the depressive disorder was found in 23.5%, followed by borderline personality disorder (BPD) (11.8%) and schizophrenia (5.9%) (Uddin et al., 2019). Another study at Comilla (Cumilla) medical college determined the prevalence of psychiatric disorders was 65% (Islam et al., 2019). Islam and his colleagues interviewed 120 patients with suicidal behavior through the Composite International Diagnostic Interview (CIDI) and diagnoses were assessed as per the DSM-5 classification (Islam et al., 2019). They identified BPD as the top most psychiatric morbidity which was found in 16.7% and depression was found in 7.5% of patients (Islam et al., 2019). In one study conducted at Rangpur Medical College in 2017 among 101 clinical patients who presented with non-fatal attempts were assessed for psychiatric morbidity where the diagnosis was assigned clinically by the Diagnostic and Statistical Manual of Mental Disorders (DSM-IV-TR) (American Psychiatric Association, 2000; Roy et al., 2016). The study revealed that 65% of the patients with non-fatal attempts had psychiatric disorders where depressive disorder was highest (18%), followed by conversion disorder (12%), psychotic disorder (12%), bipolar disorder (6%), and substance abuse disorder (4%) (Roy et al., 2016). Another case–control study published in 2013 assessed psychiatric morbidity by SCID-I in the rural part of Bangladesh (Chuadanga) among 113 respondents with suicidal behavior (Reza et al., 2013). The study revealed that psychiatric morbidity was 58.5% (Reza et al., 2013). However, it didn’t categorize the respondents based on suicidal behavior, i.e. how many were suicides and how many had only non-fatal attempts. Additionally, it was not demarcated whether the interview was conducted by a psychiatrist or any other well-trained clinician (Reza et al., 2013). A study was conducted in 2008 on 44 admitted patients in the intensive care unit (ICU) after a non-fatal attempt assessed psychiatric morbidity by clinical interview and diagnoses were confirmed as per DSM-IV criteria (Qusar et al., 2009). It identified that about 59% (n = 26) of the participants had psychiatric disorders; among them, the depressive disorder was the highest morbidity and was identified in 25% of the cases followed by personality disorder (9.1%), psychosis (9.1%), obsessive–compulsive disorder (4.5%), substance-related disorder (4.5%), and acute stress disorder (4.5%) (Qusar et al., 2009). It is important to note that these 44 cases are supposed to have severe intent and clinical outcomes as they were collected after a life-threatening attempt and admitted in ICU. Therefore, the rate of morbidity among less severe attempters may not be the same. It is important to note that prevalence has been calculated irrespective of the assessment of intent whether suicidal or non-suicidal self-harm. Interestingly, the studies revealed nearly a low prevalence (45%, 58.5% vs. 59%, and 65%) both in community (Reza et al., 2013) and clinical sample (Uddin et al., 2019; Islam et al., 2019; Roy et al., 2016; Qusar et al., 2009).
4 Psychiatric Services for Suicide and Self-Harm
Whatever the service burden, there is an extreme insufficiency and inadequate readiness for the provision of evidence-based services for suicide and self-harm in Bangladesh. The autopsy study identified the unidentified mental health need was 87% (Arafat, Mohit, Mullick, Kabir, et al., 2021). The latest mental health survey conducted in 2018–2019 identified the treatment gap of psychiatric disorder as 92.3% (World Health Organization, 2019a). After the service gaps, let us check the service delivery pattern of the health system in Bangladesh. The criminal legal status creates an additional burden for services provision as well as services receiving for non-fatal attempts. As the patients with self-harm and suicidal behavior have been considered as police case and a seal is stamped on the hospital file of the patients mentioning “police case”. This stamping is supposed to create a further psychological burden in addition to the primary distress. Private hospitals are reluctant to provide services and usually they refer such patients to the public hospitals to avoid unwanted legal hazards. Usually such patients are treated in the public hospitals starting from Upazila Health Complex to District (Sadar hospital in Bangla) and then medical college hospitals. These hospitals have a separate corner for stomach wash for patients with poisoning and medication overdose. After that, they are being grossly neglected as most of the cases are kept on the floor of the hospital veranda. In the general hospital settings, the patients with suicidal behavior have been treated by medicine specialists in the majority of the situations. There is almost no privacy and psychological support and even such patients are not being referred to the psychiatrist for evaluation of suicidal intent, mental health status, and tailored need of psychological supports. Due to these reasons, patients with NSSI do not take medical advice unless any emergency arises. If we look into available human resources for services provision, we can see that there are about 270 psychiatrists in Bangladesh, and every year about 10–20 psychiatrists are coming out including the MCPS, FCPS, MD Psychiatry, and MD child and adolescent psychiatry (Hasan et al., 2021; WHO, 2020). The country pertains 0.17 psychiatrists per 100,000 population, 0.43 mental health nurses, and 0.35 psychologist per 100,000 population (WHO, 2020). If we calculate the proportion with the prevalence of the latest national mental health survey, I find that only one psychiatrist is available for 16,800 patients. The situation is further complicated by the inequitable distribution of mental health professionals. Most of the psychiatrists are located in the city and the majority of the psychiatrists are living in Dhaka (capital city). Only about 0.5% of the total country budget has been allocated for mental health and the total mental health expenditure is about 9 Taka (0.1 USD) for an individual (WHO, 2022). Only two specialized services centers have been identified in the country; both of them are located in Dhaka city. The first Suicide Prevention Clinic (SPC) was started at the psychiatry department of Bangabandhu Sheikh Mujib Medical University (BSMMU). It was started in September 2016 aiming at providing a specialized service to the patients with active suicidal ideation or previous suicide/self-harm attempts. The clinic works at weekly two hourly basis outpatient department (OPD) services, only on Saturday from 11.00 a.m. to 1.00 p.m. (Arafat, 2018). Prof. Mohsin Ali Shah, Professor of psychiatry, started the services of milestone in the country. The clinic maintains follow-up by making phone calls to the service receivers to ascertain whether attempts are made. Reports from the clinic revealed that about two-thirds of the patients were aged under 25 years, 70% were females, and depressive disorder was the most common psychiatric morbidity (Shah et al., 2018).
The second SPC was started at the department of psychiatry of Enam Medical College and Hospital (EMCH), a private medical college in Dhaka by Dr. S. M. Yasir Arafat, a disciple of Prof. Mohsin Ali Shah. The service hour is extended from 9 a.m. to 5 p.m. on working days. It is started in October 2021. Any other specialized clinical services for suicide prevention have not been identified in Bangladesh. The visited patients at the SPC of BSMMU are mostly referred by the psychiatry OPD while the SPC of EMCH gets by self-report due to some awareness materials like banners containing basic information on suicide and self-harm. A mental health OPD is available at 72 hospitals country-wide (WHO, 2022). However, it is questionable whether any mental health specialist is available in all the centers except the medical colleges. Even, general physicians having training in mental health would be difficult to find out in every center at the primary care level of Bangladesh. Therefore, it is unexpected that these centers would be able to handle suicide and suicidal behavior efficiently. It is important to note that none of the persons in the SPCs has any formal training on suicide and suicide prevention except for their academic background.
5 Current Challenges and Way Forward for Suicide Prevention
Detailed suicide prevention activities have been discussed in Chap. 9 of this book by Hoque (2023). Here, I tried to mention the prevention activities closely associated with mental health. Criminal legal status, low-quality data, inadequate services, high out-of-pocket expense, low mental health and suicide literacy, low research, lack of national databases and suicide surveillance system, non-existence of inter-sectoral collaboration, inadequate funds, unavailability of professional training, and lack of national suicide prevention strategies are the potential challenges of suicide and self-harm prevention in Bangladesh. Self-harm behavior is a covert problem in Bangladesh. Usually, the young child(ren) hide(s) it from their parents. Parents are not aware in such a stage to consider it as a mental health issue due to high-level stigma and low mental health literacy. There is an extreme dearth of health services having adequate training and expertise to deal with the problems. The problem is yet to get the political attention to have any health policy and visible prevention activities. The mental health act of Bangladesh was passed in 2018 and contains nothing about the suicide prevention (Mental Health Act, 2018; Khan et al., 2020).
There is no alternative to raising awareness among the services providers first and then among the general population indicating that suicide is preventable and past attempt is the strongest risk factor for suicide (WHO, 2014). Adequate mental health services should be ensured throughout the country with proper psychological supports in a readily available manner. Periodic training for human resources working in suicide prevention should be ensured. General physicians should be adequately trained to identify the warning signs of suicide, depression, and substance abuse (Arafat and Kabir, 2017). Enduring collaboration is necessary between the mental health professionals, media personnel, crisis service centers, and forensic experts. Decriminalization of suicide would help people to disclose the suicidal behavior and hospitals to provide necessary services to the needy people (Soron, 2019). Initiating the school mental health programs and ensuring the gate-keeper training of teachers to identify the signs of depression, substance misuse, and suicidal behavior could be a potential area in the country (Zalsman et al., 2016). There is a dire need for research in suicide and suicide prevention to identify the role of psychiatric disorders in suicide as well as to test any culture-sensitive suicide prevention strategies.
6 Conclusions
Mental health and mental illness are closely associated with suicide and suicidal behavior in Bangladesh likewise the other parts of the world even though the available rate is lower when compared to Western countries. However, both the mental health care providers and the service receivers are not ready in either way to deal with suicidal behavior with psychiatric care. Low mental health and suicide literacy, high stigma toward suicide and mental health services, lack of service outlets, and awareness could be the potential factors. There is no alternative to raising awareness about suicide prevention among all the stakeholders in the country. Urgent attention of policymakers and responsible authorities is warranted to address the service care of patients and their family members with suicide and self-harm behavior as well as to train the service providers. Academic institutions should prioritize suicide prevention research to find out the risk factors for suicide in the country. And finally, the implication of the research findings into the policy should be started in Bangladesh.
References
Ahmed. (2018). Non-communicable diseases and their prevention: A global, regional and Bangladesh perspective. National Bulletin of Public Health (NBPH), 1(3), 2–4.
American Psychiatric Association. (2000). Diagnostic and statistical manual of mental disorders. 4th ed (text revision). Washington, DC: American Psychiatric Association.
Arafat, S. M. Y. (2017). Suicide in Bangladesh: A mini review. Journal of Behavioral Health, 6(1), 66–69. https://doi.org/10.5455/jbh.20160904090206
Arafat, S. M. Y. (2018). Suicide prevention activities in Bangladesh. Asian Journal of Psychiatry, 36, 38. https://doi.org/10.1016/j.ajp.2018.06.009
Arafat, S. M. Y. (2019a). Current challenges of suicide and future directions of management in Bangladesh: A systematic review. Global Psychiatry, 2(1), 9– 20. https://doi.org/10.2478/gp-2019-0001
Arafat, S. M. Y. (2019b). Females are dying more than males by suicide in Bangladesh. Asian Journal of Psychiatry, 40, 124– 125. https://doi.org/10.1016/j.ajp.2018.10.014
Arafat, S., Ali, S. A., Menon, V., Hussain, F., Ansari, D. S., Baminiwatta, A., Saleem, T., Singh, R., Varadharajan, N., Biyyala, D., Kar, S. K., & Khan, M. M. (2021). Suicide methods in South Asia over two decades (2001-2020). The International Journal of Social Psychiatry, 67(7), 920–934. https://doi.org/10.1177/00207640211015700
Arafat, S. Y., & Kabir, R. (2017). Suicide prevention strategies: Which one to consider? South East Asia Journal of Public Health, 7(1), 1–5. https://doi.org/10.3329/seajph.v7i1.34671
Arafat, S., Khan, M., Knipe, D., & Khan, M. M. (2021). Population attributable fractions of clinical and social risk factors for suicide in Bangladesh: Finding from a case-control psychological autopsy study. Brain and Behavior, 11(12), e2409. https://doi.org/10.1002/brb3.2409
Arafat, S. M. Y., Marthoenis, M., Khan, M. M., & Rezaeian, M. (2022). Association between suicide rate and human development index, income, and the political system in 46 Muslim-majority countries: An ecological study. European Journal of Investigation in Health, Psychology and Education, 12(7), 754–764. https://doi.org/10.3390/ejihpe12070055
Arafat, S., Menon, V., Varadharajan, N., & Kar, S. K. (2022). Psychological Autopsy Studies of Suicide in South East Asia. Indian Journal of Psychological Medicine, 44(1), 4–9. https://doi.org/10.1177/02537176211033643
Arafat, S., Mohit, M. A., Mullick, M., Kabir, R., & Khan, M. M. (2021). Risk factors for suicide in Bangladesh: Case-control psychological autopsy study. BJPsych Open, 7(1), e18. https://doi.org/10.1192/bjo.2020.152
Arafat, S., Mohit, M. A., Mullick, M., Khan, M., & Khan, M. M. (2021). Suicide with and without mental disorders: Findings from psychological autopsy study in Bangladesh. Asian Journal of Psychiatry, 61, 102690. https://doi.org/10.1016/j.ajp.2021.102690
Arafat, S. M. Y., Saleem, T., Menon, V., Ali, S. A.-e.-Z., Baminiwatta, A., Kar, S. K., Akter, H., & Singh, R. (2022). Depression and suicidal behavior in South Asia: A systematic review and meta-analysis. Global Mental Health, 9, 181–192. https://doi.org/10.1017/gmh.2022.20
Cho, S. E., Na, K. S., Cho, S. J., Im, J. S., & Kang, S. G. (2016). Geographical and temporal variations in the prevalence of mental disorders in suicide: Systematic review and meta-analysis. Journal of Affective Disorders, 190, 704–713. https://doi.org/10.1016/j.jad.2015.11.008
Feroz, A., Islam, S. N., Reza, S., Rahman, A. M., Sen, J., Mowla, M., & Rahman, M. R. (2012). A community survey on the prevalence of suicidal attempts and deaths in a selected rural area of Bangladesh. Journal of Medicine, 13(1), 3–9. https://doi.org/10.3329/jom.v13i1.10042
First, M. B., Spitzer, R. L., Gibbon, M., & Williams, J. B. (1996). Structured clinical interview for DSM-IV Axis I disorders. New York: Biometrics Research Department, New York State Psychiatric Institute.
First, M. B., Spitzer, R. L., Gibbon, M., Williams, J. B., & Benjamin, L. (1994). Structured clinical interview for DSM-IV Axis II personality disorders. New York: Biometrics Research Department, New York State Psychiatric Institute.
Giasuddin, N. A., Chowdhury, N. F., Hashimoto, N., Fujisawa, D., &Waheed, S. (2012). Pathways to psychiatric care in Bangladesh. Social Psychiatry and Psychiatric Epidemiology, 47(1), 129–136. https://doi.org/10.1007/s00127-010-0315-y
Hasan, M. T., Anwar, T., Christopher, E., Hossain, S., Hossain, M. M., Koly, K. N., Saif-Ur-Rahman, K. M., Ahmed, H. U., Arman, N., & Hossain, S. W. (2021). The current state of mental healthcare in Bangladesh: Part 1—An updated country profile. BJPsych International, 18(4), 78–82. https://doi.org/10.1192/bji.2021.41
Hoque, M. B. (2023). Suicide prevention in Bangladesh: Current status and way forward. In: Arafat, S. Y. & Khan, M. M. (eds) Suicide in Bangladesh. Cham: Springer.
Islam, M. S., Mamun, S. A. A., Haque, M. M., Mohammad Khan, N., Rashid, M. H. A., Sinha, R. K., Abedin, M. F., & Uddin, M. N. (2019). Psychiatric disorders among suicidal behavior patients attending mental health facilities: A descriptive cross sectional study. Journal of Bangladesh College of Physicians and Surgeons, 37(3), 130–134. https://doi.org/10.3329/jbcps.v37i3.41735
Kabir, R., Hasan, M. R., & Arafat, S. M. Y. (2023). Epidemiology of suicide and data quality in Bangladesh. In S. Y. Arafat & M. M. Khan (Eds.), Suicide in Bangladesh (pp. 1–16). Springer. https://doi.org/10.1007/978-981-99-0289-7_1.
Khan, A. R., Arendse, N., & Ratele, K. (2020). Suicide prevention in Bangladesh: The current state and the way forward. Asian Social Work and Policy Review, 15(1), 15–23. https://doi.org/10.1111/aswp.12214
Knipe, D., Williams, A. J., Hannam-Swain, S., Upton, S., Brown, K., Bandara, P., Chang, S. S., & Kapur, N. (2019). Psychiatric morbidity and suicidal behaviour in low- and middle-income countries: A systematic review and meta-analysis. PLoS Medicine, 16(10), e1002905. https://doi.org/10.1371/journal.pmed.1002905
Mental Health Act. (2018). Bangladesh. [Online]. https://legislativediv.gov.bd/site/page/3c13bbde-76b4-41fc-89cab738dd04a0bb (accessed on December 12, 2018).
Milner, A., Sveticic, J., & De Leo, D. (2013). Suicide in the absence of mental disorder? A review of psychological autopsy studies across countries. The International Journal of Social Psychiatry, 59(6), 545–554. https://doi.org/10.1177/0020764012444259
National Institute of Mental Health. (2021). Epidemiology of suicide nad suicidal behavior among youth and adolescents in Bangladesh (Project Report).
Nuri, N. N., Sarker, M., Ahmed, H. U., Hossain, M. D., Beiersmann, C., & Jahn, A. (2018). Pathways to care of patients with mental health problems in Bangladesh. International Journal of Mental Health Systems, 12, 39. https://doi.org/10.1186/s13033-018-0218-y
Qusar, M. S., Morshed, N. M., Azad, M. A. K., Kader, M. A., Shams, S. F., Ahmed, M. F., Haque, M. M. M., Uddin, M. A., & Shahid, S. F. B. (2009). Psychiatric morbidity among suicide attempters who needed ICU intervention. Bangabandhu Sheikh Mujib Medical University Journal, 2(2), 73–77. https://doi.org/10.3329/bsmmuj.v2i2.4761
Reza, A. S., Feroz, A. H. M., Islam, S. N., Karim, M. N., Rabbani, M. G., Shah Alam, M., Rahman, M. M., Rahman, M. R., Ahmed, H. U., Bhowmik, A. D., Khan, M. Z. R., Sarkar, M., Alam, M. T., & Jalal Uddin, M. M. (2013). Risk factors of suicide and para suicide in rural Bangladesh. Journal of Medicine, 14(2), 123–129. https://doi.org/10.3329/jom.v14i2.19653
Roy, J., Al Adiluzzaman, M. A. F., Hasan, M. T., Roy, D. D., Qusar, M. S., Shah, M. M. A., & Arafat, S. Y. (2016). Socio-demographic profile and psychiatric morbidities of suicide attempters: a cross-sectional observation in a tertiary care hospital of Bangladesh. Bangladesh Journal of Psychiatry, 30(2), 36–40. https://doi.org/10.3329/bjpsy.v30i2.45363
Salam, S. S., Alonge, O., Islam, M. I., Hoque, D., Wadhwaniya, S., UlBaset, M. K., Mashreky, S. R., & El Arifeen, S. (2017). The burden of suicide in rural Bangladesh: Magnitude and risk factors. International Journal of Environmental Research and Public Health, 14(9), 1032. https://doi.org/10.3390/ijerph14091032
Shah, M., Sajib, M., & Arafat, S. (2018). Demography and risk factor of suicidal behavior in Bangladesh: A cross-sectional observation from patients attending a suicide prevention clinic of Bangladesh. Asian Journal of Psychiatry, 35, 4–5. https://doi.org/10.1016/j.ajp.2018.04.035
Shahnaz, A. , Bagley, C., Simkhada, P., & Kadri, S. (2017) Suicidal behaviour in Bangladesh: A scoping literature review and a proposed public health prevention model. Open Journal of Social Sciences, 5, 254–282. https://doi.org/10.4236/jss.2017.57016
Soron, T. R. (2019). Decriminalizing suicide in Bangladesh. Asian Journal of Psychiatry, 39, 91–92. https://doi.org/10.1016/j.ajp.2018.12.012
The World Bank. (2022). Out-of-pocket expenditure (% of current health expenditure)—Bangladesh. https://data.worldbank.org/indicator/SH.XPD.OOPC.CH.ZS?locations=BD (last accessed on September 21, 2022).
Uddin, M. G., Biswas, R. S. R., & Mamun, S. M. H. (2019). Sociodemographic profile and intention of deliberate self-harm among patients admitted in a tertiary care hospital, Chittagong, Bangladesh. Journal of the Scientific Society, 46(2), 53. https://doi.org/10.4103/jss.JSS_9_19
World Health Organization. (2014). Preventing suicide: A global imperative. https://apps.who.int/iris/handle/10665/131056 (accessed on July 15, 2022).
World Health Organization. (2019a). Minister of Health releases first findings of National Mental Health Survey. https://cdn.who.int/media/docs/default-source/searo/bangladesh/pdf-reports/cat-2/nimh-fact-sheet-5-11-19.pdf?sfvrsn=3e62d4b0_2 (last accessed date 12 July, 2022).
World Health Organization. (2019b). Minister of Health releases first findings of National Mental Health Survey. https://cdn.who.int/media/docs/default-source/searo/bangladesh/pdf-reports/cat-2/nimh-fact-sheet-5-11-19.pdf?sfvrsn=3e62d4b0_2 (accessed on September 20, 2022).
World Health Organization. (2019c). Suicide in the world. Global health estimates. https://apps.who.int/iris/bitstream/handle/10665/326948/WHO-MSD-MER-19.3-eng.pdf (accessed on July 15, 2022).
World Health Organization (2020). Bangladesh WHO special initiative for mental health situational assessment. WHO. https://cdn.who.int/media/docs/default-source/mental-health/special-initiative/who-special-initiative-country-report---bangladesh---2020_f746e0ca-8099-4d00-b126-fa338a06ca6e.pdf?sfvrsn=c2122a0e_7 (accessed on July 15, 2022).
World Health Organization. (2021). Suicide worldwide in 2019: Global health estimates. Geneva: WHO. https://www.who.int/publications/i/item/9789240026643 (accessed on 15 September 2021).
World Health Organization. (2022). Mental Health Atlas 2020 country profile: Bangladesh. https://www.who.int/publications/m/item/mental-health-atlas-bgd-2020-country-profile (accessed on July 15, 2022)
World Population Review. (2022). Bangladesh Population 2022 (Live). https://worldpopulationreview.com/countries/bangladesh-population (accessed on September 16, 2022)
Zalsman, G., Hawton, K., Wasserman, D., van Heeringen, K., Arensman, E., Sarchiapone, M., Carli, V., Höschl, C., Barzilay, R., Balazs, J., Purebl, G., Kahn, J. P., Sáiz, P. A., Lipsicas, C. B., Bobes, J., Cozman, D., Hegerl, U., & Zohar, J. (2016). Suicide prevention strategies revisited: 10-year systematic review. The Lancet Psychiatry, 3(7), 646–659. https://doi.org/10.1016/S2215-0366(16)30030-X
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Arafat, S.M.Y. (2023). Mental Health and Suicide in Bangladesh. In: Arafat, S.M.Y., Khan, M.M. (eds) Suicide in Bangladesh. New Perspectives in Behavioral & Health Sciences. Springer, Singapore. https://doi.org/10.1007/978-981-99-0289-7_3
Download citation
DOI: https://doi.org/10.1007/978-981-99-0289-7_3
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-99-0291-0
Online ISBN: 978-981-99-0289-7
eBook Packages: Behavioral Science and PsychologyBehavioral Science and Psychology (R0)