Abstract
Appropriate haemodynamic monitoring and management is necessary for neurological patients. Various modalities of haemodynamic monitoring, both invasive and non-invasive, are available. Each of these devices has their advantages and shortcomings. In this chapter, we give a brief overview of the many haemodynamic monitoring devices available for use in neurological patients.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
Introduction
Patients with neurological insults suffer from significant alterations in haemodynamic parameters. Many patients with acute ischaemic stroke, aneurysmal subarachnoid haemorrhage, traumatic brain injury, etc. have increased intracranial pressure and present with sudden hypertension and bradycardia. Fluid and electrolyte imbalance is also very common in neurological patients as a direct result of neurological injury, due to altered consciousness, effect of diuretics and various other causes. Appropriate haemodynamic monitoring and maintaining haemodynamic parameters within recommended levels is essential for better clinical outcome in neurosurgical patients, both during intraoperative period and during ICU stay [1, 2].
There are various modalities of haemodynamic monitoring and are usually classified as invasive or non-invasive. The most common invasive and non-invasive haemodynamic monitors are enumerated in Table 1. In this chapter, we begin by describing the various haemodynamic monitors and follow it by a discussion on the merits and demerits of various haemodynamic monitors.
Invasive Haemodynamic Monitors
-
1.
Arterial cannulation—Invasive arterial blood pressure monitoring allows beat to beat of blood pressure monitoring and regulation in addition to providing access for arterial blood gas analysis. Common arteries that are cannulated include radial, dorsalis pedis, brachial, femoral, etc. A modified Allen’s test is usually performed prior to cannulation of radial artery to rule out inadequate collateral circulation. Before cannulation of the artery, the pressure–tubing–transducer system should be nearby and already flushed with saline. The pressure transducer measures blood pressure on the basis of Wheatstone bridge principle. The transducer is usually calibrated to atmospheric pressure level prior to initiation of pressure monitoring. Many devices analyse the arterial waveform to estimate cardiac output and other haemodynamic parameters. Complications of arterial cannulation include arterial thrombosis, hematoma, nerve damage, necrosis of digits, etc.
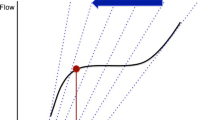
The fast flush test is used to calculate the damping coefficient and the natural frequency of the invasive blood pressure monitoring system as depicted in Fig. 1. A square wave is generated when the fast flush valve is squeezed. After the fast flush has finished, the whole transducer system returns to baseline. It does this as a harmonic oscillator, ‘bouncing’ a few times before actually coming to rest (Fig. 1c). This ‘bounce’ effect is used to find out the resonance characteristics of the system. At least, there should be one ‘bounce’ oscillation. If the system fails to oscillate, there is too much damping (Fig. 1a). Also, there shouldn’t be greater than two oscillations; a system which oscillates too much is underdamped (Fig. 1b).
-
2.
Arterial waveform-based devices—Classified as those requiring calibration and those not requiring calibration. The former include PiCCO and LiDCO, while the latter includes FloTrac.
PiCCO (Fig. 2)
It stands for pulse index continuous cardiac output. The calculation of cardiac output using PiCCO requires insertion of central venous line and an arterial line. The arterial catheter of PiCCO has a thermistor 5 mm from its tip; in addition the device consists of an injection device which is connected to the distal tip of a central venous catheter. The artery cannulated most commonly is femoral artery, while radial, brachial and axillary arteries are also used infrequently. The measured and derived values are demonstrated on a monitor.
After connecting the monitor to venous and arterial lines, calibration is started. Calibration consists of three injections of 15–30 ml of cold normal saline in an interval of 5 min; the procedure needs to be repeated every 8 h. Studies have demonstrated that PiCCO has accuracy comparable to that of PAC [3]. An advantage of PiCCO over LiDCO is that PiCCO also provides information about intrathoracic blood volume index, an important measure of fluid responsiveness. Also, complications associated with the use of PiCCO have been rare [4].
LiDCO
The device was developed by LiDCO plus (LiDCO, Cambridge, UK). An arterial and a central/peripheral access is necessary for the operation of device. It uses lithium dilution to calibrate a pulse pressure analysis algorithm. The LiDCO system consists of a disposable lithium sensitive sensor which is connected to an existing arterial cannula. A connector sends a signal from the sensor to a monitor. A small dose of lithium chloride (20–40 micromol/kg) is injected as an intravenous bolus, and cardiac output is derived from the dilution curve. In addition to the changes in cardiac output, the device also tells about pulse pressure variation (PPV) and stroke volume variation (SVV). LiDCO requires calibration every 8 h.
Patients with aortic valve pathologies, patients on lithium therapy and patients on intra-aortic balloon pump may not demonstrate accurate values when using LiDCO. There is evidence of successful application of LiDCO in paediatric patients [5].
FloTrac (Fig. 3)
FloTrac was introduced by Edwards Lifesciences in 2005. It does not require calibration. The FloTrac sensor is connected to an arterial line, and the FloTrac monitor displays cardiac output, stroke volume, stroke volume variation and systemic vascular resistance. It is an easy-to-use device but the accuracy of measurement gets affected in patients with arrhythmias, in patients with aortic valve disease and in haemodynamically unstable patients. While some studies have demonstrated accuracy of FloTrac comparable to that of PAC, others have highlighted its shortcomings in selected patient populations [6,7,8].
VolumeView
The VolumeView system was introduced by Edwards Lifesciences in 2010. The system consists of a thermistor-tipped arterial cannula, a monitor interface and a PreSep oximetry central line catheter. The various parameters displayed on the monitor include cardiac output, stroke volume, stroke volume variation, systemic vascular resistance, global end-diastolic volume, intrathoracic blood volume, pulmonary vascular permeability index and extravascular lung volume. Nakwan et al compared VolumeView and echocardiography in estimating global ejection fraction in septic patients and found that VolumeView provided a reliable estimate of ejection fraction in septic shock patients [9].
-
3.
Central venous monitoring—A central venous access in a neurological patient allows measurement of central venous pressure (CVP), fluid administration and administration of high osmolarity drugs.
Coagulopathy, infection at insertion site, right heart vegetations or tumours are contraindications to central line insertion. Subclavian and internal jugular veins are the most common sites of central venous cannulation. The line insertion can be landmark guided or ultrasound guided. Complications of central line insertion include pneumothorax, accidental arterial puncture, pleural effusion, arrhythmias, bloodstream infection, etc.
-
4.
Pulmonary artery catheter (PAC) (Fig. 4)—It is a four-lumen catheter and has a thermodilution sensor. PAC is around 110 cm long and 4–8 Fr in calibre. PAC allows determination of central venous pressure (CVP), right atrial pressure, right ventricular pressure and pulmonary artery pressure and allows calculation of cardiac output.
The four lumens are as follows:
-
(a)
First, to inflate the catheter tip with air.
-
(b)
Second, an accessory infusion port which ends 30 cm from the catheter tip.
-
(c)
Third, the distal port which ends at the catheter tip and is used to measure pressures during catheter insertion.
-
(d)
Fourth, the proximal port which ends 60 cm from the catheter tip. It measures right atrial pressures once the catheter tip is in the pulmonary artery.
Arterial waveform and the fast flush testing. (a) The square loop test. An overdamped waveform will have only one oscillation after the square wave, and the dicrotic notch will disappear. (b) Underdamped lines will have multiple oscillations after the square wave, and multiple notches can be seen in the waveform. (c) A properly damped arterial line will have two to three oscillations immediately after the square wave disappears. The tracing will then return to a normal arterial waveform. A distinct dicrotic notch should be present
Also, there is a thermistor which is used to measure cardiac output using thermodilution.
Coagulopathy, right heart endocarditis/ tumours and left bundle branch block are contraindications to PAC insertion.
The method of PAC insertion consists of acquiring central venous access using Seldinger technique. The distal port is connected to a transducer that is zeroed to the patient’s midaxillary line. The guide-wire is inserted after vein puncture and PAC sheath is threaded over the guide-wire. The PAC is then inserted and advanced until a central venous waveform appears at a length of around 15 cm. The tip balloon is then inflated and the PAC is then advanced while observing the pressure waveform and values. Pulmonary artery is usually entered at a length of around 35–45 cm. A chest x-ray can be used to later demonstrate the correct positioning of the PAC.
Complications of PAC insertion include pneumothorax, arterial puncture, air embolism, arrhythmias, infection, etc.
Calculating Cardiac Output (CO) from PAC
Calculating CO from PAC utilizes the principle of thermodilution. 2.5–10 ml of cold fluid is injected into the right atrium and the change in temperature of blood at PAC tip is sensed by the thermistor. Plotting the temperature with time on x axis provides the thermodilution curve and area under the curve is equal to cardiac output.
Trans-oesophageal Echocardiography (TEE)
Trans-oesophageal echocardiography provides real-time activity of the heart. Cardiac output can be calculated TEE by measuring cross-sectional area of the left ventricular outflow tract and multiplying it with the velocity time integral (VTI). In addition, TEE can tell about valvular abnormalities and guide regarding volume status, ejection fraction and various other parameters. However, TEE requires administration of sedation/anaesthesia. Also there is a risk of complications associated with insertion of probe into the oesophagus. Also, manipulating the probe is difficult intraoperatively during neurosurgery as the access to the mouth is lost after the patient is draped and surgery begins. TEE has been used to detect intraoperative venous air embolism during sitting craniotomies, to detect patent foramen ovale and to guide ventriculo-atrial shunt insertion, but use of TEE as a haemodynamic monitoring device has not been investigated [10, 11]. During mechanical ventilation, TEE could not perform as good as PAC for CO determination [12].
The NICO System
The NICO system is based on the partial CO2 rebreathing technique; i.e. it uses exhaled carbon dioxide as an indicator and applies Fick’s principle. The cardiac output measurement is fulfilled by data interpretation that is collected by the proprietary sensors that measure airway pressure, flow and concentration of CO2, and then combining these signals to calculate CO2 elimination. The NICO system can be applied only in mechanically ventilated patients who are sedated and paralysed.
The NICO system showed good concordance with PAC when used in critically ill patients [13]. Carretero et al. compared calculation of cardiac output using the NICO system with pulmonary artery catheter during cardiopulmonary resuscitation and found a high degree of agreement between the two techniques [14].
PRAM (Pressure Recording Analytical Method)
This system uses just an arterial line to provide information about CO, SVV, PPV and SVR. PRAM technology is based on the principle that, in any given vessel, volume changes occur mainly because of radial expansion in response to pressure variations [15].
PRAM is a non-calibrated pulse contour method. When compared with Doppler echocardiography for estimation of cardiac output in trauma patients, the two methods showed good agreement [16]. PRAM has also been found useful in estimating cardiac output in sepsis patients [17]. In paediatric patients aged 1 month–18 years, PRAM provided reliable estimates of cardiac output when compared with Doppler echocardiography [18]. However, in critically ill children, there was an unacceptably poor agreement between transpulmonary ultrasound dilution and PRAM [19].
Non-invasive Haemodynamic Monitors
There are multiple methods that have been devised for the measurement of blood pressure and cardiac output minimally invasively or non-invasively. The oldest method of haemodynamic monitoring is the non-invasive oscillometric method that utilizes an air-filled pressure cuff. But because of inaccuracy and variability of measurements, these devices are not dependable in acute conditions and don’t provide any reliable information about the cardiac function. It consists of a cuff which is air-filled that can inflate on the subject and measure the blood pressure either manually by the operator or automatically by the device itself. When the blood pressure is measured manually, it can be achieved using the palpation auscultation technique. In the palpation technique, the operator palpates the radial artery when the measurement is being carried out in the arm and deflates the cuff. The pressure where the pulses are felt is the systolic pressure. The primary advantage of this method is being quick and does not require any sophisticated instrument, but the disadvantage is that it does not measure the diastolic blood pressure. When the auscultation technique is used, the cuff pressure is increased beyond the systolic blood pressure that has already been measured using the palpation technique, following which a stethoscope is placed on the concerned artery and the Korotkoff sounds are auscultated. The first sound corresponds to the systolic blood pressure, while the few last muffled sounds correspond to the diastolic blood pressure. This technique requires the operator to be well trained. The automated system using a applies the same technique, and inflates the cuff to an already set pressure and then decreases the pressure slowly. The oscillations and sounds are then detected by the machine which corresponds to systolic and diastolic blood pressures. Mean arterial pressure corresponds to the maximum oscillations. The algorithms that these machines use are proprietary and dependent on their corresponding manufacturers.
Finger Cuffs for Continuous BP Monitoring
Many companies have introduced finger cuffs which allow continuous BP monitoring and also provide information about other haemodynamic parameters like CO, SVR, SVV, SV, etc. These can be attached to middle phalanx of the finger for a period up to 8 h, after which the finger should be changed. These devices are based on volume clamp method. The cuffs provide similar pressures on either side of the arterial wall by clamping the artery to a fixed volume. There is some evidence of these devices providing feasible estimates of BP in ICU patients, although some studies have shown these devices to be inferior to invasive BP monitoring as well [20, 21].
Special sized finger cuffs have been designed for paediatric patients and their accuracy checked with invasive blood pressure monitoring to find that these finger cuffs work well in paediatric patients as well [22]. When employed in preterm neonates, it was suggested that while finger cuffs were of limited value in estimating absolute blood pressure, the cuffs are useful in identification of beat-to-beat changes in systolic BP [23]. Another study found finger cuffs to be reliable for measurement of blood pressure in preterm infants [24].
These devices have been used intraoperatively also. When used in patients undergoing Caesarean section under subarachnoid block, the device was found to detect hypotensive episodes which the non-invasive blood pressure monitoring would have missed [25].
The ccNexfin System
Introduced by Edwards Lifesciences in 2007, it has a new version called the ClearSight system. The system consists of finger cuffs which wrap around the middle phalanx and measure blood pressure non-invasively using the volume clamp method. From the finger pressure waveform (received from the finger cuffs), the device reconstructs the brachial pressure waveform, and then cardiac output is estimated using the pulse contour method. The various haemodynamic parameters achieved using the ccNexfin system include blood pressure, stroke volume, cardiac output, stroke volume variation and systemic vascular resistance.
The ccNexfin system showed good correlation with pulmonary artery catheter in studies [26, 27].
Use of ClearSight system during heart valve interventions and cardiovascular surgery has been found to be useful, is simple and saves time [28, 29]. The use of ClearSight system for haemodynamic management during kidney transplantation has been reported [30].
Thoracic Electrical Bioimpedance (TEB)
TEB is a non-invasive alternative to monitoring of haemodynamic parameters including cardiac output, stroke volume and cardiac index. A low amplitude electrical signal is sent across the thorax. There are electrodes placed on the thorax which measure the impedance. Stroke volume is calculated on the basis of impedance change generated by the pulsatile flow and the time intervals between the changes. Surgical cautery, arrhythmias and fluid in thoracic cavity affect the accuracy of the device.
There is paucity of literature on accuracy of TEB in specific group of patients [31]. Elwan et al. found huge differences in cardiac output measured using Doppler and TEB in emergency care [32]. In normal adults, cardiac output measured using Doppler and TEB was found to be comparable [33]. A significant correlation between echocardiography and transthoracic electrical bioimpedance in the systemic haemodynamic assessment in patients with cirrhosis was observed [34]. Sabharwal et al. used TEB to determine haemodynamic changes after administration of mannitol in neurosurgical patients [35]. In aneurysmal subarachnoid haemorrhage patients undergoing surgery, non-invasive electrical velocimetry (EV) device based on the thoracic bioimpedance was compared with transpulmonary thermodilution to guide fluid therapy. The authors found that the cardiac index calculation using the two methods yielded different values in these patients [36].
Electrical Bioreactance Cardiography
Available with the name of NICOM system, the electrical bioreactance is a safe, non-invasive and continuous monitor. The basic principle is determination of change in frequency of electrical resistivity across the thorax. The system consists of four paired electrodes which are placed on the chest. One of the two paired electrodes injects an AC current of 75 kHz, while the other electrode detects the electrical signal. On the basis of analysis of the current injected and detected, along with analysis of time delay between the two signals, the NICOM system determines phase shift, and stroke volume is determined from the phase shift signals. Clinical and preclinical data demonstrates the feasibility of using blood flow-related phase shifts of transthoracic electrical signals to perform non-invasive continuous CO monitoring. NICOM is said to get affected by electrical cautery signals and the accuracy gets affected at low flows [37]. In colorectal surgery patients, oesophageal Doppler-guided GDFT was found to be comparable to NICOM-guided GDFT [38]. NICOM system was found to have an acceptable accuracy with thermodilution in ICU patients in a multicentre study [39].
Goal-Directed Haemodynamic Management in Neurosurgery and the Neuro-ICU
Concept of Fluid Responsiveness
The estimation of intravascular volume status in neurological patients remains difficult. The traditional methods of volume estimation and fluid administration like central venous pressure and Holliday-Segar formula have been proven to be insensitive [40]. This gave way to the concept of ‘fluid responsiveness’.
Fluid responsiveness is defined as an increase of stroke volume of 10–15% after the patient receives a ‘fluid challenge’ of 500 ml of crystalloid over 10–15 min. Fluid responsive patients have ‘preload reserve’ and will have an increase in stroke volume (and usually cardiac output) when fluid is administered. The presumption is that increased cardiac output will cause increased oxygen delivery (DO2) and increased tissue oxygenation.
Goal-Directed Haemodynamic Management (GDHM)
GDHM utilizes cardiac output (CO) monitoring techniques to guide clinicians for administering fluids, vasopressors and inotropes, both intraoperatively and in critical care settings. The aim of GDHM is to optimize tissue perfusion. The concept was initially suggested by Shoemaker et al. who reported a trend of decreased mortality following high-risk surgery when goal-directed haemodynamic management was used [41]. Various modalities have been described to guide GDFT including use of pulmonary artery catheter (PAC), trans-oesophageal echocardiography (TEE), arterial pulse waveform analysis, photoplethysmography, venous oxygen saturation and tissue oxygen saturation. Luo et al. showed that intraoperative GDHM strategy in high-risk patients undergoing brain surgery resulted in a shorter ICU length of stay and reduced costs, and also the postoperative morbidity was reduced [42].
The importance of optimization of intravascular volume in neurological patients cannot be overemphasized. Both hypovolaemia and hypervolaemia have been found to be associated with poor outcomes in neurological patients [43, 44]. However, determination of volume status in these patients remains difficult. Hence, using dynamic tests for determination of fluid responsiveness and administering fluids till patients are fluid responsive can help optimize volume status in these patients. Some indicators of fluid responsiveness include:
-
(a)
A pulse pressure variation of more than 12%
-
(b)
Inferior vena cava (IVC) diameter <2 cm and respiratory variation in IVC diameter of >50%
-
(c)
A systolic pulse variation of more than 10%
-
(d)
A systolic volume variation of more than 10%
-
(e)
A left ventricle outflow tract—velocity time integral of >12%
Various authors have demonstrated the effectiveness of GDHT in neurosurgery. Wu et al. compared two fluid protocols based on different stroke volume variation (SVV) cut-offs for goal-directed fluid therapy (GDFT) during supratentorial brain tumour resection and found that during GDFT for supratentorial brain tumour resection, fluid boluses targeting a lower SVV are more beneficial than a restrictive protocol [45].
Hasanin et al. compared pulse pressure variation-guided fluid therapy during supratentorial brain tumour excision with standard intraoperative fluid therapy and demonstrated that GDFT therapy leads to increased intraoperative fluid administration and improved peripheral perfusion without increasing brain swelling [46].
Presently, the evidence demonstrating improved outcomes in patients undergoing non-cardiac surgery who are administered GDFT is thin [47]. Similarly, improved outcome in neurosurgical patients due to GDFT is yet to be proven. Further studies will be necessary to determine if the use of GDFT actually improves the outcome in these patients.
References
Rasmussen M, Espelund US, Juul N, Yoo AJ, Sørensen LH, Sørensen KE, et al. The influence of blood pressure management on neurological outcome in endovascular therapy for acute ischaemic stroke. Br J Anaesth. 2018;120(6):1287–94.
Lazaridis C. Advanced hemodynamic monitoring: principles and practice in neurocritical care. Neurocrit Care. 2012;16(1):163–9.
Chakravarthy M, Patil TA, Jayaprakash K, Kalligudd P, Prabhakumar D, Jawali V. Comparison of simultaneous estimation of cardiac output by four techniques in patients undergoing off-pump coronary artery bypass surgery – a prospective observational study. Ann Card Anaesth. 2007;10:121–6.
Belda FJ, Aguilar G, Teboul JL, Pestaña D, Redondo FJ, Malbrain M, et al. Complications related to less invasive hemodynamic monitoring. Br J Anaesth. 2011;106:482–6.
Linton RA, Jonas MM, Tibby SM, Murdoch IA, O’Brien TK, Linton NWF, et al. Cardiac output measured by lithium dilution and transpulmonary thermodilution in patients in a paediatric intensive care unit. Intensive Care Med. 2000;26:1507–11.
De Backer D, Ospina-Tascon G, Salgado D, Favory R, Creteur J, Vincent JL. Monitoring the microcirculation in the critically ill patient: current methods and future approaches. Intensive Care Med. 2010;36(11):1813–25.
Mayer J, Boldt J, Poland R, Peterson A, Manecke GR. Continuous arterial pressure waveform-based cardiac output using the FloTrac/Vigileo: a review and meta-analysis. J Cardiothorac Vasc Anesth. 2009;23(3):401–6.
Marqué S, Gros A, Chimot L, Gacouin A, Lavoué S, Camus C, et al. Cardiac output monitoring in septic shock: evaluation of the third-generation Flotrac-Vigileo. J Clin Monit Comput. 2013;27(3):273–9.
Nakwan N, Chichareon P, Khwannimit B. A comparison of ventricular systolic function indices provided by VolumeView/EV1000™ and left ventricular ejection fraction by echocardiography among septic shock patients. J Clin Monit Comput. 2019;33(2):233–9.
Isaacs AM, Krahn D, Walker AM, Hurdle H, Hamilton MG. Transesophageal echocardiography-guided ventriculoatrial shunt insertion. Oper Neurosurg (Hagerstown). 2020;19(1):25–31.
Kwapisz MM, Deinsberger W, Müller M, Nopens H, Neuhäuser C, Klasen J, et al. Transesophageal echocardiography as a guide for patient positioning before neurosurgical procedures in semi-sitting position. J Neurosurg Anesthesiol. 2004;16(4):277–81.
Møller-Sørensen H, Graeser K, Hansen KL, Zemtsovski M, Sander EM, Nilsson JC. Measurements of cardiac output obtained with transesophageal echocardiography and pulmonary artery thermodilution are not interchangeable. Acta Anaesthesiol Scand. 2014;58(1):80–8.
Odenstedt H, Stenqvist O, Lundin S. Clinical evaluation of a partial CO2 rebreathing technique for cardiac output monitoring in critically ill patients. Acta Anaesthesiol Scand. 2002;46(2):152–9.
Carretero MJ, Fontanals J, Agustí M, Arguis MJ, Martínez-Ocón J, Ruiz A, et al. Monitoring in resuscitation: comparison of cardiac output measurement between pulmonary artery catheter and NICO. Resuscitation. 2010;81(4):404–9.
Romagnoli S, Bevilacqua S, Lazzeri C, Ciappi F, Dini D, Pratesi C, et al. Most care: a minimally invasive system for hemodynamic monitoring powered by the pressure recording analytical method (PRAM). HSR Pro Intensive Care Cardiovasc Anesth. 2009;1(2):20–7.
Franchi F, Falciani E, Donadello K, Zacà V, Silvestri R, Taccone FS, et al. Echocardiography and pulse contour analysis to assess cardiac output in trauma patients. Minerva Anestesiol. 2013;79(2):137–46.
Franchi F, Silvestri R, Cubattoli L, Taccone FS, Donadello K, Romano SM, et al. Comparison between an uncalibrated pulse contour method and thermodilution technique for cardiac output estimation in septic patients. Br J Anaesth. 2011;107:202–8.
Calamandrei M, Mirabile L, Muschetta S, Gensini GF, De Simone L, Romano SM. Assessment of cardiac output in children: a comparison between the pressure recording analytical method and Doppler echocardiography. Pediatr Crit Care Med. 2008;9(3):310–2.
Saxena R, Durward A, Puppala NK, Murdoch IA, Tibby SM. Pressure recording analytical method for measuring cardiac output in critically ill children: a validation study. Br J Anaesth. 2013;110(3):425–31.
Smolle KH, Schmid M, Prettenthaler H, Weger C. the accuracy of the cnap® device compared with invasive radial artery measurements for providing continuous noninvasive arterial blood pressure readings at a medical intensive care unit: a method-comparison study. AnesthAnalg. 2015;121(6):1508–16.
Lakhal K, Martin M, Faiz S, Ehrmann S, Blanloeil Y, Asehnoune K, et al. The CNAP™ finger cuff for noninvasive beat-to-beat monitoring of arterial blood pressure: an evaluation in intensive care unit patients and a comparison with 2 intermittent devices. Anesth Analg. 2016;123(5):1126–35.
Andriessen P, Schraa O, van Den Bosch-Ruis W, Jan Ten Harkel D, Settels JJ, Oetomo SB, et al. Feasibility of non-invasive continuous finger arterial blood pressure measurements in very young children, aged 0-4 years. Pediatr Res. 2008;63(6):691–6.
Andriessen P, Schoffelen RL, Berendsen RC, de Beer NA, Oei SG, Wijn PF, et al. Non-invasive assessment of blood pressure variability in preterm infants. Pediatr Res. 2004;55(2):220–3.
Yiallourou SR, Walker AM, Horne RS. Validation of a new non-invasive method to measure blood pressure and assess baroreflex sensitivity in preterm infants during sleep. Sleep. 2006;29(8):1083–8.
Gupta D, Soskin V, Marjanovic M, Amhaz H, Mazumdar A. Continuous non-invasive arterial pressure device as an adjunct to recognize fluctuating blood pressures during elective caesarean section under subarachnoid blockade (SAB). Middle East J Anaesthesiol. 2016;23(4):385–400.
Sokolski M, Rydlewska A, Krakowiak B, Biegus J, Zymlinski R, Banasiak W, et al. Comparison of invasive and non-invasive measurements of haemodynamic parameters in patients with advanced heart failure. J Cardiovasc Med (Hagerstown). 2011;12(11):773–8.
Bogert LW, Wesseling KH, Schraa O, Van Lieshout EJ, de Mol BA, van Goudoever J, et al. Pulse contour cardiac output derived from non-invasive arterial pressure in cardiovascular disease. Anaesthesia. 2010;65(11):1119–25.
Gellert G, Bramlage P. Use of the ClearSight® system for continuous noninvasive hemodynamic monitoring during heart valve interventions: review of the literature and single-site experience. Heart Surg Forum. 2018;21(6):E476–83.
Tanioku T, Yoshida A, Aratani Y, Fujii K, Kawamata T. Validation of noninvasive continuous arterial pressure measurement by ClearSight System™ during induction of anesthesia for cardiovascular surgery. BMC Anesthesiol. 2020;20(1):176.
Kakuta N, Tsutsumi MY, Murakami C, Sakai Y, Oyama T, Kasai A, et al. Effectiveness of using non-invasive continuous arterial pressure monitoring with ClearSight in hemodynamic monitoring during living renal transplantation in a recipient: a case report. J Med Investig. 2018;65(1.2):139–41.
Jordan HS, Ioannidis JPA, Goudas LC, Chung M, Kupelnick B, Miller K, et al. Thoracic electrical bioimpedance [Internet]. Rockville (MD): Agency for Healthcare Research and Quality (US); 2002.
Elwan MH, Hue J, Green SJ, Eltahan SM, Sims MR, Coats TJ. Thoracic electrical bioimpedance versus suprasternal Doppler in emergency care. Emerg Med Australas. 2017;29(4):391–3.
Harford M, Clark SH, Smythe JF, Gerry S, Villarroel M, Jorge J, et al. Non-invasive stroke volume estimation by transthoracic electrical bioimpedance versus Doppler echocardiography in healthy volunteers. J Med Eng Technol. 2019;43(1):33–7.
Dazzani F, Micati M, Caraceni P, Drago GM, Domenicali M, Pacilli P, et al. Transthoracic electrical bioimpedance: a non-invasive technique for the evaluation of the haemodynamic alterations in patients with liver cirrhosis. Dig Liver Dis. 2005;37(10):786–92.
Sabharwal N, Rao GS, Ali Z, Radhakrishnan M. Hemodynamic changes after administration of mannitol measured by a non-invasive cardiac output monitor. J Neurosurg Anesthesiol. 2009;21(3):248–52.
Mutoh T, Sasaki K, Yamamoto S, Yasui N, Ishikawa T, Taki Y. Performance of electrical velocimetry for non-invasive cardiac output measurements in perioperative patients after subarachnoid haemorrhage. J Neurosurg Anesthesiol. 2019;31(4):422–7.
Cheung H, Dong Q, Dong R, Yu B. Correlation of cardiac output measured by non-invasive continuous cardiac output monitoring (NICOM) and thermodilution in patients undergoing off-pump coronary artery bypass surgery. J Anesth. 2015;29(3):416–20.
Waldron NH, Miller TE, Thacker JK, Manchester AK, White WD, Nardiello J, et al. A prospective comparison of a non-invasive cardiac output monitor versus oesophageal Doppler monitor for goal-directed fluid therapy in colorectal surgery patients. Anesth Analg. 2014;118(5):966–75.
Raval NY, Squara P, Cleman M, Yalamanchili K, Winklmaier M, Burkhoff D. Multicenter evaluation of noninvasive cardiac output measurement by bioreactance technique. J Clin Monit Comput. 2008;22(2):113–9.
Marik PE, Ml B, Vahid B. Does central venous pressure predict fluid responsiveness? Chest. 2008;134(1):172–8.
Shoemaker WC, Appel PL, Kram HB, Waxman K, Lee TS. Prospective trial of supranormal values of survivors as therapeutic goals in high-risk surgical patients. Chest. 1988;94:1176–86.
Luo J, Xue J, Liu J, Liu B, Liu L, Chen G. Goal-directed fluid restriction during brain surgery: a prospective randomized controlled trial. Ann Intensive Care. 2017;7:16.
Wijdicks EF, Vermeulen M, Hijdra A, van Gijn J. Hyponatremia and cerebral infarction in patients with ruptured intracranial aneurysms: is fluid restriction harmful? Ann Neurol. 1985;17:137–40.
Lennihan L, Mayer SA, Fink ME, Beckford A, Paik MC, Zhang H, et al. Effect of hypervolemic therapy on cerebral blood flow after subarachnoid haemorrhage: a randomized controlled trial. Stroke. 2000;31:383–91.
Wu CY, Lin YS, Tseng HM, Cheng HL, Lee TS, Lin PL, et al. Comparison of two stroke volume variation-based goal-directed fluid therapies for supratentorial brain tumour resection: a randomized controlled trial. Br J Anaesth. 2017;119(5):934–42.
Hasanin A, Zanata T, Osman S, Abdelwahab Y, Samer R, Mahmoud M, et al. Pulse pressure variation-guided fluid therapy during supratentorial brain tumour excision: a randomized controlled trial. J Med Sci. 2019;7(15):2474–9.
Wrzosek A, Jakowicka-Wordliczek J, Zajaczkowska R, Serednicki WT, Jankowski M, Bala MM, et al. Perioperative restrictive versus goal-directed fluid therapy for adults undergoing major non-cardiac surgery. Cochrane Database Syst Rev. 2019;12(12):CD012767.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Bloria, S.D., Luthra, A., Chauhan, R., Sethi, S. (2022). Invasive Versus Non-invasive Haemodynamic Monitoring. In: Prabhakar, H., S Tandon, M., Kapoor, I., Mahajan, C. (eds) Transfusion Practice in Clinical Neurosciences. Springer, Singapore. https://doi.org/10.1007/978-981-19-0954-2_7
Download citation
DOI: https://doi.org/10.1007/978-981-19-0954-2_7
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-19-0953-5
Online ISBN: 978-981-19-0954-2
eBook Packages: MedicineMedicine (R0)