Abstract
Moyamoya disease (MMD) is a rare chronic cerebral ischemic disease with unknown etiology that shows characteristic angiographic features of intracranial collateral vessels. Revascularization surgery (RVS) is a well-known method for the augmentation of cerebral perfusion in MMD. Based on the surgical procedures, RVS for MMD is classified as direct, indirect, and combined. For RVS, there are many aspects to consider, such as age (pediatric vs. adult), surgical indication, and selection of surgical procedures (indirect vs. direct vs. combined). Along with these aspects, we analyzed and described the outcome of RVS in both pediatric and adult MMD in Korea with a review of pertinent literature.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Revascularization surgery (RVS) involves establishing a vascular connection between the brain and extracranial vessels or vascularized tissues for blood flow augmentation to the ischemic brain. RVS techniques for moyamoya disease (MMD) are classified into direct, indirect, and combined RVS procedures.
According to data from the National Health Insurance Service in South Korea, from 2008 to 2019, 18,056 patients were newly diagnosed with MMD [1, 2]. The number of newly diagnosed adult patients with MMD increased by 67.0% over the 11-year period, with 1,590 adult patients diagnosed with MMD in 2019. For adult MMD, the crude incidence in 2019 was calculated as 3.75 per 100,000 person-years, which increased by 76.9% over the 11-year period (Fig. 23.1) [1, 2]. The number of newly diagnosed pediatric patients with MMD decreased by 16.2% from 296 in 2008 to 248 in 2019. This is thought to be caused by a significant decrease in the birth rate; however, the crude incidence did not decrease as the detection rate increased. For pediatric MMD, the crude incidence in 2019 was calculated as 2.76 per 100,000 person-years, which increased by 11.1% over the 11-year period [1, 2].
The crude incidence of moyamoya disease (MMD) in Korea. The crude incidence of adult MMD in 2019 was calculated as 3.75 per 100,000 person-years, which increased by 76.9% throughout 2008–2019. For pediatric MMD, the crude incidence was 2.76 per 100,000 person-years in 2019, which increased by 11.1% from 2008
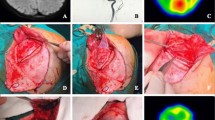
Regarding the treatment for MMD in Korea, the total number of RVS for adult MMD increased to 389 by 2012, and then slightly decreased to 364 in 2016. The number of direct RVS cases, including combined RVS cases, peaked at 266 in 2014 and then showed plateaus status to 2016. The proportion of cases in which indirect RVS was performed alone decreased from 62.5% in 2008 to 31.3% in 2016. (Fig. 23.2a) Meanwhile, RVS for pediatric MMD declined significantly over the 9-year period, with 399 and 313 operations performed in 2008 and 2016, respectively, although the number of direct RVS cases, including cases of combined RVS, increased steadily over the 9-year period (Fig. 23.2b) [1, 2].
The treatment for moyamoya disease (MMD) in Korea. (a) The total number of revascularization surgeries (RVS) for adult MMD increased to 389 by 2012 and then decreased to 364 in 2016. The number of direct RVS cases, including combined RVS cases, peaked in 2014 and then showed plateau status. The proportion of indirect RVS alone decreased from 62.5% in 2008 to 31.3% in 2016. (b) Operations for pediatric MMD declined significantly over the 9-year period, with 399 and 313 operations performed in 2008 and 2016, respectively
2 Procedure of RVS
Indirect RVS is the procedure of shifting the external carotid artery branches supplying vascularized tissue from the scalp to the surface of the ischemic brain for provoking spontaneous leptomeningeal anastomoses [3, 4]. There are various types of indirect RVS procedures. The most standard and generally used procedures for indirect RVS are encephalo-duro-arteriosynangiosis (EDAS) [5, 6], encephalo-myo-synangiosis (EMS) [7], and encephalo-duro-arterio-myo-synangiosis (EDAMS) [8]. The choice of donor tissue, such as the superficial temporal artery (STA), dura (middle meningeal artery), temporalis muscle (deep temporal artery), galea, and periosteum vary according to the operator or the institute’s preference [9,10,11]. The advantages of indirect RVS over direct RVS are its relatively easy surgical technique, short operation time, and a relatively low risk of postoperative hyperperfusion syndrome. However, because indirect RVS procedures require the process of angiogenesis, neovascularization takes time to occur in the repositioned tissue adjacent to the ischemic brain, which is not effective for immediate blood flow augmentation [10, 12]. In some cases, sufficient collateral vessels do not grow even after the indirect RVS procedure [9, 13]. Due to concerns about incomplete RVS [14,15,16,17,18], a combination of different indirect RVS procedures is used for a wide extent of revascularizations. These include procedures such as EDAS plus bifrontal encephalo-galeo-periosteal-synangiosis (EGPS) [9], multiple EDAS [19], ribbon EDAMS [20], and multiple burr holes [21].
Direct RVS, usually represented by the STA to middle cerebral artery (MCA) anastomosis, is the most used technique in adult MMD. Other variations include the occipital artery to posterior cerebral artery anastomosis and the STA to anterior cerebral artery anastomosis. Direct extracranial–intracranial artery anastomosis enables prompt flow augmentation because it does not require angiogenesis and only requires remodeling of the arterio-arterial anastomosis site called arteriogenesis [12]. However, immediate changes in hemodynamics can cause perioperative complications such as postoperative hyperperfusion syndrome [22, 23].
Combined RVS with both direct and indirect RVS is the most effective technique currently used. As the revascularization process continues after surgery, both direct bypass and indirect bypass play an important role because they have different formation processes and patterns [24]. Direct bypass plays a major role in early flow augmentation in the early postoperative period; however, the area revascularized by direct revascularization may decrease due to occlusion of the distal cerebral artery over time. In such cases, collateral vessels by the indirect bypass can play a complementary role [10]. In some cases, synergistic increases are seen in the area revascularized by both direct and indirect bypasses without regression of the flow by direct bypass [25].
3 Indication of RVS
The common idea of RVS in patients with MMD is the enhancement of intrinsic compensatory mechanisms in the nature of MMD [26]. Revascularization surgery preserves the brain that is vulnerable to stroke from cerebral ischemia by improving cerebral blood flow and preventing cerebral hemorrhage by reducing hemodynamic stress [27].
In pediatric MMD, RVS is an irreplaceable option regardless of disease severity. The young developing brain, which requires high cerebral oxygen metabolism, justifies timely RVS surgery [9, 28,29,30,31]. The younger the age at which MMD is diagnosed, the worse the clinical prognosis, which means that the earlier the surgery, the better the clinical outcome [9, 29, 30, 32].
In contrast to pediatric MMD, treatment strategies for adult MMD are selected depending on the disease state. RVS is primarily considered in adult ischemic MMD with the presence of symptoms and hemodynamic compromise [27, 33, 34]. Recently, bilateral direct RVS has been reported as an effective treatment for adult hemorrhagic MMD, reducing hemorrhagic recurrence, and improving patient prognosis since the Japan Adult Moyamoya trial [35].
As the use of magnetic resonance imaging (MRI) for diagnostic purposes increases, patients with asymptomatic MMD are increasing [1, 2]. However, the long-term clinical course and prognosis of asymptomatic MMD are indeterminate, and treatment strategies for asymptomatic MMD are unclear. Kuroda et al. [36] reported 23.8% (15/63 patients) of disease progression, with a mean time to progression from diagnosis of 60 months (1.5–8 years). MMD progression occurs in both bilateral and unilateral MMD, both the anterior and posterior circulation, and symptomatic and asymptomatic cases [36]. Yamada et al. [37] reported that 21.2% (6/33 patients) of the patients with asymptomatic MMD became symptomatic within the mean follow-up duration of 44 months. In a prospective study of patients with asymptomatic MMD [38], silent cerebral infarct and decreased cerebral hemodynamics accounted for 20% and 40%, respectively. During a mean follow-up duration of 43.7 months, seven patients experienced cerebrovascular events (transient ischemic attack, n = 3; ischemic stroke, n = 1; hemorrhagic stroke, n = 3) among 34 non-surgically treated patients (3.2% of estimated annual stroke risk). Unlike previous studies that did not separate the hemodynamic state and the presence of symptoms, Cho et al. [39] investigated the natural course of adult patients with MMD (n = 241) who were hemodynamically stable during a mean follow-up duration of 82.5 months. While the overall annual stroke rate was 4.5% per person-year (hemorrhagic presenting group, 4.3%; ischemic presenting group, 3.0%), the annual stroke rate in hemodynamically stable patients with asymptomatic MMD was 3.4% (hemorrhagic stroke, 2.5%; ischemic stroke, 0.8%). As asymptomatic MMD is not a fixed but dynamic disease, regular follow-up is necessary. Through MRI/MR angiography (MRA), disease progression, as well as silent cerebral infarction or micro-bleeding, can be confirmed. In this regard, it would be helpful to know the long-term clinical course and prognosis through the ongoing asymptomatic moyamoya registry (AMORE) study [40].
After a statement by the Research Committee of MMD of the Japanese Ministry of Health, Labour, and Welfare in 2015, unilateral MMD has also been modified to include diagnostic criteria for definitive MMD. Compared with bilateral MMD, unilateral MMD has a higher proportion of adult patients with a range of progression rates between 14.6% and 50% [41, 42]. The younger the patients’ age, the more frequently [43,44,45,46] and faster [43, 47, 48] contralateral progression occurs. In patients under 2 years of age, concurrent bilateral surgery is considered due to the high likelihood of contralateral progression and poor prognosis [32]. Except for an extremely young age, the usual treatment strategy for unilateral pediatric and adult MMD is to treat the symptomatic side first and then wait.
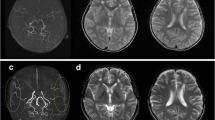
The surgical indications for adult MMD at our institution are as follows: (1) symptomatic manifestations including ischemic and hemorrhagic events; (2) asymptomatic patients with disease progression proven on computed tomography angiography (CTA), MRA, or conventional angiography; (3) functionally independent with the Karnofsky Performance Scale over 70; (4) no acute cerebral infarction or hemorrhage within 4 weeks at the time of surgery; and (5) hemodynamically unstable demonstrated by acetazolamide challenge single-photon emission computed tomography and perfusion CT or MRI [49, 50].
4 Selection of the RVS Procedure
The selection of the RVS procedure has the following limitations: heterogeneity of MMD according to age proportion, racial and geographical distribution; diversity of surgical methods by the preference of institutions and operators; relatively small number of patients; and lack of randomized controlled trials.
For a good surgical outcome for MMD, preoperative hemodynamic compromise should be considered first before the choice of surgical procedure. Without preoperative hemodynamic compromise, neovascularization would not occur, regardless of the extent of surgery [51]. Satisfactory angiographic revascularization assumes the correct location of the vascularized donor tissues or correct selection of the recipient artery on the surface of the on-demanding ischemic brain [51].
In pediatric MMD, both direct and indirect RVS procedures are comparable in surgical outcomes [52,53,54,55,56]. If there are no issues with the surgeon’s technique and facility policy, direct with indirect revascularization can be considered [25, 57]. However, in children, satisfactory revascularization can also be accomplished with only indirect bypass procedures [32, 58, 59]. In younger patients with MMD, direct RVS procedures have technical limitations because of the small size of the STA and the cortical branch of the MCA. Therefore, children under 4 years of age are not candidates for direct RVS [34]. Patients older than 5 years can be appropriate candidates for direct RVS [25, 57]. Direct flow augmentation by direct RVS can diminish the risk of perioperative stroke [25, 56, 60]. However, the possibility of watershed shift or hyperperfusion syndrome should be kept in mind [61, 62], although those chances are less likely than in adults [60, 63,64,65]. With well-developed moyamoya collateral vessels compared with adults, there is less likelihood of postoperative stroke due to progressive occlusion of the main cerebral artery [60]. In patients who experience frequent transient ischemic attacks (TIA) with severe hemodynamic compromise, it is better to consider direct revascularization for the rapid formation of collaterals [25, 56, 60].
In adult ischemic MMD, a combination of both direct and indirect RVS is the main treatment of choice [24, 25, 66,67,68]; however, the role of indirect bypass has been reported continuously [69,70,71,72]. In cases of adult hemorrhagic MMD, bilateral combined RVS for improving hemodynamic stress is considered an effective treatment [35, 73].
5 Long-term Outcome of RVS for Patients with MMD in Korea (Table 23.1)
A majority of the pediatric patients with MMD in Korea present with TIAs or cerebral infarcts (98%), while hemorrhagic manifestations occur in only around 2% of the patients [74]. In a retrospective study of indirect RVS for pediatric patients with MMD (629 patients with 1,283 surgeries) in Korea, who were followed up for more than 5 years, with a mean clinical follow-up duration of 12 years, 95% of the patients showed favorable clinical outcomes. The annual risk of developing symptomatic hemorrhage or cerebral infarction was 0.04% and 0.08%, respectively. The 10-year event-free survival rates without symptomatic infarction and hemorrhage were 99.2% and 98%, respectively [74]. Based on a comparison study between EDAS with bifrontal EGPS and simple EDAS in Korea, which showed larger revascularization with better hemodynamic improvement and more favorable outcomes in combined surgery [9], combined indirect RVS methods with bifrontal EGPS, occipital EDAS, or multiple burr hole surgery are actively utilized during the careful surveillance of disease progression. Although indirect bypass has been attempted in pediatric patients with hemorrhagic MMD, with good outcomes in a few studies, there are few reports to establish strong evidence [74, 79
].
Poor social outcomes with cognitive dysfunction are major concerns among pediatric patients with MMD. Despite satisfactory RVS without complications, patients who had preoperative neurological deficits tend to experience adaptation difficulties in their education or occupation due to intellectual impairment [80]. Patients with preoperative neurological impairment and major cerebral infarct showed poor social outcomes [32, 80, 81]. Regardless of the presence of major or borderzone infarctions, RVS can prevent further neurocognitive declination [81]. There are no comparative reports on social outcomes according to the type of revascularization.
Compared with conservative treatment [39], RVS is considered to improve cerebral hemodynamics and prevent subsequent ischemic stroke in adult ischemic MMD [24, 66, 67]. Direct or combined revascularization is a common surgical method for adult ischemic MMD. To achieve optimal surgical outcomes, combined RVS is preferred in most studies [24, 66, 67, 82]. The combined RVS is a technique for obtaining advantages of both direct and indirect RVS. Along with direct RVS for immediate flow augmentation, indirect RVS mobilizes as many vasogenic potent tissues as possible to create a revascularization channel. The revascularization area is the largest in combined RVS, followed by direct and indirect RVS [67, 83]. According to angiographic follow-up after 6–12 months of surgery, revascularization by both direct and indirect RVS explains the complementary relationships between the two methods [75]. In a prospective study of combined RVS for adult patients with ischemic MMD (77 hemispheres, 60 patients) in Korea, the annual risk of developing symptomatic hemorrhage or a cerebral infarct was 0.4% and 0.2%, respectively. The patients showed improvement in clinical, angiographic, and hemodynamic aspects until 6 months after surgery. The 5-year event-free survival rate without symptomatic hemorrhage and cerebral infarction was 98.7% [24]. According to a comparative study of patients presenting with ischemia, the 1-year and 5-year incidences of symptomatic ischemic stroke were not lower in patients who underwent combined RVS in comparison to those in the conservative treatment group because perioperative stroke offsets the benefit [66]. It was not until 10 years later that the benefit of RVS was confirmed, with the absolute risk reduction for ischemic stroke being 9.4%, and the number required for treatment was 11. Briefly, while the benefit of combined RVS for conservative treatment is generally acceptable, it depends on perioperative stroke control. Perioperative stroke developed with various incidences (2.7–13.0%) [24, 66, 67]. Although patients with an advanced Suzuki stage with a poorer perfusion status seem to be prone to perioperative stroke development, little has been reported about factors related to perioperative stroke [76].
Indirect RVS in adult patients with ischemic MMD results in a lower incidence of recurrent stroke compared with conservative treatment, although it did not show more satisfactory outcomes than a direct bypass [67, 75, 84].
A study of the natural history of hemorrhagic MMD showed that the overall estimated rate of hemorrhagic recurrence was 16.9% per person at 5 years and 26.3% per person at 10 years after the onset of initial hemorrhage [77]. Recurrent hemorrhage is the most significant poor prognostic factor in hemorrhagic MMD [77]. Hemodynamic failure in patients with hemorrhagic MMD is an independent risk factor for subsequent hemorrhage [85]. In a retrospective study of adult patients with hemorrhagic MMD in Korea (44 patients), the incidence of recurrent hemorrhage was 11.1% after direct revascularization, 22.2% after indirect revascularization, and 12.5% after combined revascularization [78].
6 Conclusion
RVS for MMD can improve radiological and clinical outcomes. The selection of the RVS procedure is determined by the patient’s age, the degree of hemodynamic compromise, the patient’s symptoms, the condition of the donor/recipient vessel, and the surgeon’s preference.
References
Lee SU, Kim T, Kwon OK, Bang JS, Ban SP, Byoun HS, et al. Trends in the incidence and treatment of cerebrovascular diseases in Korea: part II. Cerebral infarction, cerebral arterial stenosis, and Moyamoya disease. J Korean Neurosurg Soc. 2020;63(1):69–79.
Oh CW. The overall trends of neurosurgical diseases in Korea: analysis of the incidence of diseases and treatment modalities using NHIS data from 2010 to 2016. Health Insurance Review & Assessment Service; 2017.
Spetzler RF, Roski RA, Kopaniky DR. Alternative superficial temporal artery to middle cerebral artery revascularization procedure. Neurosurgery. 1980;7(5):484–7.
Suzuki J, Takaku A. Cerebrovascular “moyamoya” disease. Disease showing abnormal net-like vessels in base of brain. Arch Neurol. 1969;20(3):288–99.
Matsushima Y, Fukai N, Tanaka K, Tsuruoka S, Inaba Y, Aoyagi M, et al. A new surgical treatment of moyamoya disease in children: a preliminary report. Surg Neurol. 1981;15(4):313–20.
Matsushima Y, Inaba Y. Moyamoya disease in children and its surgical treatment. Introduction of a new surgical procedure and its follow-up angiograms. Childs Brain. 1984;11(3):155–70.
Karasawa J, Kikuchi H, Furuse S, Sakaki T. Yoshida Y. a surgical treatment of “moyamoya” disease “encephalo-myo synangiosis”. Neurol Med Chir. 1977;17(1 Pt 1):29–37.
Kinugasa K, Mandai S, Kamata I, Sugiu K, Ohmoto T. Surgical treatment of moyamoya disease: operative technique for encephalo-duro-arterio-myo-synangiosis, its follow-up, clinical results, and angiograms. Neurosurgery. 1993;32(4):527–31.
Kim SK, Wang KC, Kim IO, Lee DS, Cho BK. Combined encephaloduroarteriosynangiosis and bifrontal encephalogaleo(periosteal)synangiosis in pediatric moyamoya disease. Neurosurgery. 2002;50(1):88–96.
Houkin K, Kuroda S, Ishikawa T, Abe H. Neovascularization (angiogenesis) after revascularization in moyamoya disease. Which technique is most useful for moyamoya disease? Acta Neurochir. 2000;142(3):269–76.
Matsushima T, Inoue T, Katsuta T, Natori Y, Suzuki S, Ikezaki K, et al. An indirect revascularization method in the surgical treatment of moyamoya disease--various kinds of indirect procedures and a multiple combined indirect procedure. Neurol Med Chir. 1998;38(Suppl):297–302.
Saito N, Imai H. Insights on the revascularization mechanism for treatment of Moyamoya disease based on the histopathologic concept of angiogenesis and arteriogenesis. World Neurosurg. 2011;75(2):204–5.
Nakashima H, Meguro T, Kawada S, Hirotsune N, Ohmoto T. Long-term results of surgically treated moyamoya disease. Clin Neurol Neurosurg. 1997;99(Suppl 2):S156–61.
Shim KW, Park EK, Kim JS, Kim DS. Cognitive outcome of pediatric Moyamoya disease. J Korean Neurosurg Soc. 2015;57(6):440–4.
Pandey P, Steinberg GK. Outcome of repeat revascularization surgery for moyamoya disease after an unsuccessful indirect revascularization. Clinical article. J Neurosurg. 2011;115(2):328–36.
Miyamoto S, Kikuchi H, Karasawa J, Nagata I, Yamazoe N, Akiyama Y. Pitfalls in the surgical treatment of moyamoya disease. Operative techniques for refractory cases. J Neurosurg. 1988;68(4):537–43.
Matsushima Y. Failure of encephalo-duro-arterio-synangiosis procedure in moyamoya disease. Pediatr Neurosci. 1985;12(6):326–7.
Cahan LD. Failure of encephalo-duro-arterio-synangiosis procedure in moyamoya disease. Pediatr Neurosci. 1985;12(1):58–62.
Tenjin H, Ueda S, Multiple EDAS. (Encephalo-duro-arterio-synangiosis). Additional EDAS using the frontal branch of the superficial temporal artery (STA) and the occipital artery for pediatric moyamoya patients in whom EDAS using the parietal branch of STA was insufficient. Child’s Nervous System: ChNS: Official Journal of the International Society for Pediatric Neurosurgery. 1997;13(4):220–4.
Kinugasa K, Mandai S, Tokunaga K, Kamata I, Sugiu K, Handa A, et al. Ribbon enchephalo-duro-arterio-myo-synangiosis for moyamoya disease. Surg Neurol. 1994;41(6):455–61.
Sainte-Rose C, Oliveira R, Puget S, Beni-Adani L, Boddaert N, Thorne J, et al. Multiple bur hole surgery for the treatment of moyamoya disease in children. J Neurosurg. 2006;105(6 Suppl):437–43.
Kim JE, Oh CW, Kwon OK, Park SQ, Kim SE, Kim YK. Transient hyperperfusion after superficial temporal artery/middle cerebral artery bypass surgery as a possible cause of postoperative transient neurological deterioration. Cerebrovasc Dis (Basel, Switzerland). 2008;25(6):580–6.
Fujimura M, Kaneta T, Mugikura S, Shimizu H, Tominaga T. Temporary neurologic deterioration due to cerebral hyperperfusion after superficial temporal artery-middle cerebral artery anastomosis in patients with adult-onset moyamoya disease. Surg Neurol. 2007;67(3):273–82.
Cho WS, Kim JE, Kim CH, Ban SP, Kang HS, Son YJ, et al. Long-term outcomes after combined revascularization surgery in adult moyamoya disease. Stroke. 2014;45(10):3025–31.
Uchino H, Kim JH, Fujima N, Kazumata K, Ito M, Nakayama N, et al. Synergistic interactions between direct and indirect bypasses in combined procedures: the significance of indirect bypasses in Moyamoya disease. Neurosurgery. 2017;80(2):201–9.
Fujimura M, Tominaga T. Lessons learned from moyamoya disease: outcome of direct/indirect revascularization surgery for 150 affected hemispheres. Neurol Med Chir. 2012;52(5):327–32.
Kim JE, Jeon JS. An update on the diagnosis and treatment of adult Moyamoya disease taking into consideration controversial issues. Neurol Res. 2014;36(5):407–16.
Kim SK, Cho BK, Phi JH, Lee JY, Chae JH, Kim KJ, et al. Pediatric moyamoya disease: an analysis of 410 consecutive cases. Ann Neurol. 2010;68(1):92–101.
Suzuki Y, Negoro M, Shibuya M, Yoshida J, Negoro T, Watanabe K. Surgical treatment for pediatric moyamoya disease: use of the superficial temporal artery for both areas supplied by the anterior and middle cerebral arteries. Neurosurgery. 1997;40(2):324–9. discussion 9–30
Matsushima Y, Aoyagi M, Masaoka H, Suzuki R, Ohno K. Mental outcome following encephaloduroarteriosynangiosis in children with moyamoya disease with the onset earlier than 5 years of age. Child’s Nervous System: ChNS: Official Journal of the International Society for Pediatric Neurosurgery. 1990;6(8):440–3.
Scott RM, Smith JL, Robertson RL, Madsen JR, Soriano SG, Rockoff MA. Long-term outcome in children with moyamoya syndrome after cranial revascularization by pial synangiosis. J Neurosurg. 2004;100(2 Suppl Pediatrics):142–9.
Kim SK, Seol HJ, Cho BK, Hwang YS, Lee DS, Wang KC. Moyamoya disease among young patients: its aggressive clinical course and the role of active surgical treatment. Neurosurgery. 2004;54(4):840–4. discussion 4–6
Narisawa A, Fujimura M, Tominaga T. Efficacy of the revascularization surgery for adult-onset moyamoya disease with the progression of cerebrovascular lesions. Clin Neurol Neurosurg. 2009;111(2):123–6.
Guzman R, Lee M, Achrol A, Bell-Stephens T, Kelly M, Do HM, et al. Clinical outcome after 450 revascularization procedures for moyamoya disease. Clinical article. J Neurosurg. 2009;111(5):927–35.
Miyamoto S, Yoshimoto T, Hashimoto N, Okada Y, Tsuji I, Tominaga T, et al. Effects of extracranial-intracranial bypass for patients with hemorrhagic moyamoya disease: results of the Japan adult Moyamoya trial. Stroke. 2014;45(5):1415–21.
Kuroda S, Ishikawa T, Houkin K, Nanba R, Hokari M, Iwasaki Y. Incidence and clinical features of disease progression in adult moyamoya disease. Stroke. 2005;36(10):2148–53.
Yamada M, Fujii K, Fukui M. [clinical features and outcomes in patients with asymptomatic moyamoya disease--from the results of nation-wide questionnaire survey]. No shinkei geka. Neurol Surg. 2005;33(4):337–42.
Kuroda S, Hashimoto N, Yoshimoto T, Iwasaki Y. Radiological findings, clinical course, and outcome in asymptomatic moyamoya disease: results of multicenter survey in Japan. Stroke. 2007;38(5):1430–5.
Cho WS, Chung YS, Kim JE, Jeon JP, Son YJ, Bang JS, et al. The natural clinical course of hemodynamically stable adult moyamoya disease. J Neurosurg. 2015;122(1):82–9.
Kuroda S. Asymptomatic moyamoya disease: literature review and ongoing AMORE study. Neurol Med Chir. 2015;55(3):194–8.
Lee SC, Jeon JS, Kim JE, Chung YS, Ahn JH, Cho WS, et al. Contralateral progression and its risk factor in surgically treated unilateral adult moyamoya disease with a review of pertinent literature. Acta Neurochir. 2014;156(1):103–11.
Hayashi K, Horie N, Izumo T, Nagata I. A nationwide survey on unilateral moyamoya disease in Japan. Clin Neurol Neurosurg. 2014;124:1–5.
Smith ER, Scott RM. Progression of disease in unilateral moyamoya syndrome. Neurosurg Focus. 2008;24(2):E17.
Houkin K, Abe H, Yoshimoto T, Takahashi A. Is “unilateral” moyamoya disease different from moyamoya disease? J Neurosurg. 1996;85(5):772–6.
Hayashi K, Suyama K, Nagata I. Clinical features of unilateral moyamoya disease. Neurol Med Chir. 2010;50(5):378–85.
Kawano T, Fukui M, Hashimoto N, Yonekawa Y. Follow-up study of patients with “unilateral” moyamoya disease. Neurol Med Chir. 1994;34(11):744–7.
Park EK, Lee YH, Shim KW, Choi JU, Kim DS. Natural history and progression factors of unilateral moyamoya disease in pediatric patients. Child’s Nervous System: ChNS: Official Journal of the International Society for Pediatric Neurosurgery. 2011;27(8):1281–7.
Yeon JY, Shin HJ, Kong DS, Seol HJ, Kim JS, Hong SC, et al. The prediction of contralateral progression in children and adolescents with unilateral moyamoya disease. Stroke. 2011;42(10):2973–6.
Kim JE, Pang CH. Diagnosis and treatment of adult Moyamoya disease. Journal of the Korean Medical Association/Taehan Uisa Hyophoe Chi. 2019;62(11):577–85.
Kim JE, Kim KM, Kim JG, Kang HS, Bang JS, Son YJ, et al. Clinical features of adult moyamoya disease with special reference to the diagnosis. Neurol Med Chir. 2012;52(5):311–7.
Nariai T, Suzuki R, Matsushima Y, Ichimura K, Hirakawa K, Ishii K, et al. Surgically induced angiogenesis to compensate for hemodynamic cerebral ischemia. Stroke. 1994;25(5):1014–21.
Fung LW, Thompson D, Ganesan V. Revascularisation surgery for paediatric moyamoya: a review of the literature. Child’s Nervous System: ChNS: Official Journal of the International Society for Pediatric Neurosurgery. 2005;21(5):358–64.
Veeravagu A, Guzman R, Patil CG, Hou LC, Lee M, Steinberg GK. Moyamoya disease in pediatric patients: outcomes of neurosurgical interventions. Neurosurg Focus. 2008;24(2):E16.
Zheng J, Yu LB, Dai KF, Zhang Y, Wang R, Zhang D. Clinical features, surgical treatment, and long-term outcome of a multicenter cohort of pediatric Moyamoya. Front Neurol. 2019;10:14.
Matsushima T, Inoue T, Suzuki SO, Fujii K, Fukui M, Hasuo K. Surgical treatment of moyamoya disease in pediatric patients--comparison between the results of indirect and direct revascularization procedures. Neurosurgery. 1992;31(3):401–5.
Zhao Y, Lu J, Yu S, Li J, Deng X, Zhang Y, et al. Comparison of long-term effect between direct and indirect bypass for pediatric ischemic-type Moyamoya disease: a propensity score-matched study. Front Neurol. 2019;10:795.
Ikezaki K. Rational approach to treatment of moyamoya disease in childhood. J Child Neurol. 2000;15(5):350–6.
Adelson PD, Scott RM. Pial synangiosis for moyamoya syndrome in children. Pediatr Neurosurg. 1995;23(1):26–33.
Bao XY, Duan L, Yang WZ, Li DS, Sun WJ, Zhang ZS, et al. Clinical features, surgical treatment, and long-term outcome in pediatric patients with moyamoya disease in China. Cerebrovasc Dis (Basel, Switzerland). 2015;39(2):75–81.
Kazumata K, Ito M, Tokairin K, Ito Y, Houkin K, Nakayama N, et al. The frequency of postoperative stroke in moyamoya disease following combined revascularization: a single-university series and systematic review. J Neurosurg. 2014;121(2):432–40.
Heros RC, Scott RM, Kistler JP, Ackerman RH, Conner ES. Temporary neurological deterioration after extracranial-intracranial bypass. Neurosurgery. 1984;15(2):178–85.
Hayashi T, Shirane R, Fujimura M, Tominaga T. Postoperative neurological deterioration in pediatric moyamoya disease: watershed shift and hyperperfusion. J Neurosurg Pediatr. 2010;6(1):73–81.
Uchino H, Kuroda S, Hirata K, Shiga T, Houkin K, Tamaki N. Predictors and clinical features of postoperative hyperperfusion after surgical revascularization for moyamoya disease: a serial single photon emission CT/positron emission tomography study. Stroke. 2012;43(10):2610–6.
Fujimura M, Kaneta T, Tominaga T. Efficacy of superficial temporal artery-middle cerebral artery anastomosis with routine postoperative cerebral blood flow measurement during the acute stage in childhood moyamoya disease. Child’s Nervous System: ChNS: Official Journal of the International Society for Pediatric Neurosurgery. 2008;24(7):827–32.
Rashad S, Fujimura M, Niizuma K, Endo H, Tominaga T. Long-term follow-up of pediatric moyamoya disease treated by combined direct-indirect revascularization surgery: single institute experience with surgical and perioperative management. Neurosurg Rev. 2016;39(4):615–23.
Kim T, Oh CW, Kwon OK, Hwang G, Kim JE, Kang HS, et al. Stroke prevention by direct revascularization for patients with adult-onset moyamoya disease presenting with ischemia. J Neurosurg. 2016;124(6):1788–93.
Bang JS, Kwon OK, Kim JE, Kang HS, Park H, Cho SY, et al. Quantitative angiographic comparison with the OSIRIS program between the direct and indirect revascularization modalities in adult moyamoya disease. Neurosurgery. 2012;70(3):625–32. discussion 32–3
Kuroda S, Houkin K, Ishikawa T, Nakayama N, Iwasaki Y. Novel bypass surgery for moyamoya disease using pericranial flap: its impacts on cerebral hemodynamics and long-term outcome. Neurosurgery. 2010;66(6):1093–101. discussion 101
Bao XY, Zhang Y, Wang QN, Zhang Q, Wang H, Zhang ZS, et al. Long-term outcomes after Encephaloduroarteriosynangiosis in adult patients with Moyamoya disease presenting with ischemia. World Neurosurg. 2018;115:e482–e9.
Dusick JR, Gonzalez NR, Martin NA. Clinical and angiographic outcomes from indirect revascularization surgery for Moyamoya disease in adults and children: a review of 63 procedures. Neurosurgery. 2011;68(1):34–43. discussion
Gross BA, Du R. The natural history of moyamoya in a north American adult cohort. Journal of Clinical Neuroscience: Official Journal of the Neurosurgical Society of Australasia. 2013;20(1):44–8.
Hallemeier CL, Rich KM, Grubb RL Jr, Chicoine MR, Moran CJ, Cross DT 3rd, et al. Clinical features and outcome in north American adults with moyamoya phenomenon. Stroke. 2006;37(6):1490–6.
Takahashi JC, Funaki T, Houkin K, Kuroda S, Fujimura M, Tomata Y, et al. Impact of cortical hemodynamic failure on both subsequent hemorrhagic stroke and effect of bypass surgery in hemorrhagic moyamoya disease: a supplementary analysis of the Japan adult Moyamoya trial. J Neurosurg. 2020:1–6.
Ha EJ, Kim KH, Wang KC, Phi JH, Lee JY, Choi JW, et al. Long-term outcomes of indirect bypass for 629 children with Moyamoya disease: longitudinal and Cross-sectional analysis. Stroke. 2019;50(11):3177–83.
Kim DS, Huh PW, Kim HS, Kim IS, Choi S, Mok JH, et al. Surgical treatment of moyamoya disease in adults: combined direct and indirect vs. indirect bypass surgery. Neurol Med Chir. 2012;52(5):333–8.
Kim T, Bang JS, Kwon OK, Hwang G, Kim JE, Kang HS, et al. Hemodynamic changes after unilateral revascularization for Moyamoya disease: serial assessment by quantitative magnetic resonance angiography. Neurosurgery. 2017;81(1):111–9.
Kim KM, Kim JE, Cho WS, Kang HS, Son YJ, Han MH, et al. Natural history and risk factor of recurrent hemorrhage in hemorrhagic adult Moyamoya disease. Neurosurgery. 2017;81(2):289–96.
Choi WS, Lee SB, Kim DS, Huh PW, Yoo DS, Lee TG, et al. Thirteen-year experience of 44 patients with adult hemorrhagic Moyamoya disease from a single institution: clinical analysis by management modality. Journal of cerebrovascular and endovascular neurosurgery. 2013;15(3):191–9.
Ahn JH, Wang KC, Phi JH, Lee JY, Cho BK, Kim IO, et al. Hemorrhagic moyamoya disease in children: clinical features and surgical outcome. Child’s Nervous System: ChNS: Official Journal of the International Society for Pediatric Neurosurgery. 2012;28(2):237–45.
Phi JH, Wang KC, Cho BK, Lee MS, Lee JH, Yu KS, et al. Long-term social outcome in children with moyamoya disease who have reached adulthood. J Neurosurg Pediatr. 2011;8(3):303–9.
Lee JY, Phi JH, Wang KC, Cho BK, Shin MS, Kim SK. Neurocognitive profiles of children with moyamoya disease before and after surgical intervention. Cerebrovasc Dis (Basel, Switzerland). 2011;31(3):230–7.
Jeon JP, Kim JE, Cho WS, Bang JS, Son YJ, Oh CW. Meta-analysis of the surgical outcomes of symptomatic moyamoya disease in adults. J Neurosurg. 2018;128(3):793–9.
Choi IJ, Cho SJ, Chang JC, Park SQ, Park HK. Angiographic results of indirect and combined bypass surgery for adult moyamoya disease. J Cerebrovasc Endovasc Neurosurg. 2012;14(3):216–22.
Lee SB, Kim DS, Huh PW, Yoo DS, Lee TG, Cho KS. Long-term follow-up results in 142 adult patients with moyamoya disease according to management modality. Acta Neurochir. 2012;154(7):1179–87.
Jo KI, Kim MS, Yeon JY, Kim JS, Hong SC. Recurrent bleeding in hemorrhagic Moyamoya disease : prognostic implications of the perfusion status. J Korean Neurosurg Soc. 2016;59(2):117–21.
Acknowledgement
The authors appreciate Dr. Jin Woo Bae, Si Un Lee, and Tackeun Kim for helping with the preparation of this manuscript.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Kim, J.E., Oh, C.W. (2021). Long-Term Outcome of Revascularization Surgery for Moyamoya Disease in Korea. In: Kuroda, S. (eds) Moyamoya Disease: Current Knowledge and Future Perspectives. Springer, Singapore. https://doi.org/10.1007/978-981-33-6404-2_23
Download citation
DOI: https://doi.org/10.1007/978-981-33-6404-2_23
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-33-6403-5
Online ISBN: 978-981-33-6404-2
eBook Packages: MedicineMedicine (R0)