Abstract
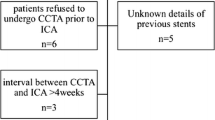
Coronary artery stenting has been an important therapeutic procedure for patients with coronary artery stenosis and the number of patients who received stenting is increasing. As a noninvasive method, coronary computed tomography angiography (CTA) has become increasingly used during the follow-up. However, beam-hardening artifacts, appearing as dark areas adjacent to metal stents, limit the diagnostic performance of cardiac CT, especially when the stent diameter is <3 mm. Recently, with the rapid technologic advances, dual-energy CT (DECT) has been applied in many clinical areas. With dual-energy CT, attenuation data from different energies are used to characterize materials, virtual monoenergetic images (VMI) and stent subtraction images can be used to improve the diagnostic performance of stent evaluation. In this chapter, based on a case, we will discuss the assessment of coronary stent by dual-energy CT imaging, and further possibly promising role of CT technology in coronary stent evaluation.
Access provided by Autonomous University of Puebla. Download chapter PDF
Similar content being viewed by others
5.1 Case of Coronary Stent
5.1.1 History
A 53-year-old male patient felt chest distress and chest pain lasting for an hour several days ago. He had a history of PCI a year ago and the stent was implanted in the proximal segment of left anterior descending artery (LAD). He was appointed to coronary CTA for suspected in-stent restenosis or coronary artery disease (CAD) progression.
Physical Examination
-
Blood pressure: 123/82 mmHg; Breathing rate: 18/min
-
Heart rate: 64 bpm without arrhythmia
Electrocardiograph
-
Standard 12-lead electrocardiograph (ECG) revealed no abnormality.
Laboratory
-
Serum myocardial enzyme spectrum showed negative results.
5.1.2 Imaging Examination
CT Images
Coronary CT angiography (CTA) was performed on dual-layer detector CT (Figs. 5.1, 5.2, and 5.3).
Conventional Coronary Angiography (Fig. 5.4)
5.1.3 Imaging Findings and Diagnosis
The coronary CTA images results showed the in-stent lumen patency of LAD was hard to diagnose because of beam-hardening artifacts (B26f). The curved multiplanar reconstruction of LAD on sharp convolution kernel (B46f) displayed the in-stent lumen of LAD better; there was no in-stent restenosis but there were noncalcified plaques in the proximal and middle segment of LAD, resulting in mild lumen stenosis. On virtual monoenergetic images, the window level and window width were set at 90 and 750, respectively; it was obvious that 100 keV image displays the stent better than conventional images and there was no ISR. The invasive coronary angiography images confirmed that there was no ISR but moderate stenosis in middle LAD, which may contribute to the symptoms.
5.1.4 Management
-
Conventional medical therapy for CAD and clinical follow-up
5.2 Discussion
Coronary artery stenting has been widely introduced into clinical practice. Patients who undergo PCI experience a reduction or disappearance of symptoms. However, caused by intimal hyperplasia, in-stent restenosis is one of the main limitations of stent placement. Usually, invasive coronary angiography is performed when ISR is clinically suspected. Accurate evaluation of stents has always been a challenge on coronary CTA. Recently, with the development of dual-energy CT, the in-lumen visibility of small stents and the diagnostic performance of coronary CTA have been improved. On coronary CTA, stent patency can be visually evaluated. If ISR happens, a darker area between the stent and the enhanced lumen can be found. Image quality can be quantified by image noise, visible lumen diameter, and in-stent attenuation difference.
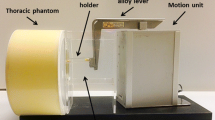
5.3 Current Technical Status and Applications of CT
In order to acquire the dual-energy data set, various technical approaches have been developed, including two temporally sequential scans, rapid switching of X-ray tube potential, multilayer detector, dual X-ray sources, and photon-counting detectors [1]. By these approaches, image sets can be created in the projection domain or in the image domain. DECT allows the creation of virtual monoenergetic reconstructions in which attenuation data approximate data that would be obtained with a mono-energy X-ray beam. Images can be created from 40 to 200 keV. VMI reconstructions at low energy allow for contrast dose reduction and image noise reduction while reconstructions at a high energy level can minimize the beam-hardening artifact [2, 3]. The visible lumen diameter, in-stent attenuation difference, image quality of VMI are better than conventional images [4].
Coronary stent subtraction CT imaging is another way to improve the diagnostic performance of coronary CTA. By subtracting non-contrast images from contrast-enhanced images, stents can be eliminated. Misregistration artifacts is a major limitation of stent subtraction CT imaging due to patient movement or changing HR [5]. With the development of dual-energy technology, iodine data can be subtracted from contrast-enhanced images to create virtual non-enhanced images, subtraction between virtual non-enhancement images and monochromatic or mixed-energy images could yield equally improved in-stent lumen visibility and diagnostic accuracy without misregistration artifact.
DECT with various reconstruction images help in the accurate evaluation of stents.
5.4 Key Points
-
In-stent restenosis is one of the main limitations of PCI treatment.
-
DECT with virtual monoenergetic images and stent subtraction images help to evaluate in-stent lumen more accurately in CTA.
References
McCollough CH, Leng S, Yu L, Fletcher JG. Dual- and multi-energy CT: principles, technical approaches, and clinical applications. Radiology. 2015;276(3):637–53. https://doi.org/10.1148/radiol.2015142631.
Secchi F, De Cecco CN, Spearman JV, Silverman JR, Ebersberger U, Sardanelli F, et al. Monoenergetic extrapolation of cardiac dual energy CT for artifact reduction. Acta Radiol. 2015;56(4):413–8. https://doi.org/10.1177/0284185114527867.
Yu L, Leng S, McCollough CH. Dual-energy CT-based monochromatic imaging. AJR Am J Roentgenol. 2012;199(5 Suppl):S9–s15. https://doi.org/10.2214/ajr.12.9121.
Hickethier T, Baessler B, Kroeger JR, Doerner J, Pahn G, Maintz D, et al. Monoenergetic reconstructions for imaging of coronary artery stents using spectral detector CT: in-vitro experience and comparison to conventional images. J Cardiovasc Comput Tomogr. 2017;11(1):33–9. https://doi.org/10.1016/j.jcct.2016.12.005.
Fuchs A, Kuhl JT, Chen MY, Helqvist S, Razeto M, Arakita K, et al. Feasibility of coronary calcium and stent image subtraction using 320-detector row CT angiography. J Cardiovasc Comput Tomogr. 2015;9(5):393–8. https://doi.org/10.1016/j.jcct.2015.03.016.
Author information
Authors and Affiliations
Corresponding author
Editor information
Editors and Affiliations
Rights and permissions
Copyright information
© 2020 Springer Nature Singapore Pte Ltd.
About this chapter
Cite this chapter
Xu, C., Wang, Y. (2020). Dual-Energy Evaluation of Coronary Artery Stent. In: Jin, Zy., Lu, B., Wang, Y. (eds) Cardiac CT. Springer, Singapore. https://doi.org/10.1007/978-981-15-5305-9_5
Download citation
DOI: https://doi.org/10.1007/978-981-15-5305-9_5
Published:
Publisher Name: Springer, Singapore
Print ISBN: 978-981-15-5304-2
Online ISBN: 978-981-15-5305-9
eBook Packages: MedicineMedicine (R0)