Abstract
One of the main goals of the healthcare system is to maximize the health status of the community. Decision-makers have to select and advise health technologies that elevate the health of society considering the limited budget of the healthcare systems. Therefore, decision-making about resource reallocating for a new intervention would have opportunity cost which means the excluded health effects of the other interventions that could be resulted from the allocation of this resource to them. Precision medicine (PM), one of the latest interventions, would result in improved outcomes and reduced adverse effects of treatments by doing pharmacogenetics tests (PGx tests). However, because of the considerable costs of precision medicine, the accessibility of this kind of intervention has been affected. Economic evaluation is a crucial tool to determine and compare the value of various interventions, especially the expensive ones, and plays a remarkable role in the decision-making process in healthcare systems. The results of these studies are an important tool for proposing the exact impending value of the PM interventions to policymakers. However, due to the precision medicine characteristics, some issues have emerged in conducting economic evaluations of PM interventions which have to be considered in designing and implementing such studies. This chapter aims to discuss the importance of economic evaluation and address the challenges and methodological concerns in the field of PM as well as the available solutions.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
FormalPara What Will You Learn in This Chapter?Precision medicine intervention is a novel health technology that created a new paradigm in the health systems. In comparison with conventional interventions, precision medicine causes improved treatment outcomes and reduced side effects. However, it has remarkably high prices, which impact the economy of the health systems. Therefore, it is necessary for health-system decision-makers to apply evidence answering whether it is worth funding such costly interventions. One of the tools, providing such evidence, is economic evaluation studies. However, regarding the special characteristics of precision medicine, applying economic evaluation studies would be associated with challenges. This chapter generally explains the importance of applying economic evaluations in the field of precision medicine, the associated challenges, and the available solutions.
FormalPara Rationale and ImportanceThe remarkable high price of precision medicine causes limited access to them. Considering the limited budget in health systems, it is necessary to decide about the resource allocation to a new health intervention based on evidence that examines the opportunity costs. Economic evaluation is a crucial tool to determine and compare the value of various interventions, especially the expensive ones, and plays a remarkable role in the decision-making process in healthcare systems. However, because of the features of precision medicine, conducting an economic evaluation of precision medicine intervention is associated with challenges. Therefore, economic evaluation of precision medicine intervention and challenges and solutions would be important issues addressed in this chapter.
10.1 The Importance of Economic Evaluation in the Field of Precision Medicine
In recent decades, personalized medicine intervention (PMI) has been introduced as a new paradigm in the diagnosis and treatment of diseases, having caused significant development in the health system, to tailor protocols and treatments of patients [1].
PMI has become a reality in practice through targeted therapies. Using genetic tests and evaluating biomarkers, patients who could potentially benefit from the medicine would be identified and delivered the treatment. The most important consequence of such a method is to increase the safety and effectiveness of treatment. Thus, the occurrence of prescribing unsafe and ineffective interventions would be minimized and healthcare outcomes are highly likely to improve. Consequently, the resource of the healthcare system would be more efficiently consumed [2].
Although PMIs have considerable benefits, they are often remarkably costly [3]. Because of the growth of their application in health systems [4], one of the main concerns about them is to provide sufficient evidence for their assumed economic impact [5]. In other words, regarding their significant costs, the rationale behind conducting an economic evaluation of PMIs is critically important which has been addressed in the previous literature [2]. Another reason why sufficient evidence is required is to justify insurance companies to allocate a portion of their limited resources to these costly interventions [4].
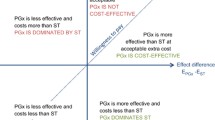
The exact economic value of PMIs would affect the extent of their application and implementation [6]. Economic evaluation (EE) studies answer the main question of whether it is cost-effective to increase the clinical effectiveness of an intervention for its additional cost [3]. Achieving this purpose, in such studies, a ratio is calculated which has been named the “incremental cost-effectiveness ratio” (ICER). This ratio is obtained through the following formula:
According to the above formula, ICER indicates how much it will cost to achieve greater outcomes from later (and possibly more costly) intervention in comparison with the previous one [7]. Conducting these studies for PMIs provides sufficient evidence applicable to making appropriate decisions about using them in healthcare systems [4].
10.2 Challenges of EEs in the Field of Precision Medicine
The results of systematic review studies on EE of PMIs have demonstrated that although these interventions are cost-effective, they are not cost-saving. Evidence suggests that the results of the economic evaluation would be dependent on factors such as the prevalence of a gene (or allele) in the population, the accuracy of genetic tests (false positive and negative), and the costs associated with tests [3, 8]. Also, these studies have shown that the reliability of the EE of PMIs needs to be improved. Evidence has revealed that there are some considerable challenges in conducting EE in the field of precision medicine [6]. Some of the issues related to the EE of PMIs are listed below:
-
1.
Lack of consistent methods for conducting economic evaluations
-
2.
Measuring the real value of personalized medicine
-
3.
Inadequate available data [3]
- 4.
10.2.1 Lack of Consistent Methods for Conducting Economic Evaluations
One of the considerations about EE of PMIs is the lack of reliable methods for conducting these studies regarding the specific characteristics of precision medicine clinical trials. Economic evaluations are mostly designed and carried out based on clinical trials [10]. Therefore, changing the specifications of the clinical studies would affect the required methods for the implementation of the EEs.
Clinical trials of PMIs are complex. Since treatment strategies are a test-and-treat strategy instead of a treat-all therapy, the approach, in which the study population has been examined for biomarkers before randomization of patients, has been adopted in conducting trials to ensure that these patients benefit from the intervention [9].
In the field of precision medicine, clinical trials have been mainly conducted based on biomarkers. In these studies, it is necessary to evaluate many separate subgroups based on the existence or nonexistence of a specific biomarker [11]. These trials have different types, some of which are mentioned below.
10.2.1.1 Enrichment Design
The common type of novel clinical trial is one in which the included patients should have the biomarker and they are randomly assigned to one of the two intervention or control groups. This type of study is useful in cases where biomarker-positive patients benefit from therapeutic intervention and is usually performed in the third phase of clinical trials. The positive point of this type of study lies in its power to find the benefits of treatment because, in these clinical trials, the only response to treatment is assessed. Thus, the required sample size is minimized [11].
10.2.1.2 Randomized All Designs
In these clinical trials, all patients included, regardless of the type of biomarker, are randomly assigned to one of the two intervention or control groups. These trials are especially applicable when the results of previous studies cannot prove the (in)effectiveness of the treatment in biomarker-negative patients. These studies examine whether the existence of biomarkers in the intervention and control groups is related to the treatment effect.
In the two types of clinical trials described above, the types of medicine and disease in the studied population are the same, and the relationship between the type of biomarker and response to treatment is assessed. Patients are evaluated only based on the type of biomarker and response to treatment [12].
10.2.1.3 Basket Clinical Trial
In this study, the effectiveness of medicine would be measured in the study population with a specific biomarker and different types of diseases [12]. The application of these studies is in the area of cancer disease [10]. In most cases, the patient inclusion criterion is the existence of one biomarker that is common to several types of cancer.
An important advantage of these studies is the efficiency of their protocol because the effect of a drug in several different diseases is simultaneously studied. Also in these trials, the protocol is always open to adding a new type of disease (tumor), which in turn keeps the study up-to-date and does not require conducting another study to evaluate new cases. In addition, such studies are more effective in finding tumor efficacy signals in all types of tumors [13].
10.2.1.4 Umbrella Trials
In this method, the number of medicines in a specific type of disease with a variety of biomarkers would be assessed [14, 15]. All participants in the umbrella study have the same type of cancer histology or organ involvement [13]. Such studies are conducted with at least one of the following purposes: (1) finding appropriate and safe doses of drugs and (2) evaluating the effectiveness of a known new compound in comparison with the standard treatment [12].
Conducting clinical studies with a biomarker evaluation approach in the study population can also lead to changes in economic evaluations because these studies are designed and implemented based on clinical trials. Thus, in EE of PMI, genetic characteristics or (non)existence of biomarkers in the hypothetical cohort have to be considered. As previously described, in clinical trials of precision medicine, participants’ selection would be based on the type of biomarker rather than that of disease. In particular, in basket trials, patients have a specific type of biomarker and various diseases. Therefore, in economic evaluations based on these studies, the hypothetical cohort has different diseases and remarkable heterogeneity. Consequently, the researchers have been challenged by how the costs and outcomes would be aggregated in this extremely heterogeneous population. According to researchers in the field of pharmacoeconomics, no economic evaluation study has been conducted on a population with one type of biomarker with different types of diseases and one cost-effectiveness ratio calculated. This necessitates further studies and finding a method specifically designed to calculate the incremental cost-effectiveness ratio in a population with the above characteristics [10].
10.2.2 Measuring the Real Value of Personalized Medicine
One of the most important outcomes measured after the administration of treatment is the quality of life or utility. This outcome is converted to the QALY (quality-adjusted life year) in EEs. QALY incorporates two aspects of the effects of an intervention. One aspect is the effect on the quality of life and the other one is the effect on length of life [7]. However, in EE of PMI, the question is whether improving the health utility following the PMI is the best way to assess the value thereof.
Not all of the benefits of PMI can be assessed through health utility. Although there are different methods for measuring outcomes in economic evaluation studies, QALY is the one most commonly used. Drummond et al. have concluded that health economists have mostly considered QALY as a usual method for assessing the value of interventions. However, QALY cannot assess all the benefits of PMI [15] because it would focus mainly on the consequences of quality of life in terms of health. The World Health Organization defines health as “the perfect social, mental, and physical condition, not just the absence of disease or disability.” Most preference-driven health status measurement tools focus mainly on the health aspects mentioned in the recent definition. Therefore, focusing on QALY in deciding on resource allocation leads to inefficiency and non-optimization of the decision because QALY cannot assess all the beneficial aspects of an intervention. Consequently, it is not possible to solely assess the value of more complex interventions through QALY because their benefits are not limited to health. Regarding the limitations of QALY discussed above, some of the alternative methods considered for assessing the real value of the PMI are explained below.
10.2.2.1 Willingness to Pay
One of the alternative methods suggested for the assessment of the value of PMI is willingness to pay (WTP). In such a method, eligible patients to receive PMI would be asked how much they are willing to pay. WTP would be preferable because, unlike QALY, it takes into account various benefits affecting the respondents’ choice.
On the other hand, the limitations of WTP are the following:
-
1.
Patients’ response depends on their ability to pay.
-
2.
Patients will easily not be able to quantify the value of health and quality of life [16].
-
3.
In the field of precision medicine, patients’ lack of knowledge makes it difficult for them to imagine the consequent condition [17].
10.2.2.2 Benefits Beyond the Health-Related Quality of Life
Applying genetic tests to select the approach of prevention and/or treatment in the field of precision medicine can lead to outcomes beyond the clinical ones. Many researchers and reviewers have believed that measuring the costs and outcomes of precision medicine has many challenges [8].
Reviewing evidence has demonstrated the composite structures used to measure the positive outcomes of health interventions. These composite structures are based on four types of frameworks:
-
1.
Benefits affecting health and well-being (personal health, mental health, potential health, and strength)
-
2.
Benefits arising from the process of providing healthcare (process utility)
-
3.
Benefits beyond the affected people (overflow effects, externalities, selection value, and distributive benefits)
-
4.
Benefits outside the healthcare sector [16]
In an article that specifically focuses on the challenges of conducting EE of PMI, it has been pointed out that process utility and capability theory would be the methods that must be considered for the assessment of the real value of PMI [15]. According to Foster et al., the personal utility method could be applied to identify a group of individuals who are most likely to benefit from the use of the precision medicine approach [17].
10.2.2.2.1 Capability Theory
Capability is the individual’s potential to do a specific or a combination of tasks that a person can do or a situation that can exist. Capability theory, which examines the competence of individuals, is categorized in the first type of framework which is benefits that affect well-being (individual well-being, psychological well-being, overall well-being, empowerment, and power). In this theory, people focus on choice and control, and it measures what people are capable to do beyond performance [16].
10.2.2.2.2 Process Utility
One of the considerations raised in the assessment of the health intervention value is to examine both the outcome and the process of achieving it. It would be important to take into consideration that health service consumer has preferences not only for health outcomes but also for the accompanying conditions of those outcomes. This (dis)utility achieved from the actual process of receiving health service is called process utility. Failure to consider this type of utility in therapeutic interventions that have the same outcomes but have different therapeutic processes can lead to ignoring several benefits and suboptimal outcomes of the interventions. Process utility considers the patient’s experience and satisfaction with the treatment process, which can be related to the quality of the provided service [16].
10.2.2.2.3 Personal Utility
One of the key features of the health service delivery process is the value of awareness and information in a way that is distinct from the value of information for decision-makers. In various studies, the benefits of information generated by healthcare interventions, often in the field of genetic testing, have been specifically examined. Some of the consequences of this awareness include anxiety (or eliminating anxiety) and requiring testing for other family members.
In a study by Grosse, the utility of genetic information can be considered from three perspectives: the public health perspective, the clinical perspective (on the effectiveness of this genetic information in diagnosis and treatment selection), and the individual perspective, which means examining the value of these tests for each person and showing the advantages and disadvantages of performing them outside of the medical field [16, 17]. Examples of personal utility are improved confidence from awareness, people’s sense of control, autonomy, and self-identity [16].
10.2.3 Inadequate Available Data
Generally, required data for economic evaluations will be obtained from clinical studies [7, 8]. For some types of PMI such as pharmacogenomic tests, clinical studies play a remarkable role in the uptake of information about the clinical utility of the tests, changes in health status, and resource utilization and costs. The major challenges related to the data needed for conducting economic evaluations of PMI are their availability and reliability [7].
One of the main barriers to practically applying PMI is the data gap about its effectiveness. In other words, before routinely applying a biomarker-driven approach to choose an appropriate treatment, clinical studies must prove the clinical utility of the test [18]. Clinical utility means “the probability that a test can change and improve patient outcomes.” This case refers to the correlation between genetic tests and the treatment [15]. Designing and implementation of adaptive clinical studies (which are carried out more quickly than conventional trials) is one of the solutions to overcome this limitation. A distinctive feature of these studies is that if the intervention proves to be effective (or ineffective), the study will be stopped as soon as possible. Thus, using adaptive clinical studies can provide the required data about the effectiveness of PMI, but this method is currently being applied only to a limited extent [6].
Another considerable challenge in the issue of data for EE of PMI is the quality of evidence. As mentioned before, economic evaluation is carried out based on the final results of clinical trials. However, in the field of precision medicine, it is necessary to obtain more evidence by conducting prospective observational studies to support the results of these trials because clinical studies of PMI have a limited population (usually subsets of patients from trials with large numbers of participants). Thus, complementary data in practice (real-world data) can increase the validity of the results of the clinical trials. In other words, performing EE of PMI using real-world data can lead to higher quality and reliability of the results of these studies, although the use of this type of data in EEs is very limited [1, 6].
10.2.4 Increasing Complexity of EEs of PMI
Many studies have addressed the challenges of EEs of PMI [6, 8, 15, 19]. Evidence concludes that EEs of PMI are associated with considerable complexity, because such studies evaluate more than one technology (at least two, one intervention, and one test). To better understand and minimize the complexities of EE of PMI, it is necessary to consider the following aspects.
10.2.4.1 Study Question
The first step in conducting an EE is defining the research question. In other words, in the beginning, the characteristics of the intervention arm, comparator arm, study population, time horizon, and perspective of the study should be completely and clearly stated. However, it would not be easily possible in the field of precision medicine regarding the complexity of the EEs of PMI. Sometimes for one intervention, more than one type of test may be needed to be performed. Moreover, it is also considered that applying a genetic test or assessing a biomarker would be performed, with different types of kits available in the market with different prices. Such cases cause complications in explicitly stating a research question in EE of PMI [4, 8, 15]. Therefore, it is recommended that the following items should be identified before conducting cost-effectiveness studies of a PMI:
-
What intervention needs to be evaluated?
-
What is the biomarker(s) of the intervention?
-
What are the types of laboratory methods used to evaluate biomarker(s)?
-
Which laboratory methods are available in the market?
And then, following the answers to these questions, the comparator arm should be determined correctly [15].
10.2.4.2 Sensitivity/Specificity and Predictive Value of the Test
The sensitivity and specificity of the tests, as well as their predictive value, should be considered in the modeling of EE of PMI. Sensitivity and specificity are important issues and should be considered in cost evaluation because test errors lead to false-positive and false-negative results which affect health status and costs. False-positive results cause unnecessary costs and side effects in patients who received the medicine incorrectly and unnecessarily. False-negative results can on the one hand cause loss of health and on the other hand lead to either increased or decreased costs [5, 6].
The concept of the predictive value of tests depends on the prevalence of biomarkers or mutation in a population [5], and in these studies, biomarkers with real prevalence associated with the increased therapeutic response should be examined [8].
10.2.4.3 Cascading Decision in EE of PMI
PMI mainly includes genetic sequencing and assessing of biomarkers, followed by decisions about the choice of treatment based on the results of these tests. The multiplicity of types of tests required in a treatment method, the sequenced or simultaneous performance of the test, and making decisions based on the results lead to complex care pathways in PMI. In other words, in these interventions, we encounter sequential or cascade testing, which affects the EE of PMI modeling, because, in these studies, a cascade modeling must be designed. Considering the risk of obtaining random results (as described in the previous sections) and the possibility of false positives or negatives and the possible costs of performing each test, PMI modeling involves many complexities [3, 15, 19, 20].
In general, complexities in economic evaluations lead to uncertainty in the results. Since health systems make decisions about resource allocation to technologies (a method of treatment or a medicine) based on the results of economic evaluations, they should be aware of the level of uncertainty in the study results. EE of PMI has considerable complexity, and performing sensitivity analysis in such situations shows the degree of uncertainty in the results and can demonstrate how likely the decision about resource allocation to PMI would be cost-effective [15].
References
Terkola R, Antoñanzas F, Postma M. Economic evaluation of personalized medicine: a call for real-world data. New York: Springer; 2017. p. 1065–7.
Fugel H, Nuijten M, Postma M, Redekop K. Economic evaluation in stratified medicine: methodological issues and challenges. Front Pharmacol. 2016;7:113.
Kasztura M, Richard A, Bempong N-E, Loncar D, Flahault A. Cost-effectiveness of precision medicine: a scoping review. Int J Public Health. 2019;64(9):1261–71.
Husereau D, Marshall DA, Levy AR, Peacock S, Hoch JS. Health technology assessment and personalized medicine: are economic evaluation guidelines sufficient to support decision making? Int J Technol Assess Health Care. 2014;30(2):179–87.
Doble B. Budget impact and cost-effectiveness: can we afford precision medicine in oncology? Scand J Clin Lab Invest. 2016;76(sup245):S6–S11.
Shabaruddin FH. Economic evaluations of personalized medicine: existing challenges and current developments. Pharmacogenomics Pers Med. 2015;8:115–26.
Rascati K. Essentials of pharmacoeconomics. Philadelphia, PA: Lippincott Williams & Wilkins; 2013.
Phillips KA, Deverka PA, Marshall DA, Wordsworth S, Regier DA, Christensen KD, et al. Methodological issues in assessing the economic value of next-generation sequencing tests: many challenges and not enough solutions. Value Health. 2018;21(9):1033–42.
Garattini L, Curto A, Freemantle N. Personalized medicine and economic evaluation in oncology: all theory and no practice? Expert Rev Pharmacoecon Outcomes Res. 2015;15(5):733–8.
Nosrati M, Nikfar S. Conducting economic evaluation based on basket clinical trial in the area of precision medicine. Taylor & Francis: New York; 2021. p. 169–71.
Janiaud P, Serghiou S, Ioannidis JP. New clinical trial designs in the era of precision medicine: an overview of definitions, strengths, weaknesses, and current use in oncology. Cancer Treat Rev. 2019;73:20–30.
Food U, Maryland DAJF. Master Protocols: efficient clinical trial design strategies to expedite development of oncology drugs and biologics Guidance for industry-draft guidance; 2018.
Cecchini M, Rubin EH, Blumenthal GM, Ayalew K, Burris HA, Russell-Einhorn M, et al. Challenges with novel clinical trial designs: master protocols. Clin Cancer Res. 2019;25(7):2049–57.
Faulkner E, Annemans L, Garrison L, Helfand M, Holtorf A-P, Hornberger J, et al. Challenges in the development and reimbursement of personalized medicine-payer and manufacturer perspectives and implications for health economics and outcomes research: a report of the ISPOR personalized medicine special interest group. Value Health. 2012;15(8):1162–71.
Annemans L, Redekop K, Payne K. Current methodological issues in the economic assessment of personalized medicine. Value Health. 2013;16(6, suppl):S20–S6.
Engel L. Going beyond health-related quality of life for outcome measurement in economic evaluation: Health Sciences: Faculty of Health Sciences; 2017.
Grosse SD, McBride CM, Evans JP, Khoury MJ. Personal utility and genomic information: look before you leap. Genet Med. 2009;11(8):575–6.
Antoniou M, Jorgensen A, Kolamunnage-Dona R. Biomarker-guided adaptive trial designs in phase II and phase III: a methodological review. PLoS One. 2016;11(2):e0149803.
Marshall DA, Grazziotin LR, Regier DA, Wordsworth S, Buchanan J, Phillips K, et al. Addressing challenges of economic evaluation in precision medicine using dynamic simulation modeling. Value Health. 2020;23(5):566–73.
Rogowski W, Payne K, Schnell-Inderst P, Manca A, Rochau U, Jahn B, et al. Concepts of ‘Personalization’in personalized medicine: implications for economic evaluation. PharmacoEconomics. 2015;33(1):49–59.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Nosrati, M., Nikfar, S., Hasanzad, M. (2022). Economic Aspects in Precision Medicine and Pharmacogenomics. In: Hasanzad, M. (eds) Precision Medicine in Clinical Practice. Springer, Singapore. https://doi.org/10.1007/978-981-19-5082-7_10
Download citation
DOI: https://doi.org/10.1007/978-981-19-5082-7_10
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-19-5081-0
Online ISBN: 978-981-19-5082-7
eBook Packages: MedicineMedicine (R0)