Abstract
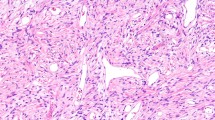
Sarcomas are a group of rare malignant neoplasms of mesenchymal origin which may occur in skeletal and extraskeletal tissue, including muscles, tendons, fat, synovium, fibrous tissue, blood vessels and the peripheral nervous system [1, 2]. Tumours of soft tissue and bone are characterised by a high degree of morphological, molecular and clinical heterogeneity. Sarcomas are classified by the World Health Organization (WHO) according to histological features into over 100 types, of which at least 70% are soft tissue sarcomas [2, 3]. The classification system for sarcomas is an evolving process, reflecting the advent of novel molecular, cytogenetic and immunohistochemical techniques which facilitate the identification of groups of sarcoma cells expressing tumour-specific markers [4]. These techniques play a pivotal role in the refinement of sarcoma diagnosis, which is currently based on tumour morphology, immunohistochemistry and clinic-pathological correlation [2].
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Sarcomas are a group of rare malignant neoplasms of mesenchymal origin which may occur in skeletal and extraskeletal tissue, including muscles, tendons, fat, synovium, fibrous tissue, blood vessels and the peripheral nervous system [1, 2]. Tumours of soft tissue and bone are characterised by a high degree of morphological, molecular and clinical heterogeneity. Sarcomas are classified by the World Health Organization (WHO) according to histological features into over 100 types, of which at least 70% are soft tissue sarcomas [2, 3]. The classification system for sarcomas is an evolving process, reflecting the advent of novel molecular, cytogenetic and immunohistochemical techniques which facilitate the identification of groups of sarcoma cells expressing tumour-specific markers [4]. These techniques play a pivotal role in the refinement of sarcoma diagnosis, which is currently based on tumour morphology, immunohistochemistry and clinic-pathological correlation [2].
2.1 Epidemiology of Sarcomas
Sarcomas represent fewer than 1 in 100 solid malignancies in adults but account for more than 1 in 5 solid malignant tumours in the paediatric population [5]. According to data from the Surveillance, Epidemiology and End Results (SEER) database [6], during the period between 1973 and 2008, soft tissue sarcomas occurred in higher frequencies than malignant bone cancers. In 1 year, 87% of sarcomas diagnosed were soft tissue sarcomas (STS), and the remaining 13% were malignant bone sarcomas. The most common malignant tumours of bone are osteosarcoma and chondrosarcoma, which cumulatively account for over 50% of bone cancer diagnoses [5]. Among STS, the category “other specified soft tissue sarcomas” was the most common, accounting for 51% of all STS. Kaposi sarcoma (9% of all sarcoma diagnoses) and fibrosarcomas (7% of all sarcoma diagnoses) were the two most frequent identifiable STS diagnosed in 2008, according to SEER data [5]. Overall, soft tissue sarcomas have an annual incidence of 6 per 100,000 persons [6]. In Europe, the estimated incidence of STS is 4 per 100,000 per year [7], while in England, the incidence of soft tissue sarcoma between 1979 and 2001 was 9.1 per million person-years at risk [8]. An increase in the overall incidence in STS has been recorded; however this may also reflect the advancement of diagnostic tools and greater research interest in the field of sarcomas.
The SEER database also shows the relationship between age and sarcoma incidence [6]. The mean ages at diagnosis for STS and malignant bone cancers were 58 and 40 years, respectively, in the 4-year period between 2004 and 2008 [9]. On the other hand, the average age of death in patients with STS and bone cancer were 65 and 58 years, respectively [9]. It is evident from results in the database that there is an increase in the rate of STS from infancy until 5 years of age. Although the incidence of STS is the lowest among young adults, this value rises gradually until age 50, after which the increase in incidence is more exaggerated. According to the SEER database, under 10 years of age, the incidence of STS was 0.9 per 100,000 children, and this increased to 18.2 per 100,000 adults over 70 years of age [1]. Malignant bone tumours have a relatively consistent incidence across all ages, with elderly individuals experiencing a slightly higher incidence. It is known, for example, that embryonal rhabdomyosarcoma is unique to young individuals, while undifferentiated pleomorphic sarcoma is primarily a tumour of older populations. Males are affected by STS more frequently than females, but the true variations in incidence according to gender and age groups are dependent on the histological type of sarcoma. The 5-year survival rate for STS has been reported as 50–60%; however there is significant variation in survival and prognosis for the various STS subtypes [10].
An investigation into the importance of race as a risk factor for sarcoma occurrence has revealed that Caucasians are much more commonly affected by Ewing’s sarcoma than Asians, Africans and African Americans [11]. It is believed that this discrepancy in prevalence of Ewing’s sarcoma between the different race groups reflects a genetic basis for the condition. Overall, Ewing’s sarcoma has an incidence of 2.1 per million in the United States and is the second most common cancer of bone in children and adolescents [12]. Interestingly, people of Black ethnicity have the highest incidence of STS malignancies at 5.1 cases per 100,000 people, while Whites have a rate of 4.5 cases per 100,000 people, and American Indians/Asian Pacific Islanders have a lower incidence rate of 2.8 per 100,000.
Geographic variations in sarcoma incidence have also become evident. For instance, chondrosarcomas occur in greater rates in America compared to Asian countries [13]. A more detailed study of sarcoma incidence across various geographical regions, titled Cancer Incidence in Five Continents, Volume XI, shows that age-standardised incidence rates of osteosarcoma for both males and females do not in fact differ greatly between Asian countries and the United States, which was contrary to reports elsewhere [13]. Nevertheless, some interesting observations were made in this study, including the discovery that Japanese migrants living in “westernised” countries had a higher risk of osteosarcoma incidence relative to the overall population. For Japanese males, the incidence rate of osteosarcoma was 1.3 per 100,000 in California and 1.1 per 100,000 in Hawaii, in comparison to an incidence rate of 0.2–0.6 cases per 100,000 males in the general population across various continents [5]. Among females in Sondrio, Italy, a high incidence of osteosarcoma cases at 1.4 per 100,000 has also been discovered [5]. This finding is in contrast with the low incidence of 0.1–0.4 per 100,000 osteosarcoma cases among females in other regions of Italy [5]. Further epidemiological studies are required to uncover the significance of this finding which is presently unclear (Figs. 2.1 and 2.2 and Table 2.1).
Percentage of deaths according to age in patients suffering from sarcomas. The illustration was reproduced from Burningham et al. [5] with permission from the publisher Biomed Central
Age-adjusted incidence rate of soft tissue sarcomas and malignant bone tumours. The illustration was reproduced from Burningham et al. [5] with permission from the publisher Biomed Central
2.2 Pathogenesis of Sarcomas
2.2.1 Understanding the Origin of Sarcomas
It is postulated that sarcomas are derived from multipotent precursor cells of mesodermal tissues which have undergone malignant transformation [6]. There have been suggestions that subtypes of sarcomas arise from lineage-specific genetic mutations in mesenchymal stem cells (MSCs) that have not yet committed to a specific line of differentiation [14]. For example, the knock-out of p53 and RB genes in multipotent MSCs has been shown to induce osteosarcoma formation [15]. However, gene expression investigations have demonstrated that the cellular profiles of various soft tissue sarcoma groups are more similar to differentiated MSCs than undifferentiated MSCs [16]. Although the various histological grades and molecular phenotypes of sarcoma cells may be reflective of the stages of MSC differentiation during which oncogenic transformation occurs [14, 17, 18], histopathological findings suggest that sarcoma development is a more complicated process that could be better delineated through investigation of micro-RNA signatures [17]. Some findings suggest that perhaps sarcomas do not arise from differentiated MSCs nor directly from their expected precursors [17]. For instance, the diagnosis of rhabdomyosarcoma relies on the histological detection of rhabdomyoblasts and expression of muscle-related biomarkers. Despite showing features of skeletal muscle differentiation, rhabdomyosarcomas can develop in sites where skeletal muscle is absent. An explanation for this phenomenon can be derived from a study which showed that the activation of sonic-hedgehog signalling in adipocytes could generate embryonic rhabdomyosarcoma [19]. Hence, the transdifferentiation of mesenchymal progenitor cells is a probable mechanism through which sarcomas can develop from a variety of cell origins unrelated to their histologically observed differentiation status. Soft tissue sarcomas of uncertain differentiation commonly contain translocations resulting in fusion genes, though the association of these genes with particular cell types is unknown [18]. Owing to the histomorphological basis for the naming of sarcomas and the need to avoid confusion during interdisciplinary communication, the names of certain sarcomas are not indicative of their origin and pathobiology. Synovial sarcoma, for instance, is not associated with synovial joints and has been shown to resemble malignant peripheral nerve sheath tumours [20]. With regard to sarcomagenesis, there is a stronger emphasis on studying the histology, molecular signature and phenotype of the tissue rather than on the concept of histogenesis.
The most common sites of soft tissue sarcoma are deep tissues of the extremities such as deep fascia and skeletal muscle [4]. However, the head, neck, abdomen, trunk and retroperitoneum are also frequently affected. In the latest edition of the WHO Classification, soft tissue sarcomas are divided into 50 subtypes, including tumours of adipocytic, fibroblastic/myofibroblastic, skeletal muscle, pericytic (perivascular), smooth muscle, so-called fibriohistiocytic, vascular, chondroosseous and unknown differentiation [6]. These types are further divided into groups according to cell of origin and whether the tumour falls into benign, intermediate (locally aggressive), intermediate (rarely metastasising) or malignant categories of biological potential. Malignant sarcomas rarely originate from benign soft tissue tumours, except in the case of neurofibromas which may lead to malignant peripheral nerve sheath tumours in patients with type 1 neurofibromatosis. Moreover, the metastatic potential of malignant sarcomas is variable, such as dermatofibrosarcoma protuberans which has a very low frequency of metastasis. Soft tissue sarcomas of intermediate malignancy rarely metastasise but are known to have a high degree of recurrence.
The pathogenesis of soft tissue sarcomas is poorly understood, and their aetiology often remains unclear throughout the course of the disease [21]. There is, however, abundant evidence for the association between various genetic, molecular, immunological, infectious and environmental risk factors and the development of sarcomas. Identification of an exact cause of sarcoma is often complicated by extended periods of latency between time of exposure to risk factors and the development of the disease.
2.3 Genetic Predisposition Syndromes
Several inherited genetic syndromes have been linked with the development of bone and soft tissue sarcomas, primarily in children [22,23,24,25,26] (e.g. Li-Fraumeni syndrome, osteosarcoma, rhabdomyosarcoma and malignant peripheral nerve sheath tumours). However, many cases of sarcoma do not appear to be associated with cancer syndromes. An international genetic study found that 638 of 1162 sarcoma probands had pathogenic germline variants across 72 cancer-related genes including TP53, ATR, ATM, BRCA2 and ERCC2, and 217 subjects had 227 known or expected variants [27]. It was also found that the cumulative burden of multiple pathogenic variants in these genes were significantly associated with earlier age of cancer diagnosis. This study also found that among 911 families, recognisable genetic cancer syndromes were seen in only 17% [27]. This shows that a large number of both known and novel oncogenes or tumour suppressor genes are associated with sarcoma risk.
2.3.1 Li-Fraumeni Syndrome
Increased susceptibility for osteosarcoma, Ewing’s sarcoma and rhabdomyosarcoma has been discovered in patients with Li-Fraumeni syndrome (LFS), an autosomal dominant condition with pathogenic mutations in the TP53 tumour suppressor gene. Between 25 and 33% of tumours in LFS patients are sarcomas [28, 29], which tend to arise at a younger age in LFS-affected patients than in patients unaffected by LFS. Data from the International Agency for Research on Cancer (IARC) database shows that 96% of sarcomas in LFS patients occur before 50 years of age, compared with 38% which occur before age 50 in the overall population [30]. Furthermore, almost 7% of paediatric soft tissue sarcoma patients are postulated to have LFS. A study of oncological patterns in families of children with soft tissue sarcomas found that about 33% of 151 families studied had a genetic predisposition syndrome and over 10% of the families had features consistent with LFS [22].
2.3.2 Retinoblastoma
Mutations in the retinoblastoma (RB) gene are known to predispose to soft tissue and bony cancers. Inheritance of a mutant copy of the RB gene and retinoblastoma of the bilateral type are linked to the development of late-onset osteosarcoma in patients suffering from retinoblastoma [31, 32]. In a longitudinal study of 1601 patients with RB, of which 963 had the inherited form, the cumulative frequency of a second cancer was 6 times higher for those with the inherited form versus the non-inherited form of RB. Sarcomas accounted for 60% of the second cancers [32].
In particular, retinoblastoma patients who receive chemotherapy or radiotherapy treatment could be at an increased risk of sarcoma development [33]. It has been reported that in patients with hereditary retinoblastoma who undergo radiotherapy, leiomyosarcomas are more likely to develop outside the field of radiation, whereas rhabdomyosarcoma, fibrosarcoma and pleomorphic sarcoma tend to arise within the radiation field [33,34,35]. A study which followed up 1601 retinoblastoma survivors demonstrated a statistically significant increase in the risk of soft tissue sarcomas in retinoblastoma patients compared to the general population, primarily for leiomyosarcoma which showed a 400-fold increase in risk [35]. Moreover, 78% of the leiomyosarcoma diagnoses were made over 30 years after the retinoblastoma diagnosis, which highlights a significant long-term risk of an additional malignancy in this cohort of patients [35].
2.3.3 Neurofibromatosis
Type 1 neurofibromatosis (NF1) is caused by mutations in the gene NF1 which undergoes a “double hit” inactivation phenomenon in which one allele is inactivated in the germline and the second allele is later knocked out by a somatic mutation, leading to development of the disease [36]. A large proportion of benign neurofibromas in NF1 may experience oncogenic transformation into malignant peripheral nerve sheath tumours (MPNSTs), which includes neurofibrosarcomas and malignant schwannomas [37, 38]. Up to 13% of NF1 patients will develop MPNSTs in their lifetimes [15]. In one study, the risk of this malignant transformation in NF1 patients was calculated to be 4.6% compared to 0.001% in the general population [39].
2.3.4 Other Sarcoma-Associated Genetic Syndromes
Patients with familial adenomatous polyposis (FAP), also known as Gardner syndrome, have a higher frequency of intra-abdominal desmoid tumours than the general population [40]. An increased risk of osteosarcoma has been discovered in patients with poikiloderma congenitale or Rothmund-Thomson syndrome—an autosomal recessive condition characterised by skeletal anomalies, short stature and unique skin changes, such as atrophy, telangiectasias and pigmentation. Other rare syndromes, such as Gorlin’s syndrome, characterised by mutations in the PTCH1 gene [41, 42], and Costello syndrome which arises due to mutations in the HRAS gene [43], have been linked with the development of rhabdomyosarcomas.
2.4 Molecular Alterations in Sarcoma
During the past 25 years, karyotype analysis has been the basis for the molecular characterisation of sarcoma pathogenesis. In the domain of cytogenetics, the conceptual dichotomy between sarcomas with a simple karyotype and sarcomas with a complex karyotype has aided our understanding of different molecular aberrations that occur with respect to the genomic phenotype of the tumours. Sarcomas with simple genomes commonly exhibit transcriptional dysregulation and abnormal kinase signalling or epigenetic programming. It is possible to identify sarcomas in this group with tumour-specific molecular markers due to the presence of recurrent and predictable genomic rearrangements and activating point mutations. On the other hand, genomically complex sarcomas have non-recurrent and diverse rearrangements and gene amplifications. Therefore, the pathogenetic mechanisms of sarcoma are better characterised for those with simpler genomes. Transcriptional deregulation and deregulated signalling represent the two categories of pathobiology attributed to sarcomas with simple genomes. Conversely, sarcomas with complex genomes show highly heterogeneous, non-specific molecular alterations which promote oncogenesis through variable disruptions in cell biology, such as abnormal cell cycle regulation or genomic instability [44].
2.4.1 Sarcomas with Simple Karyotypes
Sarcomas with stable genomes generally have diploid karyotypes with a low frequency of mutations. When mutations or copy number variations occur, they do so in recognisable patterns, leading to tumour progression in a predictable manner. Mutations and balanced chromosomal rearrangements in known oncogenes and tumour suppressor genes are characteristic of genomically simple sarcomas. This group can be divided into five sub-categories according to the observed pattern of molecular genetic changes. These are (a) tumours with chimeric transcription factors, (b) tumours with deregulated kinase signalling, (c) tumours driven by oncometabolites and (d) tumours driven by primary epigenetic deregulation [2].
Fusion oncoproteins are often produced via the transcription of fusion genes which arise from chromosomal translocations in mesenchymal tumours. These oncoproteins can function as transcription factors that deregulate the expression of other genes normally involved in cell cycle processes [45]. In Ewing’s sarcoma, for example, the gene fusions ESWR1-FLI1 (85% of translocations) and ESWR1-ERG (10% of translocations) are the best-known reciprocal translocations. ESWR1-ETS is another Ewing’s sarcoma-related hybrid oncoprotein which has been shown to abnormally upregulate genes associated with cell proliferation, including PDGF-C, CCDN1 and c-MYC, downregulate cyclin-dependent kinase inhibitors, upregulate hTERT to allow cells to avoid senescence, repress apoptotic genes such as IGFBP-3, induce angiogenesis via VEGF overexpression and activate matrix metalloproteases which increases tumour metastatic potential [44]. Similarly, transcriptome sequencing of epithelioid haemangioma has shown that aberrant fusion of the FOS gene to various other genes such as ZFP36, resulting in loss of its trans-activation domain [46]. Epithelioid haemangioma presents as multifocal lesions, similar to epithelioid haemangioendothelioma, which is a low-grade angiosarcoma in which the WWTR1-CAMTA1 fusion gene drives tumorigenesis. In general, angiosarcomas rarely contain translocations. Rather, amplifications of oncogenes such as MYC, FLT4, PLCG1 and PTPRB are more common in primary and radiation-induced angiosarcomas [47]. Moreover, 10% of angiosarcomas of the breast contain mutations in KDR. Most of these genes are associated with increased angiogenesis.
Deregulated kinase signalling may be the main oncogenic driver in many sarcomas. Abnormal activation of receptor tyrosine kinases, such as KIT in gastrointestinal stromal tumours (GIST), and PDGFR in dermatofibrosarcoma protuberans are well-characterised examples of deregulated kinase signalling in sarcomas [48]. This knowledge has led to the clinically therapeutic pharmacological inhibition of KIT/PDGFRA in GIST patients. In up to 80% of GIST cases, KIT exhibits gain-of-function mutations which drive cell proliferation and survival [48]. Three major pathways are involved in KIT and PDGFRA-mediated tumorigenesis in GIST, namely, the PI3K/AKT/mTOR pathway, the RAS/RAF/MAPK pathway and the JAK/STAT pathway [2]. The first two pathways are critical to GIST tumour proliferation and are further deregulated in advanced stages of this cancer. Although some KIT/PDGFRA mutations are associated with poor prognosis, the mutations in GIST provide more useful information regarding response to drug inhibitors than prognosis.
Epigenetic regulation and gene expression are two cellular functions that are commonly altered by mutations in metabolic enzymes leading to abnormal metabolic activity which can lead to oncogenic transformation in sarcomas. Approximately 50% of chondrosarcomas and up to 81% of patients with enchondromas show somatic mutations in isocitrate dehydrogenase [49]. These mutations allow abnormal enzymatic activity, such as the production of D-2-hydroxyglutarate (D2HG) from alpha ketoglutarate. D2HG, an oncometabolite, deactivates other oxygenase enzymes like TET2 to lead to DNA hypermethylation, particularly in chondral tumours [49]. D2HG also increases histone methylation through alternative pathways and consequently leads to an unstable epigenetic environment that has been shown to drive transdifferentiation of cells in bone towards a cartilage phenotype. Detection of IDH1 and IDH2 mutations can thus help to differentiate chondrosarcoma from chondroma and chondroblastic osteosarcoma. Mutations in IDH leading to oncometabolite generation have been reported in 86% of secondary central chondrosarcoma, up to 70% of primary central chondrosarcoma, 15% of periosteal chondrosarcoma, 54% of de-differentiated chondrosarcoma and up to 87% of Ollier-associated enchondromas [49]. In high-grade chondrosarcomas, however, IDH does not appear to be a requirement for ongoing tumour survival and growth [50, 51].
Some GIST tumours which do not show the characteristic KIT/PDGFRA mutations may contain mutations in one of the genes coding for succinate dehydrogenase (SDH) or mitochondrial complex II in the electron transport chain [52]. These mutations are associated with global DNA hypermethylation and are commonly seen in gastric GISTs affecting younger patients. Mutations in any SDH subunit is known to cause degradation of the B subunit specifically [52]. Therefore, immunohistochemical detection of SDH subunit B acts as a surrogate marker for the identification of mutations in SDH.
Primary epigenetic deregulation has been cited as one of the most important mechanistic factors in the development of various sarcomas. Mutations in genes which normally regulate chromatin structure, such as the SWI/SNF complex, the Polycomb group and PRC2 complex (involved in malignant peripheral nerve sheath tumours), are known to exacerbate pre-existing genomic instability in a range of tumour types [53]. However, epigenetic deregulation is now recognised as an increasingly common primary driver of oncogenesis in several tumours, for instance, SMARCA4 inactivation in thoracic sarcomas, SMARCB1 deletions in rhabdoid tumours [54], H3F3B gene mutations in 95% of chondroblastoma cases and H3F3A mutations in 92% of giant cell tumours of bone (GCTB) [47]. The latter two tumours are locally aggressive tumours which are more common in paediatric than adult populations. Importantly, the abnormalities in epigenetic programming that have been observed in some studies of sarcoma are thought to occur under the influence of chromosomal translocation-mediated hybrid oncoproteins, such as the SS18-SSX hybrid complex in synovial sarcoma, in which the oncoproteins disrupt the SWI/SNF chromatin remodelling complex [55]. In combination with immunohistochemical detection of mutant proteins, protein complexes and enzymes, next-generation sequencing for mutational variant analysis can also inform sarcoma diagnosis.
2.4.2 Sarcomas with Complex Karyotypes
The majority of sarcomas show diverse, non-specific genetic modifications on a background of highly complex genomes. These tumours are characterised by a high histological grade, cytological pleomorphism and variable differentiation signatures. With the exception of osteosarcomas and some radiation-induced sarcomas, which are more prevalent in children and adolescents than adults, most sarcomas with complex genomes occur more frequently in the older population [56]. High-grade myxofibrosarcoma, high-grade leiomyosarcoma, pleomorphic and undifferentiated liposarcoma, angiosarcoma and undifferentiated pleomorphic sarcoma are examples of tumours known to have complex genomes [2]. These sarcomas have a greater prevalence of gene copy number variations as opposed to single nucleotide polymorphisms [2]. Due to the high level of molecular heterogeneity in all sarcomas within this group, few tumour-specific markers are available for diagnostic use. Some of the postulated mechanisms of pathogenesis in genomically complex sarcomas include alterations in TP53 signalling, abnormal telomeric extension due to enzymatic modifications and inactivation of ATRX (a chromatin remodelling protein) and mutations in the Rb/E2F cell cycle regulatory pathway, which can engender unregulated cell proliferation and survival [2, 57].
Despite the difficulty in molecular characterisation of sarcomas containing complex unbalanced genotypes, a pattern in copy number alterations has been established in well-differentiated/de-differentiated liposarcoma (WD/DDLPS), which shows characteristic linear or ring-like neochromosomes formed from the accumulation of DNA from distinct parts of the genome [58]. Some of the genes contained within these neochromosomes include the CDK4 and MDM2 genes on chromosome 12, which are involved in progression of the cell cycle and repression of TP53, respectively [2]. Findings from research into the evolution of neochromosomes illustrate that the creation of these neochromosomes is a result of a series of intra-nuclear events involving the fragmentation, circularisation, amplification and linearisation of chromosome 12-derived genetic material [58]. Since the amplification of MDM2 and CDK4 is a recurrent feature of this disease, the abnormally excessive genetic and transcriptional products may be detected by fluorescence in situ hybridisation (FISH), immunohistochemistry or next-generation sequencing and therefore serve as diagnostic markers for WD/DDLPS.
Osteosarcoma is the most common primary high-grade tumour in humans, occurring predominantly in children and adolescents [59]. It is characterised by a high degree of genomic instability due to the presence of numerous chromosomal rearrangements, gene amplifications, mutations and deletions, the complexity of which contributes to the difficulty in the identification of genetic and molecular markers for this condition. However, molecular alterations in the RB and TP53 gene pathways (22% of osteosarcoma cases) are known to be common in high-grade bone cancers such as osteosarcoma [60]. At present, two cellular events are postulated to play a role in osteosarcoma pathogenesis. The first is chromothripsis, which describes the aberrant fragmentation and disordered assembly of chromosomes [61]. The second event is kataegis, which refers to a hypermutated area of the genome, and is observed in approximately half of all osteosarcoma cases [62]. These two phenomena may lead to the formation of osteosarcoma-associated onco-antigens, the detection of which could predict responses to cancer immunotherapy. Currently, high-grade sarcomas with complex genomes lack specific, recurrent molecular markers which can guide the management of these cancers (Table 2.2).
2.5 Infectious Risk Factors
Although the role of infectious agents in the development of sarcomas is not well understood, there is strong evidence for the association of certain viral infections with sarcoma pathogenesis [1]. In the context of a weakened immune system due to immunodeficiency syndromes, HIV infection or exposure to immunosuppressive pharmacotherapy following transplantation, human herpesvirus 8 and Epstein-Barr virus are known to cause Kaposi sarcoma [63] and a group of leiomyosarcomas, respectively [64]. There is insufficient evidence to support the role of oncogenic viruses in sarcomagenesis in the absence of immunosuppression.
2.6 Immunological Risk Factors
A weak immune system is unable to initiate and sustain strong innate or adaptive immune responses against tumour cell growth, malignant transformation, proliferation and invasion. As discussed previously, immunosuppressive medications as well as acquired and congenital immunodeficiency syndromes increase the risk of viral-mediated sarcoma pathogenesis, possibly by limiting the numbers of natural killer cells and T-cells involved in the destruction of nascent tumour cells. However, the underlying mechanism connecting immune deficiency to diverse cancer types remains to be fully uncovered. It has been suggested that acquired regional immunodeficiency in combination with chronic lymphedema, secondary to radical mastectomy (Stewart-Treves syndrome) or infectious conditions, may effect the development of rare angiosarcomas [65, 66].
2.7 Environmental Risk Factors
Several environmental risk factors are implicated in the development of sarcoma. These primarily include exposure to radiation, chemicals and a history of trauma.
2.7.1 Radiation Exposure
In the 1920s, published reports cited the increased prevalence of sarcomas in workers manufacturing radium watch dials. Over the last few decades, there has been increasing evidence for the increased risk of sarcoma in patients undergoing radiotherapy treatment for lymphoma, testicular cancer, ovarian cancer, breast cancer, lung cancer and other cancers. Although previous estimates suggested that approximately 0.5–5.5% of sarcomas are due to radiation [67], larger longitudinal population studies in patients who have undergone radiation therapy have demonstrated a lower frequency of sarcomas in this group, with an incidence of 0.8% at the most. A Swedish study of 122,991 breast cancer patients who received radiotherapy showed that breast cancer patients had at least a 0.13% risk of developing sarcoma at 10 years following radiation exposure [68].
In order to identify the cause of sarcoma as being due to radiation, several criteria must be met. These include documentation proving the development of sarcoma within the irradiated field, confirmation of sarcoma diagnosis by histology, a minimum 3-year period of latency between radiation exposure and sarcoma development and evidence that the region in which the sarcoma arose was unaffected prior to radiotherapy [69]. Post-radiation sarcomas typically arise in the margins of the field of radiation, however, which suggests that the mutagenic impact of radiation is highest at the periphery due to scatter radiation [70]. The vast majority of radiation-induced sarcomas develop in adult women, which is reflective of the high prevalence of female patients receiving radiotherapy for breast and gynaecological cancers. A clear dose-dependent correlation exists between the radiation dose and sarcoma incidence, with a high risk reported for individuals exposed to more than 5000 cGy and a negligible risk for those exposed to less than 10 Gy [71].
Radiation-induced sarcomas are known to be high grade and locally aggressive. A study of 160 post-radiation sarcomas at the Memorial Sloan-Kettering Cancer Center revealed that 87% of the tumours were high grade and the most common sarcoma subtype in this category was extraskeletal osteosarcoma with a prevalence of 21%, followed by malignant fibrous histiocytoma (16%) and angiosarcoma or lymphangiosarcoma (15%) [72]. Among the radiation-induced soft tissue sarcomas, 70% are undifferentiated pleomorphic sarcomas [1]. Since most post-radiation sarcomas are already very high grade at the time of detection, they are associated with a poor survival rate. The highest survival rate in this group is seen in patients who develop post-radiation sarcomas of the extremities (30% survival at 5 years), and the lowest rate is observed in patients with sarcomas in the vertebral column, pelvis and shoulder girdle (less than 5% survival at 5 years) [1, 73].
2.7.2 Chemical Exposure
Sarcomas have been associated with exposure to a range of different chemicals. Polyvinylchloride, use of thorotrast during carotid angiography (between 1930 and 1955) and inorganic arsenic and androgenic anabolic steroid medications have all been linked with the development of hepatic angiosarcoma (HAS) [74]. It is presumed that thorium dioxide, the main component of thorotrast solution, is sequestered by Kupffer cells of the liver, causing radiation injury to hepatic tissue, which leads to a range of hepatic malignancies. Moreover, chlorophenols, dioxin and phenoxyacetic herbicides have also been associated with sarcoma pathogenesis [75, 76]. German autopsy investigations from the 1940s and 1950s showed an increased incidence of liver disease, including HAS, due to the consumption of potassium arsenite and arsenic-contaminated water [74]. Despite a study by Leiss and Savitz which suggested a link between phenoxyacetic acid pesticides and soft tissue sarcomas in paediatric patients, additional investigations did not support this claim [77]. Nevertheless, studies in at least four countries including Sweden, Italy, the United Kingdom and New Zealand provided strong evidence to conclude that the risk of soft tissue sarcomas in patients exposed to phenoxyacetic acid and chlorophenols in agricultural settings is about six times higher than the general population [78,79,80]. In certain animal models, benzene and o-nitrotoluene have also been shown to promote sarcomagenesis [81].
2.7.3 Trauma Exposure
Trauma has been cited as a rare causal factor in the development of soft tissue sarcomas in scar tissue secondary to surgery, fracture wounds, thermal and acid burns and implantation of metal or plastic prostheses following a long period of latency of at least several years [82]. Although soft tissue sarcomas are uncommonly detected during abdominal imaging following a history of abdominal trauma or pain, the vast majority of these tumours are asymptomatic. Furthermore, the connection between trauma and sarcoma appears to be more coincidental than aetiological in nature due to the liberal use of abdominal imaging in trauma patients.
References
Goldblum JR, Folpe AL, Weiss SW, Enzinger FM, Weiss SW. Enzinger and Weiss’s soft tissue tumors. 6th ed. Philadelphia: Saunders/Elsevier; 2014. xiv, 1155 p.
Marino-Enriquez A, Bovee JV. Molecular pathogenesis and diagnostic, prognostic and predictive molecular markers in sarcoma. Surg Pathol Clin. 2016;9(3):457–73.
Fletcher CD. The evolving classification of soft tissue tumours—an update based on the new 2013 WHO classification. Histopathology. 2014;64(1):2–11.
Thway K. Pathology of soft tissue sarcomas. Clin Oncol (R Coll Radiol). 2009;21(9):695–705.
Burningham Z, Hashibe M, Spector L, Schiffman JD. The epidemiology of sarcoma. Clin Sarcoma Res. 2012;2(1):14.
Ferrari A, Sultan I, Huang TT, Rodriguez-Galindo C, Shehadeh A, Meazza C, et al. Soft tissue sarcoma across the age spectrum: a population-based study from the Surveillance Epidemiology and End Results database. Pediatr Blood Cancer. 2011;57(6):943–9.
Casali PG, Blay JY, ECECPo experts. Soft tissue sarcomas: ESMO Clinical Practice Guidelines for diagnosis, treatment and follow-up. Ann Oncol. 2010;21(Suppl 5):v198–203.
Alston RD, Rowan S, Eden TO, Moran A, Birch JM. Cancer incidence patterns by region and socioeconomic deprivation in teenagers and young adults in England. Br J Cancer. 2007;96(11):1760–6.
Howlader NNA, Krapcho M, Neyman N, Aminou R, Waldron W, Altekruse SF, Kosary CL, Ruhl J, Tatalovich Z, Cho H, Mariotto A, Eisner MP, Lewis DR, Chen HS, Feuer EJ, Cronin KA, Edwards BK. SEER cancer statistics review, 1975–2008. Bethesda: National Cancer Institute; 2011.
Jemal A, Siegel R, Ward E, Murray T, Xu J, Thun MJ. Cancer statistics, 2007. CA Cancer J Clin. 2007;57(1):43–66.
Worch J, Matthay KK, Neuhaus J, Goldsby R, DuBois SG. Ethnic and racial differences in patients with Ewing sarcoma. Cancer. 2010;116(4):983–8.
Grier HE. The Ewing family of tumors. Ewing’s sarcoma and primitive neuroectodermal tumors. Pediatr Clin N Am. 1997;44(4):991–1004.
Guo W, Xu W, Huvos AG, Healey JH, Feng C. Comparative frequency of bone sarcomas among different racial groups. Chin Med J. 1999;112(12):1101–4.
Matushansky I, Hernando E, Socci ND, Mills JE, Matos TA, Edgar MA, et al. Derivation of sarcomas from mesenchymal stem cells via inactivation of the Wnt pathway. J Clin Invest. 2007;117(11):3248–57.
Lin PP, Pandey MK, Jin F, Raymond AK, Akiyama H, Lozano G. Targeted mutation of p53 and Rb in mesenchymal cells of the limb bud produces sarcomas in mice. Carcinogenesis. 2009;30(10):1789–95.
Genadry KC, Pietrobono S, Rota R, Linardic CM. Soft tissue sarcoma cancer stem cells: an overview. Front Oncol. 2018;8:475.
Danielson LS, Menendez S, Attolini CS, Guijarro MV, Bisogna M, Wei J, et al. A differentiation-based microRNA signature identifies leiomyosarcoma as a mesenchymal stem cell-related malignancy. Am J Pathol. 2010;177(2):908–17.
Nielsen TO, West RB, Linn SC, Alter O, Knowling MA, O’Connell JX, et al. Molecular characterisation of soft tissue tumours: a gene expression study. Lancet. 2002;359(9314):1301–7.
Hatley ME, Tang W, Garcia MR, Finkelstein D, Millay DP, Liu N, et al. A mouse model of rhabdomyosarcoma originating from the adipocyte lineage. Cancer Cell. 2012;22(4):536–46.
Ladanyi M, Antonescu CR, Leung DH, Woodruff JM, Kawai A, Healey JH, et al. Impact of SYT-SSX fusion type on the clinical behavior of synovial sarcoma: a multi-institutional retrospective study of 243 patients. Cancer Res. 2002;62(1):135–40.
Windham TC, Pisters PW. Retroperitoneal sarcomas. Cancer Control. 2005;12(1):36–43.
Hartley AL, Birch JM, Blair V, Kelsey AM, Harris M, Jones PH. Patterns of cancer in the families of children with soft tissue sarcoma. Cancer. 1993;72(3):923–30.
Li FP. Cancer families: human models of susceptibility to neoplasia--the Richard and Hinda Rosenthal Foundation Award lecture. Cancer Res. 1988;48(19):5381–6.
Li FP, Fraumeni JF Jr, Mulvihill JJ, Blattner WA, Dreyfus MG, Tucker MA, et al. A cancer family syndrome in twenty-four kindreds. Cancer Res. 1988;48(18):5358–62.
Zahm SH, Fraumeni JF Jr. The epidemiology of soft tissue sarcoma. Semin Oncol. 1997;24(5):504–14.
Zhang J, Walsh MF, Wu G, Edmonson MN, Gruber TA, Easton J, et al. Germline mutations in predisposition genes in pediatric cancer. N Engl J Med. 2015;373(24):2336–46.
Ballinger ML, Goode DL, Ray-Coquard I, James PA, Mitchell G, Niedermayr E, Puri A, Schiffman JD, Dite GS, Cipponi A, Maki RG. Monogenic and polygenic determinants of sarcoma risk: an international genetic study. Lancet Oncol. 2016;17(9):1261–71.
Evans SC, Lozano G. The Li-Fraumeni syndrome: an inherited susceptibility to cancer. Mol Med Today. 1997;3(9):390–5.
Varley JM, McGown G, Thorncroft M, Santibanez-Koref MF, Kelsey AM, Tricker KJ, et al. Germ-line mutations of TP53 in Li-Fraumeni families: an extended study of 39 families. Cancer Res. 1997;57(15):3245–52.
Ognjanovic S, Olivier M, Bergemann TL, Hainaut P. Sarcomas in TP53 germline mutation carriers: a review of the IARC TP53 database. Cancer. 2012;118(5):1387–96.
DerKinderen DJ, Koten JW, Nagelkerke NJ, Tan KE, Beemer FA, Den Otter W. Non-ocular cancer in patients with hereditary retinoblastoma and their relatives. Int J Cancer. 1988;41(4):499–504.
Yu CL, Tucker MA, Abramson DH, Furukawa K, Seddon JM, Stovall M, et al. Cause-specific mortality in long-term survivors of retinoblastoma. J Natl Cancer Inst. 2009;101(8):581–91.
Kleinerman RA, Stovall M, Tarone RE, Tucker MA. Radiotherapy and genetic susceptibility to cancer in a cohort of retinoblastoma patients. Ann Epidemiol. 2004;14(8):593.
Kleinerman RA, Schonfeld SJ, Tucker MA. Sarcomas in hereditary retinoblastoma. Clin Sarcoma Res. 2012;2(1):15.
Kleinerman RA, Tucker MA, Abramson DH, Seddon JM, Tarone RE, Fraumeni JF Jr. Risk of soft tissue sarcomas by individual subtype in survivors of hereditary retinoblastoma. J Natl Cancer Inst. 2007;99(1):24–31.
Colman SD, Williams CA, Wallace MR. Benign neurofibromas in type 1 neurofibromatosis (NF1) show somatic deletions of the NF1 gene. Nat Genet. 1995;11(1):90–2.
Brekke HR, Ribeiro FR, Kolberg M, Agesen TH, Lind GE, Eknaes M, et al. Genomic changes in chromosomes 10, 16, and X in malignant peripheral nerve sheath tumors identify a high-risk patient group. J Clin Oncol. 2010;28(9):1573–82.
Mertens F, Rydholm A, Bauer HF, Limon J, Nedoszytko B, Szadowska A, et al. Cytogenetic findings in malignant peripheral nerve sheath tumors. Int J Cancer. 1995;61(6):793–8.
Ducatman BS, Scheithauer BW, Piepgras DG, Reiman HM, Ilstrup DM. Malignant peripheral nerve sheath tumors. A clinicopathologic study of 120 cases. Cancer. 1986;57(10):2006–21.
Hizawa K, Iida M, Mibu R, Aoyagi K, Yao T, Fujishima M. Desmoid tumors in familial adenomatous polyposis/Gardner’s syndrome. J Clin Gastroenterol. 1997;25(1):334–7.
Bale AE. Variable expressivity of patched mutations in flies and humans. Am J Hum Genet. 1997;60(1):10–2.
Hahn H, Wojnowski L, Zimmer AM, Hall J, Miller G, Zimmer A. Rhabdomyosarcomas and radiation hypersensitivity in a mouse model of Gorlin syndrome. Nat Med. 1998;4(5):619–22.
Gripp KW, Scott CI Jr, Nicholson L, McDonald-McGinn DM, Ozeran JD, Jones MC, et al. Five additional Costello syndrome patients with rhabdomyosarcoma: proposal for a tumor screening protocol. Am J Med Genet. 2002;108(1):80–7.
Bovee JV, Hogendoorn PC. Molecular pathology of sarcomas: concepts and clinical implications. Virchows Arch. 2010;456(2):193–9.
Hanahan D, Weinberg RA. Hallmarks of cancer: the next generation. Cell. 2011;144(5):646–74.
Antonescu CR, Chen HW, Zhang L, Sung YS, Panicek D, Agaram NP, et al. ZFP36-FOSB fusion defines a subset of epithelioid hemangioma with atypical features. Genes Chromosomes Cancer. 2014;53(11):951–9.
Behjati S, Tarpey PS, Sheldon H, Martincorena I, Van Loo P, Gundem G, et al. Recurrent PTPRB and PLCG1 mutations in angiosarcoma. Nat Genet. 2014;46(4):376–9.
Corless CL, Fletcher JA, Heinrich MC. Biology of gastrointestinal stromal tumors. J Clin Oncol. 2004;22(18):3813–25.
Amary MF, Bacsi K, Maggiani F, Damato S, Halai D, Berisha F, et al. IDH1 and IDH2 mutations are frequent events in central chondrosarcoma and central and periosteal chondromas but not in other mesenchymal tumours. J Pathol. 2011;224(3):334–43.
Suijker J, Baelde HJ, Roelofs H, Cleton-Jansen AM, Bovee JV. The oncometabolite D-2-hydroxyglutarate induced by mutant IDH1 or −2 blocks osteoblast differentiation in vitro and in vivo. Oncotarget. 2015;6(17):14832–42.
Suijker J, Oosting J, Koornneef A, Struys EA, Salomons GS, Schaap FG, et al. Inhibition of mutant IDH1 decreases D-2-HG levels without affecting tumorigenic properties of chondrosarcoma cell lines. Oncotarget. 2015;6(14):12505–19.
Killian JK, Kim SY, Miettinen M, Smith C, Merino M, Tsokos M, et al. Succinate dehydrogenase mutation underlies global epigenomic divergence in gastrointestinal stromal tumor. Cancer Discov. 2013;3(6):648–57.
Wilson BG, Wang X, Shen X, McKenna ES, Lemieux ME, Cho YJ, et al. Epigenetic antagonism between polycomb and SWI/SNF complexes during oncogenic transformation. Cancer Cell. 2010;18(4):316–28.
Lee RS, Stewart C, Carter SL, Ambrogio L, Cibulskis K, Sougnez C, et al. A remarkably simple genome underlies highly malignant pediatric rhabdoid cancers. J Clin Invest. 2012;122(8):2983–8.
Kadoch C, Crabtree GR. Reversible disruption of mSWI/SNF (BAF) complexes by the SS18-SSX oncogenic fusion in synovial sarcoma. Cell. 2013;153(1):71–85.
Guillou L, Aurias A. Soft tissue sarcomas with complex genomic profiles. Virchows Arch. 2010;456(2):201–17.
Liau JY, Lee JC, Tsai JH, Yang CY, Liu TL, Ke ZL, Hsu HH, Jeng YM. Comprehensive screening of alternative lengthening of telomeres phenotype and loss of ATRX expression in sarcomas. Mod Pathol. 2015;28(12):1545–54.
Garsed DW, Marshall OJ, Corbin VD, Hsu A, Di Stefano L, Schroder J, et al. The architecture and evolution of cancer neochromosomes. Cancer Cell. 2014;26(5):653–67.
Savage SA, Mirabello L. Using epidemiology and genomics to understand osteosarcoma etiology. Sarcoma. 2011;2011:548151.
Broadhead ML, Clark JC, Myers DE, Dass CR, Choong PF. The molecular pathogenesis of osteosarcoma: a review. Sarcoma. 2011;2011:959248.
Stephens PJ, Greenman CD, Fu B, Yang F, Bignell GR, Mudie LJ, et al. Massive genomic rearrangement acquired in a single catastrophic event during cancer development. Cell. 2011;144(1):27–40.
Chen X, Bahrami A, Pappo A, Easton J, Dalton J, Hedlund E, et al. Recurrent somatic structural variations contribute to tumorigenesis in pediatric osteosarcoma. Cell Rep. 2014;7(1):104–12.
Dourmishev LA, Dourmishev AL, Palmeri D, Schwartz RA, Lukac DM. Molecular genetics of Kaposi’s sarcoma-associated herpesvirus (human herpesvirus-8) epidemiology and pathogenesis. Microbiol Mol Biol Rev. 2003;67(2):175–212, table of contents.
McClain KL, Leach CT, Jenson HB, Joshi VV, Pollock BH, Parmley RT, et al. Association of Epstein-Barr virus with leiomyosarcomas in young people with AIDS. N Engl J Med. 1995;332(1):12–8.
Dawlatly SL, Dramis A, Sumathi VP, Grimer RJ. Stewart-Treves syndrome and the use of positron emission tomographic scanning. Ann Vasc Surg. 2011;25(5):699 e1–3.
Shon W, Ida CM, Boland-Froemming JM, Rose PS, Folpe A. Cutaneous angiosarcoma arising in massive localized lymphedema of the morbidly obese: a report of five cases and review of the literature. J Cutan Pathol. 2011;38(7):560–4.
Davidson T, Westbury G, Harmer CL. Radiation-induced soft-tissue sarcoma. Br J Surg. 1986;73(4):308–9.
Karlsson P, Holmberg E, Samuelsson A, Johansson KA, Wallgren A. Soft tissue sarcoma after treatment for breast cancer—a Swedish population-based study. Eur J Cancer. 1998;34(13):2068–75.
Arlen M, Higinbotham NL, Huvos AG, Marcove RC, Miller T, Shah IC. Radiation-induced sarcoma of bone. Cancer. 1971;28(5):1087–99.
Pisters PW. Preoperative chemotherapy and split-course radiation therapy for patients with localized soft tissue sarcomas: home run, base hit, or strike out? J Clin Oncol. 2006;24(4):549–51.
Tucker MA, D’Angio GJ, Boice JD Jr, Strong LC, Li FP, Stovall M, et al. Bone sarcomas linked to radiotherapy and chemotherapy in children. N Engl J Med. 1987;317(10):588–93.
Brady MS, Gaynor JJ, Brennan MF. Radiation-associated sarcoma of bone and soft tissue. Arch Surg. 1992;127(12):1379–85.
Billings SD, McKenney JK, Folpe AL, Hardacre MC, Weiss SW. Cutaneous angiosarcoma following breast-conserving surgery and radiation: an analysis of 27 cases. Am J Surg Pathol. 2004;28(6):781–8.
Falk H, Herbert J, Crowley S, Ishak KG, Thomas LB, Popper H, et al. Epidemiology of hepatic angiosarcoma in the United States: 1964-1974. Environ Health Perspect. 1981;41:107–13.
Kogevinas M, Ferro G, Saracci R, Andersen A, Biocca M, Coggon D, et al. Cancer mortality in an international cohort of workers exposed to styrene. IARC Sci Publ. 1993;127:289–300.
Zambon P, Ricci P, Bovo E, Casula A, Gattolin M, Fiore AR, et al. Sarcoma risk and dioxin emissions from incinerators and industrial plants: a population-based case-control study (Italy). Environ Health. 2007;6:19.
Pahwa P, McDuffie HH, Dosman JA, McLaughlin JR, Spinelli JJ, Robson D, et al. Hodgkin lymphoma, multiple myeloma, soft tissue sarcomas, insect repellents, and phenoxyherbicides. J Occup Environ Med. 2006;48(3):264–74.
Balarajan R, Acheson ED. Soft tissue sarcomas in agriculture and forestry workers. J Epidemiol Community Health. 1984;38(2):113–6.
Eriksson M, Hardell L, Adami HO. Exposure to dioxins as a risk factor for soft tissue sarcoma: a population-based case-control study. J Natl Cancer Inst. 1990;82(6):486–90.
Hardell L, Lindstrom G, van Bavel B, Fredrikson M, Liljegren G. Some aspects of the etiology of non-Hodgkin’s lymphoma. Environ Health Perspect. 1998;106(Suppl 2):679–81.
Rhodes MC, Bucher JR, Peckham JC, Kissling GE, Hejtmancik MR, Chhabra RS. Carcinogenesis studies of benzophenone in rats and mice. Food Chem Toxicol. 2007;45(5):843–51.
Piscitelli D, Ruggeri E, Fiore MG, Rossi R, Guerriero S. Undifferentiated high-grade pleomorphic sarcoma in a blind eye with a silicone prosthesis implant: a clinico-pathologic study. Orbit. 2011;30(4):192–4.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Kabir, W., Choong, P.F.M. (2021). The Epidemiology and Pathogenesis of Sarcoma. In: Choong, P.F.M. (eds) Sarcoma . Springer, Singapore. https://doi.org/10.1007/978-981-15-9414-4_2
Download citation
DOI: https://doi.org/10.1007/978-981-15-9414-4_2
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-15-9413-7
Online ISBN: 978-981-15-9414-4
eBook Packages: MedicineMedicine (R0)