Abstract
Realizing the indispensable role of the immune system in maintaining the disease-free state, concept of immunomodulation is gaining increased public perception. Rising incidences of life-threatening infections need improvement in disease resistance ability of individuals by immune stimulation. In healthy state, immunostimulants act as prophylactic on both innate and adaptive immune responses and protect body against infections, allergy, as well as life-threatening diseases like cancer. On the contrary, immunosuppressants are useful in autoimmune inflammatory diseases and transplant recipients for prevention of graft rejection. Wide range of synthetic or recombinant immunomodulators currently in use, like levamisole, tacrolimus, and thalidomide, are associated with numerous side effects. Microbiological or recombinant synthetic cytokines too exhibit severe adverse reactions. Plant-derived nutraceuticals belonging to alkaloids, flavonoids, glycosides, sterols, terpenoids, etc. not only protect the plant but also target oxidative stress in the human body and show beneficial outcome in the management of chronic inflammation, diabetes, cancer, and cardiovascular diseases and in developing immunity. The primary focus of this chapter is to provide a deep insight into scientific data on immunomodulatory properties of plant-derived nutraceuticals, mechanism of action, and challenges and clinical restraints.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Immunomodulators
The primary function of the immune system is to defend the body against infected pathogens and harmful antigens and carry out these functions through its two main branches, viz., nonspecific immunity and antigen-specific immunity. The immediate defense system of the body that protects the body from invading pathogens is known as the nonspecific immunity, while a more complex and antigen-specific or cell-mediated immunity that also results in an immunological memory due to a prior exposure to the antigen is known as antigen-specific immunity (Mohamed et al. 2017). The reaction of the body against any foreign body/pathogen is known as immune response. There are certain molecules that can alter the immune response, positively or negatively, and such molecules are known as immunomodulators (Nair et al. 2019). Depending on this effect, the molecules can be classified as stimulant, suppressor, or adjuvant. Accordingly, in the condition like an autoimmune disorder, wherein the body immune cells do not differentiate between self-cells and foreign cells and start eliminating their own body cells, an immune-suppressor molecule is required. In such a condition, an immune-suppressor molecule will help to restore or normalize the immune system. Even in conditions like organ transplant, immune suppressors are administered so as to avoid transplant rejection. While in conditions like AIDS wherein the immune system of the body is disengaged, an immune stimulator activates/boosts the immune system toward normality. Immuno-adjuvants are essentially used to augment the effect of a vaccine. An overview of immunomodulators and their functions is represented in Fig. 3.1.
All the three categories of the immunomodulators employ one or more of the activities, viz., apoptosis, protein synthesis, antigen presentation, targeting various transcription factors and immune mediators, etc., to exert their actions (Nair et al. 2019). Immunomodulator molecules either inhibit or proliferate the immune-responsive cells, viz., lymphocytes, macrophages, neutrophils, natural killer (NK) cells, and cytotoxic T lymphocytes. The immunomodulators can act by specific or nonspecific action (Bascones-Martinez et al. 2014). Immunomodulators that act on a specific immunity primarily act on the immune system of the cells depending on the attacking antigen or immunogen, with discriminatory specificity for immune response, while nonspecific immunomodulators stimulate or suppress the immune response, without activating any specific immune cell for a specific antigen. Nonspecific immunomodulators are further subdivided into three types (Bascones-Martinez et al. 2014):
-
Type I, which acts on normal immune system
-
Type II, which acts on immunosuppressed immune system
-
Type III, which acts on functionally normal and immunosuppressed immune system
Cancer is one of the diseases wherein immunomodulators have been most commonly used with an aim to prompt the immune system to respond against tumor cells. The chief immune cells involved in body’s defense against tumor cells are NK, dendritic cells, macrophages, polymorph nuclear cells, mast cells, and cytotoxic T cells. Dendritic cells are the main antigen-presenting cells (APC) and form a link between innate and adaptive immune systems. Dendritic cells capture and present the tumor-associated antigen to naïve T cells through major histocompatibility complex, classes I and II. This results in activation, cloning, and proliferation of T lymphocytes into CD4+ helper T cell and CD8+ cytotoxic T cells. Simultaneously, pro-inflammatory cytokines such as IFN-γ and IL-12 are released, thereby improving the tumor uptake by APCs and activation of Th1 response. Th1 response eventually activates the cytotoxic T lymphocytes (Wu et al. 2009a). Various immunomodulators currently used in clinical practice are tabulated in Table 3.1.
It can be observed from Table 3.1 that currently used immunomodulators have generalized effect on the immune system and several adverse effects. Therefore, safer, effective alternative having specific mechanism of immunomodulatory effect is need of the hour.
2 Immunomodulatory Phytochemicals
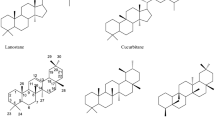
Currently, the pharmaceutical research and new drug development involve finding new molecular targets for specific diseases and focus mainly on single-molecule studies. However, the new drug development process is a time-consuming, slow, and expensive business. Chances of discovering a potent drug with high selectivity and low toxicity are extremely low. Therefore, scientists are looking for new drug candidates from the well-established and proven alternative medicines like plants, algae, and mushrooms, having better patient tolerance and acceptance. Salicin, cocaine, codeine, digitoxin, quinine, vincristine, vinblastine, pilocarpine, paclitaxel, and artemisinin are few representative isolated phytoconstituents being successful today as drugs for the treatment of various diseases. The search for natural products of plant origin as new leads for development of potent and safe immunosuppressant and immunostimulant agents is gaining much major research interest. Wide varieties of plants either whole or parts of plants have shown immunomodulatory mechanism of action, thus having application as successful antioxidant, anti-inflammatory, hepatoprotective, cardiotonic, and several other medicinal benefits. Very popular examples of such plants are Curcuma longa, Withania somnifera, Ocimum sanctum, Aloe vera, Andrographis paniculata, Asparagus racemosus, Boerhavia diffusa, and Echinacea angustifolia (Kumar et al. 2012). Isolated phytoconstituents like glycosides, coumarins, polyphenolics, flavonoids, polysaccharides, and alkaloids have been reported to be responsible for the plant-immunomodulating properties (Kesharwani and Misra 2010; Mishra et al. 2019) (Fig. 3.2).
The literature of the last decade suggests that marine algae metabolites, namely, lectins, laminarans, polyphenols, and sulfated polysaccharides like fucoidans and carrageenans, have shown biological activities and applications for the treatment of immunodeficiency diseases (Besednova et al. 2019). Lectins, carbohydrate-binding proteins without any enzymatic activity, have therapeutic potential. Cyanobacteria such as cyanovirin-N, microvirin, microcrystalline viridis-lectin scytovirin, Oscillatoria agardhii lectin, and griffithsin inhibit the infection of cells with HIV and also prevent the transmission of the pathogen from infected cells to uninfected CD4+ T lymphocytes (Singh and Walia 2018). Eckol, a phlorotannin from marine brown algae, exhibited in vivo antitumor effect in a sarcoma 180 (S180) xenograft-bearing animal model (Zhang et al. 2019a, b). Eckol showed antitumor activity by upregulation of Caspase-3 and Caspase-9 and downregulation of Bcl-2, Bax, EGFR, and p-EGFR. Microalgae biosynthesize a large number of diverse bioactive metabolites, and therefore fractions of microalgae or pure compounds isolated from microalgae have shown anticancer, anti-inflammatory, immunomodulatory properties (Martínez Andrade et al. 2018; Riccio and Lauritano 2019) and beneficial effects in neurodegenerative diseases as well (Bule et al. 2018). Compounds like sulfated polysaccharides, sulfolipids, polyunsaturated fatty acids, and astaxanthins from microalgae are potential immunomodulators. Extracts from Alexandrium tamarense, Chaetoceros calcitrans, Chaetoceros socialis, and Thalassiosira weissflogii have shown activation of IL-6 and human peripheral blood mononuclear cells (Cutignano et al. 2015). Food supplement of condensed water-soluble extract of commercially available spray-dried Spirulina sp. activates human innate immune system augmenting interferon production and NK cytotoxicity (Hirahashi et al. 2002). Sulfated polysaccharides from Tribonema sp. showed immunostimulation and anticancer activities on RAW264.7 macrophage cells and HepG2 cells and significant immunomodulatory activity by stimulating macrophage cells, upregulating IL-6, IL-10, and TNF-α (Chen et al. 2019). Manzo et al. (2017) synthesized a sulfoglycolipid using microalgae-derived sulfolipids as lead compounds and used it as vaccine adjuvant to trigger dendritic cell activation and improve immune response against cancer cell. The synthetic sulfoglycolipid stimulated the production of the pro-inflammatory cytokines IL-12 and INF-γ and increased the expression levels of IL-1α, IL-1β, IL-18, and IL-27.
Increasing body of scientific literature now suggests that, apart from plants, many phytochemicals from edible and nonedible mushrooms too have diverse biological actions (Xu et al. 2012). Mushrooms are considered as a healthy food as they contain high protein, low fat, and essential amino acids like lysine and leucine and essential micronutrient vitamins such as thiamine, riboflavin, niacin, biotin, ascorbic acid, and vitamin D (Cardwell et al. 2018; Liu et al. 2019; Sliva 2004). In addition, mushrooms also contain polysaccharides, polysaccharopeptides, phenolic compounds, and terpenoids. Polysaccharides, particularly β-d-glucans, are responsible for the immunomodulatory activity. In many cultures, mushrooms are used as a food to stimulate the immune system to cure diabetes and cancer. Mallard et al. (2019) studied immune modulation by a medicinal mixture of three different mushrooms, namely, reishi, shiitake, and maitake. The extracts of Ganoderma lucidum (reishi), Lentinula edodes (shiitake), and Grifola frondosa (maitake), alone and in combination, were evaluated for their effect on the expression of cytokines IL-1α, IL-6, IL-10, and TNF-α in human macrophages with and without lipopolysaccharide (LPS) stimulation. All the extracts were found to be highly potent immunostimulators as observed from very low effective concentrations (<100 μg/mL). Combined extract formula exhibited lowest effective concentration for TNF-α expression in LPS-stimulated macrophages compared to the individual extracts, suggesting a potential synergism. Therefore, a combination of these mushrooms is widely used in nutraceutical supplements (Keservani et al. 2016a, b, c, 2020).
Aqueous extracts from the vegetative submerged mycelia of these three mushrooms showed antitumor activity in vivo in rats with implanted kidney cancer (Vetchinkina et al. 2016; Keservani et al. 2016a, b, c, 2018). Polysaccharide fraction of Ganoderma lucidum has been extensively studied for identification of cellular immunostimulatory mechanism. It exerts antitumor effects from human neutrophils by inhibiting spontaneous and Fas-mediated apoptosis through activation of the phosphatidylinositol 3-kinase (PI3K)/Akt pathway, independent of the extracellular signal-regulated kinase pathway. It also stimulates phagocytosis and chemotaxis of neutrophils through the mitogen-activated protein kinase and protein kinase C pathways (Sliva 2004).
Considering the potential of immunoregulatory effect of plants and mushrooms, intellectual property rights are being issued to protect the new and unique key characteristics. The majority of patents and patent applications are of plant extract or extracts of combinations of plants. Being mixtures of discrete components, extracts usually display synergistic effects and multiple therapeutic actions than their isolated constituents. However, issues pertaining to quality, safety, and efficacy, viz., authentication, variability due to geographic location, seasonal changes, soil, weather, and microbial and other creature attacks, must be addressed. Advanced chromatographic fingerprinting by HPLC, HPTLC hyphenated with spectrometric detections like NMR, and MS in view of phytochemical profiling is of utmost importance to account for batch-to-batch variations. Lack of toxicity data is also of significant concern; assessing microbial content or mycotoxins would be of great help. Thus, rigorous quality control and extensive physicochemical and biological profiling can cater the need of developing potential herbal compositions into effective therapeutic agents (Gibbons 2003). Among Ayurvedic medicines, ashwagandha (Indian medicinal herb) holds the first US patent (US 2010/0285064 A1) for acting as a vaccine adjuvant. Its capability of invoking T-cell-dependent immune responses against weaker antigens such as bacterial polysaccharide has been studied. Process of preparing withanolide-rich fraction (withanolide A, withaferin A, withanolide B, withanoside IV, withanoside V, and 12-deoxy-withastramonolide of ashwagandha roots in high yields) has been patented by Jadhav et al. (2010). Adjuvant effect was studied on meningococcal A polysaccharide vaccine, and IgG estimation was carried out. Vaccine containing the adjuvant ashwagandha turned out to be more immunogenic and induced significant IgG response either if used immediately after combining with vaccine or when kept overnight with vaccine. However, higher adjuvant activity was seen when kept overnight. Additionally, significant coadjuvant effect was observed with alum, thereby suggesting its chance inclusion in adjuvant-containing formulations (Keservani et al. 2016a). Summary of few patents from the past two decades on phytoextracts as immunomodulator is presented in Table 3.2.
3 Isolated Phytochemicals as Immunoregulators
The possibility to enhance endogenous immune functions with the use of herbal bioactive constituents/herbal nutraceuticals is extensively investigated (Trung and An 2018). Several herbal nutraceuticals have been reported to modulate in immune functions; however, their potentials as immune boosters are not systematically investigated in well-controlled human clinical studies. Widely investigated isolated phytoconstituents having potent effects on innate and adaptive immunity in preclinical research, namely, resveratrol, epigallocatechol-3-gallate (EGCG), quercetin, curcumin, gingerol, and genistein, are discussed here.
3.1 Resveratrol
Resveratrol is trans-3,4′,5-trihydroxystilbene, a non-flavonoid polyphenolic phytoalexin derived from the skin of grapes and other fruits that demonstrate a broad range of biological activities. Resveratrol is effective anticancer, antioxidant, and anti-inflammatory (Pund et al. 2014; Yuan et al. 2012) having significant potential for the prevention or treatment of cardiovascular diseases, autoimmune disorders, age-related neurodegenerative diseases like Alzheimer’s and Parkinson’s disease, and other chronic disorders (Oliveira et al. 2017; Pund et al. 2020).
Resveratrol mediates its several biological effects through modulation of multiple signal inflammatory pathways which are generally dysregulated (Rieder et al. 2012). By suppressing inflammation, resveratrol alleviates inflammatory symptoms in cancer and several other autoimmune diseases such as colitis and rheumatoid arthritis (Pund et al. 2014; Gambini et al. 2015). A key mechanism of action of resveratrol is through inhibition of production of inflammatory factors through the activation of Sirt1 (Saqib et al. 2018). Sirt1(mammalian) is an important deacetylase member of the sirtuin family involved in a broad range of molecular events and physiological functions like control of gene expression, metabolism, cancer, embryonic development, and aging (Rahman and Islam 2011). Sirt1 maintains periphery T-cell tolerance and plays a major role in counteracting cellular stress and apoptosis (Cattelan et al. 2015). Sirt1 regulates two main pro-inflammatory pathways in the immune response, NF-κB and AP-1 pathways, and thus regulates the immune system (Manna et al. 2000). Sirt1 has a direct regulatory role in macrophages, the most abundant component of the innate immune system, and a main source of pro-inflammatory cytokines TNF-α, IL-6, and IL-1 secreted in response to infection and inflammation. The inhibitory effect of Sirt1 on the NF-κB pathway has an essential role in suppressing the pro-inflammatory phenotype of macrophages (Kong et al. 2012). Structural studies indicate that resveratrol binds to Sirt1, modulates the Sirt1 structure, and enhances binding activity to its substrates. RelA/p65 is an NF-κB member and principal substrate of Sirt1 that regulates leukocyte activation and inflammatory cytokine signaling (Malaguarnera 2019). Resveratrol activates Sirt1 and mediates RelA/p65 deacetylation, thus inhibiting TNF-α-induced NF-κB transcription and sensitizing cells to apoptosis (Signorelli and Ghidoni 2005). The antitumor effect of resveratrol was indirectly inhibiting its potential effect on nonspecific host immunomodulatory activity and direct inhibition of growth of implanted H22 cells tumor in Balb/c mice (Liu et al. 2003). Resveratrol by intraperitoneal route could insignificantly increase the host nonspecific immunological defense of mice with H22 tumor, by raising the level of serum IgG and TNF-α and the number of plaques forming cells.
Similar mechanisms were also observed in collagen-induced arthritis model in mice. Resveratrol inhibited T-cell activation by enhancing the expression and deacetylase activity of Sirt1, thereby decreasing the acetylation of c-Jun and blocking the translocation of c-Jun into the nucleus (Zou et al. 2013). Prophylactic or therapeutic administration of resveratrol attenuated clinical parameters and bone erosion in collagen-induced arthritis model in DBA1 mice model (Xuzhu et al. 2012). Researchers specifically assessed the immune mechanisms by which resveratrol prevented and suppressed ongoing arthritis and determined its role in the regulation of humoral immunity by measuring collagen-specific and total IgG levels in serum. Resveratrol significantly prevented the development of serum collagen-specific IgG2a and IgG1 without any influence on the levels of total IgG1 or IgG2a, suggesting that resveratrol selectively controls the collagen-specific B-cell response and is not a general B-cell-depleting/B-cell-suppressing factor (Xuzhu et al. 2012). Resveratrol prevented hyperplasia of synovial cells by disrupting mitochondrial membrane potentials, by decreasing B-cell lymphoma-extra-large expression, and by allowing cytochrome c from the mitochondria into the cytosol (Nakayama et al. 2012).Resveratrol was found to be very effective in suppressing the potent immune responses induced by inhalation of superantigen, staphylococcal enterotoxin B in C57BL/6 mice acute lung inflammation model. Upregulation of Sirt1, downregulation of NF-κB, and reduction in cytokine production were factors responsible for neutralization of toxicity of superantigen (Rieder et al. 2012). In case of inflammation in the colon induced with 2,4,6-trinitrobenzenesulfonic acid solution (TNBS) in BALB/C mice, resveratrol induced a shift from a pro-inflammatory to anti-inflammatory T-helper response in mesenteric lymph node. Resveratrol regulated several microRNAs that modulated inflammatory genes and factors. Decrease in the expression of several miRs (miR-31, Let7a, miR-132) that targets cytokines and transcription factors involved in anti-inflammatory T-cell responses (Foxp3 and TGF-β) was observed in resveratrol-treated animals (Alrafas et al. 2020). Earlier, Zhang et al. (2019a) confirmed the effectiveness of resveratrol treatment in dextran sulfate solution-induced colitis through upregulation of colonic tissue levels of Sirt1, along with downregulation of pro-inflammatory factors like autophagy-related 12, Beclin-1, and microtubule-associated protein light chain 3 II. Natural killer cells serve as an antitumor defense through their direct cytotoxic and indirect immunoregulatory capacities. Inactivation of natural killer cells causes immune escape of tumor cells leading to rapid progression of cancer and the poor efficacy of immunotherapy. Natural killer group 2 member D (NKG2D) is one of the most prominent activating receptors of natural killer cells, and resveratrol upregulates NKG2D ligands. Resveratrol promotes NKG2D recognition to induce the death of target cells by natural killer cells (Luis Espinoza et al. 2013). Resveratrol also increases the expression of major histocompatibility complex class I chain-related proteins A and B in cancer cell lines and xenograft models and thus increases cytolysis of breast cancer cells by natural killer cells (Pan et al. 2017).
Cardioprotective effect of resveratrol is also through the activation of Sirt1. It inhibits hypoxia-induced apoptosis via the Sirt1-FoxO1 pathway in H9c2 cells proving its potential in preventing cardiovascular disease, especially in coronary artery disease patients (Chen et al. 2009). Resveratrol reduces cardiomyocyte apoptosis by Sirt1 activity and NAD (+) level by an AMPK-dependent mechanism and attenuates caspase-3 cleavage via heat-shock factor 1 deacetylation and heat-shock protein expression upregulation (Cattelan et al. 2015). Peroxide-induced apoptosis in cardiomyocytes is arrested by resveratrol by activation of Sirt1, Sirt3, Sirt4, and Sirt7 (Yu et al. 2009). Activation of Sirt1 by resveratrol attenuates TNF-α-induced vascular adventitial fibroblast apoptosis, cleaves caspase-3 protein expression, and increases the Bcl-2/Bax ratio. The inhibitory effect of Sirt1 on vascular adventitial fibroblast apoptosis is partly mediated by the deacetylation of FoxO1 (Wang et al. 2013).
Resveratrol has shown to be effective for the treatment of organ-specific autoimmune diseases wherein a single organ is involved like type 1 diabetes mellitus, inflammatory bowel diseases (Al Azzaz et al. 2019; Nunes et al. 2018; Shi et al. 2017), and psoriasis (Lai et al. 2017; Oliveira et al. 2017). Beta cells in the islets of Langerhans are destroyed by the inflammatory environment resulting into insulin deficiency and hyperglycemia. Differentiation of T-helper 1-activating B lymphocytes produces autoantibodies against beta cells. Th1 will also activate macrophage and neutrophil migrations to the islet that will promote beta cell destruction by increasing ROS (Wallberg and Cooke 2013). Resveratrol inhibits Th1 cell migration by binding to chemokine receptor 6 and forming a complex with insulin for increased glucose intake (Lee et al. 2011). Leukocyte infiltrates in psoriatic lesions consist of dendritic cells, macrophages, neutrophils, and T cells. Dendritic cells synthesize various pro-inflammatory cytokines, like TNF-α, IL-1β, IL-6, and IL-23, that further promote IL-23 production in dendritic cells and IL-17 secretion from Th17 cells which are inhibited by resveratrol (Kjær et al. 2015; Lai et al. 2017). On similar lines, the adaptive immune system is generally considered as the primary contributor to IBD pathogenesis through increased pro-inflammatory cytokines driven by the T-helper cells or ineffective anti-inflammatory activity of regulatory T cells (Wallace et al. 2014). The innate immune response is mainly triggered by activation of the (NF-κB) pathway and macrophages, stimulating the secretion of pro-inflammatory cytokines such as IFN-γ, IL-1β, IL-6, IL-8, and TNF-α (Dou et al. 2014). Resveratrol has promising effects in bowel inflammation by modulation of inflammatory signaling pathways, inflammatory biomarkers, and intestinal microflora, thus improving clinical outcomes (Altamemi et al. 2014; Rahal et al. 2012; Shi et al. 2017; Yao et al. 2015; Yulug et al. 2015).
3.2 Epigallocatechin Gallate
The most popular global beverage, tea, is made from the dried leaves of the plant Camellia sinensis. Green tea encompasses 20% of the global tea consumption. It is usually prepared by steaming or panfrying the leaves; subsequently, these leaves are dried to inactivate enzymes to preserve the tea constituents from the oxidation. This process helps to preserve the distinctive polyphenols of the green tea, viz., catechins. Almost 250–375-mg catechins are present in a typical cup of brewed green tea. Majorly, these catechins include epicatechin (EC), epicatechin-3-gallate (ECG), epigallocatechin (EGC), and epigallocatechin-3-gallate (EGCG). EGCG is the most abundant and most biologically active catechin found in green tea. Peak plasma levels of EGCG reach a maximum concentration of 1 μM after 1.5–2 h of green tea consumption and have an elimination half-life of 5 h in humans. High doses of EGCG (525 mg) supplements on oral administration resulted in a peak plasma concentration of 4.4 μM, while 1600 mg of EGCG resulted in a peak concentration of 7.4 and 9 μM on administration of 2000-mg EGCG. EGCG is well distributed throughout the body, viz., the digestive tract, blood, brain, liver, kidney, and spleen, among others, and ~80% of EGCG occurs in free form in plasma. Interestingly, other catechins are found in highly conjugated forms like conjugation with glucuronic acid and/or sulfate groups. Tea catechins undergo intestinal and hepatic metabolism and undergo glucuronidation, salvation, methylation, and ring fission by the intestinal microflora. Excretion of EGCG occurs through the bile into the feces, while EGC and EC are eliminated through both bile and urine (Pae and Wu 2013). Japanese Zen monk Eisai published a book in 1211, entitled Kissa Youjouki (meaning “promotion of health by tea”) and described the benefits of tea as “tea is a marvelous preventive medicine to maintain people’s health and has an extraordinary power to prolong life.” Undeniably, recent scientific evidence supports the benefits of green tea for health promotion (Hayakawa et al. 2016). Anti-inflammatory properties along with the ability to modulate immunity enables catechins to exert protective effects against various diseases such as cancer, obesity, diabetes, arteriosclerosis, neurodegenerative diseases, tooth decay, hepatitis, allergy, and bacterial and viral infections. EGCG has been found to alter immune function of the body predominantly T-cell-related activities such as T-cell activation, proliferation, and differentiation into different subsets of effector cells, both innate and adaptive (Pae and Wu 2013). In an in vitro test, EGCG supplementation reduced the neutrophil migration induced by chemokine IL-8 in a dose-dependent manner with an IC50 of >1 mM (Dona et al. 2003) and that of cytokine-induced neutrophil chemoattractant-1 at a dose of 15 mg ml−1 or higher (Takano et al. 2004). Also, suppression of neutrophil recruitment independent of chemokine level at the inflammation site in an ovalbumin-induced rat allergic inflammation model was observed on oral administration of EGCG (1 mg/rat). Oral gavage of 2% green tea was found to inhibit proteolytic enzymes such as neutrophil elastase both in vitro (Sartor et al. 2002) and in vivo (Chan et al. 2012) indicative of an anti-proteolytic activity of EGCG on neutrophils. All these effects of EGCG on the neutrophils suggest its protective effect in preventing inflammation and inflammation-induced tissue damage (Pae and Wu 2013). EGCG also prevents chemokine monocyte chemotactic protein-1 (MCP-1)-induced monocyte migration and its adhesion to fibronectin in the human monocyte cell line, THP-1, by obstructing β1 integrin activation. Monocyte chemotaxis is facilitated by two key mediators, viz., MCP-1 secretion and its receptor (CCR2) expression. FCG has been found to reduce the MCP-1 secretion (Melgarejo et al. 2009). ECGC has been found to modulate a number of inflammatory cytokines and cells involved in their production. EGCG has been reported to inhibit TNF-α, IL-1β, and IL-6 production in various cell lines in vitro, viz., human monocyte cell lines (U937,31 THP-1) (Singh et al. 2005; Choi et al. 2009; Wu et al. 2009a, b), murine macrophage cell lines (J774.1 (Ichikawa et al. 2004), RAW 264.7 (Yang et al. 1998), and primary mouse macrophages (Choi et al. 2009)). Further, EGCG has also been shown to inhibit pro-inflammatory gene expression in LPS-stimulated bone marrow-derived macrophages including IL-6, IL-12p40, MCP-1, ICAM-1, and VCAM-1 (Joo et al. 2012). Suppression of NF-κB by EGCG has been reported to be the underlying cause for all these effects (Joo et al. 2012). Another important immune cells that are involved in the presentation of antigens are dendritic cells. Dendritic cells are the cells bridging the innate and adaptive immunity. EGCG retards dendritic cell maturation which ultimately leads to impaired functionality as antigen-presenting cells (APC) to induce antigen-specific T-cell-mediated response (Ahn et al. 2004). Also, EGCG increases IL-10 production in mature dendritic cells. IL-10 is an inhibitor of dendritic cell differentiation and function. These effects of EGCG on dendritic cells suggest the protective effect of EGCG in autoimmune diseases. Mast cells are another cell involved in the innate immunity which is activated on exposure to allergen like bacteria, etc. These cells further produce cytokines to aid the adaptive immunity. It has been reported that EGCG inhibits the degranulation that results in the release of histamine upon stimulation by an IgE-antigen complex (Matsuo et al. 1997). Dietary supplementation of EGCG has been found to suppress the T-cell proliferation. The ability of T cells to proliferate reflects the immunocompetence of an individual. It has been shown that Con A-induced splenocyte T-cell proliferation is inhibited by EGCG at a dose of 25 mg ml−1 (55 mM) and higher via T-cell mitogen concanavalin A (Wilasrusmee et al. 2002). EGCG has been reported to greatly diminish T-cell proliferation by affecting both T cells and APC (Pae and Wu 2013). Survival, expansion, and differentiation of T cells are regulated via IL-15, IL-7, and IL-2. EGCG induces the downstream signaling of these receptors and thereby inhibits their expression. This eventually results in suppression of T-cell proliferation and its effector function (Shim et al. 2008). Further, EGCG has been reported to inhibit Th1, Th9, and Th17 differentiation while promoting the Treg development. This affects the differentiation of CD4+ T cells, thus further strengthening the fact that EGCG can be effectively used in autoimmune diseases (Pae and Wu 2013). Drinking green tea phenols protects against UV-induced immunosuppression by suppressing local and systemic contact hypersensitivity. Further, UV-induced DNA damage repairing was hastened by green tea phenols along with high levels of nucleotide excision repair genes in mice (Khan et al. 2013).
All these studies clearly suggest that ECGC modulates the immune function, both innate and adaptive immunity and inflammatory responses by altering various immune cell functions. Essentially, ECGC is an anti-inflammatory and T-cell proliferation inhibitor agent, thereby modulating immune functionality. Although most of the studies have been carried out in murine models, these findings need to be validated in human volunteers.
3.3 Gingerol
Ginger (Zingiber officinale Rosc.) belonging to the family Zingiberaceae is a native of Southeast Asia. It is widely used in Indian food as a spice and condiment. Apart from being used in food, the rhizome of ginger has therapeutic utility which is attributed to its rich phytochemistry. Ginger contains more than 60 compounds in that can be categorized into two categories, i.e., volatile and nonvolatile constituents. Volatile constituent includes sesquiterpene and monoterpenoid hydrocarbons that give distinct aroma and taste to ginger, while nonvolatile pungent constituents are gingerols, shogaols, paradols, and zingerone. Zingerones are converted to gingerols or shogaols by thermal degradation (Butt and Sultan 2011). Gingerols are of major importance and are homologous series of phenols that differ in their unbranched alkyl chain length. On drying ginger, gingerols are converted to shogaols. Of the different kinds of gingerols, 6- and 8-gingerol are of prime importance. Majority of the medicinal properties of ginger have been ascribed to 6-gingerol. 6-gingerol has antioxidant properties and suppresses the production of pro-inflammatory cytokines, namely, TNF-α, IL-1, and IL-12 from macrophages (Williams et al. 2007). Treatment with 6-gingerol in tumor-bearing mice has shown a massive increase in the infiltration of tumor-reactive lymphocytes (Ju et al. 2012). In various tumor cell lines, viz., OSCC and cervical HeLa, 6-gingerol has shown antiproliferative effect by induction (Kapoor et al. 2016). Further, 6-gingerol has also exhibited inhibitory effect on COX-2 expression by downregulation of p38 MAPK and NF-кB in vivo. Additionally, an antimetastasis effect on lung B16F10 melanoma in an animal model was shown by 6-gingerol (Kim et al. 2005). 8-gingerol has been found to be capable of simultaneously inhibiting the humoral as well as cellular immune responses in mice through B- and T-cell activation suppression (Lu et al. 2011). However, detailed studies are needed to reinforce the utility of gingerols as immunosuppressive agents.
3.4 Quercetin
Quercetin (3,3′,4′,5,7-pentahydroxyflavone) is a polyphenolic secondary plant metabolite commonly found in fruits and vegetables. It is the most abundant flavonoid and largely a part of diet. Onions, broccoli, apples, berry crops, and grapes, few herbs, tea, and wine are the major dietary sources (Mlcek et al. 2016). It is known to prevent cancer and cardiovascular and neurodegenerative disorders (Ay et al. 2016). Apart from being immunomodulator, it displays wide array of activities, viz., antioxidant, antidiabetic, anticancer, anti-inflammatory, antiplatelet, antiapoptotic, nephoprotective, gastroprotective, angioprotective, cardioprotective, and chondroprotective properties (Kawabata et al. 2015; Shebeko et al. 2018).
Major cellular signaling pathways regulated by quercetin to exert various therapeutic roles are apoptosis, cell cycle arrest, NF-κB pathway, MAPK pathway, PI3K-AKT pathway, and mTOR (Sharma et al. 2018). It lowers Th1-lymphocyte differentiation, thereby reducing levels of cytokines and factors like IL-1β, IL-4, IL-6, IL-10, IL-12, IL-25, IL-33, MCP-1, NF-κB, VEGF-A, COX-2, 5-LOX, iNOS, NO, CRP, TNF-α, TNFγ, and IgE along with lowering expression of VCAM-1, ICAM-1, and MIP-2 (Burmańczuk et al. 2018).
Transcription factors of nuclear factor-kappa B family are mainly involved in the regulation of adaptive immune response, inflammation, lymphopoiesis, and osteogenesis. Quercetin helped improve conspicuously TNF-α, TRAF-2, TNFRSF1B, NF-κBp65, and IFN-γ while lowering expression when fed to healthy Arbor Acre broilers as a part of diet (Yang et al. 2020). During high-throughput screening of immunoregulatory activity of natural products in human umbilical cord blood mononuclear cells, quercetin displayed immunostimulatory effect. It reduced the CD3 expression of T cells and induced CD34 expression of stem cells (Chen et al. 2006).
Cellular immunity is promoted by cytokines IL-2, IFN gamma, and IL-12 derived by Th1, while humoral immunity is promoted by IL-4, IL-5, and IL-6 derived by Th-2. Quercetin interacts with both these pathways to exhibit antiviral and antitumor activities. Quercetin upregulates IFN gamma and downregulates IL-4 and acts as immunostimulant (Nair et al. 2002). Recently, quercetin was seen to significantly increase type I interferon-regulated genes and type I and II interferon and significantly decrease pro- and anti-inflammatory cytokine expressions in macrophages derived out of highly pathogenic porcine reproductive and respiratory syndrome virus infection (Ruansit and Charerntantanakul 2020).
Apart from being immunostimulant, it possesses strong adjuvant potential as evident by increased ovalbumin-specific serum IgG1 antibody titers indicative of boosted humoral immune response in ovalbumin immunized Balb/c mice. It enhanced infiltration of CD11c+ dendritic cells in the mouse peritoneum, and elevated levels of LPS activated IL-1b and nitric oxide by peritoneal macrophages. It also increased expression of Tbx21, GATA-3, and Oct-2 proteins in splenocytes. Unlike other plant-derived molecules, it does not show hemolysis in human RBCs dictating safety for in vivo administration (Singh et al. 2017). Quercetin exhibits leishmanicidal activity, and being potent, it is the most attractive lead among flavonoids. It induces reactive oxygen species generation in L. amazonensis-infected macrophages (Naman et al. 2018), upregulates inhibition of TNF-α in phagocyte migration, and suppresses L. major-induced apoptosis delay in vivo. It exerts weak control on NF-κB level and induces cell death by apoptosis and necrosis (Belkhelfa-Slimani and Djerdjouri 2017). Besides upregulation of Nrf2/HO-1 expression, it depleted labile iron store-infected macrophages hampering L. braziliensis replication (Cataneo et al. 2019).
Quercetin, however, had no effect on antibody production and did not alter white blood cell counts in the lambs as a consequence of road transport but protected the ruminal mucosa against the development of parakeratosis (Benavides et al. 2013). Quercetin along with melatonin is more effective in protecting lungs against hypoxic damage via downregulation of immuno-inflammatory mediators (TNF-a, IL-6, and CRP) and heat-shock protein expression vascular endothelial growth factor (VEGF, HSP70) (Al-Rasheed et al. 2017). Suppression of c-met and VEGF by liposomal quercetin in the Eca109/9706 cells has been confirmed by using immunohistochemistry assay and Western blotting (Pei et al. 2009). Quercetin is known to stabilize hypoxia-inducible factor (HIF)-1α under normal oxygen pressure because of its ability to bind iron intracellularly leading to decreased iron stores in the cells and also downregulate HIF-1 transcriptional activity by impairing the phosphorylation and nuclear accumulation (Triantafyllou et al. 2008).
Quercetin reduced expression of all inflammation-related cytokines and transcription factors (IL-1b, IL-6, IL-8, IL-10 and TNF-a, NF-κB) of LPS-stimulated THP-1 macrophages, other than COX-2 (Chanput et al. 2010). Concentration of milk leukocytes, also known as somatic cell count (SCC), is a key indicator of mastitis in dairy animals (Rainard et al. 2018). In cows with clinical mastitis, quercetin was found to significantly reduce somatic cell count after treatment for a week. However, due to intramammary administration of quercetin, no general effect on the immune system was seen; particularly no effect was seen on TNF-α (Burmańczuk et al. 2018). Recently, the role of quercetin in treating allergic inflammation was demonstrated as it inhibited ovalbumin-induced allergic conjunctivitis in 16 C57BL/6 mice. Quercetin was found to inhibit DNP-HSA/IgE induced Ca2+ 3 influx, MC degranulation, 4 and chemokine release in LAD2 cells. Also, DNP-HSA/IgE induced Lyn/PLCγ/IP3R-Ca2+ 5 and Lyn/ERK1/2; Lyn/NF-κB activation was inhibited (Ding et al. 2020). Anti-allergic action of quercetin is attributed to inhibition of enzymes, inflammatory mediators, and human mast cell activation via inhibition of Ca2+ influx, histamine, leukotrienes, and prostaglandin release (Mlcek et al. 2016). Quercetin was found effective in allergic rhinitis, elevating the production of an endogenous antioxidant protein and immunomodulator “thioredoxin” and suppressing oxidative stress responses in nasal mucosa (Edo et al. 2018).
Potential beneficial allo-herbal combination effect was observed when quercetin was tested in combination with sitagliptin for streptozotocin-induced diabetes mellitus in rats. The duo-regulated serum C-peptide, malondialdehyde, significantly raised superoxide dismutase and glutathione and decreased nuclear factor kappa B more than standalone treatment (Eitah et al. 2019). Quercetin-3-O-β-d-glucuronide is a major metabolite of quercetin in the human body that might be responsible for beneficial effects of quercetin (Kawabata et al. 2015). Isoquercetin (quercetin-3-glucoside) which is a glycoside derivative of quercetin was found to reduce ultraviolet-A radiation-induced damage in living skin equivalent cultures via reduction in 8-hydroxy-2′-deoxyguanosine, TdT-mediated dUTP nick-end labeling, and IL-1 α that too are more effective than hesperetin (Dekker et al. 2005). Another glycosylated quercetin, i.e., quercetin 3-O-xyloside, was found more effective than quercetin in activating redox-dependent ASK1/MAPK/NF-κB signaling pathway in murine macrophage cell line RAW 264.7 resulting in secretion of TNF-α and IL-6 early innate immunity hinting its immunostimulator potential (Lee et al. 2016). A new quercetin glycoside (3′-methoxy-3-O-(4″-acetylrhamnoside)-7-O-α-rhamnoside) isolated from Cleome droserifolia showed significant antitumor activity in triple-negative breast cancer. It showed a dose-dependent decrease in MDA-MB-231 proliferation and viability through stimulation of TP53, repression of its downstream miR155, and sevenfold and twofold upregulation of MHC class I polypeptide sequence A and UL-16 binding protein 2, respectively (Abdel-Latif et al. 2019).
3.5 Curcumin
A potent antioxidant and anti-inflammatory polyphenol curcumin is most extensively studied for immunomodulatory activities. Curcumin is one of the constituents of curcuminoids, a fraction isolated from rhizomes of Curcuma longa. The other two compounds in curcuminoids are demethoxycurcumin and bisdemethoxycurcumin, and all have potential therapeutic activities (Upadhyaya et al. 2009a, b; Bose et al. 2015; Kesharwani et al. 2015). As an anticancer agent, curcumin recognizes and elicits specific immune response to eradicate neoplastic cells from the host body. It regulates several molecules in cell signal transduction and downregulates several invasions, cell adhesion, and extracellular matrix molecules which are essential for sustaining metastasis (Shehzad and Lee 2013). Various mechanistic pathways are proven for its immunomodulatory effect of curcumin. Curcumin activates proliferator-activated receptor-γ (PPAR-γ) and regulates various biochemical pathways in controlling the inflammatory responses (Fig. 3.3) (Mazidi et al. 2016; Upadhyaya et al. 2009a, b; Singh et al. 2015a, b, c; Kesharwani et al. 2018).
PPAR proteins function within the cell nuclei; control metabolism, development, and homeostasis; and play an important role in cell growth, differentiation, insulin sensitivity, inflammatory response, reproduction, and adipogenesis (Wu et al. 2009b). Inflammatory pathways of curcumin suggest that the effect is achieved mostly through the downregulation of NF-κB (Shishodia 2013). Narala et al. (2009) suggested that PPAR-γ-mediated effects of curcumin are indirect and mediated through endogenous ligands. By inhibiting PPAR-γ-mediated epithelial-mesenchymal transition, curcumin prevents intestinal fibrotic stricture which is a major complication of Crohn’s disease (Xu et al. 2017) and also activates hepatic stellate cells to prevent fibrosis of the liver (Mazidi et al. 2016). Curcumin inhibited epithelial-mesenchymal transition, reduced expression of α-SMA and PAI-1, and increased E-cadherin in n renal tubular epithelial cells, thus preventing tubulointerstitial fibrosis in renal disease (Li et al. 2013). In case of progressive and irreversible pulmonary fibrosis, a distinctive form of chronic interstitial pneumonia, curcumin triggered the expression of nuclear peroxisome PPAR-γ, upregulated cathepsin B and cathepsin L, and downregulated cystatin C (Saidi et al. 2019).
Recently, the role of curcumin on induction, expression, and production of anti-inflammatory cytokine IL-10 was studied (Mollazadeh et al. 2019). IL-10 plays an important role in the prevention of infection-related tissue damage and curcumin-alleviated coccidioidal infection in naturally infected lambs by downregulating pro-inflammatory cytokines, i.e., IFN-γ, and increasing IL-10 (Cervantes-Valencia et al. 2016).
By reducing the expression of iNOS, IFN-γ, and TNF-α, curcumin showed its effect on adaptive immunity in Leishmania infection model (Adapala and Chan 2008). It activated PPAR-γ and deactivated type 1 response.
Curcumin inhibits JAK/STAT signaling by reducing IL-10 levels and increases tumor apoptosis (Shiri et al. 2015). The anticancer activity of curcumin is by blocking the tumor-induced T-cell depletion by increasing the production of IFN-γ and IL-2. Several mechanisms, responsible for the potential antitumor activity of curcumin, proposed were restoration of activated/effector CD+4 and CD+8 T cells, secretion of IFN-γ, augmentation of tumor-infiltrating lymphocytes, and upregulation of IFN-γ mRNA expression (Bhattacharyya et al. 2010).
In a hamster model of accelerated atherosclerosis, curcuma oil, i.e., lipophilic fraction from turmeric, attenuated inflammation and arterial injury (Singh et al. 2015a, b, c). It also increased IL-10 and TGF-β mRNA expression in atherosclerotic arteries and decreased mRNA expression of pro-inflammatory cytokines, namely, TNF-α, IL-6, IL-1β, and IFN-γ. Curcuma oil-treated animals showed increased IL-10 expression in peritoneal macrophages. Curcumin also regulates the expression of genes implicated in tumor cell proliferation, metastasis, and angiogenesis. Physiological and pathological angiogenesis is governed by endothelial progenitor cells. Therefore, Vyas et al. (2015) studied the effect of curcumin on the growth properties of circulating endothelial progenitor cells and showed that curcumin inhibits cell growth by inhibiting the G1 to S phase transition in the cell cycle.
Low serum IL-10 and high serum TNF-α and IL-12 concentrations observed in intestinal colitis are very well normalized by curcumin, thus reducing the disease severity (Sreedhar et al. 2016). In small intestine inflammation, mice model of hyper-acute Th1-type ileitis following peroral infection with Toxoplasma gondii, curcumin, as well resveratrol downregulated Th1-type immune responses (Bereswill et al. 2010). Significant increase in anti-inflammatory IL-10 in the ileum, mesenteric lymph nodes, and spleen was observed, whereas pro-inflammatory cytokine expressions, namely, IL-23p19, IFN-γ, TNF-α, IL-6, and MCP-1, were significantly lowered in the ileum of treated animals. Curcumin, 50 mg/kg daily, by oral route decreased serum lactic acid dehydrogenase, IL-1β, and TNF-α levels, as well as colonic myeloperoxidase and lipid peroxide levels, and increased colonic prostaglandin E2 and IL-10 in acetic acid colitis model (Gopu et al. 2015). Lelli et al. (2017) reviewed the application of curcumin in pulmonary diseases showing abnormal inflammatory responses, like asthma or chronic obstructive pulmonary disease, acute respiratory distress syndrome, pulmonary fibrosis, and acute lung injury. Curcumin has pleiotropic effects, regulating transcription factor NF-κB, cytokine IL-6, TNF-alpha, adhesion molecule ICAM-1, and matrix metalloproteases, and thus is beneficial in inflammatory lung diseases and cancer (Singh et al. 2015a).
Non-neuronal cells such as glial cells play a critical role in the pathogenesis of chronic pain, and curcumin reduces chronic pain by blocking neuroinflammation (Chen et al. 2015). A new application of curcumin, i.e., intrathecal injection for the treatment of arthritic pain, was proven in complete Freund’s adjuvant injection-induced arthritis model. Curcumin treatment efficiently reduced IL-1β, MCP-1, and monocyte inflammatory protein-1α in the spinal cord and showed similar effect in LPS-stimulated cultured astrocytes and microglia. In hind-paw incision model with C57BL/6 mice, curcumin, 50 mg/kg, significantly reduced the intensity of mechanical and heat sensitization (Sahbaie et al. 2014). In this experiment, the effectiveness of curcumin in reducing the pain and inflammation was due to the increase of TGF-β.
In progressive neurodegenerative inflammatory disorders like Parkinson’s disease and Alzheimer’s disease, curcumin exhibited neuroprotective actions. Wang et al. (2017) carried out systematic literature review of experiments performed on neuroprotective actions of curcumin in toxin-base animal models of Parkinson’s disease (Singh et al. 2014). Curcumin showed protection of substantia nigra neurons and improvement in striatal dopamine levels through anti-inflammatory and antioxidant actions. The ability of curcumin to upregulate IL-10, a potent anti-inflammatory cytokine, limits the inducible nitric oxide synthase gene expression, thus reducing the production of neurotoxic nitric oxide. Even in chronic inflammatory autoimmune disease like systemic lupus erythematosus, curcumin showed protective effect by inhibiting maturation of immature dendritic cells, differentiation of naive CD4+ T cells into Th17 and Th1 cells via inhibition of IL-6 and IL-12 production, and also reduction of IFN-γ production (Momtazi-Borojeni et al. 2018).
3.6 Genistein and Daidezin
Isoflavones are plant-derived nonsteroidal polyphenolic compounds representing most common phytoestrogens, i.e., plant-based compounds resembling vertebrate steroids, e.g., 17-β-estradiol. Phytoestrogens are broadly classified as flavonoids and non-flavonoids. Flavonoids include isoflavones, coumestans, and prenylflavonoids, and non-flavonoids include lignans. Isoflavones are considered as phytoestrogens by virtue of their estrogen receptor-binding ability. Genistein, daidzein, glycitein, biochanin A, and formononetin are important isoflavone phytoestrogens (Krizova et al. 2019). Isoflavones have numerous health benefits such as prevention of hormone-related cancers, cardiovascular disease, osteoporosis, and hormone replacement therapy and improving cognitive function (Ko 2014). Specific isoflavones have also shown remarkable biological effects, viz., genistein as antioxidant, anticancer, cardiovascular, and antidiabetic; daidzein as antioxidant, antiosteoporotic, and immunostimulator; formononetin as cardiovascular, antioxidant, and estrogenic; biochanin A as anti-inflammatory, antiproliferative, antioxidant, antiviral, and anticancer; and glycitein as anti-inflammatory (Niaz and Khan 2020).
Genistein, 4′,5,7-trihydroxyisoflavone, is a tyrosine kinase inhibitor abundant in soy products such as soybeans. It is one of the promising and innovative phytoconstituents for the treatment of cancer, osteoporosis, cardiovascular diseases, and menopause exhibiting multifaceted action within the live cell and very low toxicity (Ganai and Farooqi 2015; Polkowski and Mazurek 2000).
Genistein suppresses both the cell-mediated and humoral components of the adaptive immune system as indicated by reduction in the number of developing CD4+ and CD8+ thymocytes (Ganai and Farooqi 2015). It also inhibits tyrosine kinase which is required for NK cell activation (Burkard et al. 2017). Masilamani et al. (2012) has extensively reviewed the role of isoflavones such as genistein, daidzein, glycitein, and their metabolites in regulating immune response. In pharmacological doses, isoflavones particularly genistein exert protective effects over tight junctions between intestinal epithelial cells and the mucosal barrier helping cure inflammation conditions. Being phytoestrogens, isoflavones regulate dendritic cells and downregulate TLR-dependent IL-6 expression. Genistein inhibited NF-κB-dependent gene expression by stimulating p53 expression. In addition, genistein suppressed MHC class II molecules. Inhibition of NK cell cytotoxicity and IgE signaling are other noticeable effects. These effects are varied depending on their cellular targets and also affected by the nature of the experimental setup, strain of the animal used, and dose and duration of isoflavone treatments. Readers are strongly urged to refer the text by Masilamani et al. (2012) for detailed account on the effect of isoflavones on various cells and tissues of the immune system.
Genistein exerts anticancer effects in different types of cancers via cell cycle arrest, apoptosis, antiangiogenesis, and antimetastasis. It acts via molecular targets such as caspases, B-cell lymphoma 2, Bcl-2-associated X protein, NF-κB, phosphoinositide 3-kinase/Akt, extracellular signal-regulated kinase 1/2, mitogen-activated protein kinase, and Wingless/integration 1/β-catenin signaling pathway (Tuli et al. 2019). Immunomodulatory effect of genistein has surfaced in a mouse model of human papillomavirus-associated cervical cancer with significant increase in lymphocyte proliferation, release of lactase dehydrogenase, and significant increment in IFN-γ (Ghaemi et al. 2012).
Antitumor activity of genistein is very well studied in prostate cancer, hepatoma cancer, and pancreatic and lung cancer. Anticancer effect is seen via induction of apoptosis through activation of caspase-3 and downregulation of antiapoptotic Bcl-2 and Bcl-XL family. Induction of G2/M cell cycle arrest by inhibition of AKT phosphorylation and Cdc2 kinase, antiangiogenesis, and antimetastasis are also observe. Genistein is also helpful as an adjuvant with other anticancer drugs such as 5-flurouracil, all-trans retinoic acid, and trichostatin A (Mohamed et al. 2017).
Genistein can also be combined with antiretroviral drugs for inhibiting HIV infection and HIV-related oxidative stress. It inhibits stromal cell-derived factor 1, HIV-mediated chemotactic signaling, and HIV infection of cultured blood T cells and macrophages (Guo and Wu 2018).
Genistein reduces inflammation and enhances Th1/Th2 cytokine-mediated responses mainly via IFN-γ and IL-10, IL-4, and IL-5 in rheumatoid arthritis and allergic asthma (Gandhi et al. 2018). Genistein being immunomodulator, phytoestrogen, and kinase inhibitor showed benefits as prophylactic antiviral drug against arenaviral hemorrhagic fever in the Syrian golden hamster (Vela et al. 2010).
Desmethylangolensin and equol are two major bioactive metabolites of isoflavones. Peripheral blood mononuclear cells pretreated with genistein and equol reduce IL-12/IL-18-induced IFN-γ production by natural killer cells without consistently affecting cytotoxicity (Mace et al. 2019).
Daidzein is known to enhance animal resistance to heat stress and regulate animal immunocompetence. It was found to raise serum IgG and IFN-α significantly upon supplementation through diet to the cows in late lactation (Liu et al. 2014). Daidzein significantly decreased the B-cell population (represented by CD3-IgM+) and increased the T-cell populations (represented by CD3+IgM, CD4+CD8−, and CD4−CD8+) in hybrid B6C3F1 and inbred type 1 diabetes-prone nonobese diabetic mice (Huang et al. 2019). Daidzein supplementation to broiler breeder hens helps improve immune function in offsprings visa increase in B cells and CD4+T/CD8+T 386 ratio as well as the proliferative response of B cells, but no effect was seen on T lymphocytes of the offspring (Fan et al. 2018).
Recently, daidzein attenuated lipopolysaccharide-induced hepatic liver injury. It was found to reduce ALT and AST expressions, reactive oxygen species, IL-lβ, IL-6, and TNF-α with no cytotoxicity. Inhibition of p-ERK1/2, p-IκBα, and p-p65 expression, in addition to downregulating Keap-1, and upregulating Nrf2 expression were revealed (Yu et al. 2020).
The duo genistein and daidzein were found to slow down aging processes by affecting immune processes. Genistein reduced vitellogenin expression and also resistance versus P. luminescens, whereas daidzein increased resistance versus the pathogen in a vitellogenin-dependent manner (Fischer et al. 2012).
Glucosylated derivatives of isoflavones such as glycitein 7-O-β-glucoside, glycitein 7-O-β-maltoside, and daidzein 7-O-β-glucoside inhibited the production of IgE antibody in rats against 7S-globulin as antigen (Shimoda and Hamada 2010). Ethyl acetate extract of Cordyceps militaris rich in isoflavones (genistein, daidzein) and their derivatives (genistein 7-O-β-d-glucoside 4″-O-methylate, genistein 4′-O-β-d-glucoside 4″-O-methylate, glycitein 7-O-β-d-glucoside 4″-O-methylate, daidzein 7-O-β-d-glucoside 4″-O-methylate and adenosine) showed significant antiallergic effect by inhibition of antigen-induced degranulation in RBL-2H3 cells and passive cutaneous anaphylaxis along with reduction of IL-4 and TNF-α . In mast cells, inhibition of phosphorylation of Syk, ERK, p38, and JNK expression was seen (Oh et al. 2011).
Other prominent isoflavones exerting immunomodulatory functions include isonigricin and isoirisolidone (Nazir 2013).
4 Concluding Remarks
The immune system is the most sensitive, however equally efficient integrated functioning of numerous cells and biochemicals developed by these cells to maintain the homeostasis and preserve the integrity of the organism against external harmful stress stimuli. The systematic functioning of the immune system and the balance between all chemicals are essential to the occurrence of any disease or disorder. To date, evidence from literature highlights an increase in immunological diseases because of change in lifestyle, and a great attention has been focused on the development of molecules to modulate the immune response. There is continuously increasing upward surge of demand for new effective therapies all over the world for safe and effective treatments, and researchers are always exploring new avenues for the same. One exciting strategy is the use of herbal medicines as their use in traditional medicine for their properties and health benefits are well recognized and established with safety, since ancient times. Natural products have a wide range of diversity of multidimensional chemical structures; in the meantime, the utility of natural products as biological function modifiers has also raised considerable attention and interest. Apart from versatility, safe and cost-effective therapy and abundant availability are the added advantage of phytochemicals. Scientists have successfully used isolated natural products and combinatorial chemistry in the discovery of new drugs. Despite developments in drug discovery technology, natural products from plants and other biological sources remain an undiminished source of new pharmaceuticals.
Even though great advancements are happening in the area of fundamental molecular biology and pathophysiology, the use of phytopharmaceuticals in modern medicine era is still in preclinical stage, with very few products successful in the market. Despite having beneficial health effects, therapeutic applications of bioactive phytoconstituents are not yet successful due to its poor solubility, short biological half-life, rapid metabolism, and elimination. In order to achieve a maximum benefit of phytochemicals as immunomodulators for antioxidant, anti-inflammatory, antifibrotic, chemo-preventive agents and also for metabolic and neurological disorders for human use, efforts should be focused to improve upon the solubility, stability, and targeted delivery for improving the bioavailability. Additionally, the toxicity associated with the high doses of phytochemicals required to achieve desirable response needs to be reduced. Nanotechnological strategies may be used to improve the bioavailability and targeting efficiency, thus reducing the dose requirements.
References
Abdel-Latif M, Afifi A, Soliman R, Elkhouly A, Abdelmotaal A, Youness RA (2019) 23P—A new quercetin glycoside enhances TNBC immunological profile through TP53/miR-155/MICA/ULBP2. Ann Oncol 30:7–8
Adapala N, Chan M (2008) Long-term use of an anti-inflammatory, curcumin, suppressed type 1 immunity and exacerbated visceral leishmaniasis in a chronic experimental model. Lab Investig 88:1329–1339
Ahn SC, Kim GY, Kim JH, Baik SW, Han MK, Lee HJ, Moon DO, Lee CM, Kang JH, Kim BH, Oh YH, Park YM (2004) Epigallocatechin-3-gallate, constituent of green tea, suppresses the LPS-induced phenotypic and functional maturation of murine dendritic cells through inhibition of mitogen-activated protein kinases and NF-kappaB. Biochem Biophys Res Commun 313(1):148–155
Al Azzaz J, Rieu A, Aires V, Delmas D, Chluba J, Winckler P, Bringer MA, Lamarche J, Vervandier-Fasseur D, Dalle F, Lapaquette P, Guzzo J (2019) Resveratrol-induced xenophagy promotes intracellular bacteria clearance in intestinal epithelial cells and macrophages. Front Immunol 9:3149
Alrafas HR, Busbee PB, Nagarkatti M, Nagarkatti PS (2020) Resveratrol downregulates mir-31 to promote t regulatory cells during prevention of TNBS-induced colitis. Mol Nutr Food Res 64(1):e1900633
Al-Rasheed NM, Fadda L, Attia HA, Sharaf IA, Mohamed AM, Al-Rasheed NM (2017) Pulmonary prophylactic impact of melatonin and/or quercetin: a novel therapy for inflammatory hypoxic stress in rats. Acta Pharma 67:125–135
Altamemi I, Murphy EA, Catroppo JF, Zumbrun EE, Zhang J, McClellan JL, Singh UP, Nagarkatti PS, Nagarkatti M (2014) Role of microRNAs in resveratrol-mediated mitigation of colitis-associated tumorigenesis in Apc (Min/+) mice. J Pharmacol Exp Ther 350(1):99–109
Anonymous (1994) Randomised trial comparing tacrolimus (FK506) and cyclosporin in prevention of liver allograft rejection. European FK506 Multicentre Liver Study Group. Lancet 344(8920):423–428
Ay M, Charli A, Jin H, Anantharam V, Kanthasamy A, Kanthasamy AG (2016) Quercetin. In: Gupta RC (ed) Nutraceuticals. Academic Press, Boston, pp 447–452
Banerjee G, Bhat J, Sinkar VP, Telkar A, Upadhyaya SA (2009) Composition for enhancing immunity. US Patent 2009/0175964 A1, 9 Jul 2009
Bascones-Martinez A, Mattila R, Gomez-Font R, Meurman JH (2014) Immunomodulatory drugs: oral and systemic adverse effects. Med Oral Patol Oral Cir Bucal 19:e24–e31
Belkhelfa-Slimani R, Djerdjouri B (2017) Caffeic acid and quercetin exert caspases-independent apoptotic effects on Leishmania major promastigotes, and reactivate the death of infected phagocytes derived from BALB/c mice. Asian Pac J Trop Biomed 7:321–331
Benavides J, Martínez-Valladares M, Tejido ML, Giráldez FJ, Bodas R, Prieto N, Perez V, Andres S (2013) Quercetin and flaxseed included in the diet of fattening lambs: effects on immune response, stress during road transport and ruminal acidosis. Livestock Prod Sci 158:84–90
Bereswill S, Munoz M, Fischer A, Plickert R, Haag LM, Otto B, Kuhl AA, Loddenkemper C, Gobel UB, Heimesaat MM (2010) Anti-inflammatory effects of resveratrol, curcumin and simvastatin in acute small intestinal inflammation. PLoS One 5(12):e15099
Besednova NN, Zvyagintseva TN, Kuznetsova TA, Makarenkova ID, Smolina TP, Fedyanina LN, Kryzhanovky SP, Zaporozhets TS (2019) Marine algae metabolites as promising therapeutics for the prevention and treatment of HIV/AIDS. Metabolites 9(5):87
Bhattacharyya S, Md Sakib Hossain D, Mohanty S, Sankar Sen G, Chattopadhyay S, Banerjee S, Chakraborty J, Das K, Sarkar D, Das T, Sa G (2010) Curcumin reverses T cell-mediated adaptive immune dysfunctions in tumor-bearing hosts. Cell Mol Immunol 7(4):306–315
Bose S, Panda AK, Mukherjee S, Sa G (2015) Curcumin and tumor immune-editing: resurrecting the immune system. Cell Div 10:6
Bule MH, Ahmed I, Maqbool F, Bilal M, Iqbal H (2018) Microalgae as a source of high-value bioactive compounds. Front Biosci 10:197–216
Burkard M, Leischner C, Lauer UM, Busch C, Venturelli S, Frank J (2017) Dietary flavonoids and modulation of natural killer cells: implications in malignant and viral diseases. J Nutr Biochem 46:1–12
Burmańczuk A, Hola P, Milczak A, Piech T, Kowalski C, Wojciechowska B, Grabowski T (2018) Quercetin decrease somatic cells count in mastitis of dairy cows. Res Vet Sci 117:255–259
Butt MS, Sultan MT (2011) Ginger and its health claims: molecular aspects. Crit Rev Food Sci Nutr 51:383–393
Cardwell G, Bornman JF, James AP, Black LJ (2018) A review of mushrooms as a potential source of dietary vitamin D. Nutrients 10(10):1498
Cataneo AHD, Tomiotto-Pellissier F, Miranda-Sapla MM, Assolini JP, Panis C, Kian D, Yamauchi LM, Simao ANC, Casagrande R, Pinge-Filho P, Costa IN, Verri WA, Conchon-Costa I, Pavanelli WR (2019) Quercetin promotes antipromastigote effect by increasing the ROS production and anti-amastigote by upregulating Nrf2/HO-1 expression, affecting iron availability. Biomed Pharmacother 113:108745
Cattelan A, Ceolotto G, Bova S, Albiero M, Kuppusamy M, De Martin S, Semplicini A, Fadini GP, de Kreutzenberg SV, Avogaro A (2015) NAD (+)-dependent SIRT1 deactivation has a key role on ischemia-reperfusion-induced apoptosis. Vascul Pharmacol 70:35–44
Cervantes-Valencia ME, Alcalá-Canto Y, Sumano-Lopez H, Ducoing-Watty AM, Gutierrez-Olvera L (2016) Effects of Curcuma longa dietary inclusion against Eimeria spp. in naturally-infected lambs. Small Rumin Res 136:27–35
Chan KH, Chan SC, Yeung SC, Man RY, Ip MS, Mak JC (2012) Inhibitory effect of Chinese green tea on cigarette smoke-induced up-regulation of airway neutrophil elastase and matrix metalloproteinase-12 via antioxidant activity. Free Radic Res 46(9):1123–1129
Chanput W, Mes J, Vreeburg RAM, Savelkoul HFJ, Wichers HJ (2010) Transcription profiles of LPS-stimulated THP-1 monocytes and macrophages: a tool to study inflammation modulating effects of food-derived compounds. Food Funct 1:254–261
Chen C-J, Tsai CC, Hsieh J-F, Chien CM, Wu T-H, Chen S-T (2006) A screening platform for compounds with potential immuno-regulatory activities using human cord blood mononuclear cells. Comb Chem High Throughput Screen 9:777–784
Chen CJ, Yu W, Fu YC, Wang X, Li JL, Wang W (2009) Resveratrol protects cardiomyocytes from hypoxia-induced apoptosis through the SIRT1-FoxO1 pathway. Biochem Biophys Res Commun 378(3):389–393
Chen JJ, Dai L, Zhao LX, Zhu X, Cao S, Gao YJ (2015) Intrathecal curcumin attenuates pain hypersensitivity and decreases spinal neuroinflammation in rat model of monoarthritis. Sci Rep 5:10278
Chen X, Song L, Wang H, Liu S, Yu H, Wang X, Li R, Liu T, Li P (2019) Partial characterization, the immune modulation and anticancer activities of sulfated polysaccharides from filamentous microalgae Tribonema sp. Molecules 24(2):322
Choi KC, Jung MG, Lee YH, Yoon JC, Kwon SH, Kang HB, Kim MJ, Cha JH, Kim YJ, Jun WJ, Lee JM, Yoon HG (2009) Epigallocatechin-3-gallate, a histone acetyltransferase inhibitor, inhibits EBV-induced B lymphocyte transformation via suppression of RelA acetylation. Cancer Res 69(2):583–592
Cutignano A, Nuzzo G, Ianora A, Luongo E, Romano G, Gallo C, Sansone C, Aprea S, Mancini F, D’Oro U, Fontana A (2015) Development and application of a novel SPE-method for bioassay-guided fractionation of marine extracts. Mar Drugs 13:5736–5749
De Souza NJ, Yeole R, Jha R, Bagchi S (2002) Use of Tinospora extract in the treatment of immune system-modulated disorders. WO Patent 02/053166 A1, 11 Jul 2002
Dekker P, Parish WE, Green MR (2005) Protection by food-derived antioxidants from UV-A1-induced photodamage, measured using living skin equivalents. Photochem Photobiol 81:837–842
Ding Y, Li C, Zhang Y, Ma P, Zhao T, Che D, Cao J, Wang J, Liu R, Zhang T, He L (2020) Quercetin as a Lyn kinase inhibitor inhibits IgE-mediated allergic conjunctivitis. Food Chem Toxicol 135:110924
Dona M, DellAica I, Calabrese F, Benelli R, Morini M, Albini A, Garbisa S (2003) Neutrophil restraint by green tea: inhibition of inflammation, associated angiogenesis, and pulmonary fibrosis. J Immunol 170(8):4335–4341
Dou W, Zhang J, Ren G, Ding L, Sun A, Deng C, Wu X, Wei X, Mani S, Wang Z (2014) Mangiferin attenuates the symptoms of dextran sulfate sodium-induced colitis in mice via NF-κB and MAPK signaling inactivation. Int Immunopharmacol 23(1):170–178
Edo Y, Otaki A, Asano K (2018) Quercetin enhances the thioredoxin production of nasal epithelial cells in vitro and in vivo. Medicine 5:124
Eitah HE, Maklad YA, Abdelkader NF, Gamal el Din AA, Badawi MA, Kenawy SA (2019) Modulating impacts of quercetin/sitagliptin combination on streptozotocin-induced diabetes mellitus in rats. Toxicol Appl Pharmacol 365:30–40
Fan H, Lv Z, Gan L, Guo Y (2018) Transcriptomics-related mechanisms of supplementing laying broiler breeder hens with dietary daidzein to improve the immune function and growth performance of offspring. J Agric Food Chem 66:2049–2060
Fischer M, Regitz C, Kahl M, Werthebach M, Boll M, Wenzel U (2012) Phytoestrogens genistein and daidzein affect immunity in the nematode Caenorhabditis elegans via alterations of vitellogenin expression. Mol Nutr Food Res 56:957–965
Gambini J, Ingles M, Olaso G, Lopez-Grueso R, Bonet-Costa V, Gimeno-Mallench L, Mas-Bargues C, Abdelaziz KM, Gomez-Cabrera MC, Vina J, Borras C (2015) Properties of resveratrol: in vitro and in vivo studies about metabolism, bioavailability, and biological effects in animal models and humans. Oxid Med Cell Longev 2015:837042
Ganai AA, Farooqi H (2015) Bioactivity of genistein: a review of in vitro and in vivo studies. Biomed Pharmacother 76:30–38
Gandhi GR, Neta MTSL, Sathiyabama RG, de Quintans JSS, de Olive e Sirailva AM, de Araújo AAS, Narain N, LSJ Q, Gurgel RQ (2018) Flavonoids as Th1/Th2 cytokines immunomodulators: a systematic review of studies on animal models. Phytomedicine 44:74–84
Ghaemi A, Soleimanjahi H, Razeghi S, Gorji A, Tabaraei A, Moradi A, Alizadeh A, Vakili M (2012) Genistein induces a protective immunomodulatory effect in a mouse model of cervical cancer. Iran J Immunol 9:119–127
Gibbons S (2003) An overview of plant extracts as potential therapeutics. Expert Opin Ther Patents 13(4):489–497
Gopu B, Dileep R, Rani MU, Kumar CS, Kumar MV, Reddy AG (2015) Protective role of curcumin and flunixin against acetic acid-induced inflammatory bowel disease via modulating inflammatory mediators and cytokine profile in rats. J Environ Pathol Toxicol Oncol 34(4):309–320
Guo J, Wu Y (2018) Genistein and HIV infection. In: Preedy VR, Watson RR (eds) HIV/AIDS. Academic Press, Boston, pp 125–134
Haraoui B (2015) Leflunomide. In: Hochberg MC, Silman AJ, Smolen JS, Weinblatt ME, Weisman MH (eds) Rheumatology, 6th edn. Elsevier, pp 451–458
Hayakawa S, Saito K, Miyoshi N, Ohishi T, Oishi Y, Miyoshi M, Nakamura Y (2016) Anti-cancer effects of green tea by either anti- or pro- oxidative mechanisms. Asian Pac Cancer Prev 17:1649–1654
Hirahashi T, Matsumoto M, Hazeki K, Saeki Y, Ui M, Seya T (2002) Activation of the human innate immune system by Spirulina: augmentation of interferon production and NK cytotoxicity by oral administration of hot water extract of Spirulina platensis. Int Immunopharmacol 2:423–434
Holt S (2007) Herbal compositions, methods of stimulating immunomodulation and enhancement of immunomodulating agents using the herbal compositions US Patent 2007/0196381 A1, 23 Aug 2007
Huang G, Xu J, Guo TL (2019) Isoflavone daidzein regulates immune responses in the B6C3F1 and non-obese diabetic (NOD) mice. Int Immunopharmacol 71:277–284
Ichikawa D, Matsui A, Imai M, Sonoda Y, Kasahara T (2004) Effect of various catechins on the IL-12p40 production by murine peritoneal macrophages and a macrophage cell line, J774.1. Biol Pharm Bull 27:1353–1358
Jadhav SS, Patwardhan B, Gautam M (2010) Adjuvant composition for vaccine. US Patent 2010/0285064 A1, 11 Nov 2010
Jewett A, Tseng HC (2017) Immunotherapy. In: Dowd FJ, Johnson BS, Mariotti AJ (eds) Pharmacology and therapeutics for dentistry, 7th edn. Mosby, St. Louis, pp 504–529
Joo SY, Song YA, Park YL, Myung E, Chung CY, Park KJ, Cho SB, Lee WS, Kim HS, Rew JS, Kim NS, Joo YE (2012) Epigallocatechin-3-gallate inhibits LPS-induced NF-κB and MAPK signaling pathways in bone marrow-derived macrophages. Gut Liver 6(2):188–196
Ju SA, Park SM, Lee YS, Bae JH, Yu R, An WG, Suh JH, Kim BS (2012) Administration of 6-gingerol greatly enhances the number of tumor-infiltrating lymphocytes in murine tumors. Int J Cancer 130(11):2618–2628
Kapoor V, Aggarwal S, Das SN (2016) 6-gingerol mediates its anti tumor activities in human oral and cervical cancer cell lines through apoptosis and cell cycle arrest. Phytother Res 30(4):588–595
Kawabata K, Mukai R, Ishisaka A (2015) Quercetin and related polyphenols: new insights and implications for their bioactivity and bioavailability. Food Funct 6:1399–1417
Keservani RK, Kesharwani RK, Sharma AK, Jarouliya U (2016a) Chapter 20—Dietary supplements, nutraceutical and functional foods in immune response (immunomodulators). In: Bagchi D, Preuss HG, Swaroop A (eds) Nutraceutical and functional foods in human life and disease prevention. CRC Press, Taylor and Francis, Boca Raton, FL, pp 343–358. isbn:9781482237214
Keservani RK, Sharma AK, Kesharwani RK (2016b) An overview and therapeutic applications of nutraceutical & functional foods. In: Keservani RK, Sharma AK, Kesharwani RK (eds) Handbook of research on novel approaches for drug delivery. IGI Global Publisher, USA
Keservani RK, Sharma AK, Kesharwani RK (2016c) Nutraceutical and functional foods for cardiovascular health. In: Meghwal M, Goyal MR (eds) Food process engineering: emerging technologies and innovations in food engineering, vol 5. Apple Academic Press, CRC Press, Taylor and Francis. isbn:9781771884020
Keservani RK, Sharma AK, Kesharwani RK (2018) Nutraceutical and functional foods in disease prevention. IGI Global. isbn13:9781522532675
Keservani RK, Sharma AK, Kesharwani RK (2020) Nutraceuticals and dietary supplements: applications in health improvement and disease management. isbn:9781771888738
Kesharwani RK, Misra K (2010) Prediction of binding site for Curcuminoids at human Topoisomerase II α protein; an in silico approach. Curr Sci 101(8):1060–1064
Kesharwani RK, Srivastava V, Singh P, Rizvi SI, Adeppa K, Misra K (2015) A novel approach for overcoming drug resistance in breast cancer chemotherapy by targeting new synthetic curcumin analogues against Aldehyde Dehydrogenase 1 (ALDH1A1) and Glycogen Synthase Kinase-3 β (GSK-3β). Appl Biochem Biotechnol 2015. https://doi.org/10.1007/s12010-015-1696-x
Kesharwani RK, Singh DB, Singh DV, Misra K (2018) Computational study of curcumin analogues by targeting DNA topoisomerase II: a structure-based drug designing approach. Network Model Anal Health Infor Bioinformatics 7(1):1–7
Khan N, Monagas M, Urpi-sarda M, Llorach R, Andres-Lacueva C (2013) Contribution of bioactive foods and their emerging role in immunomodulation, inflammation, and arthritis. In: Bioactive food as dietary interventions for arthritis and related inflammatory diseases. Elsevier, Amsterdam, pp 43–65
Kim EC, Min JK, Kim TY, Lee SJ, Yang HO, Han S, Kim YM, Kwon YG (2005) [6]-Gingerol, a pungent ingredient of ginger, inhibits angiogenesis in vitro and in vivo. Biochem Biophys Res Commun 335(2):300–308
Kim BR, Yang S, Doh EJ, Choi CW, Youn SW (2018) Risk factors affecting adverse effects of cyclosporine a in a real-world psoriasis treatment. Ann Dermatol 30(2):143–149
Kjær TN, Thorsen K, Jessen N, Stenderup K, Pedersen SB (2015) Resveratrol ameliorates imiquimod-induced psoriasis-like skin inflammation in mice. PLoS One 10(5):e0126599
Ko K-P (2014) Isoflavones: chemistry, analysis, functions and effects on health and cancer. Asia Pac Cancer Prev 15:7001–7010
Kong S, McBurney MW, Fang D (2012) Sirtuin 1 in immune regulation and autoimmunity. Immunol Cell Biol 90(1):6–13
Krizova L, Dadakova K, Kasparovska J, Kasparovsky T (2019) Isoflavones. Molecules 24:1076
Kumar D, Arya V, Kaur R, Bhat ZA, Gupta VK, Kumar V (2012) A review of immunomodulators in the Indian traditional health care system. J Microbiol Immunol Infect 45:165–184
Lai CY, Su YW, Lin KI, Hsu LC, Chuang TH (2017) Natural modulators of endosomal toll-like receptor-mediated psoriatic skin inflammation. J Immunol Res 2017:7807313. https://doi.org/10.1155/2017/7807313
Lam PYS (2003) Herbal immune system stimulant. WO Patent 03/068145 A2, 21 Aug 2003
Lee SM, Yang H, Tartar DM, Gao B, Luo X, Ye SQ, Zaghouani H, Fang D (2011) Prevention and treatment of diabetes with resveratrol in a non-obese mouse model of type 1 diabetes. Diabetologia 54(5):1136–1146
Lee J, Choi JW, Sohng JK, Pandey RP, Il PY (2016) The immunostimulating activity of quercetin 3-O-xyloside in murine macrophages via activation of the ASK1/MAPK/NF-κB signaling pathway. Int Immunopharmacol 31:88–97
Lee-Huang S, Huang PL, Huang PL, Zhang D, Zhang J, Chang YT, Lee JW, Bao J, Sun Y (2009) Compositions and methods for treating obesity, obesity related disorders and for inhibiting the infectivity of human immunodeficiency virus. US Patent 2009/0061031A1, 5 Mar 2009
Lelli D, Sahebkar A, Johnston TP, Pedone C (2017) Curcumin use in pulmonary diseases: state of the art and future perspectives. Pharmacol Res Commun 115:133–148
Li R, Wang Y, Liu Y, Chen Q, Fu W, Wang H, Cai H, Peng W, Zhang X (2013) Curcumin inhibits transforming growth factor-β1-induced EMT via PPARγ pathway, not Smad pathway in renal tubular epithelial cells. PLoS One 8(3):e58848
Liu HS, Pan CE, Yang W, Liu XM (2003) Antitumor and immunomodulatory activity of resveratrol on experimentally implanted tumor of H22 in Balb/c mice. World J Gastroenterol 9(7):1474–1476
Liu D-Y, He S-J, Liu S-Q, Tang Y-G, Jin E-H, Chen H-L, Li S-H, Zhong L-T (2014) Daidzein enhances immune function in late lactation cows under heat stress. J Anim Sci 85:85–89
Liu D, Chen YQ, Xiao XW, Zhong RT, Yang CF, Liu B, Zhao C (2019) Nutrient properties and nuclear magnetic resonance-based metabonomic analysis of macrofungi. Foods 8(9):397
Lu (2008) A herbal medicine extract that induces interferon production by immune cells and activates Toll-like receptors. JP 4980305B2, 18 Jul 2012
Lu J, Guan S, Shen X, Qian W, Huang G, Deng X, Xie G (2011) Immunosuppressive activity of 8-gingerol on immune responses in mice. Molecules 16:2636–2645
Luis Espinoza J, Takami A, Trung LQ, Nakao S (2013) Ataxia-telangiectasia mutated kinase-mediated upregulation of NKG2D ligands on leukemia cells by resveratrol results in enhanced natural killer cell susceptibility. Cancer Sci 104(6):657–662
Mace TA, Ware MB, King SA, Loftus S, Farren MR, McMichael E, Scoville S, Geraghty C, Young G, Carson WE III, Clinton C, Lesinski GB (2019) Soy isoflavones and their metabolites modulate cytokine-induced natural killer cell function. Sci Rep 9:5068
Malaguarnera L (2019) Influence of Resveratrol on the Immune Response. Nutrients 11(5):946
Mallard B, Leach DN, Wohlmuth H, Tiralongo J (2019) Synergistic immuno-modulatory activity in human macrophages of a medicinal mushroom formulation consisting of Reishi, Shiitake and Maitake. PLoS One 14(11):e0224740
Manna SK, Mukhopadhyay A, Aggarwal BB (2000) Resveratrol suppresses TNF-induced activation of nuclear transcription factors NF-kappa B, activator protein-1, and apoptosis: potential role of reactive oxygen intermediates and lipid peroxidation. J Immunol 164(12):6509–6519. https://doi.org/10.4049/jimmunol.164.12.6509
Manzo E, Cutignano A, Pagano D, Gallo C, Barra G, Nuzzo G, Sansone C, Ianora A, Urbanek K, Fenoglio D, Ferrera F, Bernardi C, Parodi A, Pasquale G, Leonardi A, Filaci G, De Palma R, Fontana A (2017) A new marine-derived sulfoglycolipid triggers dendritic cell activation and immune adjuvant response. Sci Rep 7(1):6286
Martínez Andrade KA, Lauritano C, Romano G, Ianora A (2018) Marine microalgae with anti-cancer properties. Mar Drugs 16(5):165
Masilamani M, Wei J, Sampson HA (2012) Regulation of the immune response by soybean isoflavones. Immunol Res 54:95–110
Matsuo N, Yamada K, Shoji K, Mori M, Sugano M (1997) Effect of tea polyphenols on histamine release from rat basophilic leukemia (RBL-2H3) cells: the structure-inhibitory activity relationship. Allergy 52(1):58–64
Mazidi M, Karimi E, Meydani M, Ghayour-Mobarhan M, Ferns GA (2016) Potential effects of curcumin on peroxisome proliferator-activated receptor-γ in vitro and in vivo. World J Methodol 6(1):112–117
Melgarejo E, Medina MA, Sanchez-Jimenez F, Urdiales JL (2009) Epigallocatechin gallate reduces humanmonocyte mobility and adhesion in vitro. Br J Pharmacol 158(7):1705–1712
Mishra H, Kesharwani RK, Singh DB, Tripathi S, Dubey SK, Misra K (2019) Computational simulation of inhibitory effects of curcumin, retinoic acid and their conjugates on GSK-3 beta. Netw Model Anal Health Inform Bioinform 8(1):3
Mitra SK, Saxena E, Dixit MN (2009) Natural immunostimulant compositions, methods for obtaining the same and pharmaceutical formulations thereof US Patent 2009/0136602 A1, 28 May 2009
Mlcek J, Jurikova T, Skrovankova S, Sochor J (2016) Quercetin and its anti-allergic immune response. Molecules 21(5):623
Mohamed SIA, Jantan I, Haque MA (2017) Naturally occurring immunomodulators with antitumor activity: an insight on their mechanisms of action. Int Immunopharmacol 50:291–304
Mollazadeh H, Cicero A, Blesso CN, Pirro M, Majeed M, Sahebkar A (2019) Immune modulation by curcumin: the role of interleukin-10. Crit Rev Food Sci Nutr 59(1):89–101
Momtazi-Borojeni AA, Haftcheshmeh SM, Esmaeili SA, Johnston TP, Abdollahi E, Sahebkar A (2018) Curcumin: a natural modulator of immune cells in systemic lupus erythematosus. Autoimmunol Rev 17(2):125–135
Morris PJ (2014) Azathioprine. In: Morris PJ, Knechtle SJ (eds) Kidney transplantation–principles and practice, 7th edn. Elsevier, Amsterdam, pp 216–220
Nair MPN, Kandaswami C, Mahajan S, Chadha KC, Chawda R, Nair H, Kumar N, Nair R, Schwartz S (2002) The flavonoid, quercetin, differentially regulates Th-1 (IFNgamma) and Th-2 (IL4) cytokine gene expression by normal peripheral blood mononuclear cells. Biochim Biophys Acta 1593:29–36
Nair A, Chattopadhyay D, Saha B (2019) Plant-derived immunomodulators. Elsevier, Amsterdam, pp 435–499
Nakayama H, Yaguchi T, Yoshiya S, Nishizaki T (2012) Resveratrol induces apoptosis MH7A human rheumatoid arthritis synovial cells in a sirtuin 1-dependent manner. Rheumatol Int 32(1):151–157
Naman CB, Gomes CM, Gupta G (2018) Phytodrugs and immunomodulators for the therapy of leishmaniasis. In: Mandal SC, Mandal V, Konishi T (eds) Natural products and drug discovery. Elsevier, Amsterdam, pp 213–275
Narala VR, Smith MR, Adapala RK, Ranga R, Panati K, Moore BB, Leff T, Reddy VD, Kondapi AK, Reddy RC (2009) Curcumin is not a ligand for peroxisome proliferator-activated receptor-γ. Gene Ther Mol Biol 13(1):20–25
Nazir N (2013) Immunomodulatory activity of isoflavones isolated from Iris kashmiriana: effect on T-lymphocyte proliferation and cytokine production in Balb/c mice. Biom Prev Nutr 3:151–157
Niaz K, Khan F (2020) Analysis of polyphenolics. In: Sanches Silva A, Nabavi SF, Saeedi M, Nabavi SM (eds) Recent advances in natural products analysis. Elsevier, Amsterdam, pp 39–197
Nunes S, Danesi F, Del Rio D, Silva P (2018) Resveratrol and inflammatory bowel disease: the evidence so far. Nutr Res Rev 31(1):85–97
Ogino MH, Tadi P (2020) Cyclophosphamide. In: Stat Pearls. StatPearls Publishing, Treasure Island, FL
Oh JY, Choi W-S, Lee CH, Park HJ (2011) The ethyl acetate extract of Cordyceps militaris inhibits IgE-mediated allergic responses in mast cells and passive cutaneous anaphylaxis reaction in mice. J Ethnopharmacol 135:422–429
Oliveira A, Monteiro V, Navegantes-Lima KC, Reis JF, Gomes RS, Rodrigues D, Gaspar S, Monteiro MC (2017) Resveratrol role in autoimmune disease—a mini-review. Nutrients 9:1306
Oosthuizen CB (2015) Shoot extracts and compositions of Euclea natalensis for immune modulation and hepatoprotection. WO Patent 2015/049643 Al, 9 Apr 2015
Pae M, Wu D (2013) Immunomodulating effects of epigallocatechin-3-gallate from green tea: mechanisms and applications. Food Funct 4:1287–1303
Pan J, Shen J, Si W, Du C, Chen D, Xu L, Yao M, Fu P, Fan W (2017) Resveratrol promotes MICA/B expression and natural killer cell lysis of breast cancer cells by suppressing c-Myc/miR-17 pathway. Oncotarget 8:65743–65758
Patwardhan B, Kapadi AH (2004) Withasol and methods of use. US Patent 2004/0033273A1, Published on 19 Feb 2004
Pei Y, Du X, Li J, Gao H, Wang S (2009) Effect of proliferation, c-met and vascular endothelial growth factor expression in the Eca109/9706 cells by liposomal quercetin. Wei Sheng Yan Jiu 38:599–602. Abstract only
Pham PT, Pham PM, Pham SV, Pham PA, Pham PC (2011) New onset diabetes after transplantation (NODAT): an overview. Diabetes Metab Syndr Obes 4:175–186
Polkowski K, Mazurek AP (2000) Biological properties of genistein. A review of in vitro and in vivo data. Acta Pol Pharm 57:135–155
Pund S, Thakur R, More U, Joshi A (2014) Lipid based nanoemulsifying resveratrol for improved physicochemical characteristics, in vitro cytotoxicity and in vivo antiangiogenic efficacy. Colloids Surf B Biointerfaces 120:110–117
Pund S, Joshi A, Patravale V (2020) Exploration of nanonutraceuticals in neurodegenerative diseases. In: Keservani R (ed) Nutraceutical and dietary supplements. Applications in health improvement and disease management. Apple Academic Press
Pylypchuk V (2011) Composition and methods of use of an immunomodulator. US Patent 7.964.221 B2, Published on 21 Jun 2011
Rahal K, Schmiedlin-Ren P, Adler J, Dhanani M, Sultani V, Rittershaus AC, Reingold L, Zhu J, McKenna BJ, Christman GM, Zimmermann EM (2012) Resveratrol has antiinflammatory and antifibrotic effects in the peptidoglycan-polysaccharide rat model of Crohn’s disease. Inflamm Bowel Dis 18:613–623
Rahman S, Islam R (2011) Mammalian Sirt1: insights on its biological functions. Cell Commun Signal 9:11
Rainard P, Foucras G, Boichard D, Rupp R (2018) Low milk somatic cell count and susceptibility to mastitis. J Dairy Sci 101:6703–6714
Rangel O (2008) Synergistic Inmune Phyto-Nutraceutical Composition. US Patent 2008/0118582 A1, Published on 22 May 2008
Riccio G, Lauritano C (2019) Microalgae with immunomodulatory activities. Mar Drugs 18(1):2
Rieder SA, Nagarkatti P, Nagarkatti M (2012) Multiple anti-inflammatory pathways triggered by resveratrol lead to amelioration of staphylococcal enterotoxin B-induced lung injury. Br J Pharmacol 167:1244–1258
Rosmarin DM, Lebwohl M, Elewski BE, Gottlieb AB (2010) National psoriasis foundation. cyclosporine and psoriasis: 2008 national psoriasis foundation consensus conference. J Am Acad Dermatol 62:838–853
Ruansit W, Charerntantanakul W (2020) Oral supplementation of quercetin in PRRSV-1 modified-live virus vaccinated pigs in response to HP-PRRSV-2 challenge. Vaccine 38:3570–3581
Ruiz R, Kirk AD (2015) Long-term toxicity of immunosuppressive therapy. Transplant Liver:1354–1363. https://doi.org/10.1016/B978-1-4557-0268-8.00097-X
Sahbaie P, Sun Y, Liang DY, Shi XY, Clark JD (2014) Curcumin treatment attenuates pain and enhances functional recovery after incision. Anesth Analg 118:1336–1344
Saidi A, Kasabova M, Vanderlynden L, Wartenberg M, Kara-Ali GH, Marc D, Lecaille F, Lalmanach G (2019) Curcumin inhibits the TGF-β1-dependent differentiation of lung fibroblasts via PPARγ-driven upregulation of cathepsins B and L. Sci Rep 9(1):491
Saqib U, Kelley TT, Panguluri SK, Liu D, Savai R, Baig MS, Schürer SC (2018) Polypharmacology or promiscuity? Structural interactions of resveratrol with its bandwagon of targets. Front Pharmacol 9:1201
Sartor L, Pezzato E, Garbisa S (2002) (-) Epigallocatechin-3-gallate inhibits leukocyte elastase: potential of the phyto-factor in hindering inflammation, emphysema, and invasion. J Leucoc Biol 71:73–79
Sgro C (1995) Side-effects of a monoclonal antibody, muromonab CD3/orthoclone OKT3: bibliographic review. Toxicology 105:23–29
Sharma A, Kashyap D, Sak K, Tuli HS, Sharma AK (2018) Therapeutic charm of quercetin and its derivatives: a review of research and patents. Pharm Pat Anal 7:15–32
Shebeko SK, Zupanets IA, Popov OS, Tarasenko OO, Shalamay AS (2018) Chapter 27—Effects of quercetin and its combinations on health. In: Watson RR, Preedy VR, Zibadi S (eds) BT-PM of A in HH and D, 2nd edn. Academic Press, pp 373–394
Shehzad A, Lee YS (2013) Molecular mechanisms of curcumin action: signal transduction. Biofactors 39:27–36
Shi Y, Zhou J, Jiang B, Miao M (2017) Resveratrol and inflammatory bowel disease. Ann N Y Acad Sci 1403:38–47
Shim JH, Choi HS, Pugliese A, Lee SY, Chae J, Choi BY, Bode AM, Dong Z (2008) (-)-Epigallocatechin gallate regulates CD3-mediated T cell receptor signaling in leukemia through the inhibition of ZAP-70 kinase. J Biol Chem 283:28370–28379
Shimoda K, Hamada H (2010) Synthesis of beta-maltooligosaccharides of glycitein and daidzein and their anti-oxidant and anti-allergic activities. Molecules 15:5153–5161
Shiri S, Alizadeh AM, Baradaran B, Farhanghi B, Shanehbandi D, Khodayari S, Khodayari H, Tavassoli A (2015) Dendrosomal curcumin suppresses metastatic breast cancer in mice by changing m1/m2 macrophage balance in the tumor microenvironment. Asian Pac J Cancer Prev 16:3917–3922
Shishodia S (2013) Molecular mechanisms of curcumin action: gene expression. BioFactors (Oxford, England) 39:37–55
Signorelli P, Ghidoni R (2005) Resveratrol as an anticancer nutrient: molecular basis, open questions and promises. J Nutr Biochem 16:449–466
Singh RS, Walia AK (2018) Lectins from red algae and their biomedical potential. J Appl Phycol 30:1833–1858
Singh U, Tabibian J, Venugopal SK, Devaraj S, Jialal I (2005) Development of an in vitro screening assay to test the antiinflammatory properties of dietary supplements and pharmacologic agents. Clin Chem 51:2252–2256
Singh DB, Gupta M, Kesharwani R, Sagar M, Dwivedi S, Misra K (2014) Molecular drug targets and therapies for Alzheimer’s disease. Transl Neurosci 5(3):203–217
Singh P, Kesharwani RK, Misra K, Rizvi SI (2015a) Modulation of erythrocyte plasma membrane redox system (PMRS) activity by curcumin, vol 2015. Biochem Res Int, p 702039
Singh P, Kesharwani RK, Misra K, Rizvi SI (2015b) The modulation of erythrocyte Na+/K+-ATPase activity by curcumin. J Adv Res 6(6):1023–1030
Singh V, Rana M, Jain M, Singh N, Naqvi A, Malasoni R, Dwivedi AK, Dikshit M, Barthwal MK (2015c) Curcuma oil attenuates accelerated atherosclerosis and macrophage foam-cell formation by modulating genes involved in plaque stability, lipid homeostasis and inflammation. Br J Nutr 113:100–113
Singh D, Tanwar H, Jayashankar B, Sharma J, Murthy S, Chanda S et al (2017) Quercetin exhibits adjuvant activity by enhancing Th2 immune response in ovalbumin immunized mice. Biomed Pharmacother 90:354–360
Sliva D (2004) Cellular and physiological effects of Ganoderma lucidum (Reishi). Mini Rev Med Chem 4:873–879
Sreedhar R, Arumugam S, Thandavarayan RA, Karuppagounder V, Watanabe K (2016) Curcumin as a therapeutic agent in the chemoprevention of inflammatory bowel disease. Drug Discov Today 21:843–849
Stamets PE (2018) Antiviral activity from medicinal mushrooms and their active constituents. US Patent 9931316B2 Published 3 Apr 2018
Takano K, Nakaima K, Nitta M, Shibata F, Nakagawa H (2004) Inhibitory effect of (-)-epigallocatechin 3-gallate, a polyphenol of green tea, on neutrophil chemotaxis in vitro and in vivo. J Agric Food Chem 52:4571–4576
Triantafyllou A, Mylonis I, Simos G, Bonanou S, Tsakalof A (2008) Flavonoids induce HIF-1alpha but impair its nuclear accumulation and activity. Free Radic Biol Med 44:657–670
Trung LQ, An D (2018) Is resveratrol a cancer immunomodulatory molecule? Front Pharmacol 9:1255
Tuli HS, Tuorkey MJ, Thakral F, Sak K, Kumar M, Sharma AK, Sharma U, Jain A, Aggarwal V, Bishayee A (2019) Molecular mechanisms of action of genistein in cancer: recent advances. Front Pharmacol 10:1336
Upadhyaya J, Kesharwani RK, Misra K (2009a) Comparative study of antioxidants as cancer preventives through inhibition of HIF-1 alpha activity. Bioinformation 4(6):233
Upadhyaya J, Kesharwani RK, Misra K (2009b) Metabolism, pharmacokinetics and bioavailability of ascorbic acid; synergistic effect with tocopherols and curcumin. J Comput Intell Bioinform 2(1):77–84
Vela EM, Knostman KA, Mott JM, Warren RL, Garver JN, Vela LJ et al (2010) Genistein, a general kinase inhibitor, as a potential antiviral for arenaviral hemorrhagic fever as described in the Pirital virus-Syrian golden hamster model. Antivir Res 87:318–328
Vetchinkina E, Shirokov A, Bucharskaya A, Navolokin N, Prilepskii A, Burov A, Maslyakova G, Nikitina VE (2016) Antitumor activity of extracts from medicinal basidiomycetes mushrooms. Int J Med Mushrooms 18:955–964
Vyas D, Gupt S, Dixit V, Anita K, Kaur S (2015) To study the effect of curcumin on the growth properties of circulating endothelial progenitor cells. In vitro cellular & developmental biology. Animal 51:488–494
Wallace KL, Zheng LB, Kanazawa Y, Shih DQ (2014) Immunopathology of inflammatory bowel disease. World J Gastroenterol 20:6–21
Wallberg M, Cooke A (2013) Immune mechanisms in type 1 diabetes. Trends Immunol 34:583–591
Wang W, Yan C, Zhang J, Lin R, Lin Q, Yang L, Ren F, Zhang J, Ji M, Li Y (2013) SIRT1 inhibits TNF-α-induced apoptosis of vascular adventitial fibroblasts partly through the deacetylation of FoxO1. Apoptosis 18:689–701
Wang XS, Zhang ZR, Zhang MM, Sun MX, Wang WW, Xie CL (2017) Neuroprotective properties of curcumin in toxin-base animal models of Parkinson’s disease: a systematic experiment literatures review. BMC Complement Altern Med 17:412
Wilasrusmee C, Kittur S, Siddiqui J, Bruch D, Wilasrusmee S, Kittur DS (2002) In vitro immunomodulatory effects of ten commonly used herbs on murine lymphocytes. J Altern Complement Med 8:467–475
Williams AS, Richards PJ, Thomas E, Carty S, Nowell MA, Goodfellow RM, Dent CM, Williams BD, Jones SA, Topley N (2007) Interferon-gamma protects against the development of structural damage in experimental arthritis by regulating polymorphonuclear neutrophil influx into diseased joints. Arthritis Rheumatol 56:2244–2254
Wong C-H, Wu C-Y, Hsu H-Y, Liao S-F, Liang C-H (2016) Antibody-mediated anti-tumor activity induced by reishi mushroom polysaccharides. US Patent 2016/0166661 A1, Published 16 Jun 2016
Wu CH, Wu CF, Huang HW, Jao YC, Yen GC (2009a) Naturally occurring flavonoids attenuate high glucose-induced expression of proinflammatory cytokines in human monocytic THP-1 cells. Mol Nutr Food Res 53:984–995
Wu J, Chen L, Zhang D, Huo M, Zhang X, Pu D, Guan Y (2009b) Peroxisome proliferator-activated receptors and renal diseases. Front Biosci (Landmark edition) 14:995–1009
Xu T, Beelman RB, Lambert JD (2012) The cancer preventive effects of edible mushrooms. Anticancer Agents Med Chem 12:1255–1263
Xu S, Jiang B, Wang H, Shen C, Chen H, Zeng L (2017) Curcumin suppresses intestinal fibrosis by inhibition of PPARγ-mediated epithelial-mesenchymal transition. Evid Based Complement Alternat Med 2017:7876064
Xuzhu G, Komai-Koma M, Leung BP, Howe HS, McSharry C, McInnes IB, Xu D (2012) Resveratrol modulates murine collagen-induced arthritis by inhibiting Th17 and B-cell function. Ann Rheum Dis 71:129–135
Yang F, de Villiers WJ, McClain CJ, Varilek GW (1998) Green tea polyphenols block endotoxin-induced tumor necrosis factor-production and lethality in a murine model. J Nutr 128:2334–2340
Yang JX, Maria TC, Zhou B, Xiao FL, Wang M, Mao YJ (2020) Quercetin improves immune function in Arbor Acre broilers through activation of NF-κB signaling pathway. Poult Sci 99:906–913
Yao J, Wei C, Wang JY, Zhang R, Li YX, Wang LS (2015) Effect of resveratrol on Treg/Th17 signaling and ulcerative colitis treatment in mice. World J Gastroenterol 21:6572–6581
Yu W, Fu YC, Zhou XH, Chen CJ, Wang X, Lin RB, Wang W (2009) Effects of resveratrol on H2O2-induced apoptosis and expression of SIRTs in H9c2 cells. J Cell Biochem 107:741–747
Yu Z, Yang L, Deng S, Liang M (2020) Daidzein ameliorates LPS-induced hepatocyte injury by inhibiting inflammation and oxidative stress. Eur J Pharmacol 885:173399
Yuan J, Lu L, Zhang Z, Zhang S (2012) Dietary intake of resveratrol enhances the adaptive immunity of aged rats. Rejuvenation Res 15:507–515
Yulug E, Turedi S, Alver A, Turedi S, Kahraman C (2015) Effects of resveratrol on methotrexate-induced intestinal injury. Bratisl Med J 116:676–680
Zhang L, Xue H, Zhao G, Qiao C, Sun X, Pang C, Zhang D (2019a) Curcumin and resveratrol suppress dextran sulfate sodium-induced colitis in mice. Mol Med Rep 19:3053–3060
Zhang MY, Guo J, Hu XM, Zhao SQ, Li SL, Wang J (2019b) An in vivo anti-tumor effect of eckol from marine brown algae by improving the immune response. Food Funct 10:4361–4371
Zou T, Yang Y, Xia F, Huang A, Gao X, Fang D, Xiong S, Zhang J (2013) Resveratrol Inhibits CD4+ T cell activation by enhancing the expression and activity of Sirt1. PLoS One 8:e75139
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Nagaraja, S., Gawande, V., Joshi, A., Pund, S. (2022). Immunoregulatory Bioactive Phytoconstituents: Recent Trends and Future Challenges. In: Kesharwani, R.K., Keservani, R.K., Sharma, A.K. (eds) Nutraceuticals and Functional Foods in Immunomodulators. Springer, Singapore. https://doi.org/10.1007/978-981-19-2507-8_3
Download citation
DOI: https://doi.org/10.1007/978-981-19-2507-8_3
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-19-2506-1
Online ISBN: 978-981-19-2507-8
eBook Packages: Biomedical and Life SciencesBiomedical and Life Sciences (R0)