Abstract
Risk-reducing salpingo-oophorectomy (RRSO) is performed for the primary prevention of ovarian cancer in patients with hereditary breast–ovarian cancer (HBOC) syndrome. When HBOC is diagnosed without ovarian cancer, surveillance is performed using transvaginal ultrasound and serum CA125 assessment, and chemoprophylaxis is administered using oral contraceptives (OCs) or low-dose estrogen–progestin (LEP); however, RRSO is the most reliable treatment for ovarian cancer prevention. While RRSO is expected to gain popularity, due attention must be paid to the fact that this procedure is not easy to perform. Performing RRSO requires a deep understanding of the biological and anatomical characteristics of the structures surrounding ovarian cancer, paying attention to important points while performing surgical procedures, and taking precautions to facilitate pathology examination; moreover, a thorough understanding of gynecologic oncology and female reproductive medicine, such as treatment for surgical menopause, is required. Furthermore, following RRSO, minute ovarian cancers, which cannot be identified on preoperative evaluation, and occult cancers, which are serous tubal intraepithelial carcinoma (STIC) lesions of the fallopian tubes, can become apparent. To detect occult cancer, pathological examination is inadequate in cases of benign disease, and it is important to proceed with the sectioning and extensively examining the fimbriated end (SEE-FIM) protocol in collaboration with pathologists. Moreover, for RRSO to perform its original role, which is primary prevention, it should be kept in mind to introduce the procedure at the end of childbirth between the age of 35 and 40 years, as recommended in the guidelines, and at an appropriate time based on the earliest age of ovarian cancer onset among individuals in the patient’s family. To provide the maximum benefit to patients with HBOC, individuals involved in the care of such patients must deepen their knowledge not only in their own field of expertise but also in genetic medicine and incorporate this knowledge into routine medical care.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Risk-reducing salpingo-oophorectomy (RRSO)
- Hereditary breast–ovarian cancer (HBOC) syndrome
- Ovarian cancer
- Breast cancer
- Peritoneal cancer
- Concurrent hysterectomy
- Two-stage surgery
- Sectioning and extensively examining the fimbriated end (SEE-FIM) protocol
- Health care
- Hormonal replacement therapy
12.1 Significance of RRSO
Among patients with HBOC, the risk of ovarian cancer onset before the age of 80 years is high at 44% among those harboring BRCA1 gene variant and 17% among those harboring BRCA2 gene variant [1]. Prophylactic treatments against this risk include RRSO and chemoprophylaxis using low-dose oral contraceptives (OCs) or low-dose estrogen–progestin (LEP). When RRSO cannot be performed, surveillance is performed using transvaginal ultrasound and serum CA125 assessment. Reportedly, the use of OC/LEP significantly reduces the risk of ovarian cancer by approximately 50% even in patients harboring BRCA1/BRCA2 gene variants [2]. However, regarding the relationship between OC/LEP usage and breast cancer onset, some reports indicate an increased risk [3,4,5], whereas others indicate no relationship [6, 7]; thus, these issues should be fully explained when prescribing prophylactic agents. Regarding surveillance, it has been reported that screening using transvaginal ultrasound and serum CA125 assessment does not contribute to reducing mortality due to ovarian cancer [8, 9]. Nevertheless, the National Comprehensive Cancer Network (NCCN) guidelines recommend the following for patients who opt not to undergo RRSO and patients for whom the period until RRSO is long: commence surveillance via transvaginal ultrasound and serum CA 125 assessment from 35 years of age or 5–10 years before the earliest age of ovarian cancer diagnosis within the patient’s family. However, there is no clear evidence to support these recommendations, and under such circumstances, attention has been recently drawn to RRSO, which actually helps prevent ovarian cancer onset. Many reports have described the effect of RRSO on lowering the risk of ovarian cancer onset in patients harboring BRCA gene variant; in a meta-analysis of 2840 individuals harboring BRCA gene variants, it was found that the risk of ovarian cancer onset (including fallopian tube cancer and peritoneal carcinoma) was reduced by 79% following RRSO [10]. Furthermore, RRSO reportedly increases the overall survival rate and reduces the risk of onset of breast cancer and high-grade serous carcinoma (HGSC) [11]; thus, prophylactic treatment with RRSO is the most effective option for patients with HBOC. However, there are contradictory reports negating the effects of RRSO in reducing the risk of breast cancer onset [12]. Conversely, it has been reported that the probability of peritoneal carcinoma development following RRSO is 0.3% [13]; thus, surveillance for peritoneal carcinoma is necessary even after undergoing RRSO.
12.2 Standard RRSO Procedure
From the perspective of healthy organ resection, it is preferable to perform minimally invasive surgery. Reportedly, epithelial ovarian cancer, fallopian tube cancer, and peritoneal carcinoma are detected from RRSO specimens in 2.2–4.6% cases [10, 14,15,16], and if peritoneal findings are observed while performing RRSO, thorough observation of the peritoneal cavity, peritoneal lavage cytology, and biopsy must be performed. Although there are no reports of ovarian cancer developing from the residual ovary following oophorectomy among individuals harboring BRCA variants, there are reports of benign illness [17]; therefore, care must be taken to achieve total removal of the ovary or ovaries. In a prospective study of 20 patients whose uterine specimens were pathologically examined upon the excision of the fallopian tubes at the uterine horns using a procedure resembling RRSO, residual fallopian tubes with a median length of 6 mm and median surface area of 14 mm2 were found at 29 out of 40 uterine horn sites (73%) [18]. Considering these reports, the following recommendations are suggested for performing RRSO [19,20,21]:
-
Perform minimally invasive surgery (laparoscopy).
-
Observe upper abdomen, bowel surface, greater momentum, appendix, and pelvic organs, and if peritoneal findings are present, perform a biopsy.
-
Obtain pelvic washing for cytology.
-
Surgically remove 2 cm of proximal ovarian the suspensory ligament, the entire fallopian tube up to cornua, the entire peritoneum covering the ovary and fallopian tube, and particularly, the peritoneum beneath adhesions between the fallopian tube and ovary and the pelvic wall.
-
To avoid cell loss caused by operative manipulations, minimize manipulations of the fallopian tube and ovary.
-
Collect resected specimens from within the peritoneal cavity using an endobag.
12.3 Surgical Options when Performing RRSO: Concurrent Hysterectomy and Two-Stage Surgery
The suitability of concurrent hysterectomy during RRSO has long been an ongoing debate [19, 22] and remains controversial. It is thought that concurrent hysterectomy is advantageous during hormone therapy for breast cancer and hormone replacement therapy (HRT) such as that for ovarian deficiency syndrome [23, 24]. In a prospective cohort study of 1083 individuals harboring BRCA variants who underwent RRSO only, uterine cancer developed in eight individuals during the median follow-up period of 5.1 years, with there being no clear increase in the observed risk following RRSO [25]. Conversely, in individuals harboring BRCA1 gene variants, the risk of uterine body serous cancer increased (0.18 expected [O:E ratio, 22.2; 95% CI, 6.1–56.9; P < 0.001]). Reportedly, in women aged 40 years, longer overall survival (4.9 months) with higher cost-effectiveness was observed among those who underwent RRSO and total hysterectomy than among those who underwent RRSO alone [26]. Therefore, the advantages and disadvantages of performing concurrent hysterectomy should be fully explained preoperatively.
RRSO is recommended at the end of childbirth between the age of 35 and 40 years or at the earliest age of ovarian cancer onset among individuals in the patient’s family [27]. It is considered to delay RRSO until age 40–45 years in patients with BRCA2 variant [27]; however, it has been reported that performing RRSO in women of reproductive age results in surgical menopause and increases the risk of osteoporosis, coronary heart disease, and cognitive dysfunction, which shortens the survival period compared with that among women who experience natural menopause [28]. Therefore, we examined two-stage prophylactic salpingectomy with delayed oophorectomy, whereby risk-reducing salpingectomy alone is performed while ovarian function is still present and risk-reducing oophorectomy is performed at menopause. Based on the report indicating that HGSC originates from the fallopian tube epithelium [29], HGSC occurrence in the fallopian tube is prevented by surgically removing the fallopian tubes, thereby preserving the ovaries and avoiding surgical menopause. While the aim is to prevent HGSC originating in the fallopian tubes and avoid premature menopause, outcomes such as the remaining risk of ovarian cancer and the impact on breast cancer have not been fully elucidated; thus, two-stage surgery is not recommended at this stage, and the results of ongoing current clinical trials are awaited.
12.4 Pathological Examination of RRSO Samples
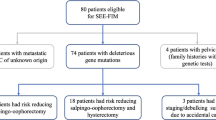
During postoperative pathological examination, due caution must be exercised to detect minute ovarian cancers, which cannot be detected on preoperative evaluation, and occult cancers, which are STIC lesions of the fallopian tubes [16, 30, 31]. Regarding the histopathological diagnosis of RRSO-resected specimens, pathological examination is inadequate to detect occult cancer in cases of benign illness. Therefore, it is preferable to perform diagnosis after preparing specimens in accordance with the SEE-FIM protocol, whereby the fimbriae of the fallopian tubes are sectioned longitudinally and slices of the ovaries and fallopian tubes are prepared at 2–3-mm intervals and evaluated as serial sections [32]. At institutions that provide genetic counseling and have a collaboration system with pathologists, it is recommended that gynecologic oncologists perform RRSO in cooperation with clinical genetic specialists [16].
12.5 Post-RRSO Health Care
Care should be paid to various conditions that might arise following RRSO, such as climacteric disturbance, dyslipidemia, and osteoporosis (seen after natural menopause) as well as severe urogenital symptoms and psychological and/or somatovegetative symptoms seen in young women who undergo RRSO prior to natural menopause [33]. In particular, in many cases, ovarian dysfunction symptoms following RRSO such as palpitations, constipation, and shoulder stiffness are observed to be more severe compared with those observed after natural menopause [34]; moreover, sexuality can be disturbed [35]. Furthermore, regarding lipid profile and cardiovascular illness, high total cholesterol levels and metabolic syndrome are more common in women who have undergone RRSO [36, 37]. Regarding bone mass, it is unlikely that RRSO decreases bone mass and increases the incidence of bone fractures compared with natural menopause [34]. However, it has been reported that following RRSO, women experience reduced bone mass postoperatively from an earlier age while they are still young and bone mass decreases more rapidly after surgical menopause than after natural menopause [38]. For these reasons, regular assessment of patient’s bone mass is important during postoperative follow-up. Health care following RRSO includes traditional Chinese medicine for ovarian insufficiency, statin therapy for dyslipidemia, and administration of calcium and bisphosphonate preparations for osteoporosis; however, HRT is considered for women with no history of breast cancer. HRT has been found to improve sexuality in women after RRSO [39, 40] and is useful for maintaining cognitive function for up to 45 years after RRSO [41]. Conversely, women harboring BRCA variant are at a high risk for breast cancer onset; therefore, risk elevation owing to HRT is a cause for concern among women in general. However, in a recent meta-analysis, HRT following RRSO was not found to increase the risk of breast cancer [42], and it is considered that HRT does not increase this risk in a short period [43].
12.6 Current State of RRSO and Future Prospects
The state of implementation of risk-reducing surgery differs between the Western and Asian countries. Reportedly, the proportion of individuals harboring a BRCA1/BRCA 2 gene variant who have undergone RRSO ranges from 10% to 78% in the Western countries and an overwhelming majority of women (86.4%–97%) were satisfied with the decision to undergo surgery [44]. The results of this study showed that RRSO has gained popularity as an option among Western patients. Conversely, the number of studies including Asian patients is limited, and in a recent Japanese study including 488 individuals diagnosed with HBOC, it was reported that of all the participants, 153 (31.4%) underwent RRSO; however, the RRSO implementation rate is lower in Japan than in the Western countries, and its use is less widespread in Japan [45]. This is due to the fact that, in Japan, a limited number of institutions perform genetic screening for BRCA1/BRCA2 and that RRSO has not gained popularity as it is not covered by public health insurance; moreover, medical staff still have insufficient knowledge and experience for performing genetic diagnosis [46]. There have been several events that drew public attention to HBOC in Korea. First, the Korean Hereditary Breast Cancer Study was started in 2007 with support from the Ministry of Health and Welfare of Korea and the Korean Breast Cancer Society [47]. Second, the strategy of BRCA testing coverage by the National Health Insurance system was promoted in May 2012. Later, American actress Angelina Jolie announced that she harbored the BRCA1 gene variant and had undergone bilateral risk-reducing mastectomy, which subsequently drew increased attention to risk-reducing surgery. This has been called the “Angelina effect.” Following her disclosure, the rate of risk-reducing surgery increased from RRSO performed in 27 patients at 25 institutions in 2009 to 75 patients at 27 institutions in 2015 [48]. In Japan, RRSO has been covered under insurance for HBOC patients with a history of breast cancer since April 2020 and is expected to gain popularity in future. Conversely, the peak age for undergoing RRSO has been delayed to the late 40s or older in Japan [31, 45]; thus, some individuals develop occult cancer by the time of surgery, and consequently, the original role of RRSO, i.e., primary prevention, cannot be achieved. We must reconfirm the role of RRSO and firmly bear in mind that RRSO should be performed at the recommended appropriate time. Furthermore, more number of individuals are expected to undergo RRSO in future. Apart from BRCA, there are genes that cause HBOC, and because BRIP1 [49], RAD51C [50], and RAD51D [51] increase the risk of ovarian cancer onset, RRSO should be considered at 45–50 years of age [27]. Other genes that might increase the risk of ovarian cancer onset include ATM [52] and PALB2 [53]; however, further study is needed to determine whether RRSO should be performed in patients harboring these genes [27].
References
Kuchenbaecker KB, Hopper JL, Barnes DR, Phillips KA, Mooij TM, Roos-Blom MJ, et al. Risks of breast, ovarian, and contralateral breast cancer for BRCA1 and BRCA2 mutation carriers. JAMA. 2017;317(23):2402–16.
Iodice S, Barile M, Rotmensz N, Feroce I, Bonanni B, Radice P, et al. Oral contraceptive use and breast or ovarian cancer risk in BRCA1/2 carriers: a meta-analysis. Eur J Cancer. 2010;46(12):2275–84.
Anothaisintawee T, Wiratkapun C, Lerdsitthichai P, Kasamesup V, Wongwaisayawan S, Srinakarin J, et al. Risk factors of breast cancer: a systematic review and meta-analysis. Asia Pac J Public Health. 2013;25(5):368–87.
Gierisch JM, Coeytaux RR, Urrutia RP, Havrilesky LJ, Moorman PG, Lowery WJ, et al. Oral contraceptive use and risk of breast, cervical, colorectal, and endometrial cancers: a systematic review. Cancer Epidemiol Biomark Prev. 2013;22(11):1931–43.
Mørch LS, Skovlund CW, Hannaford PC, Iversen L, Fielding S, Lidegaard Ø. Contemporary hormonal contraception and the risk of breast cancer. N Engl J Med. 2017;377(23):2228–39.
Ichida M, Kataoka A, Tsushima R, Taguchi T. No increase in breast cancer risk in Japanese women taking oral contraceptives: a case-control study investigating reproductive, menstrual and familial risk factors for breast cancer. Asian Pac J Cancer Prev. 2015;16(9):3685–90.
Kawai M, Minami Y, Kuriyama S, Kakizaki M, Kakugawa Y, Nishino Y, et al. Reproductive factors, exogenous female hormone use and breast cancer risk in Japanese: the Miyagi cohort study. Cancer Causes Control. 2010;21(1):135–45.
Buys SS, Partridge E, Black A, Johnson CC, Lamerato L, Isaacs C, et al. Effect of screening on ovarian cancer mortality: the prostate, lung, colorectal and ovarian (PLCO) cancer screening randomized controlled trial. JAMA. 2011;305(22):2295–303.
Evans DG, Gaarenstroom KN, Stirling D, Shenton A, Maehle L, Dørum A, et al. Screening for familial ovarian cancer: poor survival of BRCA1/2 related cancers. J Med Genet. 2009;46(9):593–7.
Rebbeck TR, Kauff ND, Domchek SM. Meta-analysis of risk reduction estimates associated with risk-reducing salpingo-oophorectomy in BRCA1 or BRCA2 mutation carriers. J Natl Cancer Inst. 2009;101(2):80–7.
Eleje GU, Eke AC, Ezebialu IU, Ikechebelu JI, Ugwu EO, Okonkwo OO. Risk-reducing bilateral salpingo-oophorectomy in women with BRCA1 or BRCA2 mutations. Cochrane Database Syst Rev. 2018;8(8):Cd012464.
Heemskerk-Gerritsen BA, Seynaeve C, van Asperen CJ, Ausems MG, Collée JM, van Doorn HC, et al. Breast cancer risk after salpingo-oophorectomy in healthy BRCA1/2 mutation carriers: revisiting the evidence for risk reduction. J Natl Cancer Inst. 2015;107(5)
Domchek SM, Friebel TM, Singer CF, Evans DG, Lynch HT, Isaacs C, et al. Association of risk-reducing surgery in BRCA1 or BRCA2 mutation carriers with cancer risk and mortality. JAMA. 2010;304(9):967–75.
Rebbeck TR, Lynch HT, Neuhausen SL, Narod SA, Van't Veer L, Garber JE, et al. Prophylactic oophorectomy in carriers of BRCA1 or BRCA2 mutations. N Engl J Med. 2002;346(21):1616–22.
Finch A, Beiner M, Lubinski J, Lynch HT, Moller P, Rosen B, et al. Salpingo-oophorectomy and the risk of ovarian, fallopian tube, and peritoneal cancers in women with a BRCA1 or BRCA2 mutation. JAMA. 2006;296(2):185–92.
Sherman ME, Piedmonte M, Mai PL, Ioffe OB, Ronnett BM, Van Le L, et al. Pathologic findings at risk-reducing salpingo-oophorectomy: primary results from gynecologic oncology group trial GOG-0199. J Clin Oncol. 2014;32(29):3275–83.
Donnez O, Squifflet J, Marbaix E, Jadoul P, Donnez J. Primary ovarian adenocarcinoma developing in ovarian remnant tissue ten years after laparoscopic hysterectomy and bilateral salpingo-oophorectomy for endometriosis. J Minim Invasive Gynecol. 2007;14(6):752–7.
Cass I, Walts A, Karlan BY. Does risk-reducing bilateral salpingo-oophorectomy leave behind residual tube? Gynecol Oncol. 2010;117(1):27–31.
Kauff ND, Barakat RR. Risk-reducing salpingo-oophorectomy in patients with germline mutations in BRCA1 or BRCA2. J Clin Oncol. 2007;25(20):2921–7.
Powell CB, Chen LM, McLennan J, Crawford B, Zaloudek C, Rabban JT, et al. Risk-reducing salpingo-oophorectomy (RRSO) in BRCA mutation carriers: experience with a consecutive series of 111 patients using a standardized surgical-pathological protocol. Int J Gynecol Cancer. 2011;21(5):846–51.
National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology. Ovarian cancer including fallopian tube cancer and primary peritoneal cancer, ver1. 2020. Accessed Sep 30, 2020.
Practice Bulletin No ACOG. 103: hereditary breast and ovarian cancer syndrome. Obstet Gynecol. 2009;113(4):957–66.
Segev Y, Iqbal J, Lubinski J, Gronwald J, Lynch HT, Moller P, et al. The incidence of endometrial cancer in women with BRCA1 and BRCA2 mutations: an international prospective cohort study. Gynecol Oncol. 2013;130(1):127–31.
Segev Y, Rosen B, Lubinski J, Gronwald J, Lynch HT, Moller P, et al. Risk factors for endometrial cancer among women with a BRCA1 or BRCA2 mutation: a case control study. Familial Cancer. 2015;14(3):383–91.
Shu CA, Pike MC, Jotwani AR, Friebel TM, Soslow RA, Levine DA, et al. Uterine cancer after risk-reducing Salpingo-oophorectomy without hysterectomy in women with BRCA mutations. JAMA Oncol. 2016;2(11):1434–40.
Havrilesky LJ, Moss HA, Chino J, Myers ER, Kauff ND. Mortality reduction and cost-effectiveness of performing hysterectomy at the time of risk-reducing salpingo-oophorectomy for prophylaxis against serous/serous-like uterine cancers in BRCA1 mutation carriers. Gynecol Oncol. 2017;145(3):549–54.
National Comprehensive Cancer Network. NCCN clinical practice guidelines in oncology. Genetic/Familial high-risk assessment: breast, Ovarian, and Pancreatic, ver1. 2020. Accessed Sep 30, 2020.
Gaba F, Manchanda R. Systematic review of acceptability, cardiovascular, neurological, bone health and HRT outcomes following risk reducing surgery in BRCA carriers. Best Pract Res Clin Obstet Gynaecol. 2020;65:46–65.
Reitsma W, de Bock GH, Oosterwijk JC, Bart J, Hollema H, Mourits MJ. Support of the ‘fallopian tube hypothesis’ in a prospective series of risk-reducing salpingo-oophorectomy specimens. Eur J Cancer. 2013;49(1):132–41.
Zakhour M, Danovitch Y, Lester J, Rimel BJ, Walsh CS, Li AJ, et al. Occult and subsequent cancer incidence following risk-reducing surgery in BRCA mutation carriers. Gynecol Oncol. 2016;143(2):231–5.
Kobayashi Y, Hirasawa A, Chiyoda T, Ueki A, Masuda K, Misu K, et al. Retrospective evaluation of risk-reducing salpingo-oophorectomy for BRCA1/2 pathogenic variant carriers among a cohort study in a single institution. Jpn J Clin Oncol 2020.
Cheng A, Li L, Wu M, Lang J. Pathological findings following risk-reducing salpingo-oophorectomy in BRCA mutation carriers: a systematic review and meta-analysis. Eur J Surg Oncol. 2020;46(1):139–47.
Stuursma A, van Driel CMG, Wessels NJ, de Bock GH, Mourits MJE. Severity and duration of menopausal symptoms after risk-reducing salpingo-oophorectomy. Maturitas. 2018;111:69–76.
Vermeulen RFM, Beurden MV, Korse CM, Kenter GG. Impact of risk-reducing salpingo-oophorectomy in premenopausal women. Climacteric. 2017;20(3):212–21.
Tucker PE, Cohen PA. Review article: sexuality and risk-reducing Salpingo-oophorectomy. Int J Gynecol Cancer. 2017;27(4):847–52.
Michelsen TM, Tonstad S, Pripp AH, Tropé CG, Dørum A. Coronary heart disease risk profile in women who underwent salpingo-oophorectomy to prevent hereditary breast ovarian cancer. Int J Gynecol Cancer. 2010;20(2):233–9.
Michelsen TM, Pripp AH, Tonstad S, Tropé CG, Dørum A. Metabolic syndrome after risk-reducing salpingo-oophorectomy in women at high risk for hereditary breast ovarian cancer: a controlled observational study. Eur J Cancer. 2009;45(1):82–9.
Ozdemir S, Celik C, Görkemli H, Kiyici A, Kaya B. Compared effects of surgical and natural menopause on climacteric symptoms, osteoporosis, and metabolic syndrome. Int J Gynaecol Obstet. 2009;106(1):57–61.
Johansen N, Liavaag AH, Tanbo TG, Dahl AA, Pripp AH, Michelsen TM. Sexual activity and functioning after risk-reducing salpingo-oophorectomy: impact of hormone replacement therapy. Gynecol Oncol. 2016;140(1):101–6.
Vermeulen RFM, Beurden MV, Kieffer JM, Bleiker EMA, Valdimarsdottir HB, Massuger L, et al. Hormone replacement therapy after risk-reducing salpingo-oophorectomy minimises endocrine and sexual problems: a prospective study. Eur J Cancer. 2017;84:159–67.
Rocca WA, Bower JH, Maraganore DM, Ahlskog JE, Grossardt BR, de Andrade M, et al. Increased risk of cognitive impairment or dementia in women who underwent oophorectomy before menopause. Neurology. 2007;69(11):1074–83.
Marchetti C, De Felice F, Boccia S, Sassu C, Di Donato V, Perniola G, et al. Hormone replacement therapy after prophylactic risk-reducing salpingo-oophorectomy and breast cancer risk in BRCA1 and BRCA2 mutation carriers: a meta-analysis. Crit Rev Oncol Hematol. 2018;132:111–5.
Vermeulen RFM, Korse CM, Kenter GG, Brood-van Zanten MMA, Beurden MV. Safety of hormone replacement therapy following risk-reducing salpingo-oophorectomy: systematic review of literature and guidelines. Climacteric. 2019;22(4):352–60.
Miller SM, Roussi P, Daly MB, Scarpato J. New strategies in ovarian cancer: uptake and experience of women at high risk of ovarian cancer who are considering risk-reducing salpingo-oophorectomy. Clin Cancer Res. 2010;16(21):5094–106.
Nomura H, Sekine M, Yokoyama S, Arai M, Enomoto T, Takeshima N, et al. Clinical background and outcomes of risk-reducing salpingo-oophorectomy for hereditary breast and ovarian cancers in Japan. Int J Clin Oncol. 2019;24(9):1105–10.
Hirasawa A, Masuda K, Akahane T, Tsuruta T, Banno K, Makita K, et al. Experience of risk-reducing salpingo-oophorectomy for a BRCA1 mutation carrier and establishment of a system performing a preventive surgery for hereditary breast and ovarian cancer syndrome in Japan: our challenges for the future. Jpn J Clin Oncol. 2013;43(5):515–9.
Han SA, Park SK, Ahn SH, Lee MH, Noh DY, Kim LS, et al. The Korean hereditary breast cancer (KOHBRA) study: protocols and interim report. Clin Oncol (R Coll Radiol). 2011;23(7):434–41.
Lee J, Kim S, Kang E, Park S, Kim Z, Lee MH. Influence of the Angelina Jolie announcement and insurance reimbursement on Practice patterns for hereditary breast cancer. J Breast Cancer. 2017;20(2):203–7.
Ramus SJ, Song H, Dicks E, Tyrer JP, Rosenthal AN, Intermaggio MP, et al. Germline mutations in the BRIP1, BARD1, PALB2, and NBN genes in women with ovarian cancer. J Natl Cancer Inst. 2015;107(11).
Loveday C, Turnbull C, Ruark E, Xicola RM, Ramsay E, Hughes D, et al. Germline RAD51C mutations confer susceptibility to ovarian cancer. Nat Genet. 2012;44(5):475–6. author reply 6
Loveday C, Turnbull C, Ramsay E, Hughes D, Ruark E, Frankum JR, et al. Germline mutations in RAD51D confer susceptibility to ovarian cancer. Nat Genet. 2011;43(9):879–82.
Lilyquist J, LaDuca H, Polley E, Davis BT, Shimelis H, Hu C, et al. Frequency of mutations in a large series of clinically ascertained ovarian cancer cases tested on multi-gene panels compared to reference controls. Gynecol Oncol. 2017;147(2):375–80.
Norquist BM, Harrell MI, Brady MF, Walsh T, Lee MK, Gulsuner S, et al. Inherited mutations in women with ovarian carcinoma. JAMA Oncol. 2016;2(4):482–90.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Kobayashi, Y., Aoki, D. (2021). Risk-Reducing Salpingo-oophorectomy (RRSO). In: Nakamura, S., Aoki, D., Miki, Y. (eds) Hereditary Breast and Ovarian Cancer . Springer, Singapore. https://doi.org/10.1007/978-981-16-4521-1_12
Download citation
DOI: https://doi.org/10.1007/978-981-16-4521-1_12
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-16-4520-4
Online ISBN: 978-981-16-4521-1
eBook Packages: MedicineMedicine (R0)