Abstract
Neutrophilic dermatoses are heterogeneous group of cutaneous inflammatory disorders characterized by sterile, predominantly neutrophilic infiltrate on histopathology. Pyoderma gangrenosum was the first ND to be reported in the literature in 1930, and other conditions which are included in this disorder are Sweet syndrome, neutrophilic eccrine hidradenitis, Behcet disease, bowel-associated dermatosis-arthritis syndrome, rheumatoid neutrophilic dermatitis, and adult Still disease.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
Keywords
- Neutrophilic dermatoses
- Pyoderma gangrenosum
- Pyodermatitis-pyostomatitis vegetans
- Behcet’s disease
- Sweet syndrome
- Subcorneal pustular dermatosis
1 Introduction
Neutrophilic dermatoses (ND) are heterogeneous group of cutaneous inflammatory disorders characterized by sterile, predominantly neutrophilic infiltrate on histopathology. The pathogenesis of ND remains incompletely understood. Existing evidence points to three main processes: altered expression of inflammatory effect or molecules, abnormal neutrophil function, and genetic predisposition.
The morphology of cutaneous lesions associated with these disorders is heterogeneous, which renders diagnosis challenging. Pyoderma gangrenosum (PG) was the first ND to be reported in the literature in 1930 and other conditions which are included in this disorder are Sweet syndrome (SS), neutrophilic eccrine hidradenitis (NEH), Behcet disease (BD), bowel-associated dermatosis-arthritis syndrome, rheumatoid neutrophilic dermatitis, and adult Still disease.
Diagnosis of ND requires thorough evaluation to exclude diseases that mimic these disorders.
While some neutrophilic dermatoses may resolve spontaneously, most require treatment to achieve remission. Delays in diagnosis and treatment can lead to significant patient morbidity and even mortality.
-
1.
A 38-year-old man came with multiple painful ulcers on the left leg for more than 10 years. He was investigated for chronic diarrhea and was on treatments for last 2 years (Fig. 12.1).
-
(a)
What is the most probable clinical diagnosis of this presentation?
-
(b)
What is the possible underline cause?
-
(c)
How do you investigate?
-
(a)
Answer
-
(a)
Pyoderma gangrenosum (PG).
-
(b)
The most possible disease association in this patient is inflammatory bowel disease (IBD)-Crohn disease or ulcerative colitis.
-
(c)
Skin biopsy for histopathology-histopathology may vary depending on the age of the ulcer, and the site of the biopsy specimen was taken. It will often demonstrate pandermal infiltration of predominantly neutrophils with dermal edema.
Skin biopsy for tissue culture—bacterial, fungal, and mycobacterial to exclude infective causes
Gastrointestinal evaluation—USS of abdomen, colonoscopy to confirm IBD
Duplex ultrasonography and ankle-brachial index testing are helpful to evaluate venous insufficiency and peripheral arterial disease.
-
2.
A 38-year-old woman referred by rheumatologist for dermatological evaluation for a painful non-healing ulcer on the left foot for more than 2 years. It started spontaneously and enlarged slowly with no response to conventional treatment. She was investigated for photosensitive skin rash and arthritis and was on treatment for last 3 years (Fig. 12.2).
-
(a)
What is the most likely diagnosis?
-
(b)
What are the differential diagnoses?
-
(c)
How do you investigate?
-
(d)
What are the treatment modalities?
-
(a)
Answer
-
(a)
Pyoderma gangrenosum (PG) in a patient with SLE
-
(b)
Small to medium vessel vasculitis, infective ulcer like tuberculosis
-
(c)
FBC, ESR, CRP
Antinuclear antibody, anti-Ds-DNA, rheumatoid factor (RF), antineutrophil.
cytoplasmic antibody (ANCA) to evaluate underline rheumatological disease
Skin biopsy for histology—to rule out vasculitis or neoplastic process
Skin biopsy for tissue culture for bacteria and mycobacteria to exclude infective causes such as tuberculosis
-
(d)
Systemic corticosteroids with steroid-sparing systemic agents: cyclosporine, azathioprine and tumor necrosis factor-a inhibitors
-
3.
A 43-year-old woman came with this painful ulcer over the left breast for 6 months which increased rapidly despite treatments. Examination did not reveal breast lump but left axillary nodes were enlarged. She was on long-term treatment for diabetes mellitus and complained of recent loss of appetite and weight (Fig. 12.3).
-
(a)
What is your clinical diagnosis?
-
(b)
What are the differential diagnoses?
-
(c)
How do you investigate?
-
(a)
Answer
-
(a)
Pyoderma gangrenosum
-
(b)
Paget’s disease of the breast, breast carcinoma infiltrating the skin, cutaneous tuberculosis
-
(c)
Erythrocyte sedimentation rate and C-reactive protein—nonspecific but often elevated
Skin biopsy specimen for histology to confirm PG and to rule out breast carcinoma or Paget’s disease
Skin biopsy for tissue culture; bacterial, fungal, and mycobacterial
Mammogram to exclude breast carcinoma
Chest X-ray to see lung involvement in CA breast or TB
-
4.
A 14-year-old boy referred by consultant gastroenterologist for dermatological evaluation for multiple painful pustular lesions on the lower lip for 10 days. Rest of the oral cavity examination showed multiple similar lesions on oral mucosa with areas of mucosal thickening. He also had fever, arthralgia and loose stools for last 1 week. He was on treatment for Chron’s disease for 1 year with salphazalazine but off treatment for last 2 months (Fig. 12.4).
-
(a)
What is the most likely diagnosis in this child?
-
(b)
What are the other possible diagnoses?
-
(c)
What investigations you want to order to diagnose the most possible underline cause?
-
(d)
How do you manage?
-
(a)
Answer
-
(a)
Pyodermatitis-pyostomatitis vegetans.
-
(b)
Pemphigus, aphthous stomatitis, Herpes simplex infection, drug-induced mucositis.
-
(c)
Mucosal biopsy for histopathology—Pyostomatitis will show intraepidermal and/or subepithelial abscesses with many eosinophils. Deeper tissue will show mixed infiltrate with neutrophils and eosinophils.
Immunofluracence both direct and indirect will be negative in most except pemphigus vulgaris
Blood culture—bacterial, fungal, mycobacterial screening to exclude infective causes
Gastrointestinal evaluation—USS of abdomen, colonoscopy to confirm IBD
Full blood count, ESR, CRP
Tzank smear to exclude herpes infection
-
(d)
Treatment for IBD will settle the ulcers. Topical steroid application and antiseptic mouth wash will help in some.
-
5.
A 20-year-old man came with recurrent painful ulcers on lips, tongue, and oral mucosa for 2 years. No fever, arthritis, or associated skin lesions. But he had few painful genital ulcers several times and healed with topical antibiotics. No significant history other than this illness, not on medications recently (Fig. 12.5).
-
(a)
What are the differential diagnoses?
-
(b)
How do you investigate to arrive at diagnosis of most possible diagnosis?
-
(a)
Answer
-
(a)
Behcet disease (BD), aphthous ulcers associate with IBD, herpes simplex infection, pemphigus vulgaris.
-
(b)
Pathergy test—A positive pathergy reaction is a sign of BD. But it is not pathognomonic, as it can also occur in patients with pyoderma gangrenosum, Crohn disease, or genital herpes infection.
Ophthalmological examination—Look for posterior uveitis (retinal vasculitis), anterior uveitis, hypopyon (pus in the anterior chamber of the eye) and features such as cataract, glaucoma, and neovascular lesions.
Skin or mucosal biopsy for histopathology—Characteristic histopathological features are neutrophilic vascular reaction with endothelial swelling, extravasation of erythrocytes, and leukocytoclasia and leukocytoclastic vasculitis in BD.
-
6.
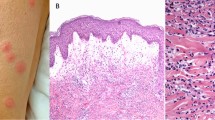
A 30-year-old man came with painless skin nodules for 1 week with high fever and arthralgia. No significant history or not taken any medication recently. Investigations showed high ESR and CRP with elevated white cell count and neutrophilia in blood film (Fig. 12.6).
-
(a)
What is the most likely diagnosis?
-
(b)
What are the differential diagnoses?
-
(c)
How do you investigate to arrive at diagnosis?
-
(a)
Answer
-
(a)
Sweet syndrome (SS)
-
(b)
Erythema multiforme, cutaneous lymphoma, tuberculids
-
(c)
Investigations
Complete blood cell count with differential which show elevated white cell count and neutrophilia.
C-reactive protein and erythrocyte sedimentation rate are often elevated.
A sterile skin biopsy specimen for tissue culture to exclude bacterial, fungal, and mycobacterial etiology, Mantoux test, chest X-Ray.
Herpes virus—serum immunoglobulins.
Deep skin biopsy for histopathology consistent with SS and to exclude infection.
-
7.
A 60-year-old woman who is diagnosed as having acute myeloblastic leukemia came with asymptomatic skin nodules over limbs and trunk for 2 days. No fever or arthralgia. Investigations showed high ESR and anemia (Fig. 12.7).
-
(a)
What are the most possible diagnoses?
-
(b)
How do you differentiate and manage?
-
(a)
Answer
-
(a)
Sweets syndrome (atypical form), leukemia cutis, papular urticaria, cutaneous TB.
-
(b)
Investigations.
Complete blood cell count with differential to exclude infections or to confirm hematological malignancy.
C-reactive protein and erythrocyte sedimentation rate are often elevated in TB and malignancy.
Skin biopsy for histopathology consistent with SS, exclude leukemic deposits and to exclude infection.
Patients should receive screening for metastasis.
-
8.
A 67-year-old woman came with fever for 3 days, sudden onset painful vesicobullous lesions on feet and arthralgia. She was on treatments for hypertension and bronchial asthma for a long time, and antibiotics for chest infection for last 1 week. Investigations revealed elevated ESR and CRP (Fig. 12.8).
-
(a)
What is the most probable clinical diagnosis?
-
(b)
What are the differential diagnoses?
-
(c)
How do you investigate this patient?
-
(a)
Answer
-
(a)
Bullous form of Sweet syndrome (SS).
-
(b)
Bullous erythema multiforme, papular urticaria, tuberculids (papular necrotic TB).
-
(c)
Investigations.
Complete blood cell count with differential to exclude infections or to confirm hematological malignancy
A sterile skin biopsy for tissue culture for bacterial, fungal, and mycobacterial etiology
Chest X ray, Mantoux test
USS abdomen or CT abdomen and chest for screening for malignancy
Deep skin biopsy for histopathology consistent with SS and to exclude infection like TB
-
9.
A 35-year-old girl with Down’s syndrome came with asymptomatic multiple pustular lesions mainly over the trunk, axillae, and groins for 4 weeks. No constitutional symptoms like fever, arthralgia, or GI symptoms. She was on treatments for diabetes, hypertension, and dyslipidemia for 3 years and had not change drugs recently (Fig. 12.9).
-
(a)
What are your differential diagnoses?
-
(b)
How do you investigate?
-
(c)
What are the treatment options in this patient?
-
(a)
Answer
-
(a)
Subcorneal pustular dermatosis (SPD), impetigo, pustular psoriasis, IgA pemphigus
-
(b)
Investigations
Skin biopsy—biopsy from early pustules will show perivascular inflammatory infiltrate with occasional eosinophils. In comparison to IgA Pemphigus where the pustules are seen subcorneally, in SPD the pustules sit on the surface of the epidermis.
Immunofluorescence for IgA autoantibodies—in the classical SPD form, it is negative but positive in IgA pemphigus.
Bacterial culture of skin swabs should be taken to exclude infection.
-
(c)
Dapsone 50–150 mg daily is the treatment of choice in SPD. Topical or oral corticosteroids may be useful. Acitretin can use if not respond to dapsone. Narrow-band UVB phototherapy has been very effective in some patients.
2 Pyoderma Gangrenosum (PG)
PG is a rare non-infectious neutrophilic dermatosis commonly associated with underlying systemic disease. It can present in many forms and usually divide in to two groups.
-
1.
Classical ulcerative form
-
2.
Atypical forms—parastomal, pustular, bullous, granulomatous, superficial
It can affect any age, but most commonly affects adults between 40 and 60 years. PG is common in women in 3:1 ratio.
Associations
Inflammatory bowel disease (IBD) is the most common association where 20–30% of patients may get PG, rheumatoid arthritis, and other sero-negative arthritis, hematological malignancy, monoclonal gammopathy, and other visceral malignancies are less commonly associated.
Clinical Features
Classical ulcerative PG is the most common morphological variant and usually associated with IBD, rheumatoid arthritis, and monoclonal gammopathies. It typically presents as inflammatory and tender nodule or pustules that rapidly expands into painful ulcers. The ulcer is typically sharply marginated with violaceous, undermined borders, and overhanging epidermal edge. As the ulcers heal, they usually develop a cribriform scarring. PG can occur as single or multiple and most commonly occurs on the lower extremities. But the lesions can occur anywhere of the body. New lesions may also develop after minor trauma to the skin in 20–30% of patients (positive pathergy test).
Bullous PG typically start as rapidly developing blue-gray bullae that quickly erode leaving behind superficial ulcers. They usually seen on face, head, or upper extremities and can associated with hematologic malignancies.
Differential Diagnosis
Vasculitides, thrombophilic conditions, malignancies, and infections.
Diagnosis is based on typical clinical features and the exclusion of those conditions which can cause cutaneous ulcerations.
Investigations
Histopathology from a skin biopsy is not diagnostic in PG but is frequently performed to exclude other conditions that may mimic PG. Histopathology may vary depending on the age of the ulcer and where the biopsy specimen was obtained. Early lesions will usually show neutrophilic pustules but in general the features are non-specific.
Infective causes to be excluded sending tissue for culture for bacterial, atypical mycobacterial, viral, and fungal pathogens.
A thorough work-up should include blood count, biochemical profile for SLE, chest X-ray, endoscopy, bone marrow aspirate, CT scan chest, abdomen, and pelvis.
Treatments
Systemic corticosteroids are the main stay of treatment for PG. Steroid-sparing systemic agents include cyclosporine and tumor necrosis factor-a inhibitors may need. Treatment for underline causative disease is mandatory. Wound care and local therapies also important (Figs. 12.10, 12.11 and 12.12) .
(a) Pyoderma gangrenosum, classical ulcerative variant. A 21-year-old pregnant woman came with an ulcer on the right shoulder which enlarged rapidly over 2 weeks despite oral antibiotics. Note characteristic violaceous undermined edges. (b) Pyoderma gangrenosum showing dramatic response to 2 weeks of oral prednisolone. (c) Pyoderma gangrenosum healed with scarring (photographed by Dr. Ranthilaka R. Ranawaka)
3 Pyodermatitis-Pyostomatitis Vegetans
Pyostomatitis vegetans is a rare disorder which is usually present with multiple pustules and “snail track” superficial ulceration of oral mucosa and oral mucosal thickening (Fig. 12.4). This is commonly associated with IBD, particularly ulcerative colitis.
It can occur at any site of oral mucosa, although the tongue is less affected. This can affect any age but common in young adults and predilection in men. When skin lesions present, they appear as vesicular, pustular, or vegetative lesions, often in flexures.
Differential Diagnosis
Pemphigus vegetans with verrucous plaques studded with pustules in flexures.
Associations
Leukemia, lymphoma, diabetes, acne conglobata, hidradenitis suppurativa, immunosuppression, and malnourishment are also known to associate with it.
Investigations
Elevated peripheral blood eosinophilia and IgE levels
Histopathology
Shows intraepithelial and/or sub-epithelial abscesses containing large numbers of eosinophils.
DIF is usually negative.
Management is usually aimed for the treatment of gastrointestinal disease.
4 Behcet Disease (BD)
BD is a chronic multisystem inflammatory disorder that classically presents with a triad of recurrent symptoms oral ulcers, genital ulcers, and uveitis. It most often affects patients in their 20s and 30s, with an overall equal gender distribution.
Etiology of the disease remains unknown, although genetic factors, infectious agents, environmental pollution, immunological mechanisms, and endothelial and clotting factors have been implicated.
Clinical Features
Oral aphthous ulcers are the most common presentation and commonly involve the lips, buccal mucosa, tongue, and soft palate (Fig. 12.5). The lesions start as erythematous papules or vesiculo-pustules. They evolve into painful oval ulcers with rolled borders and a grayish yellow necrotic base. Genital ulcers of BD are similar in appearance but may be deeper and heal with scarring. Genital ulcers involve scrotum in males and labium majora in females mostly. Other cutaneous lesions associate with BD are erythema nodosum, papulo-pustular lesions, sweet syndrome or PG like lesions and thrombophlebitis, necrotizing venulitis, or cutaneous pathergy.
BD may have cause vascular, articular, gastrointestinal, neurologic, urogenital, pulmonary, and cardiac involvement. Ocular involvement is the major cause of morbidity in patients with BD. The most diagnostically relevant lesion is posterior uveitis, and it can lead to blindness.
Diagnosis
BD is a diagnosis of exclusion. The International Study Group for Behcet Disease listed criteria for diagnosis of it may useful in diagnosis.
Differential Diagnosis
Recurrent aphthous stomatitis, HLA-B27e-related diseases, IBD, and SLE.
Management
Treatment of BD should be tailored based on impact on the patient’s quality of life. Topical therapies may be adequate to control mild disease, while systemic therapies may be required to control severe disease. Colchicine is the first-line therapy with azathioprine, minocycline, TNF alpha antagonist, and interferon alpha also can use.
5 Sweet Syndrome (SS)
SS, also known as acute febrile neutrophilic dermatosis. It can affect any age but typically affects between the ages of 30 and 60 years and is more common in women.
SS may be categorized into three sub-types, classic, malignancy associated, and drug induced.
Classical SS
This is characterized by the abrupt onset of painful erythematous plaques or nodules in associate with constitutional symptoms like fever and arthralgia. Many clinical variants of cutaneous lesions described are pustular, bullous, cellulitis-like, or necrotizing lesions on any part of the body. Targetoid lesions have been reported in some patients.
Malignancy-Associated SS
Old age, vesiculo-bullous morphology in associated with leukopenia, anemia, thrombocytopenia, elevated ESR, the absence of arthralgia is seen in this type of SS. A wide range of malignancies described in association with SS, e.g., hematologic malignancies and myeloproliferative or myelodysplastic disorders, most notably AML and myelodysplastic syndrome.
Drug-Induced SS
About 1–27% of cases of SS is due to drugs. G-CSF is the most associated drug with SS; however numerous other medications can cause it, e.g., propylthiouracil, novel antineoplastic, and immunologic agents.
Diagnosis
Careful history taking with attention to fever and other constitutional symptoms is important. Exclude upper respiratory tract or other infectious conditions. Important to find recent vaccinations, malignancies and inflammatory disorders, drug exposure, and pregnancy status in history.
Investigations
Complete blood cell count with differential to exclude infections or to confirm paraproteniemia or hematological malignancy. Bone marrow biopsy may needed in some patients.
Elevated CRP and ESR is common.
A sterile skin biopsy specimen for tissue culture to exclude bacterial, fungal, and mycobacterial etiology, and deep skin biopsy for histopathology is useful.
All patients should receive age-appropriate malignancy screening.
Management
Treatment should be tailored to the individual patient. Systemic corticosteroids are the standard for SS. Steroid-sparing systemic agents include dapsone, colchicine, and potassium iodide may need in some (Figs. 12.13–12.17).
6 Subcorneal Pustular Dermatosis (SPD)
This is a rare neutrophilic dermatosis, usually presenting with acute onset sterile subcorneal pustules affecting the flexures of the trunk and proximal extremities. The flexures, including axillae, groins, submammary area, are commonly affected and it usually spears the face and mucous membranes.
Clinical Features
It usually affects adults aged 40–60 years and is more commonly seen in women. Clinically SPD presents as discrete flaccid pustules or grouped vesicles predominantly in flexures. Annular and serpiginous lesions can occur. Evantual rupture of lesions leaves collarette of scale. Mucosa can rarely involve.
Associations
SPD can associate with benign monoclonal gammopathy, IBD, multiple myeloma, lymphomas, rheumatoid arthritis, and systemic lupus erythematosus.
Investigations
Biopsy from early lesions shows a perivascular inflammatory infiltrate with occasional eosinophils. The pustules sit on the surface of the epidermis rather than within it. Spongiosis and spongiotic pustules are absent, and acantholysis is only seen in old lesions.
Immunofluorescence in the classical form is negative.
Treatment
Dapsone 50–150 mg daily is the treatment of choice. Topical or oral corticosteroids may be useful. Acitretin can use if not responded to dapsone. Narrow-band UVB phototherapy has been very effective in some patients (Fig. 12.18).
References
Ashchyan HJ, Nelson CA, Stephen S et al (2018) Neutrophillic Dermatoses; Pyoderma gangrenosum and other bowel and arthritis associated neutrophilic dermatoses. J Am Acad Derm 79(6):1009–1022
Nelson CA, Stephen S et al (2018) Neutrophilic dermatoses pathogenesis, sweet syndrome, neutrophilic eccrine hidradenitis, and Behcet disease. J AM ACAD Derm 79:998–1000
Ormerod AD, Hampton PJ (2016) Neutrophilic dermatoses. In: Rook’s textbook of dermatology, vol 49, 9th edn. Wiley-Blackwell Science, UK, pp 1–17
Saede A, Ali L, Fazele A (2016) Pyostomatitis vegetans; a clue to diagnosis of silent Crohn’s disease. J Clin Diagn Res 10(12):ZD12
Zouboulis CC (2016) Adamantiades-Behçet disease. In: Rook’s textbook of dermatology, vol 48. Wiley-Blackwell Science, UK, pp 1–10
Author information
Authors and Affiliations
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2021 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Wijenayake, B.K.S. (2021). Neutrophilic Dermatoses. In: Ranawaka, R.R., Kannangara, A.P., Karawita, A. (eds) Atlas of Dermatoses in Pigmented Skin. Springer, Singapore. https://doi.org/10.1007/978-981-15-5483-4_12
Download citation
DOI: https://doi.org/10.1007/978-981-15-5483-4_12
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-15-5482-7
Online ISBN: 978-981-15-5483-4
eBook Packages: MedicineMedicine (R0)