Abstract
As the pandemic has evolved and the knowledge of the coronavirus disease (COVID-19) has expanded, we have seen several ocular manifestations of this deadly virus. Besides the direct involvement of the ocular tissues by the virus, ocular manifestations have been seen due to opportunistic infections and body’s exaggerated autoimmune response.
Conjunctivitis is the most commonly reported ocular manifestation of this virus. This, along with the fact that ACE-2 receptors are present on the ocular surface, strengthens the hypothesis that the eye may act as a portal of entry for the virus. Intraocular features range from uveitis to vision-threatening retinal abnormalities like a central retinal vein or artery occlusion. The most severe form of eye involvement is rhino-orbital-cerebral mucormycosis with high mortality rates despite the treatment. Central nervous system involvement in COVID-19 may present with several neuro-ophthalmic features like optic neuritis, cranial neuropathy, disc edema, eye movement disorder, and pupillary abnormalities. The occurrence of stroke is also higher with severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) than with any other virus leading to visual symptoms due to involvement along the posterior visual pathway. Based on the current evidence, this chapter outlines the important ocular manifestations related to COVID-19 infection.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
13.1 Introduction
Coronavirus disease (COVID-19) caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is an ongoing global pandemic. Earlier believed to be primarily a respiratory disease, COVID-19 has now been recognized as a multisystem disorder. Eye complications are being increasingly reported in the acute as well as recovery phase of the disease. This chapter outlines various ocular manifestations that have been reported in association with COVID-19 during and following the infection. The knowledge and understanding of these ocular manifestations is important to raise awareness about keeping COVID-19 as a differential in such cases, especially during the pandemic. This is crucial for the comprehensive management of the disease and entails adopting preventive measures for the safety of the examining clinician, who may be the first point of contact. The latter is important as Dr. Li Wenliang, an ophthalmologist, one of the first doctors who warned about the outbreak of COVID-19, died after becoming infected with SARS-CoV-2 in Wuhan, China, on February 7, 2020, at the young age of 33 years. He contracted the virus from an asymptomatic glaucoma patient in early January due to the close association with the patient during the ocular examination.
13.2 Pathophysiology
There are several proposed mechanisms for eye manifestations in SARS-CoV-2 infection.
The first hypothesis is the direct viral invasion in the tissue via angiotensin-converting enzyme-2 (ACE-2) receptor that acts as the primary functional receptor for the virus. Viral entry is facilitated by the binding of viral spike (S) protein to ACE-2 receptors. Thereafter, viral uptake and membrane fusion is promoted by priming of S protein by the host cellular transmembrane protease serine 2 (TMPRSS2). ACE-2 expression has been noted in several tissues, including the lungs, nasopharynx, heart, brain, and blood vessels. Several ocular structures express ACE-2 receptors and evidence supports the presence of ACE-2 and TMPRSS2 on ocular surface as well. This explains the tropism of SARS-CoV-2 for the ocular surface, suggesting that the eye may act as a conduit for viral entry in humans.
The second hypothesis is related to endothelial dysfunction and coagulopathy. This theory is supported by the presence of ACE-2 receptors on the endothelial cells that can lead to endothelial abnormalities such as endothelitis and microvascular dysfunction causing vasoconstriction, ischemia, and tissue edema. The heightened immune response causes increased levels of pro-inflammatory cytokines, in turn leading to hypercoagulability. This predisposes affected individuals to thrombotic events.
Thirdly, the exaggerated or dysregulated immune response-induced autoantibody production has been associated with the fresh occurrence of autoimmune disorders like antibody-positive optic neuritis, Miller Fisher syndrome, or myasthenia gravis. Autoantibody production occurs due to molecular mimicry in which viral antigens induce an immune response against self-proteins [1].
Lastly, SARS-CoV-2 pneumonia and respiratory insufficiency can lead to hypoxia-induced brain injury that may cause various neuro-ophthalmic manifestations.
13.3 Ocular and Extraocular Manifestations of COVID-19
COVID-19 may involve any part of the eye- the ocular surface, intraocular, or extraocular or may have neuro-ophthalmic manifestations. Vaccine-related ocular complications are also described. All these features have been summarized in Table 13.1.
-
1.
The ocular surface and cornea
Conjunctivitis is the most common ophthalmic involvement reported with COVID-19 infection. As discussed earlier, the ocular surface may also be the source of entry or dissemination of the virus. Various studies have reported conjunctival involvement in the range of 0.8–32% [2]. Hand-eye contact has been noted as a risk factor predisposing to conjunctival symptoms in COVID-19. Although the virus yield from the conjunctival samples has been poor on reverse transcriptase-polymerase chain reaction (RT-PCR), ocular surface is still considered the likely entry portal for the SARS-CoV-2.
Conjunctival hyperemia, chemosis, epiphora, ocular irritation, foreign body sensation, follicular conjunctivitis, and increased secretions are commonly described features. Most cases of follicular conjunctivitis have been reported in the subacute phase of the disease, i.e., the second week. Conjunctival involvement has occasionally been seen as the presenting symptom of the disease, with patients developing other respiratory signs of SARS-CoV-2 a few days later. Rarely, it may be the sole manifestation of the disease. Conjunctivitis has also been reported in the late or recovery phase of SARS-CoV-2 infection. Early-onset conjunctivitis is attributed to direct viral invasion and involves treatment with topical antibiotics. On the other hand, late-onset conjunctivitis is presumably an immune-mediated response. This has more severe manifestations such as bilateral involvement and corneal involvement and needs treatment with topical steroids and lubricants. Ribavirin has been used in some cases. Hemorrhagic and pseudomembranous forms of conjunctivitis have also been reported where a complete resolution was noted with topical antibiotics, steroids, and daily debridement of the pseudomembrane [3].
Conjunctivitis has also been seen as a manifestation of the multisystem inflammatory syndrome in children (MIS-C) that is reported to occur a few weeks after SARS-CoV-2 infection and bears a resemblance to Kawasaki disease. It is related to delayed immune response occurring following COVID-19 and is associated with elevated inflammatory markers.
Episcleritis is another rare manifestation of COVID-19 infection and is infrequently seen as a presenting symptom. It is usually self-limiting and requires no specific therapy.
-
2.
Intraocular
-
(a)
Uveitis—All forms of uveitis, i.e., anterior, intermediate, and posterior, have been described during the course of the disease.
-
(b)
Posterior segment
-
(i)
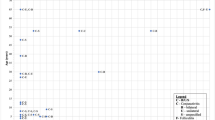
Venous occlusions—Inflammatory reaction and hypercoagulability seen with COVID-19 infection may lead to venous occlusions (Fig. 13.1). There are several reports of unilateral or bilateral central retinal vein occlusion (CRVO) and impending CRVO following COVID-19 infection in young as well as elderly individuals. Usually good visual recovery has been noted with steroids and anticoagulants. Cases with macular involvement need anti-VEGF treatment. Papillophlebitis, a milder form of CRVO, has been noted either as a manifestation of COVID-19 or as a consequence of prone positioning in ICU patients admitted for management of COVID-19. Prone positioning causes direct compression on the eye, increases orbital venous pressure, and consequently increases intraocular pressure. Therefore, fundus examination becomes necessary in prone-positioned ICU patients. Also, protective cushioning of the eyes and maintaining the head position above heart level are some preventive measures that must be implemented [4].
-
(ii)
Arterial occlusion—Central retinal artery occlusion (CRAO) is less commonly reported than CRVO in COVID-19. It is a blinding condition that has been linked with elevated inflammatory markers like interleukin-6, C-Reactive Protein (CRP), ferritin, D-dimer, and fibrinogen. Rarely, combined CRVO and CRAO can also be seen.
-
(iii)
Other retinal abnormalities
-
1.
Acute retinal necrosis (ARN) is a rare manifestation of COVID-19.
-
2.
Acute macular neuroretinopathy (AMN) and paracentral acute middle maculopathy (PAMM).
-
3.
Subclinical abnormalities on optical coherence tomography (OCT) in the retinal layers like bilateral hyperreflectivity in several layers of the retina that are more prominent at the papillomacular bundle, disruption of the ellipsoid zone and interdigitation zone, and loss of inner nuclear layer (INL) volume have been described.
-
4.
Vitritis can be seen but should be diagnosed after ruling out other infectious causes.
-
5.
Nonspecific retinal changes like peripapillary and peripheral retinal hemorrhages, cotton-wool spots, hard exudates, dilated veins, tortuous vessels, and macular pigmentation have been noted.
-
6.
OCT angiography (OCT-A) has shown significant, diffuse perfusion loss in several areas of the post-COVID-19 patients’ retinas compared with healthy eyes.
-
7.
On Fluid Attenuated Inversion Recovery (FLAIR) weighted images, abnormal magnetic resonance imaging (MRI) findings have been seen at the posterior pole in few patients with COVID-19 consisting of one or several hyperintense nodules in the macular region. These lesions are postulated to be either direct inflammatory infiltration of the retina or microangiopathic disease from viral infection.
-
1.
-
(iv)
Choroidal abnormalities—Reactivation of serpiginous choroiditis has been reported following COVID-19 infection. Other differentials like tuberculosis, hepatitis B and C, human immunodeficiency virus (HIV), and syphilis should be ruled out before initiating immunomodulatory therapy.
-
(i)
-
(a)
-
3.
Extraocular
-
(a)
Lid—Eyelid abnormalities in the form of meibomian orifice problems and lid margin hyperemia/telangiectasia may be seen. Blepharitis is seen as a late manifestation of the disease.
-
(b)
Orbital—Orbital manifestations may vary from non-specific retro-orbital pain to life-threatening invasive mucormycosis.
-
(i)
Acute dacryoadenitis as a late complication of SARS-CoV-2 has been reported in a patient otherwise devoid of any COVID-19 symptoms and later detected positive for SARS-CoV-2 antibodies. Retrograde spread of the virus to the lacrimal gland via the ductules or immunologic response to the gland are the possible mechanisms.
-
(ii)
Orbital cellulitis and sinusitis—Orbital cellulitis has been seen in young patients presenting as progressive painful orbital swelling in the absence of any chronic sinus disease. Orbital abscess with globe perforation has also been reported.
-
(iii)
Rhino-orbital-cerebral mucormycosis (Fig. 13.2) is a life-threatening opportunistic infection that is increasingly reported with moderate to severe COVID-19 infection. The risk factors are the presence of associated comorbidities like uncontrolled diabetes, diabetic ketoacidosis and corticosteroid use for the management of COVID-19. Facial or orbital pain, headache, periocular swelling, double vision, and diminution of vision may be the early features of the disease. In suspected cases, clinical assessment of vision, pupillary reactions, and ocular motility should be done. Nasal swab for KOH mount and cultures should be sent to confirm the diagnosis. Neuroimaging is useful in assessing the extent of the disease. Aggressive management with intravenous liposomal amphotericin B with or without surgical debridement, along with strict glycemic control, is required. The reported mortality despite treatment is as high as 50%, and therefore, early diagnosis and management is imperative [3, 5].
-
(i)
-
(a)
-
4.
Neuro-ophthalmic manifestations—Various neuro-ophthalmic manifestations have been documented in association with COVID-19 infection.
-
(a)
Optic neuritis (Fig. 13.3)
There are several reports of unilateral or bilateral optic neuritis during the course or following recovery of COVID-19 infection. Para- and post-infectious demyelinating syndromes are known to occur following viral illnesses. So, the occurrence of optic neuritis in association with COVID-19 may be explained by a similar demyelinating process that is initiated either by the exposure to viral antigens related to viral neurotropism or by autoantibody production. The clinical presentation could be typical, with periventricular demyelinating lesions on MRI in a young female patient suggestive of multiple sclerosis (MS), or maybe atypical with myelitis and myelin oligodendrocyte (MOG) or anti-AQP4 (NMO) antibody positivity. Optic neuritis may occur as a presenting feature of COVID-19. Usually, good visual recovery has been noted with intravenous methylprednisolone (IVMP) and/or plasma exchange (PLEX). However, other infectious and inflammatory causes should be excluded.
Panuveitis and optic neuritis as a presenting feature have also been reported. The simultaneous occurrence of uveitis and optic neuritis is explained by the presence of ACE-2 receptors in both the ocular tissues—choroid as well as central nervous system (CNS) [6].
Acute disseminated encephalomyelitis (ADEM) presenting with bilateral vision loss and sensory deficit is also known [7]. The diagnosis was made based on neuroimaging showing multiple T1 post-gadolinium-enhancing lesions in the brain, lesion in the spinal cord, and bilateral optic nerve enhancement. Significant visual recovery was noted after management with IVMP and IV immunoglobulins.
-
(b)
Idiopathic intracranial hypertension (IIH)
There are reports of fresh-onset headache with raised intracranial pressure (defined as CSF opening pressure > 250 mm of H2O) without encephalitis or meningitis following COVID-19 infection. However, disc edema may not be noted in all cases. Idiopathic intracranial hypertension with disc edema may be a presenting feature in COVID-19 and is also seen during the recovery phase (Fig. 13.4). Recovery of visual complaints and field defects occurs with lowering the CSF pressures with acetazolamide therapy. IIH is possibly caused by venous congestion due to low-grade inflammation and with hypercoagulable state precipitated by COVID-19 infection, leading to hyperviscosity and less CSF absorption.
-
(c)
Cranial neuropathy
Ocular motor palsies have been seen following COVID-19 infection either as an isolated pathology or a manifestation of underlying systemic disease like Miller Fisher syndrome. There are reports of oculomotor (Fig. 13.5), trochlear, abducent, and facial palsy with COVID-19. While some patients had pre-existing vascular comorbidities, others were healthy young adults.
Acute demyelinating inflammatory polyneuropathy leading to third nerve and abducent nerve palsy has also been reported, likely due to the virus-mediated immune response. MRI findings may include enhancement of the optic nerve sheath and posterior Tenon’s capsule, which may be due to viral leptomeningeal invasion or an ischemic process [8].
Guillain-Barre syndrome (GBS) presenting with facial paresis or diplegia, Miller Fisher syndrome with features of anosmia, ageusia, internuclear ophthalmoparesis, fascicular oculomotor palsy, ataxia, areflexia, albumino-cytologic dissociation, GD1b-IgG antibody positivity and polyneuritis cranialis with ageusia, bilateral abducens palsy, areflexia, and albumino-cytologic dissociation are some other manifestations of COVID-19 infection. Good recovery has been demonstrated with treatment in most cases [9].
-
(d)
Posterior reversible encephalopathy syndrome (PRES)
PRES is a neurological disorder characterized by vasogenic edema with a distinctive parieto-occipital involvement evident on neuroimaging. PRES has been reported in elderly patients with severe COVID-19 infection requiring intensive care unit (ICU) care with respiratory support. The patients usually present with seizures and occasionally with neuro-ophthalmic manifestations like visual field defects, cortical blindness, and visual hallucinations. There is also a report of hallucinatory palinopsia, the persistent recurrence of a visual image after the stimulus has been removed [10]. Cytokine storm, endothelial abnormalities, and SARS-CoV-2 pneumonia-related hypoxemia are the possible factors that affect cerebral autoregulation leading to cerebral vasodilatation, neuronal swelling, and vasogenic edema. Usually, good recovery has been noted in most cases.
-
(e)
Ischemic optic neuropathy
Non-arteritic ischemic optic neuropathy (NAION) has been noted in already predisposed individuals, i.e., individuals with vascular comorbidities like diabetes and hypertension. Bilateral NAION has also been reported due to prone positioning in a patient with COVID-19-related acute respiratory distress syndrome (ARDS) [11]. Prone positioning is known to affect ocular perfusion and cause raised intraocular pressure. There are also rare reports of increasing presentation of giant cell arteritis (almost five-fold high) during the pandemic [12]. However, the cause-effect relationship could not be established definitively.
-
(f)
Cortical visual impairment (CVI)
Greater incidence of stroke and younger age of incidence of stroke have been noted with SARS-CoV-2 infection than with other coronaviruses, influenza, or seasonal viruses. Coagulation disorders, endothelial abnormalities, and excessive inflammatory response are the causative factors. Therefore, early anticoagulation therapy is recommended in moderate-severe COVID-19.
Occipital and visual pathway involvement in stroke can lead to neuro-ophthalmic manifestations like vision loss and visual field defects.
-
(g)
Multisystem inflammatory syndrome in children (MIS-C)
MIS-C is characterized by inflammation of multisystem organs like the heart, lungs, kidneys, brain, skin, eyes, or gastrointestinal organs (≥2) and elevated inflammatory markers associated with recent SARS-CoV-2 infection. This is associated with an exaggerated immune response in children. Inflammatory markers like C-reactive protein (CRP), erythrocyte sedimentation rate (ESR), fibrinogen, procalcitonin, D-dimer, ferritin, lactic acid dehydrogenase (LDH), or interleukin-6 (IL-6) are elevated. Raised CSF pressures, related to altered CSF dynamics due to inflammatory or infectious meningitis, have been documented in the setting of MIS-C following COVID-19 infection. Disc edema and abducent nerve palsy due to elevated intracranial pressure have been reported in some of these patients. Usually, the recovery is good with management.
-
(h)
Myasthenia gravis
Exacerbation, as well as new cases of myasthenia gravis, may occur following COVID-19. The common presenting symptoms are diplopia and ptosis. The patients are positive for acetylcholinesterase (AchR) or muscle-specific tyrosine kinase (MuSK) antibodies and respond well to pyridostigmine.
-
(i)
Nystagmus and other eye movement disorders
There are isolated reports of nystagmus and other eye movement disorders like intermittent horizontal nystagmus with a rotatory component [13], opsoclonus (rapid, chaotic, involuntary saccadic, multidirectional eye movements), and bilateral horizontal pendular nystagmus in COVID-19 patients [14].
-
(j)
Pupillary abnormalities
Adie’s pupil due to parasympathetic denervation following viral infections is not uncommon. Adie’s tonic pupil has been documented in association with SARS-CoV-2 infection. Adie-Holmes syndrome with anisocoria and absence of deep tendon reflexes in upper and lower limbs has also been reported [15].
-
(a)
-
5.
Vaccine-related complications
As the vaccination drive is ongoing, several COVID-19 vaccines have been introduced, such as RNA vaccines, DNA vaccines, and replication-defective viral vector vaccines. Subsequently, there have been reports of vaccine-related ocular complications. The mechanism of ocular disease post-vaccination can be an immunologic response to the spike antigen, other viral antigens, or components of adenovirus causing molecular mimicry.
Mild reversible ocular adverse events like episcleritis, anterior scleritis, acute macular neuroretinopathy, paracentral acute middle maculopathy, and subretinal fluid have been reported with inactivated COVID-19 vaccine. Thromboembolic events, including CRVO, have been noted with adenovirus vector-based COVID-19 vaccines. This has been attributed to systemic inflammation, platelet, and endothelial dysfunction. There have been rare cases of a transient decrease in vision and transient visual field defects. Occurrence of autoimmune diseases like bilateral arteritic anterior ischemic optic neuropathy (AAION) and bilateral acute zonal occult outer retinopathy (AZOOR) has been seen following vaccination suggesting cross-reactivity of neutralizing antibodies against SARS-CoV-2 spike proteins and host cell antigens [16].
There are numerous reports of postvaccination optic neuritis worldwide, some of whom were positive for myelin oligodendrocyte glycoprotein (MOG) antibodies [17]. Other noteworthy ocular events are Vogt-Koyanagi-Harada (VKH) disease exacerbation, myasthenia gravis, acute macular neuroretinopathy, central serous retinopathy, thrombosis, uveitis, multiple evanescent white dot syndrome, and cranial nerve palsies.
While multiple reports of side-effects following a vaccine injection have been documented, the mere temporal relationship does not necessarily prove causality. The reported frequency of the side effects is considered rare given the millions of people who have received one or more vaccines. The possible reasons for these effects may be related to potentially susceptible individuals exhibiting a maladaptive immune response. Vaccines have added adjuvants within them to boost the immunogenic efficacy, and these adjuvants potentiate the innate and adaptive immune response, which may lead to autoimmune or inflammatory conditions in a small group of persons.
Left-sided third nerve palsy showing drooping of the lids and limitation of adduction, elevation, and depression in an elderly patient with uncontrolled diabetic status. RT-PCR was negative, and patient did not have any systemic features of COVID-19 infection. But IgG COVID-19 antibody titers were markedly elevated. Neuroimaging was unremarkable
13.4 Preventive Measures in Ophthalmic Practice
An ophthalmologist may be the first point of contact in SARS-CoV-2 infection due to these unusual ocular presentations. This necessitates the adherence to appropriate infection control measures based on the latest national and state health directives. Stratification of ophthalmic patients for clinical visits and utilization of tele-ophthalmology practices as much as possible for routine cases may be done. For outpatient examination, use of breath shields while using slit lamps, disinfection, and cleaning of instruments like tonometers, trial frames, pinhole occluders, and B-scan probes are advocated especially during the pandemic. Special care to cover the eyes, nose, and mouth with masks and face shields, use of gloves, and observing proper hand etiquette before and after patient examination are the key to prevent cross-transmission.
13.5 Conclusion
This chapter elaborates various eye manifestations of COVID-19. Considering the proximity required in the ophthalmic examination, understanding the ophthalmic manifestations of COVID-19 becomes important. Strict adherence to appropriate infection control measures while examining these patients will ensure the safety of the healthcare worker and the patients.
References
Tisdale AK, Dinkin M, Chwalisz BK. Afferent and efferent neuro-ophthalmic complications of coronavirus disease 19. J Neuroophthalmol. 2021;41:154–65.
Dhiman R, Rakheja V, Saxena R. An ophthalmologist’s insight into the viral pandemics. J Optom. 2021;15(1):35–43. https://doi.org/10.1016/j.optom.2020.10.005.
Sen M, Honavar S, Sharma N, Sachdev M. COVID-19 and eye. Indian J Ophthalmol. 2021;69:488–509. https://doi.org/10.4103/ijo.IJO_297_21.
Sun L, Hymowitz M, Pomeranz HD. Eye protection for patients with COVID-19 undergoing prolonged prone-position ventilation. JAMA Ophthalmol. 2021;139:109–12. https://doi.org/10.1001/jamaophthalmol.2020.4988.
Singh AK, Singh R, Joshi SR, Misra A. Mucormycosis in COVID-19: a systematic review of cases reported worldwide and in India. Diabetes Metab Syndr. 2021;15(4):102146. https://doi.org/10.1016/j.dsx.2021.05.019.
Benito-Pascual B, Gegúndez JA, Díaz-Valle D, Arriola-Villalobos P, Carreño E, Culebras E, Rodríguez-Avial I, Benitez-Del-Castillo JM. Panuveitis and optic neuritis as a possible initial presentation of the novel coronavirus disease 2019 (COVID-19). Ocul Immunol Inflamm. 2020;28(6):922–5. https://doi.org/10.1080/09273948.2020.1792512.
Novi G, Rossi T, Pedemonte E, Saitta L, Rolla C, Roccatagliata L, Inglese M, Farinini D. Acute disseminated encephalomyelitis after SARS-CoV-2 infection. Neurol Neuroimmunol Neuroinflamm. 2020;7(5):e797. https://doi.org/10.1212/NXI.0000000000000797.
Dinkin M, Gao V, Kahan J, Bobker S, Simonetto M, Wechsler P, Harpe J, Greer C, Mints G, Salama G, Tsiouris AJ, Leifer D. COVID-19 presenting with ophthalmoparesis from cranial nerve palsy. Neurology. 2020;95(5):221–3. https://doi.org/10.1212/WNL.0000000000009700.
Gutierrez-Ortiz C, Mendez A, Rodrigo-Rey S, et al. Miller Fisher syndrome and polyneuritis cranialis in COVID-19. Neurology. 2020;95(5):e601–1212.
Ghosh R, Lahiri D, Dubey S, Ray BK, Benito-León J. Hallucinatory palinopsia in COVID-19-induced posterior reversible encephalopathy syndrome. J Neuroophthalmol. 2020;40(4):523–6. https://doi.org/10.1097/WNO.0000000000001135.
Clarke KM, Riga V, Shirodkar AL, et al. Proning related bilateral anterior ischaemic optic neuropathy in a patient with COVID-19 related acute respiratory distress syndrome. BMC Ophthalmol. 2021;21:276. https://doi.org/10.1186/s12886-021-02028-9.
Luther R, Skeoch S, Pauling JD, Curd C, Woodgate F, Tansley S. Increased number of cases of giant cell arteritis and higher rates of ophthalmic involvement during the era of COVID-19. Rheumatol Adv Pract. 2020;4(2):rkaa067. https://doi.org/10.1093/rap/rkaa067.
Ishaq H, Durrani T, Umar Z, Khan N, McCombe P, Ul Haq MA. Post-COVID opsoclonus myoclonus syndrome: a case report from Pakistan. Front Neurol. 2021;12:672524.
Pereira Coutinho M, Faustino P, Lourenço J, Leitão L. Acquired pendular nystagmus in the setting of COVID-19. Eur J Neurol. 2021;28(Suppl 1):767.
Kaya Tutar N, Kale N, Tugcu B. Adie-Holmes syndrome associated with COVID-19 ınfection. Indian J Ophthalmol. 2021;69(3):773–4.
Maleki A, Look-Why S, Manhapra A, Foster CS. COVID-19 recombinant mRNA vaccines and serious ocular inflammatory side effects: real or coincidence? J Ophthalmic Vis Res. 2021;16(3):490–501.
Alvarez LM, Neo YN, Davagnanam I, Ashenhurst M, Acheson J, Abdel-Hay A, et al. Post vaccination optic neuritis: observations from the SARS-CoV-2 pandemic. SSRN Electron J. https://doi.org/10.2139/ssrn.3889990.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Saxena, R., Dhiman, R. (2022). Eye Complications Following COVID-19. In: Mohan, A., Mittal, S. (eds) Post COVID-19 Complications and Management. Springer, Singapore. https://doi.org/10.1007/978-981-19-4407-9_13
Download citation
DOI: https://doi.org/10.1007/978-981-19-4407-9_13
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-19-4406-2
Online ISBN: 978-981-19-4407-9
eBook Packages: MedicineMedicine (R0)