Abstract
Medical and health professions education should give attention to faculty and student wellbeing and create a supportive curriculum and teaching–learning process to assure the achievement of competency and readiness of graduates. This chapter highlights that the students, faculty, patients, and other human enterprises are the center of the process. Relevant theories and practices on resilience, burnout, and wellbeing will be discussed comprehensively in the medical and health professions education context in general and in a hierarchical-collectivist cultural context. Resilience or perseverance is the ability of an individual to respond to stress healthily and adaptively so that people may ‘bounce back’ from challenging circumstances and even become more robust in the process. On the other hand, the failed adaptation will result in burnout. The balance between resilience support and burnout prevention is believed to promote wellbeing. The concept is highly relevant to the vision of creating future medical and health professionals and in any efforts involving current students and faculty. In addition to individual processes and development, resilience is influenced by the learning environment. The socialization process within the education milieu allows students and faculties to stay motivated in achieving their goals, prevent burnout and keep developing their personal and professional identity. Studies show that interventions on the individual without paying attention to the learning environment are not adequate. The keys to nurturing and humanistic learning environment which supports resilience are at the individual, interpersonal, and organization/system levels in which culture is embedded. This chapter will also describe that positive role-modeling and mentoring can create the expected learning environment in hierarchical and collectivist cultural context.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
12.1 Introduction
12.2 Humanistic Professions
The role of students in the competency-based medical curriculum has been highlighted by the concept of student-centred learning and self-regulated learning. Student-centred learning approach empowers students to actively engage in the learning process, construct their own understanding through experience, and have their autonomy in learning and scaffolding their knowledge (Lee and Hannafin 2016). Student-centred learning approaches such as problem-based learning, case-based collaborative learning, team-based learning, technology-enhanced learning, etc., are shown to be effective in different learning environments and seem to cultivate positive learning experiences both for students and faculty (Wilson et al. 2018). Furthermore, student self-regulated learning is also as crucial to support the implementation of student-centred learning. Effective implementation of self-regulated learning enables students to be adaptive in various learning environments by realizing and revisiting their learning goals, implementing effective learning strategies, reflecting on their experiences, seeking feedback, and creating future improvements longitudinally (van Houten-Schat et al. 2018; Brydges et al. 2015).
In the current era, medical teachers are required to have mastery of technical abilities, appropriate approaches to teaching, demonstration of professionalism relating to teaching, mastery of the content, understanding of the medical curriculum, and understanding of the different roles of a teacher (Harden and Lilley 2018). Medical teachers are expected to support personalized learning and enable students to transform their knowledge and skills in the fast-growing and ever-changing world (Quirk and Chumley 2018) as well as to become positive role models in the socialization process of students’ learning in becoming future professionals (Cruess et al. 2015; Jarvis-Selinger et al. 2019). Teachers are expected to foster good mentoring and coaching relationship through effective dialogue with students. Good interactions between teachers and students are essential to provide constructive feedback and nurture reflective skills in students (Stenfors-Hayes 2011).
With the growing numbers of competencies required, a rising concern on the humanity aspect of medical profession emerges. Doctors are expected to utilize their knowledge and skills to make accurate diagnosis and provide effective treatment as time-efficient as possible. If all these competencies mapped and translated into curriculum, it can be predicted how packed and rigid the education process that our medical students experience. Research in North America showed high prevalence of mental health problems and burnout in medical students; which might indicate that the journey to become medical doctors is not an easy one. On the other hand, our future doctors are also expected to show professionalism by providing humanistic and compassionate care for their patients. Therefore, medical education should not merely provide learning opportunities for students to understand the scientific basis of diseases and the up-to-date medical technology available, but also the way to care and appreciate the person in humanly approach possible (Horton 2019).
The notion of human institution emphasizes the important role of human relationship within the process occurring in the institution. With the trends towards fast-changing world with its rapid advancement of technology and machine-assisted procedures, this brings back the ‘human’ aspect as the heart of the profession. Humanity in medical education is needed for two important reasons; to help doctors understand their patient as a person and therefore able to treat them better as clinicians; and for the doctors themselves, humanities can help maintain resilience and life balance. It provides them with an ability to restore themselves so they can remain balanced, and sensitive to their own, as well as other people’s needs (Horton 2019). Supportive relationship between teachers and students, or among peers; is also recognized as a very crucial factor in maintaining well-being. Consensus on medical students’ well-being in Australia placed peer supports, teaching adaptive strategies to deal with stress, mentoring, and reflective practice as essential points to address in order to assist students throughout their medical education journey (Kemp 2019).
We aim to elaborate the cultural implications of well-being, resilience, and burnout by exploring the role of positive learning environment and role modelling in the Asian context. We will first discuss the underpinning theories around the concepts before exploring the cultural implications and relevant recommendations. In medical profession, doctors are exposed to adversities in their practice. This could lead to the risk of ‘moral injury’ which was defined as psychological damage due to witnessing or participating in acts that contravene ordinary moral expectation. Adversities in their practice could be in the form of having to make difficult decision, witnessing patients’ suffering, handling shortage of resources and excessive bureaucracy; while pursuing their effort to deliver the best care for their patients (Litz 2009). Medical students gradually experience and face similar challenges during their clinical education as they develop their professional identity. Studies showed that medical students’ mental health worsen throughout the course of their education, showing higher prevalence of stress and burnout compared to their non-medical peers. Therefore resilience should be supported for medical students to cope with everyday situations they faced in their study (Dunn 2008).
12.3 Well-Being, Resilience, and Burnout
A conceptual model for students’ well-being was developed by Dunn (2008) showing the interplay of various factors in helping individuals cope with challenges they experienced which would later determine whether they would become burnout or develop resilience (Fig. 12.1). The coping reserve that each individual possessed is mainly based on their personality and temperament, and is affected by the positive input from the environment (psychosocial support, healthy activities, mentorship, and intellectual stimulation) as well as negative ones (stress, internal conflict, and time/energy demands). Positive input would support students in implementing positive coping mechanism which would later lead to resilience; while the negative input might deplete the coping reserve and increase the risk of burnout (Dunn 2008). Other studies have identified protective factors for resilience, which consists of 3 layers of functioning: individual (psychological, neurobiological), social (such as family cohesion and parental support), and community/society (support systems generated through social, institutional, political, and economic factors) (Windle 2010). Ledesma (2014) distinguished variables related to resilience as internal variable (personality) and external variable (relationship with others).

(modified from Dunn 2008)
The ‘coping reserve’—conceptual model for students’ well-being
According to general dictionary definitions, resilience refers to the ability of an object to recoil or spring back into shape after bending, which describes the similar ability in a person to recover quickly from difficult situations or adversities (Windle 2010). Resilience is described as individual variations in response to risk (Ledesma 2014). Resilient individuals manage their stress effectively and stay well by utilizing positive coping mechanism. These individuals learn and find meaning in their experiences, instead of perceiving it as a psychological burden or threats (Howe 2012). A challenge approach to resilience even views that adversities or negative experience, given that it is not too extreme, can actually enhance a person’s ability to adapt.
Breda (2018) distinguished resilience as a process and an outcome by using the term ‘resilience’ as the mediating process that occur in individuals after or during experiencing difficult situations (adversities); and ‘resilient’ as the positive outcome. Breda defined resilience as the multilevel processes that systems engage into better-than-expected outcomes in the face or wake of adversity. ‘Multilevel’ means that resilience involves multiple domains and layers of social ecology, placing environment as an important factor in promoting resilience (Breda 2018). Sociological approach to resilience also underlines the role of the environment in supporting or hindering resilience; and therefore modification of the social environment could potentially help developing resilience.
Resilience has been linked to several constructs, such as hardiness, self-efficacy, and, more recently, grit (Breda 2018). Grit is defined as perseverance and passion for long-term goals. Gritty individuals are portrayed as marathon runners; they have the stamina to stay on the course and keep on going despite the obstacles or distractions they might experience along the way. It is now believed that inborn intellectual or physical ability alone cannot determine long terms success, individuals must engage in deliberate practice and be able to sustain high levels of practice for a long period of time (Duckworth 2007). Given the high amount of effort needed for completing medical schools, medical students tend to have high scores on grit. Study on medical students also showed that student with high score on grit was associated with good academic performance (Miller-Matero 2018).
Factors influencing student and faculty well-being can be explored using Ryff’s criteria of well-being (Ryff 1989) and Keyes’s 13 dimensions reflecting mental health as flourishing (Keyes 2007). Ryff (1989) illustrated six dimensions/components of well-being which consist of self-acceptance, positive relations with others, autonomy, environmental mastery, purpose in life, and personal growth. Although this theory is postulated for successful ageing, it emphasises wellness, developmental, and growth-oriented within oneself from one stage to the other which is originated from the general study of well-being. Other than perspectives from one-self, Keyes takes into account life domains and social functioning as described in Table 12.1.
The two frameworks might provide us general dimensions that will affect one’s well-being. However, health professionals work in a complex and stressful environment and dealing with many intense issues at the same time. A systematic review conducted by (Huey and Palaganas 2020) recently indicates 4 main themes pertaining to factors that affect resilience in healthcare professionals. Of all the 4 main themes below, the first 3 are described in the framework: (a) The influence of individual factors (i.e. having a higher purpose, being capable of self-care, self-determined with positivity), (b) The influence of environmental and organizational factors (i.e. workplace culture, attention-identification-measurement-assessment), (c) Approaches that an individual takes when interacting with her/his professional circumstances (i.e., workload management, work-life balance, social support, meta-cognitive processes of coping and reframing), and d) Effective educational interventions (i.e. type of intervention, length and duration, required resources).
On the other hand, the concept of burnout highlights the loss of capacities of a person to engage and maintain intense involvement that has meaningful impact at work (Schaufeli et al. 2008). Burnout syndrome is demonstrated by gradual emotional exhaustion which reflects decreased motivation and commitment, personal detachment or depersonalization, and perceptions of decreased personal accomplishment (Maslach et al. 1996). First dimension of burnout, emotional exhaustion, is the physical and emotional response of stress and it often takes place as the first sign of burnout. People who are experiencing emotional exhaustion feel drained hence lowering their capacity to allocate adequate energy for their work and job demands. Second dimension of burnout, cynicism, refers to excessively negative or detached response to various aspects of the job. This dimension moves from personal aspect (i.e. emotional exhaustion) towards a more interpersonal context. Following emotional exhaustion, when people think and feel that they work too much, they will begin to detach themselves from what they are doing to protect themselves. This includes reducing their work and starting to develop negative reaction towards the work and the people. Third or last dimension of burnout, personal accomplishment, is characterized by feeling of incompetence and a lack of achievement. Such feeling leads to great dissatisfaction of a person who tends to blame him/herself for choosing the wrong career path. The occurrence of inefficiency feeling may further lead to loss of confidence and depression (Maslach et al. 1996).
Burnout is also linked with work engagement concept which can be further explained with Job Demands-Resources (JDR) model (van den Berg et al. 2017). Work engagement is a positive well-being outcome which is at the opposite site with burnout and it is characterized by high levels of vigour, dedication, and absorption of ones towards their work. The JDR model explains the relations between work characteristics, work outcomes (such as health, well-being, performance, burnout), and personal characteristics. All physical, psychological, social, and organizational aspects of the job which require sustained efforts hence can be influential to psychological and physical conditions is the ‘job resources’. Whereas job resources concerns all of those aspects which can reduce job demands and the impacts, are functional to achieve job goals, and stimulate personal growth, learning, and development (Schaufeli and Bakker 2004).
The JDR concept can be applied in medical and health professional education context and is very relevant to the role of medical and health professions teachers, students, residents, and health practitioners (van den Berg et al. 2017). Those with good engagement show motivational outcomes such as proactiveness, cooperation, being helpful to the team and ability to strive for quality, hence they tend to be healthier, have better well-being, and have capacity to prevent burnout. Such level of engagement is necessary to strive in demanding and long journey of medical and health professions education and healthcare. Different roles of faculty in teaching, doing research, providing patient care requires various level of engagement which leads to different job crafting. In other words, faculties who are excel in patient care do not necessarily perform well in teaching or research (van den Berg et al. 2017, 2018). Therefore, active processes in job crafting: seeking of social resources, challenging demands, structural resources, and avoiding of hindering demands, should be considered contextually for each role and this should become the note for faculty development and attempts to provide organizational support (van den Berg et al. 2018).
Studies show that medical students and residents often experience burnout (IsHak et al. 2013; Dyrbye et al. 2014). Burnout in this population should raise serious concerns given the impact on personal and professional development as well as future patient care (Dyrbye and Shanafelt 2016). The root cause of burnout among medical students and residents is believed to be in the learning and work environment, instead of personal characteristics and attributes (Williams et al. 2002). The JDR as described above also highlights the role of learning and work environment which can be both considered as ‘demands’ or ‘resources’ (van den Berg et al. 2017). Students’ satisfaction on their learning environment especially in regards to level of support, faculty’s high priority in education, collaborative environment, low number of cynical residents and interns, organized rotations, supervision from faculty and residents, constructive feedback, variety of medical problems, weakness identification, clinical rotation, and workload, seem to be attributable towards prevention or occurrence of burnout (Dyrbye et al. 2009).
Based on the JDR theory understanding and the importance of individual resources in managing burnout, it is also important to discuss the role of motivation in preventing burnout. Based on Self-Determination Theory, motivation has been understood as a spectrum ranging from the self-determined end also known as intrinsic motivation, extrinsic motivation, to amotivation at the other end (Kusurkar et al. 2011). Intrinsic motivation comes from within the students and is supported by students’ sense of autonomy, feeling of competence, and relatedness to the environment. Extrinsic motivation, on the other hand, relies more on external factors as the reward for learning. Studies showed that intrinsically motivated students employ deep learning approach and it correlates with better academic performance. These students also show higher intention to continue their medical studies and become lifelong learners (Kusurkar et al. 2011, 2013).
Students’ feeling of competence and relatedness to the environment might be related to burnout. In burnout, the emotional exhaustion experienced by students left them feeling helpless. They distance themselves from their learning and can sometimes become resentful and cynical towards it. As burnout progressed, students’ sense of personal accomplishment also decline. They stopped seeing themselves as capable of doing their tasks and unable to see the importance of what they are trying to accomplish (Felaza et al. 2020). Studies in an undergraduate medical education setting in Indonesia highlights that when motivation is more externally controlled, the higher the tendency towards burnout, especially in regards to decreased perceptions on personal accomplishment (Felaza et al. 2020). In the similar setting, a study also shows that during transition from preclinical to clinical training, students with high interest motivation show low tendency towards depersonalization and high perceptions on personal accomplishment (Dianti and Findyartini 2019). Amotivation is related with high burnout and low quality of life among undergraduate medical students (Lyndon et al. 2017).
Different from studies concerning burnout among medical and health professions students and residents, studies exploring burnout among faculty or academic staff are quite rare. A scoping review on the studies on burnout of university lecturers reveals that high number of students strongly predict the experience of the teachers’ burnout. Male teachers tend to be at risk of depersonalization while female teachers are more at risk towards emotional exhaustion. Younger teachers are also more vulnerable to emotional exhaustion (Watts and Robertson 2011). A study in Indonesia setting aiming at exploring the use of Maslach Burnout Inventory—Educator Survey (MBI-ES) in medical education highlights that for medical teachers, the possible source of burnout comes from the roles in school administration and management and research and publication demands. Dealing with students and residents seems to be the resources that can have positive influence in preventing burnout (Marlina and Findyartini 2020). Using JDR concept, van der Berg et al. (2018) also suggests that clinical teachers experience different level of work engagement when teaching and providing patient care. Institutions are suggested to provide adequate support for faculty to perform well in different roles. In addition, acknowledging that being clinical teacher is an integral part of a physician’s daily work is expected to support the adaptation of the teachers in engaging in patient care and teaching roles equally (van der Berg et al. 2018).
12.4 Learning Environment and Role Modelling
Following elaboration on well-being, resilience, and burnout, the following section will discuss about key concepts on humanistic learning environment and role modelling. Learning environment is one of the key components which can determine the effectiveness of a competency-based medical curriculum (Schönrock-Adema et al. 2012). It is a system that consists of students (including external relations and other factors affecting the student), the individual who interacts with the student, the circumstances, and objectives of the interaction, and the formal and informal policies that govern the interaction. Theoretically, learning environment is constructed by a goal of learning, relationship between people in the learning environment and organization, including culture, rules, and system (Schönrock-Adema et al. 2012).
Studies exploring learning environment in preclinical and clinical stages of undergraduate medical program, as well as those in postgraduate medical program have been conducted for the past 20 years (e.g. Soemantri et al. 2010; Strand et al. 2013; Findyartini and Utami 2018). Academic learning environment measure such as Dundee Readiness Environment Measure (DREEM) (Soemantri et al. 2010) reflects learning environment based on perceptions of learning, perceptions of teachers, academic self-perceptions, perceptions of the environment, and social self-perceptions. In undergraduate clinical learning environment, there are more variations of the subscales and include perceptions towards learning opportunities and engagement, interactions with patients, communications and interactions with colleagues and supervisors, facility and individual treatment, supervision process, and self-confidence and awareness (Findyartini and Utami 2018). In the clinical learning environment, the physical space, artefact, and rhythm will also influence the learning climate (Sheehan et al. 2017). Nordquist and colleagues (2019) suggest that clinical learning environment is very critical in medical education and it should consider the quality of and interactions among several factors: educational, psychological, socio-cultural, architectural, digital and diversity, and inclusion aspects.
In regards to postgraduate setting, learning environment refers to social, cultural, and material contexts (Isba et al. 2011). Supportive learning environment should allow residents to have supervised patient care activities, coaching, assessment and feedback, deliberate practice which lead to gradual development of competence and professional identity (Boor et al. 2011). Given challenges in creating supportive learning environment for postgraduate training, a national consensus in UK has been discussed and suggests a comprehensive approach and improvement in various areas systematically (Kilty et al. 2017).
Professional physicians are defined by their ability to fulfil their contract with society. In the 4.0 industrial revolution era, public demand a physician who can collaborate with them to manage their health problems. An ideal future physician needs to have ability to build rapport with the patient, win their trust and empower them to solve their problems (Wartman 2018). They need to have all of humanistic values which are integrity, honesty, altruism, compassion, empathy, and respect. The humanistic values need to be grown inside every physician to make them professional (Pellegrino 2006). Humanistic learning environment therefore is required to assure that those humanistic values can be internalized and practiced. This can be nurtured by first recognizing the humanistic values as part of learning outcomes and inseparable component in human interaction in the learning environment, and supportive organization and policy towards humanistic values development in medical and health professions education (Schӧnrock-Adema 2012).
Finally, role modelling has been highlighted as an essential component of clinical teaching in medicine. It has been defined as the “process in which faculty members demonstrate clinical skills, model and articulate thought processes and manifest positive professional characteristics” (Irby 1986). Many have been published on the influence of role modelling, be it positive and negative, to the students in health professionals. It is known that role models are essential to facilitate student learning and assist in the development of professional identity (Haider et al. 2016; Passi and Johnson 2016a), assist in the development of professionalism and career choice (Passi and Johnson 2016a) and development of students’ character (Jochemsen-van der Leeuw et al. 2013). However, the impact of role modelling in student well-being is rarely discussed but should not be neglected.
According to Bandura (Bandura 1989), trainees learn essential professional competencies by observing a role model. Observing alone is insufficient, it also involves a four-step process whereby the learner pay attention to what is being modelled, create a mental representation of what was modelled, providing feedback to the learner on his or her attempts to reproduce what has been modelled, and motivating the learner to continue to practice the modelled behaviours. These processes are influenced by environment, behaviour, and personal factors. Learning through observation is an important feature in Bandura’s theory. A positive role model could provide learners/trainees alternatives in looking at the issues differently through observation (Passi and Johnson 2016a). By using these interventions observed, individual could create a mental representative on how to develop, implement, and cope with the situations better and eventually motivate the individual to move forward or becoming more resilient.
Passi and Johnson (2016b) also proposed a hidden process of positive doctor role modelling. In the exposure phase, trainees/learners are exposed to different aspects such as clinical expertise, relationship with patients, relationship with colleagues, and relationship with students, personality, and inspirational characteristics. The students will emulate a doctor who they perceive is similar to them and who they feel that they ‘could be like him/her’ in future. In the next phase, the evolution phase, students/trainees will start with observing the role model’s behaviour in the clinical setting and make a judgement on whether to carry out the observed behaviour of the role model. Although negative experience stays longer than the positive experience, students did highlight that negative modelling also helped them to make a judgement on what not to behave. Following the judgement phase, the students are involved in a cyclical action which is known as ‘Model-Trialling Cycle’ which involves assembly, imitation, experimentation, adaptation, and assimilation. These processes are important as the students/trainees start ‘picking up’ behaviour and experiment the desired behaviour. Resilient behaviour can be learned and the strategies should be easily accessible and open to everyone and this could be fostered through modelling.
12.5 Well-Being from Cultural Lens
12.5.1 Cultural Perspectives on Well-Being and Resilience
Resilience has been defined in many ways across the literature. Resilience derives from the Latin verb ‘resilire’, meaning to leap or spring back; to rebound, recoil (Theron et al. 2015). Howe et al. (2012) described resilience as a dynamic capability which allows people to thrive on challenges given appropriate social and personal context. Ungar (2006) pointed out that large empirical investigations on resilience focus on: (1) western context with an emphasis on individual and relational factors; and (2) lacking sensitivity to community and cultural factors. As a result, there have been little findings associated with resilience in non-western culture and context. Hence, many research on resilience has called to consider larger, contextual factors which include cultural influence in developing resilience (Clauss-Ehlers et al. 2006).
A growing body of literature delineates how culture may influence the development of resilience in youth from diverse racial and ethnic background (Clauss-Ehlers 2008). A study by Tse and Liew (2004) found that extended-family structures and community-centred ideologies are two major characteristics of most Asian cultures. Harmonious relationship among parents, children, and elderly provides the necessary physical and emotional support to members during time of stress. The strong culture of connectedness that influences the development of resilience is prominent in Asian culture. Academically, Caleon et al. (2017) also found that the notion of autonomous learning strategies (such as asking questions, verbalizing ideas during class) appears to be less compatible with the collectivistic and authority-centric culture orientation of Asian societies. Relatedness was found more important for optimal functioning in a collectivist context as compared to autonomy and competence. However, this aspect is often understudied in health professions education. While connectedness and collectivism can be supporters for resilience in non-western context, large power distance and competitiveness may hinder it given limited dialogue and less positive environment, especially when people attempt to express their vulnerability and failure.
Cultural resilience is a term presented by (Clauss-Ehlers 2006) to illustrate the degree to which the strengths of one's culture promote the development of coping. This type of resilience has a number of aspects including a developmental trajectory within a cultural matrix composed of norms, family structure, and peer relationships. Human capacity in adapting towards challenges is distributed across interacting systems which include system within the individual and his/her relationship with other system such as family, community, and culture (Wright and Masten 2015; Gunnestad 2006).
Although resilience has been increasingly sensitive to the role of culture, it is often dynamic and every new generation interprets culture differently due to the societal norm that they live in. Therefore, carrying out research to assess resilience among different cultural groups is challenging. Ungar (2015) in his article illustrated 3 assumptions related to culture for future research on resilience and interventions.
Three assumptions to be aware of in conducting culture-related research on resilience:
-
(a)
The influence of the dominant culture. There is a tendency that one cultural group influences one another in one context through socialization. For example, the study of Asian American will be different from the study of Asian itself as they have been acculturated in the context they are living in.
-
(b)
Within group resistance to subgroup norms. Even within one cultural group, there are often individual who resist conforming to group norms. Their own experience and socio-economy status might influence how they view resilience and the type of support they received.
-
(c)
Cultural difference in discursive power. In discussing cultural differences in resilience, sometimes one culture tends to be given more authority (more discursive power) than the others due to its social characteristics or influence. However, we have to be cognizant that “the more marginalised the cultural group, the less likely they are to have the power to influence others and convince them that their pathways to resilience make sense” Their voice should also be heard (Fig. 12.2).
12.5.2 Cultural Perspectives on Burnout
Burnout concept can be understood differently in different settings (Schaufeli et al. 2008). Some countries such as Netherlands and Sweden consider burnout as a medical diagnosis under stress-related disorders comprising distress, nervous breakdown, and burnout as the end stage of the diagnosis. Most countries consider burnout as a psychological phenomenon related to stress and workplace. Historically, burnout concept becomes a social phenomenon following sociocultural conditions in the United States in the final decades of twenty-first century. The conditions encompass professionalization of human services, more demanding public towards professions related to human service and lack of reciprocal recognition of the professions and increased ‘narcissistic culture’ that produce individuals with need of immediate gratification (Schaufeli et al. 2017).
Globalization, privatization, and liberalization are believed to change modern life which requires rapid adaptation of new skills, higher productivity, increased time pressures, etc., which may lead to burnout. While emotional exhaustion is conceptualized rather similarly in global context, the last two burnout dimensions: depersonalization and decreased personal accomplishment, are thought to be more culturally bound in Western context. Depersonalization and decreased personal accomplishment concepts are centralized in ‘self’ or ‘individual achievement’ which is rooted in individualist rather than collectivist culture which recognizes team or group achievement rather than individual achievement (Schaufeli 2017).
In accordance with Hofstede’s cultural framework (Hofstede 2001), it is postulated that higher levels of uncertainty avoidance and career success orientation (i.e. higher masculinity) lead to higher burnout level. Individual difference from cultural norms in low individualistic and high power distance, as in many culture in Asia, may also lead to higher prevalence of burnout among professionals (Savicki 2003). A systematic review conducted in China to explore burnout among medical doctors suggests that despite similar results on burnout profiles compared to the studies conducted in Western context, burnout in this setting should be understood comprehensively according to the local culture and change of public expectation. Burnout seems to be more prevalent in young doctors who probably hold dilemma between perceptions of good, high moral duty and respected doctors who should not easily show any signs of burnout according to Confucian culture, and pressures from patients who mistrust the doctors especially those working in small-scale community hospitals (Lo et al. 2018). The results further emphasize the implication of culture in burnout. High uncertainty avoidance culture in which society is more assured by more specialized healthcare services, and individual differences in high power distance society faced by the young doctors, contribute to the burnout prevalence (Savicki 2003; Hofstede 2001).
Collectivism culture highlights social support for medical and health professions education and teacher has given sense of relatedness and recognition of competence especially from the community of practice (van den Berg et al. 2017), hence clear support from the environment is necessary to alleviate or prevent burnout. Studies in non-western setting show that safe clinical learning environment and teacher–student interaction is one of the important factors that can prevent burnout. In this regard, factors which may hinder supportive interactions such as in feedback dialogue, should be anticipated. Factors in learning environment which influence burnout occurrence are actually modifiable (Dyrbye et al. 2009); therefore, management of burnout in medical and health professions education should pay attention to cultural aspects influencing components within clinical learning environment. This includes well-arranged workload schedule and clearly defined role expectations (Nishimura et al. 2019). Simply arranging schedule and limiting work hour to prevent burnout among residents however is not always the best way since it potentially introduces conflict within the residents who would like to exercise and develop their professional autonomy by having more clinical experiences (Nishimura et al. 2019).
A meta-analysis of studies using JDR theory and Hofstede’s cultural framework in different regions of the world show that job demands are positively correlated with burnout (r = 0.32, p < 0.001) and negatively correlated with engagement (r = -0.06, p < 0.001). On the other hand, job resources are negatively correlated with burnout (r = -0.25, p < 0.001) and positively correlated with engagement (r = 0.34, p < 0.001) (Rattrie et al. 2020). Further analyses discussing the moderating effect of cultural values based on Hofstede’s framework are presented below (Rattrie et al. 2020): (a) Culture with strong masculinity will intensify the harm of job demands regarding burnout and engagement. In other words, in culture with high preference towards achievement, heroism, assertiveness and material rewards for success, high competitiveness in workplace may lead to burnout and high job demands may have larger influence towards burnout compared to countries with strong femininity culture which more emphasizes on social values and cooperation. (b) Culture with high power distance can undermine the potential influence of resources to prevent burnout or to increase engagement. Attention towards resources including social and peer support therefore is important to prevent burnout in culture with high power distance. (c) Culture with strong long-term orientation in which pragmatic and education encouragement for the future is high, also tends to reduce positive influence of resources. Internal motivation tends to be ‘muted’ in such cultural setting hence its protective effect towards burnout or strengthening effect towards engagement is lessen. (e) Individualism significantly strengthens the positive effect of resources towards engagement and intensifies negative effect of resources on burnout. This could be due to more focus on personal interest which may enable individuals to optimize resources to strengthen their motivation or well-being, whereas in a more collectivist culture, individuals tend to be preoccupied with group goals which may distract him/her from their own motivation or well-being. This study is by far the first meta-analysis aggregating empirical studies using JDR theory. In regards to cultural framework, it is interesting that moderating effect of each cultural dimension is strongly related to either the consequences of demands on burnout/engagement or on the effects of resources on burnout/engagement, and did not affect both. In addition, it should be noted that the influence of cultural dimensions is not independent to each other (Rattrie et al. 2020).
12.5.3 Cultural Perspectives on Learning Environment
Creating nurturing and humanistic learning environment is critical for the well-being of students and faculty in medical and health professions education (Dyrbye et al. 2009; van Vendeloo et al. 2018). Various interventions to create a more positive learning environment involve multiple components, including regulations, curricular interventions, faculty or staff development, grading practices, instructional interventions, and physical and virtual spaces (Gruppen et al. 2018). The unnecessary ignorance of the role of culture in various interactions of the learning environment components may lead to development of hidden curriculum which may further increase the negative impact towards competence achievement of the students and well-being of the students and faculty. Therefore, this section will elaborate further challenges in learning environment and the hidden curriculum in particular.
Hidden curriculum refers to those practices in students’ behaviour, teachers’ behaviour, student–teacher interaction, teaching–learning processes, assessment, and so on which actually are not formally planned and documented by the institution (Hafferty 1998). Hidden curriculum can be seen from different perspectives (Lawrence 2017): From organization and institution concepts: Hidden curriculum is factors which influence the curriculum at the level of organization and culture, physical resources and infrastructure of the organization, and structures and organizational culture which influence the learning process. From interpersonal-social concept: Hidden curriculum and formal curriculum are socialization processes which involves complex interactions between doctor and patients, other professions and community. It highlights interpersonal processes both structured and unstructured which further impact students’ learning through interaction. Consequently, students learn professional behaviours from their interaction with teachers, residents/trainees, other health professionals, and patients in clinical learning environment. The role modelling process therefore becomes the key. From context and culture concepts: Hidden curriculum is all informal aspects beyond formal curriculum which describes wider cultural atmosphere within an institution and most of the time are beyond control of the leadership or organizer. From motivation and psychology concepts: Hidden curriculum concerns on informal teaching–learning process which happen through dialogue and informal interaction. This involves subconscious beliefs, values, and implicit attitude which further influence students’ motivation and learning behaviour and teachers’ teaching belief and attitude.
Those happen in hidden curriculum are not always supportive towards students’ academic development nor humanistic learning environment (Ofri 2017). Discrepancies in formal and hidden curriculum would give mixed message to the students and teachers, and may bring helplessness feelings and internal conflicts which hamper humanistic values and professional development (Hopkins et al. 2016). A survey in the US reports that 45% internal medicine residents feel that their learning environment is not humanistic and this leads to burnout (Billings 2011); for example, observation of uncomfortable communications being done by senior clinicians or conduct of unprofessional behaviours by fellow residents. These phenomena underline the negativity bias theory which state that negative aspects in learning environment can be very influential for the students and faculty (Haizlip 2012).
Given the importance of workplace-based learning and dynamic interactions in medical and health professions education, hidden curriculum should be managed and recognized: those with positive impacts should be strengthened and those with negative impacts should be mitigated (Aultman 2005). Studies on hidden curriculum focus more on the negative impact such as emotional neutralization, ethical and integrity erosion, hierarchical acceptance, and false confidence of actual learning to become medical doctors, which are all the anti-thesis for humanism (Martimianakis and Hafferty 2016). Therefore, internalization of humanistic values and personal and professional development of trainees can be assured through positive and humanistic learning environment. Positive and humanistic learning environment can be encouraged through role modelling of good doctor-patient interaction and development of safe environment to discuss feedback. Faculty development hence becomes more important to support the teachers’ role in becoming role model and in creating humanistic learning environment (Branch et al. 2015).
12.5.4 Cultural Perspectives on Role Modelling
Given collectivist and high power distance culture in South East Asia/Asia setting, positive role modelling can be a strong approach to create supportive learning environment which also considers student well-being. Medical and health professions teachers are also encouraged to be aware of their teaching beliefs and concepts which most of the time are tied closely with the organizational culture. Studies which compared postgraduate medical education in Thailand and Canada (Wong 2011), clinical reasoning teaching in undergraduate medical educations in Australia and Indonesia (Findyartini et al. 2016) and feedback practices in undergraduate medical education in the Netherlands and Indonesia (Suhoyo et al. 2017) provide further insights on the importance of recognizing cultural dimensions and values in the learning environment.
Asian students really value the teaching process, feedback, and modelling provided by experts (Findyartini et al. 2016; Suhoyo et al. 2017). Wong AK (2011) notes that teachers in Thailand consider the faculty-resident/student relationship as family and teachers should actively seek alternatives to enhance student active learning and provide them with corrective feedback. In Canadian setting, on the contrary, teachers consider the relationship as collegial and their efforts more concentrate on providing safe learning environment which promotes learning and makes feedback with care more available to students/residents. Findyartini et al. (2016) and Suhoyo et al. (2017) also recognize the high power distance dimension in Indonesia setting which influence how teachers position themselves as resource person and role model and in providing feedback. Teachers may attempt to provide examples on how to reflect on their performance and seek feedback from their peers and students which are then utilized to improve their future performance.
12.6 Way Forward to Assure Student and Faculty Well-Being Considering Cultural Perspectives
Well-being is influenced by culture and values since it is constructed by individual-related factors, environmental and organizational factors, approaches that an individual takes when interacting with her/his professional circumstances, and effective educational interventions. Therefore, any attempts at preserving well-being which includes encouragement of resilience and prevention of burnout among students and faculty in medical and health professions education should consider the individual, interpersonal, and organizational/system factors.
As well-being is culturally related, the concept of culture has to be emphasized that it is beyond symbols (i.e. languages, pictures, dresses) or rituals (i.e. gestures to show respect, religious ceremonies, and daily interactions). The core of culture is valued, which mainly shows one’s preference among feelings that is dynamically acquired during a person’s lifetime (i.e.: good vs. bad, permitted vs. forbidden, clean vs. dirty) as shown in five cultural dimensions: power distance, masculinity vs. femininity, collectivism vs. individualism, uncertainty avoidance, long-term orientation vs. short-term orientation, and indulgence vs. restraint. These cultural dimensions provide ways to embrace the richness of culture and values in each medical and health professions’ education settings.
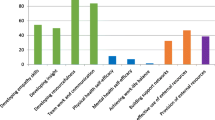
Given the aforementioned factors related to well-being in this chapter (i.e. distress level and burnout, level of resilience, and learning environment), it is important to explore interventions to ensure student and faculty well-being, including psychological safety, both at individual level and at system level. The interventions should consider the cultural dimensions in Asia, which predominantly have higher power distance and higher collectivism. We recommend the following approaches to be conducted to help assuring students and faculty well-being in the Asian setting:
-
1.
Identify struggling students and faculty members in academic/ career and personal issues through observations, dialogues, and discussions (Wright, et al. 2017; Vogan, et al. 2014)
What?
Dialogue helps to explore the root cause of problems, thus making it possible to screen for any risks of burnouts and distress among students or faculty members. Identifying students and faculties with potential problems in their well-being is necessary.
How?
Conducting regular inquiry process and two-way dialogue is important to be conducted on daily basis, making use of interactions within or outside classrooms, during informal periods such as lunch time, as it facilitates teachers in developing self-awareness, and promote self-management process. Prompt and just-in-time responses are also critical following the diagnosis of struggling students and faculty members.
Possible challenge and how to overcome the challenge in higher power distance and collectivist culture?
Students might be more reluctant to open up with faculty members about their concerns and problems. Hence, involvement of peers in identifying possible root cause is deemed important. Therefore, beside faculty development for teachers, training for students as peers on identifying symptoms of burnouts, risks of distress among students, and providing appropriate supports for other students at risk are also necessary.
-
2.
Sufficient student support from faculty members or community of practice through coaching and mentoring (White et al . 2014 , Sambunjak et al. 2010 ; Tan et al. 2018 ; Pinalla et al. 2015 ; Greviana et al. 2020 ; Pacifico et al. 2018 )
What?
Coaching and mentoring can be conducted among students, for students and faculty members, or among junior and senior faculty members. In coaching mentoring process, mentors and mentees are engaged in a two-way non-judgemental relationship and dialogue aiming to provide supports for mentees learning and development. Mentoring program is slightly different from coaching in terms of mentors’ role as advisor and expert, therefore it is possible to include a teaching sessions during the mentoring program. Coaching and mentoring program is usually concluded with agreed plan to overcome the problem, in which mentor also agree on at the end of the session. Coaching and mentoring program can be conducted individually on one-on-one session, or group mentoring with the ideal number of 5–8 students in each group.
How?
Informal interactions: discussions about difficult topics; such as difficult, death, and dying patients; mistakes; workloads; inadequate resources; or other dilemmas; informal chatting, group trips or capacity building with games as a wellness program, or group discussions.
Formal/ teaching sessions: lectures, small group discussions, literature reading, role play, and reflective writing exercise; courses in wellness and resilience, such as stressors in medical education, concept of resilience and its training
Possible challenge and how to overcome the challenge in higher power distance and collectivist culture?
Common problem in coaching mentoring is that mentee does not appear to listen or act on the feedback or the agreed plan. This may be due to the misaligned expectations of both mentors and mentees. Therefore, it is important to start each mentoring session by discussing mentees’ needs so that mentors could select appropriate guidance approach. Some mentees may need directions and direct advice to follow, while some others need help in identifying strategies that students can comfortably engage with. Group mentoring would be more favourable in higher collectivist culture, however, it is important for mentors to pay attention to individual needs and expectations. Interactive reflective writing following the group mentoring session using electronic platform (i.e.: private chat, reflective e-portfolio) that enable follow-up written private communication between mentors and each mentees may be used to further discuss and provide safer environment for each individual to reflect. Electronic platform is preferred to be used, compare to conventional written reflection using pen and pencil, due to the characteristics of students nowadays, the Generation-Z, who are digital natives and technological savvy. Furthermore, electronic platform could be modified with some hidden reflective writing features which may also be used for practice during early stage of implementation to provide safe learning environment, as some students might feel uncomfortable to share their reflections.
-
3.
Workshop and training on well-being and mindfulness (Scheepers RA et al. 2020; Kushner et al. 2011; Wald et al. 2016)
What?
Attempts to enhance well-being of students and faculty has to be conducted with attempt to increase the knowledge of stakeholders with the basic concept of well-being itself and why it is important for health professionals (i.e. health professionals with burnout are at risk in exhibiting low professionalism and providing suboptimal health care to patients). This relevance is required in order for stakeholders to pay greater attention to their own and others’ well-being around them. Besides, it is also known that ones with knowledge of wellness strategies are at lower risk to suffer severe burnout than those who know less about it
How?
Workshops, trainings, and addition about the well-being concept in the curriculum is potential aim to prevent burnout, strengthen resilience, and manage multifactorial attributes influencing overall well-being. Some options of wellness strategies and coping strategies followed could be taught during the workshops and reflected by participants including to spend more time with their loved ones, create feasible timetable according to priority scales, explore meaning and values of their study, practice their religion, encourage positive attitude and point of view, and practice self-care.
Possible challenge and how to overcome the challenge in higher power distance and collectivist culture?
As workshops are conducted usually in larger groups, the challenge would be the low participation of students or faculty members. This low participation might be caused by the low knowledge about its importance. Therefore, to increase its relevance, the concept of well-being itself should be made explicit in the curriculum, making it a shared vision and values in the institution, not only personal or individual goals. In higher power distance culture, workshops that are made mandatory would also result in more attention paid by stakeholders about its importance. Sustainability about the workshop results also has to be considered. Follow-up coaching and mentoring processes and reflections should also be conducted as means to ensure the sustainability of well-being practice among stakeholders.
What?
Maintaining of well-being is an important part of maintaining one’s professional behaviour as it is known that some unprofessional behaviours of health professionals are associated with well-being. Medical school leaders, administrators, teachers, and peers have opportunity to personally role model well-being and healthy behaviours in order to promote a supportive learning environment and a culture of well-being. Role modelling is also an important aspect in creating effective learning environment in medical education.
How?
Everyone can be a role model through personally practicing and maintaining well-being, which can be achieved through good time-management and health (i.e.: exercise, sleep, nutrition, hydration, stress management), modelling reflective habit of well-being practice. Medical school administrators and teachers become role model in well-being practice through proactively checking in students’ workloads and offer supports when necessary, encourage and invite feedback. Leaders may show regular consideration of their leadership style and approach which may impact others’ well-being.
Possible challenge and how to overcome the challenge in higher power distance and collectivist culture?
Some negative role models might be found in the workplace. A study in Asian country setting showed negative role modelling by medical teachers due to poor time management and heavy workloads, which somehow related to well-being concept. Negative role modelling was also known to be easier to memorise than the positive ones, hence, it became one of a challenge of role modelling well-being, as students in higher power distance society tend to feel discouraged to discuss and speak up against negative role models. Therefore, opportunities to conduct self-reflection, both for the role models and for the students are important to corporate role modelling process of maintaining ones’ well-being.
-
5.
Peer Assisted Learning (Ross and Cumming 2013 )
What?
As most strugglers in medical education showed academic challenges, supports from peers become important. Peer-assisted learning (PAL) is defined as teaching–learning interactions conducted by people from similar social groupings, and not by professional teachers. Both tutors, tutees, and institutions advantage through peer-assisted learning, of which created psychological safety for students, thus benefit for well-being maintenance of students.
How?
In planning and conducting PAL, it is important to understand the situations and aims of PAL. Explicitly mentioning criteria of tutors and tutees will also be necessary as well as the interaction and its evaluation. PAL can be conducted formally or informally.
Possible challenge in higher power distance and collectivist culture?
PAL approach is beneficial especially for students from higher collectivist culture. However, students in higher power distance society may question the tutors’ experience and knowledge and skills thus further reduce tutees’ confidence and decrease participation. Therefore, it may be beneficial if PAL in this society is accompanied with prior tutor training by faculty members.
12.7 Summary
In regards to Hofstede’s cultural framework, there are not many studies using the framework to explore and discuss the concepts in this chapter. However, given understanding on the cultural dimensions and factors which influence conceptualization of well-being, burnout, and resilience as well as learning environment, we advocate the importance of providing the medical students and residents tools or venues to voice their concerns in regards to these issues. In addition, it is important to encourage feeling of acceptance in the workplace-based settings by the community of practice and this can be done by delegating clinical entrustment to the students appropriately with adequate supervision, and putting efforts to enhance non-blaming culture and respectful interactions within interprofessional teams. The efforts to bridge the distance between students/residents with the community of practice and with the system are important. Finally, it becomes prominent that these issues should be understood and addressed properly by the teachers, the curriculum, and the overall system in order to foster future resilient and adaptive medical and health professionals.
Key Learning Points
-
Resilience is a significant capacity of students and teachers to overcome dynamic challenges in medical and health professions education.
-
Resilience, burnout, and well-being are culture-sensitive i.e., they can be conceptualized and practiced differently in different cultures, including between individualistic and collectivistic cultures or between those with high and low power distance.
-
Strategies to strengthen resilience in medical and health professions education require an understanding of nurturing learning environment, positive role-modeling, and embedded cultural context.
-
Students and teachers in medical and health professions education should be made aware of the importance of fostering resilience, preventing burnout, and promoting well-being in order to engage actively in the dynamic processes at the individual, interpersonal and system levels.
References
Aultman JM (2005) Uncovering the hidden medical curriculum through a pedagogy of discomfort. Advan Health Educ Theory Pract 10:263–273
Armyanti I, Mustika R, Soemantri D (2020) Dealing with negative role modelling in shaping profssional physician: an exploratory study. J Pakistan Med Educ 70(9):1527–1532
Bandura A (1989) Social cognitive theory. In: VASTA R (ed) Annals of child development, vol 6. Six theories of child development. JAI Press, Greenwich CT
Billings ME, Lazarus ME, Wenrich M et al (2011) The effect of hidden curriculum on resident burnout and cynicsm. J Grad Med Educ 3(4):503–510
Boor K, Van Der Vleuten C, Teunissen P et al (2011) Development and analysis of D-RECT, an instrument measuring residents’ learning climate. Med Teach 33:820–827
Branch WT (2015) Teaching professional and humanistic values: Suggestion for a practical and theoretical model. Patient Educ Couns. 98:162–7
Breda AD (2018) A critical review of resilience theory and its relevance for social work. Soc Work 54:1–17
Brydges R, Manzone J, Shanks D (2015) Self-regulated learning in simulation-based training: a systematic review and meta-analysis. Med Educ 49:368–378
Caleon IS, Wui MGL, Chiam CL (2017) Personal strengths and perceived teacher support as predictors of Singapore students’ academic risk status. Educ Psychol 37:983–1000
Clauss-ehlers CS (2008) Sociocultural factors, resilience, and coping: support for a culturally sensitive measure of resilience. J Appl Dev Psychol 29:197–212
Clauss-ehlers CS, Yang YTT, Chen WCJ (2006) Resilience from childhood stressors: the role of cultural resilience, ethnic identity, and gender identity. J Infant, Child Adolesc Psychoth 5:124–138
Cruess RL, Cruess SR, Boudreau D et al (2015) A schematic representation of the professional identity formation and socialization of medical students and residents: a guide for medical educators. Acad Med 90(6):718–725
Dianti NA, Findyartini A (2019) The relationship between type of motivation and burnout in medical student during transition from preclinical to clinical stages in Universitas Indonesia 2018. E-J Kedokteran Indonesia 7(2):115–121
Duckworth AL, Peterson C, Matthews MD et al (2016) Grit: perseverance and passion for long-term goals. J Pers Soc Psychol 92:1087–1101
Dunn LB, Iglewicz A, Moutier C (2008) A conceptual model of medical students’ well-being: promoting resilience and preventing burnout. Acad Psychiatry 32(1):44–53
Dyrbye LN, Thomas MR, Harper W et al (2009) The learning environment and medical student burnout: a multicentre study. Med Educ 43:274–282
Dyrbye LN, West CP, Satele D et al (2014) Burnout among U.S. medical students, residents, and early career physicians relative to the general U.S. population. Acad Med 89:443–451
Dyrbye LN, Shanafelt T (2016) A narrative review on burnout experience by medical students and residents. Med Educ 50:132–149
Felaza E, Findyartini A, Mustika R et al (2020) How motivation correlates with academic burnout: study conducted in undergraduate medical students. Educ Med J 12(1):43–52
Findyartini A, Hawthorne L, McColl G, a., (2016) How clinical reasoning is taught and learned: cultural perspectives from the University of Melbourne and Universitas Indonesia. BMC Med Educ 16:185
Findyartini A, Utami DB (2018) Development of clinical learning environment measure in the undergraduate medical program. Adv Sci Lett 24:6097–6108
Greviana N, Mustika R, Soemantri D (2020) e-Portfolio system development for undergraduate clinical dentistry: an action research study. Padjadjaran J Dent 32(2):91–100
Gruppen L, Irby D, Durning S et al. (2018) Interventions designed to improve the learning environment in the health professions: a scoping review. MedEdPublish 7(3). doi:https://doi.org/10.15694/mep.2018.0000211.1
Gunnestad A (2006) Resilience in a cross-cultural perspective: how resilience is generated in different cultures. https://www.immi.se/intercultural/nr11/gunnestad.htm. Accessed 12 Feb 2020
Hafferty FW (1998) Beyond curriculum reform: confronting medicine’s hidden curriculum. Acad Med 73:403–407
Haider SI, Snead DRJ, Bari MF (2016) Medical students’ perceptions of clinical teachers as role model. PLoS ONE 11:e0150478–e0150478
Haizlip J, May N, Schorling J et al (2012) Perspective: the negativity bias, medical education, and the culture of academic medicine: why culture change is hard. Acad Med 87:1205–1209
Harden RM, Lilley P (2018) The eight roles of the medical teacher: the purpose and function of a teacher in the healthcare professions. Elsevier Health Sciences
Hochberg MS, Berman RS, Kalet AL et al (2013) The stress of residency: recognizing the signs of depression and suicide in you and your fellow residents. Am J Surg 205(2):141–146
Hofstede G (2001) Culture’s consequences: Comparing values, behaviours, institutions, and organisations across nations. 2nd edition. Thousand Oaks, CA: Sage
Hopkins L, Saciragic L, Kim J et al. (2016) The hidden curriculum: Exposing the unintended lessons of medical education. Cureus 8(10):e845
Horton ME (2019) The orphan child: humanities in modern medical education. Philos Ethics Humanit Med 14:1–6
Howe A, Smajdor A, Stockl (2012) A towards an understanding of resilience and its relevance to medical training. Med Educ 46:349−356
Huey CWT, Palaganas JC (2020) What are the factors affecting resilience in health professionals? A synthesis of systematic reviews. Med Teach 42(5):550–560
Irby DM (1986) Clinical teaching and the clinical teacher. J Med Educ 61:35–45
Isba R, Boor K (2011) Creating a learning environment. In: Dornan T, Mann KV, Scherpbier A, Spencer J (eds) Medical education: theory and practice. Churchill Livingstone, London, pp 99–114
Ishak W, Nikravesh R, Lederer S et al (2013) Burnout in medical students: a systematic review. Clin Teac 10:242–245
Jarvis-Selinger S, MacNeil KA, Costello GRL et al (2019) Understanding professional identity formation in early clerkship: a novel framework. Acad Med 94(10):1574–1580
Jochemsen-van der Leeuw HGAR, van Dijk N, van Etten-Jamaludin FS et al (2013) The attributes of the clinical trainer as a role model: a systematic review. Acad Med 88:26–34
Kemp S, Hu W, Bishop J et al (2019) Medical students well-being: a consensus statement from Australia and New Zealand. BMC Med Educ 19:1–8
Keyes CL (2007) Promoting and protecting mental health as flourishing: a complementary strategy for improving national mental health. Am Psychol 62:95
Kilty C, Wiese A, Bergin C et al (2017) A national stakeholder consensus study of challenges and priorities for clinical learning environments in postgraduate medical education. BMC Med Educ 17:226
Kushner RF, Kessler S, McGaghie WC (2011) Using behavior change plans to improve medical student self-care. Acad Med 86(7):901–906
Kusurkar RA, Ten Cate TJ, Van Asperen M et al (2011) Motivation as an independent and dependent variable in medical education: a review of the literature. Med Teach 33(5):e242-262
Kusurkar RA, Croiset G, Galindo-Garré et al. (2013) Motivational profiles of medical students: association with study effort, academic performance, and exhaustion. BMC Med Educ 13:1−8
Lawrence C, Mhlaba T, Stewart K, Molestsane R (2017) The hidden curricula of medical education: a scoping review. Acad Med 93(4):1
Ledesma J (2014) Conceptual frameworks and research models on resilience in leadership. SAGE Open 4(3):2158244014545464
Lee E, Hannafin MJ (2016) A design framework for enhancing engagement in student-centered learning: own it, learn it, and share it. Educ Tech Res Dev 64:707–734
Lo D, Wu F, Chan M et al (2018) A systematic review of burnout among doctors in China: a cultural perspective. Asia Pac Fam Med 17:3
Lyndon MP, Henning MA, Alyami H et al (2017) Burnout, quality of life, motivation, and academic achievement among medical students: a person-oriented approach. Perspec Med Educ 6:108–114
Marlina M, Findyartini A (2020) Content validity of burnout measurement of medical teacher in Indonesia. E-J Kedokteran Indonesia 8(1):23–30
Martimianakis MA, Hafferty FW (2016) Exploring the interstitial space between the ideal and the practised: humanism and the hidden curriculum of system reform. Med Educ 50:278–280
Maslach C, Jackson SE, Leiter MP (1996) MBI: The Maslach Burnout Inventory: Manual. Consulting Psychologists Press, Palo Alto, CA
Miller-Matero LR, Martinez S, Maclean L et al (2018) Grit: a predictor of medical students performance. Education for Health 31:109–113
Nishimura Y, Miyoshi T, Obika M et al (2019) Factors related to burnout in resident physicians in Japan. Int J Med Educ 10:129–135
Nordquist J, Hall J, Caverzagie K et al (2019) The clinical learning environment. Med Teach 41(4):366–372. https://doi.org/10.1080/0142159X.2019.1566601
Ofri D (2017) Medical humanities: the Rx for uncertainty? Acad Med 92:1657–1658
Pacifico JL, van der Vleuten CPM, Muijtjens AMM et al (2018) Cross-validation of a learning climate instrument in a non-western postgraduate clinical environment. BMC Med Educ 18:22
Passi V, Johnson N (2016) The impact of positive doctor role modeling. Med Teach 38:1139–1145
Passi V, Johnson N (2016) The hidden process of positive doctor role modelling. Med Teach 38:700–707
Pellegrino ED (2006) Toward a reconstruction of medical morality. Am J Bioeth 6(2):65–71
Pinalla S, Pander T, von der Borch P et al. (2015) 5 years of experience with a large-scale mentoring program for medical students. GMS J Med Educ 32(1):Doc5
Quirk M, Chumley H (2018) The adaptive medical curriculum: a model for continuous improvement. Med Teach 40(8):786–790
Rattrie LTB, Kittler MG, Paul KI (2020) Culture, burnout and engagement: a meta-analysis on national cultural values as moderators in JD-R theory. Appl Pscyhol Int Rev 69(1):176–220
Ross MT, Cumming DA (2013) Peer assisted learning. Dent JA. Elsevier, Harden RM. Practical guide for medical teachers. Churchil Livingstone, pp 134–141
Ryff CD (1989) Beyond ponce de leon and life satisfaction: new directions in quest of successful ageing. Int J Behav Dev 12:35–55
Sambunjak D, Straus SE, Marusic A (2010) A systematic review of qualitative research on the meaning and characteristics of mentoring in academic medicine. J Gen Intern Med 25(1):72–78
Savicki V (2003) A cross-cultural study of burnout and job roles. Soc Work Europe 10(1):41–48
Schönrock-Adema J, Bouwkamp-Timmer T, Hell EAV et al (2012) Key elements in assessing the educational environment: where is the theory? Adv Health Sci Educ Theo Pract 17:727–742
Schaufeli WB, Leiter MP, Maslach C (2008) Burnout: 35 years of research and practice. Career Dev Int 14(3):204–220
Schaufeli WB, Bakker AB (2004) Job demands, job resources, and their relationship with burnout and engagement: a multi-sample study. J Organiz Beh 25:293–315
Schaufeli WB (2017) Burnout: a short socio-cultural history. In: Neckel S, Schaffner AK, Wagner G (eds) Burnout, fatigue, exhaustion: an interdisciplinary perspective of a modern affliction. Springer Nature, Switzerland
Scheepers RA, Emke H, Epstein RM et al (2020) The impact of mindfulness-based interventions on doctors’ well-being and performance: a systematic review. Med Educ 54:138–149
Sheehan D, Jowsey T, Parwaiz M et al (2017) Clinical learning environments: place, artefacts and rhythm. Med Educ 51(10):1049–1060
Soemantri D, Herrera C, Riquelme A (2010) Measuring the educational environment in health professions studies: a systematic review. Med Teach 32(12):947–952
Stenfors-Hayes T, Hult H, Dahlgren LO (2011) What does it mean to be a good teacher and clinical supervisor in medical education? Adv Health Sci Educ Theory Pract 16(2):197–210
Strand P, Sjöborg K, Stalmeijer R et al (2013) Development and psychometric evaluation of the Undergraduate Clinical Education Environment Measure (UCEEM). Med Teach 35(12):1014–1026
Suhoyo Y, Van Hell EA, Kerdijk W et al (2017) Influence of feedback characteristics on perceived learning value of feedback in clerkships: does culture matter? BMC Med Educ 17:69
Tan YS, Teo SWA, Pei Y et al (2018) A framework for mentoring of medical students: thematic analysis of mentoring programmes between 2000 and 2015. Adv Health Sci Edu Theory Pract 23(4):671–697
Theron LC, Liebenberg L, Ungar M (2015) Youth resilience and culture: commonalities and complexities. Springer, Netherlands, Dordrecht
Tse S, Liew T (2004) New Zealand experiences: How is community resilience manifested in Asian communities? E-comm Int J Mental Health Add 2:1–8
Ungar M (2006) Resilience across cultures. Brit J Soc Work 38:218–235
Ungar M (2015) Resilience and culture: the diversity of protective processes and positive adaptation. In: Theron lC, Liebenberg l, Ungar M (eds) Youth resilience and culture: Commonalities and complexities. Springer Netherlands, Dordrecht
van den Berg JW, Mastenbroek NJJM, Scheepers RA et al (2017) Work engagement in health professions education. Med Teach 39(11):1110–1118
van den Berg JW, Verberg CPM, Scherpbier AJ et al (2018) Faculty’s work engagement in patient care: Impact on job crafting of the teacher. BMC Med Educ 18:312
van Houten-Schat MA, Berkhout JJ, van Dijk N (2018) Self-regulated learning in the clinical context: a systematic review. Med Educ 52(10):1008–1015
van Vendeloo SN, Godderis D, Brand PLP (2018) Resident burnout: Evaluating the role of the learning environment. BMC Med Educ 18:54
Vogan CL, McKimm J, Da Silva AL et al (2014) Twelve tips for providing effective student support in undergraduate medical education. Med Teach 36(6):480–485
Wald HS, Haramati A, Bachner YG et al (2016) Promoting resiliency for interprofessional faculty and senior medical students: outcomes of a workshop using mind-body medicine and interactive reflective writing. Med Teach 38(5):525–528
Wartman SA, Combs CD (2018) Medical education must move from the information age to the age of artificial intelligence. Acad Med 93(8):1107–1109
Watts J, Robertson N (2011) Burnout in university teaching staff: a systematic literature review. Educ Res 53(1):33–50
White MK, Barnett P (2014) A five step model of appreciative coaching: a positive process for remediation. In: Kalet A, Chou CL Remediation in medical education: a Mid- Course Correction. Springer Science and Business Media, New York
Williams ES, Konrad TR, Linzer M et al (2002) Physician, practice, and patient characteristics related to primary care physician physical and mental health: Results from the physician work life study. Health Serv Res 37:119–141
Wilson AB, Brown KM, Misch J et al (2018) Breaking with tradition: a scoping meta-analysis analyzing the effects of student-centered learning and computer-aided instruction on student performance in anatomy. Anat Sci Educ 12(1):61–73
Windle G (2011) What is resilience? A review and concept analysis. Rev Clin Gerontol 21(2):152
Wong AK (2011) Culture in medical education: Comparing a Thai and a Canadian residency programme. Med Educ 45:1209–2119
Wright EM, Matthai MT, Warren N (2017) Methods for alleviating stress and increasing resilience in the midwifery community: a scoping review of the literature. J Mid Women’s Health 62(6)
Wright MOD, Masten AS (2015) Pathways to resilience in context. In: Theron IC, Liebenberg l, Ungar M (eds) Youth resilience and culture. Cross-cultural advancements in positive psychology. Springer, Dordrecht
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2022 The Author(s), under exclusive license to Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Findyartini, A., Lee, S.S., Felaza, E., Mustika, R., Greviana, N. (2022). Strengthening Resilience in Medical and Health Professions Education: The Dynamic Interaction of Culture, Humanistic Environment, and Positive Role Modelling. In: Claramita, M., Findyartini, A., Samarasekera, D.D., Nishigori, H. (eds) Challenges and Opportunities in Health Professions Education. Springer, Singapore. https://doi.org/10.1007/978-981-16-7232-3_12
Download citation
DOI: https://doi.org/10.1007/978-981-16-7232-3_12
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-16-7231-6
Online ISBN: 978-981-16-7232-3
eBook Packages: MedicineMedicine (R0)