Abstract
Low birth weight (LBW) and preterm births make babies more vulnerable for disease and death in the neonatal period in India and worldwide (Estimates generated by the WHO and Maternal and Child Epidemiology Estimation Group (MCEF) 2018: leading causes of neonatal deaths in India. http://data.unicef.org). Of the 20 million LBW babies born globally each year, 97% are born in low–middle income countries (40% in India), and 80% of neonatal deaths occur in this group. Unlike LBW, preterm births are prevalent in both high- and low-income countries and are the most common cause of disability and death. Of more than 15 million preterm births (10.6% of total live births), 81% are in Asia and sub-Saharan Africa. In India, premature birth rate is 14 per 1000 live births. Worldwide, 10% of all neonatal deaths occur in premature births (in Indian up to 44% mortality). This risk is on the rise with the increase in preterm birth rate in many countries. Neonatal mortality rate (NMR) is an indicator of a country’s health status. Indian NMR has decreased from 5.7% to 4.1% over 10 years, as in 2017 (Estimates generated by the WHO and Maternal and Child Epidemiology Estimation Group (MCEF) 2018: leading causes of neonatal deaths in India. http://data.unicef.org).
Of the various factors impacting NMR, maternal factors (undernutrition, anaemia, and diseases) are most important affecting fetal growth, maturation, and overall neonatal outcome. Surgical mortality in neonates is also very high, varying on a country’s health infrastructure and development, ranging from 6.7% in South Korea (Lee et al., J Korean Assoc Pediatr Surg 2006, http://www.koreamed.org/SearchBasic.php?RID=0053JKAPS/2006.12.2.137&DT=1) to 7.5% in Japan (Taguchi, Surg Today 38:379–89, 2008) and 35% in India (Gangopadhyay et al., Indian J Pediatr 75:1025–30, 2008) to 45% in Nigeria (Chirdan et al., Semin Pediatr Surg 21:151–9, 2012).
This chapter will discuss the impact of maternal health and common medical diseases on fetal growth and development and the risks in the baby after birth. This will also affect perioperative morbidity and mortality in the surgical neonates.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Undernutrition
- Fetal growth restriction (FGR)
- Anaemia
- Obesity
- Maternal diseases
- Chemotherapy
- Multiple pregnancies
- COVID
1 Introduction
Low birth weight (LBW) and Preterm births make babies more vulnerable for disease and death in the neonatal period in India and Worldwide. Of 20 million LBW babies born annually, global, 97% are from low-middle income countries (nearly 40% from India), and responsible for 80% of neonatal deaths (neonatal mortality). However, incidence of preterm births is independent of income status, and is the most common cause of disability, and death. in India, premature birth rate is 14 per 1000 live births, with nearly 44% mortality rate. [1] of various factors affecting Neonatal Mortality Rate (NMR), maternal factors (undernutrition, anemia, diseases) and health have a direct and profound impact on intrauterine fetal health , the foundation of neonatal and infant health. Surgical mortality in this age group is very high, depending on a country’s development and health infrastructure, nearly 6.7% in South Korea [2], 7.5% in Japan [3], 35% in India [4] and 45% in Nigeria [5]. To optimize neonatal outcome , it is extremely important to maintain good maternal health.
Health is not merely absence of disease and starts with preconceptional nutritional status of the woman, along with the absence of adverse environmental factors (smoking, alcohol, drug abuse, and stress), and encompasses supervised healthy antenatal period.
Undernutrition is an important factor, basis of most diseases in women in the reproductive age group, worldwide. Undernutrition tops the list of medical disorders , obstetric , and miscellaneous maternal factors that impact neonatal health.
Besides maternal health and disease status, other factors contributing to neonatal mortality rate (NMR) are age at delivery , educational status , nutritional status , and parity . Risk of neonatal deaths and low birth weight (LBW) babies is 50% more in mothers under 20 years of age.
Maternal factors affecting fetal health and thereby neonatal death are listed in Table 2.1.
2 Undernutrition in Pregnancy
Maternal nutrition plays a key role in ensuring appropriate fetal growth and development. Nutritional requirement (macronutrient and micronutrients ) is greatly augmented in pregnancy, with additional 350–450 kcal/day in the 2nd and 3rd trimesters. Adequate balanced diet is essential for good feto-maternal outcome and neonatal well-being.
Maternal undernutrition impairs the formation of placenta, uteroplacental circulation, and nutrient delivery to the fetus, resulting in FGR/IUGR, LBW, small for gestational age (SGA), preterm delivery, and birth defects.
Prematurity and congenital anomalies are two important factors of high NMR . 74.8% of all deaths due to prematurity occur in 1st week of life (30% within 1st few hours of birth). 75% of all deaths from congenital defects occur in 1st week of life (almost 50% within 24 h of birth).
Maternal weight gain and gestational weight gain are parameters of maternal nutritional status and fetal growth. Optimal maternal weight should be > 45 kg at any period of gestation, and gestational weight gain should be >300 g/week. The Barker hypothesis [6] postulates that undernutrition during pregnancy results in fetal programming, i.e., permanent alteration in fetal morphology and physiology. Epidemiologic studies have shown increased risk of ischemic heart disease and related disorders in later life in babies born during famine situation.
2.1 Micronutrients [7,8,9,10]
Deficiency of micronutrients (iron , vitamins , calcium , zinc , iodine , folic acid , and magnesium ) is also associated more with feto-maternal complications.
-
1.
Iron is a cofactor for synthesis of haemoglobin (Hb) and myoglobin, and various cellular functions (O2 transport, respiration, growth, gene regulation, and iron-dependent enzymes). Iron deficiency is the most common cause of anaemia in pregnancy worldwide and is associated with greater risk of preterm birth, LBW, SGA, infections, and abnormal psychomotor and cognitive function development in babies.
-
2.
Vitamins
-
(a)
Vitamin A is important for growth, bone metabolism, immune and antioxidant function, gene transcription, vision, and sight. Its deficiency increases the risk of LBW and neonatal mortality. Vitamin A supplement does not reduce the incidence of complications.
-
(b)
Vitamin B complex (B1 (Thiamine ), B2 (Riboflavin ), B3 (Niacin ), B6 (Pyridoxine ), and B12 (Cyanocobalamin )) are required metabolism and energy production at cellular level, RBC formation, and conversion of homocysteine to methionine (role in methylation of RNA, DNA, neurotransmitters, and phospholipids). Vitamin B deficiency affects cellular growth and nerve tissue development. B1 deficiency impairs fetal brain development, B2 deficiency increases risk of CHD and LBW, and B12 deficiency causes macrocytic anaemia and increases the risk of abruptio placenta, still birth, LBW, and preterm delivery.
-
(c)
Vitamin C and Vitamin E promote antioxidation and reduce production of free radicals, thereby reducing oxidative stress. Vitamin C also mobilizes iron from body stores, increases GI absorption of iron, and prevents megaloblastic and iron deficiency anaemias, besides its role in collagen synthesis and connective tissue stabilization. Vitamin C by its antioxidant role, and ability to cross-placental barrier, reduces the effects of PET, IUGR, preterm birth, and premature rupture of membranes. Vitamin E cannot cross placental barrier.
-
(d)
Vitamin D has a role in calcium homeostasis and bone integrity. It also has a role in glucose metabolism, inflammatory and immune responses and angiogenesis, and gene transcription. It is important for fetal bone growth, and its deficiency is the cause of neonatal rickets, preterm, and LBW babies.
-
(a)
-
3.
Calcium is essential for bone mineralization and maintains cell wall integrity and role in haemostasis and coagulation cascade, muscle contraction, enzyme and hormone homeostasis, neurotransmitter release, and nerve cell function. Its deficiency is a risk factor for preterm labor, LBW, preterm birth, and reduced fetal mineralization. Calcium supplement reduces the risks of these complications.
-
4.
Zinc is a catalytic for various enzymes and is a part of nucleotide, proteins, and hormones. It has a role in protein nucleic acid synthesis and metabolism, cell division, gene expression, antioxidation, wound healing and immune responses, vision, and neurological function. Its deficiency is associated with LBW, IUGR, congenital defects, and pre- and post-term births and is a reason for high maternal and infant deaths in developing countries. Zinc supplement is beneficial.
-
5.
Iodine is essential for growth and development and synthesis of thyroid hormones. It has a key role in fetal brain and CNS development, and myelination. Its deficiency causes fetal and neonatal hypothyroidism, goitre, and cognitive impairment. Severe deficiency leads to stunted growth (cretinism), irreversible neurological damage, and death.
-
6.
Folic acid is a coenzyme for methylation process (DNA, neurotransmitters) protein metabolism, and cell multiplication, and is especially important mineral in the fetal embryonic stage. Its deficiency leads to homocysteine accumulation, fetal anomalies, and neural tube defects . Folic acid supplementation is preventive. Folic acid supplements are beneficial.
-
7.
Magnesium is important for enzyme functioning, cell membrane integrity, synthesis of DNA, RNA ATP, and cAMP. Fetal effects of its deficiency are growth retardation, SGA, IUGR, and preterm birth. Magnesium supplementation can reduce these risks.
3 Assessment of Fetal Health
Impact on fetal growth and development and thereby neonatal outcome can be assessed by:
-
1.
Estimated fetal weight (EFW)
-
2.
BW
3.1 EFW [11,12,13,14]
Both small and large for gestational age (SGA, LGA) neonates carry high risk of morbidity and mortality. Timely detection can reduce this risk. Various methods to detect growth in antenatal period include symphysis fundal height ( SFH in centimetres is equal to the GA in weeks), ultrasonography (Hadlock equation is used for GA and Shepard and Hadlock equation for fetal weight), and biometric parameters (BPD —biparietal diameter, HC—head circumference, and FL—femur length).
Average fetus weighs 80 g (2.8 oz) by end of 1st trimester and grows reaching weekly weight increase of 220 g (7.8 oz) up to 35 weeks, followed by a decline to weekly gain of 185 G (6.5 oz) until 40 weeks.
3.1.1 Fetal Growth Restriction (FGR/IUGR) [15,16,17,18]
The fetus fails to attain full growth potential, as estimated by EFW or abdominal circumference less than 10th percentile for the GA (ACOG). Moderate FGR is BW in the 3rd–10th percentile, while severe FGR is BW less than 3rd percentile.
FGR is associated with mild-to-moderate chronic O2 and substrate deficiency and depending on the time of pathological exposure (Table 2.2), and is classified as:
-
1.
Symmetric (20–30% of all FGR): exposure early in the gestation period, characterized by global impairment of cellular hyperplasia and proportional decrease in all fetal organs
-
2.
Asymmetric (70–80% of all FGR): exposure late in gestation, characterized by a greater decrease in abdominal size (liver volume and subcutaneous fat tissue) than the HC. The fetus adapts by redistribution of blood flow to vital organs (brain, heart, and placenta), compromising flow to nonvital organs (abdominal viscera, lungs, kidneys, and skin)
FGR causes fetal heart rate (FHR) abnormalities and fetal distress (passage of meconium, preterm births, birth asphyxia, still births, and acidosis), 10% are associated with congenital abnormalities (omphalocele, gastroschisis, diaphragmatic hernia, skeletal dysplasia, and congenital heart defects), and 20–60% of malformed neonates are SGA.
Reduced subcutaneous fat and impaired thermoregulation puts them at risk of hypothermia. Chronic intrauterine hypoxia results in polycythemia, hyperviscosity, hypoglycaemia (low hepatic glycogen reserve), and other metabolic abnormalities. They are afflicted with dual morbid states (prematurity and dysmaturity ) with adverse consequences (necrotizing enterocolitis (NEC), low Apgar score, IVH—intraventricular haemorrhage, and HIE—hypoxic ischemic encephalopathy) and its sequelae , broncho pulmonary dysplasia (BPD), respiratory distress syndrome (RDS), chronic lung disease, retinopathy of prematurity (ROP), prolonged NICU stay, sepsis, and death . Long-term adverse neurodevelopmental outcomes (cognitive impairment and cerebral palsy) occur in survivors.
FGR neonates require expert care at birth and baby should be evaluated for signs of structural and chromosomal abnormalities and infections. Because of accelerated postnatal growth, they are at risk of obesity, hyperlipidaemia, metabolic dysfunction, insulin resistant type 2 diabetes, cardiovascular, and renal disease in childhood.
3.2 Birth Weight [19,20,21,22]
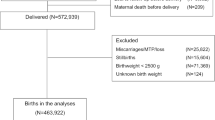
Antenatal fetal weight estimate is important because of the potential complications during labor and puerperium arising from fetal prematurity or IUGR . Common classification uses BW alone: LBW (1501–2500 g), very LBW (VLBW) (1001–1500 g), extremely LBW (ELBW) (500–1000 g), and micropremies (<400 g).
BW over 4000 g is considered as overweight (fetal macrosomia ) and may be associated with birth injuries (shoulder dystocia, brachial plexus palsy, and fractures), prolonged/obstructed labor /cephalopelvic disproportion (CPD)/instrumental/Caesarean deliveries, birth asphyxia /low Apgar scores , maternal injuries, and post-partum hemorrhage (PPH).
Factors that influence BW include:
-
a. Fetal factors (GA, gender)
-
b. Maternal factors [race, height, weight, parity , weight gain, physical activity, Hb concentration, tobacco use, DM, pregnancy-induced hypertension (PIH), and eclampsia]
-
c. Others (paternal factors and ambient altitude)
4 Maternal Diseases Affecting Neonatal Health
4.1 Anaemia [23,24,25,26,27,28]
Anaemia is the most common haematological disorder in women of reproductive age group. As per the World Health Statistics data 2016, almost 30% of reproductive aged and 40% pregnant women are anaemic. There is wide regional and global variation in the prevalence of anaemia in pregnancy, reflecting socioeconomic and nutritional status differences. In the South–East Asian countries, about 50% of all maternal deaths are due to anaemia or its complications. Prevalence of anaemia in pregnancy in India has decreased from 58% in NFHS-3 (National family health survey-3) to 50% in NFHS-4 survey (2015–16).
Causes of anaemia in pregnancy include:
-
1.
Physiological (dilutional)
-
2.
Iron deficiency
-
3.
Other nutritional deficiencies: folate and vitamin B12
-
4.
Hemoglobinopathies
-
5.
Hypothyroidism
-
6.
Chronic kidney disease (CKD)
-
7.
Chronic infections/helminthic infections
-
8.
Autoimmune haemolysis
There is a correlation between maternal anaemia and risk of preterm birth, low BW, SGA, low Apgar scores, and increased perinatal and maternal mortality. Iron deficiency is the most common cause of anaemia and a leading cause of anaemia-related maternal deaths [2]. Hb <10.9 g% as a cutoff to define anaemia in pregnancy. Prevalence of anaemia increases from 7% in 1st trimester to 24–39% in 2nd and 3rd trimesters. (Table 2.3)
The incidence and severity of anaemia is much higher in resource poor as compared to the developed countries, due to low socio-economic status, poor nutrition, lack of access to adequate health care facilities, prevalence of helminthic infections, malaria, inflammatory, and infectious conditions. Severity of anaemia is graded into mild (10–10.9g%), moderate (7–9.9g%), severe (4–6.9g%), and very severe (<4g%), depending on the Hb concentration.
Iron requirement in pregnancy is three times that of nonpregnant state, and the demand increases as pregnancy progresses from 4 to 6 mg/day in the 2nd trimester to 10 mg/day in the 3rd trimester. The total iron requirement is 840 mg (accounting for fetus, placenta, expansion of maternal red cell mass, and the blood loss at delivery).
Maternal iron deficiency predisposes fetus to iron deficiency. Iron is important for normal brain development, dendritic growth, synapse formation, and behaviours (grooming, timidity, poor spatial learning, and tasks requiring executive function). Long-term follow-up of infants who had iron deficiency for 3 months or more in their 1st year of life revealed that they were at high risk of cognitive impairment and autistic disorders, but since iron deficiency coexists with other nutritional deficiencies, it is difficult to attribute iron deficiency as a direct cause of cognitive impairment [29].
4.2 Haematological Disorders in Pregnancy
4.2.1 Thalassemia
Beta thalassemia minor is not associated with any higher risk of adverse outcomes in the neonates, except for higher incidence of neural tube defects due to relative folate deficiency in the mother. β-Thalassemia major women tend to be infertile due to chronic iron overload and associated endocrinopathies. However, pregnancies are associated with higher risk of pregnancy loss, prematurity, and FGR due to fetal hypoxia from maternal anaemia. Teratogenic effects of iron chelating agents include vertebral aplasia, abnormalities of ribs and retarded bone ossification, cephalo-pelvic disproportion, and operative deliveries.
4.2.2 Pregnancy in Women with Sickle Cell Disease
Pregnancy in women with sickle cell disease may cause worsening maternal anaemia and sickling crisis. They may also develop pyelonephritis, haematuria, PET, prematurity, IUGR, and abruption.
4.3 Obesity and Pregnancy
Obesity is associated with an array of maternal and perinatal complications , degree of risk amplified with increasing severity of obesity. Class II obesity or greater and high gestational weight gain are at the highest risk of complications. Obesity is defined by a body mass index (BMI) >30 kg/m2 and can be further stratified into three severity classes, class 1 (30–34.9 kg/m2), class 2 (35–39.9 kg/m2), and class 3 (>40 kg/m2). In Indian population, BMI >25 kg/m2 is classified as obese, on account of the higher metabolic risks at lower BMI as compared to the west.
Obesity is a metabolic dysregulator. Excessive adipose tissue has a dysregulatory effect on metabolic, vascular, and inflammatory pathways, affecting placental growth and function, with risk of preeclampsia and FGR. Obesity-associated insulin resistance exposes fetus to high sugar levels, insulin, lipids, and inflammatory mediators, inducing epigenetic changes in the metabolic pathways and increasing the risk of hypertension, coronary artery disease, and diabetes in middle age ( Barker hypothesis ) [6].
Obese pregnant women are at risk of obstructive sleep apnea (OSA) , early pregnancy loss, developing gestational hypertension and diabetes , occult type 2 diabetes, and PIH , and eclampsia. Multifetal pregnancy, congenital abnormalities , preterm and post-term birth , operative delivery , fetal death , still birth, birth asphyxia , and congenital defects (neural tube defects, cardiovascular anomalies, cleft palate, Anorectal atresia, and limb reduction anomalies) are also common [30].
4.4 Antiphospholipid Syndrome
Antiphospholipid syndrome can present with recurrent miscarriages , uteroplacental insufficiency and FGR , preterm delivery , PET , abruption , and fetal death . These occur due to impaired development of trophoblast and thrombosis of uteroplacental vasculature . Babies born are at a higher risk of vascular thrombosis (arterial, venous or small vessel).
4.5 Diabetes Mellitus in Pregnancy [31, 32]
Gestational diabetes mellitus (GDM) accounts for 90% cases of DM in pregnancy and 50% develop DM within 5–10 years. In 2019, there were 223 million diabetic women (20–79 years) and 20 million births. In 16% of live births, there was form of hyperglycaemia during pregnancy, and 1 in 6 births was affected by GDM. A vast majority of GDM cases were from low- and middle-income countries.
In GDM, pancreatic β-cell dysfunction prevents increase in insulin secretion, leading to maternal and fetal hyperglycaemia . In the fetus, insulin secretion increases. Insulin is an important growth factor. Hyperinsulinemia results in fetal macrosomia (BW > 4000 g), increased subcutaneous fat, and muscle mass.
4.5.1 Effects Maternal GDM on the Baby
The risks to the newborn are due to macrosomia , hyperglycaemia and hyperinsulinemia and increased incidence of intra uterine death (IUD ) and perinatal asphyxia :
-
1.
Diabetic embryopathy and congenital anomalies —heart disease, anencephaly, spina bifida, microcephaly, and caudal regression syndrome
-
2.
LGA , i.e., BW at or above the 90th percentile for GA, and macrosomia (BW ≥4500 g), fetal hyperglycaemia, hyperviscosity, polyuria, hyperinsulinemia (fetal islet cell hyperplasia), and asymmetric fetal growth (broader shoulders, large thoracic, and abdomen). These increase the risk of operative or instrumental delivery, still birth and birth injuries (shoulder dystocia, brachial plexus injury, and fracture), and neonatal depression
-
3.
Newborn hypoglycaemia due to islet cell hyperplasia, hyperbilirubinemia, hypocalcaemia, hypomagnesemia, polycythemia, cardiomyopathy, and birth defects
-
4.
Risk of RDS from hyperinsulinemia blocking cortisol-induced lung maturation
-
5.
Long-term consequences : risk of childhood obesity, diabetes, insulin resistance, cardiovascular diseases, and poor neurodevelopmental outcomes
4.6 Pregnancy and Infectious Diseases [33,34,35]
Infectious diseases are the major cause of late neonatal death (8–28 days). 30–40% of all neonatal deaths occur from infections, 50% occur in 1st week, 30% in 2nd week, and 20% in the 3rd–4th week of age. Common infections are acute respiratory infections (ARI) (30%), bacterial sepsis (40%), meningitis (40%), diarrhea (0.6%), and tetanus.
-
(a)
ARI : commonest organism isolated is streptococci pneumonia. Mortality is high in LBW, malnourished, and preterm neonates.
-
(b)
Maternal tuberculosis increases the risk of fetal loss, preterm delivery, and LBW.
-
(c)
Neonatal diarrhea contributes to 3% of all deaths.
-
(d)
Neonatal tetanus is contracted from an unimmunized mother, unhygienic delivery , and poor cord care. Once contracted, it is almost fatal. Newborn loses ability to suck at 3–10 days of age and develops spasms, stiffness, and convulsions, and dies.
-
(e)
Sexually transmitted diseases (STD) : Syphilis is usually transmitted from the mother via placenta and can result in fetal death or disability in 50–80% affected pregnancies. Congenital syphilis is associated with IUGR, anemia, thrombocytopenia, jaundice, hepato-splenomegaly, and neurological manifestations (mental retardation, hydrocephalus, cranial nerve palsies, and seizures) in the baby. Gonorrhea increases the risk of conjunctivitis in the newborn and later blindness. Chlamydia also exposes newborn to conjunctivitis and pneumonia. Genital herpes can lead to neonatal herpes with high mortality and neurodevelopmental sequelae among survivors.
-
(f)
UTI and untreated bacteriuria are associated with increased risk of LBW, preterm birth, and high perinatal mortality [33].
-
(g)
Malaria is associated with IUGR and LBW.
-
(h)
Omphalitis (umbilical infection) is a unique problem in developing countries, attributed to unhygienic home deliveries, poor cord hygiene (nonsterile cutting and unhygienic tying), and local umbilical infection (leads to necrotizing fasciitis).
-
(i)
Omphalitis along with neonatal tetanus increases the risk of neonatal sepsis and death.
4.6.1 Rubella (German Measles ) [ 36,37,38,39]
Rubella is a self-limited infection, but maternal rubella can spread trans placentally to the fetus. Hematogenous spread in the fetus causes vascular cellular damage and ischemia of the affected organs. Rubella infection in pregnancy gains its significance from its teratogenic effects. Preconception or 1st trimester Rubella is associated with the risk of abortion, still birth, and birth defects. The risk of fetal infection is up to 81% in 1st trimester, 25% in 2nd, and 35% at 27–30 weeks and 100% after 36 weeks of gestation. Rubella is an important cause of severe birth defects in endemic countries. During 1996–2010 of more than one lakh infants with congenital rubella syndrome (CRS) , 38% were from India.
During the global rubella pandemic of 1964–65, there were thousands of abortions, neonatal deaths, and CRS in newborns in United States. Rubella vaccine was introduced in 1969 and US has been able to eliminate CRS only in 2004. Rubella outbreaks (>2000 cases) were reported from Romania, Japan, and Poland in 2012.
Indian scenario : during a surveillance (2016–18) of 645 suspected CRS cases, 21.2% (137) were confirmed CRS. Of these 137 CRS patients, 78.8% had cardiac defects, 59.9% had eye signs (cataract, glaucoma, and retinopathy), and 38.6% had hearing impairment. 24.1% died over 2-year period.
CRS and the neonate : the classical triad of CRS includes Congenital cataract and glaucoma, congenital heart disease (CHD) patent ductus arteriosus (PDA), pulmonary stenosis (PS), and sensorineural deafness. Other effects are developmental delays, purpura, retinopathy, hepatosplenomegaly, jaundice, IUGR, myocarditis, microcephaly, and meningoencephalitis. DM, thyroid disorder, and panencephalitis can occur later in life [39].
Active rubella infection in a woman is a contraindication to conception until sero-negativity is achieved.
4.7 Liver Disease [40,41,42]
Babies of mothers with hepatitis are at risk of getting the infection from the mother:
-
(a)
Intrahepatic cholestasis of pregnancy (IHCP) is associated with adverse perinatal outcomes (preterm birth, fetal distress, perinatal death, and meconium staining of liquor). Bile acids in circulation cause vasoconstriction of placental chorionic vessels, fetal asphyxia, and uterine hypertony.
-
(b)
Acute viral hepatitis ( Hepatitis B ) may be associated with miscarriage, preterm labor, and LBW. The risk of vertical transmission to the newborn is 20–30%. If the mother is both HBsAg and HBeAg positive, the risk of transmission is 90%.
-
(c)
In Hepatitis C infection , risk of vertical transmission is 5–10%.
4.8 Renal Disease [43,44,45,46]
Women with significant chronic kidney disease (CKD ) are less likely to become pregnant. Even mild disease is associated with adverse maternal and fetal outcomes. Acute pyelonephritis can trigger preterm labor from fever-induced uterine hyperactivity but usually with no fetal loss.
CKD (with proteinuria and hypertension) is associated with higher incidence of SGA, LBW, FGR, and preterm birth. Fetal survival is poor when preconception blood pressure is uncontrolled (>140/90 mmHg). MAP >105 mmHg at conception carries tenfold higher risk of fetal death, higher risk of maternal events than in normotensive CKD, while during dialysis, intravascular volume and blood pressure fluctuations can be deleterious to the fetus.
Renal transplant recipients have a much lower pregnancy rate either due to infertility or from counselling (use of teratogenic drugs). There is fetal risk of prematurity, FGR, congenital anomalies, RDS, suppressed haematopoiesis, and liver dysfunction.
Drugs for CKD: angiotensin converting enzyme inhibitors (ACEI) and angiotensin receptor blockers (ARB) are preferred drugs because of their antihypertensive and antiproteinuric effects. However, they can cause fetal abnormalities. Diuretics also should be used sparingly and in minimal doses (to prevent volume contraction and electrolyte abnormalities). Loop diuretics (Lasix) are safe in pregnancy. Women on immunosuppressants (calcineurin inhibitors/glucocorticoids) are at higher risk of GDM, infections, and bacterial UTI and adverse fetal consequences.
4.9 Maternal Malignancy and the Fetus [47,48,49]
With advancement in perinatal care and cancer therapy, one is more likely to face a situation where pregnancy is complicated by malignancy in the mother. Malignancy is a high stress state with pathophysiological, metabolic, and biochemical effects in the body, and adverse maternal and fetal effects .
Four treatment modalities exist : surgery , chemotherapeutic (CT) drugs, radiotherapy (RT) , and a combination of these:
-
1.
Surgery can be performed during any trimester.
-
2.
Radiotherapy can be given in the 1st and 2nd trimesters, but is associated with risk of birth defects, IUGR, miscarriage, higher risk of childhood cancer.
-
3.
Chemotherapy is rarely used during pregnancy. The risks depend on the drug used and period of gestation. They should not be used in the 1st trimester when organogenesis is occurring because of the risk of congenital malformations and fetal loss. The effect of CT drugs on the fetus may be in the form of IUGR, LBW, SGA, bone marrow toxicity, cognitive impairment, and cardiac effects. Prematurity is most common accompanied by its own adverse effects on the baby.
-
4.
Tamoxifen and Transtuzumab are contraindicated in pregnancy. Women with history of breast cancer are at higher risk of Preterm labor, LBW, or SGA, especially if they received CT or gave birth within 2 years of diagnosis.
However, a study in 2015 could not demonstrate a significant difference in cognitive ability, school performance or behavioral competence in children exposed to CT in utero compared to nonexposed children > 18 months of age, though prematurity was more prevalent in the CT exposed children.
4.10 Epilepsy in Pregnancy [50,51,52,53,54,55]
Epilepsy is a common neurological disorder with prevalence up to 1% in pregnancy. Pregnancy is usually uneventful, but they are at risk of fetal complications (poor fetal growth FGR/IUGR, congenital malformations, prematurity, preterm labor, and adverse neurodevelopmental outcomes in neonates).
Women with epilepsy suffer from anxiety and distress, for fear of harming or injuring the baby and the effect of anti-epileptic drugs (AED) . Maternal AED exposure is associated with increased risk of preterm birth, FGR, and congenital malformations (4–6%). Common malformations include neural tube, congenital heart and urinary tract defects, skeletal abnormalities, and oral clefts (Table 2.4). Babies born to mothers on AED may have excessive sedation, lethargy, feeding difficulty, and withdrawal symptoms with inconsolable crying, particularly in preterms.
AEDs have anti folate reductase activity. Low serum folate level is independently associated with higher risk of congenital malformations. Folic acid supplementation diminishes this risk and improves autistic, cognitive, and behavioural outcomes. Family history of birth defects and low level of maternal education are additional risk factors.
Valproate is the major risk, while topiramate , phenytoin , and phenobarbital are of intermediate risk, and levetiracetam and Lamotrigine are least teratogenic and safer in pregnancy.
Enzyme-inducing drugs (carbamazepine, phenytoin, phenobarbital, primidone, oxcarbazepine, and topiramate) can affect the fetal microsomal enzymes and vitamin K degradation in the fetus, inhibiting clotting factor precursors, increasing the risk of haemorrhagic disease of newborn.
Maternal seizures , especially generalized tonic–clonic seizures (GTCS), are hazardous for the fetus. Hypoxia and lactic acidosis during a seizure episode leads to fetal hypoxia due to decreased placental transfer of O2 or postictal apnea in the mother, with decelerations lasting up to 30 min after the seizure. GTCS of 5 or more can cause developmental delay in the fetus and is a negative predictor of verbal intelligence quotient. Other types of seizures are associated with FGR, preterm delivery, and fetal injury. Epileptic seizures in labour are managed by benzodiazepines. There is a risk of neonatal withdrawal syndrome with use of benzodiazepines and AED.
5 Multiple Pregnancy
This is associated with higher miscarriage rate, preterm labour (due to overdistension of uterus, hydramnios, and premature rupture of membranes), discordant twin growth (difference of EFW of >25% between the twins), and single IUD with neurological complications in second twin. Fetal anomalies are more common in monozygotic twins including anencephaly, microcephaly, hydrocephalus, cardiac anomalies, and Down’s syndrome.
6 COVID in Pregnancy
COVID is a new infection, and much data are not available, suggesting increased risk of miscarriage or congenital malformations, FGR, because of COVID-19. However, possibly 2/3rd pregnancies with SARS suffered FGR. Maternal COVID can lead to placental insufficiency and poor uteroplacental perfusion (chorionic intervillous inflammation, thrombosis, and focal avascularisation of the villi), fetal hypoxia, and risk of prematurity.
As per the UK obstetric surveillance system (UKOSS) cohort in 2020, of 265 newborns born to COVID positive mothers, 75% were preterm, 25% required NICU care, and 5% tested positive for COVID [56].
7 Conclusion
Maternal health and disease are the most important factors that can affect development and growth of the fetus. Maternal undernutrition, micronutrient deficiency, diseases commonly being anaemia, and others can have adverse effects on the fetus and the newborn baby. Common is IUGR/FGR, SGA, congenital defects, perinatal asphyxia, CHD, craniovertebral anomalies and neural tube defects, RDS, BPD, IVH, and prematurity.
Anaesthesiologist will likely face these neonates during the course of treatment in NICU or for surgery, and complete evaluation must be done for any birth defects and anomalies. Maternal details, e.g., age at delivery, educational and economic status, parity, whether ANC care provided and regarding complications during the period of pregnancy, etc., can provide a clue to the status of the neonate, and help assess risk of anesthesia and surgery, and take precautions to reduce them.
Most mishaps happen during transport of these sick premature babies from one area to another, especially if unsupervised. These neonates must be transported in preheated incubators with humidity and temperature control and facility for providing O2 and under supervision of a medical personnel. This can go a long way in improving perioperative outcome.
References
Estimates generated by the WHO and Maternal and Child Epidemiology Estimation Group (MCEF) 2018: Leading Causes of Neonatal Deaths In India. http://data.unicef.org
Lee EJ, Choi KJ. Mortality analysis of surgical neonates: a 20-year experience by a single surgeon. J Korean Assoc Pediatr Surg. 2006. Disponível em: http://www.koreamed.org/SearchBasic.php?RID=0053JKAPS/2006.12.2.137&DT=1.
Taguchi T. Current progress in neonatal surgery. Surg Today. 2008;38(5):379–89.
Gangopadhyay AN, Upadhyaya VD, Sharma SP. Neonatal surgery: a ten year audit from a university hospital. Indian J Pediatr. 2008;75(10):1025–30.
Chirdan LB, Ngiloi PJ, Elhalaby EA. Neonatal surgery in Africa. Semin Pediatr Surg. 2012;21(2):151–9.
Barker DJ. Fetal origins of coronary disease. BMJ. 1995;311:171–4. PMC free article.
Blumfield ML, Hure AJ, Macdonald-Wicks L, et al. A systematic review and meta-analysis of micronutrient intakes during pregnancy in developed countries. Nutr Rev. 2013;71:118–32. https://doi.org/10.1111/nure.12003.
Gernand AD, Schulze KJ, Stewart CP, West KP Jr, Christian P. Micronutrient deficiencies in pregnancy worldwide: health effects and prevention. Nat Rev Endocrinol. 2016;12:274–89. https://doi.org/10.1038/nrendo.2016.37.
Dalton MD, Ni Fhloinn DM, Gaydadzhieva GT, et al. Magnesium in pregnancy. Nutr Rev. 2016;74(9):549–57. https://doi.org/10.1093/nutrit/nuw018. Epub 2016 Jul 21.
Mousa A, Nagash A, Lim S. Macronutrient and micronutrient intake during pregnancy: an overview of recent evidence. Nutrients. 2019;11(2):443. https://doi.org/10.3390/nu11020443.
Hadlock FP, et al. Sonographic estimation of fetal age and weight. Radiol Clin North Am. 1990;28(1):39–50.
Shepard MJ, Richards VA, Berkowitz RL, et al. An evaluation of two equations for predicting fetal weight by ultrasound. Am J Obstet Gynecol. 1982;142:47.
Hadlock FP, et al. Estimation of fetal weight with the use of head, body, and femur measurements—a prospective study. Am J Obstet Gynecol. 1985;151(3):333–7.
Shivkumar S, et. al., An ultrasound-based fetal weight reference for twins. Am J Obstet Gynecol 2015;213(2):224.e1-224.e9. https://doi.org/10.1016/j.ajog.2015.04.015
Ott WJ. The diagnosis of altered fetal growth. Obstet Gynecol Clin North Am. 1988;15(2):237–63.
American College of Obstetricians and Gynecologists. Fetal growth restriction. Practice Bulletin No. 134. Obstet Gynecol. 2013;121:1122–33.5.
Society of Obstetricians and Gynaecologists of Canada. Intrauterine growth restriction: screening, diagnosis, and management. SOGC Clinical Practice Guideline No. 295, August 2013. J Obstet Gynaecol Can. 2013;35(8):741–8.
http://sogc.org/wp-content/uploads/2013/08/August2013-CPG295-ENG-Revised.pdf
Unterscheider J, Daly S, Geary MP, Kennelly MM, et al. Optimizing the definition of intrauterine growth restriction: the multicenter prospective PORTO Study. Am J Obstet Gynecol. 2013;208(4):290.e1–6. https://doi.org/10.1016/j.ajog.2013.02.007.
American College of Obstetricians and Gynecologists. Fetal macrosomia number 22, November 2000 (Reaffirmed 2015). http://www.acog.org/Resources_And_Publications/Practice_Bulletins/Committee_on_Practice_Bulletins_Obstetrics/Fetal_Macrosomia
Boulet SL, Alwxander GR, Salihu HM, Pass MA. Macrosomic births in the united states: determinants, outcomes, and proposed grades of risk. Am J Obstet Gynecol. 2003;188(5):1372–8. https://pubmed.ncbi.nlm.nih.gov/12748514
Faschingbauer F, Dammer E, Raabe E, Schneider M, et al. Sonographic weight estimation in fetal macrosomia: influence of the time interval between estimation and delivery. Arch Gynecol Obstet. 2015;292(1):59–67. https://doi.org/10.1007/s00404-014-3604-y.
Kriplani A, Sharma A, Radhika AG, Rizvi ZA, et al. Management of iron deficiency anaemia in pregnancy. FOGSI General Clinical Practice Recommendations. https://www.fogsi.org/wp-content/uploads/2017/07/gcpr-recommend
American College of Obstetricians and Gynecologists. ACOG Practice Bulletin No. 95: anemia in pregnancy. Obstet Gynecol. 2008;112(1):201–7. https://doi.org/10.1097/AOG.0b013e3181809c0d. Erratum in: Obstet Gynecol. 2020 Jan;135(1):222.
Auerbach M, Abernathy J, Juul S, Short V, Derman R. Prevalence of iron deficiency in first trimester, nonanemic pregnant women. J Matern Fetal Neonatal Med. 2021;34(6):1002–5. https://doi.org/10.1080/14767058.2019.1619690. Epub 2019 Jun 3.
Juul SE, Derman RJ, Auerbach M. Perinatal Iron deficiency: implications for mother and infants. Neonatology. 2019;115(3):269–74.
Ren A, Wang J, Ye RW, et al. Low first trimester haemoglobin and low birth weight, preterm birth and small for gestational age newborns. Int J Gynaecol Obstet. 2007;98:124.
Rohilla M, Raveendran A, Dhaliwal LK, Chopra S. Severe anaemia: a tertiary hospital experience from northern India. J Obstet Gynaecol. 2010;30:694.
Hemoglobin concentrations for diagnosis of anaemia and assessment of severity. Vitamin and mineral nutrition information system. Geneva, World Health Organization; 2011.
Robinson HE, O’Connell CM, Joseph KS, McLeod NL. Maternal outcomes in pregnancies complicated by obesity. Obstet Gynecol. 2005;106:1357.
Stewart A, Malhotra A. Gestational diabetes and the neonate: challenges and solutions. Res Reports Neonatol. 2015;5:31–9. https://doi.org/10.2147/RRN.S30971.
International Diabetes Federation. IDF Atlas. 9th ed. Brussels, Belgium: International Diabetes Federation; 2019.
Sobel JD, Kaye D. Urinary tract infections. In: Mandell GL, Bennett JE, Dolin R, editors. Mandell, Douglas, and Bennett’s principles and practice of infectious diseases, 7, vol. 1. Philadelphia: Elsevier; 2010. p. 957.
Nicolle LE, Gupta K, Bradley SF, et al. Clinical practice guideline for the management of asymptomatic bacteriuria: 2019 update by the infectious diseases Society of America. Clin Infect Dis. 2019;68:e83.
Smaill FM, Vazquez JC. Antibiotics for asymptomatic bacteriuria in pregnancy. Cochrane Database Syst Rev. 2019;2019
Documentation and verification of measles, rubella and congenital rubella syndrome elimination in the region of the Americas United States National Report, March 28, 2012. pdf icon.[1.4 MB, 62 pages].
Rubella and congenital rubella syndrome control and elimination—global progress, 2000–2012. Morbid Mortal Wkly Report. 2013;62(48):983–6.
Papania M, Wallace GS, Rota PA, Icenogle JP, et al. Elimination of endemic measles, rubella, and congenital rubella syndrome from the western hemisphere—the US Experience. 2014 external icon. JAMA Pediatr. 2014;168(2):148–55.
Murhekar M, Verma S, Singh K, Bavdekar A, Benakappa N, et al. Epidemiology of congenital rubella syndrome (CRS) in India, 2016-18, based on data from sentinel surveillance. PLoS Negl Trop Dis. 2020;14(2):e0007982. https://doi.org/10.1371/journal.pntd.0007982.
Tran TT, Joseph A, Reau N. ACG clinical guideline: liver disease and pregnancy. Am J Gastroenterol. 2016;111(2):176–94. https://doi.org/10.1038/ajg.2015.430.
Westbrook RH, Dusheiko G, Williamson C. Pregnancy and liver disease. J Hepatol. 2016;64j:933–45.
Mikolasevic I, Filipec-Kanizaj T, Jakopcic I, Majurec I, et al. Liver disease during pregnancy: a challenging clinical issue. Med Sci Monit. 2018;15(24):4080–90. https://doi.org/10.12659/MSM.907723.
Millar LK, DeBuque L, Wing DA. Uterine contraction frequency during treatment of pyelonephritis in pregnancy and subsequent risk of preterm birth. J Perinat Med. 2003;31:41.
Tangren J, Nadel M, Hladunewich MA. Pregnancy and end-stage renal disease. Blood Purif. 2018;45:194–200. https://doi.org/10.1159/000485157.
Gonzalez Suarez ML, Kattah A, Grande JP, Garovic V. Renal disorders in pregnancy: core curriculum. 2019;73(1):119–30. https://doi.org/10.1053/j.ajkd.2018.06.006.
Hui D, Hladunewich MA. Chronic Kidney Disease and Pregnancy. Obstetrics & Gynecology. 2019;133(6):1182–94. https://doi.org/10.1097/AOG.0000000000003256.
Brewer M, Kueck A, Runowicz CD. Chemotherapy in pregnancy. Clin Obstet Gynecol. 2011;54(4):602–18. https://doi.org/10.1097/GRF.0b013e318236e9f9.
Dekrem J, Van Calsteren K, Amant F. Effects of fetal exposure to maternal chemotherapy. Paediatr Drugs. 2013;15(5):329–34. https://doi.org/10.1007/s40272-013-0040-6.
Cardonick EH, Gringlas MB, Hunter K, Greenspan J. Development of children born to mothers with cancer during pregnancy: comparing in utero chemotherapy-exposed children with nonexposed controls. Am J Obstet Gynecol. 2015;212(5):658.e1–8. https://doi.org/10.1016/j.ajog.2014.11.032. Epub 2014 Nov 27.
MacDonald SC, Bateman BT, McElrath TF, et al. Mortality and morbidity during delivery hospitalization among pregnant women with epilepsy in the United States. JAMA Neurol. 2015;72:981.
Kapoor D, Wallace S. Trends in maternal deaths from epilepsy in the United Kingdom: a 30-year retrospective review. Obstet Med. 2014;7:160.
Tomson T, Battino D, Bromley R, et al. Management of epilepsy in pregnancy: a report from the International League Against Epilepsy Task Force on Women and Pregnancy. Epileptic Disord. 2019;21:497.
Meador KJ, Pennell PB, May RC, et al. Fetal loss and malformations in the MONEAD study of pregnant women with epilepsy. Neurology. 2020;94:e1502.
Hernández-Díaz S, Werler MM, Walker AM, Mitchell AA. Folic acid antagonists during pregnancy and the risk of birth defects. N Engl J Med. 2000;343:1608.
Tomson T, Battino D, Bonizzoni E, et al. Dose-dependent risk of malformations with antiepileptic drugs: an analysis of data from the EURAP epilepsy and pregnancy registry. Lancet Neurol. 2011;10:609.
Characteristics and outcomes of pregnant women admitted to hospital with confirmed SARS-CoV-2 infection in UK: national population based cohort study. BMJ. 2020;369:m2107. https://doi.org/10.1136/bmj.m2107.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2023 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Kathuria, K. (2023). Impact of Maternal Health and Disease on Neonatal Outcome. In: Saha, U. (eds) Clinical Anesthesia for the Newborn and the Neonate. Springer, Singapore. https://doi.org/10.1007/978-981-19-5458-0_2
Download citation
DOI: https://doi.org/10.1007/978-981-19-5458-0_2
Publisher Name: Springer, Singapore
Print ISBN: 978-981-19-5457-3
Online ISBN: 978-981-19-5458-0
eBook Packages: MedicineMedicine (R0)