Abstract
Liver transplantation (LT) is the standard surgical definite treatment for end-stage liver disease (ESLD) with different indications encompassing a wide spectrum of liver failure patients with variable clinical profile and status ranging from fulminant to chronic liver failure. It is a high-risk surgery requiring critical vascular volume assessment and fluid management; there are multiple hemodynamic drifts resulting from major blood loss, fluid shifts, and vasomotor tone. Liver transplant recipients suffer many complications, some of which are intervention or approach related. On an average, liver transplant recipients suffer more than three postoperative complications, with over half of them being severe. Perioperative acute renal failure is frequent (13–71%) and is associated with postoperative mortality [1, 2]. Several perioperative events and factors including inappropriate fluid therapy seem associated with the risk of complications ranging from insignificant insult to multiorgan dysfunction syndrome and mortality as a consequence of hypoperfusion and tissue hypoxia, often exacerbated by a microcirculatory injury and increased tissue metabolic demands [3, 4]. This insult sets in a chain of sequential molecular reactions resulting in further ischemic and hypoxic tissue injury. This may be further compounded by cytopathic hypoxic injury due to mitochondrial dysfunction [5, 6]. If not all, many of these complications are preventable, but at least can be minimized with good perioperative care. Liver transplantation is a growing and evolving specialty. Strategies to improve recipient’s survival are needed. One of these strategies is restrictive fluid strategies and has been found better postoperative outcomes than liberal fluid management strategies.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Liver transplantation (LT) is the standard surgical definite treatment for end-stage liver disease (ESLD) with different indications encompassing a wide spectrum of liver failure patients with variable clinical profile and status ranging from fulminant to chronic liver failure. It is a high-risk surgery requiring critical vascular volume assessment and fluid management; there are multiple hemodynamic drifts resulting from major blood loss, fluid shifts, and vasomotor tone. Liver transplant recipients suffer many complications, some of which are intervention or approach related. On an average, liver transplant recipients suffer more than three postoperative complications, with over half of them being severe. Perioperative acute renal failure is frequent (13–71%) and is associated with postoperative mortality [1, 2]. Several perioperative events and factors including inappropriate fluid therapy seem associated with the risk of complications ranging from insignificant insult to multiorgan dysfunction syndrome and mortality as a consequence of hypoperfusion and tissue hypoxia, often exacerbated by a microcirculatory injury and increased tissue metabolic demands [3, 4]. This insult sets in a chain of sequential molecular reactions resulting in further ischemic and hypoxic tissue injury. This may be further compounded by cytopathic hypoxic injury due to mitochondrial dysfunction [5, 6]. If not all, many of these complications are preventable, but at least can be minimized with good perioperative care. Liver transplantation is a growing and evolving specialty. Strategies to improve recipient’s survival are needed. One of these strategies is restrictive fluid strategies and has been found better postoperative outcomes than liberal fluid management strategies.
Fluid management strategy is one of the important aspects of perioperative care in liver transplant surgery. In critically ill cirrhotic patients with altered pathophysiology at different levels including organ dysfunction, endocrine imbalance, and receptor response alteration, volume status evaluation is difficult leading to inappropriate fluid therapy. Fluid overload is related to several complications like pulmonary edema, ileus, cardiac failure, delayed wound healing and tissue breakdown, infections, and increased mortality. Therefore, the evaluation of volume status is crucial in the optimal management of fluid therapy. Successful fluid overload treatment depends on the precise assessment of individual volume status, understanding the pathophysiology and principles of perioperative fluid management, concerns of volume over- and underload on graft function and other organs, and clear treatment goals. Perioperative fluid therapy is not just simple fluid to supplement volume for hemodynamics but needs to be prescribed as any other drug prescription. If fluid administration is in excess, it leads to tissue edema of every organ including the gut and lungs affecting adversely translocation of bacteria and oxygenation resulting in delayed recovery. It may lead to graft congestion particularly in living transplant recipients. If there is deficit and hypovolemia, it increases the risk of ischemic and thrombotic complications (Table 19.1). More importantly, a recent multicenter clinical trial showed an increased incidence of acute renal failure when a fixed restrictive perioperative fluid strategy was compared to a liberal one during a major abdominal surgery [7]. There is substantial data against the use of starch-based solutions in septic patients where endothelial capillary leak fails to retain fluid intravascularly and detrimental effects on the kidney and immune system.
Current fluid therapy-related practice issues. There is wide variation in practice. The choice of fluids is largely based on traditional beliefs, context of practice, location, and cost. It seems that there is more of personnel choices rather than scientific approach. Most of transplant anesthesiologists are quite experienced and skillful. Despite the knowledge and skills there is ample evidence that practices are not uniform and there is wide deviation in choice of goals and parameter targets, monitoring, and type of fluids and management strategy. Secondly as outcome is dependent on many factors so this makes difficult to design evidence-based fixed fluid therapy protocols. All choices and preferences are not having equivalent outcome. However, everyone justifies his/her own approach being an expert and experienced senior. Thus, there is a need to find the best strategy. The Liver Transplant Anesthesia Consortium (LTrAC) did a series of four comprehensive, web-based surveys in the United States and internationally. There was a very interesting finding that there were geographical differences in practice pattern. Clinicians from the UK, China, and Australia relied primarily on colloid therapy (55–75% of time), whereas only 13% of clinicians in the United States used colloid for treating hypovolemia. In the United States, normal saline was a frequent choice, followed by a pH-adjusted crystalloid in 74%. Albumin was a common colloid for volume expansion (85%; 95% CI, 70–93%). The synthetic colloids HES in saline (Hespan) or HES in balanced electrolyte solution (Hextend) had been used nearly in half of programs at that time prior to restriction by many international agencies on starch fluids [8].
Understanding altered pathophysiology and perioperative fluid management. It is well established that fluid balance has an impact on outcome in liver transplant surgery or any other major abdominal surgery, particularly in high-risk candidates. It is important to understand that it is not only the type of fluid or over-jealous fluid therapy consequences but also happens because of capillary leak which may occur due to sepsis or reperfusion or altered membrane function resulting from other perioperative insults. This happens secondary to the release of host responses in the form of complement factors, cytokines and prostaglandin products, and altered organ microcirculation [9,10,11]. In presence of increased capillary permeability to proteins and increased trans-capillary hydrostatic pressure, hypervolemia secondary to inappropriate fluid administration to maintain pressures results in excessive leak [12]. There is neurohumoral alteration in body homeostasis with marked activation of sympathetic and renin-angiotensin-aldosterone systems in these patients resulting in sodium retention with very low urinary excretion of sodium. The “splanchnic steal” and leaky endothelium in cirrhotic make fluid management difficult. There is an inability of body to mobilize ascites despite adherence to the dietary salt restriction. There is rapid reaccumulation of fluid after therapeutic paracentesis despite adherence to a sodium-restricted diet. These changes put cirrhotic patients at risk of renal and another organ failure in the perioperative period, and a challenging situation for the treating physician [13]. The amount of fluid that leaks into the interstitium correlates with infused fluid volume and that remained intravascular varies with the type of fluid and it’s terminal half life [14]. There is a paradigm shift in membrane function conceptualization. Traditionally it was thought that fluid transfer across endothelial membrane is based on oncotic and hydrostatic pressure balance, i.e., Starling principle. Current concept is “Double-barrier concept” or endothelial Glycocalyx layer. The endothelial glycocalyx layer is a web of membrane-bound glycoproteins and proteoglycans. Sub-glycocalyx intercellular spaces are almost protein-free. Capillaries filter fluid to ISF throughout their length. Absorption through venous capillaries/venules does not occur. Most filtered fluid returns to circulation via lymph. Oxidative stress, attenuation of leucocyte, and platelet adhesion lead to damage of endothelial glycocalyx layer, thus resulting in capillary leak. The integrity or leakiness of this layer and hence potential to develop interstitial edema varies substantially among organ systems, particularly under reperfusion and other inflammatory conditions like sepsis, SIRS of surgery, trauma, and overfluid resuscitation [15].
1 Vascular Component Approach for Guiding Fluid Therapy: A Novel and Critical Way of Volume Status Assessment [16]
The blood volume and the portion of the volume containing red blood cells represent the vital elements of the Vascular content (vC). If the patient has a decreased vC irrespective of the reason, it equals “hypovolemia.” Here, it is important to understand that the vC may be low relatively secondary to vasodilator drugs, in response to anesthesia or redistribution of volume. The classical scenario is that of vasoplegia. The definite therapy will be to restore the vascular tone to normal range but at times may be difficult. Clinically, an important feature of any clinical assessment is “the patient's volume status.” However, for better management, we need to look at all components tone, integrity, and hemodynamics rather than volume status only resulting in inappropriate therapy. The separate evaluation of these different components allows better assessment and management of the patient. These four main components are
-
1.
Blood flow (BF)
-
2.
Vascular content (vC)
-
3.
Vascular barrier (vB)
-
4.
Vascular tone (vT)
An obvious limitation to assess each component reliably bedside is not easy with routine monitoring tools. This concept needs translation in clinical practice to avoid unnecessary fluids in volume responsive patient where vasopressors may prove to be a better option.
2 Restrictive vs. Liberal Strategy
The impact of perioperative fluid balance and fluid therapy has been studied on postoperative complications in last decades in complex surgical populations and septic patients including cardiac, liver transplant and liver resections, with many different combinations of fluid management protocols, strategies, and hemodynamic goals. It is difficult to find the ideal or optimal protocol. ERAS guidelines emphasize on restrictive fluid strategy for enhanced recovery in major abdominal surgery. Perioperative fluid imbalance, defined as too little or too much fluid, had been associated with a greater than 60% increase in postoperative complications after major abdominal surgery [17, 18].
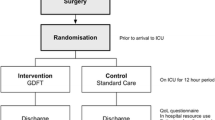
Even in restrictive strategy, there is a need to define target if zero balance or negative balance or minimal positive balance or to which side we can err while moving in gray shades. To implement a strategy, there is a need to know the best monitoring tool to guide fluid therapy. All devices and related parameters to guide fluid management protocol have some caveats and limitations. If the physician is unaware of these pitfalls, one can make mistakes not only in therapy but in research analysis leading to biased results. There are many restrictive fluid strategies such as early goal-directed protocols, weight-based protocols, low-CVP protocols, SVV or cardiac output or PAP-based protocols. Recent systematic reviews done on major surgeries particularly abdominal suggest that cardiac output-guided fluid administration, compared to either fixed restrictive or fixed liberal strategies, reduces postoperative complications by 20–30% in patients undergoing major surgery highlighting and signifying preference to restrictive fluid strategy in these subgroups of these patients [19,20,21].
Thus, current evidence favors to a specific target using restrictive strategy. Sometimes when the patient is too leaky to hold fluid into the vascular compartment, edema sets in despite keeping low vascular volume. Fluid overload is not only a consequence of fluid therapy but also occurs because of altered capillary endothelial function and high hydrostatic pressure from volume overload resulting in leak during severe sepsis secondary to the release of complement factors, cytokines and prostaglandin products, and altered organ microcirculation. Edema in a vicious cycle results in impaired oxygen and metabolite diffusion, distorted tissue architecture, obstruction of capillary blood flow and lymphatic drainage, and disturbed cell to cell interactions that may then contribute to progressive organ dysfunction. Encapsulated organs suffer these insults greater than other organs and tissues [22, 23].
3 Composition of Fluids and Its Impact on Outcome
The right choice of fluid replacement has been a matter of debate. We have three types of fluids broadly: crystalloids, colloids, and albumin. Further we have balanced and non-balanced crystalloid fluids with different electrolyte composition. Colloids include starch-based, gelofusine-based, and albumin with different strengths. Colloids have an edge over crystalloids in expanding the plasma volume and stays longer in the intravascular compartment. The volume administered is less thereby lower incidence of pulmonary, and other organ edema. There is substantial evidence that supports its benefits on microcirculation, blood rheology, and inflammatory mediators. However, starch-based fluids are almost out particularly in septic patients and other critically ill patients because of their adverse effects and ban by various regulatory agencies. Some of the adverse effects are acute and chronic toxicity, coagulopathy, and hypersensitivity reactions in addition to its cost [24, 25]. Most of these studies are from intensive care settings where most of these patients are septic with altered endothelial function. There are few studies from cardiac surgeries debating for the safety of these HES fluids. These studies underlined the difficulties in establishing hardcore outcome data, even in large cohort studies. Although the findings seemed to diminish the magnitude of risk using HES, it cannot nullifies the results of metanalysis and systemic reviews [26,27,28,29]. There is data from animal studies suggesting that 6% HES 130/0.4 exerts protective effects on glycocalyx integrity and attenuates the increase of vascular permeability during systemic inflammation [30]. However, with current literature the safety of starch-based colloids is questionable in critically ill patients.
Human serum albumin has been widely used for many decades in clinical settings with variable reputation as choice over time, but a frequent choice in cirrhotic patients. Albumin is the most abundant protein in the human body, accounting for ∼55% of the total protein content in plasma, with many physiologic functions including binding and transporting a large number of drugs and both endogenous and exogenous substances. It plays an important role as defensive quality by trapping the toxic matter. Moreover, it has antioxidant, free radical scavenger, antithrombotic, and anticoagulant effects and seems to limit increased capillary permeability during inflammation [31, 32]. Albumin as a perioperative fluid therapy is not the first choice as it is costly. However, it is often used whenever there is large ascites and fluid requirement is large. Currently it is recommended in spontaneous bacterial peritonitis with ascites, refractory ascites not responsive to diuretics, large-volume paracentesis, post-paracentesis syndrome, and the treatment of hepatorenal syndrome as an adjunct to vasoconstrictors. New indications for albumin therapy include the antioxidant activity and its effects on capillary integrity. In recent years, large-pore hemofiltration and albumin exchange have emerged as promising liver support therapies for liver failure and other toxic syndromes. They are designed to remove a broad range of blood-borne toxins and to restore normal functions of the circulating albumin by replacing defective forms of albumin and albumin molecules saturated with toxins with normal albumin [32]. In recent years, the use of albumin has been questioned in many studies by the growing concern about the cost-effectiveness of medical treatments. Many of the metanalysis comparing saline and albumin has not shown discernible benefit of albumin [33,34,35,36,37,38]. In a recent study in cardiac surgical intensive care, albumin infusion decreased the need for fresh frozen plasma transfusion, reduced mortality, and lowered serum lactate level but increased financial burden for patients, compared to normal saline group [39]. However, currently careful patient assessment is necessary before administering albumin to see appropriateness as there are a number of contraindications and growing concern of cost-effectiveness [34,35,36, 40]. The adverse effects of albumin have been reported such as interstitial pulmonary edema, multiorgan failure in capillary leak syndrome, or antihemostatic and antiplatelet properties that may worsen blood loss, particularly in post-surgical or trauma patients. In view of high cost and some other associated concerns, appropriateness of prescription is paramount.
In a recent review by Zhou et al. comparing the efficacy and safety of normal saline (NS) for fluid therapy in critically ill with other fluids and colloids, there is no significant different in mortality and incidence of AKI when compared with 10% HES, albumin, and buffered crystalloid solution [41]. A good understanding of individual fluid with its advantage and disadvantage and its interaction in liver recipient with altered homeostasis and neurohumoral response when compared with other fluids prescribed for critically ill patients is conducive to make good clinical decision. There is substantial evidence and experience to support the use of albumin as a part of fluid therapy in liver transplant recipients but its use should be restricted and prescribed judiciously to make liver transplant economical.
4 Monitoring of Volume Status and Perioperative Fluid Management
Intravenous fluid therapy plays a key role in the perioperative management of transplant, and many authors believe that it should be like drug prescription where drug, dose, time, and route matter. Considering the type, dose-effect relationship, and side effects of fluids, fluid therapy should be regarded similar to other drug therapy with specific indications and tailored recommendations. By emphasizing the necessity to individualize fluid therapy, we hope to reduce the risk to our patients and improve their outcome. Weight gain greater than 10% is considered a risk factor for increased pulmonary complications in major abdominal surgeries. Observational studies in nontransplant critically ill patients who required continuous renal replacement therapy (CRRT) have shown an association between fluid overload and mortality [42, 43].
The clinical determination of the intravascular volume can be extremely difficult in critically ill and surgical patients who have altered vascular tone and volume due to anesthesia and major surgery. This is problematic as fluid loading is considered the first step in the resuscitation of hemodynamically unstable patients. However, recent data suggest that only about 50% of hemodynamically unstable patients in the ICU and operating room respond to a fluid challenge [44,45,46]. Traditionally used CVP and other cardiac filling pressures over the last many decades are unable to predict fluid responsiveness. Over the last decade a number of studies have been reported where heart–lung interactions have been used to assess fluid responsiveness in mechanically ventilated patients. Particularly, the pulse pressure variation derived from analysis of the arterial waveform and the stroke volume variation derived from pulse contour analysis have been found to be highly predictive of fluid responsiveness and a better tool to guide fluid therapy. In difficult situations and particularly transplant surgery, transesophageal echocardiography is a more accurate measure of preload than either the central venous pressure or pulmonary artery occlusion pressure using left ventricular end-diastolic area as TEE not only predicts fluid responsiveness but provides functional status of the heart as well as the dynamic indices. There are always controversial results as study design and bias factors change. However, with less expertise and cost issues, TEE in many centers is underutilized.
Although there is current trend in using SVV calibrated and uncalibrated both in liver transplant recipients despite controversial literature, many centers use uncalibrated SVV along with derived cardiac index and SVRI as a routine tool. There are many studies where authors have documented poor performance with uncalibrated SVV. A couple of studies using pulse pressure variations and protocolized fluid therapy based on pulse pressure variation and cardiac index in the setting of brain death donors to guide fluid therapy failed to demonstrate any discernible benefit [47].
In transplant recipients, in order to maintain perfusion of graft and vital organs, restore cardiac output, systemic blood pressure, and renal perfusion an adequate fluid resuscitation is essential. Overload is detrimental to gut function and overall recovery delay. Low perfusion state carries the risky of hepatic artery thrombosis. Achieving an appropriate level of volume management requires knowledge of the underlying pathophysiology, evaluation of volume status, and selection of appropriate monitoring device or making good judgment from corroborative multiple data, appropriate solution for volume repletion, and maintenance and modulation of the tissue perfusion [48,49,50,51].
Fluid overload recognition and assessment requires an accurate documentation of all intakes and outputs, yet there is a wide variation in practice: how it is evaluated, reviewed, and utilized. But in a nutshell it is equally important to look at assessing the intravascular status and cumulative balance. Accurate volume status evaluation is essential for appropriate therapy since errors of volume evaluation can result in either lack of essential treatment or unnecessary fluid administration, and both scenarios are associated with increased mortality. It is important to discuss fluid therapy in the team meeting - whether to adopt restrictive or liberal fluid regime. There are several methods to evaluate the fluid status; however, most of the tests currently used are fairly inaccurate. Diuretics, especially loop diuretics, remain a valid therapeutic alternative in posttransplant period to optimize the balance. Fluid overload refractory to medical therapy requires the application of extracorporeal therapies [52].
5 Fluid Assessment in ICU
It is challenging at times to evaluate a critically ill or transplant recipient in the perioperative period with altered vascular tone particularly if there is an element of sepsis. Fluid evaluation requires a critical review of intake and output chart to monitor with advance gadgets in collaboration considering the limitations of each device. Accurate volume status evaluation is essential and critical for appropriate fluid prescription. Volume status assessment errors can result in over- or under-fluid treatment, both associated with increased dysfunction of different organs leading to morbidity and mortality. There are several clinical and device tools to evaluate the fluid status; however, most of the tests currently used are fairly inaccurate at times. We need to understand and know the limitation of the device and pitfalls in the monitoring technique. Each method has gray areas where the performance is equivocal. We should try to consider other data streams and interpret in collaboration.
-
1.
Nursing documentation calculations
-
(a)
Daily fluid balance: daily difference in all intakes and all outputs including drains, CRRT fluid removal if applied which frequently does not include insensible losses.
-
(b)
Cumulative fluid balance: sum of each day fluid balance over a period of time including intraoperative balance.
-
(c)
Weight gain: Percentage of fluid overload adjusted for bodyweight: cumulative fluid balance that is expressed as a percent.
$$ \textrm{Fluid}\kern0.17em \textrm{overload}\kern0.17em \textrm{or}\kern0.17em \textrm{weight}\kern0.17em \textrm{gain}=\frac{\textrm{Total}\kern0.17em \textrm{fluid}\kern0.17em \textrm{in}-\textrm{total}\kern0.17em \textrm{fluid}\kern0.17em \textrm{out}\%}{\textrm{Admission}\kern0.17em \textrm{body}\kern0.17em \textrm{weight}}\times 100 $$ -
(d)
Clinical signs of fluid overload: usually implies a degree of pulmonary edema (PaO2/FiO2 ratios) or peripheral edema (chemosis).
-
(a)
-
2.
Radiological Imaging
-
(a)
Chest X-ray Chest X-ray has been one of the most used tests to evaluate for hypervolemia. Radiographic sings of volume overload include dilated upper lobe vessels, cardiomegaly, interstitial edema, enlarged pulmonary artery, pleural effusion, alveolar edema, prominent superior vena cava, and Kerley lines. However, a reliable single tool is not available to comment on fluid overload or cardiac dysfunction may not be good tool as may miss subtle changes.
-
(b)
Ultrasonographic assessment of IVC, lung ultrasound and jugular veins. Blue protocol and Sonographic artifacts known as B-lines that suggest thickened interstitial or fluid-filled alveoli can be detected using thoracic ultrasound. PCWP and fluid accumulation in lungs have been correlated with the presence of B-lines (“comet-tail images”) in patients with congestive heart failure and volume overload. Agricola et al. found significant correlations between comet-tail images score and extravascular lung water determined by the PiCCO System, between comet score and PCWP, and between comet-tail images score and radiologic sings of fluid overload in the lungs [34]. The measurement of the inferior vena cava (IVC) diameter can also be used to assess volume status. Normal diameter of IVC is 1.5–2.5 cm (measured 3 cm from the right atrium); volume depletion is considered with an IVC diameter <1.5 cm while an IVC diameter >2.5 cm suggests volume overload. Other IVC signs are collapsibility and distensibility in spontaneously breathing patients and in mechanically ventilated patients respectively. In an observational study Lyon et al. found significant differences between the inferior vena cava diameter during inspiration (IVCdi) and during expiration (IVCde), before and after blood donation of 450 mL [35]. There are other studies supporting the use of IVC diameter. We also use ultrasonography quite a lot in the perioperative period to evaluate the fluid and cardiac status. We try eyeballing different parameters of ultrasonography such as lung ultrasound, IJV and IVC diameters and collapsibility along with cardiac chamber sizes. In patients treated for hypovolemia, Zengin et al. evaluated the IVC and right ventricle (RVd) diameters and diameter changes with the diameters and diameter changes of healthy volunteers. The IVCd was measured ultrasonographically by M-mode in the subxiphoid area and the RVd was measured in the third and fourth intercostal spaces before and after fluid resuscitation. As compared with healthy volunteers, average diameters in hypovolemic patients of the IVC during inspiration and expiration, and right ventricle diameter were significantly lower. After fluid resuscitation, there was a significant increase in mean IVC diameters during inspiration and expiration as well as in the right ventricle diameter [36]. Bedside inferior vena cava diameter and right ventricle diameter evaluation could be a practical noninvasive instrument for fluid status estimation and for evaluating the response to fluid therapy in critically ill patients.
-
(a)
-
3.
Biochemistry: BNP levels High levels of BNP can be found with diastolic dysfunction and volume overload commonly; however, some conditions like myocardial infraction and pulmonary embolism can cause elevated levels of BNP. Other conditions that have to be taken into account when evaluating BNP levels are renal failure, which is associated with high BNP levels and obesity where there is lower BNP levels. The greatest utility of BNP levels is in the absence of elevation, since low BNP levels have a high negative predictive value for excluding heart failure diagnosis [53,54,55].
Medical history, record review, clinical signs along with routine diagnostic studies (chest radiograph, electrocardiogram, and serum B-type natriuretic peptide (BNP)) helps in overload assessment as well as to differentiate heart failure from other causes.
-
4.
Bioimpedance analysis
It is a noninvasive and inexpensive versatile test that transforms electrical properties of tissues into clinical information. Bioimpedance vector analysis (BIVA) measures whole body water. This technology is evolving to evaluate hydration status in the postoperative period particularly in patients who are on dialysis [56]. Its role may get more explored in the perioperative period to assess the excess water gain.
6 Special Considerations
6.1 LDLT vs. Cadaveric
Brain-dead donors currently remain the primary source of grafts for solid organ transplantation in the western world except in southeast Asian countries where live donor program is the backbone. In this context, appropriate management of organ donors from the diagnosis of brain death to the end of the organ procurement (OP) procedure is of paramount importance to optimize the function of potential grafts. As there is altered pathophysiology in brain-dead donors, there is dying endocrine function leading to diabetes insipidus and hemodynamic instability requiring special attention to maintain organ function of individual organ. Thus, it is of utmost importance to maintain strict balance as per the organ retrieval. However, data is limited to make an evidence-based recommendation. The current practice is of restrictive strategy using fluids with chloride restriction and starch free balanced salt solutions in this subset of patients. A French survey done by Champigneulle et al. in collaboration with SFAR research network also found similar practices and concerns by the respondents [57].
Hormonal substitution should be used to maintain hemodynamics for organ procurement particularly where retrieval is delayed in days.
As most of LDLT cases are performed electively, living donor recipients may have better compensated liver disease at the time of surgery than cadaver donor recipients. A study by Niemann et al. found that while intraoperative fluid and transfusion requirements are similar in LDLT and cadaveric recipients, the impact of transplantation on pulmonary gas exchange and reperfusion syndromes is more pronounced in patients receiving organs from cadaveric donors. Intraoperative transfusion and fluid requirements were also not significantly different in recipients from living donors versus cadaveric donors with regard to red blood cells, fresh frozen plasma, platelets, and cryoprecipitate. Authors thought that this difference probably arose from longer cold ischemia times present in the cadaveric donor group [58].
References
Parikh A, Washburn KW, Matsuoka L, Pandit U, Kim JE, Almeda J, et al. A multicenter study of 30 days complications after deceased donor liver transplantation in the model for end-stage liver disease score era. Liver Transpl. 2015;21:1160–8.
Pereira AA, Bhattacharya R, Carithers R, Reyes J, Perkins J. Clinical factors predicting readmission after orthotopic liver transplantation. Liver Transpl. 2012;18:1037–45.
Ince C, Sinaasappel M. Microcirculatory oxygenation and shunting in sepsis and shock. Crit Care Med. 1999;27:1369–77.
Beal AL, Cerra FB. Multiple organ failure syndrome in the 1990’s: systemic inflammatory response and organ dysfunction. JAMA. 1994;271:226–33.
Fink MP. Bench-to-bedside review: cytopathic hypoxia. Crit Care. 2002;6:491–9.
Fink MP, Cytopathic hypoxia. Is oxygen use impaired in sepsis as a result of an acquired intrinsic derangement in cellular respiration? Crit Care Clin. 2002;18:165–75.
Myles PS, Bellomo R, Corcoran T, Forbes A, Peyton P, Story D, et al. Restrictive versus liberal fluid therapy for major abdominal surgery. N Engl J Med. 2018;378(24):2263–74.
LTrAC survey report: US choice of resuscitation fluid in OLT. Transpl Proc. 2013;45:2258–62.
Andreucci M, Federico S, Andreucci VE. Edema and acute renal failure. Semin Nephrol. 2001;21(3):251–6.
Schrier RW, Wang W. Acute renal failure and sepsis. N Engl J Med. 2004;351(2):159–69.
Murphy CV, Schramm GE, Doherty JA, Reichley RM, Gajic O, Afessa B, et al. The importance of fluid management in acute lung injury secondary to septic shock. Chest. 2009;136(1):102–9.
Bouchard J, Mehta RL. Fluid balance issues in the critically ill patient. Contrib Nephrol. 2010;164:69–78.
McAvoy NC, et al. Alimentary pharmacology & therapeutics, vol. 43. Hoboken: Wiley; 2016. p. 947–54.
Hahn RG, Lyons G. The half-life of infusion fluids. Eur J Anaesthesiol. Jul 2016;3(7):75–482.
Myburgh JA. Resuscitation fluids. N Engl J Med. 2013;369:1243–51.
Chawla LS, Ince C, Chappell D, Gan TJ, Kellum JA, Mythen M, Shaw AD. Vascular content, tone, integrity, and haemodynamics for guiding fluid therapy: a conceptual approach. Br J Anaesth. 2014;113(5):748–55.
Wilms H, Mittal A, Haydock MD, van den Heever M, Devaud M, Windsor JA. A systematic review of goal directed fluid therapy: rating of evidence for goals and monitoring methods. J Crit Care. 2014;29:204–9.
Varadhan KK, Lobo DN. A meta-analysis of randomised controlled trials of intravenous fluid therapy in major elective open abdominal surgery: getting the balance right. Proc Nutr Soc. 2010;69:488–98.
Corcoran T, Emma Joy Rhodes J, Clarke S, Myles PS, Ho KM. Perioperative fluid management strategies in major surgery. Anesth Analg. 2012;114:640–51.
Pearse RM, Harrison DA, MacDonald N, Gillies MA, Blunt M, Ackland G, et al. Effect of a perioperative, cardiac output–guided hemodynamic therapy algorithm on outcomes following major gastrointestinal surgery. JAMA. 2014;311:2181.
Boland MR, Noorani A, Varty K, Coffey JC, Agha R, Walsh SR. Perioperative fluid restriction in major abdominal surgery: systematic review and meta-analysis of randomized clinical trials. World J Surg. 2013;37:1193–202.
Schumann R, Mandell S, Mercaldo N, Michaels D, Robertson A, Banerjee A, et al. Anesthesia for liver transplantation in United States academic centers: intraoperative practice. J Clin Anesth. 2013;25:542–50.
Gurusamy KS, Pissanou T, Pikhart H, Vaughan J, Burroughs AK, Davidson BR. Methods to decrease blood loss and transfusion requirements for liver transplantation. In: Gurusamy KS, editor. Cochrane database of systematic reviews, vol. 63. Chichester: Wiley; 2011. p. CD009052.
Wiedermann CJ, Joannidis M. Accumulation of hydroxyethyl starch in human and animal tissues: a systematic review. Intensive Care Med. 2014;40(2):160–70.
Serpa Neto A, Veelo DP, Peireira VG, de Assunção MS, Manetta JA, Espósito DC, Schultz MJ. Fluid resuscitation with hydroxyethyl starches in patients with sepsis is associated with an increased incidence of acute kidney injury and use of renal replacement therapy: a systematic review and meta-analysis of the literature. J Crit Care. 2014;29(1):185.
Van der Linden P, Dumoulin M, Van Lerberghe C, Torres CS, Willems A, Faraoni D. Efficacy and safety of 6% hydroxyethyl starch 130/0.4 (Voluven) for perioperative volume replacement in children undergoing cardiac surgery: a propensity-matched analysis. Crit Care. 2015;19(1):87.
Ryhammer PK, Tang M, Hoffmann-Petersen J, Leonaviciute D, Greisen J, Storebjerg Gissel M, Jakobsen CJ. Colloids in cardiac surgery-friend or foe? J Cardiothorac Vasc Anesth. 2017;31(5):1639–48.
Raiman M, Mitchell CG, Biccard BM, Rodseth RN. Comparison of hydroxyethyl starch colloids with crystalloids for surgical patients: a systematic review and meta-analysis. Eur J Anaesthesiol. 2016;33(1):42–8.
He B, Xu B, Xu X, Li L, Ren R, Chen Z, Xiao J, Wang Y, Xu B. Hydroxyethyl starch versus other fluids for non-septic patients in the intensive care unit: a meta-analysis of randomized controlled trials. Crit Care. 2015;19:92.
Margraf A, Herter JM, Kühne K, Stadtmann A, Ermert T, Wenk M, Meersch M, Van Aken H, Zarbock A, Rossaint J. 6% hydroxyethyl starch (HES 130/0.4) diminishes glycocalyx degradation and decreases vascular permeability during systemic and pulmonary inflammation in mice. Crit Care. 2018;22(1):11.
Quinlan GJ, Martin GS, Evans TW. Albumin: biochemical properties and therapeutic potential. Hepatology. 2005;41:1211–9.
Farrugia A. Albumin usage in clinical medicine: tradition or therapeutic? Transfus Med Rev. 2010;24:53–63.
Rozga J, Piątek T, Małkowski P. Human albumin: old, new, and emerging applications. Ann Transplant. 2013;18:205–17.
Vanek VW. The use of serum albumin as a prognostic or nutrition marker and the pros and cons of IV albumin therapy. Nutr Clin Pract. 1998;3:110–22.
Yim JM, Vermeulen LC, Erstad BL, et al. Albumin and nonprotein colloid solution use in US academic health centers. Arch Intern Med. 1995;155:2450–5.
Tarín Remohí MJ, Sánchez Arcos A, Santos Ramos B, et al. Costs related to inappropriate use of albumin in Spain. Ann Pharmacother. 2000;34:1198–205.
Schierhout G, Roberts I. Fluid resuscitation with colloid or crystalloid solutions in critically ill patients: a systematic review of randomized trials. BMJ. 1998;316:961–4.
Casuccio A, Nalbone E, Immordino P, Laseta C, Sanfilippo P, Tuttolomondo A, Vitale F. Appropriateness of requests for human serum albumin at the University Hospital of Palermo, Italy: a prospective study. Int J Qual Health Care. 2015;27(2):154–60.
Zhang Z, Dai X, Qi J, Ao Y, Yang C, Li Y. Effect of albumin administration on post-operation mortality, duration on ventilator, and hospital stay on patients in cardiac intensive care: an observational study. Trop J Pharm Res. 2019;18(6):1339–45.
Boldt J, Knothe C, Zickmann B, et al. Influence of different intravascular volume therapies on platelet function in patients undergoing cardiopulmonary bypass. Anesth Analg. 1993;76:1185–90.
Zhou FH, Liu C, Mao Z, Ma PL. Normal saline for intravenous fluid therapy in critically ill patients (Review Article). Chin J Traumatol. 2018;21:11–5.
Bouchard J, Soroko SB, Chertow GM, Himmelfarb J, Ikizler TA, Paganini EP, et al. Fluid accumulation, survival and recovery of kidney function in critically ill patients with acute kidney injury. Kidney Int. 2009;76(4):422–7.
Hoste EA, Maitland K, Brudney CS, Mehta R, Vincent JL, Yates D, Kellum JA, Mythen MG, Shaw AD, ADQI XII Investigators Group. Four phases of intravenous fluid therapy: a conceptual model. Br J Anaesth. 2014;113(5):740–7.
Marik PE. Hemodynamic parameters to guide fluid therapy. Transfus Alter Transfus Med. 2010;11(3):102–12.
Marik PE, Cavallazzi R, Vasu T, et al. Dynamic changes in arterial waveform derived variables and fluid responsiveness in mechanically ventilated patients. A systematic review of the literature. Crit Care Med. 2009;37:2642–7.
Michard F, Teboul JL. Predicting fluid responsiveness in ICU patients: a critical analysis of the evidence. Chest. 2002;121:2000–8.
Cinotti R, Roquilly A, Mahé P-J, Feuillet F, Yehia A, Belliard G, et al. Pulse pressure variations to guide fluid therapy in donors: a multicentric echocardiographic observational study. J Crit Care. 2014;29:489–94.
Al-Khafaji A, Elder M, Lebovitz DJ, Murugan R, Souter M, Stuart S, et al. Protocolized fluid therapy in brain-dead donors: the multicenter randomized MOnIToR trial. Intensive Care Med. 2015;41:418–26.
Prowle JR, Echeverri JE, Ligabo EV, Ronco C, Bellomo R. Fluid balance and acute kidney injury. Nat Rev Nephrol. 2010;6(2):107–15.
Levy MM, Artigas A, Phillips GS, Rhodes A, Beale R, Osborn T, et al. Outcomes of the Surviving Sepsis Campaign in intensive care units in the USA and Europe: a prospective cohort study. Lancet Infect Dis. 2012;12(12):919–24.
Kellum JA, Lameire N, Kidney Disease Improving Global Outcomes (KDIGO) Working Group. Section 3: prevention and treatment of AKI. Kidney Int Suppl (2011). 2012;2(1):37–68.
Mehta RL, Bouchard J. Controversies in acute kidney injury: effects of fluid overload on outcome. Contrib Nephrol. 2011;174:200–11.
Granado RC-D, Mehta RL. Fluid overload in the ICU: evaluation and management. BMC Nephrol. 2016;17:109.
Peacock WF, Soto KM. Current techniques of fluid status assessment. Contrib Nephrol. 2010;164:128–42.
Bagshaw SM, Cruz DN. Fluid overload as a biomarker of heart failure and acute kidney injury. Contrib Nephrol. 2010;164:54–68.
Lukaski HC, Diaz NV, Talluri A, Nescolarde L. Classification of hydration in clinical conditions: indirect and direct approaches using bioimpedance. Nutrients. 2019;11:809.
Champigneulle B, Arthur Neuschwander A, Bronchard R, Favé G, Josserand J, Lebas B, Bastien O, Pirracchio R, SFAR Research Network. Intraoperative management of brain-dead organ donors by anesthesiologists during an organ procurement procedure: results from a French survey. BMC Anesthesiol. 2019;19:108.
Carrier FM, Chassé M, Wang HT, Aslanian P, Bilodeau M, Turgeon AF. Effects of perioperative fluid management on postoperative outcomes in liver transplantation: a systematic review protocol. Syst Rev. 2018;7:180.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Gautam, P.L. (2023). Fluid Therapy in Liver Transplant. In: Vohra, V., Gupta, N., Jolly, A.S., Bhalotra, S. (eds) Peri-operative Anesthetic Management in Liver Transplantation. Springer, Singapore. https://doi.org/10.1007/978-981-19-6045-1_19
Download citation
DOI: https://doi.org/10.1007/978-981-19-6045-1_19
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-19-6044-4
Online ISBN: 978-981-19-6045-1
eBook Packages: MedicineMedicine (R0)