Abstract
Oral cancer which is also known as mouth cancer is defined as a malignant neoplasm arising in the oral cavity or on the lip. Although the term oral cancer is synonymous with oral squamous cell carcinoma (OSCC), various other malignancies such as malignant melanoma, different types of sarcomas, salivary gland cancers, and odontogenic malignancies account for a small proportion of total oral cancers. This chapter illustrates more than 30 different clinical presentations of oral cancers.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords

-
1.
A 42-year-old man came with a non-healing ulcer on the tongue.
-
(a)
What is the most likely diagnosis?
-
(b)
List two clinical features in this lesion that can affect the prognosis.
-
(c)
What are the possible etiological factors for this condition?

-
(a)
-
2.
A 48-year-old man came with a nonhealing ulcer on the tongue.
-
(a)
What is the most likely diagnosis?
-
(b)
List three clinical features which help in diagnosing this lesion.

-
(a)
-
3.
A 62-year-old man came with an exophytic lesion on the tongue.
-
(a)
List the differential diagnoses.
-
(b)
What is the investigation that should be carried out in order to confirm the diagnosis?
-
(a)
-
4.
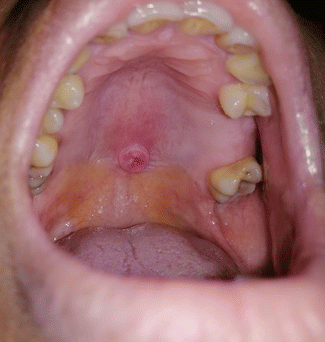
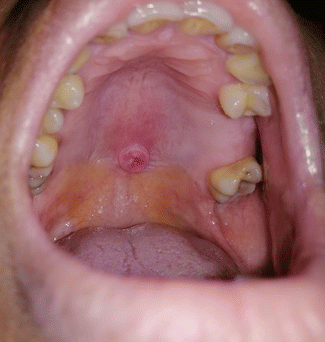
A 32-year-old patient came with an ulcer on the palate.
-
(a)
State the differential diagnoses.
-
(b)
What is the most likely diagnosis?
-
(c)
What is the investigation that you would carry out to confirm the diagnosis?
-
(a)
-
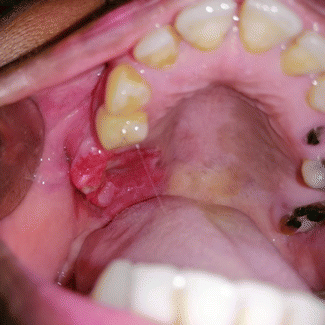
5.
A 47-year-old man came with a nonhealing ulcer on the posterior plate. He does not use tobacco, areca nut, or alcohol. He was diagnosed with diabetes and having a poor diabetic control.
-
(a)
What are your differential diagnoses?
-
(b)
What is the most likely diagnosis?
-
(c)
List three investigations that you would carry out in this patient.

-
(a)
-
6.
A 32-year-old woman came with an exophytic ulcerative lesion on the lower lip.
-
(a)
What is the most likely diagnosis?
-
(b)
List two clinical features in this lesion that can affect the prognosis.

-
(a)
-
7.
A 62-year-old man came with a white patch on the buccal mucosa extending to commissural region.
-
(a)
What is the most likely diagnosis?
-
(b)
How would you investigate this patient in order to arrive at a definitive diagnosis?

-
(a)
-
8.
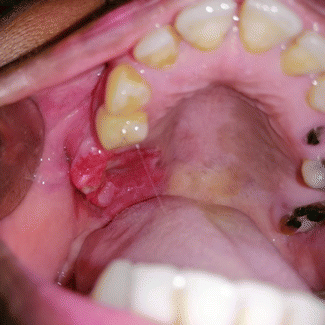
A 32-year-old patient came with an ulcer on the palate.
-
(a)
State the differential diagnoses?
-
(b)
What is the most likely diagnosis?
-
(c)
What is the investigation that you would carry out to confirm the diagnosis?
-
(a)
Answers
-
1.
-
(a)
Oral cancer.
-
(b)
Larger size, site (tongue).
-
(c)
Tobacco, areca nut, alcohol, HPV infection.
-
(a)
-
2
-
(a)
Oral cancer.
-
(b)
Rolled edges, induration, necrotic center.
-
(a)
-
3.
-
(a)
Verrucous carcinoma, verrucous leukoplakia, papilloma.
-
(b)
Incisional biopsy.
-
(a)
-
4.
-
(a)
Minor salivary gland tumor, papilloma, fibroepithelial hyperplasia.
-
(b)
Minor salivary gland tumor.
-
(c)
FNAC, incisional biopsy.
-
(a)
-
5.
-
(a)
Deep fungal infection, oral cancer, or any other malignancy.
-
(b)
Deep fungal infection.
-
(c)
Incisional biopsy, radiography to assess maxillary antrum, and microbiological test for a sample from the ulcer.
-
(a)
-
6.
-
(a)
Oral cancer.
-
(b)
Present on the lip and young age.
-
(a)
-
7.
-
(a)
Oral cancer arising in the background of leukoplakia.
-
(b)
Multiple incisional biopsies not to miss the transformed areas.
-
(a)
-
8.
-
(a)
Minor salivary gland tumor, SCC.
-
(b)
Minor salivary gland tumor.
-
(c)
FNAC, incisional biopsy.
-
(a)
1 Definitions of Oral Cancer
Oral cancer which is also known as mouth cancer is defined as a malignant neoplasm arising in the oral cavity or on the lip. Although the term oral cancer is synonymous with oral squamous cell carcinoma (OSCC), various other malignancies such as malignant melanoma, different types of sarcomas, salivary gland cancers, and odontogenic malignancies account for a small proportion of total oral cancers.
2 Epidemiology of Oral Cancer
Oral and pharyngeal cancer is a leading malignancy in some parts of the world. In the year 2018, the annual incidence of cancers of the lip and oral cavity exceeded 354,864 new cases, and it was the cause of approximately 177,384 deaths worldwide (Bray et al. 2018). Oral cancer(OSCC) which is the cancer of the oral cavity excluding the pharynx and oropharynx is a major health problem in South and Southeast Asia. Being the second most frequent cancer in Sri Lanka, oral cancer alone accounts for 12.7% of all cancers. It is the number one cancer in Sri Lankan males, and incidence among men was 15.6 per 100,000 population as reported in 2014. Most commonly it occurs in middle-aged and older individuals (Sri Lanka Cancer Registry).
According to the Sri Lanka Cancer Registry, lip, oral cavity, and pharynx are the leading cancer sites among Sri Lankan males. In 2005, it accounts for 20.4% of all the cancer, whereas it has increased up to 24.0% in 2010. Cancers of the lip, tongue, and mouth account for 18% in 2011 and 15.8% in 2014. Lip, oral cavity, and pharynx cancers account for 5.1% of all the cancers among Sri Lankan females, whereas it has increased up to 6.0% in 2010 (Sri Lanka Cancer Registry).
4 Human Papilloma Virus (HPV) and Oral Cancer
Human papilloma virus (HPV) infection has been increasingly recognized as a major etiologic factor for a subset of OSCC and OPMD. Oropharyngeal cancers are mostly due to HPV infection, and HPV-induced cancers differ in their behavior, treatment response, and prognosis compared to oral cavity cancers. E6 and E7 antigens of HPV destroy P53 and retinoblastoma onco-suppressor genes, respectively, and predispose the individual to develop cancer (Jayasooriya et al. 2003).
5 Clinical Features of Oral Cancer
Oral cancer is a life-threatening disease but an easily preventable and easily detectable cancer involving the oral cavity. It is preventable, as the primary etiological agents such as tobacco products, use of areca nut and heavy use of alcohol, and combination of these are identified as carcinogens. Therefore, it is not difficult to target preventive measures in order to avoid the use of these agents. More than 90% of oral cancer patients give a history of tobacco use. All forms of tobacco use are implicated, including the use of smokeless tobacco. Traditional betel quid used in South Asia contains both carcinogenic substances, tobacco, and areca nut. Early detection of oral cancer allows for 5-year survival rate of 90%. Unfortunately, most of the oral cancers are diagnosed at advanced stage, with a 5-year survival rate of 20%, and it has one of the worst prognosis of all major cancers. 60% of the oral cancers are diagnosed at advanced stage, namely, stage III and IV. No specialized techniques are required to examine the oral cavity for the presence of precursor lesions or early oral cancers. Prevention and early diagnosis are therefore of utmost importance.
Oral cancer is commonly seen in middle-aged and elderly males. Commonest anatomical site is the buccal mucosa followed by the tongue, alveolar mucosa, and floor of the mouth especially in South Asia (Siriwardena et al. 2015b).
Early lesions are usually painless and appear as small, apparently harmless areas of induration, erosion, or keratosis (Figs. 45.1, 45.2, 45.3, and 45.4), but advanced lesions present as a persistent painless ulcer with indurated and rolled margins (Figs. 45.5, 45.6, 45.7, 45.8, 45.9, 45.10, and 45.11). Many patients present with trismus or impaired tongue movement. Tumor may be fixed to underlying soft tissues or bone, and it spread to regional lymph nodes easily resulting in cervical lymphadenopathy (Figs. 45.12 and 45.13). Lymph nodes are usually painless unless secondarily infected. Rarely, patients present with persistent, severe pain due to involvement of nerves.
Warning signs and symptoms of oral cancer include:
-
1.
Ulcers, swellings, lumps, or thick patches anywhere in the mouth
-
2.
Areas of red or white lesions in the mouth
-
3.
Numbness, pain, or tenderness anywhere in the mouth
-
4.
Pain in one of the ears but without any loss of hearing
-
5.
Difficulties in moving the lower jaw or tongue or with chewing, swallowing, or speaking
-
6.
Mobility of teeth with no apparent dental cause
Oral cancer is subjected to the “field cancerization phenomenon,” having highest risk of development of second primary tumors out of any cancer. Other than the late presentation, this is considered as an important reason for poor prognosis. In addition to the possibility of occurrence of second primary, oral cancers can present as multiple tumors in multiple sites at the same time (Figs. 45.14 and 45.15). They are called as synchronous tumors. Surprisingly, single primary tumors have a poor prognosis than the synchronous tumors (Dissanayake and Tilakaratne 2011).
Soft tissue sarcomas such as leiomyosarcoma, rhabdomyosarcoma, malignant peripheral nerve sheath tumor, fibrosarcoma, liposarcoma, and various other entities also occur rarely in the oral mucosa (Figs. 45.16, and 45.17). They usually present as polypoid growths. Malignant melanomas of different histopathological types also occur in the oral mucosa as blackish nodular growths or irregular pigmented patches (Figs. 45.18, 45.19, and 45.20).
6 Differential Diagnoses
All chronic painless ulcers present in the mouth are not oral cancers. Infections like deep fungal infections (Figs. 45.21 and 45.22) or TB (Fig. 45.23), trauma (Fig. 45.24), major aphthous ulceration (Fig. 45.25), and many other conditions can mimic oral cancer clinically; therefore, confirmation of the clinical diagnosis with histopathology is essential.
7 Histopathological Features of Oral Cancer
Most of the oral cancers reported in Sri Lanka are squamous cell carcinomas (SCC). Multiple subtypes of squamous cell carcinomas have been reported other than the conventional type. Basaloid SCCs are common in the tongue, and adenosquamous carcinomas are more common in the palate, whereas verrucous carcinomas (Fig. 45.26) are more common in buccal mucosa especially in the commissural areas (Siriwardena et al. 2015a, b).
Oral squamous cell carcinoma arises from OPMDs with different grades of epithelial dysplasia or without a history of any preexisting lesion. The hallmark of OSCC is the breaching of basement membrane of the epithelium and epithelial cells invading into underlying connective tissue. These cells may invade as islands, thin strands, or individual cells. Depending on the level of differentiation, OSCC is graded into well, moderate, or poorly differentiated cancers (Fig. 45.27). There is a significant relationship between level of differentiation and prognosis. The tumor cells show varying degrees of cytological atypia. In addition, there are different subtypes of SCC such as verrucous (Fig. 45.28), basaloid (Fig. 45.29), adenosquamous, spindle cell, adenoid, and papillary depending on the morphology. Depth of invasion, pattern of invasion (Fig. 45.30), vascular invasion (Fig. 45.31), perineural invasion (Fig. 45.32), and level of immune response (Fig. 45.33) are some of the important histological parameters that the clinicians can use to plan the treatment for a given cancer as they are directly related to prognosis. Basaloid SCC has the worst histological features out of all the subtypes of OSCC and hence the poorest prognosis while verrucous carcinoma at the other end of the spectrum having favorable histological features and best prognosis.
Malignant melanoma is rare in the oral mucosa, and histopathology (Fig. 45.34) varies according to the type of melanoma, namely, superficially spreading, nodular, lentigo maligna, or acral lentiginous. Some melanomas do not produce melanin; hence, the term amelanotic melanoma is used for those tumors.
8 Treatment and Prognosis of Oral Cancer
Oral cancer is a major cause of morbidity and mortality in patients with head and neck cancer. Even though the treatment modalities have improved over the period, outcomes of the oral cancer management remain stagnant with only around 5% improvement in overall survival in the last two decades. Surgical resection remains as the primary treatment modality for the management of oral cancer, but several areas in the decision-making of the management including workup, management of the primary tumors, neck metastasis, and adjuvant therapy are not straightforward. Radiotherapy is also considered as a primary treatment modality, and recent advances in radiotherapy have helped to improve the outcomes for patients by reducing side effects and complications of radiotherapy. Recently, chemotherapy and immunotherapy specially the addition of cetuximab have shown promising results with minimal side effects, but it still remains only as adjuvant therapy. Advances in reconstruction of the resected area by microvascular free flaps have extended the limits of resection and help greatly in improving the functional outcome and esthetics and thereby the quality of life of the patients (Figs. 45.35, 45.36, 45.37, 45.38, 45.39, 45.40, 45.41, 45.42, 45.43, and 45.44). Unfortunately, the advances in the treatment have not led to significant survival benefit in oral cancers (Chinn and Myers 2015).
Natural or herbal plants are rich in antioxidants which have the ability of reducing or reversing DNA damage seen in oral cancer cells. Different extracts of such plants have shown some promising results with in vitro and in vivo studies (Illeperuma et al. 2019; Heein et al. 2017).
The cost of management of oral cancer patients in the developing world is extremely high. This has negative impacts on the economy of individual families as well as on national economy. Early identification can reduce the cost of management of oral cancer significantly (Amarasinghe et al. 2019).
9 Prognostic Markers of Oral Cancer
Multifactorial etiology of the oral cancer with some well-established causative factors such as tobacco, areca nut, and human papilloma virus has been clearly identified. Prognosis of oral cancer is determined by multiple factors. These prognostic factors include clinical and histopathological factors and molecular markers. A single factor alone cannot influence the prognosis of oral cancer, and final prognosis depends on the combination of all factors.
Clinical prognostic markers of oral cancer include age, gender, race, habits, nutritional status, medical condition of the patient, anatomical site and size of the cancer, surgical margins of the resection, as well as lymph node involvement, their number, size, and location (Rajapakshe et al. 2015; Siriwardena et al. 2015a, b; Dissanayaka et al. 2012). Histopathological prognostic factors include tumor subtype, level of differentiation, perineural invasion, vascular invasion, host immune response, pattern of invasive tumor front, depth of invasion, number of positive lymph nodes, presence of extracapsular spread in lymph nodes, increased mitosis, and presence of abnormal mitosis (Siriwardena et al. 2018; De Silva et al. 2018).
There are several molecular markers that may predict prognosis of oral cancer. There are angiogenesis-related factors such as vascular endothelial growth factor (VEGF), epidermal growth factor receptor, transforming growth factor alpha, HIF-1apha, expression of various combinations of cytokeratin, and many more (Tilakaratne 2012, Tilakaratne and Nissanka-Jayasooriya 2011; Siriwardena et al. 2008). Dysregulation of different types of RNA is considered as important molecular change in the carcinogenesis of oral cancer. Both micro-RNA (Mic-RNAs) and long noncoding RNA (Inc-RNAs) have been considered. High or low expression of RNAs could serve as a tissue-specific biomarker associated with clinicopathological features and survival of oral cancer. They can be used as possible therapeutic targets, and this needs further research (Pentenero et al. 2019a, b).
References
Amarasinghe H, Jayasinghe R, Dharmagunawardene D et al (2019) Economic burden of managing oral cancer patients in Sri Lanka. BMJ Open 9:e027661. https://doi.org/10.1136/bmjopen-2018-027661
Bray F, Ferlay J, Soerjomataram I et al (2018) Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: A Cancer Journal for Clinicians 68:394–424. https://doi.org/10.3322/caac.21492
Chinn SB, Myers JN (2015) Oral cavity carcinoma: current management, controversies, and future directions. J Clin Oncol 33(29):3269–3276. https://doi.org/10.1200/JCO.2015.61.2929
De Silva RK, Siriwardena BSMS, Samaranayaka A et al (2018) A model to predict nodal metastasis in patients with oral squamous cell carcinoma. PLoS One 13(8):e0201755. https://doi.org/10.1371/journal.pone.0201755
Dissanayaka WL, Pitiyage G, Kumarasiri PVR et al (2012) Clinical and histopathological parameters in Survival of oral squamous cell carcinoma. Oral Surg Oral Med Oral Pathol Oral Radiol 113(4):518–525
Dissanayake WL, Tilakaratne WM (2011) A histopathologic comparison between synchronous and single primary oral squamous cell carcinomas. In Reply. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 111(1):9–10
Heein Y, Junhee P, Kwang-Kyun P et al (2017) Methanol extract of Holarrhena antidysenterica bark inhibits the growth of human oral squamous cell carcinoma cells and osteoclastogenesis of bone marrow macrophages. Evid Based Complement Alternat Med 6:1–8
Illeperuma R, Bandara K, Kyeong KD et al (2019) Antioxidant rich tropical herbs to combat areca-nut induced OPMDs. Oral Surg Oral Med Oral Pathol Oral Radiol 128(1): e80–e81
Jayasooriya PR, Kurose K, Tera M et al (2003) Human papillomavirus in oral cancer from Sri Lanka: prevalence and relationship with clinico-pathological parameters. Jpn Oral Med Pathol 8:45–50
Pentenero M, Bowers L, Jayasinghe R et al (2019a) Functional pathways involving differentially expressed lncRNAs in oral squamous cell carcinoma. Oral Diseases 25(Suppl. 1):79–78. https://doi.org/10.1111/odi.13051
Pentenero M, Bowers L, Jayasinghe R et al (2019b) Clinical evidence of differential expression of lncRNAs in oral squamous cell carcinoma: a scoping review. Oral Dis 25(Suppl. 1):88–101. https://doi.org/10.1111/odi.13076
Rajapakshe RMAR, Pallegama RW, Jayasooriya PR et al (2015) A retrospective analysis to determine factors contributing to the survival of patients with oral squamous cell carcinoma. J Cancer Epidemiol 39(3):360–366
Siriwardena BSMS, Kudo Y, Ogawa I, Tilakaratne WM, Takata T (2008) VEGF-C is associated with lymphatic status and invasion in oral cancer. J Clin Pathol. 61(1):103–108
Siriwardena BSMS, Rasnayaka RMSGK, Masood YMM et al (2015a) A predictive model of oral cancer metastasis for different cancer sites and age groups. J Invest Clin Dent 6:1–5
Siriwardena BSMS, Jayathilake DSY, Pitakotuwage TN et al (2015b) Demographic and histopathological differences of oral squamous cell carcinoma; analysis of 4394 cases from Sri Lanka. J Clin Exp Oncol 4:4
Siriwardena BSMS., Rambukewela IK, Pitakotuwage TN et al (2018) A predictive model to determine the pattern of nodal metastasis in oral squamous cell carcinoma. Biomed Res Int 2018:8925818. https://doi.org/10.1155/2018
Sri Lanka Cancer Registry 2005, 2010, 2011 and 2014 (provisional), National Cancer Control Program, Ministry of Health, Sri Lanka
Tilakaratne WM (2012) Oral Cancer and Precancer; Novel markers in malignant transformation and prognosis. Sri Lanka J Med 21(2):12–21
Tilakaratne WM, Nissanka-Jayasooriya EH (2011) Value of HIF-1alpha as an independent prognostic marker in oral squamous cell carcinoma. Expert Rev Mol Diagn 11(2):145–147
Warnakulasuriya S. (2009) Causes of oral cancer—an appraisal of controversies. Br Dent J 207(10):471–475
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Jayasinghe, R.D., Tilakaratne, W.M. (2021). Oral Cancer. In: Ranawaka, R.R., Kannangara, A.P., Karawita, A. (eds) Atlas of Dermatoses in Pigmented Skin. Springer, Singapore. https://doi.org/10.1007/978-981-15-5483-4_45
Download citation
DOI: https://doi.org/10.1007/978-981-15-5483-4_45
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-15-5482-7
Online ISBN: 978-981-15-5483-4
eBook Packages: MedicineMedicine (R0)