Abstract
The preterm babies with retinopathy of prematurity (ROP) can have poor visual prognosis if not treated early. Presence of cataract in these babies may further delay proper screening and adequate treatment. Also, cataract can develop post-treatment for ROP, making follow-up assessment of disease activity difficult. Amblyopia is another important component to be addressed in these small individuals. This chapter highlights the different aspects of cataract in a ROP case including the causes, pathophysiology, types, and management. The preoperative workup, intraoperative challenges and postoperative care required in such babies is discussed.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- retinopathy of prematurity(ROP)
- Complicated cataract
- Steroid-induced cataract
- Cryotherapy
- Laser
- Thermal injury
- Tunica Vasculosa Lentis (TVL)
- aggressive posterior ROP (APROP)
- Anterior segment ischemia
- Uveal effusion
- Post-injection
- anti-VEGF
- Post-surgery
- YAG capsulotomy
- Coats Disease
- Persistent Hyperplastic Primary Vitreous (PHPV)
- Hereditary Syndromes
- Ocular Trauma
- Ocular tumor
1 Introduction
Preterm babies with retinopathy of prematurity (ROP) can have poor visual prognosis if not treated early. Presence of cataract in these individuals may further delay proper screening and adequate treatment. Cataract can also develop post-treatment for ROP, making follow-up assessment of disease activity difficult. Amblyopia is another important component to be addressed in these small individuals. This chapter highlights the different aspects of cataract in a ROP case including the causes, pathophysiology, types, and management. The preoperative workup, intraoperative challenges and postoperative care required in such babies is discussed.
2 Epidemiology
Cataract is defined as any opacity in the lens and prevalence of 1.2–6 cases per 10,000 infants [1]. The normal development of fetus occurs up to 40 weeks gestational age (GA). Those babies born before 34 weeks gestational age, having birth weight less than 1750 g and those >34 weeks GA or >1750 g with high-risk factors are at risk for retinopathy of prematurity (ROP) and hence screened [2]. The incidence of ROP in these preterm babies has increased due to an increased survival rate of preterm and poor health care regulations regarding neonatal care and screening guidelines. These preterm low birth weight babies are also at risk to have cataract and an incidence of 0.97–1.9% is seen in these preterms [3, 4]. These lenticular opacities can lead to difficulty in assessment of the posterior segment status and management of same.
3 Type of Cataract
The different morphologies of cataract seen in preterm babies include [3, 5,6,7,8,9]:
-
1.
Focal opacities either punctate or vacuolated—These are usually transient, visually insignificantly and resolve spontaneously. Seen in approximately 2.7% of low birth weight infants [10, 11](Fig. 16.1)
-
2.
Zonular cataract
-
3.
Total cataract (Fig. 16.2)
-
4.
Anterior or posterior subcapsular cataract
-
5.
Complicated cataract—Seen as posterior subcapsular cataract with polychromatic luster or partially absorbed membranous cataract. Usually associated with retinal detachment.
4 Causes
Infantile cataract can develop due to intrauterine infections, drug-related, metabolic disorders, or inherited disorders. While many of these cases are bilateral, asymmetrical presentation is also commonly seen [1, 12]. In a premature child, cataract can form because of the systemic status, retinopathy of prematurity or due to treatment of same. Cataract development is seen at different duration ranging from 10 days to 13 months in laser-treated and 2 months to 5.6 years in post-vitrectomised eyes [3, 4, 13,14,15]. Pathophysiology of cataract in ROP can be divided according to the etiology:
-
1.
Systemic factors
The preterm babies are at risk of metabolic acidosis and sepsis during their NICU stay. These factors can lead to osmotic changes in the lens leading to development of cataract. The usual form seen is the bilateral clear vacuoles formation along the apices of posterior lens surface. These are transient and mostly clears over the course of several months but can progress to total opacification in some cases [1, 4, 10, 11].
-
2.
Complicated cataract
Complicated cataract is seen in those associated with retinal detachment, mostly in cases with advanced stage retinopathy [16]. It may present as posterior subcapsular cataract or partially absorbed membranous cataract.
-
3.
Posttreatment
Cataract in preterm child may or may not be associated with systemic treatment and ocular management [4, 8, 15]. The actual incidence of the same in retinopathy of prematurity may be less reported.
-
(a)
Steroid-induced cataract: Though long-term steroids are known to cause cataract, there are no reports of steroid-induced cataract in preterm babies.
-
(b)
Cryotherapy
Cryotherapy was previously used as a treatment for threshold ROP. It can cause more inflammation due to blood-retinal barrier breakdown. But cataract was not seen as a major complication in various studies [17,18,19].
-
(c)
Laser
Laser is preferred over cryotherapy because of lesser complications of pain, adnexal edema, exudative retinal detachment, vitreoretinal traction, and vitreous hemorrhage. The incidence of cataract in laser-treated ROP ranges from 0.003 to 6% [4, 15, 20,21,22,23]. The type of laser used in treatment of ROP includes argon, diode and df-NdYAG laser. Argon laser had higher association with cataract among them [15, 24]. Prominent anterior vasculosa lentis, inadvertent burns placed on the iris or ciliary body and confluent laser therapy are the risk factors for cataract formation post-laser in a preterm baby. Following mechanisms play a role:
-
Thermal injury
The total amount of laser energy used depends on the type, power, duration of laser and number of laser spots. Lens protein and hemoglobin absorbs the energy of laser. This is especially important in case of persistent tunica vasculosa lentis (TVL), commonly present in preterm babies [20]. The incidence of cataract is lower in cases with diode laser energy as longer wavelength energy (810 nm) is lesser absorbed by hemoglobin as compared to argon laser [25]. However, some studies have found no correlation between development of cataract and energy of the laser used [4].
-
Tunica Vasculosa Lentis (TVL)
Premature infants have some amount of intact TVL. The hemoglobin absorbs laser energy at the lens surface leading to alteration in permeability of lens anterior capsule. This further affects the osmotic balance and leads to formation of cataract. In a very premature child, the disease may present in more aggressive form like aggressive posterior ROP (APROP) which has iris neovascularization with poor pupillary dilatation, hazy vitreous and severe plus disease. These cases require higher power, duration and more laser leading to higher energy being used, further increasing the risk. But studies have also shown similar incidence of cataract in ROP cases not having prominent TVL indicating other factors also do play a role [20, 21].
-
Anterior segment ischemia
The anterior segment of the eye is supplied by the anastomosis of anterior ciliary artery (ACA) and long posterior ciliary artery (LPCA). Damage to the LPCA can lead to anterior segment ischemia [26]. It can present as congestion, corneal edema, shallow anterior chamber, hyphema, cataract, posterior synechiae in the acute phase and hypotony, iris atrophy, ciliary body atrophy in the late phase. Some of these eyes do progress to phthisis bulbi [26, 27].
-
Uveal effusion
The higher amount of thermal energy and the immature blood-retinal barrier puts the baby at higher risk of uveal effusion. It can lead to anterior rotation of ciliary body and shallow anterior chamber which may cause corneo-lenticular apposition and cataract formation [25].
-
-
(d)
Post-injection
In adults, cataract incidence varies in cases receiving intravitreal anti-VEGF [28, 29]. VEGF is an important molecule involved in the cascade of events in ROP. It is one of the factors involved in both angiogenesis and vasculogenesis phase. The use of intravitreal anti-VEGF in ROP allows for fast disease regression and improved vascular re-growth. This allows for a better field of vision but various regression patterns including vascular arrest along with high risk of recurrence is noted [23, 30, 31].
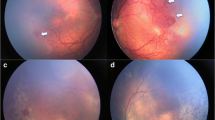
Cataract in anti-VEGF most commonly occurs due to the lens injury. In preterm babies, the lens is thicker as compared to other ocular structures and the pars plana is also not formed [32, 33]. Hence, if one is not familiar with the anatomy of these small eyes, there is a higher chance of mechanical lens injury. The injection in these children is usually given at 1.75 mm from the limbus with the needle tip directed posteriorly towards the optic disc. But, there have been reports of cataract formation in post-intravitreal anti-VEGF with no lens injury documented, which could be probably relate to the molecule itself (Figs. 16.3 and 16.4). Preexisting dehiscence of the posterior capsule has also been suspected [9]. Also until now, there is no level I evidence of the ocular, visual, systemic and neurodevelopmental safety profile of anti-VEGF in these babies.
-
(e)
Post-surgery
Stage 4 or 5 ROP can be associated with cataract or the retina can be near the posterior capsule which may necessitate lensectomy along with vitrectomy to achieve optimal results. Cataract formation after lens sparing vitrectomy for ROP surgery can occur but is less frequent as compared to pars plana vitrectomy in adults [3, 13, 14]. The lens retina approximation is one of the risk factors for cataract formation because of the probability of lens touch. The chemical changes also are known to occur with vitrectomy itself and depending on the type of tamponade agent used.
-
(a)
Same patient as Fig. 16.3, developed bilateral total cataract OD&OS 6 weeks after anti-VEGF administration
5 Management
Treatment of ROP is important and first priority as early intervention in these cases can prevent adverse outcomes. Obscuration of posterior segment visualization by cataract can preclude the screening and management of these cases. Hence, the need to manage cataract as soon as possible is essential to allow intervention for the posterior segment, monitor the disease and prevent amblyopia. As discussed, lensectomy might be required in addition to vitrectomy in some cases of stage 4 and stage 5 ROP, where the lens is cataractous or the retina is in close approximation with the lens. In cases where retina is hazily seen allowing staging of the disease but laser could not be performed, early cataract surgery is required for management of the posterior segment and prevent progression of ROP.
5.1 Preoperative Challenges
Pediatric cataract surgery is challenging in terms of smaller eye with lesser scleral rigidity, higher elasticity of anterior capsule, and steeper anterior curvature of lens. The anterior segment in a preterm child is further different from a normal child eye in terms of steeper cornea, shallow anterior chamber, more anteriorly inserted iris, thicker and more spherical lens [33, 34]. Further these parameters may vary with spontaneously regressed and laser-treated ROP. These differences not only pose intraoperative challenges but also affect the pattern of ocular growth [5, 33, 35,36,37,38]. This has a significant effect on the selection of appropriate intraocular lens power and the amount of under-correction required in these babies. Poor pupillary dilatation can further create problems during surgery.
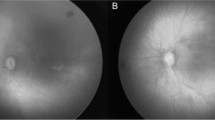
Tropicamide (0.5%) and phenylephrine (2.5%) combination is used for dilatation in these preterm babies. As used for ROP screening, the drops should be instilled two times 10 min apart half an hour before the surgery. In cases with APROP, neovascularization of iris is often present. This causes non-dilation of the pupil, difficulty in visualization of lens status and posterior segment, and risk of bleeding. These cases are also at risk of having postoperative inflammation, posterior synechiae and visual axis opacification (VAO). Also, the posterior segment in these cases needs urgent treatment to avoid further complications leading to poor visual prognosis. Preoperative B-scan imaging is important to rule out the possibility of retinal detachment in cases where posterior segment is not visible. Preoperative ultrasound biomicroscopy (UBM) can help us to determine the area of the posterior synechiae, whether the posterior iris has adhered to anterior capsule, the status of the posterior capsule for presence of any preexisting posterior capsular defects and the sulcus to sulcus diameter (Fig. 16.2). The preoperative detection of preexisting posterior capsular defect can help one to anticipate complications and take necessary steps to prevent them. In APROP cases with severe neovascularization in absence of retinal detachment, intravitreal anti-VEGF before cataract surgery may help in the regression of the neovascularization. This decreases the risk of bleeding and allows dilatation of the pupil. All the challenges including posterior segment status, treatment required, amblyopia therapy, prognosis, need for postoperative care, refractive correction, and complications associated should be explained to the parents/caregivers.
5.2 Intraoperative Challenges
-
Approach and dilatation
The preferable approach in preterm babies is superior corneal incision as with other pediatric cases. The superior wound is covered with the upper eyelid and hence is at lesser risk of trauma and exposure, thereby decreasing the risk of infection. Pupillary miosis and posterior synechiae can be present especially in cases with advanced ROP or APROP. The use of high-density viscocohesive like Healon-GV is preferred to maintain the anterior chamber and have minimum fluctuations in anterior chamber. The synechiae could be initially released to assess pupillary dilatation. In case of non-dilating pupil, various maneuvers like mechanical stretching, sphincterotomy, and use of mechanical devices like iris hooks can be tried. The use of other mechanical devices like the Malyugin ring in such small eyes is not preferable due to lesser space for maneuvering these devices.
-
Anterior capsulorhexis and lens aspiration:
The anterior capsule can be stained using 0.06% Trypan Blue dye to visualize it. Trypan blue dye is known to have biochemical effects on the lens capsule, decreasing its elasticity [39]. The anterior continuous capsulorhexis (ACC) can be started with the capsulotomy 26 Gauge needle and further performed using capsulorhexis forceps. The forceps allow for controlled maneuvering of the elastic capsule. But before starting the anterior chamber should be formed with high-density viscocohesive substance like Healon-GV which would allow minimum fluctuation in anterior chamber and flatten the anterior capsule in the center. Appropriate size of the ACC is approximately 5 mm. The use of Callisto guided marking system can help us in this aspect. The lens aspiration can be performed using bimanual technique which allows complete removal of the lens matter without undue stress on the bag. Any residual lens matter could lead to excess inflammation in these pediatric cases and hence preferably be avoided.
-
Posterior capsulorhexis, vitrectomy and fundus examination
A posterior continuous capsulorhexis (PCC) can be made after partially filling the posterior chamber with high-density viscocohesive. Complete fill should be avoided as these may lead to increased bowing of the posterior capsule causing increasing angulation of the instrument leading to difficult maneuvering. Also, there is an increase in the pressure on the posterior capsule especially at the posterior-most point creating a high risk of irregular extension. The PCC is performed with capsulorhexis forceps after initiation with a capsulotomy needle (Fig. 16.3a). This is followed by anterior vitrectomy (AV). The anterior vitrectomy as in other pediatric cataract cases should cover beyond the margin and 2 mm deeper from the posterior capsule. A complete anterior vitrectomy and PCC reduces the chances of postoperative posterior capsular opacification (PCO) significantly [40, 41]. However, caution must be exercised and overzealous anterior vitrectomy beyond the margins should be avoided as these cases may have peripheral vitreoretinal traction. The posterior segment can be visualized at this stage using endoilluminator and wide-angle retinal lens (Fig. 16.3). The anterior chamber should be formed with viscoelastic before inserting the endoilluminator. This allows us to assess the status of optic disc, posterior pole and also the periphery. Hence, zone of vascularization, presence of ROP, stage, and presence of plus disease can be determined. This visualization helps in further management of the posterior segment as postoperative examination with speculum and indentation may not be possible in the initial 2 weeks considering the wound stability.
-
Intraocular lens (IOL)
Another question arises if the IOL can be placed, and if yes, what power to be used? The intraocular lens can be placed if the size of corneal diameter >9 mm, the sulcus to sulcus diameter >8 mm, axial length >17 mm and if no additional ocular features precluding the use of IOL are present. The type of IOL depends on the availability of sulcus. In cases where the anterior and posterior capsulorhexis is intact and well sized, the IOL can be placed in the bag while in compromised capsulorhexis, a multipiece IOL can be placed in the sulcus (Fig. 16.3b). Optic capture involves fixing the lens optic behind the posterior capsule while the haptics remains in place allowing better stabilization of the lens. In case of no capsular support, iris-fixated IOL or ACIOL can also be used. These ROP cases usually have myopia, thin sclera and retinal involvement. Hence, scleral fixated IOL are avoided. The IOL power in pediatric cases depends on the age of the patient at the time surgery, preoperative biometry and predicted postoperative change [12, 42]. Various formulae have been given over a period, but variance is seen more in children less than 2 years [42, 43]. Further, these preterm eyes will have more growth at a rapid rate initially as compared to normal eyes. The usual correlation between the axial length and refractive error is not seen in small preterm babies [13, 34]. Also, those treated with laser will have more axial length growth as compared to those treated with anti-VEGF or spontaneously regressed. These factors need to be taken into consideration as these cases may require more under-correction as compared to normal eyes.
Technique—A single piece hydrophobic acrylate IOL can be placed in the bag using proper technique if the criteria for IOL placement are fulfilled. A 3.5 mm incision allows easy insertion of injector without any undue pressure on the wound, thereby maintaining the anterior chamber. The anterior chamber and the intraocular bag should be adequately filled with viscocohesive substance. While injecting the IOL, the leading haptic should be placed against the posterior surface of the anterior capsule to avoid any unnecessary strain on posterior capsule and dislocation of the IOL into the vitreous cavity. The trailing haptic can be released in the pupillary plane and then tucked in the bag using a Sinskey hook. The viscoelastic should be completely removed and wound sutured using 10-0 monofilament nylon suture. In cases where IOL cannot be placed, secondary IOL can be planned after 2 years of age.
-
Intraoperative challenges in vitrectomized eyes:
Further cataract surgery in a vitrectomized eye would be moreover challenging [44, 45]. The loss of posterior support can lead to hypotony, zonular instability, complicated capsulorhexis, and damage to the posterior capsule. Zonular instability along with the increased iris lens diaphragm mobility may lead to anterior chamber depth fluctuation. In cases with lens touch or preexisting defect which may be detected on the UBM, there is risk of posterior dislocation of the lens fragments. The sudden collapse of the anterior chamber should be avoided at any step in these cases. The irrigation parameters to be kept on the lower side and the overfilling of AC with viscoelastic to be avoided. Hydrodelineation should be done gently while hydrodissection and lens rotation should be completely avoided [46]. The lens aspiration should be performed trying to maintain the posterior cortex which should be aspirated at the end. In case of a posterior capsular opening, it’s important not to panic and remove the instruments suddenly from the eye. The anterior chamber should be formed with a combination of Sodium hyaluronate 3.0%-Chondroitin sulfate 4.0% (Viscoat) before removing instruments. It coats the posterior capsular opening and prevents posterior dislocation of the lens matter. Lens matter in the anterior chamber can be removed using a vitreous cutter or wire vectis followed by complete anterior vitrectomy. Depending on the sulcus availability, a multipiece IOL can be placed. If the defect at the posterior capsule is small, it can be converted to PCC and a single piece IOL can be placed in the bag.
In cases with posteriorly dislocated lens fragments, depending on the amount, further approach can be decided. If the fragments size is small, it can be left as most of the time absorbs completely. Steroids may be required to avoid inflammation in these cases. If the fragments amount is large, a vitreoretinal surgeon may be called upon to remove it from the posterior segment. Simultaneous bilateral cataract surgery in one sitting is considered in small babies to avoid the risk of repeated anesthesia and the danger of developing amblyopia in case one eye is operated and the other could not be done due to systemic risk.
5.3 Postoperative
The postoperative complications of cataract surgery include inflammation, pupillary membrane formation, posterior synechiae, glaucoma, reproliferation of lens material, posterior capsule opacity, and retinal detachment. Postoperative treatment with topical cycloplegics and steroids is important. The severity of postoperative inflammation is higher in cases with iris neovascularization and those having posterior synechiae because of the iris manipulation and bleeding risk. Hence, topical steroids are required frequently and tapered slowly over a long period in these cases. This prevents the postoperative formation of posterior iris synechiae which may hamper visualization of the retina especially in the periphery and could lead to glaucoma.
Follow-up post cataract surgery should be synchronized with ROP monitoring and treatment to prevent unwanted outcomes. In children, refractive changes after cataract surgery are extensively studied and myopic shift is seen. This shift was more in younger children and aphakic eyes. Long-term refractive changes as previously described depends on various factors including gestational age, age of the child at the time of surgery, presence of ROP, type of treatment received and progression of myopia over a period [35,36,37,38, 42]. How much each of these factors contributes and affects the growth of the eyeball is unknown and still being studied. Hence, frequent refraction with appropriate correction glasses should be provided to avoid amblyopia. The glasses with appropriate fitting and counseling of the parents/caregivers to ensure use of glasses are needed.
Improvement in visual acuity and fixation is evident after cataract surgery in ROP cases but is limited because of the ocular morbidities (Table 16.1) [3, 6, 44, 47]. VAO is common after pediatric cataract surgery in children less than 1 year and depends whether PCCC and anterior vitrectomy is done or not [40, 48]. This can cause significant vision loss with risk of amblyopia. Hence, the importance of performing PCCC with anterior vitrectomy and to look for VAO in follow-up period [41]. To avoid VAO, PCCC should be done in all cases less than 6 years. Anterior vitrectomy to be done till 5 years of age. In older cases with mental retardation and those who cannot cooperate for slit lamp YAG capsulotomy, PCCC and anterior vitrectomy can be done [12]. Glaucoma is a common complication associated with both premature babies and pediatric cataract surgery [40, 49, 50]. The difference in the anterior segment of these individuals increases the risk of glaucoma [33]. Hence, the intraocular pressure and the optic disc cupping in these individuals should be monitored on follow-up. Retinal detachment (RD) is also one of the complications seen with pediatric cataract surgery and well documented after cataract surgery in adult ROP cases [6, 47, 51]. In preterm children with ROP, RD occurred in 3.5% of cases after cataract surgery [3]. It can occur in the preterm babies with progression of the ROP itself, and hence cannot be attributed to the cataract surgery alone. The ETROP study had 16% cases with RD after treatment by 9 months of the corrected age. Thus, the disease itself is at risk of progression even after treatment and good prognosis is obtained in stage 4 as compared to stage 5 ROP disease [13, 19]. Thus, these cases need a long-term follow-up for early detection of RD and intervention for the same.
Preterm children with cataract are at risk of vision loss because of various factors including retinal changes, glaucoma, and amblyopia. With an appropriate approach and combined effort of pediatrician, ophthalmologist, and anesthesiologist, early identification, prompt intervention, precise surgical techniques, proper counseling, and postoperative care including amblyopia management, these children can have good vision.
6 Cataract in Other Pediatric Retinal Disorders
Pediatric cases and adult cases differ in the type of retinal detachment along with cause and outcome of the same. The anatomical and functional outcomes are different from the adult cases [52]. The pediatric cases may be detected late as symptoms are usually ignored and difficulty in obtaining medical history [52]. The presence of cataract may further complicate the scenario. Posterior segment abnormalities can be associated with lens disorders like cataract or subluxated lens. The anatomical and functional success is poorer in pediatric cases with lens disorders as compared to those without lens involvement [53]. The various pediatric vitreoretinal disorders with cataract include incontinentia pigment, Coats disease, persistent hyperplastic primary vitreous (PHPV), familial exudative vitreoretinopathy (FEVR), and Stickler syndrome. Few of them are described here.
7 Coats Disease
Coats disease is seen in young males as a unilateral presentation characterized by telangiectatic vessels and exudation. Lenticular involvement seen in 8–28% of cases with Coats disease especially in the advanced stages includes total white cataract, posterior subcapsular cataract and less commonly as anterior subcapsular cataract [54,55,56]. The possible factors affecting the cataract formation in coats disease includes stage of the disease, extension of telangiectasia and exudation, presence of exudative retinal detachment, rubeosis iridis and neovascular glaucoma [56]. Presence of the exudative retinal detachment and advanced stage of the disease was one of the important factors in association with cataract formation and also a significant predictor for worse final visual outcome [56]. The cortical degeneration and the posterior migration of the lens epithelium was seen in enucleated eyes of cases with Coats disease and cataract [57]. The chronic exudation and inflammation do play a role in the cataract formation. The breakdown of the blood-retinal barrier and the oxidative stress are key factors. Though laser treatment is known to cause cataract in ROP, its role in coats disease with cataract have not been explored. Tunica vasculosa lentis which is a risk factor in ROP cases is not seen with coats disease. Hence, probably laser does not have any role in cataract formation. Cataract extraction does improve the fundus visualization but may not necessarily lead to improvement in vision.
8 Persistent Hyperplastic Primary Vitreous (PHPV)
PHPV is a congenital abnormality with failure of regression of the embryologic primary vitreous and hyaloid vasculature. Most cases are unilateral with microphthalmos, cataract, persistent hyaloid vasculature, and persistent tunica vasculosa lentis [58]. Advanced cases can have severe microphthalmos, foveal hypoplasia, retinal dysplasia or retinal detachment. PHPV is of three types—anterior, posterior, and combined. The posterior PHPV has poorer prognosis as compared to anterior PHPV [59, 60]. But untreated PHPV have high rate of progressing to phthisis bulbi, secondary glaucoma or painful blind eye requiring enucleation. The removal of the anterior traction relieves the pulling force on the ciliary body does decreasing the possibility of phthisis bulbi [59].The anatomical differences makes it difficult to perform cataract surgery and further implantation of an IOL is a challenge. In cases where corneal diameter is more than 10 mm and adequate capsular support is present, IOL implantation can be done. Being unilateral disease most of the time, amblyopia is another concern. The surgical outcomes are further compromised by high rate of intraoperative and post-operative complications like hyphemia, vitreous hemorrhage, recurrent VAO, glaucoma, strabismus and retinal detachment [59,60,61]. The presence of vascular membrane and stalk is a risk factor for bleeding. Diathermy or Fugo plasma blade can be used to cauterize the same [62].
9 Hereditary Syndromes
Cataract has been associated with various hereditary syndrome including Stickler syndrome, FEVR, retinitis pigmentosa, Usher syndrome, and others. In most of the diseases, it appears to be a secondary effect of the vitreoretinal degeneration and underlying effect rather than being a primary component of the genetic disorder. Further, the high risk of retinal detachment inherent to the pathology and to vitreal changes induced after the cataract surgery can significantly affect the visual outcome. Thus, follow-up examination of the fundus post cataract surgery is important at every visit to detect any posterior segment changes earlier.
Many studies have documented a higher association of same with retinitis pigmentosa [63]. The posterior subcapsular type is the most common type seen in retinitis pigmentosa and causes significant glare abnormalities especially in advanced cases with decrease in the visual fields (Fig. 16.5). But many of these present at a later stage of life. Cases with normal macular area may significantly benefit from the cataract surgery. Also some amount of zonular laxity is known to be associated with RP and these cases are hence prone to have subluxations or postoperative anterior capsular phimosis (Fig. 16.6) [64,65,66]. Hence, few considerations to be kept in mind while performing the surgery. The preoperative evaluation should include assessment of the visual fields if possible to explain the prognosis and benefits obtained by surgery. The ACC should be adequate and in case of any zonular laxity, CTR can be placed in the bag.
Pseudophakia with severe anterior capsular phimosis 2 years after surgery in OS of the same patient as Fig. 16.5. Note no capsular tension ring put in OS
Lens involvement in Wagner disease is seen in adolescent age group and includes discrete anterior and posterior polar dot-like opacities, PSC, and nuclear sclerosis. They slowly progress to visual incapacitation at a later stage. The cataract surgery in these cases can cause vitreous changes and its related complications [67]. Stickler syndrome, also known as hereditary progressive arthro-ophthalmopathy, is a connective tissue disorder presenting with ocular, hearing abnormalities, midfacial underdevelopment, palatal abnormalities, mild spondyloepiphyseal dysplasia or precocious arthritis [68]. Ocular involvement can include myopia, glaucoma, strabismus, vitreoretinal degeneration, retinal detachment or cataract. Lens involvement is seen as wedge and fleck cataracts distinctively (Fig. 16.7) [69]. In a study of 70 members of 22 families, they found that the prevalence of cataract was 20% below the age of 10 years and increased to 83% in more than 50 years group [70]. FEVR is considered as one of the differential diagnosis of ROP. These cases develop cataract and retinal detachment as late complications. However, the pathogenesis of the cataract in same is unclear.
10 Ocular Trauma
Posterior segment can be involved in both the open and closed globe injuries and can be also associated with lens involvement. After the primary injury repair, one can assess the status of the posterior segment using ultrasonography in the setting of cataract. In presence of retinal detachment or endophthalmitis, removal of lens by phacoemulsification or lens aspiration may be required for posterior segment management. The technique of lens aspiration further depends on the multiple factors like mode of injury, cornea status, cornea clarity, intactness of anterior and posterior capsule, or presence of hypotony. Thus stepwise method evaluating each step is required in cases with traumatic cataract and posterior segment abnormalities. Further secondary IOL implantation, wearing appropriate refractive error glasses and occlusion therapy after management for trauma related posterior segment injuries and cataract in children allows treatment of deprivation amblyopia and obtain good vision [71].
10.1 Ocular tumor
Retinoblastoma (RB) is the commonest intraocular malignancy of childhood. It is differential diagnosis for leukocoria. Ultrasonography is required to make a presumptive diagnosis of RB. USG showing mass lesion with calcification is highly suggestive (Fig. 16.8). Rather than the disease, cataract is most commonly a complication of radiation therapy received in the course of disease treatment [72]. Simultaneous occurrence of cataract with retinoblastoma is <1% [73, 74]. Surgical outcomes in radiation induced cataract depend on the primary location of regressed RB, with macular lesion showing worse prognosis than peripheral lesions.
Keypoints
-
Cataract in ROP children can be because of the systemic status, retinal detachment, ROP itself or treatment of ROP.
-
Early diagnosis and management of cataract is important to plan for posterior segment intervention.
-
In case of severe neovascularization, anti-VEGF injection may be useful for stabilization of the disease till cataract is managed.
-
Preoperative USG and UBM can help in determining preexisting retinal detachment and posterior capsular defect.
-
A combined approach with postoperative care and counseling is important to maintain good vision in these preterm individuals. Long-term follow-up is necessary.
-
Pediatric retinal disorders differ from adult disorder in term of cause and outcome. Presence of cataract further affects the prognosis.
-
Regular follow-up with fundus examination is important after cataract surgery in pediatric cases with vitreoretinal abnormalities.
References
Lambert SR, Drack AV. Infantile cataracts. Surv Ophthalmol. 1996;40(6):427–58. https://doi.org/10.1016/S0039-6257(96)82011-X.
Vander JF, McNamara JA, Tasman W, Brown GC. Revised indications for early treatment of retinopathy of prematurity. Arch Ophthalmol. 2005;123(3):406–7; discussion 409–10. https://doi.org/10.1001/archopht.123.3.406-b.
Ezisi CN, Kekunnaya R, Jalali S, et al. Cataract surgery in children with retinopathy of prematurity (ROP): surgical outcomes. Br J Ophthalmol. 2017;101(8):1128–31. https://doi.org/10.1136/bjophthalmol-2016-309392.
Davitt BV, Christiansen SP, Hardy RJ, Tung B, Good WV, Early Treatment for Retinopathy of Prematurity Cooperative Group. Incidence of cataract development by 6 months’ corrected age in the Early Treatment for Retinopathy of Prematurity study. J AAPOS. 2013;17(1):49–53. https://doi.org/10.1016/j.jaapos.2012.10.011.
Yu YS, Kim S-J, Chang BL. Cataract surgery in children with and without retinopathy of prematurity. J Cataract Refract Surg. 2004;30(1):89–94. https://doi.org/10.1016/S0886-3350(03)00059-2.
Krolicki TJ, Tasman W. Cataract extraction in adults with retinopathy of prematurity. Arch Ophthalmol. 1995;113(2):173–7. https://doi.org/10.1001/archopht.1995.01100020057028.
Vanathi M, Kumawat D, Singh R, Chandra P. Iatrogenic crystalline lens injury in pediatric eyes following intravitreal injection for retinopathy of prematurity. J Pediatr Ophthalmol Strabismus. 2019;56(3):162–7. https://doi.org/10.3928/01913913-20190211-02.
Chandra P, Khokhar S, Kumar A. Bilateral total cataract after laser treatment of aggressive posterior retinopathy of prematurity. Indian Pediatr. 2016;53(Suppl 2):S157–8.
Khokhar S, Chandra P, Gupta Y, Kumawat D, Dhull C. Bilateral total cataract after intravitreal bevacizumab injection in aggressive posterior retinopathy of prematurity. J Pediatr Ophthalmol Strabismus. 2019;56:e28–30. https://doi.org/10.3928/01913913-20190219-02.
Alden ER, Kalina RE, Hodson WA. Transient cataracts in low-birth-weight infants. J Pediatr. 1973;82(2):314–8. https://doi.org/10.1016/s0022-3476(73)80180-5.
Drack AV, Burke JP, Pulido JS, Keech RV. Transient punctate lenticular opacities as a complication of argon laser photoablation in an infant with retinopathy of prematurity. Am J Ophthalmol. 1992;113(5):583–4. https://doi.org/10.1016/s0002-9394(14)74733-6.
Khokhar SK, Pillay G, Dhull C, Agarwal E, Mahabir M, Aggarwal P. Pediatric cataract. Indian J Ophthalmol. 2017;65(12):1340–9. https://doi.org/10.4103/ijo.IJO_1023_17.
Choi J, Kim JH, Kim S-J, Yu YS. Long-term results of lens-sparing vitrectomy for stages 4B and 5 retinopathy of prematurity. Korean J Ophthalmol. 2011;25(5):305–10. https://doi.org/10.3341/kjo.2011.25.5.305.
Lakhanpal RR, Davis GH, Sun RL, Albini TA, Holz ER. Lens clarity after 3-port lens-sparing vitrectomy in stage 4A and 4B retinal detachments secondary to retinopathy of prematurity. Arch Ophthalmol. 2006;124(1):20–3. https://doi.org/10.1001/archopht.124.1.20.
Gold RS. Cataracts associated with treatment for retinopathy of prematurity. J Pediatr Ophthalmol Strabismus. 1997;34(2):123–4.
Knight-Nanan DM, Algawi K, Bowell R, O’Keefe M. Advanced cicatricial retinopathy of prematurity--outcome and complications. Br J Ophthalmol. 1996;80(4):343–5. https://doi.org/10.1136/bjo.80.4.343.
Trese MT, Shokoohi FK. Immediate complications of cryotherapy in children. Retina (Philadelphia, Pa). 1990;10(2):159.
Cryotherapy for Retinopathy of Prematurity Cooperative Group. Multicenter trial of cryotherapy for retinopathy of prematurity. Preliminary results. Arch Ophthalmol. 1988;106(4):471–9. https://doi.org/10.1001/archopht.1988.01060130517027.
Repka MX, Tung B, Good WV, et al. Outcome of eyes developing retinal detachment during the Early Treatment for Retinopathy of Prematurity Study (ETROP). Arch Ophthalmol. 2006;124(1):24–30. https://doi.org/10.1001/archopht.124.1.24.
Christiansen SP, Bradford JD. Cataract in infants treated with argon laser photocoagulation for threshold retinopathy of prematurity. Am J Ophthalmol. 1995;119(2):175–80. https://doi.org/10.1016/s0002-9394(14)73870-x.
O’Neil JW, Hutchinson AK, Saunders RA, Wilson ME. Acquired cataracts after argon laser photocoagulation for retinopathy of prematurity. J AAPOS. 1998;2(1):48–51. https://doi.org/10.1016/s1091-8531(98)90110-0.
Paysse EA, Miller A, Brady McCreery KM, Coats DK. Acquired cataracts after diode laser photocoagulation for threshold retinopathy of prematurity. Ophthalmology. 2002;109(9):1662–5. https://doi.org/10.1016/s0161-6420(02)01169-7.
Mintz-Hittner HA, Kennedy KA, Chuang AZ. BEAT-ROP Cooperative Group. Efficacy of intravitreal bevacizumab for stage 3+ retinopathy of prematurity. N Engl J Med. 2011;364(7):603–15. https://doi.org/10.1056/NEJMoa1007374.
Cuthbertson F, Newsom R. UK retinopathy of prematurity treatment survey. Eye (Lond). 2007;21(2):156–7. https://doi.org/10.1038/sj.eye.6702230.
Campolattaro BN, Lueder GT. Cataract in infants treated with argon laser photocoagulation for threshold retinopathy of prematurity. Am J Ophthalmol. 1995;120(2):264–6. https://doi.org/10.1016/s0002-9394(14)72627-3.
Kaiser RS, Trese MT. Iris atrophy, cataracts, and hypotony following peripheral ablation for threshold retinopathy of prematurity. Arch Ophthalmol. 2001;119(4):615–7.
Quan AV, Pineles SL, Tsui I, Velez FG. Phthisis bulbi following lensectomy in retinopathy of prematurity eyes previously treated with laser photocoagulation. Retin Cases Brief Rep. 2015;9(1):67–71. https://doi.org/10.1097/ICB.0000000000000086.
Fung AE, Rosenfeld PJ, Reichel E. The International Intravitreal Bevacizumab Safety Survey: using the internet to assess drug safety worldwide. Br J Ophthalmol. 2006;90(11):1344–9. https://doi.org/10.1136/bjo.2006.099598.
Meyer CH, Rodrigues EB, Michels S, et al. Incidence of damage to the crystalline lens during intravitreal injections. J Ocul Pharmacol Ther. 2010;26(5):491–5. https://doi.org/10.1089/jop.2010.0045.
Stahl A, Lepore D, Fielder A, et al. Ranibizumab versus laser therapy for the treatment of very low birthweight infants with retinopathy of prematurity (RAINBOW): an open-label randomised controlled trial. Lancet. 2019;394(10208):1551–9. https://doi.org/10.1016/S0140-6736(19)31344-3.
Chen TA, Shields RA, Bodnar ZH, Callaway NF, Schachar IH, Moshfeghi DM. A spectrum of regression following intravitreal bevacizumab in retinopathy of prematurity. Am J Ophthalmol. 2019;198:63–9. https://doi.org/10.1016/j.ajo.2018.09.039.
Hairston RJ, Maguire AM, Vitale S, Green WR. Morphometric analysis of pars plana development in humans. Retina (Philadelphia, Pa). 1997;17(2):135–8. https://doi.org/10.1097/00006982-199703000-00009.
Chang SHL, Lee Y-S, Wu S-C, et al. Anterior chamber angle and anterior segment structure of eyes in children with early stages of retinopathy of prematurity. Am J Ophthalmol. 2017;179:46–54. https://doi.org/10.1016/j.ajo.2017.04.010.
Fledelius HC. Pre-term delivery and the growth of the eye an oculometric study of eye size around term-time. Acta Ophthalmol. 1992;70(S204):10–5. https://doi.org/10.1111/j.1755-3768.1992.tb04915.x.
Laws DE, Haslett R, Ashby D, O’Brien C, Clark D. Axial length biometry in infants with retinopathy of prematurity. Eye. 1994;8(4):427–30. https://doi.org/10.1038/eye.1994.101.
Azad RV, Lakshminarayana P, Kumar H, Talwar D, Pal N, Chandra P. Ocular growth pattern in cryotherapy- and laser-treated infants with prethreshold retinopathy of prematurity. J Pediatr Ophthalmol Strabismus. 2005;42(3):149–54.
Axer-Siegel R, Bourla D, Kremer I, Weinberger D, Snir M. Effect of peripheral retinal ablation with cryotherapy versus diode laser photocoagulation on axial length in the growing rabbit eye. Br J Ophthalmol. 2006;90(4):491–5. https://doi.org/10.1136/bjo.2005.082768.
Cook A, White S, Batterbury M, Clark D. Ocular growth and refractive error development in premature infants with or without retinopathy of prematurity. Invest Ophthalmol Vis Sci. 2008;49(12):5199–207. https://doi.org/10.1167/iovs.06-0114.
Dick HB, Aliyeva SE, Hengerer F. Effect of trypan blue on the elasticity of the human anterior lens capsule. J Cataract Refract Surg. 2008;34(8):1367–73. https://doi.org/10.1016/j.jcrs.2008.03.041.
Astle WF, Alewenah O, Ingram AD, Paszuk A. Surgical outcomes of primary foldable intraocular lens implantation in children: understanding posterior opacification and the absence of glaucoma. J Cataract Refract Surg. 2009;35(7):1216–22. https://doi.org/10.1016/j.jcrs.2009.02.028.
Vasavada AR, Praveen MR, Tassignon M-J, et al. Posterior capsule management in congenital cataract surgery. J Cataract Refract Surg. 2011;37(1):173–93. https://doi.org/10.1016/j.jcrs.2010.10.036.
Khokhar SK, Tomar A, Pillay G, Agarwal E. Biometric changes in Indian pediatric cataract and postoperative refractive status. Indian J Ophthalmol. 2019;67(7):1068–72. https://doi.org/10.4103/ijo.IJO_1327_18.
McClatchey SK. Choosing IOL power in pediatric cataract surgery. Int Ophthalmol Clin. 2010;50(4):115–23. https://doi.org/10.1097/IIO.0b013e3181f0f2e0.
Nguyen H, Yen KG. Outcome of cataract surgery in patients treated for retinopathy of prematurity. Open J Ophthalmol. 2017;7(4):293–302. https://doi.org/10.4236/ojoph.2017.74038.
Cole CJ, Charteris DG. Cataract extraction after retinal detachment repair by vitrectomy: visual outcome and complications. Eye (Lond). 2009;23(6):1377–81. https://doi.org/10.1038/eye.2008.255.
Saeed MU, Prasad S. Management of cataract caused by inadvertent capsule penetration during intravitreal injection of ranibizumab. J Cataract Refract Surg. 2009;35(11):1857–9. https://doi.org/10.1016/j.jcrs.2009.05.050.
Farr AK, Stark WJ, Haller JA. Cataract surgery by phacoemulsification in adults with retinopathy of prematurity. Am J Ophthalmol. 2001;132(3):306–10. https://doi.org/10.1016/s0002-9394(01)01006-6.
O’Keefe M, Fenton S, Lanigan B. Visual outcomes and complications of posterior chamber intraocular lens implantation in the first year of life. J Cataract Refract Surg. 2001;27(12):2006–11. https://doi.org/10.1016/s0886-3350(01)00973-7.
Bremer DL, Rogers DL, Good WV, Tung B, Hardy RJ, Fellows R. Glaucoma in the Early Treatment for Retinopathy of Prematurity (ETROP) study. J AAPOS. 2012;16(5):449–52. https://doi.org/10.1016/j.jaapos.2012.06.011.
Chandra P, Tewari R, Salunkhe N, Kumawat D, Chaurasia AK, Gupta V. Short-term incidence and management of glaucoma after successful surgery for stage 4 retinopathy of prematurity. Indian J Ophthalmol. 2019;67(6):917. https://doi.org/10.4103/ijo.IJO_33_18.
Kaiser RS, Fenton GL, Tasman W, Trese MT. Adult retinopathy of prematurity: retinal complications from cataract surgery. Am J Ophthalmol. 2008;145(4):729–735.e1. https://doi.org/10.1016/j.ajo.2007.11.007.
Rumelt S, Sarrazin L, Averbukh E, Halpert M, Hemo I. Paediatric vs adult retinal detachment. Eye (Lond). 2007;21(12):1473–8. https://doi.org/10.1038/sj.eye.6702511.
Wang NK, Chen TL, Lai CC, et al. Clinical characteristics and surgical outcomes of pediatric retinal detachments with lens disorders. J Pediatr Ophthalmol Strabismus. 2009;46(3):160–7. https://doi.org/10.3928/01913913-20090505-07.
Shields JA, Shields CL, Honavar SG, Demirci H. Clinical variations and complications of Coats disease in 150 cases: the 2000 Sanford Gifford Memorial Lecture. Am J Ophthalmol. 2001;131(5):561–71. https://doi.org/10.1016/S0002-9394(00)00883-7.
Shields JA, Shields CL, Honavar SG, Demirci H, Cater J. Classification and management of Coats disease: the 2000 Proctor Lecture. Am J Ophthalmol. 2001;131(5):572–83. https://doi.org/10.1016/S0002-9394(01)00896-0.
Daruich A, Matet A, Munier FL. Cataract development in children with Coats disease: risk factors and outcome. J AAPOS. 2018;22(1):44–9. https://doi.org/10.1016/j.jaapos.2017.09.009.
Chang MM, McLean IW, Merritt JC. Coats’ disease: a study of 62 histologically confirmed cases. J Pediatr Ophthalmol Strabismus. 1984;21(5):163–8.
Goldberg MF. Persistent fetal vasculature (PFV): an integrated interpretation of signs and symptoms associated with persistent hyperplastic primary vitreous (PHPV). LIV Edward Jackson Memorial Lecture. Am J Ophthalmol. 1997;124(5):587–626.
Pollard ZF. Persistent hyperplastic primary vitreous: diagnosis, treatment and results. Trans Am Ophthalmol Soc. 1997;95:487–549.
Jinagal J, Gupta PC, Ram J, et al. Outcomes of cataract surgery in children with persistent hyperplastic primary vitreous. Eur J Ophthalmol. 2018;28(2):193–7. https://doi.org/10.5301/ejo.5001017.
Johnson CP, Keech RV. Prevalence of glaucoma after surgery for PHPV and infantile cataracts. J Pediatr Ophthalmol Strabismus. 1996;33(1):14–7. https://doi.org/10.3928/0191-3913-19960101-05.
Sinha R, Bali SJ, Kumar C, et al. Results of cataract surgery and plasma ablation posterior capsulotomy in anterior persistent hyperplastic primary vitreous. Middle East Afr J Ophthalmol. 2013;20(3):217–20. https://doi.org/10.4103/0974-9233.114794.
Heckenlively J. The frequency of posterior subcapsular cataract in the hereditary retinal degenerations. Am J Ophthalmol. 1982;93(6):733–8. https://doi.org/10.1016/0002-9394(82)90469-X.
Dikopf MS, Chow CC, Mieler WF, Tu EY. Cataract extraction outcomes and the prevalence of zonular insufficiency in retinitis pigmentosa. Am J Ophthalmol. 2013;156(1):82–88.e2. https://doi.org/10.1016/j.ajo.2013.02.002.
Gocho K, Kameya S, Akeo K, et al. High-resolution imaging of patients with Bietti crystalline dystrophy with CYP4V2 mutation. Lai TY, ed. J Ophthalmol. 2014;2014:283603. https://doi.org/10.1155/2014/283603.
Jackson H, Garway-Heath D, Rosen P, Bird AC, Tuft SJ. Outcome of cataract surgery in patients with retinitis pigmentosa. Br J Ophthalmol. 2001;85(8):936–8. https://doi.org/10.1136/bjo.85.8.936.
Manning LM. Wagner’s hereditary vitreoretinal degeneration. Aust J Opthalmol. 1980;8(1):29–33. https://doi.org/10.1111/j.1442-9071.1980.tb00885.x.
Robin NH, Moran RT, Ala-Kokko L. Stickler syndrome. In: Adam MP, Ardinger HH, Pagon RA, et al., editors. GeneReviews®. Seattle: University of Washington; 1993. http://www.ncbi.nlm.nih.gov/books/NBK1302/. Accessed June 2, 2020.
Seery CM, Pruett RC, Liberfarb RM, Cohen BZ. Distinctive cataract in the Stickler syndrome. Am J Ophthalmol. 1990;110(2):143–8. https://doi.org/10.1016/S0002-9394(14)76982-X.
Liberfarb RM, Hirose T, Holmes LB. The Wagner-Stickler syndrome: a study of 22 families. J Pediatr. 1981;99(3):394–9. https://doi.org/10.1016/s0022-3476(81)80324-1.
Bai H, Meng X, Wang D, Han J. Treatment for amblyopia after surgery for cataract and vitreoretina in pediatric ocular trauma. Eye Sci. 2013;28(2):68–72.
Brooks HL Jr, Meyer D, Shields JA, Balas AG, Nelson LB, Fontanesi J. Removal of radiation-induced cataracts in patients treated for retinoblastoma. Arch Ophthalmol. 1990;108:1701–8.
Brown GC, Shields JA, Oglesby RB. Anterior polar cataracts associated with bilateral retinoblastoma. Am J Ophthalmol. 1979;87:276.
Balasubramanya R, Pushker N, Bajaj MS, Ghose S, Kashyap S, Rani A. Atypical presentations of retinoblastoma. J Pediatr Ophthalmol Strabismus. 2004;41:18–24.
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
1 Electronic Supplementary Material
Cataract surgery in ROP. (Sudarshan Khokhar, Chirakshi Dhull) (MP4 181286 kb)
Cataract surgery in pre-existing RD. (Sudarshan Khokhar, Chirakshi Dhull) (MP4 173007 kb)
Cataract surgery in oil filled eye. (Sudarshan Khokhar, Chirakshi Dhull) (MP4 321788 kb)
Rights and permissions
Copyright information
© 2022 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Surve, A., Dhull, C., Khokhar, S.K. (2022). Cataract Associated with ROP and Other Retinal Pathologies. In: Khokhar, S.K., Dhull, C. (eds) Essentials of Pediatric Cataract Surgery. Springer, Singapore. https://doi.org/10.1007/978-981-16-0212-2_16
Download citation
DOI: https://doi.org/10.1007/978-981-16-0212-2_16
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-16-0211-5
Online ISBN: 978-981-16-0212-2
eBook Packages: MedicineMedicine (R0)