Abstract
Hypoglycemia in neonates has been reported for a long time [1], and subsequently, the association between neonatal hypoglycemia and neurological sequelae has been reported successively.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
-
In recent years, the association and prognosis of neonatal hypoglycemia and neurological sequelae have been reported successively.
-
The risk factors for neonatal hypoglycemia include maternal diabetes mellitus, late preterm, SGA, and LGA infants, and neonatal hypoglycemia is thought to be particularly likely to damage the cerebral white matter.
-
Regarding the relationship between neonatal hypoglycemia and neurological sequelae, it has been reported that neurodevelopmental and literacy deficits occur in mid-childhood, and the possibility of very long-term neurodevelopmental complications must be considered.
-
The interventional glucose threshold is controversial. Currently, blood glucose should be kept at least 47 mg/dL (2.6 mmol/L).
Hypoglycemia in neonates has been reported for a long time [1], and subsequently, the association between neonatal hypoglycemia and neurological sequelae has been reported successively.
In this section, we define neonatal hypoglycemia and discuss about its relation to neurological disorders leading to cerebral palsy (CP).
1 What Is Neonatal Hypoglycemia?
Although specific uniform standards for neonatal hypoglycemia have not been established, European and American societies [American Academy of Pediatrics (AAP), Pediatric Endocrine Society (PES)] have issued guidelines for the management of blood glucose over time using limited observational data (Table 1) [2, 3].
In 1988, Lucas et al. conducted a multicenter study of 661 preterm infants, defining neonatal hypoglycemia as less than 47 mg/dL (2.6 mmol/L), and discussed the neurological prognosis with 47 mg/dL as the boundary [4]. This will be discussed later.
2 Risk Factors for Neonatal Hypoglycemia
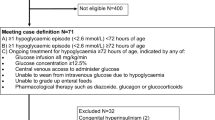
Risk factors for neonatal hypoglycemia include maternal diabetes mellitus, late preterm infants, small-for-gestational-age (SGA) infants, and large-for-gestational-age (LGA) infants. All of these factors are risk factors that should be considered for postnatal hypoglycemia, and more severe hypoglycemia should be considered when multiple factors are present (Fig. 1) [5].
In addition, the use of ritodrine hydrochloride has been cited as a risk of neonatal hypoglycemia in the perinatal period that has recently been reported from Japan, and the possibility of neonatal hypoglycemia must be kept in mind, especially with the long-term use of ritodrine hydrochloride and its discontinuation immediately before delivery [6].
3 The Mechanism of Neonatal Hypoglycemia Causing Neurological Disorders
There are several theories on the mechanism by which neonatal hypoglycemia causes neurological disorders. It has been reported that under hypoglycemic conditions, excitatory neurotoxin is excessively secreted, stimulating N-methyl-D-aspartate (NMDA)-type glutamate receptors and producing free radicals, which induce neuronal apoptosis and alter brain energy metabolism [7, 8]. It is also reported to alter the energy metabolism of the brain [7, 8].
In addition, Charlotte et al. [9] reported that the MRI of 35 children with neonatal hypoglycemia showed white matter lesions in 94% of the children as a region susceptible to damage by neonatal hypoglycemia. In addition, 51% of the children had cortical lesions and 40% had basal ganglia and thalamus lesions (Table 2) [7].
Thus, the reason for the high incidence of white matter lesions in neonatal hypoglycemia has been reported in animal models, in which a significant decrease in cerebral blood flow was observed in the white matter due to an unbalanced redistribution of cerebral blood flow in hypoglycemic conditions [10]. This vulnerability in the white matter region of the brain is thought to be one of the reasons why neonates are more susceptible to damage during hypoglycemia.
4 The Association Between Neonatal Hypoglycemia and Cerebral Palsy
The relationship between neonatal hypoglycemia and neurological sequelae has been reported since the 1960s [11], and in 1988, Lucas et al. investigated neonatal hypoglycemia of less than 47 mg/dL (2.6 mmol/L) and the number of days of onset in 661 preterm infants (weight less than 1850 g). The longer the number of days of hypoglycemia, the worse the neurological prognosis at 18 months of correction [4].
In 1999, hypoglycemia of less than 47 mg/dL (2.6 mmol/L) occurred in 72.9% of 85 SGA children, and children with two or more episodes of hypoglycemia had significantly lower psychomotor development at 3.5 and 5 years of age than those with a single episode of hypoglycemia [12].
In a 2019 systematic review meta-analysis, neonatal hypoglycemia did not worsen neurodevelopmental outcomes in early childhood [n = 1657, odds ratio (OR) 1.16 [95% confidence interval (95% CI): 0.86–1.57]], but it did cause visuomotor dysfunction [n = 508, OR 3.46 (95% CI: 1.13–10.57)], visuomotor impairment [n = 508, OR 3.46 (95% CI: 1.13–10.57)], and executive function impairment [n = 463, OR 2.50 (95% CI: 1.20–5.22)]. In mid-childhood, neurodevelopmental deficits [n = 54, OR 3.62 (95% CI: 1.05–12.42)] and literacy deficits [n = 1395, OR 2.04 (95% CI: 1.20–3.47)] were observed. However, developmental assessment in adolescence has not yet been performed [13]. Based on these results, the possibility that neonatal hypoglycemia may lead to very long-term neurodevelopmental complications must be considered.
With regard to the hypoglycemic threshold for neurological impairment, a neurological outcomes cohort study was reported in 2015 in The New England Journal of Medicine (NEJM), in which blood glucose was kept at 47 mg/dL (2.6 mmol/L). A total of 404 hypoglycemic risk children [born <37 weeks, low birth weight (<10th percentile or <2500 g), high birth weight (>90th percentile or >4500 g)] were intermittently followed for blood glucose until 7 days after birth. Of these, 216 (53%) had hypoglycemia and were treated with additional feeding, dextrose gel, and intravenous fluids to maintain blood glucose levels above 47 mg/dL. At 2 years of age, developmental assessment by the Bayley scales of infant development III (BSID III) showed no significant difference compared with the control group without hypoglycemia. As a result, developmental evaluation of the Bayley scales of infant development III (BSID III) at 2 years of age showed no significant difference compared with the control group without hypoglycemia [14].
On the other hand, a paper on the therapeutic threshold for neonatal hypoglycemia was reported in the NEJM in 2020. According to the paper, the developmental assessment of BSID III at 18 months modified proved non-inferiority when the treatment threshold was 36 mg/dL (2.0 mmol/L), which is lower than the conventional treatment threshold of 47 mg/dL (2.6 mmol/L). In other words, a treatment threshold of 36 mg/dL (2.0 mmol/L) did not result in a worse developmental outcome than the conventional threshold of 47 mg/dL (2.6 mmol/L) [15]. A comparison of developmental outcomes over a longer period of time will be necessary in the future.
Neonatal hypoglycemia is frequent in infants at risk for maternal ritodrine hydrochloride use, preterm birth, maternal diabetes, SGA, and LGA. Studies have shown that neonatal hypoglycemia can cause cerebral cell damage, particularly in the cerebral white matter, and may pose a risk of long-term neurodevelopmental impairment. Although there are various theories on the interventional blood glucose threshold, at this stage, it should be managed so that the blood glucose level does not fall below 47 mg/dL (2.6 mmol/L) as shown in Table 1 over time and as a constant value.
References
Brown RJ, Wallis PG. Hypoglycaemia in the newborn infant. Lancet. 1963;1:1278–82.
Adamkin DH. Postnatal glucose homeostasis in late-preterm and term infants. Pediatrics. 2011;127:575–9.
UpToDate®: management and outcome of neonatal hypoglycemia.
Lucas A, Morley R, Cole TJ. Adverse neurodevelopmental outcome of moderate neonatal hypoglycaemia. BMJ. 1988;297:1304–8.
Stark J, Simma B, Blassnig-Ezeh A. Incidence of hypoglycemia in newborn infants identified as at risk. J Matern Fetal Neonatal Med. 2020;33(18):3091–6.
Yada Y, Ohkuchi A, Otsuki K, et al. Synergic interaction between ritodrine and magnesium sulfate on the occurrence of critical neonatal hyperkalemia: a Japanese nationwide retrospective cohort study. Sci Rep. 2020;10:7804.
Papagapiou MP, Auer RN. Regional neuroprotective effects of the NMDA receptor antagonist MK-801 (dizocilpine) in hypoglycemic brain damage. J Cereb Blood Flow Metab. 1990;10:270–6.
Wieloch T. Hypoglycemia-induced neuronal damage prevented by an N-methyl-D-aspartate antagonist. Science. 1985;230:681–3.
Burns CM, Rutherford MA, Boardman JP, et al. Patterns of cerebral injury and neurodevelopmental outcomes after symptomatic neonatal hypoglycemia. Pediatrics. 2008;122:65–74.
Mujsce DJ, Christensen MA, Vannucci RC. Regional cerebral blood flow and glucose utilization during hypoglycemia in newborn dogs. Am J Physiol. 1989;256(6 Pt 2):H1659–66.
Cornblath M, Reisner SH. Blood glucose in the neonate and its clinical significance. N Engl J Med. 1965;273:378–81.
Duvanel CB, Fawer CL, Cotting J, et al. Long-term effects of neonatal hypoglycemia on brain growth and psychomotor development in small-for gestational-age preterm infants. J Pediatr. 1999;134:492–8.
Shah R, Harding J, Brown J, et al. Neonatal glycaemia and neurodevelopmental outcomes: a systematic review and meta-analysis. Neonatology. 2019;115:116–26.
McKinlay CJ, Alsweiler JM, Ansell JM, et al. Neonatal Glycemia and neurodevelopmental outcomes at 2 years. N Engl J Med. 2015;373:1507–18.
van Kempen A, Eskes PF, Nuytemans D, et al. Lower versus traditional treatment threshold for neonatal hypoglycemia. N Engl J Med. 2020;382:534–44.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Mukai, T., Takahashi, N. (2022). Neonatal Hypoglycemia. In: Matsuda, Y. (eds) Cerebral Palsy. Springer, Singapore. https://doi.org/10.1007/978-981-19-2217-6_30
Download citation
DOI: https://doi.org/10.1007/978-981-19-2217-6_30
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-19-2216-9
Online ISBN: 978-981-19-2217-6
eBook Packages: MedicineMedicine (R0)