Abstract
Microsporidia are obligate intracellular parasites that can affect individuals irrespective of immune status. The intracellular spore is the infective form of the organism with the characteristic polar tubule. Ocular microsporidiosis predominantly affects the cornea and can manifest either in the form of superficial epithelial keratopathy or deep stromal keratitis. Systemic and local immunosuppression has been found to be associated with this entity. Usually, history of trauma or exposure to environmental agents such as dust, dirty water, soil, insects, or bathing in unclean river water may predispose to such infections. The epithelial lesions typically present as multifocal, coarse, round-oval lesions with typical “stuck on” appearance. Often it becomes difficult to differentiate from adenoviral keratoconjunctivitis and Thygeson’s superficial punctate keratopathy. Stromal involvement presents as chronic, grayish white infiltration clinically mimicking HSV stromal keratitis. KOH + CFW and Ziehl–Neelsen stain have been found to be the most sensitive test for identification of the spores. Superficial variant is usually self-limited and there exists no specific treatment. Nevertheless, therapeutic debridement at times may be of some help. Microsporidial stromal keratitis requires surgical intervention for definite treatment in the form of lamellar or penetrating keratoplasty.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
10.1 Introduction
Microsporidia are eukaryotic unicellular organisms belonging to phylum Microspora and kingdom Protista [1,2,3]. Recently, it has been classified as fungi [4]. It infects both vertebrates and invertebrates. Microsporidiosis occurs worldwide. The prevalence varies depending on the region, method of diagnosis, and characteristic of population. This pathogen can affect eye, respiratory tract, intestine, muscles, kidneys, and central nervous system.
10.2 Organism
The number of microsporidian species are estimated to be between 1000 to 1500. The common genera involved in human disease are Encephalitozoon (Septata), Nosema, Vittaforma, Pleistophora, Trachipleistophora, and Anncaliia (Brachiola) [4].
Microsporidia exists as a single highly organized spore [5]. The size of the spore varies from 1 to 40 μm. The intracellular spore is the infective form of the organism. A normal unit membrane and two rigid extracellular walls bind the spores. Within the spore membrane is the sporoplasm, which is infective material of microsporidia. The most obvious organelle associated with infection is the polar filament or the polar tube. The polar filament is attached to the apex of the spore via anchoring disk, from which it extends to the posterior end of the spore. The number of coils and their arrangement is diagnostic of particular species [6]. Inside the host cell, there are two distinct phases in the development of microsporidia: a proliferative phase (merogony) and a sporogonic phase (sporogony).
10.3 Risk Factors
Although fecal-oral transmission is the likely route of intestinal microsporidiosis, the source of ocular infection is not clear. There are two distinct clinical microsporidial corneal infections: keratoconjunctivitis and stromal keratitis. Several cases of microsporidial keratoconjunctivitis have been reported in patients infected with human immunodeficiency virus (HIV) [7,8,9,10]. However, keratoconjunctivitis has been reported in healthy individuals in recent reports [11,12,13,14]. Systemic immunosuppression has been associated with keratoconjunctivitis [15]. The contact lens may act as a vector for an organism to reach the cornea, either by prolonging retention on the ocular surface or by the colonization of organism on contact lens reaching the eye [16, 17].
Topical corticosteroid may predispose to microsporidial infection by local immunosuppression. It has been reported in a corneal graft [18]. Association with trauma has been reported [12, 13]. Close contact with domestic animals may be a source of ocular infection [9, 19]. Exposure to muddy water has been described as a risk factor for keratoconjunctivitis [17].
10.4 Clinical Features
Microsporidia primarily affects the cornea and may present either in the form of superficial epithelial keratopathy or deep stromal keratitis. Rarely uvea and sclera have been reported to be involved [20]. In the past, the two clinical entities have been described, the superficial epithelial variant commonly seen in immunocompromised persons and the deep stromal keratitis seen in immunocompetent individuals [20]. Keratoconjunctivitis is mostly caused by the genus Encephalitozoon and stromal keratitis by Nosema and Microsporidium [13].
10.4.1 Keratoconjunctivitis
The first case of microsporidial infection was reported by Lowder et al. [21] in a young seropositive man who had a chronic history of conjunctivitis nonresponding to topical antibiotics. Patients present with history of “red eye” presumed to be of viral etiology and are often pretreated with steroids. They complain of unilateral or rarely bilateral pain, redness, photophobia, and watering along with blurring of vision. Past history of trauma or exposure to environmental agents such as dust, dirty water, soil, insects, or bathing in unclean river water may be present.
Slit lamp biomicroscopy reveals diffuse, multifocal, elevated, coarse, and round-oval lesions with characteristic “stuck on” appearance (Fig. 10.1). These lesions may be epithelial, subepithelial, or involve anterior stroma. They may or may not stain positively with fluorescein. Surrounding conjunctiva appears mild-moderately congested, nonpurulent with papillary and/or follicular response [13]. Lewis et al. have reported a case of microsporidial keratoconjunctivitis in a 33-year-old immunocompetent patient who had follicular conjunctivitis and diffuse punctate lesions with anterior stromal involvement [22]. Fresh, pigmented keratic precipitates were reported in 20.1% of patients presenting with superficial keratoconjunctivitis and appeared 6.9 ± 2.7 days after presentation [12]. Multiple “target like” epithelial lesions along with classic punctate lesions were described by Raymond and coworkers [17]. Recent reports have shown that microsporidial keratoconjunctivitis can occur in healthy immunocompetent individuals contrary to previously published reports. It occurs more commonly than believed and the punctate lesions can be mistaken easily for adenoviral infection even to trained eyes.
10.4.2 Stromal Keratitis
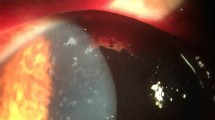
Stromal keratitis has an indolent course and can affect individuals of any age. This entity is less common than the superficial variant. First reported in 1991, it clinically resembles HSV keratitis and often treated with antivirals and steroids with no response. Clinically, it presents with diffuse congestion, grayish white stromal infiltration, and edema without suppuration (Fig. 10.2). It may have a chronic course with corneal opacity with vascularization [23]. Anterior chamber involvement manifesting as cellular reaction is common.
Case report of microsporidial keratoconjunctivitis causing sclerouveitis and retinal detachment has been reported [24]. Spores of microsporidia were detected in vitrectomy samples. Endophthalmitis has been reported in patients suffering from Acute myelogenous leukemia [25]. Limbitis can also develop in requiring addition of topical corticosteroids.
10.5 Differential Diagnosis
10.5.1 Keratoconjunctivitis
Microsporidia | Adenoviral | Thygeson’s SPK | |
|---|---|---|---|
Laterality | Usually unilateral | Bilateral in 70% cases | Asymmetrically bilateral |
Lesions | Multifocal, elevated, coarse, round-oval lesions, “stuck-on” appearance | Multifocal, fine punctate subepithelial infiltrates as a result of cellular reaction against viral antigens | Coarse, oval shaped, slightly raised lesions |
Appearance of lesions | Appears in one phase | Gradually appear | Evanescent pattern |
Location | Epithelial, subepithelial, anterior stromal | Subepithelial | Classically intraepithelial, but can be subepithelial and anterior stromal |
Staining pattern (fluorescein) | Stains positively and negatively | Stains positively | Stains minimally |
Duration | Mean duration of symptoms was 7.7 ± 6.2 (range: 1–60) days | 1–2 weeks but may persist for longer duration | 2 months to 41 years |
Conjunctival involvement | Papillary and or follicular reaction | Follicular conjunctivitis | Rarely involved |
Treatment | Lubricants | Lubricants and topical steroids, PTK | Topical steroids, tacrolimus, cyclosporine, BCL, PTK |
Scarring | Rarely scars only if subepithelial | Usually subepithelial haze and scarring noticed | Scars when Bowman’s membrane and anterior stroma involved |
Systemic associations | None | Pharyngoconjunctival fever | Viral associations-Varicella zoster, HSV, HLADR3 |
10.5.2 Stromal Keratitis
Microsporidial stromal keratitis presents as multifocal, dense grayish infiltrates with surrounding edema, endoexudates, and keratic precipitates with or without vascularization. The abovementioned clinical features along with prolong history of recurrent redness with partial and no response to steroids should create a high index of suspicion for microsporidial etiology [26].
10.5.2.1 HSV Stromal Keratitis
HSV stromal keratitis can present primarily in two forms: the commoner being non-necrotizing variant and the less common necrotizing one. Microsporidial stromal keratitis is often misdiagnosed as non-necrotizing variant due to its indolent nature and early response to steroids. It present as a focal, multifocal, or diffuse infiltration associated with scarring, thinning, and vascularization.
10.5.3 Acanthamoeba Keratitis
Acanthamoeba keratitis patients present with severe pain out of proportion to the clinical signs. Few typical features seen in the early stage are punctate keratopathy, pseudodendrites, epithelial and subepithelial infiltrates, and classic perineural infiltrates. Later may develop anterior uveitis, hypopyon, and occasionally lead to endothelial plaque and disciform like stromal edema. History of previous contact lens wear may be helpful in clinching towards the diagnosis. However, microbiological workup is necessary to confirm the diagnosis [27].
10.6 Diagnosis
There are several methods to detect microsporidia. Ocular specimens are submitted as corneal scrapings and corneal biopsy. Formalin (5–10%) fixation is required for routine histopathology, glutaraldehyde for electron microscopy, and fresh specimens for molecular methods and cell cultures [28].
10.6.1 Smears and Stains
Staining techniques that have been recommended for the detection of microsporidial spores include Gram, Giemsa, 10% potassium hydroxide with calcofluor white (KOH + CFW) wet mount, modified Ziehl–Neelsen, modified trichrome, and immunofluorescence tests. In a retrospective analysis of the relative performance of four standard techniques for detection of Microsporidia included Gram, Giemsa, 10% KOH + CFW, and Ziehl–Neelsen staining. Ziehl–Neelsen and 10% KOH + CFW were found to be most sensitive in the identification of the spores followed by Gram and Giemsa. Giemsa was reported to have the least efficacious among the four techniques [29].
10.6.2 Histopathology and Tissue Stains
Numerous stains have been described for detection of spores in histopathology specimens comprising biopsy and scrapings. Tissue gram stain (Brown-Hopps and Brown-Brenn) show birefringence of the spores that distinguishes them from intracytoplasmic granules, debris, etc. Spores appear as oval nonbudding intracellular or extracellular structures. Gram stain, Giemsa, calcofluor white, modified Ziehl–Neelsen (1% H2SO4), and Warthin-Starry (silver stain) are most effective in detecting spores. Hematoxylin and Eosin stains the spores as refractile gold bodies and is not reliable in routine formalin-fixed specimens [20, 28].
10.6.3 Transmission Electron Microscopy (TEM)
TEM remains the gold standard for detection and species identification of microsporidial spores. Microsporidial spores have a characteristic polar tubule that is required to inject contents of the sporoplasm intracellularly. However, TEM is not easily accessible to most laboratories, and species-level identification may need additional molecular or cell culture techniques [28, 30].
10.6.4 Confocal Microscopy
Confocal microscopy is a useful method to scan the cornea in vivo and an useful noninvasive adjunct for the diagnosis of infective keratitis [31]. Tiny intraepithelial opacities were seen in epithelial keratitis that were corroborated to be microsporidia in chromatrope stains of conjunctival scraping [32]. Microsporidia appear as hyperreflective dots in between keratocytes against a dark background of the confocal image in deep stromal keratitis. The spores are aligned along the corneal lamella in microsporidial stromal disease [33]. The hyperreflective dots suggestive of spores disappeared on treatment. Thus, confocal microscopy assists in imaging and monitoring the progress of deep-seated corneal lesions.
10.6.5 Antigen-Based Assays
Antigen-based detection of microsporidia uses antibodies to identify species of microsporidia by immunofluorescence assay (IFA) as antibodies against particular species are available [34]. Washed spores of Encephalitazoon are injected into mice to produce antiserum which was adsorbed with formalin fixed fecal debris to remove cross reacting antibodies. Pooled antiserum was tagged with fluorescein to stain histopathology specimens. Microsporidia spores showed apple green fluorescence [34, 35]. An experiment comparing three stains—calcofluor white, modified trichrome blue, and IFA with TEM as a standard of reference—reported sensitivity of 83.3% for IFA as opposed to 100% sensitivity of calcofluor white and modified trichrome blue. Specificity was higher at 96% with IFA technique. This is important for species identification if species-specific antibodies are available [35, 36].
10.6.6 Cell Culture
Microsporidia are obligate intracellular parasites that can be cultivated in a variety of cell lines by primary cell cultures. These include monkey and rabbit kidney (vero and RK13), Madin-Darby canine kidney, human fetal lung fibroblasts (MRC-%), etc. The monolayer cell culture can help to propagate the parasite by replenishing the growth medium and allows harvesting of large number of spores. In a comparison of growth-promoting properties of three cell lines for four types of microsporidial species, Joseph et al. reported good growth in SIRC cells for E. cuniculi and E. intestinalis at an inoculum size of 1 × 10 [4] spores/ml compared to HeLa cell lines [37]. The technique of cultivating microsporidia from cell lines is time consuming, expensive, and with limited availability to a few laboratories. However, inclusion of cell lines whenever available improves the diagnostic yield and is an important step for developing molecular diagnostic methods.
10.6.7 PCR-Based Molecular Methods
Polymerase chain reaction (PCR) based assays have improved the sensitivity and specificity of detection of Microsporidia. Small and large subunit rRNA and intergenic sequences have highly conserved regions that may be amplified and detected as a target sequence. A sequencing and BLAST analysis helps in validating the results. Joseph et al. have reported the use of pan microsporidian 16S rRNA for identification of E. hellum, E. cuniculi, and E. intestinalis in ocular samples for patients with microsporidial keratitis [38]. They have reported a sensitivity of 83% and specificity of 98%. Due to limitation of PCR-based assays such as laborious and reagent consuming processes of extraction of microsporidian DNA and design of species-specific primers, an alternative technique is an oligonucleotide probe. Species-specific oligonucleotide microarray probes produced from specific 18S SSU-rRNA genes immobilized on a microchip can detect four microsporidian species. Clinical samples detected that coinfection with various species is quite common. This technique can reliably detect samples containing as less as 100 spores [39].
10.7 Treatment
Microsporidia can affect individuals irrespective of immune status. It may cause ocular manifestations such as keratoconjunctivitis or stromal keratitis. Several drugs have been described for the treatment, viz., fluoroquinolone, fumagillin, albendazole, and itraconazole. The management of microsporidia can be described under two subcategories: keratoconjunctivitis and stromal keratitis.
No definitive treatment regimen exists for microsporidial keratoconjunctivitis. While several drugs have been reported to have a therapeutic effect the condition is known to resolve on its own. A single-center double-masked randomized control trial subdivided 145 patients in two arms of 0.05% polyhexamethylene biguanide (PHMB) versus lubricants for management of microsporidial keratoconjunctivitis. The mean resolution time was 4.9 ± 2.2 and 4.6 ± 2.3 days with PHMB and lubricants, respectively. The study conclusively provided evidence of the self-limiting nature of the condition [40]. In a retrospective case series, topical fluoroquinolones, fumagillin 0.3%, and oral albendazole were administered. The study recommended topical monotherapy with fluoroquinolones as a viable first-line treatment option in microsporidial keratitis, the visual acuity was largely unaffected and associated corneal edema and limbitis needed adjuvant corticosteroid treatment [17]. Debridement of the epithelial lesions has also been reported to have beneficial effects in debulking the cornea of infective load and hastening resolution [41]. Despite a multitude of treatment options microsporidial keratoconjunctivitis remains a self-limited disease with 75% of patients regaining 20/30 vision or better with a mean resolution time of 6.0 ± 2.9 days with no specific treatment or placebo [12].
Microsporidial stromal keratitis is the possible diagnosis in chronic culture-negative stromal keratitis. Fumagillin, a methionine aminopeptidase 2 inhibitor, has been described on the management of microsporidial stromal keratitis. Topical chlorhexidine gluconate 0.02% in combination with albendazole has been described for management of stromal keratitis. It requires long-term therapy of several weeks duration [42].
The definitive treatment of microsporidial stromal keratitis remains surgical as the disease tends to smolder in the deeper stromal layers. Often the topical drugs are unable to eliminate deep stromal infection and the treatment options include deep anterior lamellar keratoplasty (DALK) or full thickness penetrating keratoplasty (PKP). Big bubble DALK with removal of all stromal tissue may lead to complete eradication of the disease without recurrences and has been described to have a favorable outcome in stromal microsporidiosis [43]. Microsporidial spores have been reported to cross the Descemet’s membrane and are also found in the anterior chamber exudates [44]. Recurrences have been described post DALK for microsporidial stromal keratitis if there is insufficient removal of the stromal layers or the organism has crossed the Descemet’s membrane [45].
Microsporidial stromal keratitis may present as a slow indolent deep stromal keratitis of 1 month to several years duration. There is no definitive treatment for this condition and often the disease natural history is marred by episodic inflammation, corneal thinning, and recurrences. It has also been reported to cross the Descemet’s membrane. Therefore, the definitive treatment includes complete removal of the diseased cornea by performing full thickness PKP in order to eradicate the infection and achieve disease-free remission [46]. In a large case series of 34 patients of microbiologically proven microsporidial stromal keratitis, five patients responded to topical PHMB 0.02% and Chlorhexidine 0.02% with formation of a vascularized corneal scar. Twenty five patients required keratoplasty of which 21 were full thickness grafts. All the patients had control of infection post PKP. Five of 25 grafts were clear at the end of 1 year of follow-up. The only case of recurrence was noted in a patient who had DALK and seven patients were lost to follow-up. The study concluded that surgical excision is the best management option for the treatment of microsporidial stromal keratitis [47]. Post penetrating keratoplasty treatment regimen included use of topical corticosteroids as in routine PKP procedures.
References
Weber R, Bryan RT, Schwartz DA, Owen RL. Human microsporidial infections. Clin Microbiol Rev. 1994;7(4):426–61.
Friedberg DN, Ritterband DC. Ocular microsporidiosis. In: Wittner M, Weiss LM, editors. The microsporidia and microsporidiosis. Washington DC: ASM Press; 1999. p. 293–313.
Keeling PJ, Fast NM. Microsporidia: biology and evolution of highly reduced intracellular parasites. Annu Rev Microbiol. 2002;56:93–116.
Franzen C. Microsporidia: a review of 150 years of research. Open Parasitol J. 2008;2:1–34.
Vávra J, Larsson JIR. Structure of the microsporidia. In: Wittner M, Weiss LM, editors. The microsporidia and microsporidiosis. Washington DC: ASM Press; 1999. p. 7–84.
Sprague V, Becnel JJ, Hazard EI. Taxonomy of phylum microspora. Crit Rev Microbiol. 1992;18(5–6):285–395.
Friedberg DN, Stenson SM, Orenstein JM, Tierno PM, Charles NC. Microsporidial keratoconjunctivitis in acquired immunodeficiency syndrome. Arch Ophthalmol. 1990;108(4):504–8.
Lowder CY, McMahon JT, Meisler DM, Dodds EM, Calabrese LH, Didier ES, Cali A. Microsporidial keratoconjunctivitis caused by Septata intestinalis in a patient with acquired immunodeficiency syndrome. Am J Ophthalmol. 1996;121(6):715–7.
McCluskey PJ, Goonan PV, Marriott DJ, Field AS. Microsporidial keratoconjunctivitis in AIDS. Eye. 1993;7(1):80–3.
Yee RW, Tio FO, Martinez JA, Held KS, Shadduck JA, Didier ES. Resolution of microsporidial epithelial keratopathy in a patient with AIDS. Ophthalmology. 1991;98(2):196–201.
Chan CM, Theng JT, Li L, Tan DT. Microsporidial keratoconjunctivitis in healthy individuals: a case series. Ophthalmology. 2003;110(7):1420–5.
Das S, Sharma S, Sahu SK, Nayak SS, Kar S. Diagnosis, clinical features and treatment outcome of microsporidial keratoconjunctivitis. Br J Ophthalmol. 2012;96(6):793–5.
Joseph J, Sridhar MS, Murthy S, Sharma S. Clinical and microbiological profile of microsporidial keratoconjunctivitis in southern India. Ophthalmology. 2006;113(4):531–7.
Agashe R, Radhakrishnan N, Pradhan S, Srinivasan M, Prajna VN, Lalitha P. Clinical and demographic study of microsporidial keratoconjunctivitis in South India: a 3-year study (2013-2015). Br J Ophthalmol. 2017;101(10):1436–9.
Silverstein BE, Cunningham ET Jr, Margolis TP, Cevallos V, Wong IG. Microsporidial keratoconjunctivitis in a patient without human immunodeficiency virus infection. Am J Ophthalmol. 1997;124(3):395–6.
Theng J, Chan C, Ling ML, Tan D. Microsporidial keratoconjunctivitis in a healthy contact lens wearer without human immunodeficiency virus infection. Ophthalmology. 2001;108(5):976–8.
Loh RS, Chan CM, Ti SE, Lim L, Chan KS, Tan DT. Emerging prevalence of microsporidial keratitis in Singapore: epidemiology, clinical features, and management. Ophthalmology. 2009;116(12):2348–53.
Kakrania R, Joseph J, Vaddavalli PK, Gangopadhyay N, Sharma S. Microsporidia keratoconjunctivitis in a corneal graft. Eye. 2006;20(11):1314–5.
Didier ES, Didier PJ, Friedberg DN, Stenson SM, Orenstein JM, Yee RW, Tio FO, Davis RM, Vossbrinck C, Millichamp N, Shadduck JA. Isolation and characterization of a new human microsporidian, Encephalitozoon hellem (n. sp.), from three AIDS patients with keratoconjunctivitis. J Infect Dis. 1991;163(3):617–21.
Sharma S, Das S, Joseph J, Vemuganti GK, Murthy S. Microsporidial keratitis: need for increased awareness. Surv Ophthalmol. 2011;56(1):1–22.
Lowder CY, Meisler DM, McMahon JT, Longworth DL, Rutherford I. Microsporidia infection of the cornea in a man seropositive for human immunodeficiency virus. Am J Ophthalmol. 1990;109(2):242–4.
Lewis NL, Francis IC, Hawkins GS, Coroneo MT. Bilateral microsporidial keratoconjunctivitis in an immunocompetent non-contact lens wearer. Cornea. 2003;22(4):374–6.
Rauz S, Tuft S, Dart JKG, Bonshek R, Luthert P, Curry A. Ultrastructural examination of two cases of stromal microsporidial keratitis. J Med Microbiol. 2004;53(8):775–81.
Mietz H, Franzen C, Hoppe T, Bartz-Schmidt KU. Microsporidia-induced sclerouveitis with retinal detachment. Arch Ophthalmol. 2002;120(6):864–5.
Yoken J, Forbes B, Maguire AM, Prenner JL, Carpentieri D. Microsporidial endophthalmitis in a patient with acute myelogenous leukemia. Retina. 2002;22(1):123–5.
Garg P. Microsporidia infection of the cornea-a unique and challenging disease. Cornea. 2013;32(Suppl-1):S33–8.
Dart JK, Saw VP, Kilvington S. Acanthamoeba keratitis: diagnosis and treatment update 2009. Am J Ophthalmol. 2009;148(4):487–99.
Garcia LS. Laboratory identification of the microsporidia. J Clin Microbiol. 2002;40(6):1892–901.
Joseph J, Murthy S, Garg P, Sharma S. Use of different stains for microscopic evaluation of corneal scrapings for diagnosis of microsporidial keratitis. J Clin Microbiol. 2006;44(2):583–5.
Xu Y, Weiss LM. The microsporidian polar tube: a highly specialised invasion organelle. Int J Parasitol. 2005;35(9):941–53.
Hau SC, Dart JK, Vesaluoma M, Parmar DN, Claerhout I, Bibi K, Larkin DF. Diagnostic accuracy of microbial keratitis with in vivo scanning laser confocal microscopy. Br J Ophthalmol. 2010;94(8):982–7.
Shah GK, Pfister D, Probst LE, Ferrieri P, Holland E. Diagnosis of microsporidial keratitis by confocal microscopy and the chromatrope stain. Am J Ophthalmol. 1996;121(1):89–91.
Sagoo MS, Mehta JS, Hau S, Irion LD, Curry A, Bonshek RE, Tuft SJ. Microsporidium stromal keratitis: in vivo confocal findings. Cornea. 2007;26(7):870–3.
Schwartz DA, Visvesvara GS, Diesenhouse MC, Weber R, Font RL, Wilson LA, Corrent G, Serdarevic ON, Rosberger DF, Keenen PC, Grossnikiaus HE, Hewan-Lowe K, Bryan RT. Pathologic features and immunofluorescent antibody demonstration of ocular microsporidiosis (Encephalitozoon hellem) in seven patients with acquired immunodeficiency syndrome. Am J Ophthalmol. 1993;115(3):285–92.
Didier ES, Orenstein JM, Aldras A, Bertucci D, Rogers LB, Janney FA. Comparison of three staining methods for detecting microsporidia in fluids. J Clin Microbiol. 1995;33(12):3138–45.
Aldras AM, Orenstein JM, Kotler DP, Shadduck JA, Didier ES. Detection of microsporidia by indirect immunofluorescence antibody test using polyclonal and monoclonal antibodies. J Clin Microbiol. 1994;32(3):608–12.
Joseph J, Sharma S. In vitro culture of various species of microsporidia causing keratitis: evaluation of three immortalized cell lines. Indian J Med Microbiol. 2009;27(1):35–9.
Joseph J, Sharma S, Murthy SI, Krishna PV, Garg P, Nutheti R, Kenneth J, Balasubramanian D. Microsporidial keratitis in India: 16S rRNA gene-based PCR assay for diagnosis and species identification of microsporidia in clinical samples. Invest Ophthalmol Vis Sci. 2006;47(10):4468–73.
Wang Z, Orlandi PA, Stenger DA. Simultaneous detection of four human pathogenic microsporidian species from clinical samples by oligonucleotide microarray. J Clin Microbiol. 2005;43(8):4121–8.
Das S, Sahu SK, Sharma S, Nayak SS, Kar S. Clinical trial of 0.02% polyhexamethylene biguanide versus placebo in the treatment of microsporidial keratoconjunctivitis. Am J Ophthalmol. 2010;150(1):110–5.
Sridhar MS, Sharma S. Microsporidial keratoconjunctivitis in a HIV-seronegative patient treated with debridement and oral itraconazole. Am J Ophthalmol. 2003;136(4):745–6.
Sangit VA, Murthy SI, Garg P. Microsporidial stromal keratitis successfully treated with medical therapy: a case report. Cornea. 2011;30(11):1264–6.
Ang M, Mehta JS, Mantoo S, Tan D. Deep anterior lamellar keratoplasty to treat microsporidial stromal keratitis. Cornea. 2009;28(7):832–5.
Murthy SI, Sangit VA, Rathi VM, Vemuganti GK. Microsporidial spores can cross the intact Descemet membrane in deep stromal infection. Middle East Afr J Ophthalmol. 2013;20(1):80–2.
Font RL, Samaha AN, Keener MJ, Chevez-Barrios P, Goosey JD. Corneal microsporidiosis. Report of case, including electron microscopic observations. Ophthalmology. 2000;107(9):1769–75.
Vemuganti GK, Garg P, Sharma S, Joseph J, Gopinathan U, Singh S. Is microsporidial keratitis an emerging cause of stromal keratitis? A case series study. BMC Ophthalmol. 2005;5:19.
Sabhapandit S, Murthy SI, Garg P, Korwar V, Vemuganti GK, Sharma S. Microsporidial stromal keratitis: clinical features, unique diagnostic criteria, and treatment outcomes in a large case series. Cornea. 2016;35(12):1569–74.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Das, S., Priyadarshini, S.R., Roy, A. (2021). Microsporidial Keratitis. In: Das, S., Jhanji, V. (eds) Infections of the Cornea and Conjunctiva. Springer, Singapore. https://doi.org/10.1007/978-981-15-8811-2_10
Download citation
DOI: https://doi.org/10.1007/978-981-15-8811-2_10
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-15-8810-5
Online ISBN: 978-981-15-8811-2
eBook Packages: MedicineMedicine (R0)