Abstract
Video-assisted thoracic surgery (VATS) for lobectomy or segmentectomy is considered as a good alternative to thoracotomy because of its usefulness and safety; reducing postoperative pain, lowering morbidity, and shortening hospital stay. However, despite these advantages of VATS, it has been difficult to perform VATS pneumonectomy due to the high morbidity and mortality rate of pneumonectomy. Recently, as VATS technique has been developed and usefulness of VATS pneumonectomy has been continuously reported, VATS pneumonectomy is gradually increasing in large volume centers. This article describes VATS pneumonectomy with a focus on the surgical technique.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
1 Introduction
Over the last two decades, the video-assisted thoracic surgery (VATS) technique has become the main treatment option for peripheral small lung nodules as well as major lung resection, including lobectomy. However, because complications observed after pneumonectomy were thought to be caused by the large amount of lung tissue resected rather than by the differences in the surgical method, VATS pneumonectomy was not actively performed compared to VATS lobectomy. This has contributed to our limited understanding of whether the advantages of VATS in lobectomy are also apparent in pneumonectomy. However, according to recent studies, VATS pneumonectomy is not inferior to open pneumonectomy in oncologic aspects and leads to superior results in postoperative pain and recovery [1]. In locally advanced lung cancer where pneumonectomy is the main treatment option, adjuvant therapy must be started as early as possible after operation; thus, postoperative pain management and rapid recovery are important [2]. For these reasons, VATS pneumonectomy has greater advantages over open pneumonectomy [3].
2 Indications for VATS Pneumonectomy
Similar to open pneumonectomy, the main indication for VATS pneumonectomy is locally advanced lung cancer that cannot be completely resected by lobectomy, bilobectomy, or sleeve lobectomy. Patients must be able to tolerate one-lung ventilation during the surgery and have sufficient lung function for their daily lives after pneumonectomy. VATS pneumonectomy should not be performed when complete resection is impossible, even with pneumonectomy or in patients with positive N3 nodes. Although there are no absolute criteria for the mass size, VATS must be carefully considered for large masses. In addition, VATS pneumonectomy should be carefully considered in patients who underwent preoperative chemotherapy or chemoradiation therapy and resection of the opposite lung.
3 Preoperative Evaluation
The preoperative evaluation for VATS pneumonectomy is similar to that for open pneumonectomy: a transthoracic echocardiogram and pulmonary function test. In patients with marginal functions whose condition cannot accurately be evaluated using these routine tests, a supplementary lung perfusion or cardiopulmonary exercise test must be conducted. For a more accurate assessment of the cardiopulmonary function, the pulmonary artery (PA) on the side to be resected may be ballooned during cardiac catheterization to analyze cardiac output, right ventricular function, and systemic arterial blood gas. And, cardiac function can be evaluated by clamping the main PA under the intraoperative transesophageal echocardiogram.
4 Anesthesia
VATS pneumonectomy is performed under general anesthesia using one-lung ventilation. General anesthesia is induced through inhalation or intravenous injection of anesthetic agents, after which the patient is intubated with a double lumen endotracheal tube. The double lumen endotracheal tube tip can be placed in either side of the main bronchus depending on the resection side; however, if the tip enters the main bronchus in the resection direction, the tip can also be resected during main bronchus resection. Therefore, the anesthesiologist must inform the surgeon about the direction of the tube tip prior to bronchus resection.
Intraoperative hypoxemia requires special considerations for VATS pneumonectomy. In open pneumonectomy, continuous positive airway pressure can be applied to the non-ventilated lung to improve hypoxia. However, during VATS pneumonectomy, the same procedure cannot be performed as it can limit the visual field and movement of the instruments. Therefore, hypoxemia during VATS pneumonectomy can be corrected by applying positive end expiatory pressure or conducting intermittent two-lung ventilation after discussing with the surgeon.
In order to minimize injury of the opposite (non-resected) lung after pneumonectomy, airway pressure must be maintained at a low level and the inhaled oxygen concentration must be minimized during the surgery. In addition, intravenous fluids must not be infused in large quantities [4].
5 Surgical Technique
5.1 General Concept
Right VATS pneumonectomy has a higher risk of postoperative respiratory failure and bronchopleural fistula (BPF) than left VATS pneumonectomy; however, right VATS pneumonectomy is technically easier than left side because the pulmonary vasculature and carina are well-exposed. As the extracted specimen is often larger in VATS pneumonectomy than in lobectomy, specimens may not be obtained using the usual VATS incision. In this case, it may be necessary to extend the incision for extraction.
During pneumonectomy, both inferior and superior pulmonary veins (PV) must be sufficiently isolated before the division of one of these veins. This can isolate and divide the main PA without delay after the division of the two PV. This technique reduces the time required to isolate and divide the PA, thereby preventing vascular congestion.
In completion pneumonectomy or cases of deep mass invasion toward the center, vessels may need to be divided inside the pericardium. In bronchus division, as in open pneumonectomy, dissection must be done until the carinal level to ensure that the bronchus stump is as short as possible.
5.2 Patient Positioning
The position of the patients is the same as in VATS lobectomy. The patients need to be in a full lateral decubitus position, and the operation bed is flexed. This widens the intercostal space (ICS) and improves access and control of thoracoscopic devices.
5.3 Incision
The number and location of incisions differ for each surgeon. Here, we will introduce a general three-port technique. First, a trocar is inserted to the eighth ICS posterior axillary line and the sixth ICS anterior axillary line, respectively. The thoracoscope and thoracoscopic devices are inserted through these trocars to observe the inside of the thoracic cavity. After confirming the location and invasion extent of the tumor to assess indications for VATS pneumonectomy, a 4-cm-long working window is created at the fifth ICS. If surgery is contraindicated due to pleural metastasis, the surgery needs to be terminated. If VATS cannot be performed, conversion to thoracotomy is necessary.
5.4 Division of Pulmonary Veins
There is a controversy over whether the PV or artery must be divided first. If the PV is divided first, pulmonary congestion may occur. On the other hand, if the PA is divided first, the cancer cells may metastasize through the bloodstream during surgery [5]. Technically, the division of the PV prior to that of the PA leads to an easier and safer exposure and division of the PA.
To divide the PV, the inferior pulmonary ligament must be dissected up to the bottom of the inferior PV (IPV). Once the IPV is exposed, vessel loops or umbilical tape can be used to encircle the IPV, which can then be divided using a stapler. When the IPV is divided, the lower boundary of the superior PV (SPV) is well-exposed (Fig. 6.1). As the SPV is in very close proximity with the anterior part of the PA, caution is required to avoid injury of the PA during encircling. The SPV can be divided using a stapler in the same way as the IPV.
5.5 Division of Pulmonary Artery
After lifting the lung upward and exposing the lower parts of the PA and bronchus, the space between the PA and bronchus can be dissected. The lung can be retracted downward to expose the subaortic area. After dissecting tissues around the upper part of the PA, the PA is encircled. After encircling the vessel loop or umbilical tape, enough space must be secured for the stapler to pass through (Fig. 6.2). If the tissues around the PA are not dissected properly, the staplers may cause vessel injuries. In rare cases, the stapler may distort the main PA or contralateral PA. Therefore, the PA should not be divided immediately after closure, and changes in hemodynamics must be observed for a sufficient time before PA division. If the mass is located too close to the origin of the PA, it may be difficult to place the stapler. In such cases, intrapericardial division can be considered and it is safe to proceed with conversion to thoracotomy.
5.6 Division of Bronchus
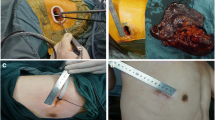
As described earlier, it is essential to keep the bronchus stump as short as possible. In the left lung, the bronchus in the subaortic area must be sufficiently dissected to leave a short bronchus stump. Dissection of the subcarinal node after bronchus division makes it technically challenging to expose the subcarinal area. Therefore, it is better to perform node dissection before bronchus division. During dissection of the subcarinal node, a clip or scissors are recommended over energy devices, which may cause devascularization. When bronchus is divided before PA division, the PA may rotate or be pulled, leading to injuries. Therefore, in general, PA division is conducted before bronchus division (Fig. 6.3). However, if the mass is located in front of the PA, limiting hilar dissection, bronchus division can be performed first. Excessive dissection of the tissue at the bronchus resection margin impairs blood circulation, which increases the risk of BPF. In VATS pneumonectomy, extraction of the lung specimen is challenging. Extracting the specimen through a narrow working window may damage the bag, which can cause the dissemination of cancer cells. In this case, the intercostal muscle must be divided sufficiently such that the specimen can be extracted safely to the subcutaneous space. Cancers that require VATS pneumonectomy may be located close to the bronchus resection margin. Thus, frozen sections of the bronchus margin need to be requested for examination by the pathologist. If cancer cells are present in the margin, additional resection of the bronchus stump may be necessary.
Because long bronchus stump can cause bronchopleural fistula, it is essential to keep the bronchus stump as short as possible. When bronchus is divided before pulmonary artery (PA) division, the PA may rotate or be pulled, leading to injuries. PA division is generally conducted before bronchus division. PV pulmonary vein
5.7 Coverage of Drainage after Bronchus Stump
Once the lung specimens are extracted, the thoracic cavity is irrigated with warm saline. Some surgeons may also mix antibiotics with the irrigation fluid. During irrigation, air leakage in the bronchus must be checked. If an air leakage is observed, the bronchus can be sutured or stapled again. Subsequently, some surgeons may cover the bronchus stump with surrounding tissues rich in blood vessels. Commonly used tissues are pericardial fat pads, pleura, and intercostal muscles. Since right pneumonectomy and neoadjuvant treatment induce a high risk of BFF, it is safer to cover the stump.
5.8 Drainage After VATS Pneumonectomy
Although drainage after pneumonectomy can be done in various ways, the necessity of drainage is also debated. In general, a chest tube connected to a three-bottle system is commonly used. Inserting drains can help control mediastinum positioning immediately after surgery, and it is useful to identify the characteristics of the drained content, such as blood and chyle. The chest tube is not maintained for a long time unless complications are observed in the immediate postoperative period.
6 Postoperative Management
6.1 Pleural Space After Pneumonectomy
After VATS pneumonectomy, fluids accumulate in the empty thoracic cavity. On chest radiographs, approximately 70% of the thoracic cavity is commonly filled with fluid on the third postoperative day, and 2–3 months are required for the thoracic cavity to be completely filled with fluid [6]. Rapid postoperative fluid accumulation indicates possible bleeding and chylothorax. If the mediastinum is severely deviated to the opposite side of the operation, the subcutaneous emphysema is suddenly aggravated or fluid does not fill above the carinal level, BPF should be suspected.
6.2 Fluid Management
An excessive fluid supply during or after surgery increases the possibility of pulmonary edema in the remaining lung, which is associated with postoperative mortality. As described above, severe fluid restriction is also dangerous as the thoracic cavity is filled with fluid within a short period of time. The urine output and renal function must be closely monitored to supply appropriate amounts of fluid.
7 Conclusion
VATS pneumonectomy is often conducted for patients with locally advanced lung cancer with central lesions. The surgical technique is complex, and the risk of postoperative complications limits the use of VATS pneumonectomy compared to VATS lobectomy. However, the gradual development of the VATS technique and experience would help to replace open pneumonectomy for the treatment of lung cancer in the near future.
References
Nwogu CE, Yendamuri S, Demmy TL. Does thoracoscopic pneumonectomy for lung cancer affect survival? Ann Thorac Surg. 2010;89:S2102–6.
Petersen RP, Pham D, Burfeind WR, et al. Thoracoscopic lobectomy facilitates the delivery of chemotherapy after resection for lung cancer. Ann Thorac Surg. 2007;83:1245–50.
Yang CJ, Yendamuri S, Mayne NR, et al. The role of thoracoscopic pneumonectomy in the management of non-small cell lung cancer: a multicenter study. J Thorac Cardiovasc Surg. 2019;158:252–64.
Hackett S, Jones R, Kapila R. Anaesthesia for pneumonectomy. BJA Educ. 2019;19:297–304.
Song PP, Zhang W, Zhang B, Liu Q, Du J. Effects of different sequences of pulmonary artery and vein ligations during pulmonary lobectomy on blood micrometastasis of non-small cell lung cancer. Oncol Lett. 2013;5:463–8.
Munden RF, O'Sullivan PJ, Liu P, Vaporciyan AA. Radiographic evaluation of the pleural fluid accumulation rate after pneumonectomy. Clin Imaging. 2015;39:247–50.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Ethics declarations
None.
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Haam, S. (2022). Video-Assisted Thoracic Surgery for Pneumonectomy. In: Kim, K., Haam, S., Kim, H.K. (eds) Techniques in Minimally Invasive Thoracic Surgery. Springer, Singapore. https://doi.org/10.1007/978-981-19-2472-9_6
Download citation
DOI: https://doi.org/10.1007/978-981-19-2472-9_6
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-19-2471-2
Online ISBN: 978-981-19-2472-9
eBook Packages: MedicineMedicine (R0)